Development Project Stakeholder Map for Youth Mental Health
VerifiedAdded on 2020/04/07
|6
|1966
|50
Project
AI Summary
This project analyzes the development of a National Youth Mental Health Foundation, focusing on stakeholder mapping, patient assessment, and system design. It begins with an examination of internal and external stakeholders, including healthcare case workers, administrative staff, clinicians, and patients, along with the roles and responsibilities of each group. A questionnaire is presented to gather information about patient problems, health history, and personal relationships to aid in developing individualized healthcare plans. The project also includes use case diagrams illustrating interactions within the system, such as new patient intake, family member inquiries, and emergency service scenarios. A sample use case description provides a detailed scenario of a patient requiring emergency care, outlining the process from initial contact with a case worker to clinician examination and treatment recommendations. The project references several scholarly articles to support its analysis and recommendations.
National Youth Mental Health Foundation Development Project
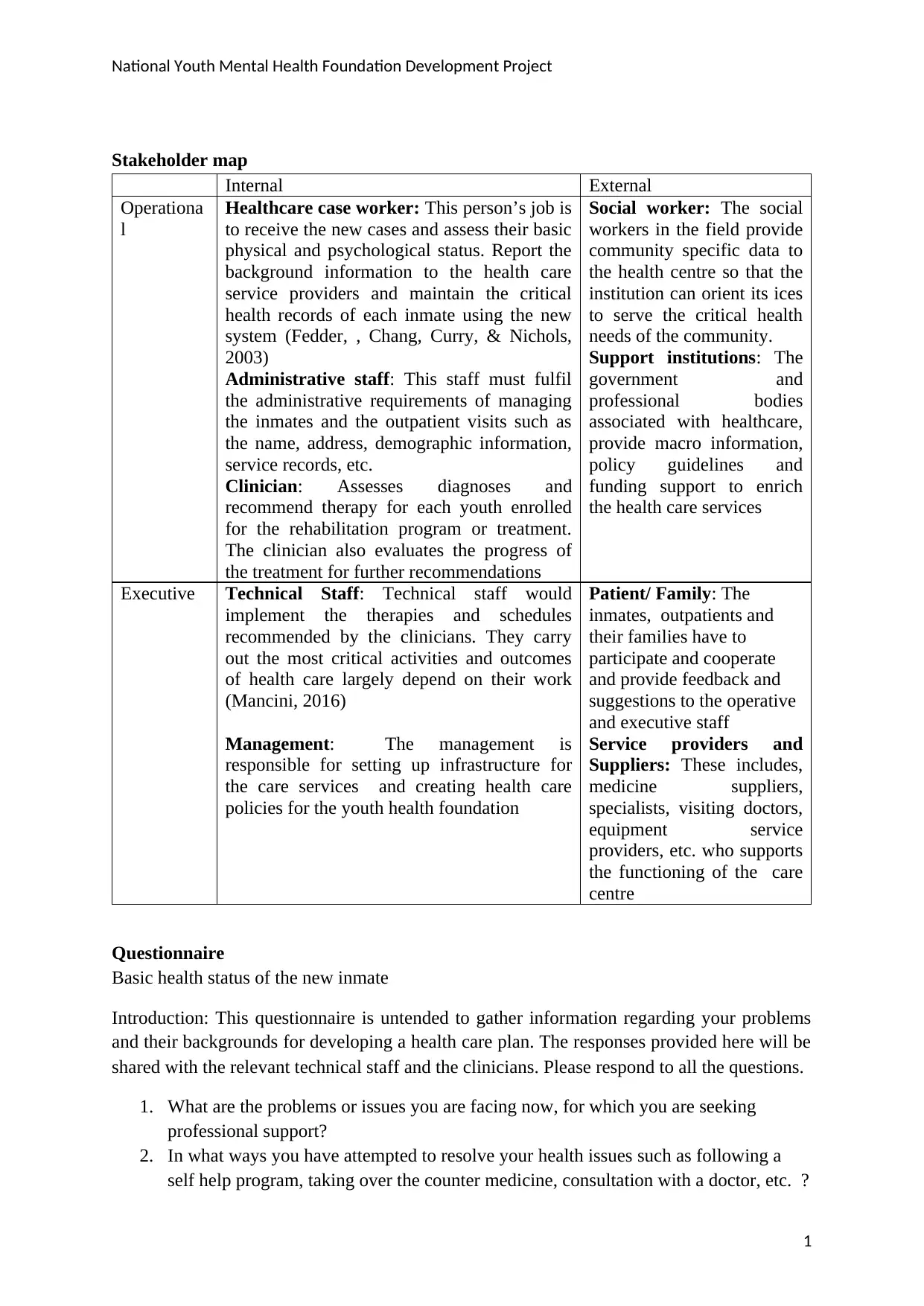
Stakeholder map
Internal External
Operationa
l
Healthcare case worker: This person’s job is
to receive the new cases and assess their basic
physical and psychological status. Report the
background information to the health care
service providers and maintain the critical
health records of each inmate using the new
system (Fedder, , Chang, Curry, & Nichols,
2003)
Administrative staff: This staff must fulfil
the administrative requirements of managing
the inmates and the outpatient visits such as
the name, address, demographic information,
service records, etc.
