Pathogenesis and Management of Acute Asthma: A Nursing Perspective
Added on 2023-06-05
11 Pages3411 Words280 Views
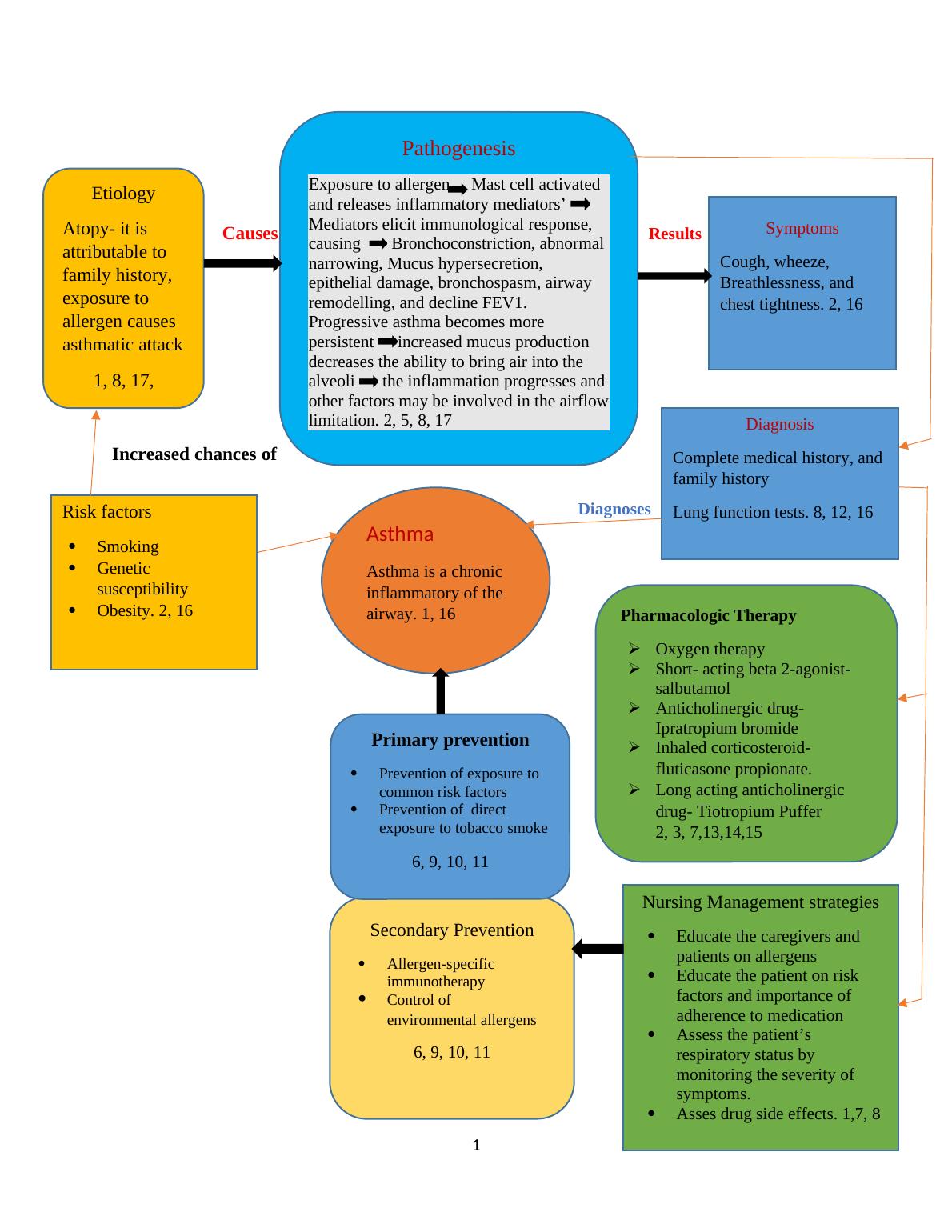
Causes Results
Caues
Increased chances of
Diagnoses
Control
1
Asthma
Asthma is a chronic
inflammatory of the
airway. 1, 16
Pathogenesis
Exposure to allergen Mast cell activated
and releases inflammatory mediators’
Mediators elicit immunological response,
causing Bronchoconstriction, abnormal
narrowing, Mucus hypersecretion,
epithelial damage, bronchospasm, airway
remodelling, and decline FEV1.
Progressive asthma becomes more
persistent increased mucus production
decreases the ability to bring air into the
alveoli the inflammation progresses and
other factors may be involved in the airflow
limitation. 2, 5, 8, 17
Symptoms
Cough, wheeze,
Breathlessness, and
chest tightness. 2, 16
Diagnosis
Complete medical history, and
family history
Lung function tests. 8, 12, 16
Pharmacologic Therapy
Oxygen therapy
Short- acting beta 2-agonist-
salbutamol
Anticholinergic drug-
Ipratropium bromide
Inhaled corticosteroid-
fluticasone propionate.
