The Role of Clinical Leadership in Healthcare
VerifiedAdded on 2020/03/13
|9
|2309
|85
AI Summary
This assignment delves into the significance of clinical leadership within the healthcare sector. It examines how effective leadership can contribute to enhanced patient safety, improved quality of care, and a more positive healthcare environment. The discussion encompasses various aspects of clinical leadership, drawing upon relevant research, case studies, and industry standards.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Leadership
Leadership
Question-1
Quality in Health system with TQM and CQI elements
The term ‘Quality’ means the degree/ grade of excellence. According to Institute of-
Medicine, health care quality is defined as ‘the grade/ degree to which the health-related services
that are rendered to persons and communities maximizes the chance of getting desired health-
related outcomes as well as consistent with prevailing health care professional knowledge’
(AHRQ, 2012). Quality in health organization involves practicing health care interventions
appropriately based on the pre-established procedural standards, with an objective of satisfying
the patients as well as maximizing health outcomes without creating health- related risks and/or
unnecessary expenditure.
The elements of quality include providing safe, effective, patient- centered, timely,
efficient and equitable care (AHRQ, 2017). There are various approaches of quality management
in which total quality management (TQM) that is called as continuous quality improvement
(CQI) in a health system, indulges itself in analyzing the health- related issues, planning
corrective actions, implementing these actions in needed areas and evaluating the effectiveness
of these action (NCCHC, 2017). TQM helps to constantly improve the work performance at all
the levels of system in each and every departmental (functional) area of a health organization
utilizing man, money and material resources. AIHW (2017) has stated that Australia peaks high
internationally in quality improvement and remains as one of the top performer in OECD
countries. CQI aims to minimize the capital and waste of poorer quality-care. The elements of
TQM and CQI are as follows: a). the customer/patients focus, whose health-needs are paramount
in quality determination. Customer satisfaction, analyzing ownership with services by
1
Leadership
Question-1
Quality in Health system with TQM and CQI elements
The term ‘Quality’ means the degree/ grade of excellence. According to Institute of-
Medicine, health care quality is defined as ‘the grade/ degree to which the health-related services
that are rendered to persons and communities maximizes the chance of getting desired health-
related outcomes as well as consistent with prevailing health care professional knowledge’
(AHRQ, 2012). Quality in health organization involves practicing health care interventions
appropriately based on the pre-established procedural standards, with an objective of satisfying
the patients as well as maximizing health outcomes without creating health- related risks and/or
unnecessary expenditure.
The elements of quality include providing safe, effective, patient- centered, timely,
efficient and equitable care (AHRQ, 2017). There are various approaches of quality management
in which total quality management (TQM) that is called as continuous quality improvement
(CQI) in a health system, indulges itself in analyzing the health- related issues, planning
corrective actions, implementing these actions in needed areas and evaluating the effectiveness
of these action (NCCHC, 2017). TQM helps to constantly improve the work performance at all
the levels of system in each and every departmental (functional) area of a health organization
utilizing man, money and material resources. AIHW (2017) has stated that Australia peaks high
internationally in quality improvement and remains as one of the top performer in OECD
countries. CQI aims to minimize the capital and waste of poorer quality-care. The elements of
TQM and CQI are as follows: a). the customer/patients focus, whose health-needs are paramount
in quality determination. Customer satisfaction, analyzing ownership with services by
1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Leadership
customer/patient opinion surveys, minimizing errors, avoiding reasons for dissatisfaction,
maintaining societal relationships, following business ethics, maintaining safe environment,
sharing quality- standards in organization are needed (McLaughlin, 2012). b). Strategic planning
with leadership to promote customer’s expectations, newer diagnostic techniques, advanced
developments, evolving customer-care system and societal expectations. c). Continuous
improvement with learning: regular planning, implementation and evolution. d). Empowerment
with team-work. e) Improving process management. f). Team-building and group-integration
tools. g) Quality Assurance and Control.
Question-2
Client safety & maintenance of safe healthcare
The entire health system revolves around the patients by keeping them as their
cornerstone. All the health professionals and organizations work for the welfare of the patients
and hence they should be the core of quality performance. Their safety represents the quality of
health organization and the safety of health organization also means the same. Safety is one of
the quality dimensions which involve preventing harm to the clients that could be either
temporary or permanent (Douglas, 2012). The health organizations should provide a safe
environment to the patients by keeping them free from injuries due to accidents or preventable
traumas that occurs in health organization (AHRQ, 2012). Safety means protecting the clients
from harm/ injuries and Quality means maintaining appropriateness and effectiveness and hence
safety and quality in health systems means People + Systems i.e. providing appropriate and
effective care to clients without causing harm.