Clinician: Assesses diagnoses and
recommend therapy for each youth enrolled
for the rehabilitation program or treatment.
The clinician also evaluates the progress of
the treatment for further recommendations
Social worker: The social
workers in the field provide
community specific data to
the health centre so that the
institution can orient its ices
to serve the critical health
needs of the community.
Support institutions: The
government and
professional bodies
associated with healthcare,
provide macro information,
policy guidelines and
funding support to enrich
the health care services
Executive Technical Staff: Technical staff would
implement the therapies and schedules
recommended by the clinicians. They carry
out the most critical activities and outcomes
of health care largely depend on their work
(Mancini, 2016)
Management: The management is
responsible for setting up infrastructure for
the care services and creating health care
policies for the youth health foundation
Patient/ Family: The
inmates, outpatients and
their families have to
participate and cooperate
and provide feedback and
suggestions to the operative
and executive staff
Service providers and
Suppliers: These includes,
medicine suppliers,
specialists, visiting doctors,
equipment service
providers, etc. who supports
the functioning of the care
centre
Questionnaire
Basic health status of the new inmate
Introduction: This questionnaire is untended to gather information regarding your problems
and their backgrounds for developing a health care plan. The responses provided here will be
shared with the relevant technical staff and the clinicians. Please respond to all the questions.
1. What are the problems or issues you are facing now, for which you are seeking
professional support?
2. In what ways you have attempted to resolve your health issues such as following a
self help program, taking over the counter medicine, consultation with a doctor, etc. ?
1
Stakeholder map
Internal External
Operationa
l
Healthcare case worker: This person’s job is
to receive the new cases and assess their basic
physical and psychological status. Report the
background information to the health care
service providers and maintain the critical
health records of each inmate using the new
system (Fedder, , Chang, Curry, & Nichols,
2003)
Administrative staff: This staff must fulfil
the administrative requirements of managing
the inmates and the outpatient visits such as
the name, address, demographic information,
service records, etc.
Clinician: Assesses diagnoses and
recommend therapy for each youth enrolled
for the rehabilitation program or treatment.
The clinician also evaluates the progress of
the treatment for further recommendations
Social worker: The social
workers in the field provide
community specific data to
the health centre so that the
institution can orient its ices
to serve the critical health
needs of the community.
Support institutions: The
government and
professional bodies
associated with healthcare,
provide macro information,
policy guidelines and
funding support to enrich
the health care services
Executive Technical Staff: Technical staff would
implement the therapies and schedules
recommended by the clinicians. They carry
out the most critical activities and outcomes
of health care largely depend on their work
(Mancini, 2016)
Management: The management is
responsible for setting up infrastructure for
the care services and creating health care
policies for the youth health foundation
Patient/ Family: The
inmates, outpatients and
their families have to
participate and cooperate
and provide feedback and
suggestions to the operative
and executive staff
Service providers and
Suppliers: These includes,
medicine suppliers,
specialists, visiting doctors,
equipment service
providers, etc. who supports
the functioning of the care
centre
Questionnaire
Basic health status of the new inmate
Introduction: This questionnaire is untended to gather information regarding your problems
and their backgrounds for developing a health care plan. The responses provided here will be
shared with the relevant technical staff and the clinicians. Please respond to all the questions.
1. What are the problems or issues you are facing now, for which you are seeking
professional support?
2. In what ways you have attempted to resolve your health issues such as following a
self help program, taking over the counter medicine, consultation with a doctor, etc. ?
