National Youth Mental Health Project
VerifiedAdded on 2019/11/12
|8
|1759
|23
Project
AI Summary
This project report details the development of a system for a National Youth Mental Health Foundation. It includes a stakeholder map identifying key players (patients, families, healthcare workers, clinicians, administrators, etc.), a questionnaire designed to gather patient information, a use case diagram visually representing system interactions, and detailed use case descriptions outlining various scenarios within the system. The report thoroughly documents the system's functionality, from initial patient contact to treatment and follow-up, addressing potential exceptions and providing relevant references. The document aims to create a functional and efficient system for managing youth mental health cases.

[Draw your reader in with an engaging
abstract. It is typically a short summary of
the document. When you’re ready to add
your content, just click here and start
typing.]
[Document title]
[Document subtitle]
A
abstract. It is typically a short summary of
the document. When you’re ready to add
your content, just click here and start
typing.]
[Document title]
[Document subtitle]
A
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

National Youth Mental Health Foundation
Development Project
Table of Contents
Stakeholder map.......................................................................................................................2
Questionnaire............................................................................................................................2
Use Case Diagram....................................................................................................................3
Use case model....................................................................................................................................3
Use cases..............................................................................................................................................4
Use case description...........................................................................................................................4
References.................................................................................................................................5
Development Project
Table of Contents
Stakeholder map.......................................................................................................................2
Questionnaire............................................................................................................................2
Use Case Diagram....................................................................................................................3
Use case model....................................................................................................................................3
Use cases..............................................................................................................................................4
Use case description...........................................................................................................................4
References.................................................................................................................................5