Long acting anticholinergic
drug- Tiotropium Puffer
2, 3, 7,13,14,15
Nursing Management strategies
Educate the caregivers and
patients on allergens
Educate the patient on risk
factors and importance of
adherence to medication
Assess the patient’s
respiratory status by
monitoring the severity of
symptoms.
Asses drug side effects. 1,7, 8
Secondary Prevention
Allergen-specific
immunotherapy
Control of
environmental allergens
6, 9, 10, 11
Primary prevention
Prevention of exposure to
common risk factors
Prevention of direct
exposure to tobacco smoke
6, 9, 10, 11
Etiology
Atopy- it is
attributable to
family history,
exposure to
allergen causes
asthmatic attack
1, 8, 17,
Risk factors
Smoking
Genetic
susceptibility
Obesity. 2, 16
Caues
Increased chances of
Diagnoses
Control
1
Asthma
Asthma is a chronic
inflammatory of the
airway. 1, 16
Pathogenesis
Exposure to allergen Mast cell activated
and releases inflammatory mediators’
Mediators elicit immunological response,
causing Bronchoconstriction, abnormal
narrowing, Mucus hypersecretion,
epithelial damage, bronchospasm, airway
remodelling, and decline FEV1.
Progressive asthma becomes more
persistent increased mucus production
decreases the ability to bring air into the
alveoli the inflammation progresses and
other factors may be involved in the airflow
limitation. 2, 5, 8, 17
Symptoms
Cough, wheeze,
Breathlessness, and
chest tightness. 2, 16
Diagnosis
Complete medical history, and
family history
Lung function tests. 8, 12, 16
Pharmacologic Therapy
Oxygen therapy
Short- acting beta 2-agonist-
salbutamol
Anticholinergic drug-
Ipratropium bromide
Inhaled corticosteroid-
fluticasone propionate.
Long acting anticholinergic
drug- Tiotropium Puffer
2, 3, 7,13,14,15
Nursing Management strategies
Educate the caregivers and
patients on allergens
Educate the patient on risk
factors and importance of
adherence to medication
Assess the patient’s
respiratory status by
monitoring the severity of
symptoms.
Asses drug side effects. 1,7, 8
Secondary Prevention
Allergen-specific
immunotherapy
Control of
environmental allergens
6, 9, 10, 11
Primary prevention
Prevention of exposure to
common risk factors
Prevention of direct
exposure to tobacco smoke
6, 9, 10, 11
Etiology
Atopy- it is
attributable to
family history,
exposure to
allergen causes
asthmatic attack
1, 8, 17,
Risk factors
Smoking
Genetic
susceptibility
Obesity. 2, 16
References
1. Aitken, L., & Chaboyer, W. (2016). ACCCN's Critical Care Nursing. Elsevier Health
Sciences.
2. Andrzejowski, P., & Carroll, W. (2016). Salbutamol in paediatrics: pharmacology,
prescribing and controversies. Archives of Disease in Childhood-Education and Practice,
101(4), 194-197.
3. Bullock, S., & Manias, E. (2013). Fundamentals of pharmacology. Pearson Higher
Education AU.
4. Cornforth, A. (2013). COPD self-management supportive care: chaos and complexity
theory. British Journal of Nursing, 22(19), 1101-1104
5. Craft, J., Gordon, C., Huether, S. E., McCance, K. L., & Brashers, V. L. (2015).
Understanding pathophysiology-ANZ adaptation. Elsevier Health Sciences.
6. Fleischer, D. M., Sicherer, S., Greenhawt, M., Campbell, D., Chan, E. S., Muraro, A., ...
& Sampson, H. (2015). Consensus communication on early peanut introduction and the
prevention of peanut allergy in high-risk infants. World Allergy Organization Journal,
8(1), 1.
7. Hazeldine, V. (2013). Pharmacological management of acute asthma exacerbations in
adults. Nursing Standard (through 2013), 27(33), 43.
8. Kaufman, G. (2011). Asthma: pathophysiology, diagnosis and management. Nursing
Standard, 26(5).
9. Morjaria, J. B., Caruso, M., Emma, R., Russo, C., & Polosa, R. (2018). Treatment of
allergic rhinitis as a strategy for preventing asthma. Current allergy and asthma reports,
18(4), 23.
10. Nieto, A., Wahn, U., Bufe, A., Eigenmann, P., Halken, S., Hedlin, G., ... & Lau, S.
(2014). Allergy and asthma prevention 2014. Pediatric Allergy and Immunology, 25(6),
516-533.
