Acute Coronary Syndrome: A Case Study
VerifiedAdded on 2022/11/17
|17
|4648
|83
AI Summary
Read this case study on Acute Coronary Syndrome to understand its pathophysiology, pharmacology and psychological aspects. Learn about the drugs GTN, diltiazem and pravastatin and their mechanism of action. Also, know about the use of aspirin and ticagrelor in cardiac patients and the use of morphine in Acute Coronary Syndrome (ACS).
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: ACUTE CORONARY SYNDROME: A CASE STUDY
ACUTE CORONARY SYNDROME: A CASE STUDY
Name of the Student
Name of the University
Author’s Note
ACUTE CORONARY SYNDROME: A CASE STUDY
Name of the Student
Name of the University
Author’s Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1ACUTE CORONARY SYNDROME: A CASE STUDY
Table of Contents
Introduction................................................................................................................................2
1. Rationale for ECG request.....................................................................................................2
2a. Pathophysiology of angina...................................................................................................3
2b. Risk factors that increase the risk of Acute Coronary Syndrome........................................5
3. Interpretation of the ECG report............................................................................................5
4. Central findings leading to the diagnosis of Acute Coronary Syndrome...............................6
5. The table discussing the drugs GTN, diltiazem and pravastatin............................................6
6. Mechanism of action and use of aspirin and ticagrelor in cardiac patients............................8
7. The use of morphine in Acute Coronary Syndrome (ACS)...................................................8
8. Increased risk of depression with chronic illness...................................................................9
Conclusion................................................................................................................................10
References................................................................................................................................11
Table of Contents
Introduction................................................................................................................................2
1. Rationale for ECG request.....................................................................................................2
2a. Pathophysiology of angina...................................................................................................3
2b. Risk factors that increase the risk of Acute Coronary Syndrome........................................5
3. Interpretation of the ECG report............................................................................................5
4. Central findings leading to the diagnosis of Acute Coronary Syndrome...............................6
5. The table discussing the drugs GTN, diltiazem and pravastatin............................................6
6. Mechanism of action and use of aspirin and ticagrelor in cardiac patients............................8
7. The use of morphine in Acute Coronary Syndrome (ACS)...................................................8
8. Increased risk of depression with chronic illness...................................................................9
Conclusion................................................................................................................................10
References................................................................................................................................11
2ACUTE CORONARY SYNDROME: A CASE STUDY
Introduction
The case study involves a 72 year old woman named Betsy Blogger who is admitted
in the surgical ward had complaints of nausea and shortness of breath but denied chest pains.
She had an uneventful fixation of a right tibula and fibula fracture with no immediate
complications two days prior to her readmission. Her past medical history showed a
prevalence of coronary heart disease and chronic obstructive pulmonary disease (COPD)
along with hypertension and hyperglycemia due to type 2 diabetes and presently her blood
sugar level is 5.5. She has had three coronary artery bypass grafts over the last eight years.
She had a heart rate of 90 along with 145/85 blood pressure. Her skin looked pale and is
sweaty and has a temperature of 37°C. Her oxygen saturation level is 94% with a respiratory
rate of 26. The case study discusses the pathophysiology, pharmacology and psychological
aspects of the patient’s condition along with a thorough analysis of her ailments.
1. Rationale for ECG request
ECG was requested because she had a medical history of coronary heart disease and
has had three coronary artery bypass grafts over the last eight years. Betsy Blogger is also a
patient of COPD, suffering from type 2 diabetes and hypertension as well. Coronary heart
disease causes cardiac conditions by causing tachycardia and blockages which is further
elevated by hyperglycemic conditions, leading to angina and myocardial infarction (Tran et
al., 2018). She had an elevated heart rate of 90 along with 145/85 blood pressure which
required EGC monitoring to detect anomaly (Penzel et al., 2016). Her low oxygen saturation
level of 94% might be attributed to the low respiratory rate of 26 making the medical
condition even more severe. Due to the surgery two days back for her tibula fibula fracture,
Betsy is under pain medications such as endone, paracetamol, and so on which might be
Introduction
The case study involves a 72 year old woman named Betsy Blogger who is admitted
in the surgical ward had complaints of nausea and shortness of breath but denied chest pains.
