Burns Management and Stroke/TIA Care
VerifiedAdded on 2021/04/17
|14
|4826
|158
AI Summary
This assignment provides a detailed examination of anesthesia management in the context of stroke and transient ischemic attack (TIA). It covers the causes of these conditions, including blood clots and emboli that interrupt blood flow to the brain. The assessment section outlines clinical presentations such as hemiplegia, dysphagia, and visual disturbances, as well as mimics like conversion disorder, seizures, and post-ictal states. Management strategies are discussed, including oxygen therapy, medications like anti-emetics and analgesia, and antiplatelet therapy with aspirin and clopidogrel. The impact of treatment options is also explored, highlighting the benefits of aspirin and clopidogrel in preventing clot formation and reducing stroke risk.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
AA 5.1 - ASSIGNMENT (Clinical Practice 2)
Common Disorders
Name:
Date:
Common Disorders
Name:
Date:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
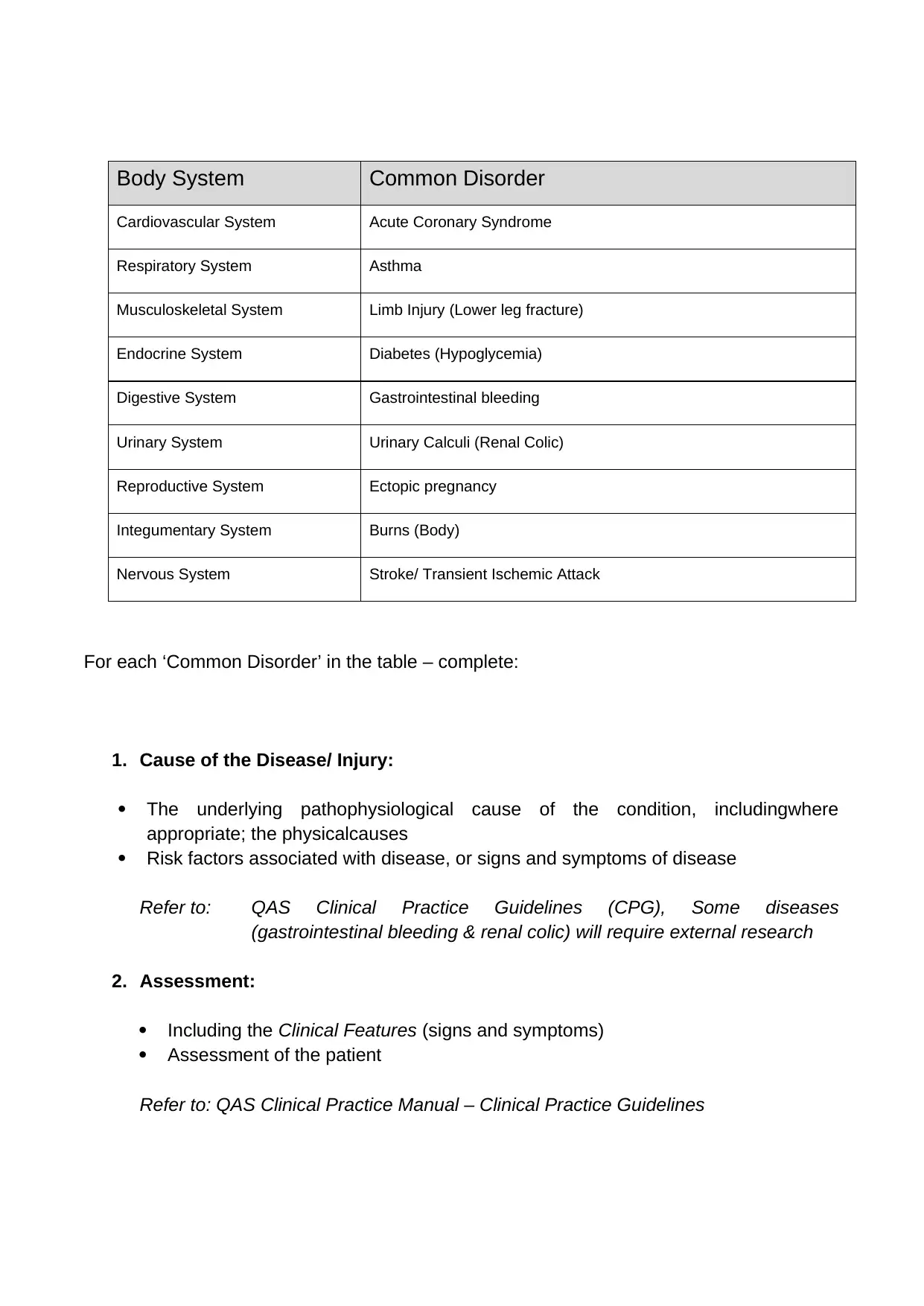
Body System Common Disorder
Cardiovascular System Acute Coronary Syndrome
Respiratory System Asthma
Musculoskeletal System Limb Injury (Lower leg fracture)
Endocrine System Diabetes (Hypoglycemia)
Digestive System Gastrointestinal bleeding
Urinary System Urinary Calculi (Renal Colic)
Reproductive System Ectopic pregnancy
Integumentary System Burns (Body)
Nervous System Stroke/ Transient Ischemic Attack
For each ‘Common Disorder’ in the table – complete:
1. Cause of the Disease/ Injury:
The underlying pathophysiological cause of the condition, includingwhere
appropriate; the physicalcauses
Risk factors associated with disease, or signs and symptoms of disease
Refer to: QAS Clinical Practice Guidelines (CPG), Some diseases
(gastrointestinal bleeding & renal colic) will require external research
2. Assessment:
Including the Clinical Features (signs and symptoms)
Assessment of the patient
Refer to: QAS Clinical Practice Manual – Clinical Practice Guidelines
Cardiovascular System Acute Coronary Syndrome
Respiratory System Asthma
Musculoskeletal System Limb Injury (Lower leg fracture)
Endocrine System Diabetes (Hypoglycemia)
Digestive System Gastrointestinal bleeding
Urinary System Urinary Calculi (Renal Colic)
Reproductive System Ectopic pregnancy
Integumentary System Burns (Body)
Nervous System Stroke/ Transient Ischemic Attack
For each ‘Common Disorder’ in the table – complete:
1. Cause of the Disease/ Injury:
The underlying pathophysiological cause of the condition, includingwhere
appropriate; the physicalcauses
Risk factors associated with disease, or signs and symptoms of disease
Refer to: QAS Clinical Practice Guidelines (CPG), Some diseases
(gastrointestinal bleeding & renal colic) will require external research
2. Assessment:
Including the Clinical Features (signs and symptoms)
Assessment of the patient
Refer to: QAS Clinical Practice Manual – Clinical Practice Guidelines
3. Management:
The treatment plan, including procedures (skills) and pharmacology (drugs) for
your scope as an Advanced Care Paramedic
Indicate ‘cautions’ and ‘contraindications’ for drugs being used
Identify possible requirements for assistance from higher levels of care
(Critical Care Paramedics)
Refer to: QAS Clinical Scope of Practice
QAS Clinical Practice Manual – Clinical Practice Guidelines
QAS Clinical Practice Manual – Drug Therapy Protocols
4. Impact of Management:
What are the short term, and/or long term impacts the management and
treatment for this patient may have on the patient for both the procedures and
pharmacology that may be provided at your level? (eg Adverse effects and
their causes)
Refer to: QAS Clinical Practice Manual – Drug Therapy Protocols
Additional information:
When locating signs and symptoms – refer toQAS Clinical Practice Guidelines to
assist
For ‘Risks Factors’ associated with disease – refer to QAS Clinical Practice
Guidelines
When searching QAS Clinical Practice Guidelines – not all diseases have specific
treatment guidelines. Where there is no specific guideline, refer to the region, or
signs and symptoms related to the compliant. An example would be ‘Acute
Appendicitis’ – there is no specific pre-hospital treatment for this disease, however it
does fall into the category of an ‘Abdominal Emergency’, same as ‘Acute Bowel
Obstruction’ and many more.