The Australian- National health performance committee has stated about maintaining
safety in health organization by linking it with preventing and/or reducing harm that actually or
2
customer/patient opinion surveys, minimizing errors, avoiding reasons for dissatisfaction,
maintaining societal relationships, following business ethics, maintaining safe environment,
sharing quality- standards in organization are needed (McLaughlin, 2012). b). Strategic planning
with leadership to promote customer’s expectations, newer diagnostic techniques, advanced
developments, evolving customer-care system and societal expectations. c). Continuous
improvement with learning: regular planning, implementation and evolution. d). Empowerment
with team-work. e) Improving process management. f). Team-building and group-integration
tools. g) Quality Assurance and Control.
Question-2
Client safety & maintenance of safe healthcare
The entire health system revolves around the patients by keeping them as their
cornerstone. All the health professionals and organizations work for the welfare of the patients
and hence they should be the core of quality performance. Their safety represents the quality of
health organization and the safety of health organization also means the same. Safety is one of
the quality dimensions which involve preventing harm to the clients that could be either
temporary or permanent (Douglas, 2012). The health organizations should provide a safe
environment to the patients by keeping them free from injuries due to accidents or preventable
traumas that occurs in health organization (AHRQ, 2012). Safety means protecting the clients
from harm/ injuries and Quality means maintaining appropriateness and effectiveness and hence
safety and quality in health systems means People + Systems i.e. providing appropriate and
effective care to clients without causing harm.
The Australian- National health performance committee has stated about maintaining
safety in health organization by linking it with preventing and/or reducing harm that actually or
2
Leadership
potentially occurs in an organization or in an internal (hospital) environment to an acceptable
limit. It was estimated that nearly 12% of the adverse events occurs every year in Australia in