She had an uneventful fixation of a right tibula and fibula fracture with no immediate
complications two days prior to her readmission. Her past medical history showed a
prevalence of coronary heart disease and chronic obstructive pulmonary disease (COPD)
along with hypertension and hyperglycemia due to type 2 diabetes and presently her blood
sugar level is 5.5. She has had three coronary artery bypass grafts over the last eight years.
She had a heart rate of 90 along with 145/85 blood pressure. Her skin looked pale and is
sweaty and has a temperature of 37°C. Her oxygen saturation level is 94% with a respiratory
rate of 26. The case study discusses the pathophysiology, pharmacology and psychological
aspects of the patient’s condition along with a thorough analysis of her ailments.
1. Rationale for ECG request
ECG was requested because she had a medical history of coronary heart disease and
has had three coronary artery bypass grafts over the last eight years. Betsy Blogger is also a
patient of COPD, suffering from type 2 diabetes and hypertension as well. Coronary heart
disease causes cardiac conditions by causing tachycardia and blockages which is further
elevated by hyperglycemic conditions, leading to angina and myocardial infarction (Tran et
al., 2018). She had an elevated heart rate of 90 along with 145/85 blood pressure which
required EGC monitoring to detect anomaly (Penzel et al., 2016). Her low oxygen saturation
level of 94% might be attributed to the low respiratory rate of 26 making the medical
condition even more severe. Due to the surgery two days back for her tibula fibula fracture,
Betsy is under pain medications such as endone, paracetamol, and so on which might be
3ACUTE CORONARY SYNDROME: A CASE STUDY
camouflaging her pain thereby leading to the denial of chest pains. Therefore, request for an
ECG is the correct rationale.
2a. Pathophysiology of angina
Angina pectoris or angina is a heart condition featured with chest pain due to
inadequate flow of blood to the muscle of the heart. It is caused by the obstruction of the
arteries which supplies blood to the heart muscles along with causes including abnormal heart
rhythms heart failure and anaemia (Pollack & Riese, 2019). Atherosclerosis, where the
insides of the arteries narrows down due to the plaque formation leading to the blockage and
insufficient blood supply to the heart muscles, is attributed as the main reason behind the
cause of angina (Verheye et al., 2015). Hyperglycemia, elevated lipid profiles are behind the
formation of such plaques leading to atherosclerosis (Tran et al., 2018). Although the disease
does not present with any notable symptoms at the early stages, however, as the disease
progresses the severity of the disease increases leading to stroke, pulmonary artery disease,
coronary artery disease and other heart complications (Marinescu et al., 2015).
Stable Angina
Stable Angina is related to myocardial ischemia, which involves the plaque formation
in the arteries of heart that creates an obstruction in the supply of blood to the heart muscle
and it is one of the most common type of cardiovascular diseases (Ohman, 2016). Plaque is
constituted of excess glucose, cholesterol, calcium, fat and other substances found in the
blood (Brown & Redberg, 2018). Since, the arteries get tapered and narrow, limiting the
blood flow to the heart causing angina. The plaque produced makes the muscle cells of the
blood vessels to stretch to compensate the additional bulk that eventually thickens the
endothelial lining thereby increasing the separation between the lumen and the plaque
(Verheye et al., 2015). This condition somewhat counterbalances the narrowing that is caused
camouflaging her pain thereby leading to the denial of chest pains. Therefore, request for an
ECG is the correct rationale.
2a. Pathophysiology of angina
Angina pectoris or angina is a heart condition featured with chest pain due to
inadequate flow of blood to the muscle of the heart. It is caused by the obstruction of the
arteries which supplies blood to the heart muscles along with causes including abnormal heart
rhythms heart failure and anaemia (Pollack & Riese, 2019). Atherosclerosis, where the
insides of the arteries narrows down due to the plaque formation leading to the blockage and
insufficient blood supply to the heart muscles, is attributed as the main reason behind the
cause of angina (Verheye et al., 2015). Hyperglycemia, elevated lipid profiles are behind the
formation of such plaques leading to atherosclerosis (Tran et al., 2018). Although the disease
does not present with any notable symptoms at the early stages, however, as the disease
progresses the severity of the disease increases leading to stroke, pulmonary artery disease,
coronary artery disease and other heart complications (Marinescu et al., 2015).