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
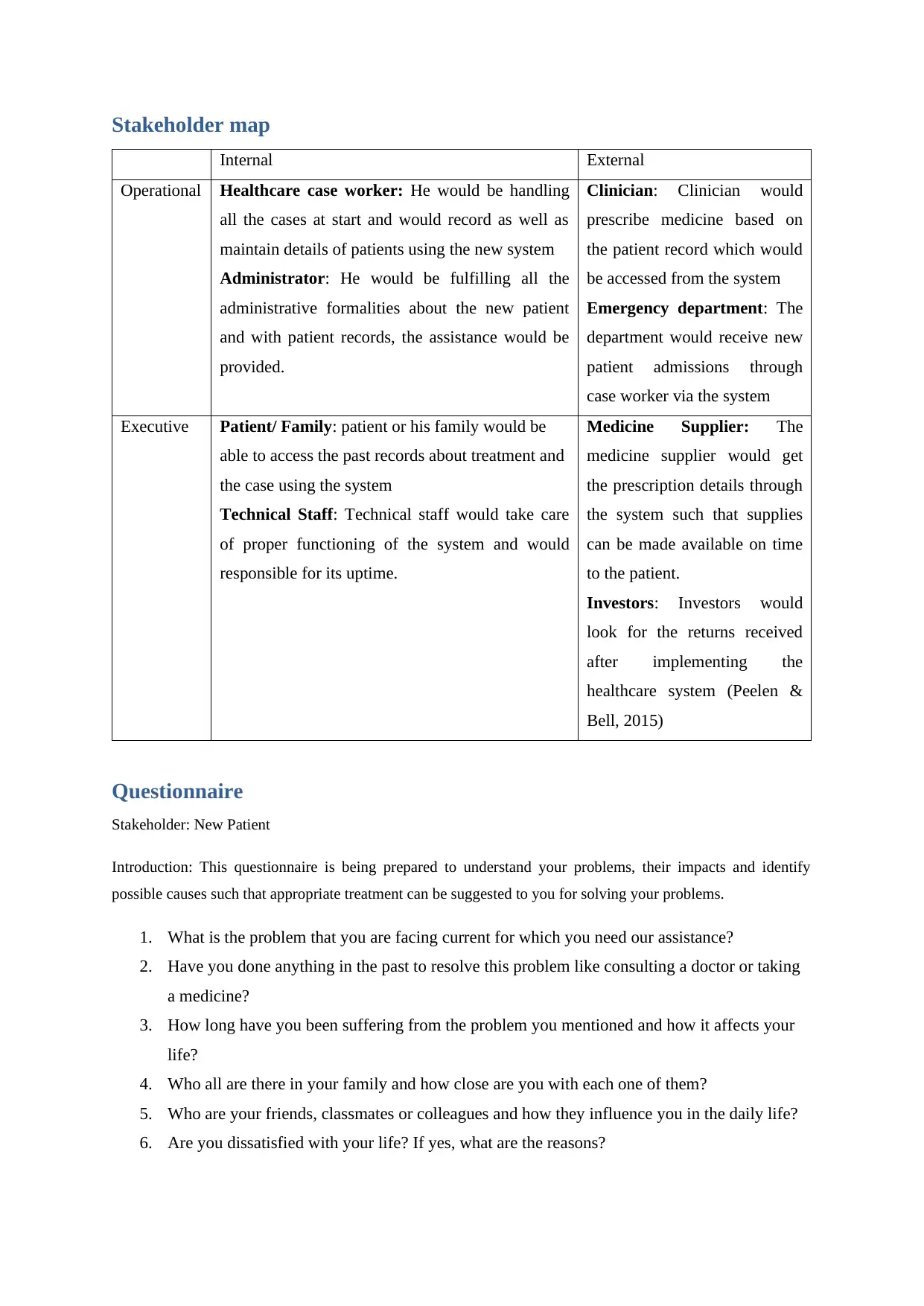
Stakeholder map
Internal External
Operational Healthcare case worker: He would be handling
all the cases at start and would record as well as
maintain details of patients using the new system
Administrator: He would be fulfilling all the
administrative formalities about the new patient
and with patient records, the assistance would be
provided.
Clinician: Clinician would
prescribe medicine based on
the patient record which would
be accessed from the system
Emergency department: The
department would receive new
patient admissions through
case worker via the system
Executive Patient/ Family: patient or his family would be
able to access the past records about treatment and
the case using the system
Technical Staff: Technical staff would take care
of proper functioning of the system and would
responsible for its uptime.
Medicine Supplier: The
medicine supplier would get
the prescription details through
the system such that supplies
can be made available on time
to the patient.
Investors: Investors would
look for the returns received
after implementing the
healthcare system (Peelen &
Bell, 2015)
Questionnaire
Stakeholder: New Patient
Introduction: This questionnaire is being prepared to understand your problems, their impacts and identify
possible causes such that appropriate treatment can be suggested to you for solving your problems.
1. What is the problem that you are facing current for which you need our assistance?
2. Have you done anything in the past to resolve this problem like consulting a doctor or taking
a medicine?
3. How long have you been suffering from the problem you mentioned and how it affects your
life?
4. Who all are there in your family and how close are you with each one of them?
5. Who are your friends, classmates or colleagues and how they influence you in the daily life?
6. Are you dissatisfied with your life? If yes, what are the reasons?
Internal External
Operational Healthcare case worker: He would be handling
all the cases at start and would record as well as
maintain details of patients using the new system
Administrator: He would be fulfilling all the
administrative formalities about the new patient
and with patient records, the assistance would be
provided.
Clinician: Clinician would
prescribe medicine based on
the patient record which would
be accessed from the system
Emergency department: The
department would receive new
patient admissions through
case worker via the system
Executive Patient/ Family: patient or his family would be
able to access the past records about treatment and
the case using the system
Technical Staff: Technical staff would take care
of proper functioning of the system and would
responsible for its uptime.
Medicine Supplier: The
medicine supplier would get
the prescription details through
the system such that supplies
can be made available on time
to the patient.
Investors: Investors would
look for the returns received
after implementing the
healthcare system (Peelen &
Bell, 2015)
Questionnaire
Stakeholder: New Patient
Introduction: This questionnaire is being prepared to understand your problems, their impacts and identify
possible causes such that appropriate treatment can be suggested to you for solving your problems.