which 50% of them are avoidable and at-least 1 in 300 has chance of getting injury as compared
to only 1 in 1 million aircraft traveller. Nearly 0.04% (1,782) Australian patients encounter death
or serious harm and 0.149% of patients encounter temporary or less harm every year. They
commonly encounter harm due to drug error, patient falls, and hospital acquired infection and
suicide. Approximately 500,000 Australians become sick due to hospital admissions and turn
back for further treatment (Dunlevy, 2013). Hence, maintaining safety in an organization is
crucial to protect patients from harm and thereby to improve quality.
Question- 3
NSQHS standards- Quality
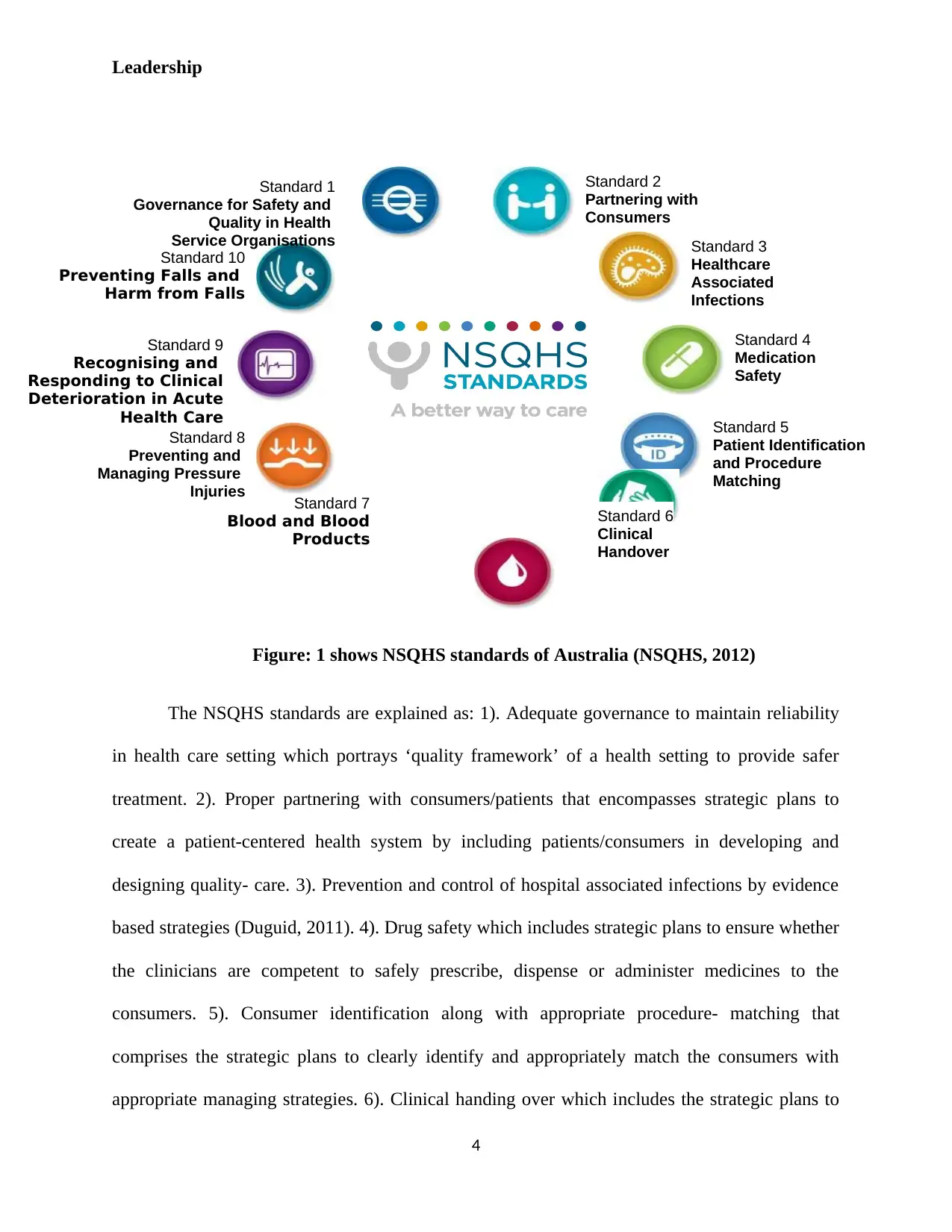
In 2012, Australia- Commission on safety with quality in health care has proposed
NSQHS standards to assist health organizations to render safe as well as high quality- care (Fig:
1). These standards were framed after an elaborate public, healthcare professionals and
stakeholder collaboration. Protecting people from harm and improving quality of the health-
services provided were the two aims of these standards. They form the basis for the accreditation
process as it helps in determining how and with what a health- organization’s performance will
be evaluated. The health-service organizations can compare these standards with its
performances and can use in internal quality-assurance and/or in external- accreditation process
(NSQHS, 2012).
3
potentially occurs in an organization or in an internal (hospital) environment to an acceptable
limit. It was estimated that nearly 12% of the adverse events occurs every year in Australia in
which 50% of them are avoidable and at-least 1 in 300 has chance of getting injury as compared
to only 1 in 1 million aircraft traveller. Nearly 0.04% (1,782) Australian patients encounter death
or serious harm and 0.149% of patients encounter temporary or less harm every year. They
commonly encounter harm due to drug error, patient falls, and hospital acquired infection and
suicide. Approximately 500,000 Australians become sick due to hospital admissions and turn
back for further treatment (Dunlevy, 2013). Hence, maintaining safety in an organization is
crucial to protect patients from harm and thereby to improve quality.
