Analyzing Asthma: A Case Study on Pathophysiology and Nursing
VerifiedAdded on 2023/06/05
|11
|3411
|280
Case Study
AI Summary
This assignment presents a case study focusing on asthma, detailing its pathogenesis, etiology, and appropriate nursing management strategies. It begins by outlining the pathophysiology of asthma, highlighting the role of allergens, inflammatory mediators, and immunological responses leading to bronchoconstriction, mucus hypersecretion, and airway remodeling. The study further discusses diagnostic methods, risk factors, and both primary and secondary prevention strategies. Pharmacological interventions, including oxygen therapy, beta2-agonists, anticholinergic drugs, and corticosteroids, are examined alongside crucial nursing management strategies such as patient education, allergen control, and respiratory status assessment. The case study also delves into the management of acute asthma attacks, emphasizing the importance of pharmacological therapy, correct inhaler techniques, and collaborative care between healthcare providers and patients. The assignment concludes by addressing specific pharmacological treatments like nebulized salbutamol, ipratropium bromide, and hydrocortisone, explaining their mechanisms of action and associated nursing implications.
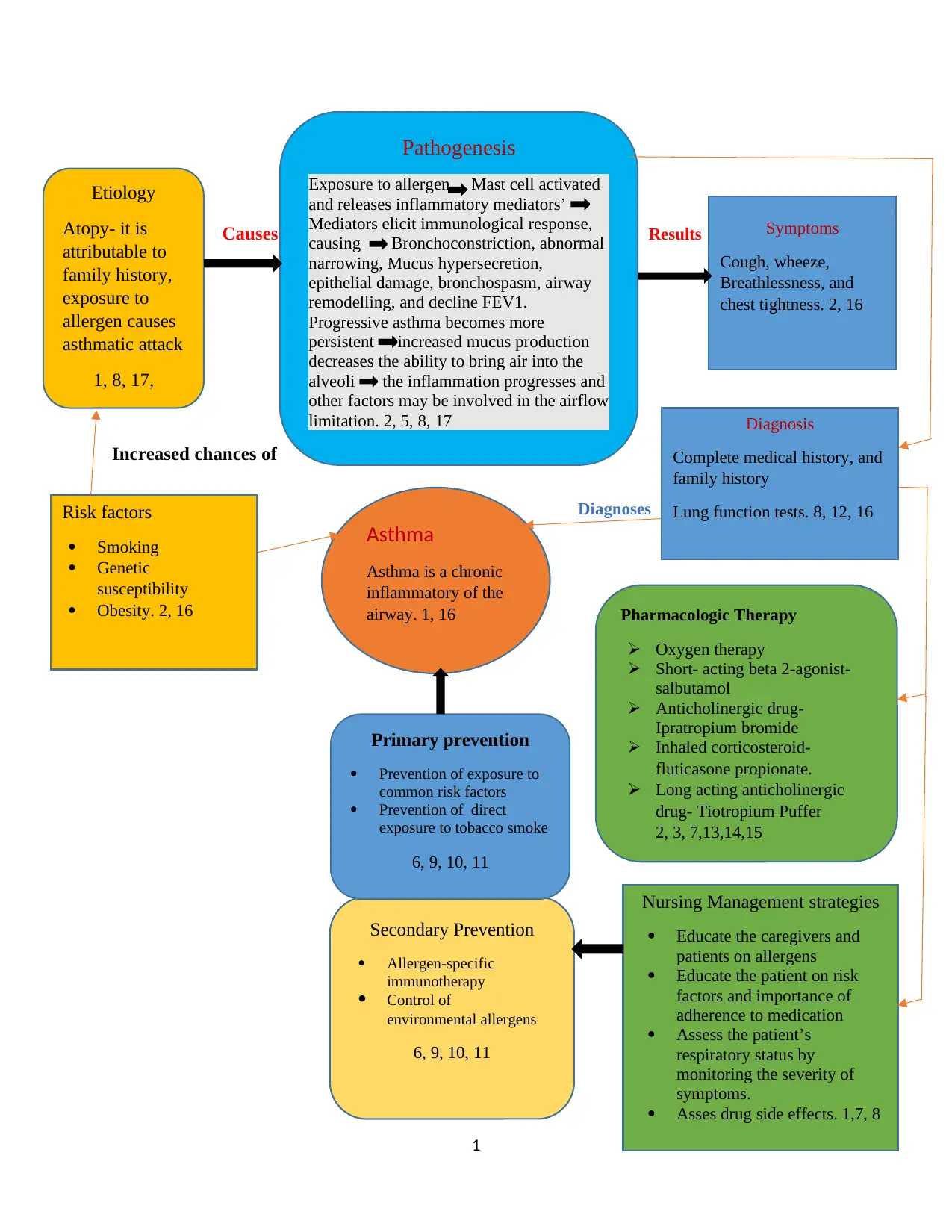
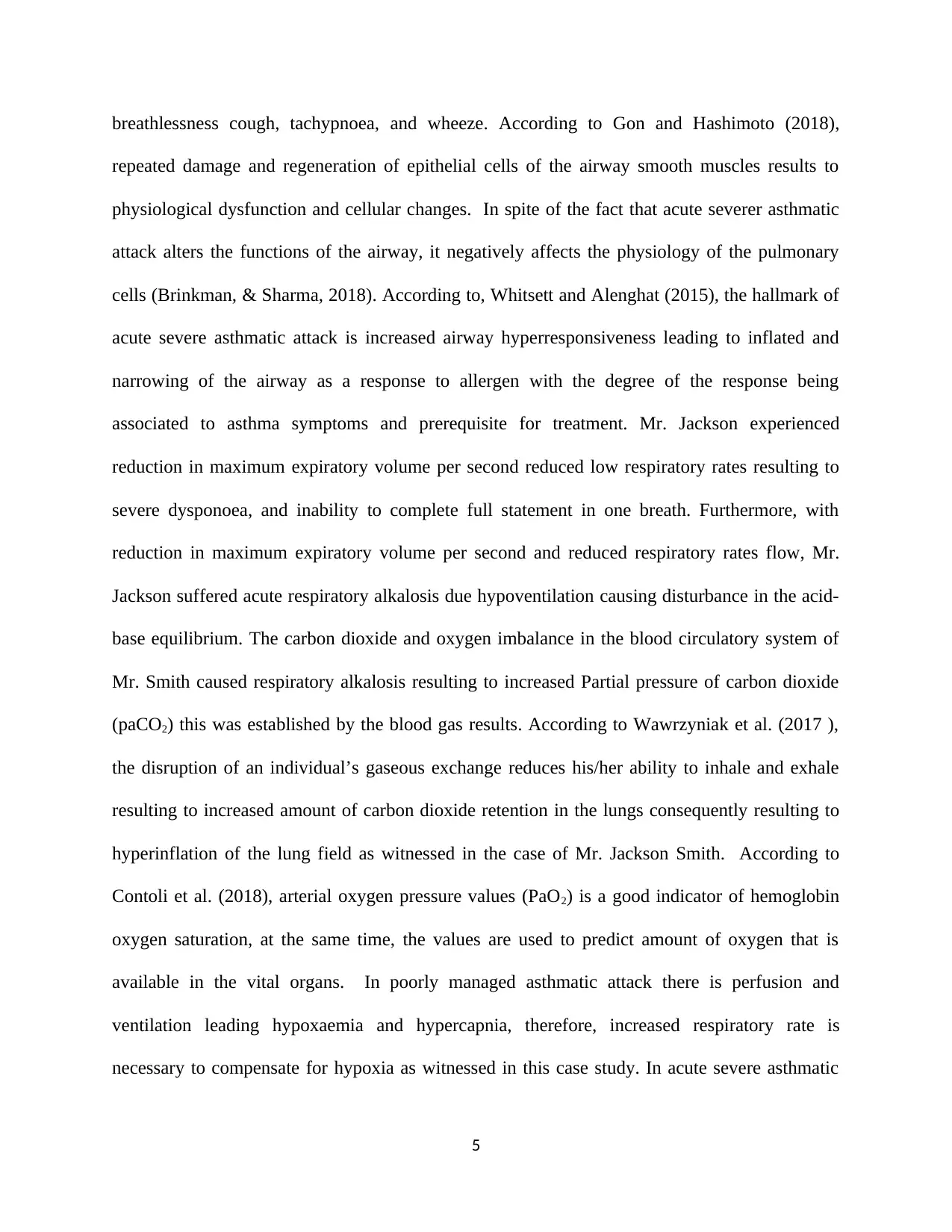
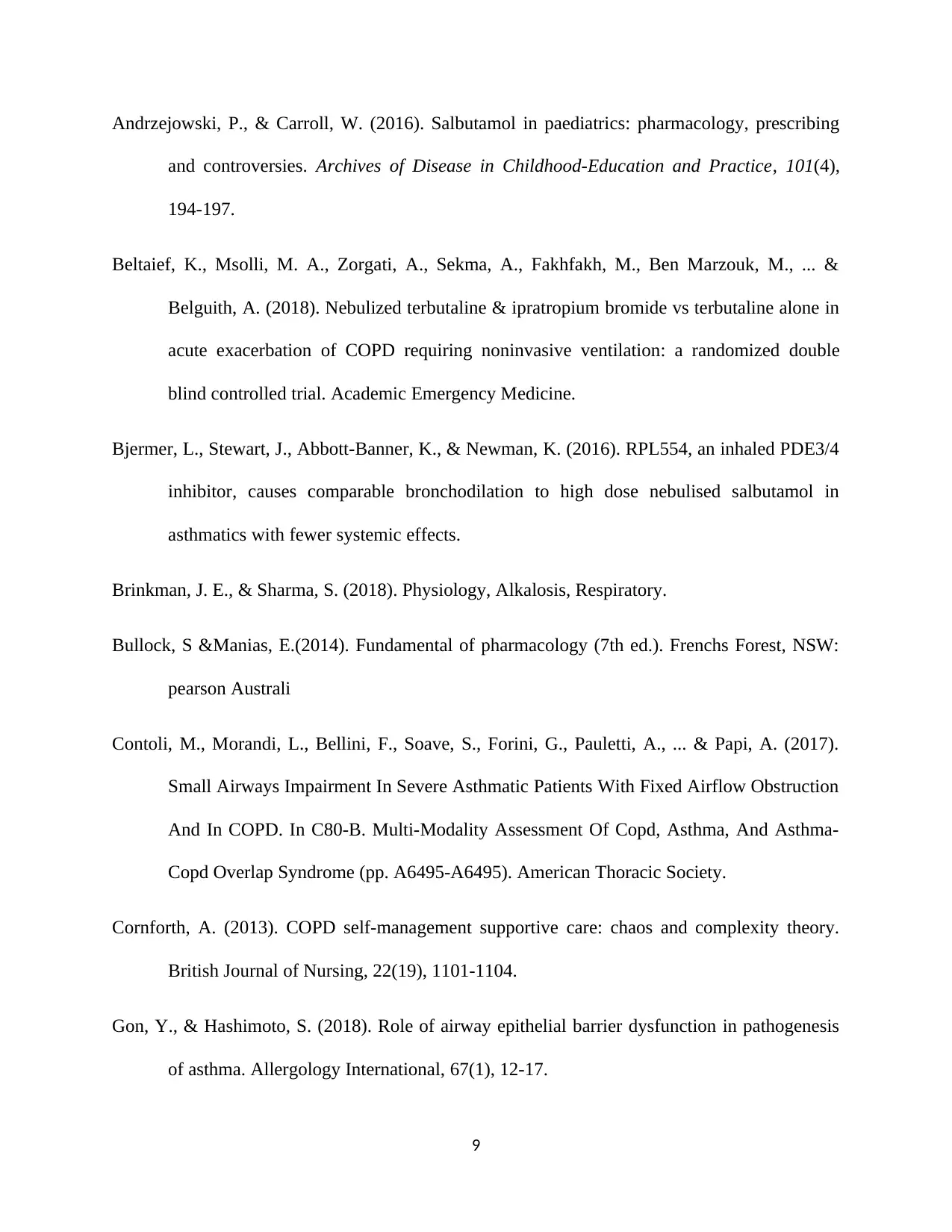
Causes Results
Caues
Increased chances of
Diagnoses
Control
1
Asthma
Asthma is a chronic
inflammatory of the
airway. 1, 16
Pathogenesis
Exposure to allergen Mast cell activated
and releases inflammatory mediators’
Mediators elicit immunological response,
causing Bronchoconstriction, abnormal
narrowing, Mucus hypersecretion,
epithelial damage, bronchospasm, airway
remodelling, and decline FEV1.