When completing the section on ‘Management’ useQAS Clinical Practice Guidelines
to assist.
For ‘Pharmacology – cautions and contraindications – refer to QAS Drug Therapy
Protocols.
The treatment plan, including procedures (skills) and pharmacology (drugs) for
your scope as an Advanced Care Paramedic
Indicate ‘cautions’ and ‘contraindications’ for drugs being used
Identify possible requirements for assistance from higher levels of care
(Critical Care Paramedics)
Refer to: QAS Clinical Scope of Practice
QAS Clinical Practice Manual – Clinical Practice Guidelines
QAS Clinical Practice Manual – Drug Therapy Protocols
4. Impact of Management:
What are the short term, and/or long term impacts the management and
treatment for this patient may have on the patient for both the procedures and
pharmacology that may be provided at your level? (eg Adverse effects and
their causes)
Refer to: QAS Clinical Practice Manual – Drug Therapy Protocols
Additional information:
When locating signs and symptoms – refer toQAS Clinical Practice Guidelines to
assist
For ‘Risks Factors’ associated with disease – refer to QAS Clinical Practice
Guidelines
When searching QAS Clinical Practice Guidelines – not all diseases have specific
treatment guidelines. Where there is no specific guideline, refer to the region, or
signs and symptoms related to the compliant. An example would be ‘Acute
Appendicitis’ – there is no specific pre-hospital treatment for this disease, however it
does fall into the category of an ‘Abdominal Emergency’, same as ‘Acute Bowel
Obstruction’ and many more.
When completing the section on ‘Management’ useQAS Clinical Practice Guidelines
to assist.
For ‘Pharmacology – cautions and contraindications – refer to QAS Drug Therapy
Protocols.
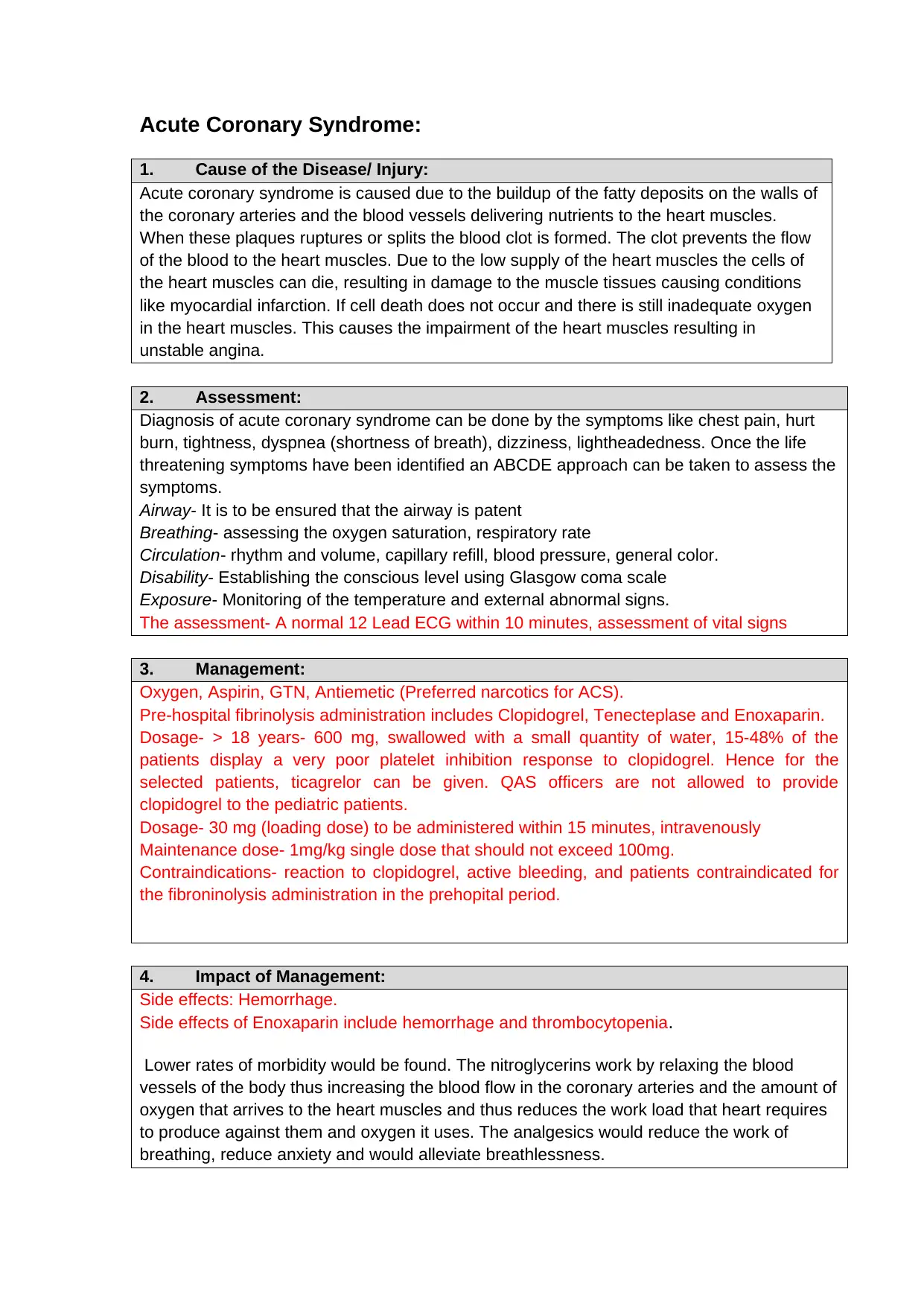
Acute Coronary Syndrome:
1. Cause of the Disease/ Injury:
Acute coronary syndrome is caused due to the buildup of the fatty deposits on the walls of
the coronary arteries and the blood vessels delivering nutrients to the heart muscles.
When these plaques ruptures or splits the blood clot is formed. The clot prevents the flow
of the blood to the heart muscles. Due to the low supply of the heart muscles the cells of
the heart muscles can die, resulting in damage to the muscle tissues causing conditions
like myocardial infarction. If cell death does not occur and there is still inadequate oxygen
in the heart muscles. This causes the impairment of the heart muscles resulting in
unstable angina.