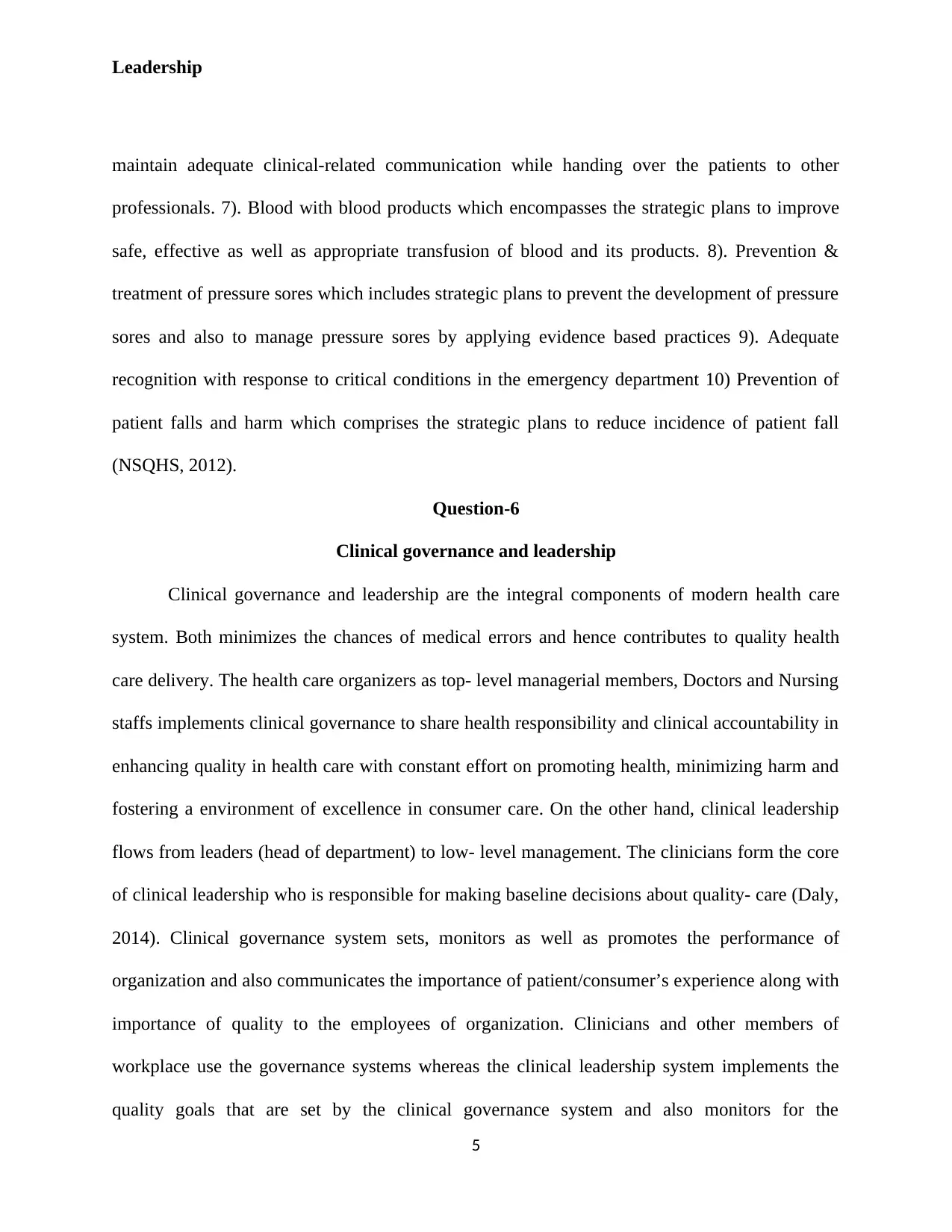
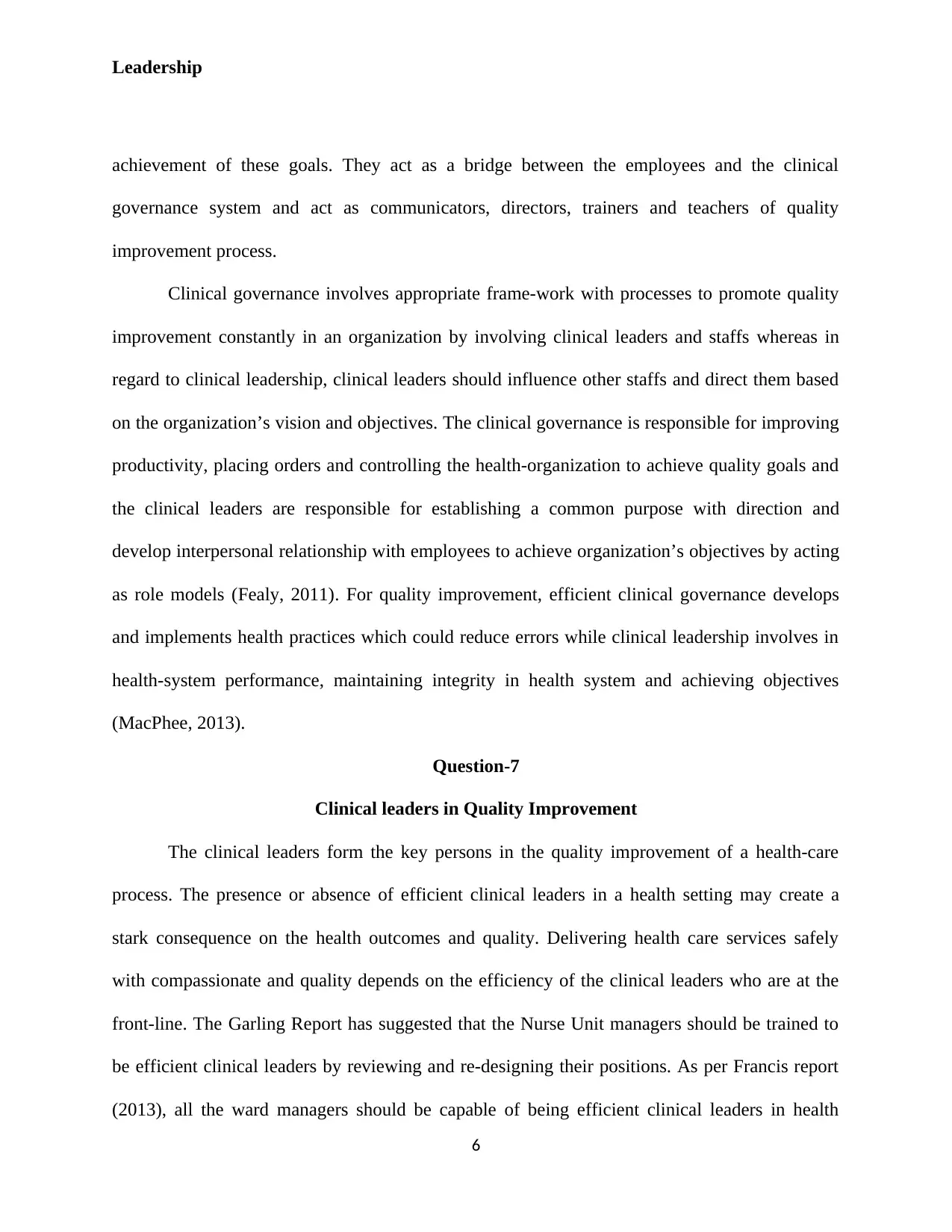
Question- 3
NSQHS standards- Quality
In 2012, Australia- Commission on safety with quality in health care has proposed
NSQHS standards to assist health organizations to render safe as well as high quality- care (Fig:
1). These standards were framed after an elaborate public, healthcare professionals and
stakeholder collaboration. Protecting people from harm and improving quality of the health-
services provided were the two aims of these standards. They form the basis for the accreditation
process as it helps in determining how and with what a health- organization’s performance will
be evaluated. The health-service organizations can compare these standards with its
performances and can use in internal quality-assurance and/or in external- accreditation process
(NSQHS, 2012).
3
Leadership
Figure: 1 shows NSQHS standards of Australia (NSQHS, 2012)
The NSQHS standards are explained as: 1). Adequate governance to maintain reliability
in health care setting which portrays ‘quality framework’ of a health setting to provide safer
treatment. 2). Proper partnering with consumers/patients that encompasses strategic plans to
create a patient-centered health system by including patients/consumers in developing and
designing quality- care. 3). Prevention and control of hospital associated infections by evidence
based strategies (Duguid, 2011). 4). Drug safety which includes strategic plans to ensure whether
the clinicians are competent to safely prescribe, dispense or administer medicines to the
consumers. 5). Consumer identification along with appropriate procedure- matching that
comprises the strategic plans to clearly identify and appropriately match the consumers with
appropriate managing strategies. 6). Clinical handing over which includes the strategic plans to
4
Standard 7
Blood and Blood
Products
Standard 10
Preventing Falls and
Harm from Falls
Standard 1
Governance for Safety and
Quality in Health
Service Organisations
Standard 2
Partnering with
Consumers
Standard 4
Medication
Safety
Standard 3
Healthcare
Associated
Infections
Standard 8
Preventing and
Managing Pressure
Injuries
Standard 9
Recognising and
Responding to Clinical
Deterioration in Acute
Health Care Standard 5
