Social Determinants of Health in a Case Study
Added on 2022-12-27
10 Pages2558 Words99 Views
1 Assignment 2
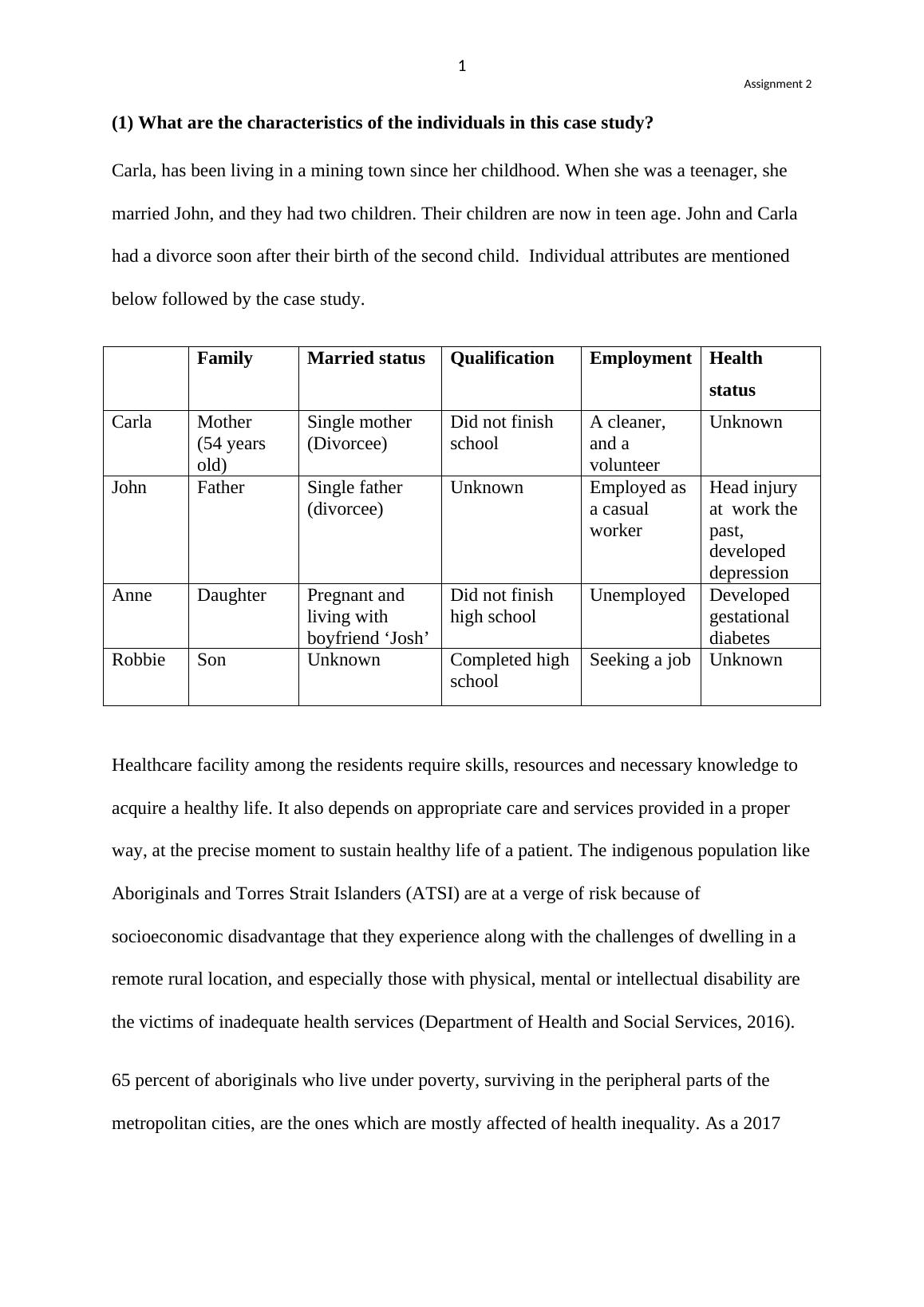
(1) What are the characteristics of the individuals in this case study?
Carla, has been living in a mining town since her childhood. When she was a teenager, she
married John, and they had two children. Their children are now in teen age. John and Carla
had a divorce soon after their birth of the second child. Individual attributes are mentioned
below followed by the case study.
Family Married status Qualification Employment Health
status
Carla Mother
(54 years
old)
Single mother
(Divorcee)
Did not finish
school
A cleaner,
and a
volunteer
Unknown
John Father Single father
(divorcee)
Unknown Employed as
a casual
worker
Head injury
at work the
past,
developed
depression
Anne Daughter Pregnant and
living with
boyfriend ‘Josh’
Did not finish
high school
Unemployed Developed
gestational
diabetes
Robbie Son Unknown Completed high
school
Seeking a job Unknown
Healthcare facility among the residents require skills, resources and necessary knowledge to
acquire a healthy life. It also depends on appropriate care and services provided in a proper
way, at the precise moment to sustain healthy life of a patient. The indigenous population like
Aboriginals and Torres Strait Islanders (ATSI) are at a verge of risk because of
socioeconomic disadvantage that they experience along with the challenges of dwelling in a
remote rural location, and especially those with physical, mental or intellectual disability are
the victims of inadequate health services (Department of Health and Social Services, 2016).