Progressive asthma becomes more
persistent increased mucus production
decreases the ability to bring air into the
alveoli the inflammation progresses and
other factors may be involved in the airflow
limitation. 2, 5, 8, 17
Symptoms
Cough, wheeze,
Breathlessness, and
chest tightness. 2, 16
Diagnosis
Complete medical history, and
family history
Lung function tests. 8, 12, 16
Pharmacologic Therapy
Oxygen therapy
Short- acting beta 2-agonist-
salbutamol
Anticholinergic drug-
Ipratropium bromide
Inhaled corticosteroid-
fluticasone propionate.
Long acting anticholinergic
drug- Tiotropium Puffer
2, 3, 7,13,14,15
Nursing Management strategies
Educate the caregivers and
patients on allergens
Educate the patient on risk
factors and importance of
adherence to medication
Assess the patient’s
respiratory status by
monitoring the severity of
symptoms.
Asses drug side effects. 1,7, 8
Secondary Prevention
Allergen-specific
immunotherapy
Control of
environmental allergens
6, 9, 10, 11
Primary prevention
Prevention of exposure to
common risk factors
Prevention of direct
exposure to tobacco smoke
6, 9, 10, 11
Etiology
Atopy- it is
attributable to
family history,
exposure to
allergen causes
asthmatic attack
1, 8, 17,
Risk factors
Smoking
Genetic
susceptibility
Obesity. 2, 16
Caues
Increased chances of
Diagnoses
Control
1
Asthma
Asthma is a chronic
inflammatory of the
airway. 1, 16
Pathogenesis
Exposure to allergen Mast cell activated
and releases inflammatory mediators’
Mediators elicit immunological response,
causing Bronchoconstriction, abnormal
narrowing, Mucus hypersecretion,
epithelial damage, bronchospasm, airway
remodelling, and decline FEV1.
Progressive asthma becomes more
persistent increased mucus production
decreases the ability to bring air into the
alveoli the inflammation progresses and
other factors may be involved in the airflow
limitation. 2, 5, 8, 17
Symptoms
Cough, wheeze,
Breathlessness, and
chest tightness. 2, 16
Diagnosis
Complete medical history, and
family history
Lung function tests. 8, 12, 16
Pharmacologic Therapy
Oxygen therapy
Short- acting beta 2-agonist-
salbutamol
Anticholinergic drug-
Ipratropium bromide
Inhaled corticosteroid-
fluticasone propionate.
Long acting anticholinergic
drug- Tiotropium Puffer
2, 3, 7,13,14,15
Nursing Management strategies
Educate the caregivers and
patients on allergens
Educate the patient on risk
factors and importance of
adherence to medication
Assess the patient’s
respiratory status by
monitoring the severity of
symptoms.
Asses drug side effects. 1,7, 8
Secondary Prevention
Allergen-specific
immunotherapy
Control of
environmental allergens
6, 9, 10, 11
Primary prevention
Prevention of exposure to
common risk factors
Prevention of direct
exposure to tobacco smoke
6, 9, 10, 11
Etiology
Atopy- it is
attributable to
family history,
exposure to
allergen causes
asthmatic attack
1, 8, 17,
Risk factors
Smoking
Genetic
susceptibility
Obesity. 2, 16
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
References
1. Aitken, L., & Chaboyer, W. (2016). ACCCN's Critical Care Nursing. Elsevier Health
Sciences.
2. Andrzejowski, P., & Carroll, W. (2016). Salbutamol in paediatrics: pharmacology,
prescribing and controversies. Archives of Disease in Childhood-Education and Practice,
101(4), 194-197.
3. Bullock, S., & Manias, E. (2013). Fundamentals of pharmacology. Pearson Higher
Education AU.
4. Cornforth, A. (2013). COPD self-management supportive care: chaos and complexity
theory. British Journal of Nursing, 22(19), 1101-1104
5. Craft, J., Gordon, C., Huether, S. E., McCance, K. L., & Brashers, V. L. (2015).
Understanding pathophysiology-ANZ adaptation. Elsevier Health Sciences.
6. Fleischer, D. M., Sicherer, S., Greenhawt, M., Campbell, D., Chan, E. S., Muraro, A., ...
& Sampson, H. (2015). Consensus communication on early peanut introduction and the
prevention of peanut allergy in high-risk infants. World Allergy Organization Journal,
8(1), 1.
7. Hazeldine, V. (2013). Pharmacological management of acute asthma exacerbations in
adults. Nursing Standard (through 2013), 27(33), 43.
8. Kaufman, G. (2011). Asthma: pathophysiology, diagnosis and management. Nursing
Standard, 26(5).
9. Morjaria, J. B., Caruso, M., Emma, R., Russo, C., & Polosa, R. (2018). Treatment of
allergic rhinitis as a strategy for preventing asthma. Current allergy and asthma reports,
18(4), 23.
10. Nieto, A., Wahn, U., Bufe, A., Eigenmann, P., Halken, S., Hedlin, G., ... & Lau, S.
(2014). Allergy and asthma prevention 2014. Pediatric Allergy and Immunology, 25(6),
516-533.
11. Prevention strategies for asthma-secondary prevention. (2005). CMAJ: Canadian Medical
Association Journal, 173(6 Suppl), S25–S27.
12. Sarver N, Murphy K (2009). Management of asthma. New approaches to establishing
control. Journal of The American Academy of Nurse Practitioners. 21, 1, 54-65.