1. What is the problem that you are facing current for which you need our assistance?
2. Have you done anything in the past to resolve this problem like consulting a doctor or taking
a medicine?
3. How long have you been suffering from the problem you mentioned and how it affects your
life?
4. Who all are there in your family and how close are you with each one of them?
5. Who are your friends, classmates or colleagues and how they influence you in the daily life?
6. Are you dissatisfied with your life? If yes, what are the reasons?
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7. Do you have someone as your loving partner? If yes, how is your relationship with him or
her?
8. Do you have friends? If no, please explain the reasons and if yes, how comfortable are you
with them for sharing your concerns?
9. Who is your support system in friends, family and professional network?
10. Do you think the problem that you are facing such as depression or anxiety is causing your
personal and professional life to suffer? If yes, please give details of how (IFS, 2009).
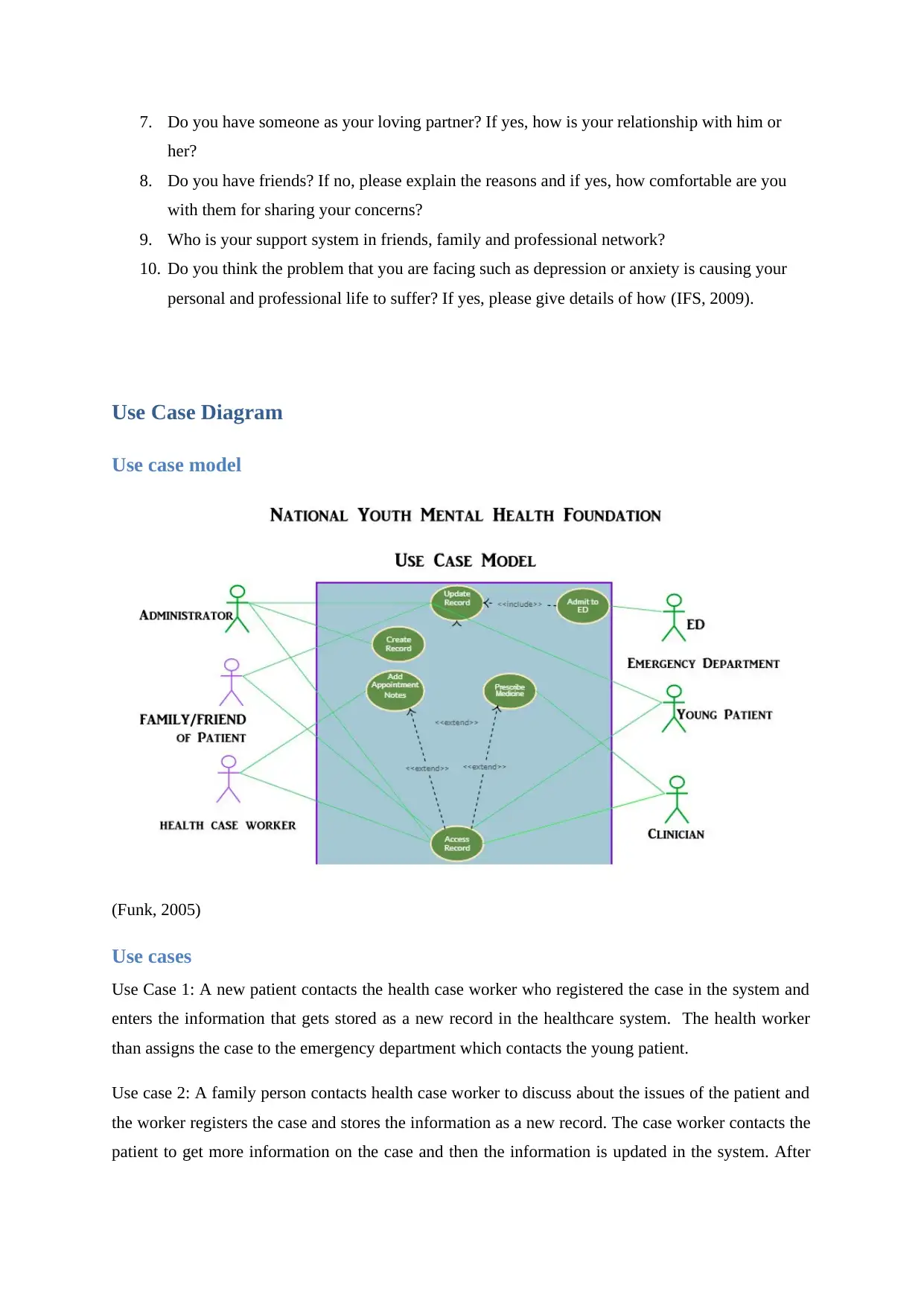
Use Case Diagram
Use case model
(Funk, 2005)
Use cases
Use Case 1: A new patient contacts the health case worker who registered the case in the system and
enters the information that gets stored as a new record in the healthcare system. The health worker
than assigns the case to the emergency department which contacts the young patient.
Use case 2: A family person contacts health case worker to discuss about the issues of the patient and
the worker registers the case and stores the information as a new record. The case worker contacts the
patient to get more information on the case and then the information is updated in the system. After
her?
8. Do you have friends? If no, please explain the reasons and if yes, how comfortable are you
with them for sharing your concerns?
9. Who is your support system in friends, family and professional network?
10. Do you think the problem that you are facing such as depression or anxiety is causing your
personal and professional life to suffer? If yes, please give details of how (IFS, 2009).
Use Case Diagram
Use case model
(Funk, 2005)
Use cases
Use Case 1: A new patient contacts the health case worker who registered the case in the system and
enters the information that gets stored as a new record in the healthcare system. The health worker
than assigns the case to the emergency department which contacts the young patient.
Use case 2: A family person contacts health case worker to discuss about the issues of the patient and
the worker registers the case and stores the information as a new record. The case worker contacts the