Patient Identification
and Procedure
Matching
Standard 6
Clinical
Handover
Figure: 1 shows NSQHS standards of Australia (NSQHS, 2012)
The NSQHS standards are explained as: 1). Adequate governance to maintain reliability
in health care setting which portrays ‘quality framework’ of a health setting to provide safer
treatment. 2). Proper partnering with consumers/patients that encompasses strategic plans to
create a patient-centered health system by including patients/consumers in developing and
designing quality- care. 3). Prevention and control of hospital associated infections by evidence
based strategies (Duguid, 2011). 4). Drug safety which includes strategic plans to ensure whether
the clinicians are competent to safely prescribe, dispense or administer medicines to the
consumers. 5). Consumer identification along with appropriate procedure- matching that
comprises the strategic plans to clearly identify and appropriately match the consumers with
appropriate managing strategies. 6). Clinical handing over which includes the strategic plans to
4
Standard 7
Blood and Blood
Products
Standard 10
Preventing Falls and
Harm from Falls
Standard 1
Governance for Safety and
Quality in Health
Service Organisations
Standard 2
Partnering with
Consumers
Standard 4
Medication
Safety
Standard 3
Healthcare
Associated
Infections
Standard 8
Preventing and
Managing Pressure
Injuries
Standard 9
Recognising and
Responding to Clinical
Deterioration in Acute
Health Care Standard 5
Patient Identification
and Procedure
Matching
Standard 6
Clinical
Handover
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Leadership
maintain adequate clinical-related communication while handing over the patients to other
professionals. 7). Blood with blood products which encompasses the strategic plans to improve
safe, effective as well as appropriate transfusion of blood and its products. 8). Prevention &
treatment of pressure sores which includes strategic plans to prevent the development of pressure
sores and also to manage pressure sores by applying evidence based practices 9). Adequate
recognition with response to critical conditions in the emergency department 10) Prevention of
patient falls and harm which comprises the strategic plans to reduce incidence of patient fall
(NSQHS, 2012).