2
1. Aitken, L., & Chaboyer, W. (2016). ACCCN's Critical Care Nursing. Elsevier Health
Sciences.
2. Andrzejowski, P., & Carroll, W. (2016). Salbutamol in paediatrics: pharmacology,
prescribing and controversies. Archives of Disease in Childhood-Education and Practice,
101(4), 194-197.
3. Bullock, S., & Manias, E. (2013). Fundamentals of pharmacology. Pearson Higher
Education AU.
4. Cornforth, A. (2013). COPD self-management supportive care: chaos and complexity
theory. British Journal of Nursing, 22(19), 1101-1104
5. Craft, J., Gordon, C., Huether, S. E., McCance, K. L., & Brashers, V. L. (2015).
Understanding pathophysiology-ANZ adaptation. Elsevier Health Sciences.
6. Fleischer, D. M., Sicherer, S., Greenhawt, M., Campbell, D., Chan, E. S., Muraro, A., ...
& Sampson, H. (2015). Consensus communication on early peanut introduction and the
prevention of peanut allergy in high-risk infants. World Allergy Organization Journal,
8(1), 1.
7. Hazeldine, V. (2013). Pharmacological management of acute asthma exacerbations in
adults. Nursing Standard (through 2013), 27(33), 43.
8. Kaufman, G. (2011). Asthma: pathophysiology, diagnosis and management. Nursing
Standard, 26(5).
9. Morjaria, J. B., Caruso, M., Emma, R., Russo, C., & Polosa, R. (2018). Treatment of
allergic rhinitis as a strategy for preventing asthma. Current allergy and asthma reports,
18(4), 23.
10. Nieto, A., Wahn, U., Bufe, A., Eigenmann, P., Halken, S., Hedlin, G., ... & Lau, S.
(2014). Allergy and asthma prevention 2014. Pediatric Allergy and Immunology, 25(6),
516-533.
11. Prevention strategies for asthma-secondary prevention. (2005). CMAJ: Canadian Medical
Association Journal, 173(6 Suppl), S25–S27.
12. Sarver N, Murphy K (2009). Management of asthma. New approaches to establishing
control. Journal of The American Academy of Nurse Practitioners. 21, 1, 54-65.
2
13. Sher, L., Yiu, G., Sakov, A., Liu, S., & Caracta, C. (2017). Treatment of Asthmatic
Patients with Fluticasone Propionate and Fluticasone Propionate/Salmeterol Multidose
Dry Powder Inhalers Compared with Placebo: Patient-Reported Outcomes and Quality of
Life. Journal of Allergy and Clinical Immunology, 139(2), AB97.
14. Sullivan, P. W., Ghushchyan, V. H., Globe, G., & Schatz, M. (2018). Oral corticosteroid
exposure and adverse effects in asthmatic patients. Journal of Allergy and Clinical
Immunology, 141(1), 110-
15. Thomas, V., Gefen, E., Gopalan, G., Mares, R., McDonald, R., Ming, S. W. Y., & Price,
D. B. (2017). Ipratropium/Salbutamol Comparator Versus Originator for Chronic
Obstructive Pulmonary Disease Exacerbations: USA Observational Cohort Study Using
the Clinformatics™ Health Claims Database. Pulmonary Therapy, 3(1), 187-205.
16. Vogelmeier, C. F., Criner, G. J., Martinez, F. J., Anzueto, A., Barnes, P. J., Bourbeau,
J., ... & Frith, P. (2017). Global strategy for the diagnosis, management, and prevention
of chronic obstructive lung disease 2017 report. GOLD executive summary. American
journal of respiratory and critical care medicine, 195(5), 557-582.
17. Whitsett, J. A., & Alenghat, T. (2015). Respiratory epithelial cells orchestrate pulmonary
innate immunity. Nature immunology, 16(1), 27.
3
Patients with Fluticasone Propionate and Fluticasone Propionate/Salmeterol Multidose
Dry Powder Inhalers Compared with Placebo: Patient-Reported Outcomes and Quality of
Life. Journal of Allergy and Clinical Immunology, 139(2), AB97.
14. Sullivan, P. W., Ghushchyan, V. H., Globe, G., & Schatz, M. (2018). Oral corticosteroid
exposure and adverse effects in asthmatic patients. Journal of Allergy and Clinical
Immunology, 141(1), 110-
15. Thomas, V., Gefen, E., Gopalan, G., Mares, R., McDonald, R., Ming, S. W. Y., & Price,
D. B. (2017). Ipratropium/Salbutamol Comparator Versus Originator for Chronic
Obstructive Pulmonary Disease Exacerbations: USA Observational Cohort Study Using
the Clinformatics™ Health Claims Database. Pulmonary Therapy, 3(1), 187-205.
16. Vogelmeier, C. F., Criner, G. J., Martinez, F. J., Anzueto, A., Barnes, P. J., Bourbeau,
J., ... & Frith, P. (2017). Global strategy for the diagnosis, management, and prevention
of chronic obstructive lung disease 2017 report. GOLD executive summary. American
journal of respiratory and critical care medicine, 195(5), 557-582.
17. Whitsett, J. A., & Alenghat, T. (2015). Respiratory epithelial cells orchestrate pulmonary
innate immunity. Nature immunology, 16(1), 27.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Answers to assignment 2
Pathogenesis of acute asthma
Mr. Jackson Smith diagnosis was confirmed by laboratory diagnosis including blood gas after he
presented with symptoms including breathlessness, severer dysponoea, and wheeze. At the same
time, his past medical history confirmed that he was diagnosed with asthma at the age of two
years. Acute severe asthmatic attack occurs when an individual is exposed to environmental
allergens such as smoke, dust, pollen grain among others. According to Kaufman (2012), during
acute severe asthmatic attack the normal functioning of the lower respiratory tract that include
the trachea, the bronchi, and the bronchioles is greatly affected. The constriction of bronchial and
the abnormal narrowing of the airways due to epithelial damage, mucus hypersecretion, and
bronchospasm have been mostly cited as the main cause of adverse symptoms experienced by
the asthmatic patient (Hamid, Mahboub, & Ramakrishnan, 2018). Acute asthmatic attack occurs
when an individual is exposed to an allergen that is capable of eliciting immunological reactions
leading to production of inflammatory mediators by mast cells among others. The result of the
immunological response is airways smooth muscles constriction, and hypersecretion of mucus
leading to narrowing and blockage of the airway. According to Whitsett and Alenghat (2015),
hypersensitivity induced by environmental allergen leading to bronchoconstriction and airway
inflammation can be attributed to IgE-dependent mediators that are released by the mast cells
including histamine and prostaglandins whose activities directly cause constriction to the airways
smooth muscles.