patient to get more information on the case and then the information is updated in the system. After
updating the information, the health case worker assigns the case to the emergency department that
contacts the patient (Sanborn, 1983).
Use Case 3: A new patient contacts the health case worker who registers the case in the system and
creates a new record for the patient. The case worker realises that the condition is not severe and such
cases have already been handled in past with medication so he assigns the case to a clinician who
prescribes the medicine to the patient.
Use Case 4: A family person contacts health case worker to discuss about the issues of the patient and
the worker registers the case and stores the information as a new record. The case worker realises that
the condition is not severe and such cases have already been handled in past with medication so he
assigns the case to a clinician who prescribes the medicine for the patient.
Use Case 5: The patient has already visited the health case worker and an emergency department has
been given the case. The case worker receives the information that the patient has been released as the
ED updates it to the patient record which generates a notification to the case worker. So the case
worker contacts the patient and gives an appointment to the patient. In the meeting with patient,
appointment notes are taken and updated in the record by the case worker (MHC, 011).
Use Case 6: The patient revisits the health worker after taking medicine and the health worker realises
that the patient still needs help. The worker updates the patient record and assigns the case to the
Emergency department. The emergency department gets the notification of new assignment and
contacts the patient for admission (Benningfield, 2015).
Use Case 7: The Parent of the patient has approached the case worker after the child has already gone
through the medication asking for help. The case worker would receive a call from the parent and the
update given would be updated in the patient record. A new appointment would be given to the case
patient to take the case forward (McKenzie, et al., 2016).
Use case description
Scenario: The patient has already used medication which did not work and now patient needs
emergency care.
Triggering Event: Patient approaching the case worker again to discuss the case
Brief Description: The patient checks his health records and sends a request to case worker for
intervention who receives a notification and gives the appointment to the young patient. The patient
meets the worker and the case is updated with additional information. The case worker then forwards
the case to ED which gets the notification of assignment and calls back the patient for admission.
