Pathophysiology of Obesity and its Link to Arthritis
VerifiedAdded on 2022/12/26
|19
|5318
|73
AI Summary
This article discusses the pathophysiology of obesity and its link to arthritis. It explains how obesity affects organ systems and metabolism, leading to the accumulation of adipocytes within the joint capsule. The article also highlights the role of adipokines and the impact of obesity on joint health.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
1. Mr Jankovic has presented with severe osteo-arthritis requiring a hip replacement.
Discuss briefly the pathophysiology of obesity and its link to Ivan’s arthritis. (2
marks)
Obesity is defined as having a BMI greater than 26 said by Nuttall (2015) and results in a state of
low-grade inflammation where the organ system and subsequently metabolism are affected
(Heymsfield & Wadden, 2017). Obesity is multifactorial however it commonly results from a
high storage of fats in the form of triacylglycerol in adipocyte due to a high caloric intake
(Garvey, Hurley& Kushner, 2016). The increased levels of fatty acids leads to its release in the
body which results in lipotoxicity and a build-up of oxidant stress to the organelles. This in turn
causes a low secretion of insulin which can also lead to further storage of fatty acid and release
of adipokines. Adipokines such as visfatin and resistin often causes an accumulation of
adipocytes within the joint capsule, causing arthritis (Gul et al., 2015). Obesity is one of the
major factors that leads to osteoarthritis (Glyn-Jones et al., 2015). Obesity causes damage to
joints and adipokines, effecting the cartilage, bone and synovium (Kulkarni et al., 2016)
potentially worsening obesity as it results in difficulty mobilising. The abnormally large weight
increase the mechanical pressure on the knee joints especially, further wearing down the
cartilage and deteriorating the joint to the point of clinical osteoarthritis. Heart stuff, diabetes,
obesity costs the healthcare system around $2501 per person with obesity as compared with
$1998 per person with normal weight thus, increased mortality rates (Lee et al., 2018).
Discuss briefly the pathophysiology of obesity and its link to Ivan’s arthritis. (2
marks)
Obesity is defined as having a BMI greater than 26 said by Nuttall (2015) and results in a state of
low-grade inflammation where the organ system and subsequently metabolism are affected
(Heymsfield & Wadden, 2017). Obesity is multifactorial however it commonly results from a
high storage of fats in the form of triacylglycerol in adipocyte due to a high caloric intake
(Garvey, Hurley& Kushner, 2016). The increased levels of fatty acids leads to its release in the
body which results in lipotoxicity and a build-up of oxidant stress to the organelles. This in turn
causes a low secretion of insulin which can also lead to further storage of fatty acid and release
of adipokines. Adipokines such as visfatin and resistin often causes an accumulation of
adipocytes within the joint capsule, causing arthritis (Gul et al., 2015). Obesity is one of the
major factors that leads to osteoarthritis (Glyn-Jones et al., 2015). Obesity causes damage to
joints and adipokines, effecting the cartilage, bone and synovium (Kulkarni et al., 2016)
potentially worsening obesity as it results in difficulty mobilising. The abnormally large weight
increase the mechanical pressure on the knee joints especially, further wearing down the
cartilage and deteriorating the joint to the point of clinical osteoarthritis. Heart stuff, diabetes,
obesity costs the healthcare system around $2501 per person with obesity as compared with
$1998 per person with normal weight thus, increased mortality rates (Lee et al., 2018).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1Case Study - Ivan Jankovic
2. When you watch the pre-operative videos, what communication issues do you
observe? Critically analyse the situation and consider both the patient and the nurse
perspective and what may have contributed to this? (4 marks)
After watching the video various communication errors have been seen between the nurse and
the patient. When the nurse came to give medicine, the patient was not informed about what
medication he was being given and why. From the perspective of the patient, it’s important they
receive all the relevant information regarding the type of treatment and diagnosis of the illness,
including medications. Further communication error has been noticed in how the nurse
preformed the checklist. Highly unprofessional language was used throughout the process and
the patient was made to feel like the nurse was just rushing through the checklist, rather than
using it as a tool to ensure all patient details are correct and the procedure goes smoothly. The
nurse didn’t get the patient or his wife to verbally state their full name, date of birth, phone
number and other important details, rather the nurse simply checked there was something in
those boxes. Body language was very poor from the nurse during the check, the nurse towered
over the patient the entire time and gave a posture that indicated disinterest and a lack of
professionalism.
3. Explain the importance of the pre-operative checklists and how these link to patient
safety and the NSQHS standards? (2 marks)
The perioperative checklist is important as this tool is used to identify, document the condition of
patient and communicate any risk factors associated with the procedure. The checklist gives an
important baseline for information about the vital signs of patient and whether it is within normal
limits, alongside ensuring the right patient is undergoing the right procedure (Molina etal., 2016).
Hence, this gives insight to the doctors and nurses about the potential consequences of
2. When you watch the pre-operative videos, what communication issues do you
observe? Critically analyse the situation and consider both the patient and the nurse
perspective and what may have contributed to this? (4 marks)
After watching the video various communication errors have been seen between the nurse and
the patient. When the nurse came to give medicine, the patient was not informed about what
medication he was being given and why. From the perspective of the patient, it’s important they
receive all the relevant information regarding the type of treatment and diagnosis of the illness,
including medications. Further communication error has been noticed in how the nurse
preformed the checklist. Highly unprofessional language was used throughout the process and
the patient was made to feel like the nurse was just rushing through the checklist, rather than
using it as a tool to ensure all patient details are correct and the procedure goes smoothly. The
nurse didn’t get the patient or his wife to verbally state their full name, date of birth, phone
number and other important details, rather the nurse simply checked there was something in
those boxes. Body language was very poor from the nurse during the check, the nurse towered
over the patient the entire time and gave a posture that indicated disinterest and a lack of
professionalism.
3. Explain the importance of the pre-operative checklists and how these link to patient
safety and the NSQHS standards? (2 marks)
The perioperative checklist is important as this tool is used to identify, document the condition of
patient and communicate any risk factors associated with the procedure. The checklist gives an
important baseline for information about the vital signs of patient and whether it is within normal
limits, alongside ensuring the right patient is undergoing the right procedure (Molina etal., 2016).
Hence, this gives insight to the doctors and nurses about the potential consequences of
2Case Study - Ivan Jankovic
anaesthesia and any increased risk of complications the surgical procedure may have on the
health of patient. Pre-operative checklist aids in providing safety to the patient, it is related to
NSQHS standard of comprehensive care, as it focuses on development of care plan and
minimising the harm of patients by observing the delivery of care given. (Haugen et al., 2015)
The motive can be accomplished by method of pre-operative checklist in which all the data of
the patient can be collected and monitored accordingly, thusly a proper plan can be implemented
to give quality care to the patients. NSQHS 5 refers to patient identification and procedure
matching. This links directly to the checklist system as the patient is asked at least 3 times
throughout the perioperative area to state their name and what procedure they are having done in
their own words.
4.State 3 risks to Mr Jankovic linked to his obesity pose when having a General
Anaesthetic? Support your answer with contemporary literature. (3 marks)
The three major risk of health in Mr Jankovic related to obesity while having anaesthesia are:
Difficulty in intubation- From the study of Dohrn et al. (2016) it can be said that in
morbid obese person, there is problem in managing the airway of the patients. Obesity by
itself is a challenge and risk factor for intubation. In administration of anaesthesia, the
greatest risk is maintaining the safe apnea period, which is the duration of time between
muscle paralysis and apnoea and obesity is related with short apnea period. There is drop
in oxyhaemoglobin saturation to the danger level and the Safe Apnea Period is too short.
(Kido et al., 2015,)
Risk of dose effect- In obese people, dosing adjustment is one of the various difficulties.
As anaesthesia is calculated by the patient’s weight, an obese person requires large doses
anaesthesia and any increased risk of complications the surgical procedure may have on the
health of patient. Pre-operative checklist aids in providing safety to the patient, it is related to
NSQHS standard of comprehensive care, as it focuses on development of care plan and
minimising the harm of patients by observing the delivery of care given. (Haugen et al., 2015)
The motive can be accomplished by method of pre-operative checklist in which all the data of
the patient can be collected and monitored accordingly, thusly a proper plan can be implemented
to give quality care to the patients. NSQHS 5 refers to patient identification and procedure
matching. This links directly to the checklist system as the patient is asked at least 3 times
throughout the perioperative area to state their name and what procedure they are having done in
their own words.
4.State 3 risks to Mr Jankovic linked to his obesity pose when having a General
Anaesthetic? Support your answer with contemporary literature. (3 marks)
The three major risk of health in Mr Jankovic related to obesity while having anaesthesia are:
Difficulty in intubation- From the study of Dohrn et al. (2016) it can be said that in
morbid obese person, there is problem in managing the airway of the patients. Obesity by
itself is a challenge and risk factor for intubation. In administration of anaesthesia, the
greatest risk is maintaining the safe apnea period, which is the duration of time between
muscle paralysis and apnoea and obesity is related with short apnea period. There is drop
in oxyhaemoglobin saturation to the danger level and the Safe Apnea Period is too short.
(Kido et al., 2015,)
Risk of dose effect- In obese people, dosing adjustment is one of the various difficulties.
As anaesthesia is calculated by the patient’s weight, an obese person requires large doses
3Case Study - Ivan Jankovic
that are harder to reverse if something changes, and are linked to poorer outcomes
(Tjeertes et al., 2015). If incorrect or high dose is given, people might face a loss of
stimulator response (Nightingale, C et al., 2015), death.
Risk of hypoventilation- Obese people when under anaesthesia start to breathe slowly,
they can encounter the problem of hypoventilation, which might accompanied by hypoxia
and hypercapnia (Surve et al., 2015). Bouroche and Bourgain (2015) said that with
occurrence of hypoventilation, people may increase the chance of vascular resistance
which can lead to heart stroke.