Wawrzyniak et al. (2017), suggested that whenever, smooth flow of air into the lung is
interrupted as a result of narrowing of the airways and bronchial wall inflammation there is an
increase in the decline of Forced Expiratory Volume in one second (FEV1) resulting to
4
Pathogenesis of acute asthma
Mr. Jackson Smith diagnosis was confirmed by laboratory diagnosis including blood gas after he
presented with symptoms including breathlessness, severer dysponoea, and wheeze. At the same
time, his past medical history confirmed that he was diagnosed with asthma at the age of two
years. Acute severe asthmatic attack occurs when an individual is exposed to environmental
allergens such as smoke, dust, pollen grain among others. According to Kaufman (2012), during
acute severe asthmatic attack the normal functioning of the lower respiratory tract that include
the trachea, the bronchi, and the bronchioles is greatly affected. The constriction of bronchial and
the abnormal narrowing of the airways due to epithelial damage, mucus hypersecretion, and
bronchospasm have been mostly cited as the main cause of adverse symptoms experienced by
the asthmatic patient (Hamid, Mahboub, & Ramakrishnan, 2018). Acute asthmatic attack occurs
when an individual is exposed to an allergen that is capable of eliciting immunological reactions
leading to production of inflammatory mediators by mast cells among others. The result of the
immunological response is airways smooth muscles constriction, and hypersecretion of mucus
leading to narrowing and blockage of the airway. According to Whitsett and Alenghat (2015),
hypersensitivity induced by environmental allergen leading to bronchoconstriction and airway
inflammation can be attributed to IgE-dependent mediators that are released by the mast cells
including histamine and prostaglandins whose activities directly cause constriction to the airways
smooth muscles.
Wawrzyniak et al. (2017), suggested that whenever, smooth flow of air into the lung is
interrupted as a result of narrowing of the airways and bronchial wall inflammation there is an
increase in the decline of Forced Expiratory Volume in one second (FEV1) resulting to
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
breathlessness cough, tachypnoea, and wheeze. According to Gon and Hashimoto (2018),
repeated damage and regeneration of epithelial cells of the airway smooth muscles results to
physiological dysfunction and cellular changes. In spite of the fact that acute severer asthmatic
attack alters the functions of the airway, it negatively affects the physiology of the pulmonary
cells (Brinkman, & Sharma, 2018). According to, Whitsett and Alenghat (2015), the hallmark of
acute severe asthmatic attack is increased airway hyperresponsiveness leading to inflated and
narrowing of the airway as a response to allergen with the degree of the response being
associated to asthma symptoms and prerequisite for treatment. Mr. Jackson experienced
reduction in maximum expiratory volume per second reduced low respiratory rates resulting to
severe dysponoea, and inability to complete full statement in one breath. Furthermore, with
reduction in maximum expiratory volume per second and reduced respiratory rates flow, Mr.
Jackson suffered acute respiratory alkalosis due hypoventilation causing disturbance in the acid-
base equilibrium. The carbon dioxide and oxygen imbalance in the blood circulatory system of
Mr. Smith caused respiratory alkalosis resulting to increased Partial pressure of carbon dioxide
(paCO2) this was established by the blood gas results. According to Wawrzyniak et al. (2017 ),
the disruption of an individual’s gaseous exchange reduces his/her ability to inhale and exhale
resulting to increased amount of carbon dioxide retention in the lungs consequently resulting to
hyperinflation of the lung field as witnessed in the case of Mr. Jackson Smith. According to
Contoli et al. (2018), arterial oxygen pressure values (PaO2) is a good indicator of hemoglobin
oxygen saturation, at the same time, the values are used to predict amount of oxygen that is
available in the vital organs. In poorly managed asthmatic attack there is perfusion and
ventilation leading hypoxaemia and hypercapnia, therefore, increased respiratory rate is
necessary to compensate for hypoxia as witnessed in this case study. In acute severe asthmatic
5
repeated damage and regeneration of epithelial cells of the airway smooth muscles results to
physiological dysfunction and cellular changes. In spite of the fact that acute severer asthmatic
attack alters the functions of the airway, it negatively affects the physiology of the pulmonary
cells (Brinkman, & Sharma, 2018). According to, Whitsett and Alenghat (2015), the hallmark of
acute severe asthmatic attack is increased airway hyperresponsiveness leading to inflated and
narrowing of the airway as a response to allergen with the degree of the response being
associated to asthma symptoms and prerequisite for treatment. Mr. Jackson experienced
reduction in maximum expiratory volume per second reduced low respiratory rates resulting to
severe dysponoea, and inability to complete full statement in one breath. Furthermore, with
reduction in maximum expiratory volume per second and reduced respiratory rates flow, Mr.
Jackson suffered acute respiratory alkalosis due hypoventilation causing disturbance in the acid-
base equilibrium. The carbon dioxide and oxygen imbalance in the blood circulatory system of
Mr. Smith caused respiratory alkalosis resulting to increased Partial pressure of carbon dioxide
(paCO2) this was established by the blood gas results. According to Wawrzyniak et al. (2017 ),
the disruption of an individual’s gaseous exchange reduces his/her ability to inhale and exhale
resulting to increased amount of carbon dioxide retention in the lungs consequently resulting to
hyperinflation of the lung field as witnessed in the case of Mr. Jackson Smith. According to
Contoli et al. (2018), arterial oxygen pressure values (PaO2) is a good indicator of hemoglobin
oxygen saturation, at the same time, the values are used to predict amount of oxygen that is
available in the vital organs. In poorly managed asthmatic attack there is perfusion and
ventilation leading hypoxaemia and hypercapnia, therefore, increased respiratory rate is
necessary to compensate for hypoxia as witnessed in this case study. In acute severe asthmatic
5
attack as witnessed in the case of Mr. Smith PaO2 there is hypoventilation caused by
bronchoconstriction and inflammation that disrupted pulmonary functions resulting to low levels
of PaO2 and accumulation of lactic acid in the blood as revealed by the blood gas results. At the
same time, capillaries may dilate the consequences microvascular leakage include oedema, lack
of clearance by mucociliary, and increased bronchial hypersecretion.