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
National Youth Mental Health Foundation Development Project
3. How long have you been suffering from the problems you have mentioned above?
4. How do these problems affect your life?
5. Name the people in your family and indicate the degree of closeness and intimacy you
have with them
6. Name friends, colleagues and peers who you are close with, and feel comfortable to
disclose your problems and issues with them
7. To what extent you feel satisfied with your life? Why do you feel so?
8. Describe your close relationships and provide evaluations regarding those
relationships?
9. What are your personal strengths and weaknesses?
10. What are your ambitions, aspirations and life goals?
11. What outcomes do you foresee from the programs of this health care centre?
12. What other information about you that the clinician or health care professionals
should know?
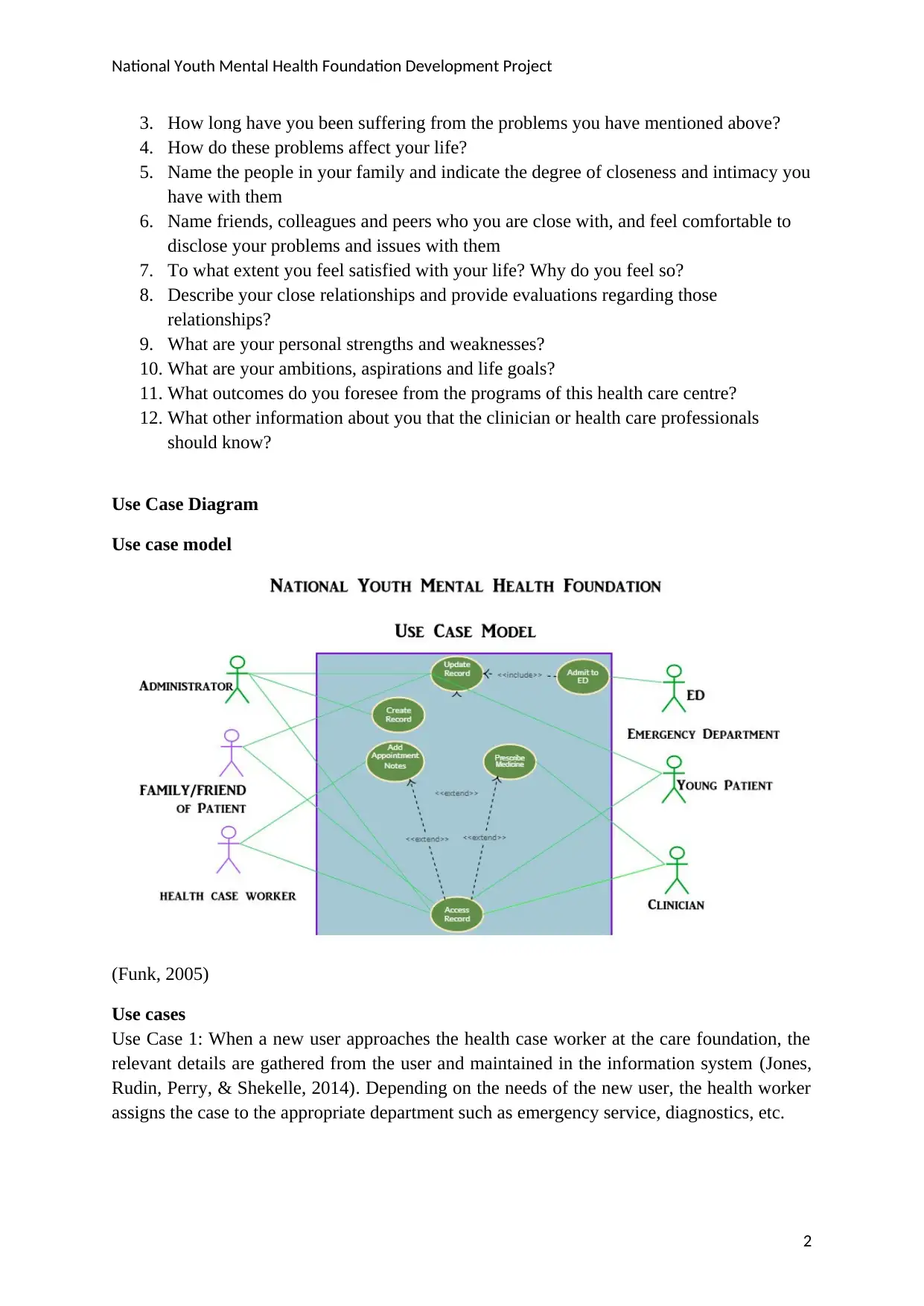
Use Case Diagram
Use case model
(Funk, 2005)
Use cases
Use Case 1: When a new user approaches the health case worker at the care foundation, the
relevant details are gathered from the user and maintained in the information system (Jones,
Rudin, Perry, & Shekelle, 2014). Depending on the needs of the new user, the health worker
assigns the case to the appropriate department such as emergency service, diagnostics, etc.