2. Assessment:
Diagnosis of acute coronary syndrome can be done by the symptoms like chest pain, hurt
burn, tightness, dyspnea (shortness of breath), dizziness, lightheadedness. Once the life
threatening symptoms have been identified an ABCDE approach can be taken to assess the
symptoms.
Airway- It is to be ensured that the airway is patent
Breathing- assessing the oxygen saturation, respiratory rate
Circulation- rhythm and volume, capillary refill, blood pressure, general color.
Disability- Establishing the conscious level using Glasgow coma scale
Exposure- Monitoring of the temperature and external abnormal signs.
The assessment- A normal 12 Lead ECG within 10 minutes, assessment of vital signs
3. Management:
Oxygen, Aspirin, GTN, Antiemetic (Preferred narcotics for ACS).
Pre-hospital fibrinolysis administration includes Clopidogrel, Tenecteplase and Enoxaparin.
Dosage- > 18 years- 600 mg, swallowed with a small quantity of water, 15-48% of the
patients display a very poor platelet inhibition response to clopidogrel. Hence for the
selected patients, ticagrelor can be given. QAS officers are not allowed to provide
clopidogrel to the pediatric patients.
Dosage- 30 mg (loading dose) to be administered within 15 minutes, intravenously
Maintenance dose- 1mg/kg single dose that should not exceed 100mg.
Contraindications- reaction to clopidogrel, active bleeding, and patients contraindicated for
the fibroninolysis administration in the prehopital period.
4. Impact of Management:
Side effects: Hemorrhage.
Side effects of Enoxaparin include hemorrhage and thrombocytopenia.
Lower rates of morbidity would be found. The nitroglycerins work by relaxing the blood
vessels of the body thus increasing the blood flow in the coronary arteries and the amount of
oxygen that arrives to the heart muscles and thus reduces the work load that heart requires
to produce against them and oxygen it uses. The analgesics would reduce the work of
breathing, reduce anxiety and would alleviate breathlessness.
1. Cause of the Disease/ Injury:
Acute coronary syndrome is caused due to the buildup of the fatty deposits on the walls of
the coronary arteries and the blood vessels delivering nutrients to the heart muscles.
When these plaques ruptures or splits the blood clot is formed. The clot prevents the flow
of the blood to the heart muscles. Due to the low supply of the heart muscles the cells of
the heart muscles can die, resulting in damage to the muscle tissues causing conditions
like myocardial infarction. If cell death does not occur and there is still inadequate oxygen
in the heart muscles. This causes the impairment of the heart muscles resulting in
unstable angina.
2. Assessment:
Diagnosis of acute coronary syndrome can be done by the symptoms like chest pain, hurt
burn, tightness, dyspnea (shortness of breath), dizziness, lightheadedness. Once the life
threatening symptoms have been identified an ABCDE approach can be taken to assess the
symptoms.
Airway- It is to be ensured that the airway is patent
Breathing- assessing the oxygen saturation, respiratory rate
Circulation- rhythm and volume, capillary refill, blood pressure, general color.
Disability- Establishing the conscious level using Glasgow coma scale
Exposure- Monitoring of the temperature and external abnormal signs.
The assessment- A normal 12 Lead ECG within 10 minutes, assessment of vital signs
3. Management:
Oxygen, Aspirin, GTN, Antiemetic (Preferred narcotics for ACS).
Pre-hospital fibrinolysis administration includes Clopidogrel, Tenecteplase and Enoxaparin.
Dosage- > 18 years- 600 mg, swallowed with a small quantity of water, 15-48% of the
patients display a very poor platelet inhibition response to clopidogrel. Hence for the
selected patients, ticagrelor can be given. QAS officers are not allowed to provide
clopidogrel to the pediatric patients.
Dosage- 30 mg (loading dose) to be administered within 15 minutes, intravenously
Maintenance dose- 1mg/kg single dose that should not exceed 100mg.
Contraindications- reaction to clopidogrel, active bleeding, and patients contraindicated for
the fibroninolysis administration in the prehopital period.
4. Impact of Management:
Side effects: Hemorrhage.
Side effects of Enoxaparin include hemorrhage and thrombocytopenia.
Lower rates of morbidity would be found. The nitroglycerins work by relaxing the blood
vessels of the body thus increasing the blood flow in the coronary arteries and the amount of
oxygen that arrives to the heart muscles and thus reduces the work load that heart requires
to produce against them and oxygen it uses. The analgesics would reduce the work of
breathing, reduce anxiety and would alleviate breathlessness.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Asthma:
1. Cause of the Disease/ Injury:
Asthma is a condition that is characterized by the narrowing of the airways, swelling and the
production of extra mucus. The obstruction of the lower airways is caused due to
bronchospasm, inflammation and the edema of the airways, plugging of the mucus and
hyperplasia and hypertrophy of the airway smooth muscles. The risk factors that can
increase the chance of developing asthma are exposure to second hand smoke, obesity and
occupational triggers like factory fumes, constructional debris.
2. Assessment:
Monitoring of the breathing pattern. Asthma can be measured by spirometry. In order to rule
out the chance of respiratory infections or COPD, physical examination has to be done.
Peak flow meter can be used to measure the lung function, which is a simple device for
measuring how hard one can breathe out. Lower than the usual peak flow readings indicate
that the lungs might not be working well. Other tests involve nitric oxide test, allergic testing,
chest x-ray or high resolution computerized tomography.
Assessment includes identification of wheezing. Other risk assessments include prior ICU
admissions, current medications. Respiratory status assessment can be done which
includes conscious state, speech, ventilatory rate, ventilatory rhythm, pulse rate and
breathing sounds.
3. Management:
To assess the severity of the Asthma. In case of severe Asthma, Adrenaline (IV/IM) ,
oxygen, IPPV (adult:
4–6 b/m
large child:
8–10 b/m
small child:
10–15 b/m) can be given. Salbutamol, Magnesium Sulphate, Ipratropium bromide neb,
CPAP, hydrocortisone can be given. Intubation can be given.
Face masks can be used while working in the construction sites or factories.
Vaccination for influenza and pneumonia can be taken to avoid the chance of asthma flare-
ups.
Contraindications: no contraindications for Adrenaline.
Contraindications related to Salbutamol- Adverse drug reaction.
4. Impact of Management:
Effects of adrenaline- Adrenaline or the epinephrine is a naturally occurring catecholamine
that causes bronchodilation.
Side effects of adrenaline- anxiety, pupil dilation, tremor, hypertension.
Side effects of Salbutamol are tremors, tachrhythmias and metabolic acidosis.
1. Cause of the Disease/ Injury:
Asthma is a condition that is characterized by the narrowing of the airways, swelling and the
production of extra mucus. The obstruction of the lower airways is caused due to
bronchospasm, inflammation and the edema of the airways, plugging of the mucus and
hyperplasia and hypertrophy of the airway smooth muscles. The risk factors that can
increase the chance of developing asthma are exposure to second hand smoke, obesity and
occupational triggers like factory fumes, constructional debris.
2. Assessment:
Monitoring of the breathing pattern. Asthma can be measured by spirometry. In order to rule
out the chance of respiratory infections or COPD, physical examination has to be done.