5.You realise that Ivan has been given incorrect medication. He received the medication for the
person in the next bed and has incorrectly received
• Metformin 500mg
• Gliclazide 5mg
• Aspirin 100mg
• Omeprazole 20mg
What are your immediate responsibilities as an RN to ensure Ivan’s safety? (1mark)
It was noted that Mr Jankovic has received incorrect medication, in account of this, the registered
nurse should immediately escalate the issue to the treating team and the team leader of the
nursing department for quick assessment and action. It is the duty of nurse to inform the patient
and their family the type of care and treatment plan given to correct the error, nurse should also
communicate these issues to them as soon as possible (Smolowitze et al., 2015). The patient
needs to get assessed and blood glucose level should be checked as Metformin and Gliclazide are
known to decrease the BGL level (Hassan & Abd-Allah, 2015). As platelet disruption is a side of
that are harder to reverse if something changes, and are linked to poorer outcomes
(Tjeertes et al., 2015). If incorrect or high dose is given, people might face a loss of
stimulator response (Nightingale, C et al., 2015), death.
Risk of hypoventilation- Obese people when under anaesthesia start to breathe slowly,
they can encounter the problem of hypoventilation, which might accompanied by hypoxia
and hypercapnia (Surve et al., 2015). Bouroche and Bourgain (2015) said that with
occurrence of hypoventilation, people may increase the chance of vascular resistance
which can lead to heart stroke.
5.You realise that Ivan has been given incorrect medication. He received the medication for the
person in the next bed and has incorrectly received
• Metformin 500mg
• Gliclazide 5mg
• Aspirin 100mg
• Omeprazole 20mg
What are your immediate responsibilities as an RN to ensure Ivan’s safety? (1mark)
It was noted that Mr Jankovic has received incorrect medication, in account of this, the registered
nurse should immediately escalate the issue to the treating team and the team leader of the
nursing department for quick assessment and action. It is the duty of nurse to inform the patient
and their family the type of care and treatment plan given to correct the error, nurse should also
communicate these issues to them as soon as possible (Smolowitze et al., 2015). The patient
needs to get assessed and blood glucose level should be checked as Metformin and Gliclazide are
known to decrease the BGL level (Hassan & Abd-Allah, 2015). As platelet disruption is a side of
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4Case Study - Ivan Jankovic
effect of Aspirin, the wound site should be assessed by the nurse immediately for strikethrough
and monitored. To address the side effects of the incorrect administration, correct medication
should be given in consultation with doctor.
It is the responsibility of the nurse in administration of medicine to respect the standard of
medicine safety. The nurse should document the patient information accurately and always check
patient details before administering any medications. The complete list of medications of the
patients should be provided by the clinician when they need to handover the case to the other
staff during the handover period. Full, detailed information needs to be given to the patient and
their family regarding any changes to their medication management (Smolowitz et al., 2015).
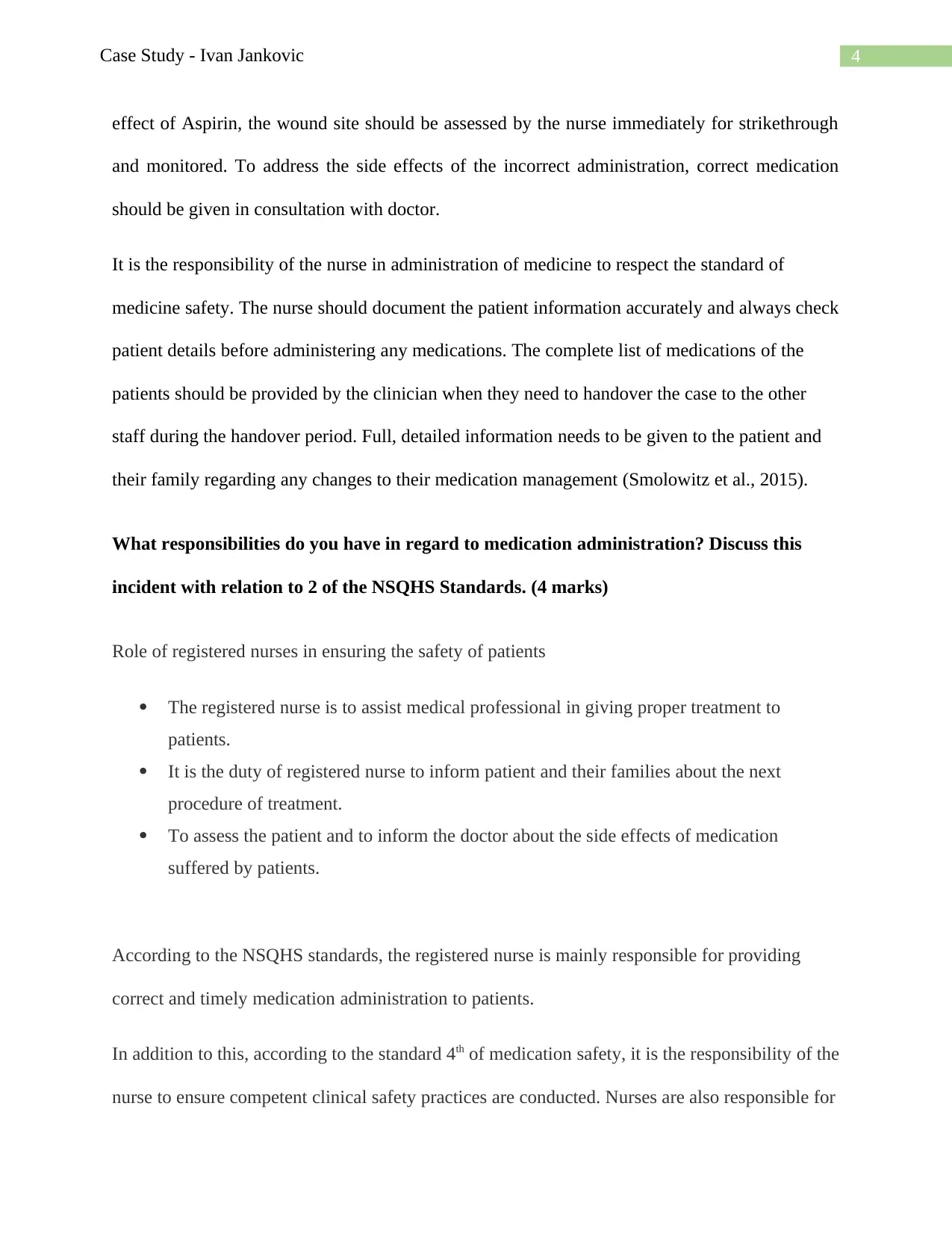
What responsibilities do you have in regard to medication administration? Discuss this
incident with relation to 2 of the NSQHS Standards. (4 marks)
Role of registered nurses in ensuring the safety of patients
The registered nurse is to assist medical professional in giving proper treatment to
patients.
It is the duty of registered nurse to inform patient and their families about the next
procedure of treatment.
To assess the patient and to inform the doctor about the side effects of medication
suffered by patients.
According to the NSQHS standards, the registered nurse is mainly responsible for providing
correct and timely medication administration to patients.
In addition to this, according to the standard 4th of medication safety, it is the responsibility of the
nurse to ensure competent clinical safety practices are conducted. Nurses are also responsible for
effect of Aspirin, the wound site should be assessed by the nurse immediately for strikethrough
and monitored. To address the side effects of the incorrect administration, correct medication
should be given in consultation with doctor.
It is the responsibility of the nurse in administration of medicine to respect the standard of
medicine safety. The nurse should document the patient information accurately and always check
patient details before administering any medications. The complete list of medications of the
patients should be provided by the clinician when they need to handover the case to the other
staff during the handover period. Full, detailed information needs to be given to the patient and
their family regarding any changes to their medication management (Smolowitz et al., 2015).
What responsibilities do you have in regard to medication administration? Discuss this
incident with relation to 2 of the NSQHS Standards. (4 marks)
Role of registered nurses in ensuring the safety of patients
The registered nurse is to assist medical professional in giving proper treatment to
patients.
It is the duty of registered nurse to inform patient and their families about the next
procedure of treatment.
To assess the patient and to inform the doctor about the side effects of medication
suffered by patients.
According to the NSQHS standards, the registered nurse is mainly responsible for providing
correct and timely medication administration to patients.
In addition to this, according to the standard 4th of medication safety, it is the responsibility of the
nurse to ensure competent clinical safety practices are conducted. Nurses are also responsible for
5Case Study - Ivan Jankovic
ensuring the proper disposal as well as administration of medicines. They are also accountable
for monitoring the side effects of medicines on patient health (Urden, Stacy and Lough, 2019).