Question-6
Clinical governance and leadership
Clinical governance and leadership are the integral components of modern health care
system. Both minimizes the chances of medical errors and hence contributes to quality health
care delivery. The health care organizers as top- level managerial members, Doctors and Nursing
staffs implements clinical governance to share health responsibility and clinical accountability in
enhancing quality in health care with constant effort on promoting health, minimizing harm and
fostering a environment of excellence in consumer care. On the other hand, clinical leadership
flows from leaders (head of department) to low- level management. The clinicians form the core
of clinical leadership who is responsible for making baseline decisions about quality- care (Daly,
2014). Clinical governance system sets, monitors as well as promotes the performance of
organization and also communicates the importance of patient/consumer’s experience along with
importance of quality to the employees of organization. Clinicians and other members of
workplace use the governance systems whereas the clinical leadership system implements the
quality goals that are set by the clinical governance system and also monitors for the
5
maintain adequate clinical-related communication while handing over the patients to other
professionals. 7). Blood with blood products which encompasses the strategic plans to improve
safe, effective as well as appropriate transfusion of blood and its products. 8). Prevention &
treatment of pressure sores which includes strategic plans to prevent the development of pressure
sores and also to manage pressure sores by applying evidence based practices 9). Adequate
recognition with response to critical conditions in the emergency department 10) Prevention of
patient falls and harm which comprises the strategic plans to reduce incidence of patient fall
(NSQHS, 2012).
Question-6
Clinical governance and leadership
Clinical governance and leadership are the integral components of modern health care
system. Both minimizes the chances of medical errors and hence contributes to quality health
care delivery. The health care organizers as top- level managerial members, Doctors and Nursing
staffs implements clinical governance to share health responsibility and clinical accountability in
enhancing quality in health care with constant effort on promoting health, minimizing harm and
fostering a environment of excellence in consumer care. On the other hand, clinical leadership
flows from leaders (head of department) to low- level management. The clinicians form the core
of clinical leadership who is responsible for making baseline decisions about quality- care (Daly,
2014). Clinical governance system sets, monitors as well as promotes the performance of
organization and also communicates the importance of patient/consumer’s experience along with
importance of quality to the employees of organization. Clinicians and other members of
workplace use the governance systems whereas the clinical leadership system implements the
quality goals that are set by the clinical governance system and also monitors for the
5
Leadership
achievement of these goals. They act as a bridge between the employees and the clinical
governance system and act as communicators, directors, trainers and teachers of quality
improvement process.
Clinical governance involves appropriate frame-work with processes to promote quality
improvement constantly in an organization by involving clinical leaders and staffs whereas in
regard to clinical leadership, clinical leaders should influence other staffs and direct them based
on the organization’s vision and objectives. The clinical governance is responsible for improving
productivity, placing orders and controlling the health-organization to achieve quality goals and
the clinical leaders are responsible for establishing a common purpose with direction and
develop interpersonal relationship with employees to achieve organization’s objectives by acting
as role models (Fealy, 2011). For quality improvement, efficient clinical governance develops
and implements health practices which could reduce errors while clinical leadership involves in
health-system performance, maintaining integrity in health system and achieving objectives
(MacPhee, 2013).
Question-7
Clinical leaders in Quality Improvement
The clinical leaders form the key persons in the quality improvement of a health-care
process. The presence or absence of efficient clinical leaders in a health setting may create a
stark consequence on the health outcomes and quality. Delivering health care services safely
with compassionate and quality depends on the efficiency of the clinical leaders who are at the
front-line. The Garling Report has suggested that the Nurse Unit managers should be trained to
be efficient clinical leaders by reviewing and re-designing their positions. As per Francis report
(2013), all the ward managers should be capable of being efficient clinical leaders in health
6
achievement of these goals. They act as a bridge between the employees and the clinical
governance system and act as communicators, directors, trainers and teachers of quality
improvement process.