Stable Angina
Stable Angina is related to myocardial ischemia, which involves the plaque formation
in the arteries of heart that creates an obstruction in the supply of blood to the heart muscle
and it is one of the most common type of cardiovascular diseases (Ohman, 2016). Plaque is
constituted of excess glucose, cholesterol, calcium, fat and other substances found in the
blood (Brown & Redberg, 2018). Since, the arteries get tapered and narrow, limiting the
blood flow to the heart causing angina. The plaque produced makes the muscle cells of the
blood vessels to stretch to compensate the additional bulk that eventually thickens the
endothelial lining thereby increasing the separation between the lumen and the plaque
(Verheye et al., 2015). This condition somewhat counterbalances the narrowing that is caused
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4ACUTE CORONARY SYNDROME: A CASE STUDY
due to the growth of plaque, but the wall get stiffen and becomes less complaint to stretching
with each heartbeat (Ford, Corcoran & Berry, 2018). The symptoms of stable angina includes
chest discomfort and other related symptoms that are precipitated by activities like walking,
running or swimming and so on. However, symptoms typically subside several moments after
the activity and again reoccur when the activity is resumed (Tran et al., 2018).
Unstable Angina
Unstable angina is an acute heart condition and identified as clinically worsening
angina, which does not follow any pattern and is generally unpredictable, lasts longer and
aggravates leading to health deterioration (Sandoval, Apple & Smith, 2018). It results from
acute obstruction of a coronary artery without myocardial infarction. The symptoms are chest
discomfort with diaphoresis, dyspnea or nausea. Anomalous endothelial function causes
variations in the atrial tone leading to damage to the endothelium by the atheromas whose
stress instead of dilation which is the normal response causes vasoconstriction leading to
unstable angina (Pollack & Riese, 2019).
Non-STEMI
Non-ST-elevation myocardial infarction or Non-STEMI is referred to myocardial
infarction or a heart attack where the ST is in reference to the ST segment of the ECG
analytical test performed to diagnose a heart attack (Milosevic et al., 2016). It is generally
caused by partial but severely narrowed coronary artery blockage which leads to the
myocardial infarction.
STEMI
STEMI or ST-elevation myocardial infarction is referred to heart attack which is
caused by complete blockage of the coronary artery of the heart leading to the sudden onset
due to the growth of plaque, but the wall get stiffen and becomes less complaint to stretching
with each heartbeat (Ford, Corcoran & Berry, 2018). The symptoms of stable angina includes
chest discomfort and other related symptoms that are precipitated by activities like walking,
running or swimming and so on. However, symptoms typically subside several moments after
the activity and again reoccur when the activity is resumed (Tran et al., 2018).
Unstable Angina
Unstable angina is an acute heart condition and identified as clinically worsening
angina, which does not follow any pattern and is generally unpredictable, lasts longer and
aggravates leading to health deterioration (Sandoval, Apple & Smith, 2018). It results from
acute obstruction of a coronary artery without myocardial infarction. The symptoms are chest
discomfort with diaphoresis, dyspnea or nausea. Anomalous endothelial function causes
variations in the atrial tone leading to damage to the endothelium by the atheromas whose
stress instead of dilation which is the normal response causes vasoconstriction leading to
unstable angina (Pollack & Riese, 2019).
Non-STEMI
Non-ST-elevation myocardial infarction or Non-STEMI is referred to myocardial
infarction or a heart attack where the ST is in reference to the ST segment of the ECG
analytical test performed to diagnose a heart attack (Milosevic et al., 2016). It is generally
caused by partial but severely narrowed coronary artery blockage which leads to the
myocardial infarction.
STEMI
STEMI or ST-elevation myocardial infarction is referred to heart attack which is
caused by complete blockage of the coronary artery of the heart leading to the sudden onset
5ACUTE CORONARY SYNDROME: A CASE STUDY
of myocardial infarction. The ECG pattern of STEMI showed elevated ST peaks indicative of
major heart failure (Yellon et al., 2015).