2
3. How long have you been suffering from the problems you have mentioned above?
4. How do these problems affect your life?
5. Name the people in your family and indicate the degree of closeness and intimacy you
have with them
6. Name friends, colleagues and peers who you are close with, and feel comfortable to
disclose your problems and issues with them
7. To what extent you feel satisfied with your life? Why do you feel so?
8. Describe your close relationships and provide evaluations regarding those
relationships?
9. What are your personal strengths and weaknesses?
10. What are your ambitions, aspirations and life goals?
11. What outcomes do you foresee from the programs of this health care centre?
12. What other information about you that the clinician or health care professionals
should know?
Use Case Diagram
Use case model
(Funk, 2005)
Use cases
Use Case 1: When a new user approaches the health case worker at the care foundation, the
relevant details are gathered from the user and maintained in the information system (Jones,
Rudin, Perry, & Shekelle, 2014). Depending on the needs of the new user, the health worker
assigns the case to the appropriate department such as emergency service, diagnostics, etc.
2
National Youth Mental Health Foundation Development Project
Use case 2: When a family member of the user contacts the health case worker regarding the
health service, the worker gathers basic information from the member and maintains them in
the new IT system developed. On arrival of the user, the worker further examines the patient
and updates other relevant information needed for the health service. After this process the
incoming patient is assigned to the appropriate department (Marakas & Marakas, 2007).
Use Case 3: When a new patient with minor symptoms approaches the health case worker in
the health foundation, after gathering the basic information, the user is assigned to the
available clinician. The clinicians transcripts are then stored in the computer for further
access.
Use Case 4: When a family member enrols a new patient with minor symptoms, the health
case worker collects basic information and assigns a clinician to examine the new comer. On
completion of the service by the clinician, the patient is either released or retained in the
centre for further service (World Health Organization, 2015). All the relevant data regarding
the health service will be recorded and maintained in the new system.
Use Case 5: When a registered patient approaches the health case worker, after retrieving the
relevant information, the incoming patient is assigned to the emergency department. The
emergency department, based on the previous records and patient health status, administers
the health service and update the health records in the computer.
Use Case 6: When a patient revisits the health worker for a follow up, the health professional
examines the progress and records the present status of the patients Depending on the health
condition of the outpatient, the health care user is assigned to an appropriate department
(Vourlekis, 2017). The medical officers in the respective departments will decide the course
of action and the details are entered into the computer (Curtis & Cobham, 2013).
Use Case 7: When the parent of a minor child approaches the health worker regarding the
conditions of the patient, the health worker access the records and update the reports
presented by the parent. The parent’s concern will be notified to the appropriate department
for further action.