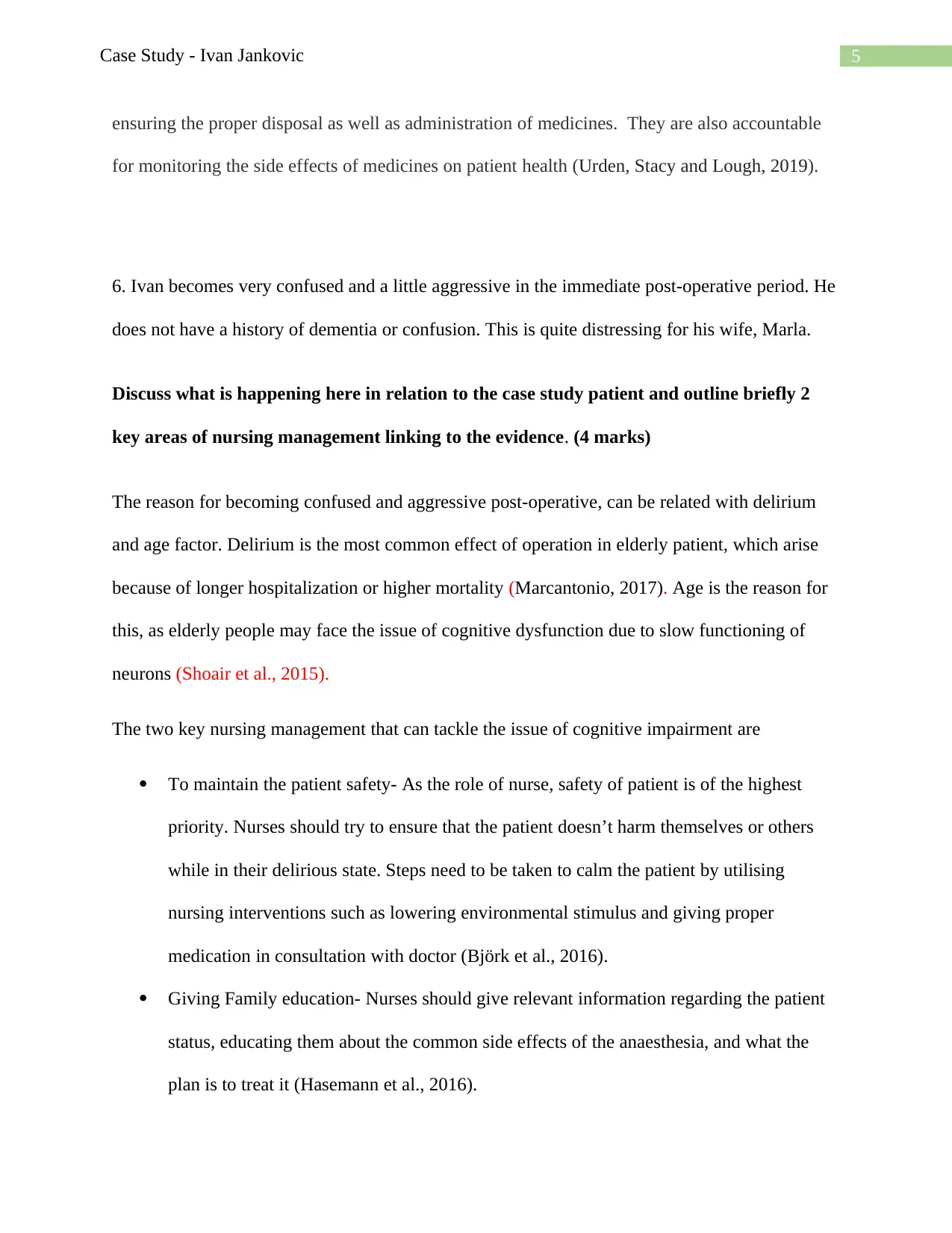
6. Ivan becomes very confused and a little aggressive in the immediate post-operative period. He
does not have a history of dementia or confusion. This is quite distressing for his wife, Marla.
Discuss what is happening here in relation to the case study patient and outline briefly 2
key areas of nursing management linking to the evidence. (4 marks)
The reason for becoming confused and aggressive post-operative, can be related with delirium
and age factor. Delirium is the most common effect of operation in elderly patient, which arise
because of longer hospitalization or higher mortality (Marcantonio, 2017). Age is the reason for
this, as elderly people may face the issue of cognitive dysfunction due to slow functioning of
neurons (Shoair et al., 2015).
The two key nursing management that can tackle the issue of cognitive impairment are
To maintain the patient safety- As the role of nurse, safety of patient is of the highest
priority. Nurses should try to ensure that the patient doesn’t harm themselves or others
while in their delirious state. Steps need to be taken to calm the patient by utilising
nursing interventions such as lowering environmental stimulus and giving proper
medication in consultation with doctor (Björk et al., 2016).
Giving Family education- Nurses should give relevant information regarding the patient
status, educating them about the common side effects of the anaesthesia, and what the
plan is to treat it (Hasemann et al., 2016).
ensuring the proper disposal as well as administration of medicines. They are also accountable
for monitoring the side effects of medicines on patient health (Urden, Stacy and Lough, 2019).
6. Ivan becomes very confused and a little aggressive in the immediate post-operative period. He
does not have a history of dementia or confusion. This is quite distressing for his wife, Marla.
Discuss what is happening here in relation to the case study patient and outline briefly 2
key areas of nursing management linking to the evidence. (4 marks)
The reason for becoming confused and aggressive post-operative, can be related with delirium
and age factor. Delirium is the most common effect of operation in elderly patient, which arise
because of longer hospitalization or higher mortality (Marcantonio, 2017). Age is the reason for
this, as elderly people may face the issue of cognitive dysfunction due to slow functioning of
neurons (Shoair et al., 2015).
The two key nursing management that can tackle the issue of cognitive impairment are
To maintain the patient safety- As the role of nurse, safety of patient is of the highest
priority. Nurses should try to ensure that the patient doesn’t harm themselves or others
while in their delirious state. Steps need to be taken to calm the patient by utilising
nursing interventions such as lowering environmental stimulus and giving proper
medication in consultation with doctor (Björk et al., 2016).
Giving Family education- Nurses should give relevant information regarding the patient
status, educating them about the common side effects of the anaesthesia, and what the
plan is to treat it (Hasemann et al., 2016).
6Case Study - Ivan Jankovic
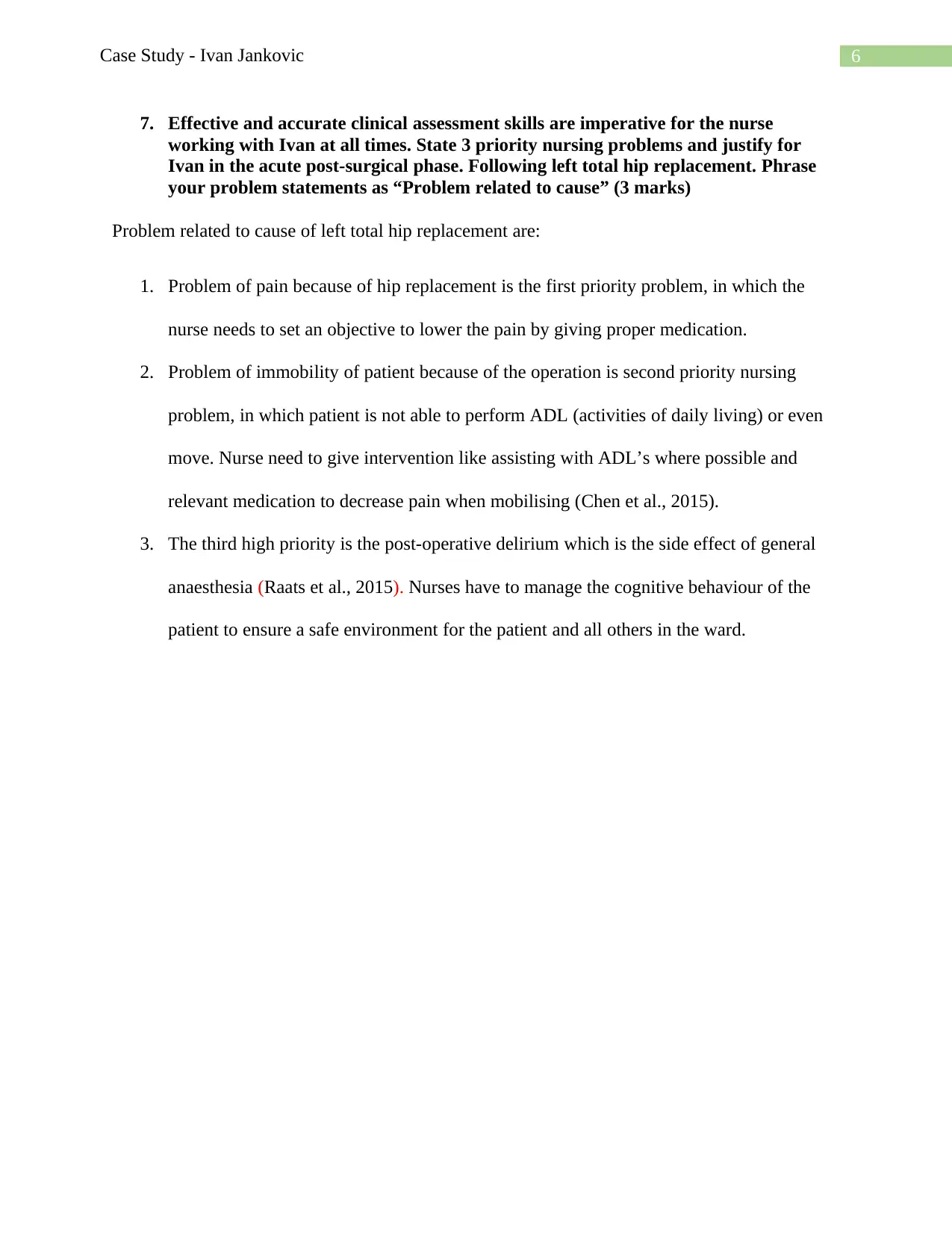
7. Effective and accurate clinical assessment skills are imperative for the nurse
working with Ivan at all times. State 3 priority nursing problems and justify for
Ivan in the acute post-surgical phase. Following left total hip replacement. Phrase
your problem statements as “Problem related to cause” (3 marks)
Problem related to cause of left total hip replacement are:
1. Problem of pain because of hip replacement is the first priority problem, in which the
nurse needs to set an objective to lower the pain by giving proper medication.
2. Problem of immobility of patient because of the operation is second priority nursing
problem, in which patient is not able to perform ADL (activities of daily living) or even
move. Nurse need to give intervention like assisting with ADL’s where possible and
relevant medication to decrease pain when mobilising (Chen et al., 2015).
3. The third high priority is the post-operative delirium which is the side effect of general
anaesthesia (Raats et al., 2015). Nurses have to manage the cognitive behaviour of the
patient to ensure a safe environment for the patient and all others in the ward.