Answers to Question 2
The main objective of the nursing strategies in the treatment and management of acute severe
asthma is to reduce the mortality and morbidity rates. In the case of Mr. Smith the desired
outcome would be to improve airway clearance through pharmacological therapy and
rehabilitation. According to Cornforth (2013), the critical ingredient in the acute asthma
management strategy involves collaborative working between healthcare providers such as
nurses and the patients with dissemination of comprehensive information to the patient and
caregivers about acute asthma. The correct inhaler techniques and medication adherence can
only be achieved through proper nursing education, regular monitoring, and partnership working
between nurses and patients which critical (Sarver and Murphy, 2009). Nursing education will
inform the asthmatic patients and their caregivers that by avoiding environmental allergens there
is reduced risks of episodic attacks, at the same time, it is helps highlight the importance of
adherence to pharmacological therapy. According to Papiris (2009), the findings from different
studies focusing on interventions that were introduced before the inception of acute asthmatic
attack to minimize the condition, at the same time, intervention introduced after the onset of the
asthmatic attack yielded good results . However, such interventions have been established to be
ineffective in situations where there is no controlled interventions that requires coordinated
partnership and regular monitoring to record peak flow by the nurses.
6
bronchoconstriction and inflammation that disrupted pulmonary functions resulting to low levels
of PaO2 and accumulation of lactic acid in the blood as revealed by the blood gas results. At the
same time, capillaries may dilate the consequences microvascular leakage include oedema, lack
of clearance by mucociliary, and increased bronchial hypersecretion.
Answers to Question 2
The main objective of the nursing strategies in the treatment and management of acute severe
asthma is to reduce the mortality and morbidity rates. In the case of Mr. Smith the desired
outcome would be to improve airway clearance through pharmacological therapy and
rehabilitation. According to Cornforth (2013), the critical ingredient in the acute asthma
management strategy involves collaborative working between healthcare providers such as
nurses and the patients with dissemination of comprehensive information to the patient and
caregivers about acute asthma. The correct inhaler techniques and medication adherence can
only be achieved through proper nursing education, regular monitoring, and partnership working
between nurses and patients which critical (Sarver and Murphy, 2009). Nursing education will
inform the asthmatic patients and their caregivers that by avoiding environmental allergens there
is reduced risks of episodic attacks, at the same time, it is helps highlight the importance of
adherence to pharmacological therapy. According to Papiris (2009), the findings from different
studies focusing on interventions that were introduced before the inception of acute asthmatic
attack to minimize the condition, at the same time, intervention introduced after the onset of the
asthmatic attack yielded good results . However, such interventions have been established to be
ineffective in situations where there is no controlled interventions that requires coordinated
partnership and regular monitoring to record peak flow by the nurses.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Answers to Question 3
Pharmacological therapy
When treating acute asthmatic attack opportune administration of β2-agonist, corticosteroid,
oxygen, and anticholinergic drugs is critical to improve the patients outcome as suggested by
Montuschi et al. (2014).
Nebulized Salbutamol
Salbutamol drug is categorized as β2 agonist, its mode of action involves stimulation of beta2
receptors found on the smooth muscles of the airways leading to muscles relaxation and causing
bronchodilation (Andrzejowski and Carroll, 2016; Bullock, &Manias, 2014). Therefore,
Salbutamol causes reduced air flow obstruction allowing free air flow through airways into the
alveoli leading to improved patient breathing. According to Vogelmeier et al. (2017), drugs that
have the capability to cause bronchodilation are used to increase FEV1 and reduce hyperinflation
hence, they are given on regular basis to prevent or reduce symptoms. It is recommended to use
oxygen-driven nebuliser to administer salbutamol (Bjermer et al., 2016). However, the nurses
should monitor the flow rate due to the fact that aerosols particles size is dependent on the
nebuliser flow rate. According to Papiris et al. (2009), the larger aerosols particles are deposited
in the upper airway, whereas alveoli can only accommodate the smaller aerosol particles size
(0.8-3.0 micrometers).
Ipratropium bromide
7
Pharmacological therapy
When treating acute asthmatic attack opportune administration of β2-agonist, corticosteroid,
oxygen, and anticholinergic drugs is critical to improve the patients outcome as suggested by
Montuschi et al. (2014).
Nebulized Salbutamol
Salbutamol drug is categorized as β2 agonist, its mode of action involves stimulation of beta2
receptors found on the smooth muscles of the airways leading to muscles relaxation and causing
bronchodilation (Andrzejowski and Carroll, 2016; Bullock, &Manias, 2014). Therefore,
Salbutamol causes reduced air flow obstruction allowing free air flow through airways into the
alveoli leading to improved patient breathing. According to Vogelmeier et al. (2017), drugs that
have the capability to cause bronchodilation are used to increase FEV1 and reduce hyperinflation
hence, they are given on regular basis to prevent or reduce symptoms. It is recommended to use
oxygen-driven nebuliser to administer salbutamol (Bjermer et al., 2016). However, the nurses
should monitor the flow rate due to the fact that aerosols particles size is dependent on the
nebuliser flow rate. According to Papiris et al. (2009), the larger aerosols particles are deposited
in the upper airway, whereas alveoli can only accommodate the smaller aerosol particles size
(0.8-3.0 micrometers).