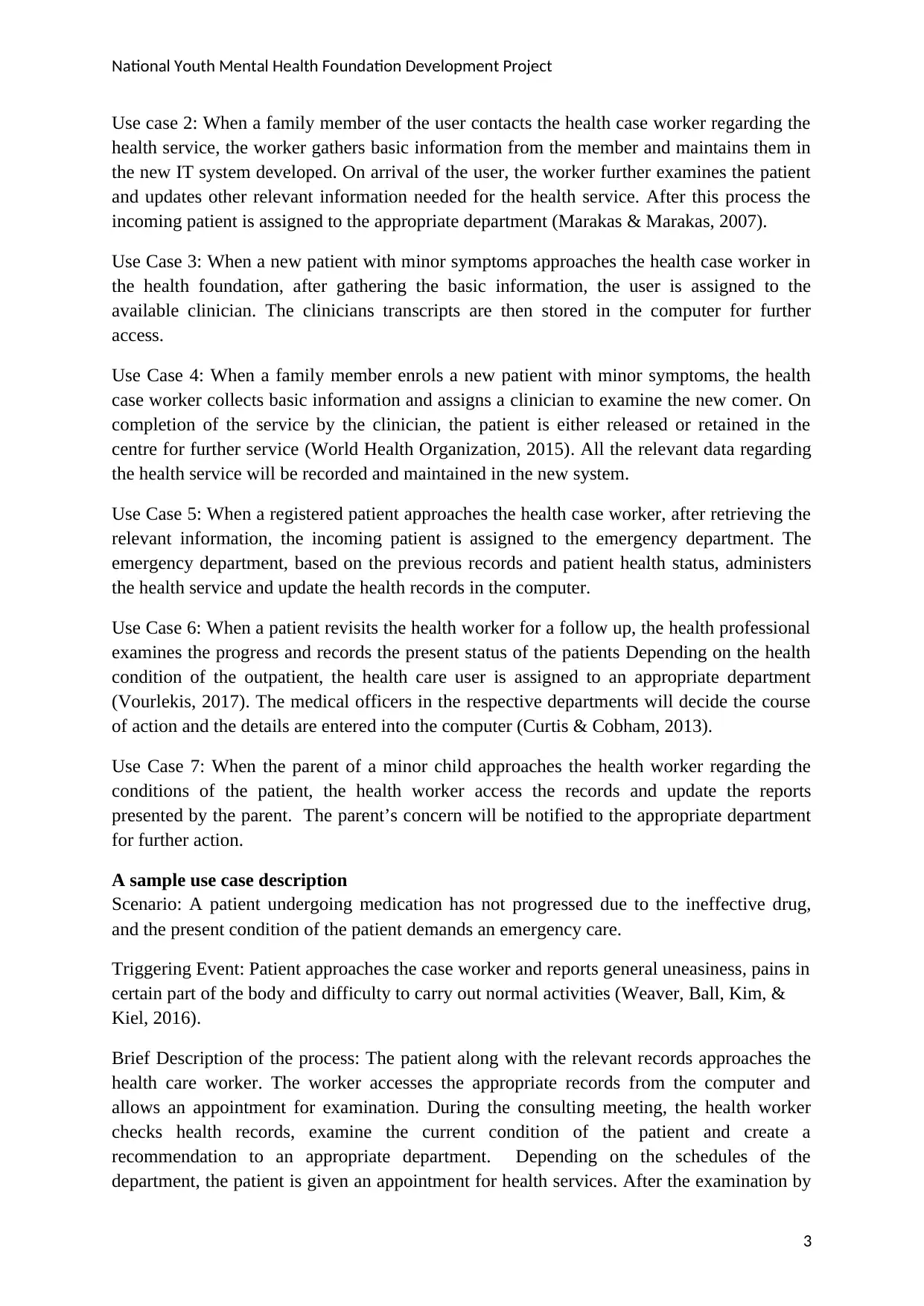
A sample use case description
Scenario: A patient undergoing medication has not progressed due to the ineffective drug,
and the present condition of the patient demands an emergency care.
Triggering Event: Patient approaches the case worker and reports general uneasiness, pains in
certain part of the body and difficulty to carry out normal activities (Weaver, Ball, Kim, &
Kiel, 2016).
Brief Description of the process: The patient along with the relevant records approaches the
health care worker. The worker accesses the appropriate records from the computer and
allows an appointment for examination. During the consulting meeting, the health worker
checks health records, examine the current condition of the patient and create a
recommendation to an appropriate department. Depending on the schedules of the
department, the patient is given an appointment for health services. After the examination by
3
Use case 2: When a family member of the user contacts the health case worker regarding the
health service, the worker gathers basic information from the member and maintains them in
the new IT system developed. On arrival of the user, the worker further examines the patient
and updates other relevant information needed for the health service. After this process the
incoming patient is assigned to the appropriate department (Marakas & Marakas, 2007).
Use Case 3: When a new patient with minor symptoms approaches the health case worker in
the health foundation, after gathering the basic information, the user is assigned to the
available clinician. The clinicians transcripts are then stored in the computer for further
access.
Use Case 4: When a family member enrols a new patient with minor symptoms, the health
case worker collects basic information and assigns a clinician to examine the new comer. On
completion of the service by the clinician, the patient is either released or retained in the
centre for further service (World Health Organization, 2015). All the relevant data regarding
the health service will be recorded and maintained in the new system.