7. Effective and accurate clinical assessment skills are imperative for the nurse
working with Ivan at all times. State 3 priority nursing problems and justify for
Ivan in the acute post-surgical phase. Following left total hip replacement. Phrase
your problem statements as “Problem related to cause” (3 marks)
Problem related to cause of left total hip replacement are:
1. Problem of pain because of hip replacement is the first priority problem, in which the
nurse needs to set an objective to lower the pain by giving proper medication.
2. Problem of immobility of patient because of the operation is second priority nursing
problem, in which patient is not able to perform ADL (activities of daily living) or even
move. Nurse need to give intervention like assisting with ADL’s where possible and
relevant medication to decrease pain when mobilising (Chen et al., 2015).
3. The third high priority is the post-operative delirium which is the side effect of general
anaesthesia (Raats et al., 2015). Nurses have to manage the cognitive behaviour of the
patient to ensure a safe environment for the patient and all others in the ward.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7Case Study - Ivan Jankovic
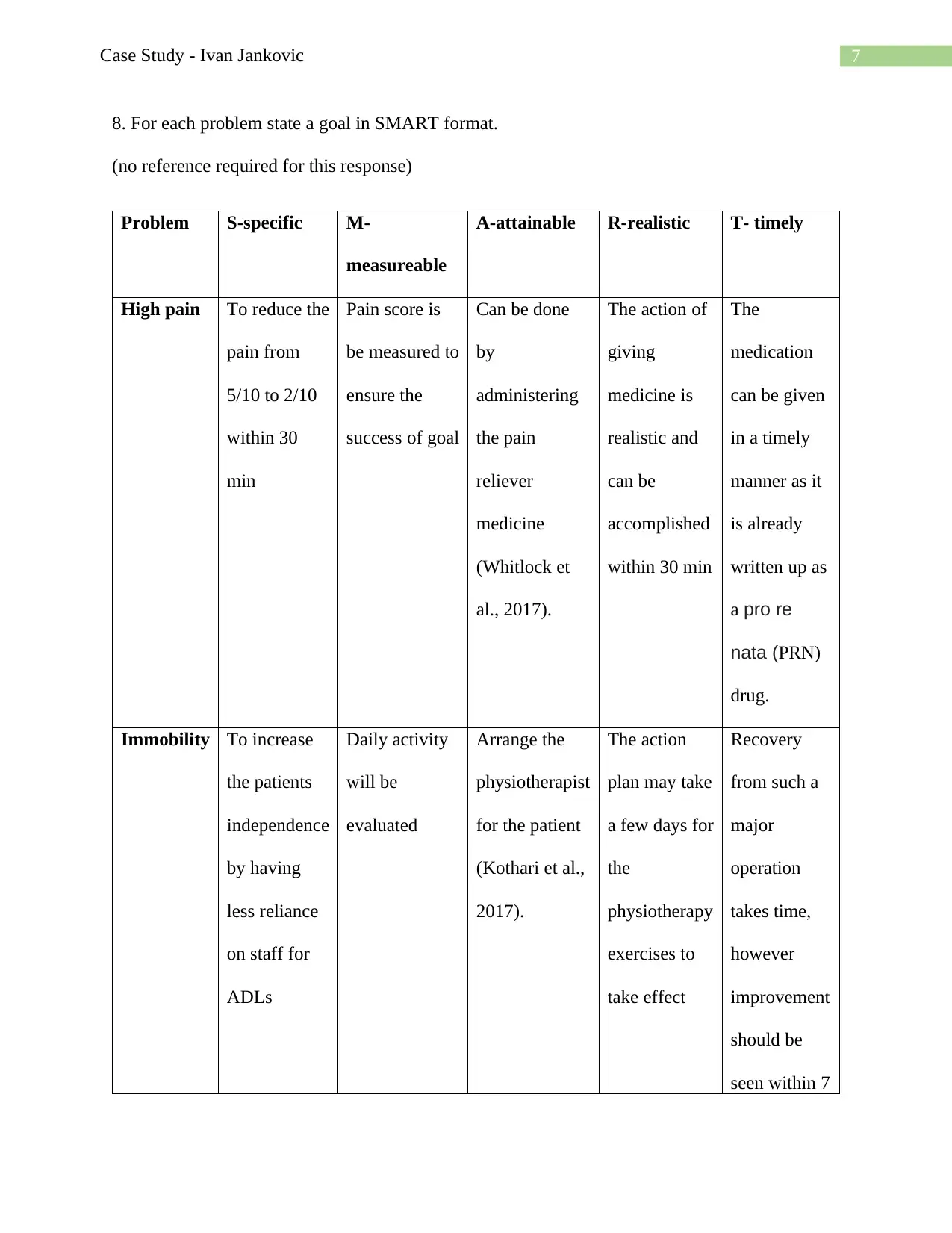
8. For each problem state a goal in SMART format.
(no reference required for this response)
Problem S-specific M-
measureable
A-attainable R-realistic T- timely
High pain To reduce the
pain from
5/10 to 2/10
within 30
min
Pain score is
be measured to
ensure the
success of goal
Can be done
by
administering
the pain
reliever
medicine
(Whitlock et
al., 2017).
The action of
giving
medicine is
realistic and
can be
accomplished
within 30 min
The
medication
can be given
in a timely
manner as it
is already
written up as
a pro re
nata (PRN)
drug.
Immobility To increase
the patients
independence
by having
less reliance
on staff for
ADLs
Daily activity
will be
evaluated
Arrange the
physiotherapist
for the patient
(Kothari et al.,
2017).
The action
plan may take
a few days for
the
physiotherapy
exercises to
take effect
Recovery
from such a
major
operation
takes time,
however
improvement
should be
seen within 7
8. For each problem state a goal in SMART format.
(no reference required for this response)
Problem S-specific M-
measureable
A-attainable R-realistic T- timely
High pain To reduce the
pain from
5/10 to 2/10
within 30
min
Pain score is
be measured to
ensure the
success of goal
Can be done
by
administering
the pain
reliever
medicine
(Whitlock et
al., 2017).
The action of
giving
medicine is
realistic and
can be
accomplished
within 30 min
The
medication
can be given
in a timely
manner as it
is already
written up as
a pro re
nata (PRN)
drug.
Immobility To increase
the patients
independence
by having
less reliance
on staff for
ADLs
Daily activity
will be
evaluated
Arrange the
physiotherapist
for the patient
(Kothari et al.,
2017).
The action
plan may take
a few days for
the
physiotherapy
exercises to
take effect
Recovery
from such a
major
operation
takes time,
however
improvement
should be
seen within 7
8Case Study - Ivan Jankovic
days.
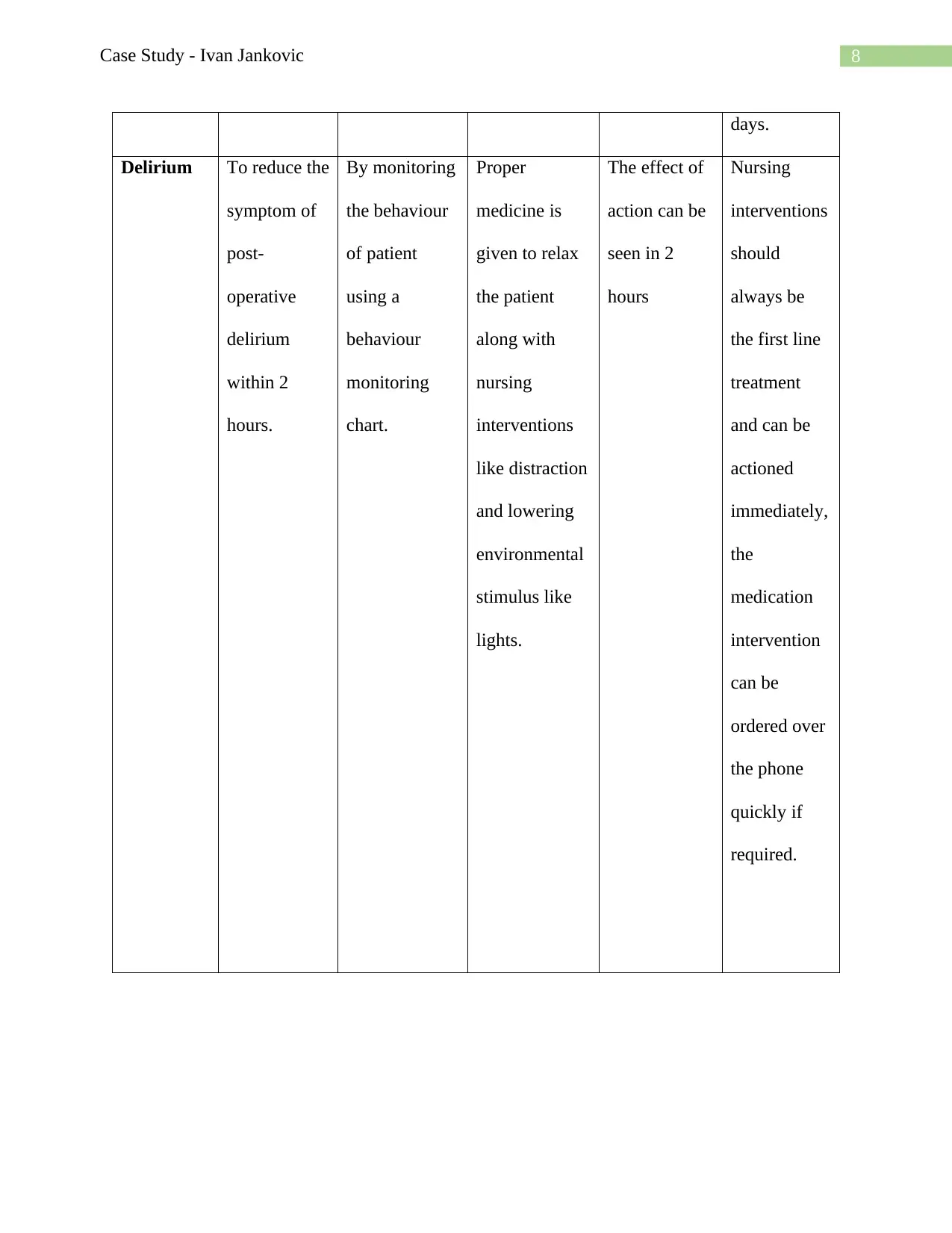
Delirium To reduce the
symptom of
post-
operative
delirium
within 2
hours.