Ipratropium bromide
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Ipratropium bromide is categorized as anticholinergic drug, its mechanism of action involves
stopping vagally mediated reflection actions by antagonizing the acetylcholine neurotransmitter
as suggested by Thomas et al. (2017). Therefore, it prevents bronchospasm thereby resulting to
bronchodilation and enabling relaxation of airway smooth muscles. The actions of this drug
therefore, help to reduce the obstruction of the airway, increased alveoli ventilation, and
increased FEV1. A studies review through meta-analysis established that early administration of
inhaled beta2 agonist combined with conducted by anticholinergic drugs reduces the admission
of asthmatic attack patient by 30% (Beltaief et al., 2018; Hazeldine, 2013). The Dr prescribed
Ipratropium bromide to Mr. Smith to improve the symptoms he was experiencing including
dysponoea, normalized respiratory rates, and wheezing among others.
Hydrocortisone
According to Keskin et al. (2016), hydrocortisone is categorized as glucocorticosteroid, they act
by reducing the sensitivity of beta-adrenergic receptors and preventing the migration of
inflammatory cells (Hazeldine, 2013). Therefore, this drug was necessary to reduce the
inflammatory responses experienced by Mr. Smith.
Nursing implications
The nurses should monitor various side effects caused by the prescribed drugs and offer nursing
education to help in the rehabilitation of the patient. Nurses should frequently monitor the
patients electrolyte levels, this is attributed to the fact that salbutamol is known to cause
hypokalaemia as suggested by Andrzejowski and Carroll (2016). There should be continuous
monitoring of vital signs such as heart rate and oxygen saturation. Nursing education is critical to
help the patient identify environmental allergens that might trigger asthmatic attack.
References
8
stopping vagally mediated reflection actions by antagonizing the acetylcholine neurotransmitter
as suggested by Thomas et al. (2017). Therefore, it prevents bronchospasm thereby resulting to
bronchodilation and enabling relaxation of airway smooth muscles. The actions of this drug
therefore, help to reduce the obstruction of the airway, increased alveoli ventilation, and
increased FEV1. A studies review through meta-analysis established that early administration of
inhaled beta2 agonist combined with conducted by anticholinergic drugs reduces the admission
of asthmatic attack patient by 30% (Beltaief et al., 2018; Hazeldine, 2013). The Dr prescribed
Ipratropium bromide to Mr. Smith to improve the symptoms he was experiencing including
dysponoea, normalized respiratory rates, and wheezing among others.
Hydrocortisone
According to Keskin et al. (2016), hydrocortisone is categorized as glucocorticosteroid, they act
by reducing the sensitivity of beta-adrenergic receptors and preventing the migration of
inflammatory cells (Hazeldine, 2013). Therefore, this drug was necessary to reduce the
inflammatory responses experienced by Mr. Smith.
Nursing implications
The nurses should monitor various side effects caused by the prescribed drugs and offer nursing
education to help in the rehabilitation of the patient. Nurses should frequently monitor the
patients electrolyte levels, this is attributed to the fact that salbutamol is known to cause
hypokalaemia as suggested by Andrzejowski and Carroll (2016). There should be continuous
monitoring of vital signs such as heart rate and oxygen saturation. Nursing education is critical to
help the patient identify environmental allergens that might trigger asthmatic attack.
References
8
Andrzejowski, P., & Carroll, W. (2016). Salbutamol in paediatrics: pharmacology, prescribing
and controversies. Archives of Disease in Childhood-Education and Practice, 101(4),
194-197.
Beltaief, K., Msolli, M. A., Zorgati, A., Sekma, A., Fakhfakh, M., Ben Marzouk, M., ... &
Belguith, A. (2018). Nebulized terbutaline & ipratropium bromide vs terbutaline alone in
acute exacerbation of COPD requiring noninvasive ventilation: a randomized double
blind controlled trial. Academic Emergency Medicine.
Bjermer, L., Stewart, J., Abbott-Banner, K., & Newman, K. (2016). RPL554, an inhaled PDE3/4
inhibitor, causes comparable bronchodilation to high dose nebulised salbutamol in
asthmatics with fewer systemic effects.
Brinkman, J. E., & Sharma, S. (2018). Physiology, Alkalosis, Respiratory.
Bullock, S &Manias, E.(2014). Fundamental of pharmacology (7th ed.). Frenchs Forest, NSW:
pearson Australi
Contoli, M., Morandi, L., Bellini, F., Soave, S., Forini, G., Pauletti, A., ... & Papi, A. (2017).
Small Airways Impairment In Severe Asthmatic Patients With Fixed Airflow Obstruction
And In COPD. In C80-B. Multi-Modality Assessment Of Copd, Asthma, And Asthma-
Copd Overlap Syndrome (pp. A6495-A6495). American Thoracic Society.
Cornforth, A. (2013). COPD self-management supportive care: chaos and complexity theory.
British Journal of Nursing, 22(19), 1101-1104.
Gon, Y., & Hashimoto, S. (2018). Role of airway epithelial barrier dysfunction in pathogenesis
of asthma. Allergology International, 67(1), 12-17.
9
and controversies. Archives of Disease in Childhood-Education and Practice, 101(4),
194-197.
Beltaief, K., Msolli, M. A., Zorgati, A., Sekma, A., Fakhfakh, M., Ben Marzouk, M., ... &
Belguith, A. (2018). Nebulized terbutaline & ipratropium bromide vs terbutaline alone in
acute exacerbation of COPD requiring noninvasive ventilation: a randomized double
blind controlled trial. Academic Emergency Medicine.
Bjermer, L., Stewart, J., Abbott-Banner, K., & Newman, K. (2016). RPL554, an inhaled PDE3/4
inhibitor, causes comparable bronchodilation to high dose nebulised salbutamol in
asthmatics with fewer systemic effects.
Brinkman, J. E., & Sharma, S. (2018). Physiology, Alkalosis, Respiratory.
Bullock, S &Manias, E.(2014). Fundamental of pharmacology (7th ed.). Frenchs Forest, NSW:
pearson Australi
Contoli, M., Morandi, L., Bellini, F., Soave, S., Forini, G., Pauletti, A., ... & Papi, A. (2017).