Actors: Patient, Case Worker, ED
contacts the patient (Sanborn, 1983).
Use Case 3: A new patient contacts the health case worker who registers the case in the system and
creates a new record for the patient. The case worker realises that the condition is not severe and such
cases have already been handled in past with medication so he assigns the case to a clinician who
prescribes the medicine to the patient.
Use Case 4: A family person contacts health case worker to discuss about the issues of the patient and
the worker registers the case and stores the information as a new record. The case worker realises that
the condition is not severe and such cases have already been handled in past with medication so he
assigns the case to a clinician who prescribes the medicine for the patient.
Use Case 5: The patient has already visited the health case worker and an emergency department has
been given the case. The case worker receives the information that the patient has been released as the
ED updates it to the patient record which generates a notification to the case worker. So the case
worker contacts the patient and gives an appointment to the patient. In the meeting with patient,
appointment notes are taken and updated in the record by the case worker (MHC, 011).
Use Case 6: The patient revisits the health worker after taking medicine and the health worker realises
that the patient still needs help. The worker updates the patient record and assigns the case to the
Emergency department. The emergency department gets the notification of new assignment and
contacts the patient for admission (Benningfield, 2015).
Use Case 7: The Parent of the patient has approached the case worker after the child has already gone
through the medication asking for help. The case worker would receive a call from the parent and the
update given would be updated in the patient record. A new appointment would be given to the case
patient to take the case forward (McKenzie, et al., 2016).
Use case description
Scenario: The patient has already used medication which did not work and now patient needs
emergency care.
Triggering Event: Patient approaching the case worker again to discuss the case
Brief Description: The patient checks his health records and sends a request to case worker for
intervention who receives a notification and gives the appointment to the young patient. The patient
meets the worker and the case is updated with additional information. The case worker then forwards
the case to ED which gets the notification of assignment and calls back the patient for admission.
Actors: Patient, Case Worker, ED
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
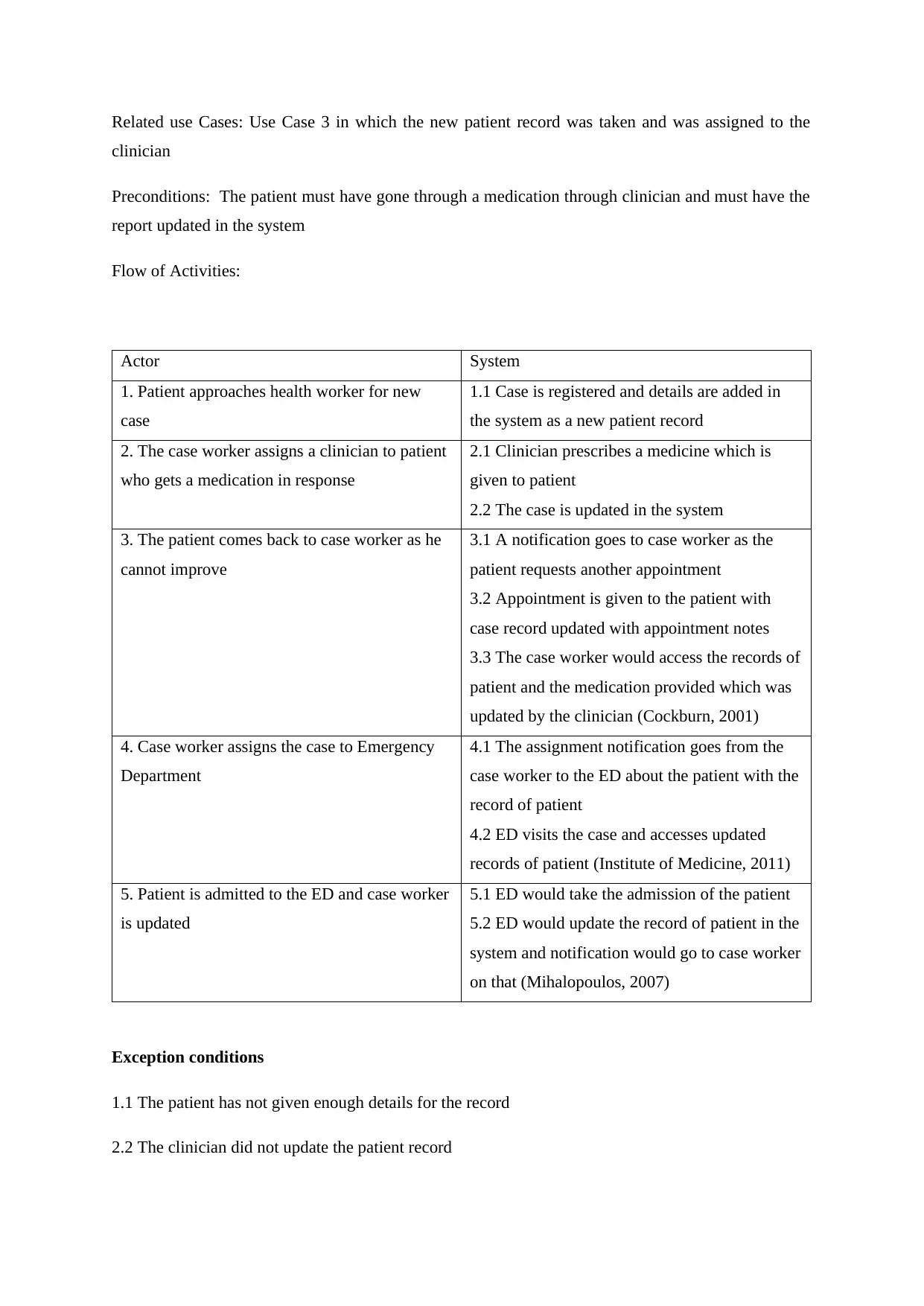
Related use Cases: Use Case 3 in which the new patient record was taken and was assigned to the
clinician
Preconditions: The patient must have gone through a medication through clinician and must have the
report updated in the system
Flow of Activities:
Actor System
1. Patient approaches health worker for new
case
1.1 Case is registered and details are added in
the system as a new patient record