Clinical governance involves appropriate frame-work with processes to promote quality
improvement constantly in an organization by involving clinical leaders and staffs whereas in
regard to clinical leadership, clinical leaders should influence other staffs and direct them based
on the organization’s vision and objectives. The clinical governance is responsible for improving
productivity, placing orders and controlling the health-organization to achieve quality goals and
the clinical leaders are responsible for establishing a common purpose with direction and
develop interpersonal relationship with employees to achieve organization’s objectives by acting
as role models (Fealy, 2011). For quality improvement, efficient clinical governance develops
and implements health practices which could reduce errors while clinical leadership involves in
health-system performance, maintaining integrity in health system and achieving objectives
(MacPhee, 2013).
Question-7
Clinical leaders in Quality Improvement
The clinical leaders form the key persons in the quality improvement of a health-care
process. The presence or absence of efficient clinical leaders in a health setting may create a
stark consequence on the health outcomes and quality. Delivering health care services safely
with compassionate and quality depends on the efficiency of the clinical leaders who are at the
front-line. The Garling Report has suggested that the Nurse Unit managers should be trained to
be efficient clinical leaders by reviewing and re-designing their positions. As per Francis report
(2013), all the ward managers should be capable of being efficient clinical leaders in health
6
Leadership
setting (Daly, 2014). Therefore, the clinical leaders should strive to enhance health- care
performances and improve quality in health care by collaborating with clinicians and consumers
in this reform process (McNamara, 2011).
Clinical leader’s role is not predefined but emerges from hospital setting after gaining
expertise and their method of developing and facilitating sound interrelationships with health
team. The clinical leaders should be efficient in promoting innovations with changes through
quality improvement which could be achieved by understanding, influencing, and motivating
persons by establishing effective interpersonal relationship so as to exchange and learn practice
from others (McNamara, 2011). They should make the health team to understand about
organizational process which could in-turn enable quality-based changes.
The physician leaders must bring the physician perspective, implement initiatives and
communicates importance of quality to others and the nursing leaders must bring nursing
perspective, practice to their full extent, gain higher degrees, full collaborators with clinicians
and other health professionals and should make effective work-force planning with policy-
developing to improve quality in health setting (IOM, 2011, AHRQ, 2017). The clinical leaders
should make creative and innovative changes in health care, be efficient communicator in
consumer- staff environment, be courageous to handle situations, solve quality issues and
provide consumer-based care to promote quality.
7
setting (Daly, 2014). Therefore, the clinical leaders should strive to enhance health- care
performances and improve quality in health care by collaborating with clinicians and consumers
in this reform process (McNamara, 2011).
Clinical leader’s role is not predefined but emerges from hospital setting after gaining
expertise and their method of developing and facilitating sound interrelationships with health
team. The clinical leaders should be efficient in promoting innovations with changes through
quality improvement which could be achieved by understanding, influencing, and motivating
persons by establishing effective interpersonal relationship so as to exchange and learn practice
from others (McNamara, 2011). They should make the health team to understand about
organizational process which could in-turn enable quality-based changes.
The physician leaders must bring the physician perspective, implement initiatives and
communicates importance of quality to others and the nursing leaders must bring nursing
perspective, practice to their full extent, gain higher degrees, full collaborators with clinicians
and other health professionals and should make effective work-force planning with policy-
developing to improve quality in health setting (IOM, 2011, AHRQ, 2017). The clinical leaders
should make creative and innovative changes in health care, be efficient communicator in
consumer- staff environment, be courageous to handle situations, solve quality issues and
provide consumer-based care to promote quality.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Leadership
Reference
AHRQ. (2012). Agency for Healthcare Research and Quality: U.S. Department of Health &
Human Services. Retrieved from https://www.ahrq.gov/professionals/quality-patient-
safety/quality-resources/tools/chtoolbx/understand/index.html
AHRQ. (2017). Leadership Role in Improving Safety: U.S. Department of Health & Human
Services. Retrieved from https://psnet.ahrq.gov/primers/primer/32/organizational-
leadership-and-its-role-in-improving-safety
AIHW. (2017). Safety and quality of health care: Australian Institute of Health and Welfare-
Australian Government. Retrieved from http://www.aihw.gov.au/safety-and-quality-of-
health-care/
Daly, J et al. (2014). The importance of clinical leadership in the hospital setting: Journal of
Healthcare Leadership. 6: 75-83. Retrieved from https://doi.org/10.2147/JHL.S46161
Douglas, C. (2012). Potter and Perry’s Fundamentals of Nursing- Australian version. Missouri:
Elsevier
Duguid, M & Cruickshank, M. (2011). Antimicrobial Stewardship in Australian Hospitals.
Sydney: ACSHQC
Dunlevy, S. (2013). Why are hospitals are making us sick?: News Corp Australia Network.