By monitoring
the behaviour
of patient
using a
behaviour
monitoring
chart.
Proper
medicine is
given to relax
the patient
along with
nursing
interventions
like distraction
and lowering
environmental
stimulus like
lights.
The effect of
action can be
seen in 2
hours
Nursing
interventions
should
always be
the first line
treatment
and can be
actioned
immediately,
the
medication
intervention
can be
ordered over
the phone
quickly if
required.
days.
Delirium To reduce the
symptom of
post-
operative
delirium
within 2
hours.
By monitoring
the behaviour
of patient
using a
behaviour
monitoring
chart.
Proper
medicine is
given to relax
the patient
along with
nursing
interventions
like distraction
and lowering
environmental
stimulus like
lights.
The effect of
action can be
seen in 2
hours
Nursing
interventions
should
always be
the first line
treatment
and can be
actioned
immediately,
the
medication
intervention
can be
ordered over
the phone
quickly if
required.
9Case Study - Ivan Jankovic
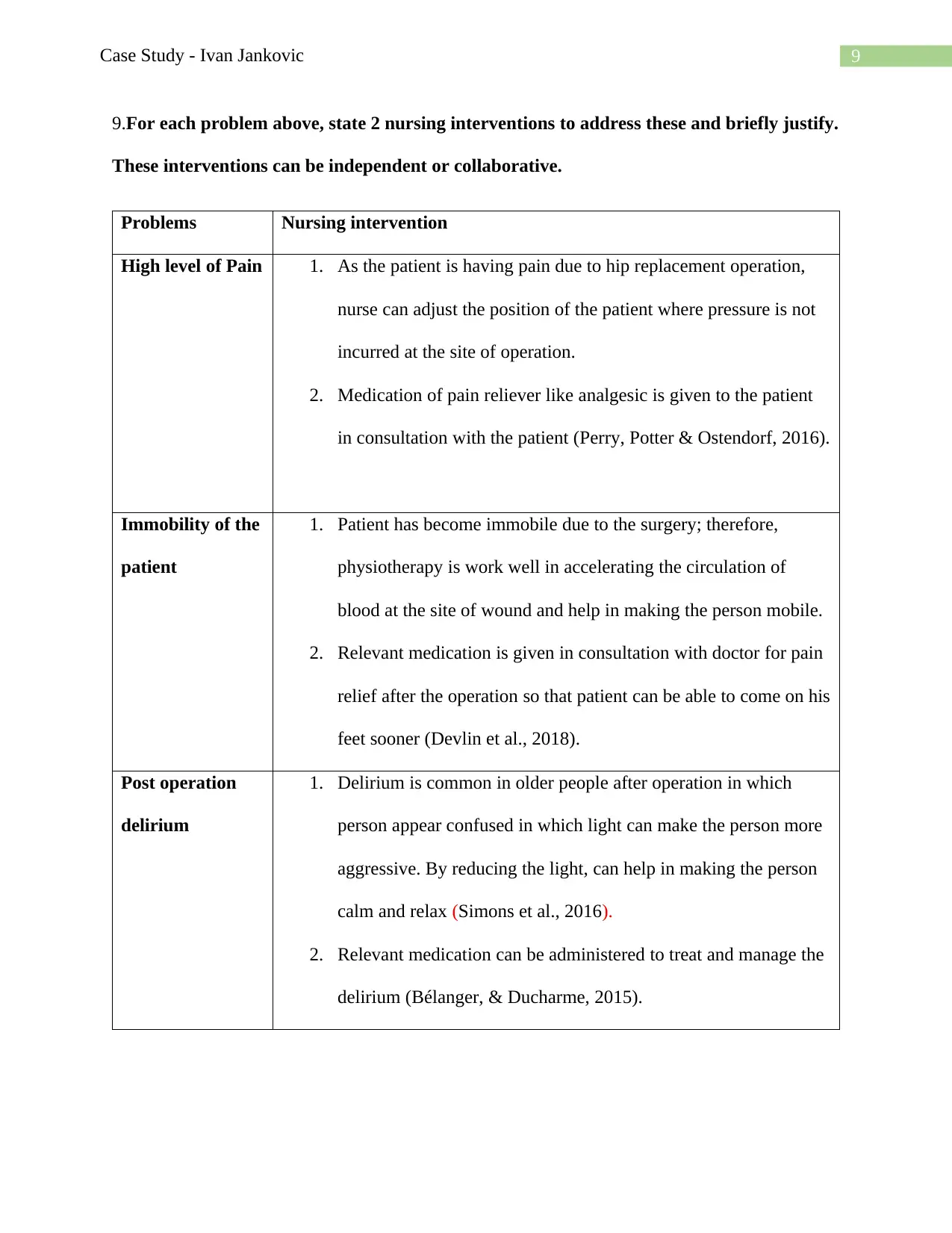
9.For each problem above, state 2 nursing interventions to address these and briefly justify.
These interventions can be independent or collaborative.
Problems Nursing intervention
High level of Pain 1. As the patient is having pain due to hip replacement operation,
nurse can adjust the position of the patient where pressure is not
incurred at the site of operation.
2. Medication of pain reliever like analgesic is given to the patient
in consultation with the patient (Perry, Potter & Ostendorf, 2016).
Immobility of the
patient
1. Patient has become immobile due to the surgery; therefore,
physiotherapy is work well in accelerating the circulation of
blood at the site of wound and help in making the person mobile.
2. Relevant medication is given in consultation with doctor for pain
relief after the operation so that patient can be able to come on his
feet sooner (Devlin et al., 2018).
Post operation
delirium
1. Delirium is common in older people after operation in which
person appear confused in which light can make the person more
aggressive. By reducing the light, can help in making the person
calm and relax (Simons et al., 2016).
2. Relevant medication can be administered to treat and manage the
delirium (Bélanger, & Ducharme, 2015).
9.For each problem above, state 2 nursing interventions to address these and briefly justify.
These interventions can be independent or collaborative.
Problems Nursing intervention
High level of Pain 1. As the patient is having pain due to hip replacement operation,
nurse can adjust the position of the patient where pressure is not
incurred at the site of operation.
2. Medication of pain reliever like analgesic is given to the patient
in consultation with the patient (Perry, Potter & Ostendorf, 2016).
Immobility of the
patient
1. Patient has become immobile due to the surgery; therefore,
physiotherapy is work well in accelerating the circulation of
blood at the site of wound and help in making the person mobile.
2. Relevant medication is given in consultation with doctor for pain
relief after the operation so that patient can be able to come on his
feet sooner (Devlin et al., 2018).
Post operation
delirium
1. Delirium is common in older people after operation in which
person appear confused in which light can make the person more
aggressive. By reducing the light, can help in making the person
calm and relax (Simons et al., 2016).
2. Relevant medication can be administered to treat and manage the
delirium (Bélanger, & Ducharme, 2015).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10Case Study - Ivan Jankovic
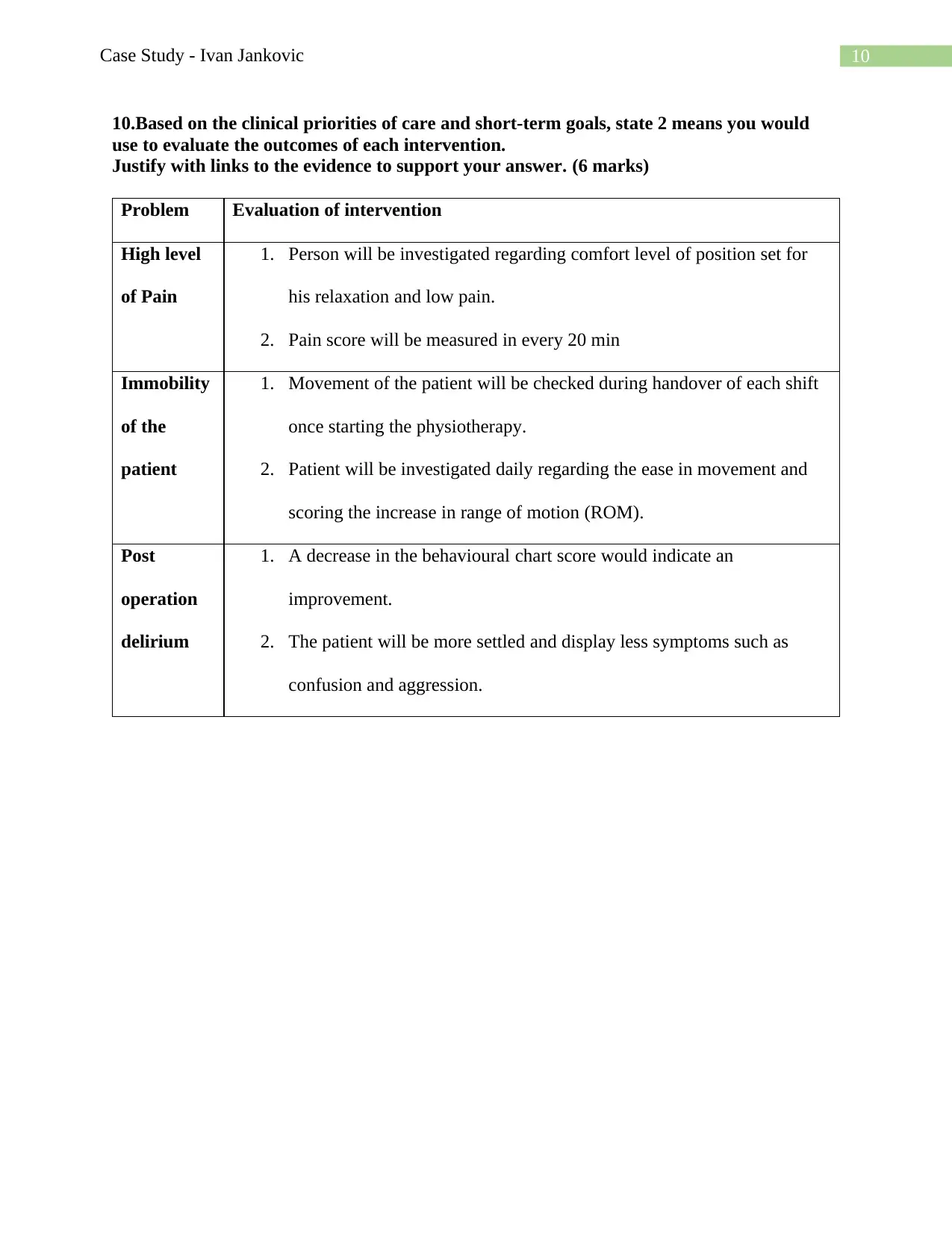
10.Based on the clinical priorities of care and short-term goals, state 2 means you would
use to evaluate the outcomes of each intervention.