Small Airways Impairment In Severe Asthmatic Patients With Fixed Airflow Obstruction
And In COPD. In C80-B. Multi-Modality Assessment Of Copd, Asthma, And Asthma-
Copd Overlap Syndrome (pp. A6495-A6495). American Thoracic Society.
Cornforth, A. (2013). COPD self-management supportive care: chaos and complexity theory.
British Journal of Nursing, 22(19), 1101-1104.
Gon, Y., & Hashimoto, S. (2018). Role of airway epithelial barrier dysfunction in pathogenesis
of asthma. Allergology International, 67(1), 12-17.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Hamid, Q., Mahboub, B., & Ramakrishnan, R. K. (2018). Asthma-chronic obstructive
pulmonary disease overlap: A distinct pathophysiological and clinical entity. In Asthma,
COPD, and Overlap (pp. 55-66). CRC Press.
Hazeldine, V. (2013). Pharmacological management of acute asthma exacerbations in adults.
Nursing Standard (through 2013), 27(33), 43.
Kaufman, G. (2012). Asthma: assessment, diagnosis, and treatment adherence. Nurse
Prescribing, 10(7), 331-338.
Keskin, O., Uluca, U., Keskin, M., Gogebakan, B., Kucukosmanoglu, E., Ozkars, M. Y., ... &
Coskun, Y. (2016). The efficacy of single-high dose inhaled corticosteroid versus oral
prednisone treatment on exhaled leukotriene and 8-isoprostane levels in mild to moderate
asthmatic children with asthma exacerbation. Allergologia et immunopathologia, 44(2),
138-148.
Montuschi, P., Malerba, M., Santini, G., & Miravitlles, M. (2014). Pharmacological treatment of
chronic obstructive pulmonary disease: from evidence-based medicine to phenotyping.
Drug discovery today, 19(12), 1928-1935.
Papiris S, Manali E, Kolilekas L, Triantafillidou C, Tsangaris I (2009) Acute severe asthma: new
approaches to assessment and treatment. Drugs. 69, 17, 2363-2391.
Sarver N, Murphy K (2009). Management of asthma. New approaches to establishing control.
Journal of The American Academy of Nurse Practitioners. 21, 1, 54-65.
Thomas, V., Gefen, E., Gopalan, G., Mares, R., McDonald, R., Ming, S. W. Y., & Price, D. B.
(2017). Ipratropium/Salbutamol Comparator Versus Originator for Chronic Obstructive
10
pulmonary disease overlap: A distinct pathophysiological and clinical entity. In Asthma,
COPD, and Overlap (pp. 55-66). CRC Press.
Hazeldine, V. (2013). Pharmacological management of acute asthma exacerbations in adults.
Nursing Standard (through 2013), 27(33), 43.
Kaufman, G. (2012). Asthma: assessment, diagnosis, and treatment adherence. Nurse
Prescribing, 10(7), 331-338.
Keskin, O., Uluca, U., Keskin, M., Gogebakan, B., Kucukosmanoglu, E., Ozkars, M. Y., ... &
Coskun, Y. (2016). The efficacy of single-high dose inhaled corticosteroid versus oral
prednisone treatment on exhaled leukotriene and 8-isoprostane levels in mild to moderate
asthmatic children with asthma exacerbation. Allergologia et immunopathologia, 44(2),
138-148.
Montuschi, P., Malerba, M., Santini, G., & Miravitlles, M. (2014). Pharmacological treatment of
chronic obstructive pulmonary disease: from evidence-based medicine to phenotyping.
Drug discovery today, 19(12), 1928-1935.
Papiris S, Manali E, Kolilekas L, Triantafillidou C, Tsangaris I (2009) Acute severe asthma: new
approaches to assessment and treatment. Drugs. 69, 17, 2363-2391.
Sarver N, Murphy K (2009). Management of asthma. New approaches to establishing control.
Journal of The American Academy of Nurse Practitioners. 21, 1, 54-65.
Thomas, V., Gefen, E., Gopalan, G., Mares, R., McDonald, R., Ming, S. W. Y., & Price, D. B.
(2017). Ipratropium/Salbutamol Comparator Versus Originator for Chronic Obstructive
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Pulmonary Disease Exacerbations: USA Observational Cohort Study Using the
Clinformatics™ Health Claims Database. Pulmonary Therapy, 3(1), 187-205.
Vogelmeier, C. F., Criner, G. J., Martinez, F. J., Anzueto, A., Barnes, P. J., Bourbeau, J., ... &
Frith, P. (2017). Global strategy for the diagnosis, management, and prevention of
chronic obstructive lung disease 2017 report. GOLD executive summary. American
journal of respiratory and critical care medicine, 195(5), 557-582.
Wawrzyniak, P., Wawrzyniak, M., Wanke, K., Sokolowska, M., Bendelja, K., Rückert, B., &
Akdis, M. (2017). Regulation of bronchial epithelial barrier integrity by type 2 cytokines
and histone deacetylases in asthmatic patients. Journal of Allergy and Clinical
Immunology, 139(1), 93-103.
Whitsett, J. A., & Alenghat, T. (2015). Respiratory epithelial cells orchestrate pulmonary innate
immunity. Nature immunology, 16(1), 27.
11
Clinformatics™ Health Claims Database. Pulmonary Therapy, 3(1), 187-205.
Vogelmeier, C. F., Criner, G. J., Martinez, F. J., Anzueto, A., Barnes, P. J., Bourbeau, J., ... &
Frith, P. (2017). Global strategy for the diagnosis, management, and prevention of
chronic obstructive lung disease 2017 report. GOLD executive summary. American
journal of respiratory and critical care medicine, 195(5), 557-582.
Wawrzyniak, P., Wawrzyniak, M., Wanke, K., Sokolowska, M., Bendelja, K., Rückert, B., &
Akdis, M. (2017). Regulation of bronchial epithelial barrier integrity by type 2 cytokines
and histone deacetylases in asthmatic patients. Journal of Allergy and Clinical
Immunology, 139(1), 93-103.
Whitsett, J. A., & Alenghat, T. (2015). Respiratory epithelial cells orchestrate pulmonary innate
immunity. Nature immunology, 16(1), 27.
11
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