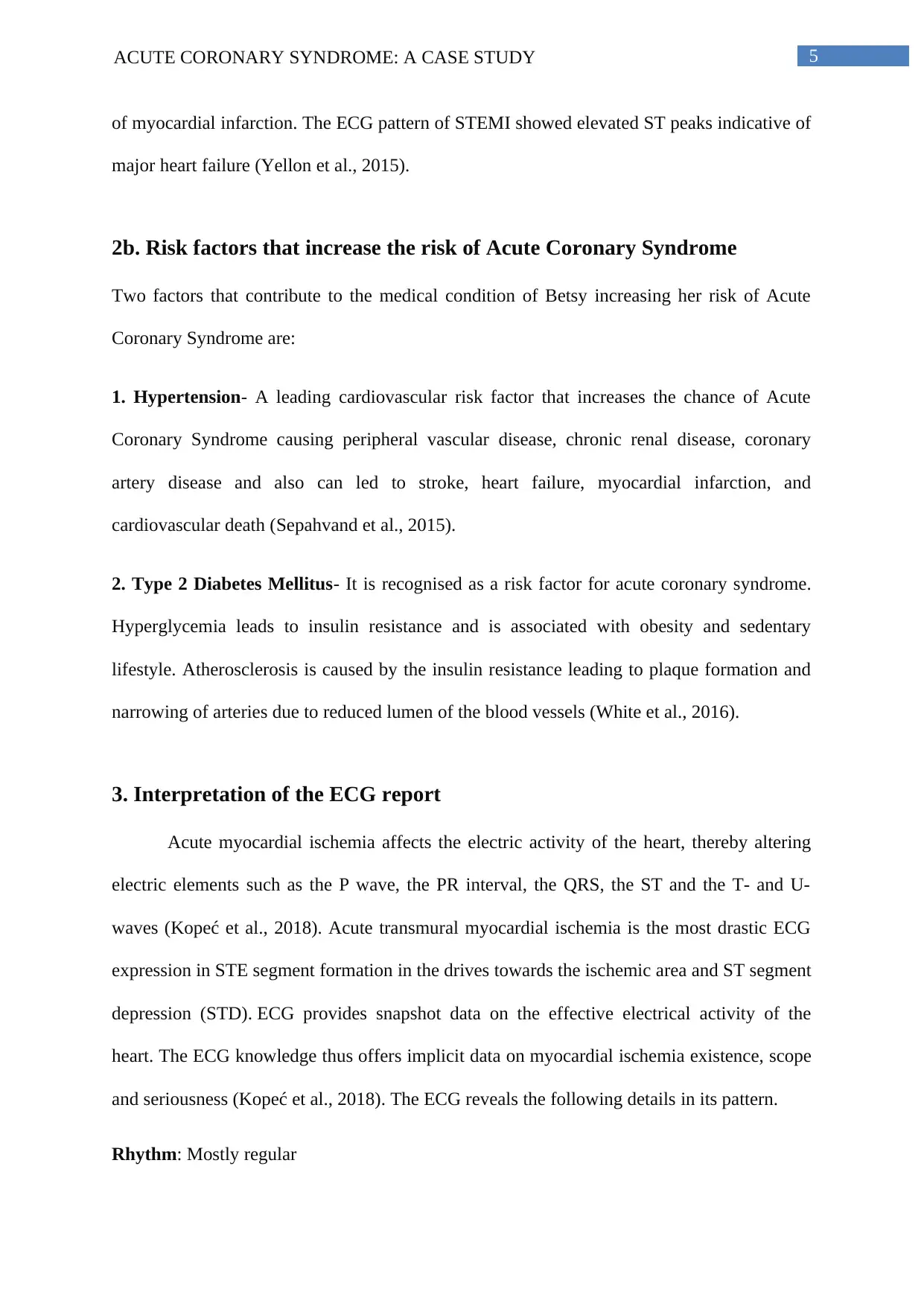
2b. Risk factors that increase the risk of Acute Coronary Syndrome
Two factors that contribute to the medical condition of Betsy increasing her risk of Acute
Coronary Syndrome are:
1. Hypertension- A leading cardiovascular risk factor that increases the chance of Acute
Coronary Syndrome causing peripheral vascular disease, chronic renal disease, coronary
artery disease and also can led to stroke, heart failure, myocardial infarction, and
cardiovascular death (Sepahvand et al., 2015).
2. Type 2 Diabetes Mellitus- It is recognised as a risk factor for acute coronary syndrome.
Hyperglycemia leads to insulin resistance and is associated with obesity and sedentary
lifestyle. Atherosclerosis is caused by the insulin resistance leading to plaque formation and
narrowing of arteries due to reduced lumen of the blood vessels (White et al., 2016).
3. Interpretation of the ECG report
Acute myocardial ischemia affects the electric activity of the heart, thereby altering
electric elements such as the P wave, the PR interval, the QRS, the ST and the T- and U-
waves (Kopeć et al., 2018). Acute transmural myocardial ischemia is the most drastic ECG
expression in STE segment formation in the drives towards the ischemic area and ST segment
depression (STD). ECG provides snapshot data on the effective electrical activity of the
heart. The ECG knowledge thus offers implicit data on myocardial ischemia existence, scope
and seriousness (Kopeć et al., 2018). The ECG reveals the following details in its pattern.