Use Case 5: When a registered patient approaches the health case worker, after retrieving the
relevant information, the incoming patient is assigned to the emergency department. The
emergency department, based on the previous records and patient health status, administers
the health service and update the health records in the computer.
Use Case 6: When a patient revisits the health worker for a follow up, the health professional
examines the progress and records the present status of the patients Depending on the health
condition of the outpatient, the health care user is assigned to an appropriate department
(Vourlekis, 2017). The medical officers in the respective departments will decide the course
of action and the details are entered into the computer (Curtis & Cobham, 2013).
Use Case 7: When the parent of a minor child approaches the health worker regarding the
conditions of the patient, the health worker access the records and update the reports
presented by the parent. The parent’s concern will be notified to the appropriate department
for further action.
A sample use case description
Scenario: A patient undergoing medication has not progressed due to the ineffective drug,
and the present condition of the patient demands an emergency care.
Triggering Event: Patient approaches the case worker and reports general uneasiness, pains in
certain part of the body and difficulty to carry out normal activities (Weaver, Ball, Kim, &
Kiel, 2016).
Brief Description of the process: The patient along with the relevant records approaches the
health care worker. The worker accesses the appropriate records from the computer and
allows an appointment for examination. During the consulting meeting, the health worker
checks health records, examine the current condition of the patient and create a
recommendation to an appropriate department. Depending on the schedules of the
department, the patient is given an appointment for health services. After the examination by
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
National Youth Mental Health Foundation Development Project
the clinician in the concerned department, the health records of the patient are updated
(Lavin, Harper, & Barr, 2015).
Actors: Patient, Case Worker, clinician in the assigned department
Associated use Cases: Use Case 3 is appropriate for the above scenario where the care worker
assigns a clinician to the incoming patient.
Preconditions: The patient must be registered with the care institution and has undergone a
treatment. For a new patient, this use case will not be appropriate.
Flow of Activities:
Actor System
1. Patient approaches health worker with a
new issue
1.1 Case is acknowledged, past records
retrieved, and new information is appended
to the patient’s record
2. The patient is given an appointment to
attend the examination
2.1 A notification for appointment is
generated which will be sent to the patient,
case worker and the department
2.2 Appointment is served to the patient
with appropriate updating of the records
2.3 The case worker accesses the records of
patient and verifies everything is in order
before the appointment (Sultan, 2014)
3. Case worker assigns the case to an
appropriate Department
3.1 On arrival of the patient, the assignment
notification is sent to the department with
access to relevant records
3.2 The department professional attends the
patient , updates records and assigns an
appropriate clinician
4. The Department assigns a clinician for
the concerned issue
4.1 Clinician examines the patient and
identifies the medical causes.
4.2 The clinician prescribes suitable
medicine and therapy for the patient
4.3 The information regarding the care
service is updated in the system
5. Patient is admitted to the centre or
released
5.1 The clinician either recommends
admission to the centre or release with
appropriate prescription
5.2 The case worker updates the record of
patient in the system and the information
goes to the concerned department
Exceptional conditions and contexts
1.1 The patient has not provided sufficient information or details to the health case worker
2.2 The clinician did not update the patient record
4
the clinician in the concerned department, the health records of the patient are updated
(Lavin, Harper, & Barr, 2015).
Actors: Patient, Case Worker, clinician in the assigned department
Associated use Cases: Use Case 3 is appropriate for the above scenario where the care worker
assigns a clinician to the incoming patient.
Preconditions: The patient must be registered with the care institution and has undergone a
treatment. For a new patient, this use case will not be appropriate.
Flow of Activities:
Actor System
1. Patient approaches health worker with a
new issue
1.1 Case is acknowledged, past records
retrieved, and new information is appended
to the patient’s record
2. The patient is given an appointment to
attend the examination
2.1 A notification for appointment is
generated which will be sent to the patient,
case worker and the department
2.2 Appointment is served to the patient
with appropriate updating of the records
2.3 The case worker accesses the records of
patient and verifies everything is in order
before the appointment (Sultan, 2014)
3. Case worker assigns the case to an
appropriate Department
3.1 On arrival of the patient, the assignment
notification is sent to the department with
access to relevant records
3.2 The department professional attends the
patient , updates records and assigns an
appropriate clinician
4. The Department assigns a clinician for
the concerned issue
4.1 Clinician examines the patient and
identifies the medical causes.