11. Prevention strategies for asthma-secondary prevention. (2005). CMAJ: Canadian Medical
Association Journal, 173(6 Suppl), S25–S27.
12. Sarver N, Murphy K (2009). Management of asthma. New approaches to establishing
control. Journal of The American Academy of Nurse Practitioners. 21, 1, 54-65.
2
1. Aitken, L., & Chaboyer, W. (2016). ACCCN's Critical Care Nursing. Elsevier Health
Sciences.
2. Andrzejowski, P., & Carroll, W. (2016). Salbutamol in paediatrics: pharmacology,
prescribing and controversies. Archives of Disease in Childhood-Education and Practice,
101(4), 194-197.
3. Bullock, S., & Manias, E. (2013). Fundamentals of pharmacology. Pearson Higher
Education AU.
4. Cornforth, A. (2013). COPD self-management supportive care: chaos and complexity
theory. British Journal of Nursing, 22(19), 1101-1104
5. Craft, J., Gordon, C., Huether, S. E., McCance, K. L., & Brashers, V. L. (2015).
Understanding pathophysiology-ANZ adaptation. Elsevier Health Sciences.
6. Fleischer, D. M., Sicherer, S., Greenhawt, M., Campbell, D., Chan, E. S., Muraro, A., ...
& Sampson, H. (2015). Consensus communication on early peanut introduction and the
prevention of peanut allergy in high-risk infants. World Allergy Organization Journal,
8(1), 1.
7. Hazeldine, V. (2013). Pharmacological management of acute asthma exacerbations in
adults. Nursing Standard (through 2013), 27(33), 43.
8. Kaufman, G. (2011). Asthma: pathophysiology, diagnosis and management. Nursing
Standard, 26(5).
9. Morjaria, J. B., Caruso, M., Emma, R., Russo, C., & Polosa, R. (2018). Treatment of
allergic rhinitis as a strategy for preventing asthma. Current allergy and asthma reports,
18(4), 23.
10. Nieto, A., Wahn, U., Bufe, A., Eigenmann, P., Halken, S., Hedlin, G., ... & Lau, S.
(2014). Allergy and asthma prevention 2014. Pediatric Allergy and Immunology, 25(6),
516-533.
11. Prevention strategies for asthma-secondary prevention. (2005). CMAJ: Canadian Medical
Association Journal, 173(6 Suppl), S25–S27.
12. Sarver N, Murphy K (2009). Management of asthma. New approaches to establishing
control. Journal of The American Academy of Nurse Practitioners. 21, 1, 54-65.
2
13. Sher, L., Yiu, G., Sakov, A., Liu, S., & Caracta, C. (2017). Treatment of Asthmatic
Patients with Fluticasone Propionate and Fluticasone Propionate/Salmeterol Multidose
Dry Powder Inhalers Compared with Placebo: Patient-Reported Outcomes and Quality of
Life. Journal of Allergy and Clinical Immunology, 139(2), AB97.
14. Sullivan, P. W., Ghushchyan, V. H., Globe, G., & Schatz, M. (2018). Oral corticosteroid
exposure and adverse effects in asthmatic patients. Journal of Allergy and Clinical
Immunology, 141(1), 110-
15. Thomas, V., Gefen, E., Gopalan, G., Mares, R., McDonald, R., Ming, S. W. Y., & Price,
D. B. (2017). Ipratropium/Salbutamol Comparator Versus Originator for Chronic
Obstructive Pulmonary Disease Exacerbations: USA Observational Cohort Study Using
the Clinformatics™ Health Claims Database. Pulmonary Therapy, 3(1), 187-205.
16. Vogelmeier, C. F., Criner, G. J., Martinez, F. J., Anzueto, A., Barnes, P. J., Bourbeau,
J., ... & Frith, P. (2017). Global strategy for the diagnosis, management, and prevention
of chronic obstructive lung disease 2017 report. GOLD executive summary. American
journal of respiratory and critical care medicine, 195(5), 557-582.
17. Whitsett, J. A., & Alenghat, T. (2015). Respiratory epithelial cells orchestrate pulmonary
innate immunity. Nature immunology, 16(1), 27.
3
Patients with Fluticasone Propionate and Fluticasone Propionate/Salmeterol Multidose
Dry Powder Inhalers Compared with Placebo: Patient-Reported Outcomes and Quality of
Life. Journal of Allergy and Clinical Immunology, 139(2), AB97.
14. Sullivan, P. W., Ghushchyan, V. H., Globe, G., & Schatz, M. (2018). Oral corticosteroid
exposure and adverse effects in asthmatic patients. Journal of Allergy and Clinical
Immunology, 141(1), 110-
15. Thomas, V., Gefen, E., Gopalan, G., Mares, R., McDonald, R., Ming, S. W. Y., & Price,
D. B. (2017). Ipratropium/Salbutamol Comparator Versus Originator for Chronic
Obstructive Pulmonary Disease Exacerbations: USA Observational Cohort Study Using
the Clinformatics™ Health Claims Database. Pulmonary Therapy, 3(1), 187-205.