Peak flow meter can be used to measure the lung function, which is a simple device for
measuring how hard one can breathe out. Lower than the usual peak flow readings indicate
that the lungs might not be working well. Other tests involve nitric oxide test, allergic testing,
chest x-ray or high resolution computerized tomography.
Assessment includes identification of wheezing. Other risk assessments include prior ICU
admissions, current medications. Respiratory status assessment can be done which
includes conscious state, speech, ventilatory rate, ventilatory rhythm, pulse rate and
breathing sounds.
3. Management:
To assess the severity of the Asthma. In case of severe Asthma, Adrenaline (IV/IM) ,
oxygen, IPPV (adult:
4–6 b/m
large child:
8–10 b/m
small child:
10–15 b/m) can be given. Salbutamol, Magnesium Sulphate, Ipratropium bromide neb,
CPAP, hydrocortisone can be given. Intubation can be given.
Face masks can be used while working in the construction sites or factories.
Vaccination for influenza and pneumonia can be taken to avoid the chance of asthma flare-
ups.
Contraindications: no contraindications for Adrenaline.
Contraindications related to Salbutamol- Adverse drug reaction.
4. Impact of Management:
Effects of adrenaline- Adrenaline or the epinephrine is a naturally occurring catecholamine
that causes bronchodilation.
Side effects of adrenaline- anxiety, pupil dilation, tremor, hypertension.
Side effects of Salbutamol are tremors, tachrhythmias and metabolic acidosis.
Limb Injury (lower leg fracture):
1. Cause of the Disease/ Injury:
A lower leg fracture occurs when one or both the bones of the lower leg, the tibia and the
fibula break.
Trauma or the unnatural rotation of the tibia and fibula can give rise to a broken leg.
Lower leg fracture can be caused due to a number of reasons such as falls, motor vehicle
accidents. Fractures can occur if the knees become jammed against the dashboard during a
collision. Hyperextension of the legs during contract sport can break a leg. Repetitive force
or overuse can pressurize the stress fractures. Leg fracture may also be caused due to
osteoporosis. Some of the clinical features include pain, swelling, loss of function, bruising,
bony crepitus and deformities
2. Assessment:
Some of the clinical features include pain, swelling, loss of function, bruising, bony crepitus
and deformities.
To assess whether the patient is shocked or the limb is poorly perfused. Assessment of the
lower leg fractures can be done by physical examination such as examining the affected
area for any tenderness, deformity or swelling or wound. X-ray is usually used for detecting
the exact location of the fracture and the extent of the injury. For more detailed imaging
computerized tomography (CT) or magnetic resonance imaging can be used.
3. Management:
The management or the treatment of the broken lower leg depends upon the severity of the
injury. Sometimes the bones that have been displaced can be reorganized or realigned for
before the immobilization. Open wounds or fractures should be washed with 1-2 liters of
saline solutions following analgesia. Muscle relaxants and painkillers such as Ibuprofen can
be given before the procedure. For reducing the pain and the inflammation pain killers such
as acetaminophen or ibuprofen or a combination of two can be used. After the removal of
the cast and the splint physical therapy can be taken up for reducing the stiffness and
restoration of the movement of the injured leg.
Contraindications- Renal impairment, hypovalemia, risk in pregnancy, peptic ulcer and GI
tract bleeding.
4. Impact of Management:
1. Cause of the Disease/ Injury:
A lower leg fracture occurs when one or both the bones of the lower leg, the tibia and the
fibula break.
Trauma or the unnatural rotation of the tibia and fibula can give rise to a broken leg.
Lower leg fracture can be caused due to a number of reasons such as falls, motor vehicle
accidents. Fractures can occur if the knees become jammed against the dashboard during a
collision. Hyperextension of the legs during contract sport can break a leg. Repetitive force
or overuse can pressurize the stress fractures. Leg fracture may also be caused due to
osteoporosis. Some of the clinical features include pain, swelling, loss of function, bruising,
bony crepitus and deformities
2. Assessment:
Some of the clinical features include pain, swelling, loss of function, bruising, bony crepitus
and deformities.
To assess whether the patient is shocked or the limb is poorly perfused. Assessment of the
lower leg fractures can be done by physical examination such as examining the affected
area for any tenderness, deformity or swelling or wound. X-ray is usually used for detecting
the exact location of the fracture and the extent of the injury. For more detailed imaging
computerized tomography (CT) or magnetic resonance imaging can be used.
3. Management:
The management or the treatment of the broken lower leg depends upon the severity of the
injury. Sometimes the bones that have been displaced can be reorganized or realigned for
before the immobilization. Open wounds or fractures should be washed with 1-2 liters of
saline solutions following analgesia. Muscle relaxants and painkillers such as Ibuprofen can
be given before the procedure. For reducing the pain and the inflammation pain killers such
as acetaminophen or ibuprofen or a combination of two can be used. After the removal of
the cast and the splint physical therapy can be taken up for reducing the stiffness and
restoration of the movement of the injured leg.
Contraindications- Renal impairment, hypovalemia, risk in pregnancy, peptic ulcer and GI
tract bleeding.
4. Impact of Management:
Effects: - Analgesics and NSAIDs inhibit the synthesis of prostaglandins resulting in anti-
pyretic, analgesic and inflammatory actions.
Adverse effects- Analgesics may cause side effects such as Nausea, Dizziness, GI tract
bleeding.
Precautions have to be taken in case of asthma, GI bleeding and Hepatic dysfunction.
Diabetes (Hypoglycaemia):
1. Cause of the Disease/ Injury:
Diabetes is a metabolic disorder in which a person has high glucose level either because the
insulin production is inadequate or the body cells do not respond to insulin. Type 1 diabetes
is caused when the immune system attacks and destroys the beta cells of the pancreas that
produces insulin. Type 2 diabetes is caused when the body becomes resistant to insulin or
when pancreas stops producing insulin. The inability of the cell to use the insulin properly
affects the cells of the fat tissues of the muscle and forms insulin resistance. The symptoms
of diabetes occur because the glucose stays in the blood and is not being used for the
production of energy. The body often tries to lessen the blood glucose level the removing the
excess glucose out of the body as urine.
2. Assessment:
Clinical manifestations involve diaphoresis, tingling effect around the mouth, pallor,
palpitation and anxiety, tachcardia. These clinical signs may disappear with prolonged
hypoglycemia.
Assessment of diabetes can be done by Glycated haemoglobin (A1C) test. This blood test
helps to indicate the average blood sugar level for the past two to three months. It measure
the percentage of blood sugar attached to haemoglobin. The higher is the level of the blood
sugar level more is the haemoglobin will have the sugar attached. Other tests include
random blood sugar test, where the blood will be collected at a random time. The blood
glucose level should be 4.0-8 mmol/L
3. Management:
pyretic, analgesic and inflammatory actions.
Adverse effects- Analgesics may cause side effects such as Nausea, Dizziness, GI tract
bleeding.
Precautions have to be taken in case of asthma, GI bleeding and Hepatic dysfunction.