2. The case worker assigns a clinician to patient
who gets a medication in response
2.1 Clinician prescribes a medicine which is
given to patient
2.2 The case is updated in the system
3. The patient comes back to case worker as he
cannot improve
3.1 A notification goes to case worker as the
patient requests another appointment
3.2 Appointment is given to the patient with
case record updated with appointment notes
3.3 The case worker would access the records of
patient and the medication provided which was
updated by the clinician (Cockburn, 2001)
4. Case worker assigns the case to Emergency
Department
4.1 The assignment notification goes from the
case worker to the ED about the patient with the
record of patient
4.2 ED visits the case and accesses updated
records of patient (Institute of Medicine, 2011)
5. Patient is admitted to the ED and case worker
is updated
5.1 ED would take the admission of the patient
5.2 ED would update the record of patient in the
system and notification would go to case worker
on that (Mihalopoulos, 2007)
Exception conditions
1.1 The patient has not given enough details for the record
2.2 The clinician did not update the patient record
clinician
Preconditions: The patient must have gone through a medication through clinician and must have the
report updated in the system
Flow of Activities:
Actor System
1. Patient approaches health worker for new
case
1.1 Case is registered and details are added in
the system as a new patient record
2. The case worker assigns a clinician to patient
who gets a medication in response
2.1 Clinician prescribes a medicine which is
given to patient
2.2 The case is updated in the system
3. The patient comes back to case worker as he
cannot improve
3.1 A notification goes to case worker as the
patient requests another appointment
3.2 Appointment is given to the patient with
case record updated with appointment notes
3.3 The case worker would access the records of
patient and the medication provided which was
updated by the clinician (Cockburn, 2001)
4. Case worker assigns the case to Emergency
Department
4.1 The assignment notification goes from the
case worker to the ED about the patient with the
record of patient
4.2 ED visits the case and accesses updated
records of patient (Institute of Medicine, 2011)
5. Patient is admitted to the ED and case worker
is updated
5.1 ED would take the admission of the patient
5.2 ED would update the record of patient in the
system and notification would go to case worker
on that (Mihalopoulos, 2007)
Exception conditions
1.1 The patient has not given enough details for the record
2.2 The clinician did not update the patient record
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
3.3 The case worker could not find the record of the medicine given to the patient
4.2 The Emergency department cannot find required details in the updated record of the patient
5.2 The emergency department admits the case but does not update the patient record
References
Benningfield, M., 2015. School Mental Health, An Issue of Child and Adolescent Psychiatric
Clinics .... s.l.:Elsevier Health Sciences.