65 percent of aboriginals who live under poverty, surviving in the peripheral parts of the
metropolitan cities, are the ones which are mostly affected of health inequality. As a 2017
(1) What are the characteristics of the individuals in this case study?
Carla, has been living in a mining town since her childhood. When she was a teenager, she
married John, and they had two children. Their children are now in teen age. John and Carla
had a divorce soon after their birth of the second child. Individual attributes are mentioned
below followed by the case study.
Family Married status Qualification Employment Health
status
Carla Mother
(54 years
old)
Single mother
(Divorcee)
Did not finish
school
A cleaner,
and a
volunteer
Unknown
John Father Single father
(divorcee)
Unknown Employed as
a casual
worker
Head injury
at work the
past,
developed
depression
Anne Daughter Pregnant and
living with
boyfriend ‘Josh’
Did not finish
high school
Unemployed Developed
gestational
diabetes
Robbie Son Unknown Completed high
school
Seeking a job Unknown
Healthcare facility among the residents require skills, resources and necessary knowledge to
acquire a healthy life. It also depends on appropriate care and services provided in a proper
way, at the precise moment to sustain healthy life of a patient. The indigenous population like
Aboriginals and Torres Strait Islanders (ATSI) are at a verge of risk because of
socioeconomic disadvantage that they experience along with the challenges of dwelling in a
remote rural location, and especially those with physical, mental or intellectual disability are
the victims of inadequate health services (Department of Health and Social Services, 2016).
65 percent of aboriginals who live under poverty, surviving in the peripheral parts of the
metropolitan cities, are the ones which are mostly affected of health inequality. As a 2017
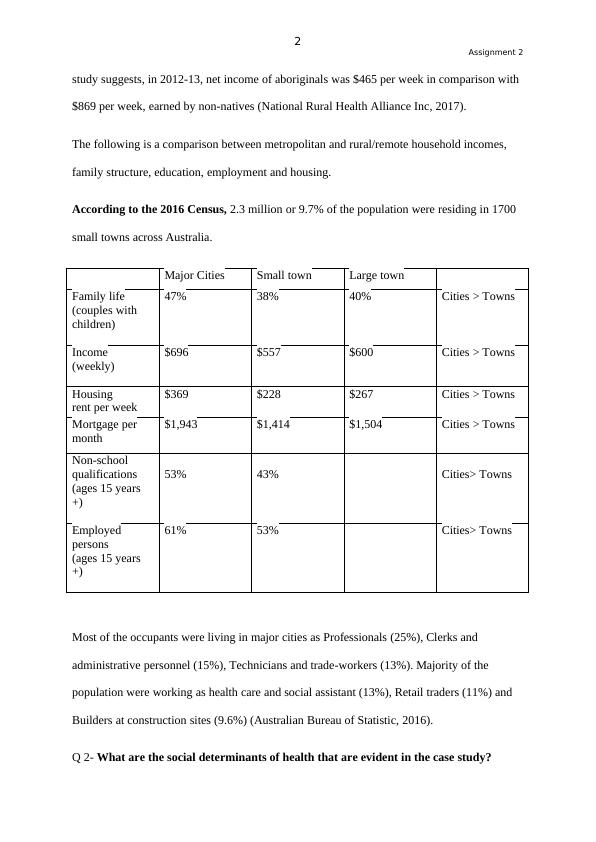
2 Assignment 2
study suggests, in 2012-13, net income of aboriginals was $465 per week in comparison with
$869 per week, earned by non-natives (National Rural Health Alliance Inc, 2017).
The following is a comparison between metropolitan and rural/remote household incomes,
family structure, education, employment and housing.
According to the 2016 Census, 2.3 million or 9.7% of the population were residing in 1700
small towns across Australia.
Major Cities Small town Large town
Family life
(couples with
children)
47% 38% 40% Cities > Towns
Income
(weekly)
$696 $557 $600 Cities > Towns
Housing
rent per week
$369 $228 $267 Cities > Towns
Mortgage per
month
$1,943 $1,414 $1,504 Cities > Towns
Non-school
qualifications
(ages 15 years
+)
53% 43% Cities> Towns
Employed
persons
(ages 15 years
+)
61% 53% Cities> Towns
Most of the occupants were living in major cities as Professionals (25%), Clerks and
administrative personnel (15%), Technicians and trade-workers (13%). Majority of the
population were working as health care and social assistant (13%), Retail traders (11%) and
Builders at construction sites (9.6%) (Australian Bureau of Statistic, 2016).