Justify with links to the evidence to support your answer. (6 marks)
Problem Evaluation of intervention
High level
of Pain
1. Person will be investigated regarding comfort level of position set for
his relaxation and low pain.
2. Pain score will be measured in every 20 min
Immobility
of the
patient
1. Movement of the patient will be checked during handover of each shift
once starting the physiotherapy.
2. Patient will be investigated daily regarding the ease in movement and
scoring the increase in range of motion (ROM).
Post
operation
delirium
1. A decrease in the behavioural chart score would indicate an
improvement.
2. The patient will be more settled and display less symptoms such as
confusion and aggression.
10.Based on the clinical priorities of care and short-term goals, state 2 means you would
use to evaluate the outcomes of each intervention.
Justify with links to the evidence to support your answer. (6 marks)
Problem Evaluation of intervention
High level
of Pain
1. Person will be investigated regarding comfort level of position set for
his relaxation and low pain.
2. Pain score will be measured in every 20 min
Immobility
of the
patient
1. Movement of the patient will be checked during handover of each shift
once starting the physiotherapy.
2. Patient will be investigated daily regarding the ease in movement and
scoring the increase in range of motion (ROM).
Post
operation
delirium
1. A decrease in the behavioural chart score would indicate an
improvement.
2. The patient will be more settled and display less symptoms such as
confusion and aggression.
11Case Study - Ivan Jankovic
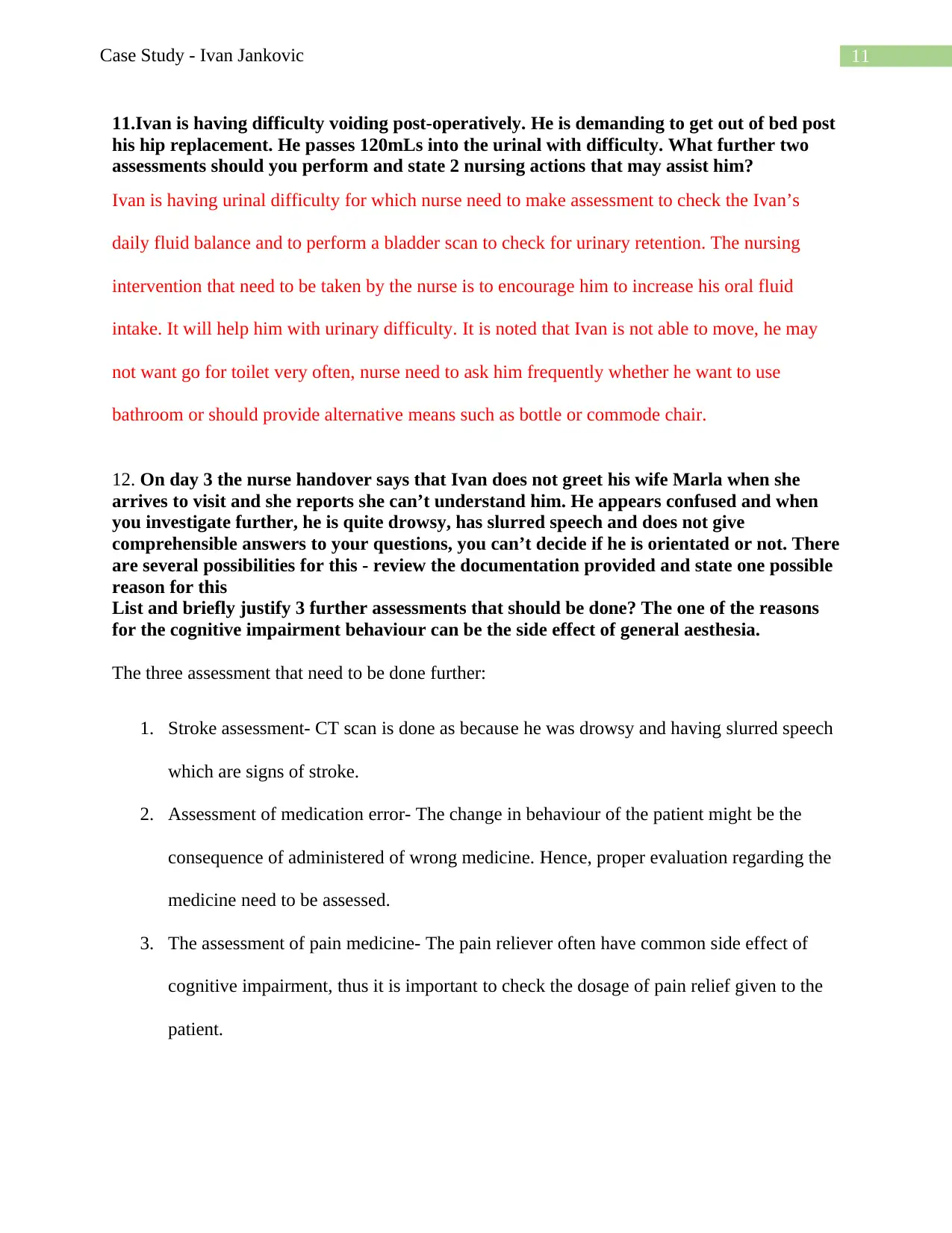
11.Ivan is having difficulty voiding post-operatively. He is demanding to get out of bed post
his hip replacement. He passes 120mLs into the urinal with difficulty. What further two
assessments should you perform and state 2 nursing actions that may assist him?
Ivan is having urinal difficulty for which nurse need to make assessment to check the Ivan’s
daily fluid balance and to perform a bladder scan to check for urinary retention. The nursing
intervention that need to be taken by the nurse is to encourage him to increase his oral fluid
intake. It will help him with urinary difficulty. It is noted that Ivan is not able to move, he may
not want go for toilet very often, nurse need to ask him frequently whether he want to use
bathroom or should provide alternative means such as bottle or commode chair.
12. On day 3 the nurse handover says that Ivan does not greet his wife Marla when she
arrives to visit and she reports she can’t understand him. He appears confused and when
you investigate further, he is quite drowsy, has slurred speech and does not give
comprehensible answers to your questions, you can’t decide if he is orientated or not. There
are several possibilities for this - review the documentation provided and state one possible
reason for this
List and briefly justify 3 further assessments that should be done? The one of the reasons
for the cognitive impairment behaviour can be the side effect of general aesthesia.
The three assessment that need to be done further:
1. Stroke assessment- CT scan is done as because he was drowsy and having slurred speech
which are signs of stroke.
2. Assessment of medication error- The change in behaviour of the patient might be the
consequence of administered of wrong medicine. Hence, proper evaluation regarding the
medicine need to be assessed.
3. The assessment of pain medicine- The pain reliever often have common side effect of
cognitive impairment, thus it is important to check the dosage of pain relief given to the
patient.
11.Ivan is having difficulty voiding post-operatively. He is demanding to get out of bed post
his hip replacement. He passes 120mLs into the urinal with difficulty. What further two
assessments should you perform and state 2 nursing actions that may assist him?
Ivan is having urinal difficulty for which nurse need to make assessment to check the Ivan’s
daily fluid balance and to perform a bladder scan to check for urinary retention. The nursing
intervention that need to be taken by the nurse is to encourage him to increase his oral fluid
intake. It will help him with urinary difficulty. It is noted that Ivan is not able to move, he may
not want go for toilet very often, nurse need to ask him frequently whether he want to use
bathroom or should provide alternative means such as bottle or commode chair.
12. On day 3 the nurse handover says that Ivan does not greet his wife Marla when she
arrives to visit and she reports she can’t understand him. He appears confused and when
you investigate further, he is quite drowsy, has slurred speech and does not give
comprehensible answers to your questions, you can’t decide if he is orientated or not. There
are several possibilities for this - review the documentation provided and state one possible
reason for this
List and briefly justify 3 further assessments that should be done? The one of the reasons
for the cognitive impairment behaviour can be the side effect of general aesthesia.
The three assessment that need to be done further:
1. Stroke assessment- CT scan is done as because he was drowsy and having slurred speech
which are signs of stroke.
2. Assessment of medication error- The change in behaviour of the patient might be the
consequence of administered of wrong medicine. Hence, proper evaluation regarding the
medicine need to be assessed.
3. The assessment of pain medicine- The pain reliever often have common side effect of
cognitive impairment, thus it is important to check the dosage of pain relief given to the
patient.
12Case Study - Ivan Jankovic
13. Outline the importance of discharge planning and 3 realistic strategies that could be put
into place for this elderly couple. (4 marks)
Discharge planning is important because it gives the accurate information about the health of
patient. It also ensures the type of quality care given and its connection between hospital and
community. The discharge planning is significant for the patients as it aims to reduce the length
of stay in the hospital and help to manage the unplanned readmission to the patients. Further, this
also improves the coordination of the type of service followed by the discharge from the hospital.