Rhythm: Mostly regular
of myocardial infarction. The ECG pattern of STEMI showed elevated ST peaks indicative of
major heart failure (Yellon et al., 2015).
2b. Risk factors that increase the risk of Acute Coronary Syndrome
Two factors that contribute to the medical condition of Betsy increasing her risk of Acute
Coronary Syndrome are:
1. Hypertension- A leading cardiovascular risk factor that increases the chance of Acute
Coronary Syndrome causing peripheral vascular disease, chronic renal disease, coronary
artery disease and also can led to stroke, heart failure, myocardial infarction, and
cardiovascular death (Sepahvand et al., 2015).
2. Type 2 Diabetes Mellitus- It is recognised as a risk factor for acute coronary syndrome.
Hyperglycemia leads to insulin resistance and is associated with obesity and sedentary
lifestyle. Atherosclerosis is caused by the insulin resistance leading to plaque formation and
narrowing of arteries due to reduced lumen of the blood vessels (White et al., 2016).
3. Interpretation of the ECG report
Acute myocardial ischemia affects the electric activity of the heart, thereby altering
electric elements such as the P wave, the PR interval, the QRS, the ST and the T- and U-
waves (Kopeć et al., 2018). Acute transmural myocardial ischemia is the most drastic ECG
expression in STE segment formation in the drives towards the ischemic area and ST segment
depression (STD). ECG provides snapshot data on the effective electrical activity of the
heart. The ECG knowledge thus offers implicit data on myocardial ischemia existence, scope
and seriousness (Kopeć et al., 2018). The ECG reveals the following details in its pattern.
Rhythm: Mostly regular
6ACUTE CORONARY SYNDROME: A CASE STUDY
Rate: 90, regular
Presence and regularity of p-waves: In the first strip P wave is prominent. However, in
other ECG strip, P wave is irregular.
ST segment: Elevated ST segments
4. Central findings leading to the diagnosis of Acute Coronary Syndrome
Acute coronary syndromes is characterised by chest pain however due to the surgery
two days back for the tibula fibula fracture, Betsy is under pain medications such as endone,
paracetamol which might be camouflaging her pain thereby leading to the denial of chest
pains. She has a medical history of coronary heart disease and has had three coronary artery
bypass grafts over the last eight years. Betsy Blogger had complaints of nausea and shortness
of breath with an elevated heart rate of 90 along with 145/85 blood pressure which required
EGC monitoring to detect anomaly (Penzel et al., 2016). She is also a patient of COPD which
elevates her chances of developing acute coronary syndrome (Rothnie et al., 2016). She is
also a hyperglycemic, suffering from type 2 diabetes and hypertension as well (Tran et al.,
2018). Coronary heart disease causes cardiac conditions by causing tachycardia and
blockages which is further elevated by hyperglycemic conditions, leading to angina and
myocardial infarction (Tran et al., 2018).