Diabetes (Hypoglycaemia):
1. Cause of the Disease/ Injury:
Diabetes is a metabolic disorder in which a person has high glucose level either because the
insulin production is inadequate or the body cells do not respond to insulin. Type 1 diabetes
is caused when the immune system attacks and destroys the beta cells of the pancreas that
produces insulin. Type 2 diabetes is caused when the body becomes resistant to insulin or
when pancreas stops producing insulin. The inability of the cell to use the insulin properly
affects the cells of the fat tissues of the muscle and forms insulin resistance. The symptoms
of diabetes occur because the glucose stays in the blood and is not being used for the
production of energy. The body often tries to lessen the blood glucose level the removing the
excess glucose out of the body as urine.
2. Assessment:
Clinical manifestations involve diaphoresis, tingling effect around the mouth, pallor,
palpitation and anxiety, tachcardia. These clinical signs may disappear with prolonged
hypoglycemia.
Assessment of diabetes can be done by Glycated haemoglobin (A1C) test. This blood test
helps to indicate the average blood sugar level for the past two to three months. It measure
the percentage of blood sugar attached to haemoglobin. The higher is the level of the blood
sugar level more is the haemoglobin will have the sugar attached. Other tests include
random blood sugar test, where the blood will be collected at a random time. The blood
glucose level should be 4.0-8 mmol/L
3. Management:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Intravenous glucose is the first line of management strategy that is unable to swallow oral
glucose. While attending the patient with hypoglyceamia it is necessary to check whether the
insulin delivering pump can be administered, whether the patient can orally take glucose,
then oral glucose can be administered and diabetic services can be referred.
Dosage- 250 ml of 10% glucose (25 gm). Intravenously 150 ml boluses are repeated after
every 5 minutes. In case of the incapability of the patient to take oral glucose, IV access
should be checked; if IV access is not achieved then glucagon can be considered.
The patient can be advised to take complex carbohydrates.
Contraindications-Nil
4. Impact of Management:
Caution should be made in case the patient is agitated or violent. Care should be taken
regarding the overdose of the medications.
Side effects- no side effects.
Gastrointestinal bleeding:
1. Cause of the Disease/ Injury:
Gastrointestinal bleeding can be caused by Angiodysplasia, benign tumours or cancer,
colitis, colon polyps, Diverticular disease, esphageal disease, gastritis, esophagitis. In
angiodysplasia the enlarged blood vessel in the GI tract can cause gastrointestinal bleeding.
Benign tumors or cancer weakens the lining of the GI tract and may cause bleeding.
Presence of more than one colon polyp may cause CI bleeding. Diverticular disease can be
formed when rashes or small pouches push outward through the weak spots in the colon
wall. In gastritis the stomach lining may worn away and cause intestinal bleeding.
2. Assessment:
The clinical symptoms include vomiting of blood, bloody stools, stomach pain, fatigue and
pale in appearance.
The underlying source of the bleeding should be identified. For acute GI bleeding the risk
scores such as Rockall score and Glasgow Blatchford score (GBS) has been validated and
developed. Investigations for acute GI bleeding can be done by upper endoscopy or
colonoscopy, CT angiogram, scintigraphy, catheter angiography (to be done in hospital after
the referrals by the paramedic). The options for the investigation are guided by the clinical
presentation. Upper endoscopy is considered as the best option for acute upper intestinal
bleeding. In case of lower GI bleeding colonoscopy can be done. It is utilized as the initial
modality in the patients which are hemodynamically stable. Radionuclide imaging helps in
detecting the slowest bleeding rates.
3. Management:
glucose. While attending the patient with hypoglyceamia it is necessary to check whether the
insulin delivering pump can be administered, whether the patient can orally take glucose,
then oral glucose can be administered and diabetic services can be referred.
Dosage- 250 ml of 10% glucose (25 gm). Intravenously 150 ml boluses are repeated after
every 5 minutes. In case of the incapability of the patient to take oral glucose, IV access
should be checked; if IV access is not achieved then glucagon can be considered.
The patient can be advised to take complex carbohydrates.
Contraindications-Nil
4. Impact of Management:
Caution should be made in case the patient is agitated or violent. Care should be taken
regarding the overdose of the medications.
Side effects- no side effects.
Gastrointestinal bleeding:
1. Cause of the Disease/ Injury:
Gastrointestinal bleeding can be caused by Angiodysplasia, benign tumours or cancer,
colitis, colon polyps, Diverticular disease, esphageal disease, gastritis, esophagitis. In
angiodysplasia the enlarged blood vessel in the GI tract can cause gastrointestinal bleeding.
Benign tumors or cancer weakens the lining of the GI tract and may cause bleeding.
Presence of more than one colon polyp may cause CI bleeding. Diverticular disease can be
formed when rashes or small pouches push outward through the weak spots in the colon
wall. In gastritis the stomach lining may worn away and cause intestinal bleeding.
2. Assessment:
The clinical symptoms include vomiting of blood, bloody stools, stomach pain, fatigue and
pale in appearance.
The underlying source of the bleeding should be identified. For acute GI bleeding the risk
scores such as Rockall score and Glasgow Blatchford score (GBS) has been validated and
developed. Investigations for acute GI bleeding can be done by upper endoscopy or
colonoscopy, CT angiogram, scintigraphy, catheter angiography (to be done in hospital after
the referrals by the paramedic). The options for the investigation are guided by the clinical
presentation. Upper endoscopy is considered as the best option for acute upper intestinal
bleeding. In case of lower GI bleeding colonoscopy can be done. It is utilized as the initial
modality in the patients which are hemodynamically stable. Radionuclide imaging helps in
detecting the slowest bleeding rates.
3. Management:
Medications like Omeprazole and Lansoprazolel can be given. It decreases the amount of
acid made by the stomach. Omeprazole can be given 40 mg orally in a day.
Treatment of gastrointestinal bleeding can be done by endoscopic thermal probe that is
done by burning the abnormal tissues or the blood vessels. Endoscopic injection can be
given such as diluted epinephrine at the bleeding site. Argon and plasma coagulation are
being used. Radiofrequency ablation can be used for treating the abnormal blood vessels in
the stomach. Endoscopic clips can be used for closing the bleeding. Endoscopic band
ligation can be used for treating the hemorrhoids and the varices in the esophagus.
Angiographic embolisation injects particles into the blood vessels for stopping the bleeding.
In rare cases a patient might require a surgery.
4. Impact of Management:
Side effects include lightheadedness, dizziness, tiredness, nausea and vomiting. On suitable
management the patient will no longer display bleeding from the GI tract. The patient will not
display bloody stool or bloody urine signifying no bleeding. The portal venous pressure will
be less. Beta blockers and the nitrates would stop bleeding.
Urinary Calculi (Renal Colic):
1. Cause of the Disease/ Injury:
Renal Calculi are hard deposits of salts and minerals form the body.
A renal calculus does not have any definite cause. Kidney stones are formed when the urine
contains crystal forming compounds such as crystals of calcium, uric acid and oxalate. The
urine may also lack the substances that helps in preventing the crystals form sticking
together. Most of the kidney stones are calcium stones that are found in the form of calcium
stones. Medical conditions like urinary tract infections, crohn's diseases, urinary tract
infection and renal tubular acidosis, medullary sponge kidney, hyperparathyroidism and
Dent's diseases can increase the risk of the kidney stones.