The three realistic strategies that help the wellbeing of the elderly patient are as follows:
1. Recommendation for community service- The strategy will help the elderly patients to
get domestic assistance through which he can get helped in his daily life activities and
living habits. As he the patient having problem in movement, taxi voucher can be given
to the patient to get assistance in travelling (Grossman et al., 2018).
2. Recommendation for community nurse- This will help the patient to get help proper
follow up medical care and reduce the chances of rehospitalisation (McTiernan &
McDonald, 2015).
3. Recommendation to community physiotherapist- This will help in giving proper and
timely exercise to the patient to further increase his mobility, along with suggesting
alterations around the home such as nonslip mats and rails in the shower that will help
prevent future falls. (Lewis, Peiris & Shields, 2017)
13. Outline the importance of discharge planning and 3 realistic strategies that could be put
into place for this elderly couple. (4 marks)
Discharge planning is important because it gives the accurate information about the health of
patient. It also ensures the type of quality care given and its connection between hospital and
community. The discharge planning is significant for the patients as it aims to reduce the length
of stay in the hospital and help to manage the unplanned readmission to the patients. Further, this
also improves the coordination of the type of service followed by the discharge from the hospital.
The three realistic strategies that help the wellbeing of the elderly patient are as follows:
1. Recommendation for community service- The strategy will help the elderly patients to
get domestic assistance through which he can get helped in his daily life activities and
living habits. As he the patient having problem in movement, taxi voucher can be given
to the patient to get assistance in travelling (Grossman et al., 2018).
2. Recommendation for community nurse- This will help the patient to get help proper
follow up medical care and reduce the chances of rehospitalisation (McTiernan &
McDonald, 2015).
3. Recommendation to community physiotherapist- This will help in giving proper and
timely exercise to the patient to further increase his mobility, along with suggesting
alterations around the home such as nonslip mats and rails in the shower that will help
prevent future falls. (Lewis, Peiris & Shields, 2017)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13Case Study - Ivan Jankovic
Reference
Bélanger, L., & Ducharme, F. (2015). Narrative-based educational nursing intervention for
managing hospitalized older adults at risk for delirium: field testing and qualitative
evaluation. Geriatric Nursing, 36(1), 40-46.
Björk, S., Juthberg, C., Lindkvist, M., Wimo, A., Sandman, P. O., Winblad, B., & Edvardsson,
D. (2016). Exploring the prevalence and variance of cognitive impairment, pain,
neuropsychiatric symptoms and ADL dependency among persons living in nursing
homes; a cross-sectional study. BMC geriatrics, 16(1), 154.
Bouroche, G., & Bourgain, J. L. (2015). Preoxygenation and general anesthesia: a
review. Minerva Anestesiol, 81(8), 910-20.
Chen, H., Gao, J., Su, S., Zhang, X., & Wang, Z. (2015). A visual-aided wireless monitoring
system design for total hip replacement surgery. IEEE transactions on biomedical
circuits and systems, 9(2), 227-236.
Devlin, J. W., Skrobik, Y., Gélinas, C., Needham, D. M., Slooter, A. J., Pandharipande, P. P., ...
& Balas, M. C. (2018). Clinical practice guidelines for the prevention and management of
pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the
ICU. Critical care medicine, 46(9), e825-e873.
Dohrn, N., Sommer, T., Bisgaard, J., Rønholm, E., & Larsen, J. F. (2016). Difficult tracheal
intubation in obese gastric bypass patients. Obesity surgery, 26(11), 2640-2647.
Garvey, W. T., Hurley, D. L., & Kushner, R. F. (2016). Patient-centered care of the patient with
obesity. Endocrine Practice, 22, 9.
Reference
Bélanger, L., & Ducharme, F. (2015). Narrative-based educational nursing intervention for
managing hospitalized older adults at risk for delirium: field testing and qualitative
evaluation. Geriatric Nursing, 36(1), 40-46.
Björk, S., Juthberg, C., Lindkvist, M., Wimo, A., Sandman, P. O., Winblad, B., & Edvardsson,
D. (2016). Exploring the prevalence and variance of cognitive impairment, pain,
neuropsychiatric symptoms and ADL dependency among persons living in nursing
homes; a cross-sectional study. BMC geriatrics, 16(1), 154.
Bouroche, G., & Bourgain, J. L. (2015). Preoxygenation and general anesthesia: a
review. Minerva Anestesiol, 81(8), 910-20.
Chen, H., Gao, J., Su, S., Zhang, X., & Wang, Z. (2015). A visual-aided wireless monitoring
system design for total hip replacement surgery. IEEE transactions on biomedical
circuits and systems, 9(2), 227-236.
Devlin, J. W., Skrobik, Y., Gélinas, C., Needham, D. M., Slooter, A. J., Pandharipande, P. P., ...
& Balas, M. C. (2018). Clinical practice guidelines for the prevention and management of
pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the
ICU. Critical care medicine, 46(9), e825-e873.
Dohrn, N., Sommer, T., Bisgaard, J., Rønholm, E., & Larsen, J. F. (2016). Difficult tracheal
intubation in obese gastric bypass patients. Obesity surgery, 26(11), 2640-2647.
Garvey, W. T., Hurley, D. L., & Kushner, R. F. (2016). Patient-centered care of the patient with
obesity. Endocrine Practice, 22, 9.
14Case Study - Ivan Jankovic
Glyn-Jones, S., Palmer, A. J. R., Agricola, R., Price, A. J., Vincent, T. L., Weinans, H., & Carr,
A. J. (2015). Osteoarthritis. The Lancet, 386(9991), 376-387.
Grossman, D. C., Curry, S. J., Owens, D. K., Barry, M. J., Caughey, A. B., Davidson, K. W., ...
& Kubik, M. (2018). Interventions to prevent falls in community-dwelling older adults:
US Preventive Services Task Force recommendation statement. Jama, 319(16), 1696-
1704.
Gul, O. O., Cander, S., Gul, B., Açıkgoz, E., Sarandol, E., & Ersoy, C. (2015). Evaluation of
insulin resistance and plasma levels for visfatin and resistin in obese and non-obese
patients with polycystic ovary syndrome. European cytokine network, 26(4), 73-78.
Hasemann, W., Tolson, D., Godwin, J., Spirig, R., Frei, I. A., & Kressig, R. W. (2016). A before
and after study of a nurse led comprehensive delirium management programme
(DemDel) for older acute care inpatients with cognitive impairment. International
journal of nursing studies, 53, 27-38.
Hassan, M. H., & Abd-Allah, G. M. (2015). Effects of metformin plus gliclazide versus
metformin plus glimepiride on cardiovascular risk factors in patients with type 2 diabetes
mellitus. Pakistan journal of pharmaceutical sciences, 28(5).
Haugen, A. S., Søfteland, E., Almeland, S. K., Sevdalis, N., Vonen, B., Eide, G. E., ... &
Harthug, S. (2015). Effect of the World Health Organization checklist on patient
outcomes: a stepped wedge cluster randomized controlled trial. Annals of
surgery, 261(5), 821-828.
Heymsfield, S. B., & Wadden, T. A. (2017). Mechanisms, pathophysiology, and management of
obesity. New England Journal of Medicine, 376(3), 254-266.
Glyn-Jones, S., Palmer, A. J. R., Agricola, R., Price, A. J., Vincent, T. L., Weinans, H., & Carr,
A. J. (2015). Osteoarthritis. The Lancet, 386(9991), 376-387.
Grossman, D. C., Curry, S. J., Owens, D. K., Barry, M. J., Caughey, A. B., Davidson, K. W., ...
& Kubik, M. (2018). Interventions to prevent falls in community-dwelling older adults:
US Preventive Services Task Force recommendation statement. Jama, 319(16), 1696-
1704.
Gul, O. O., Cander, S., Gul, B., Açıkgoz, E., Sarandol, E., & Ersoy, C. (2015). Evaluation of
insulin resistance and plasma levels for visfatin and resistin in obese and non-obese
patients with polycystic ovary syndrome. European cytokine network, 26(4), 73-78.
Hasemann, W., Tolson, D., Godwin, J., Spirig, R., Frei, I. A., & Kressig, R. W. (2016). A before
and after study of a nurse led comprehensive delirium management programme
(DemDel) for older acute care inpatients with cognitive impairment. International
journal of nursing studies, 53, 27-38.
Hassan, M. H., & Abd-Allah, G. M. (2015). Effects of metformin plus gliclazide versus
metformin plus glimepiride on cardiovascular risk factors in patients with type 2 diabetes
mellitus. Pakistan journal of pharmaceutical sciences, 28(5).
Haugen, A. S., Søfteland, E., Almeland, S. K., Sevdalis, N., Vonen, B., Eide, G. E., ... &
Harthug, S. (2015). Effect of the World Health Organization checklist on patient
outcomes: a stepped wedge cluster randomized controlled trial. Annals of
surgery, 261(5), 821-828.
Heymsfield, S. B., & Wadden, T. A. (2017). Mechanisms, pathophysiology, and management of
obesity. New England Journal of Medicine, 376(3), 254-266.
15Case Study - Ivan Jankovic
Kido, H., Komasawa, N., Matsunami, S., Kusaka, Y., & Minami, T. (2015). Comparison of
McGRATH MAC and Macintosh laryngoscopes for double-lumen endotracheal tube
intubation by anesthesia residents: a prospect
Kothari, M. K., Shah, K. C., Tikoo, A., & Nene, A. M. (2016). Surgical management in elderly
patients with tuberculous spondylodiscitis: ten year mortality audit study. Asian spine
journal, 10(5), 915.
Kulkarni, K., Karssiens, T., Kumar, V., & Pandit, H. (2016). Obesity and
osteoarthritis. Maturitas, 89, 22-28.