16. Vogelmeier, C. F., Criner, G. J., Martinez, F. J., Anzueto, A., Barnes, P. J., Bourbeau,
J., ... & Frith, P. (2017). Global strategy for the diagnosis, management, and prevention
of chronic obstructive lung disease 2017 report. GOLD executive summary. American
journal of respiratory and critical care medicine, 195(5), 557-582.
17. Whitsett, J. A., & Alenghat, T. (2015). Respiratory epithelial cells orchestrate pulmonary
innate immunity. Nature immunology, 16(1), 27.
3
Answers to assignment 2
Pathogenesis of acute asthma
Mr. Jackson Smith diagnosis was confirmed by laboratory diagnosis including blood gas after he
presented with symptoms including breathlessness, severer dysponoea, and wheeze. At the same
time, his past medical history confirmed that he was diagnosed with asthma at the age of two
years. Acute severe asthmatic attack occurs when an individual is exposed to environmental
allergens such as smoke, dust, pollen grain among others. According to Kaufman (2012), during
acute severe asthmatic attack the normal functioning of the lower respiratory tract that include
the trachea, the bronchi, and the bronchioles is greatly affected. The constriction of bronchial and
the abnormal narrowing of the airways due to epithelial damage, mucus hypersecretion, and
bronchospasm have been mostly cited as the main cause of adverse symptoms experienced by
the asthmatic patient (Hamid, Mahboub, & Ramakrishnan, 2018). Acute asthmatic attack occurs
when an individual is exposed to an allergen that is capable of eliciting immunological reactions
leading to production of inflammatory mediators by mast cells among others. The result of the
immunological response is airways smooth muscles constriction, and hypersecretion of mucus
leading to narrowing and blockage of the airway. According to Whitsett and Alenghat (2015),
hypersensitivity induced by environmental allergen leading to bronchoconstriction and airway
inflammation can be attributed to IgE-dependent mediators that are released by the mast cells
including histamine and prostaglandins whose activities directly cause constriction to the airways
smooth muscles.
Wawrzyniak et al. (2017), suggested that whenever, smooth flow of air into the lung is
interrupted as a result of narrowing of the airways and bronchial wall inflammation there is an
increase in the decline of Forced Expiratory Volume in one second (FEV1) resulting to
4
Pathogenesis of acute asthma
Mr. Jackson Smith diagnosis was confirmed by laboratory diagnosis including blood gas after he
presented with symptoms including breathlessness, severer dysponoea, and wheeze. At the same
time, his past medical history confirmed that he was diagnosed with asthma at the age of two
years. Acute severe asthmatic attack occurs when an individual is exposed to environmental
allergens such as smoke, dust, pollen grain among others. According to Kaufman (2012), during
acute severe asthmatic attack the normal functioning of the lower respiratory tract that include
the trachea, the bronchi, and the bronchioles is greatly affected. The constriction of bronchial and
the abnormal narrowing of the airways due to epithelial damage, mucus hypersecretion, and
bronchospasm have been mostly cited as the main cause of adverse symptoms experienced by
the asthmatic patient (Hamid, Mahboub, & Ramakrishnan, 2018). Acute asthmatic attack occurs
when an individual is exposed to an allergen that is capable of eliciting immunological reactions
leading to production of inflammatory mediators by mast cells among others. The result of the
immunological response is airways smooth muscles constriction, and hypersecretion of mucus
leading to narrowing and blockage of the airway. According to Whitsett and Alenghat (2015),
hypersensitivity induced by environmental allergen leading to bronchoconstriction and airway
inflammation can be attributed to IgE-dependent mediators that are released by the mast cells
including histamine and prostaglandins whose activities directly cause constriction to the airways
smooth muscles.
Wawrzyniak et al. (2017), suggested that whenever, smooth flow of air into the lung is
interrupted as a result of narrowing of the airways and bronchial wall inflammation there is an
increase in the decline of Forced Expiratory Volume in one second (FEV1) resulting to
4
End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Pathogenesis and Treatment of Acute Severe Asthmalg...
|9
|3225
|337
Pathophysiology of Asthma: Bronchial Constriction, Inflammation, and Wheezinglg...
|7
|708
|51
Pharmacology and Pathophysiologylg...
|12
|3125
|20
Understanding Allergic Asthma: Pathophysiology, Treatment and Educationlg...
|7
|1690
|115
Acute Severe Asthma: Causes, Symptoms, Diagnosis, Treatmentlg...
|2
|589
|285
Asthma: Pathophysiology, Treatment and Educationlg...
|7
|1665
|323