Q 2- What are the social determinants of health that are evident in the case study?
study suggests, in 2012-13, net income of aboriginals was $465 per week in comparison with
$869 per week, earned by non-natives (National Rural Health Alliance Inc, 2017).
The following is a comparison between metropolitan and rural/remote household incomes,
family structure, education, employment and housing.
According to the 2016 Census, 2.3 million or 9.7% of the population were residing in 1700
small towns across Australia.
Major Cities Small town Large town
Family life
(couples with
children)
47% 38% 40% Cities > Towns
Income
(weekly)
$696 $557 $600 Cities > Towns
Housing
rent per week
$369 $228 $267 Cities > Towns
Mortgage per
month
$1,943 $1,414 $1,504 Cities > Towns
Non-school
qualifications
(ages 15 years
+)
53% 43% Cities> Towns
Employed
persons
(ages 15 years
+)
61% 53% Cities> Towns
Most of the occupants were living in major cities as Professionals (25%), Clerks and
administrative personnel (15%), Technicians and trade-workers (13%). Majority of the
population were working as health care and social assistant (13%), Retail traders (11%) and
Builders at construction sites (9.6%) (Australian Bureau of Statistic, 2016).
Q 2- What are the social determinants of health that are evident in the case study?
3 Assignment 2
Carla is living in poverty and could not afford bus fare to commute to the city. Individuals
living in pastoral and remote areas of Australia sustain greater difficulties tackling poverty
from their gross income (25 % versus 18%) to those living in metropolitan areas, and endure
higher levels of mental and physical distress. Almost 65% of the ATSI or Aboriginal and
Torres Strait Islanders experience the direct consequence of poverty, as most of these people
live beyond city limits (National Rural Health Alliance Inc, 2017, p. 1). Women working as
miners are mostly illiterate and are unaware about their own health conditions (Sharma &
Ress, 2007).
Her ex-husband (John) did not report his head injury to his employer due to being worried
about his job. He then developed depression. Generally, lack of employment opportunities
and long term unemployment can develop clinical depression. Higher stress due to poverty
can increase multiple health risks, like deprived diet and higher smoking frequency.
Residents dwelling in remote locations of Australia are more susceptible to healthcare
inequality due to expense of medical treatment, lack of available services, costs of
transportation and accommodation, and the stigma of seeking mental health care in small
communities (Carson et al, 2016). This can delay or skip treatment resulting in poor health
outcomes (National Rural Health Alliance Inc, 2017, p. 2).
Two of her teenager children have left town for better job opportunities in the city. Young
people in socially deprived areas have fewer exposure and quality resource. As a result,
quality of living is deteriorated along with employment status, physical and mental health,
and education. In 2016, three primary reasons of utmost concern among Australian youth
were drugs (24.5%), mental health (17.6%), discrimination and equity (23.2%) applicable for
all existing socioeconomic groups. (Mission Australia, 2017).
Carla is living in poverty and could not afford bus fare to commute to the city. Individuals
living in pastoral and remote areas of Australia sustain greater difficulties tackling poverty
from their gross income (25 % versus 18%) to those living in metropolitan areas, and endure
higher levels of mental and physical distress. Almost 65% of the ATSI or Aboriginal and
Torres Strait Islanders experience the direct consequence of poverty, as most of these people
live beyond city limits (National Rural Health Alliance Inc, 2017, p. 1). Women working as
miners are mostly illiterate and are unaware about their own health conditions (Sharma &
Ress, 2007).
Her ex-husband (John) did not report his head injury to his employer due to being worried
about his job. He then developed depression. Generally, lack of employment opportunities
and long term unemployment can develop clinical depression. Higher stress due to poverty
can increase multiple health risks, like deprived diet and higher smoking frequency.
Residents dwelling in remote locations of Australia are more susceptible to healthcare
inequality due to expense of medical treatment, lack of available services, costs of
transportation and accommodation, and the stigma of seeking mental health care in small
communities (Carson et al, 2016). This can delay or skip treatment resulting in poor health
outcomes (National Rural Health Alliance Inc, 2017, p. 2).
Two of her teenager children have left town for better job opportunities in the city. Young
people in socially deprived areas have fewer exposure and quality resource. As a result,
quality of living is deteriorated along with employment status, physical and mental health,
and education. In 2016, three primary reasons of utmost concern among Australian youth
were drugs (24.5%), mental health (17.6%), discrimination and equity (23.2%) applicable for
all existing socioeconomic groups. (Mission Australia, 2017).
End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Case Study about Carla's Life a Small Coastal Town Girllg...
|5
|1686
|37
Social Determinants of Health and Role of Healthcare Professionals Case Study 2022lg...
|8
|1839
|50
Social Determinants of Health in Australialg...
|8
|1651
|209
Case Study of Carlalg...
|8
|1694
|230
socio demographic characteristics Case Study 2022lg...
|10
|2343
|20
Case Study on Social Determinants of Healthlg...
|7
|1797
|96