Lee, C. M. Y., Goode, B., Nørtoft, E., Shaw, J. E., Magliano, D. J., & Colagiuri, S. (2018). The
cost of diabetes and obesity in Australia. Journal of medical economics, 21(10), 1001-
1005.
Lewis, M., Peiris, C. L., & Shields, N. (2017). Long-term home and community-based exercise
programs improve function in community-dwelling older people with cognitive
impairment: a systematic review. Journal of physiotherapy, 63(1), 23-29.
Marcantonio, E. R. (2017). Delirium in hospitalized older adults. New England Journal of
Medicine, 377(15), 1456-1466.
McTiernan, K., & McDonald, N. (2015). Occupational stressors, burnout and coping strategies
between hospital and community psychiatric nurses in a D ublin region. Journal of
psychiatric and mental health nursing, 22(3), 208-218.
Molina, G., Jiang, W., Edmondson, L., Gibbons, L., Huang, L. C., Kiang, M. V., ... & Singer, S.
J. (2016). Implementation of the surgical safety checklist in South Carolina hospitals is
Kido, H., Komasawa, N., Matsunami, S., Kusaka, Y., & Minami, T. (2015). Comparison of
McGRATH MAC and Macintosh laryngoscopes for double-lumen endotracheal tube
intubation by anesthesia residents: a prospect
Kothari, M. K., Shah, K. C., Tikoo, A., & Nene, A. M. (2016). Surgical management in elderly
patients with tuberculous spondylodiscitis: ten year mortality audit study. Asian spine
journal, 10(5), 915.
Kulkarni, K., Karssiens, T., Kumar, V., & Pandit, H. (2016). Obesity and
osteoarthritis. Maturitas, 89, 22-28.
Lee, C. M. Y., Goode, B., Nørtoft, E., Shaw, J. E., Magliano, D. J., & Colagiuri, S. (2018). The
cost of diabetes and obesity in Australia. Journal of medical economics, 21(10), 1001-
1005.
Lewis, M., Peiris, C. L., & Shields, N. (2017). Long-term home and community-based exercise
programs improve function in community-dwelling older people with cognitive
impairment: a systematic review. Journal of physiotherapy, 63(1), 23-29.
Marcantonio, E. R. (2017). Delirium in hospitalized older adults. New England Journal of
Medicine, 377(15), 1456-1466.
McTiernan, K., & McDonald, N. (2015). Occupational stressors, burnout and coping strategies
between hospital and community psychiatric nurses in a D ublin region. Journal of
psychiatric and mental health nursing, 22(3), 208-218.
Molina, G., Jiang, W., Edmondson, L., Gibbons, L., Huang, L. C., Kiang, M. V., ... & Singer, S.
J. (2016). Implementation of the surgical safety checklist in South Carolina hospitals is
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16Case Study - Ivan Jankovic
associated with improvement in perceived perioperative safety. Journal of the American
College of Surgeons, 222(5), 725-736.
National Safety and Quality Health Service Standards (2012) Retrieved from
https://www.safetyandquality.gov.au/wp-content/uploads/2011/09/NSQHS-Standards-
Sept-2012.pdf
Nightingale, C. E., Margarson, M. P., Shearer, E., Redman, J. W., Lucas, D. N., ... & Skues, M.
(2015). Peri‐operative management of the obese surgical patient 2015: Association of
Anaesthetists of Great Britain and Ireland Society for Obesity and Bariatric
Anaesthesia. Anaesthesia, 70(7), 859-876.
Nuttall, F. Q. (2015). Body mass index: obesity, BMI, and health: a critical review. Nutrition
today, 50(3), 117.
Perry, A. G., Potter, P. A., & Ostendorf, W. (2015). Nursing Interventions & Clinical Skills-E-
Book. Elsevier Health Sciences.
Raats, J. W., van Eijsden, W. A., Crolla, R. M., Steyerberg, E. W., & van der Laan, L. (2015).
Risk factors and outcomes for postoperative delirium after major surgery in elderly
patients. PLoS One, 10(8), e0136071.
Shoair, O. A., Grasso II, M. P., Lahaye, L. A., Daniel, R., Biddle, C. J., & Slattum, P. W. (2015).
Incidence and risk factors for postoperative cognitive dysfunction in older adults
undergoing major noncardiac surgery: a prospective study. Journal of anaesthesiology,
clinical pharmacology, 31(1), 30.
associated with improvement in perceived perioperative safety. Journal of the American
College of Surgeons, 222(5), 725-736.
National Safety and Quality Health Service Standards (2012) Retrieved from
https://www.safetyandquality.gov.au/wp-content/uploads/2011/09/NSQHS-Standards-
Sept-2012.pdf
Nightingale, C. E., Margarson, M. P., Shearer, E., Redman, J. W., Lucas, D. N., ... & Skues, M.
(2015). Peri‐operative management of the obese surgical patient 2015: Association of
Anaesthetists of Great Britain and Ireland Society for Obesity and Bariatric
Anaesthesia. Anaesthesia, 70(7), 859-876.
Nuttall, F. Q. (2015). Body mass index: obesity, BMI, and health: a critical review. Nutrition
today, 50(3), 117.
Perry, A. G., Potter, P. A., & Ostendorf, W. (2015). Nursing Interventions & Clinical Skills-E-
Book. Elsevier Health Sciences.
Raats, J. W., van Eijsden, W. A., Crolla, R. M., Steyerberg, E. W., & van der Laan, L. (2015).
Risk factors and outcomes for postoperative delirium after major surgery in elderly
patients. PLoS One, 10(8), e0136071.
Shoair, O. A., Grasso II, M. P., Lahaye, L. A., Daniel, R., Biddle, C. J., & Slattum, P. W. (2015).
Incidence and risk factors for postoperative cognitive dysfunction in older adults
undergoing major noncardiac surgery: a prospective study. Journal of anaesthesiology,
clinical pharmacology, 31(1), 30.
17Case Study - Ivan Jankovic
Simons, K. S., Laheij, R. J., van den Boogaard, M., Moviat, M. A., Paling, A. J., Polderman, F.
N., ... & de Jager, C. P. (2016). Dynamic light application therapy to reduce the incidence
and duration of delirium in intensive-care patients: a randomised controlled trial. The
Lancet Respiratory Medicine, 4(3), 194-202.
Smolowitz, J., Speakman, E., Wojnar, D., Whelan, E. M., Ulrich, S., Hayes, C., & Wood, L.
(2015). Role of the registered nurse in primary health care: Meeting health care needs in
the 21st century. Nursing Outlook, 63(2), 130-136.
Smolowitz, J., Speakman, E., Wojnar, D., Whelan, E. M., Ulrich, S., Hayes, C., & Wood, L.
(2015). Role of the registered nurse in primary health care: Meeting health care needs in
the 21st century. Nursing Outlook, 63(2), 130-136.
Surve, R., Bansal, S., Sriganesh, K., Subbakrishna, D. K., Thirthalli, J., & Rao, G. S. U. (2015).
Incidence and risk factors for oxygen desaturation during recovery from modified
electroconvulsive therapy: A prospective observational study. Journal of
anaesthesiology, clinical pharmacology, 31(1), 99.
Tjeertes, E. E., Hoeks, S. S., Beks, S. S., Valentijn, T. T., Hoofwijk, A. A., & Stolker, R. J. R.
(2015). Obesity–a risk factor for postoperative complications in general surgery?. BMC
anesthesiology, 15(1), 112.
Urden, L.D., Stacy, K.M. and Lough, M.E., 2019. Priorities in critical care nursing. Elsevier
Health Sciences.
Whitlock, E. L., Diaz-Ramirez, L. G., Glymour, M. M., Boscardin, W. J., Covinsky, K. E., &
Smith, A. K. (2017). Association between persistent pain and memory decline and
dementia in a longitudinal cohort of elders. JAMA internal medicine, 177(8), 1146-1153.
Simons, K. S., Laheij, R. J., van den Boogaard, M., Moviat, M. A., Paling, A. J., Polderman, F.
N., ... & de Jager, C. P. (2016). Dynamic light application therapy to reduce the incidence
and duration of delirium in intensive-care patients: a randomised controlled trial. The
Lancet Respiratory Medicine, 4(3), 194-202.
Smolowitz, J., Speakman, E., Wojnar, D., Whelan, E. M., Ulrich, S., Hayes, C., & Wood, L.
(2015). Role of the registered nurse in primary health care: Meeting health care needs in
the 21st century. Nursing Outlook, 63(2), 130-136.
Smolowitz, J., Speakman, E., Wojnar, D., Whelan, E. M., Ulrich, S., Hayes, C., & Wood, L.
(2015). Role of the registered nurse in primary health care: Meeting health care needs in
the 21st century. Nursing Outlook, 63(2), 130-136.
Surve, R., Bansal, S., Sriganesh, K., Subbakrishna, D. K., Thirthalli, J., & Rao, G. S. U. (2015).
Incidence and risk factors for oxygen desaturation during recovery from modified
electroconvulsive therapy: A prospective observational study. Journal of
anaesthesiology, clinical pharmacology, 31(1), 99.
Tjeertes, E. E., Hoeks, S. S., Beks, S. S., Valentijn, T. T., Hoofwijk, A. A., & Stolker, R. J. R.
(2015). Obesity–a risk factor for postoperative complications in general surgery?. BMC
anesthesiology, 15(1), 112.
Urden, L.D., Stacy, K.M. and Lough, M.E., 2019. Priorities in critical care nursing. Elsevier
Health Sciences.
Whitlock, E. L., Diaz-Ramirez, L. G., Glymour, M. M., Boscardin, W. J., Covinsky, K. E., &
Smith, A. K. (2017). Association between persistent pain and memory decline and
dementia in a longitudinal cohort of elders. JAMA internal medicine, 177(8), 1146-1153.

18Case Study - Ivan Jankovic
1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.