2. Assessment:
There are several tests for detecting the kidney stones. A clicky pain in the groin and the
lower end near the kidneys can be assessed by a physical examination by the physician. As
the stone moves down the ureter, the pain migrates caudally and medially.
A Urinalysis can be done in order to detect the presence of blood or infection in the urine. A
CT scan of the abdomen can help to detect the exact size of the kidney stone, its location
and the status of the organs like aorta, appendix and pancreas. Pregnant women can
receive an ultrasound instead of CT scan for preventing unnecessary radiation. Simple X-
ray can be used to track the progress of the stone through the excretory system.
3. Management:
. In a clinical setting the patient might be rehydrated with an intravenous tube along with the
application of the anti-inflammatory medications. Narcotics can be used to treat the pain and
the anti-emetics are generally used for preventing the symptoms of nausea and vomiting.
acid made by the stomach. Omeprazole can be given 40 mg orally in a day.
Treatment of gastrointestinal bleeding can be done by endoscopic thermal probe that is
done by burning the abnormal tissues or the blood vessels. Endoscopic injection can be
given such as diluted epinephrine at the bleeding site. Argon and plasma coagulation are
being used. Radiofrequency ablation can be used for treating the abnormal blood vessels in
the stomach. Endoscopic clips can be used for closing the bleeding. Endoscopic band
ligation can be used for treating the hemorrhoids and the varices in the esophagus.
Angiographic embolisation injects particles into the blood vessels for stopping the bleeding.
In rare cases a patient might require a surgery.
4. Impact of Management:
Side effects include lightheadedness, dizziness, tiredness, nausea and vomiting. On suitable
management the patient will no longer display bleeding from the GI tract. The patient will not
display bloody stool or bloody urine signifying no bleeding. The portal venous pressure will
be less. Beta blockers and the nitrates would stop bleeding.
Urinary Calculi (Renal Colic):
1. Cause of the Disease/ Injury:
Renal Calculi are hard deposits of salts and minerals form the body.
A renal calculus does not have any definite cause. Kidney stones are formed when the urine
contains crystal forming compounds such as crystals of calcium, uric acid and oxalate. The
urine may also lack the substances that helps in preventing the crystals form sticking
together. Most of the kidney stones are calcium stones that are found in the form of calcium
stones. Medical conditions like urinary tract infections, crohn's diseases, urinary tract
infection and renal tubular acidosis, medullary sponge kidney, hyperparathyroidism and
Dent's diseases can increase the risk of the kidney stones.
2. Assessment:
There are several tests for detecting the kidney stones. A clicky pain in the groin and the
lower end near the kidneys can be assessed by a physical examination by the physician. As
the stone moves down the ureter, the pain migrates caudally and medially.
A Urinalysis can be done in order to detect the presence of blood or infection in the urine. A
CT scan of the abdomen can help to detect the exact size of the kidney stone, its location
and the status of the organs like aorta, appendix and pancreas. Pregnant women can
receive an ultrasound instead of CT scan for preventing unnecessary radiation. Simple X-
ray can be used to track the progress of the stone through the excretory system.
3. Management:
. In a clinical setting the patient might be rehydrated with an intravenous tube along with the
application of the anti-inflammatory medications. Narcotics can be used to treat the pain and
the anti-emetics are generally used for preventing the symptoms of nausea and vomiting.
Shock wave therapy can be given to break the stones into small pieces such that it is easier
to pass through the urine (After being admitted to the hospital). Patients with large stones in
regions where lithotripsy cannot be performed may require a surgical procedure. Proper
fluids will keep the patient hydrated.
Contraindication: Some of the contraindications of anti-emetic are that it can cause
congenital long QT syndrome, intestinal obstruction, and hepatic impairment.
4. Impact of Management:
Effects. Anti-emetic is a serotonin that reduces the activity of the vagus nerve that activates
the vomiting centre of the vagus nerve.
Adverse effects: Adverse effects includes nausea, vomiting, diarrhea
Ectopic pregnancy:
1. Cause of the Disease/ Injury:
Ectopic pregnancy is caused when the fertilized egg implants itself to a place other than the
uterus. Most of the ectopic pregnancy occurs in the fallopian tube. The fallopian tubes are
not responsible for holding the embryo but are responsible for the passage of the egg and
the process of fertilization. The implantation of the zygote takes place exclusively in the
uterus. Ectopic pregnancies can be caused because of the presence of blockage in the
fallopian tube due to inflammation. Any previous surgery in the pelvic region in the tubes can
result in adhesions. Scar tissue due to any previous infection can impede the movement of
the egg. The fallopian tube can be abnormally shaped due to birth defects.
Clinical features- History of amenorrhea, abnormal vaginal bleeding, pelvic and abdominal
pain, nausea and the presyncopal symptoms.
Risk factors- It can lead to hemorrhagic shock.
2. Assessment:
Ectopic pregnancy can be assessed by performing a performing a pelvic exam for locating
the pain, mass or tenderness in the abdomen. An ultrasound can be done for detecting any
developing fetus in the uterus (after taking the patient to the hospital). The patient may
exhibit hypovolemic shock. The patient may show tachycardia, syncope and may have pale
or cool skin, in case of a ruptured pregnancy. hCG levels should also be measured as lower
levels of hCG levels can be used to detect e may detect ectopic pregnancy. Progesterone
level can also be measured as low levels of progesterone may indicate towards ectopic
to pass through the urine (After being admitted to the hospital). Patients with large stones in
regions where lithotripsy cannot be performed may require a surgical procedure. Proper
fluids will keep the patient hydrated.
Contraindication: Some of the contraindications of anti-emetic are that it can cause
congenital long QT syndrome, intestinal obstruction, and hepatic impairment.
4. Impact of Management:
Effects. Anti-emetic is a serotonin that reduces the activity of the vagus nerve that activates
the vomiting centre of the vagus nerve.
Adverse effects: Adverse effects includes nausea, vomiting, diarrhea
Ectopic pregnancy:
1. Cause of the Disease/ Injury:
Ectopic pregnancy is caused when the fertilized egg implants itself to a place other than the
uterus. Most of the ectopic pregnancy occurs in the fallopian tube. The fallopian tubes are
not responsible for holding the embryo but are responsible for the passage of the egg and
the process of fertilization. The implantation of the zygote takes place exclusively in the
uterus. Ectopic pregnancies can be caused because of the presence of blockage in the
fallopian tube due to inflammation. Any previous surgery in the pelvic region in the tubes can
result in adhesions. Scar tissue due to any previous infection can impede the movement of
the egg. The fallopian tube can be abnormally shaped due to birth defects.
Clinical features- History of amenorrhea, abnormal vaginal bleeding, pelvic and abdominal
pain, nausea and the presyncopal symptoms.
Risk factors- It can lead to hemorrhagic shock.
2. Assessment:
Ectopic pregnancy can be assessed by performing a performing a pelvic exam for locating
the pain, mass or tenderness in the abdomen. An ultrasound can be done for detecting any
developing fetus in the uterus (after taking the patient to the hospital). The patient may
exhibit hypovolemic shock. The patient may show tachycardia, syncope and may have pale
or cool skin, in case of a ruptured pregnancy. hCG levels should also be measured as lower
levels of hCG levels can be used to detect e may detect ectopic pregnancy. Progesterone
level can also be measured as low levels of progesterone may indicate towards ectopic
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
pregnancy. Risk assessment- A high index of suspicion has to be maintained for ectopic
pregnancy, in any female patient having the clinical features.