Retrieved from http://www.news.com.au/national/why-are-hospitals-are-making-us-
sick/news-story/372d84c34ba6f9c2a06718990217062b
Fealy, G et al. (2011). Barriers to clinical leadership development: findings from a national
survey: J Clin Nurs. 20:2023–2032.
8
Reference
AHRQ. (2012). Agency for Healthcare Research and Quality: U.S. Department of Health &
Human Services. Retrieved from https://www.ahrq.gov/professionals/quality-patient-
safety/quality-resources/tools/chtoolbx/understand/index.html
AHRQ. (2017). Leadership Role in Improving Safety: U.S. Department of Health & Human
Services. Retrieved from https://psnet.ahrq.gov/primers/primer/32/organizational-
leadership-and-its-role-in-improving-safety
AIHW. (2017). Safety and quality of health care: Australian Institute of Health and Welfare-
Australian Government. Retrieved from http://www.aihw.gov.au/safety-and-quality-of-
health-care/
Daly, J et al. (2014). The importance of clinical leadership in the hospital setting: Journal of
Healthcare Leadership. 6: 75-83. Retrieved from https://doi.org/10.2147/JHL.S46161
Douglas, C. (2012). Potter and Perry’s Fundamentals of Nursing- Australian version. Missouri:
Elsevier
Duguid, M & Cruickshank, M. (2011). Antimicrobial Stewardship in Australian Hospitals.
Sydney: ACSHQC
Dunlevy, S. (2013). Why are hospitals are making us sick?: News Corp Australia Network.
Retrieved from http://www.news.com.au/national/why-are-hospitals-are-making-us-
sick/news-story/372d84c34ba6f9c2a06718990217062b
Fealy, G et al. (2011). Barriers to clinical leadership development: findings from a national
survey: J Clin Nurs. 20:2023–2032.
8
Leadership
Francis, R. (2013). Report of the Mid Staffordshire NHS Trust Public Inquiry-Executive
Summary. London, UK: The Stationary Office. Retrieved from
http://www.midstaffspublicinquiry.com/sites/default/files/report/Executive
%20summary.pdf
IOM-Institute of Medicine, (2011). Committee on the Robert Wood Johnson Foundation
Initiative on the Future of Nursing: The future of nursing: Leading change, advancing
health. Washington, DC: National Academies Press.
MacPhee, M et al. (2013). Global health care leadership development: trends to consider: J
Healthcare Leadership: 21–29.
McLaughlin, C.P. (2012). Implementing Continuous Quality Improvement in Health Care: A
Global Casebook. Sudbury, MA: Jones and Bartlett learning
McNamara, M et al. (2011). Boundary matters: clinical leadership and the distinctive
disciplinary contribution of nursing to multidisciplinary care: J Clin Nurs. 20 (23–
24):3502–3512.
NCCHC. (2017). Continuous quality improvement: National Commission on correctional Health
care. http://www.ncchc.org/spotlight-on-the-standards-24-1
NSQHS. (2012). National Safety and Quality Health Service Standards: Australian’s
Commission on Safety & Quality in health-care. Retrieved from
https://www.safetyandquality.gov.au/wp-content/uploads/2011/09/NSQHS-Standards-
Sept-2012.pdf
9
Francis, R. (2013). Report of the Mid Staffordshire NHS Trust Public Inquiry-Executive
Summary. London, UK: The Stationary Office. Retrieved from
http://www.midstaffspublicinquiry.com/sites/default/files/report/Executive
%20summary.pdf
IOM-Institute of Medicine, (2011). Committee on the Robert Wood Johnson Foundation
Initiative on the Future of Nursing: The future of nursing: Leading change, advancing
health. Washington, DC: National Academies Press.
MacPhee, M et al. (2013). Global health care leadership development: trends to consider: J
Healthcare Leadership: 21–29.
McLaughlin, C.P. (2012). Implementing Continuous Quality Improvement in Health Care: A
Global Casebook. Sudbury, MA: Jones and Bartlett learning
McNamara, M et al. (2011). Boundary matters: clinical leadership and the distinctive
disciplinary contribution of nursing to multidisciplinary care: J Clin Nurs. 20 (23–
24):3502–3512.
NCCHC. (2017). Continuous quality improvement: National Commission on correctional Health
care. http://www.ncchc.org/spotlight-on-the-standards-24-1
NSQHS. (2012). National Safety and Quality Health Service Standards: Australian’s
Commission on Safety & Quality in health-care. Retrieved from
https://www.safetyandquality.gov.au/wp-content/uploads/2011/09/NSQHS-Standards-
Sept-2012.pdf
9
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.