4.2 The clinician prescribes suitable
medicine and therapy for the patient
4.3 The information regarding the care
service is updated in the system
5. Patient is admitted to the centre or
released
5.1 The clinician either recommends
admission to the centre or release with
appropriate prescription
5.2 The case worker updates the record of
patient in the system and the information
goes to the concerned department
Exceptional conditions and contexts
1.1 The patient has not provided sufficient information or details to the health case worker
2.2 The clinician did not update the patient record
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
National Youth Mental Health Foundation Development Project
3.3 The case worker is unable to retrieve the previous records or update the current status
4.2 The department or clinician cannot retrieve the past records or update the current
information
5.2 The department or clinician examines the patient but fails to update the information
5
3.3 The case worker is unable to retrieve the previous records or update the current status
4.2 The department or clinician cannot retrieve the past records or update the current
information
5.2 The department or clinician examines the patient but fails to update the information
5
National Youth Mental Health Foundation Development Project
References
Curtis, G., & Cobham, D. (2013). Business information systems. Harlow, England: Prentice
Hall, Financial Times.
Fedder, D. O., Chang, R. J., Curry, S., & Nichols, G. (2003). The effectiveness of a
community health worker outreach program on healthcare utilization of west
baltimore city medicaid patients with diabetes with or without hypertension. Ethnicity
and Disease, 13(1), 22-27.
Jones, S. S., Rudin, R. S., Perry, T., & Shekelle, P. G. (2014). Health information technology:
an updated systematic review with a focus on meaningful use. Annals of internal
medicine, 160(1), 48-54.
Lavin, M., Harper, E., & Barr, N. (2015). Health information technology, patient safety, and
professional nursing care documentation in acute care settings. OJIN: The Online
Journal of Issues in Nursing, 20(2).
Mancini, M. A. (2016). Mental Health Treatment Planning: A Dis/Empowering Process.
In The Palgrave Handbook of Adult Mental Health (pp. 352-370). Palgrave
Macmillan UK.
Marakas, G., & Marakas, G. (2006). Systems analysis & design. Boston: McGraw-Hill/Irwin.
Sultan, N. (2014). Making use of cloud computing for healthcare provision: Opportunities
and challenges. International Journal of Information Management, 34(2), 177-184.
Vourlekis, B. (Ed.). (2017). Social work case management. Routledge.
Weaver, C. A., Ball, M. J., Kim, G. R., & Kiel, J. M. (2016). Healthcare information
management systems. Cham: Springer International Publishing.
World Health Organization. (2015). Health Worker Role in Providing Safe Abortion Care
and Post Abortion Contraception. World Health Organization.
6
References
Curtis, G., & Cobham, D. (2013). Business information systems. Harlow, England: Prentice
Hall, Financial Times.
Fedder, D. O., Chang, R. J., Curry, S., & Nichols, G. (2003). The effectiveness of a
community health worker outreach program on healthcare utilization of west
baltimore city medicaid patients with diabetes with or without hypertension. Ethnicity
and Disease, 13(1), 22-27.
Jones, S. S., Rudin, R. S., Perry, T., & Shekelle, P. G. (2014). Health information technology:
an updated systematic review with a focus on meaningful use. Annals of internal
medicine, 160(1), 48-54.
Lavin, M., Harper, E., & Barr, N. (2015). Health information technology, patient safety, and
professional nursing care documentation in acute care settings. OJIN: The Online
Journal of Issues in Nursing, 20(2).
Mancini, M. A. (2016). Mental Health Treatment Planning: A Dis/Empowering Process.
In The Palgrave Handbook of Adult Mental Health (pp. 352-370). Palgrave
Macmillan UK.
Marakas, G., & Marakas, G. (2006). Systems analysis & design. Boston: McGraw-Hill/Irwin.
Sultan, N. (2014). Making use of cloud computing for healthcare provision: Opportunities
and challenges. International Journal of Information Management, 34(2), 177-184.
Vourlekis, B. (Ed.). (2017). Social work case management. Routledge.
Weaver, C. A., Ball, M. J., Kim, G. R., & Kiel, J. M. (2016). Healthcare information
management systems. Cham: Springer International Publishing.
World Health Organization. (2015). Health Worker Role in Providing Safe Abortion Care
and Post Abortion Contraception. World Health Organization.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