Cockburn, A., 2001. Writing Effective Use Cases. s.l.:Pearson Education India.
Funk, M., 2005. MENTAL HEALTH INFORMATION SYSTEMS, China: WHO.
IFS, 2009. Mental Health Care Patient Management System , s.l.: IFS.
Institute of Medicine, 2011. Digital Infrastructure for the Learning Health System: The Foundation
for Continuous Improvement in Health and Health Care: Workshop Series Summary. s.l.:National
Academies Press.
McKenzie, K., Agic, B., Tuck, A. & Antwi, M., 2016. The Case for Diversity, s.l.: MENTAL
HEALTH COMMISSION OF CANADA.
MHC, 011. Making the Case for Investing in Mental Health in Canada, s.l.: Mental Health
Commission of Canada.
Mihalopoulos, C., 2007. Does the triple P-positive parenting program provide value for money.
Australian and New Zealand Journal of Psychiatry, 41(3), pp. 239-246..
Peelen, M. & Bell, T., 2015. Use Case Highlights: Mental Health Center of Denver, s.l.: Kodak
Alaris.
Sanborn, C. J., 1983. Case Management in Mental Health Services. s.l.:The Haworth Press.
4.2 The Emergency department cannot find required details in the updated record of the patient
5.2 The emergency department admits the case but does not update the patient record
References
Benningfield, M., 2015. School Mental Health, An Issue of Child and Adolescent Psychiatric
Clinics .... s.l.:Elsevier Health Sciences.
Cockburn, A., 2001. Writing Effective Use Cases. s.l.:Pearson Education India.
Funk, M., 2005. MENTAL HEALTH INFORMATION SYSTEMS, China: WHO.
IFS, 2009. Mental Health Care Patient Management System , s.l.: IFS.
Institute of Medicine, 2011. Digital Infrastructure for the Learning Health System: The Foundation
for Continuous Improvement in Health and Health Care: Workshop Series Summary. s.l.:National
Academies Press.
McKenzie, K., Agic, B., Tuck, A. & Antwi, M., 2016. The Case for Diversity, s.l.: MENTAL
HEALTH COMMISSION OF CANADA.
MHC, 011. Making the Case for Investing in Mental Health in Canada, s.l.: Mental Health
Commission of Canada.
Mihalopoulos, C., 2007. Does the triple P-positive parenting program provide value for money.
Australian and New Zealand Journal of Psychiatry, 41(3), pp. 239-246..
Peelen, M. & Bell, T., 2015. Use Case Highlights: Mental Health Center of Denver, s.l.: Kodak
Alaris.
Sanborn, C. J., 1983. Case Management in Mental Health Services. s.l.:The Haworth Press.
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





![Stakeholder Map, Questionnaire, and Use Case Project - [Course Name]](/_next/image/?url=https%3A%2F%2Fdesklib.com%2Fmedia%2Fimages%2Fuw%2F8778cb6c6be74a2880d3e3960b21de93.jpg&w=256&q=75)