3. Management:
Analgesia, Antimetic (Ondansetron)and IV fluids can be given.
An ectopic pregnancy can be treated pharmacologically by the application of Methotrexate,
which would allow the body to absorb the pregnancy tissue and save the oviduct, depending
upon the extent of the pregnancy. 4-8 mg of Ondansetron can be administered in adults.
Some of the contraindications of anti-emetic are that it can cause congenital long QT
syndrome, intestinal obstruction, and hepatic impairment.
It has to be remembered that all the IV lines and cannulae should be thoroughly flushed with
0.95 of sodium chloride after the administration of each medication. If the oviduct has
already started bleeding then emergency surgery is required. The hCG levels have to be
monitored daily until it reaches zero if one has not her entire fallopian tube removed (to be
done after transporting the patient to the hospital).
4. Impact of Management:
Adverse effects- Some of the contraindications of anti-emetic are that it can cause
congenital long QT syndrome, intestinal obstruction, and hepatic impairment. Anti-emetic is
a serotonin that reduces the activity of the vagus nerve that activates the vomiting centre of
the vagus nerve.
Analgesics may cause nausea, diarrhea, vomiting, hair loss and skin rashes. It can also
affect the lever. Long term side effects include lung infections, ulcerative stomatitis.
Burns (body):
1. Cause of the Disease/ Injury:
Wounds caused due to burns are due to the injury caused in the cutanous level and the
subsequent destruction of the underlying tissue. Burns can be caused due to flames, scalds,
exposure to natural gases, alcohols or combustible liquids, contact with hot metal or liquids,
electrical burns, chemical burn, cold injury or the frost bites, ionization and sun burns.
Severe damage to the epidermal or the dermal layer of the skin may be caused by electrical
or chemical burns such as acids and alkalis.
2. Assessment:
Clinical features- Superficial burns- erythyma and brisk cap refill. burn is painful
Superficial dermal burns-Reddened wound with blisters and brisk cap refill. Painful burn
Deep dermal- Reddened and mottled white slough, cap refill is absent. Excessive pain.
full thickness- Cap refill is absent, wound is dry and charred, less pain. The surface area
pregnancy, in any female patient having the clinical features.
3. Management:
Analgesia, Antimetic (Ondansetron)and IV fluids can be given.
An ectopic pregnancy can be treated pharmacologically by the application of Methotrexate,
which would allow the body to absorb the pregnancy tissue and save the oviduct, depending
upon the extent of the pregnancy. 4-8 mg of Ondansetron can be administered in adults.
Some of the contraindications of anti-emetic are that it can cause congenital long QT
syndrome, intestinal obstruction, and hepatic impairment.
It has to be remembered that all the IV lines and cannulae should be thoroughly flushed with
0.95 of sodium chloride after the administration of each medication. If the oviduct has
already started bleeding then emergency surgery is required. The hCG levels have to be
monitored daily until it reaches zero if one has not her entire fallopian tube removed (to be
done after transporting the patient to the hospital).
4. Impact of Management:
Adverse effects- Some of the contraindications of anti-emetic are that it can cause
congenital long QT syndrome, intestinal obstruction, and hepatic impairment. Anti-emetic is
a serotonin that reduces the activity of the vagus nerve that activates the vomiting centre of
the vagus nerve.
Analgesics may cause nausea, diarrhea, vomiting, hair loss and skin rashes. It can also
affect the lever. Long term side effects include lung infections, ulcerative stomatitis.
Burns (body):
1. Cause of the Disease/ Injury:
Wounds caused due to burns are due to the injury caused in the cutanous level and the
subsequent destruction of the underlying tissue. Burns can be caused due to flames, scalds,
exposure to natural gases, alcohols or combustible liquids, contact with hot metal or liquids,
electrical burns, chemical burn, cold injury or the frost bites, ionization and sun burns.
Severe damage to the epidermal or the dermal layer of the skin may be caused by electrical
or chemical burns such as acids and alkalis.
2. Assessment:
Clinical features- Superficial burns- erythyma and brisk cap refill. burn is painful
Superficial dermal burns-Reddened wound with blisters and brisk cap refill. Painful burn
Deep dermal- Reddened and mottled white slough, cap refill is absent. Excessive pain.
full thickness- Cap refill is absent, wound is dry and charred, less pain. The surface area
affected by the burn should be estimated by using the rules of nine and Lund Browder burn
chart. The skin with the isolated erythyma should not be taken under calculation. It is
essential to assess whether the patient is haemodynamically stable.
Assessment of burns involves clinical examination of the body and the assessment of the
ABCs (airway, breathing and circulation). It is essential to establish the tetanus immunization
of the patient, drug therapies, and drug sensitivities. If the burn is sustained in an enclosed
space then there is a possibility for the inhalation injury. It is essential to monitor the body
surface area such as the anatomical regions, palmer surface of the hand of the patient,
depth of the burn (first, second and third degree).
3. Management:
The initial management of patients with burns involves airway management, homeostasis,
and maintenance of body temperature.
If there is a sign of airway burn then, oxygen, IPPV and early airway management is
necessary. If the patient is haemodynamically unstable then the patient should be assessed
for injuries like blast or cyanide toxicity. In case the patient is having pain, active cooling
packs for 20 minutes should be administered and analgesics, Ketamine and Midazolam can
be given. 1-2.5 mg of Midazolam can be taken every 3-5 minutes. 10-30mg of Ketamine
can be repeated every 2- minutes. The maximum amount of dosage is 1mg/Kg. In patients
without acute pain, cling wrap and burn-aid dressings should be done (only if <20% BSA
adults).
In order to manage burns, the health care providers may cover the burned area by using the
sterile bandages with topical antibiotics.
Contraindications- Patient can get hypersensitive to Midazolam.
For Ketamine:
Analgesia-
Hypersensitivity to ketamine, suspected ACS and acute heart failure.
4. Impact of Management:
Effect- Ketamine is used as an anesthesia that is a NMDA antagonist. When applied in low
doses, it produces analgesic effect and the respiratory drives or the airway reflexes are
preserved.
Adverse effects- Some of the side effects of Midazolam are hypotension, respiratory
depression when taken with other depressant medication, narcotics and alcohol. Side effects
involving Ketamine may involve Disinhibition, Emergence, Hypertension, Tachcardia,
depression of consciousness, Hypersalivation, nausea and vomiting.
Stroke/ Transient Ischemic Attack:
chart. The skin with the isolated erythyma should not be taken under calculation. It is
essential to assess whether the patient is haemodynamically stable.
Assessment of burns involves clinical examination of the body and the assessment of the
ABCs (airway, breathing and circulation). It is essential to establish the tetanus immunization
of the patient, drug therapies, and drug sensitivities. If the burn is sustained in an enclosed
space then there is a possibility for the inhalation injury. It is essential to monitor the body
surface area such as the anatomical regions, palmer surface of the hand of the patient,
depth of the burn (first, second and third degree).
3. Management:
The initial management of patients with burns involves airway management, homeostasis,
and maintenance of body temperature.
If there is a sign of airway burn then, oxygen, IPPV and early airway management is
necessary. If the patient is haemodynamically unstable then the patient should be assessed
for injuries like blast or cyanide toxicity. In case the patient is having pain, active cooling
packs for 20 minutes should be administered and analgesics, Ketamine and Midazolam can
be given. 1-2.5 mg of Midazolam can be taken every 3-5 minutes. 10-30mg of Ketamine
can be repeated every 2- minutes. The maximum amount of dosage is 1mg/Kg. In patients
without acute pain, cling wrap and burn-aid dressings should be done (only if <20% BSA
adults).
In order to manage burns, the health care providers may cover the burned area by using the
sterile bandages with topical antibiotics.
Contraindications- Patient can get hypersensitive to Midazolam.
For Ketamine:
Analgesia-
Hypersensitivity to ketamine, suspected ACS and acute heart failure.
4. Impact of Management:
Effect- Ketamine is used as an anesthesia that is a NMDA antagonist. When applied in low
doses, it produces analgesic effect and the respiratory drives or the airway reflexes are
preserved.
Adverse effects- Some of the side effects of Midazolam are hypotension, respiratory
depression when taken with other depressant medication, narcotics and alcohol. Side effects
involving Ketamine may involve Disinhibition, Emergence, Hypertension, Tachcardia,
depression of consciousness, Hypersalivation, nausea and vomiting.
Stroke/ Transient Ischemic Attack:
1. Cause of the Disease/ Injury:
The brain cells needs oxygen and glucose for the functioning. When the blood supply is lost
and the nutrients are lost, then the brain cells stops working. The blood supply to the brain
can be loss or depleted by a number of ways. Blood clots can form in the arteries of the
brain known as thrombosis. This occurs by the gradual narrowing of the blood vessels by the
building up of fatty acids. The blood clots flow downstream from the heart and get
accumulated in tiny blood vessels. The blood clot is formed due to the embolus. This
interruption of the blood flow to that part of the brain that causes a temporary stroke like
symptoms.
2. Assessment:
Some of the clinical presentations involve hemiplegia and hemiparesis, dyspahagia and
visual disturbances. Sudden onset of headaches may also occur. There are certain
conditions that mimics stroke and should be considered while the visual assessment. Those
are conversion disorder, seizures and post ictal states, hemiplagic migraines and electrolyte
abnormalities.
The mental state should be assessed for making certain that the patient is oriented and
alert. It is necessary to check the eye range of motion and the facial movement for
evaluating the cranial nerves. The neck should be listened to and checked with stethoscope
for detecting abnormal sounds. The arms and the legs should be examined. The
coordination and the balance of the patient should be checked. Electrocardiogram has to be
used for confirming the regular heart rate. CT scan for assessing the bleeding. CT
angiogram for evaluating cerebral, vertebral and the carotid arteries (to be done after
admission to the hospital).
3. Management:
The main considerations after stroke should be oxygen therapy; medications like Anti-
emetic, analgesia and IV fluids can be given. If the assessment finds out a clear indication of
stroke then acute stroke referrals should be given.
TIA can be managed by antiplatelet therapy. Medicines like aspirin, dipyridamole,
clopidogrel, aspirin has to be given for widening the arteries. 300 mg of aspirin can be given,
that can be chewed or swallowed with water. 600 mg of clopidogrel can be given with a sip
of water.
If an area containing carotid artery is affected due to the TIA then cardioendarectomy can
also be done (Only after being referred to critical care unit).
Contraindications of Aspirin- Hypersensitivity to aspirins, bleeding or clotting disorders, chest
pain with overdose of the psycho-stimulants.
Contraindications for clopidogrel- Hypersensitive reaction to clopidogrel, active bleeding, and
patients contraindicated for the fibroninolysis administration in the prehopital period.
4. Impact of Management:
The brain cells needs oxygen and glucose for the functioning. When the blood supply is lost
and the nutrients are lost, then the brain cells stops working. The blood supply to the brain
can be loss or depleted by a number of ways. Blood clots can form in the arteries of the
brain known as thrombosis. This occurs by the gradual narrowing of the blood vessels by the
building up of fatty acids. The blood clots flow downstream from the heart and get
accumulated in tiny blood vessels. The blood clot is formed due to the embolus. This
interruption of the blood flow to that part of the brain that causes a temporary stroke like
symptoms.
2. Assessment:
Some of the clinical presentations involve hemiplegia and hemiparesis, dyspahagia and
visual disturbances. Sudden onset of headaches may also occur. There are certain
conditions that mimics stroke and should be considered while the visual assessment. Those
are conversion disorder, seizures and post ictal states, hemiplagic migraines and electrolyte
abnormalities.
The mental state should be assessed for making certain that the patient is oriented and
alert. It is necessary to check the eye range of motion and the facial movement for
evaluating the cranial nerves. The neck should be listened to and checked with stethoscope
for detecting abnormal sounds. The arms and the legs should be examined. The
coordination and the balance of the patient should be checked. Electrocardiogram has to be
used for confirming the regular heart rate. CT scan for assessing the bleeding. CT
angiogram for evaluating cerebral, vertebral and the carotid arteries (to be done after
admission to the hospital).
3. Management:
The main considerations after stroke should be oxygen therapy; medications like Anti-
emetic, analgesia and IV fluids can be given. If the assessment finds out a clear indication of
stroke then acute stroke referrals should be given.
TIA can be managed by antiplatelet therapy. Medicines like aspirin, dipyridamole,
clopidogrel, aspirin has to be given for widening the arteries. 300 mg of aspirin can be given,
that can be chewed or swallowed with water. 600 mg of clopidogrel can be given with a sip
of water.
If an area containing carotid artery is affected due to the TIA then cardioendarectomy can
also be done (Only after being referred to critical care unit).
Contraindications of Aspirin- Hypersensitivity to aspirins, bleeding or clotting disorders, chest
pain with overdose of the psycho-stimulants.
Contraindications for clopidogrel- Hypersensitive reaction to clopidogrel, active bleeding, and
patients contraindicated for the fibroninolysis administration in the prehopital period.
4. Impact of Management:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Effects- Aspirin inhibits the aggregation of the4 platelets by inhibiting the cyclo- oxygenase,
thus the blood thins and prevents the formation of clots, thus reducing the chance of stroke.
Clopidogrel is a platelet aggregation inhibitor that inhibits the aggregation by binding to
Adenosine diphosphate.
Side effects of Aspirin- Nausea, vomiting, GI bleeding and bronchospasm induced by
NSAIDs.
Side effects with clopidogrel- Haemorrhage.
thus the blood thins and prevents the formation of clots, thus reducing the chance of stroke.
Clopidogrel is a platelet aggregation inhibitor that inhibits the aggregation by binding to
Adenosine diphosphate.
Side effects of Aspirin- Nausea, vomiting, GI bleeding and bronchospasm induced by
NSAIDs.
Side effects with clopidogrel- Haemorrhage.
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