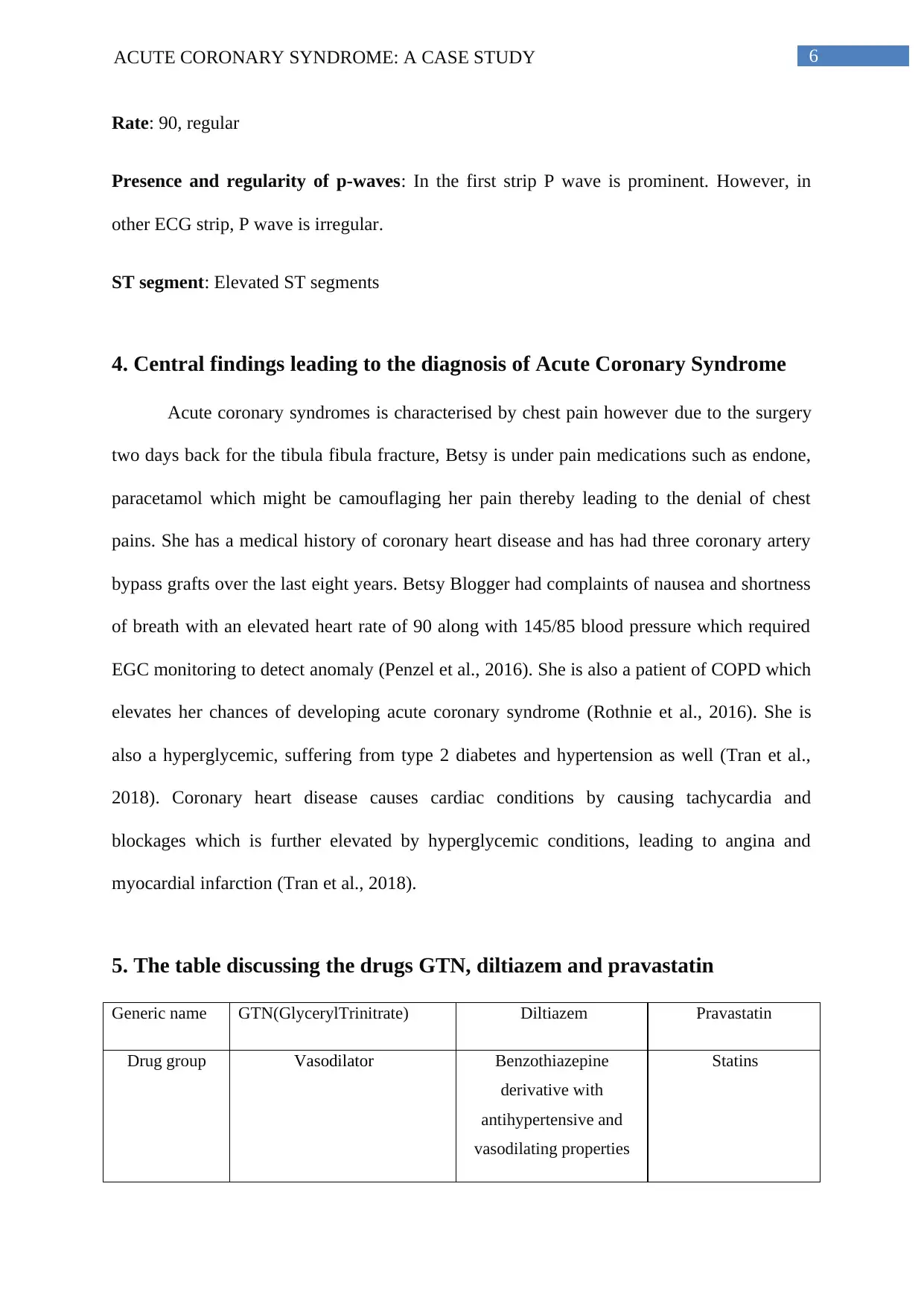
5. The table discussing the drugs GTN, diltiazem and pravastatin
Generic name GTN(GlycerylTrinitrate) Diltiazem Pravastatin
Drug group Vasodilator Benzothiazepine
derivative with
antihypertensive and
vasodilating properties
Statins
Rate: 90, regular
Presence and regularity of p-waves: In the first strip P wave is prominent. However, in
other ECG strip, P wave is irregular.
ST segment: Elevated ST segments
4. Central findings leading to the diagnosis of Acute Coronary Syndrome
Acute coronary syndromes is characterised by chest pain however due to the surgery
two days back for the tibula fibula fracture, Betsy is under pain medications such as endone,
paracetamol which might be camouflaging her pain thereby leading to the denial of chest
pains. She has a medical history of coronary heart disease and has had three coronary artery
bypass grafts over the last eight years. Betsy Blogger had complaints of nausea and shortness
of breath with an elevated heart rate of 90 along with 145/85 blood pressure which required
EGC monitoring to detect anomaly (Penzel et al., 2016). She is also a patient of COPD which
elevates her chances of developing acute coronary syndrome (Rothnie et al., 2016). She is
also a hyperglycemic, suffering from type 2 diabetes and hypertension as well (Tran et al.,
2018). Coronary heart disease causes cardiac conditions by causing tachycardia and
blockages which is further elevated by hyperglycemic conditions, leading to angina and
myocardial infarction (Tran et al., 2018).
5. The table discussing the drugs GTN, diltiazem and pravastatin
Generic name GTN(GlycerylTrinitrate) Diltiazem Pravastatin
Drug group Vasodilator Benzothiazepine
derivative with
antihypertensive and
vasodilating properties
Statins
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
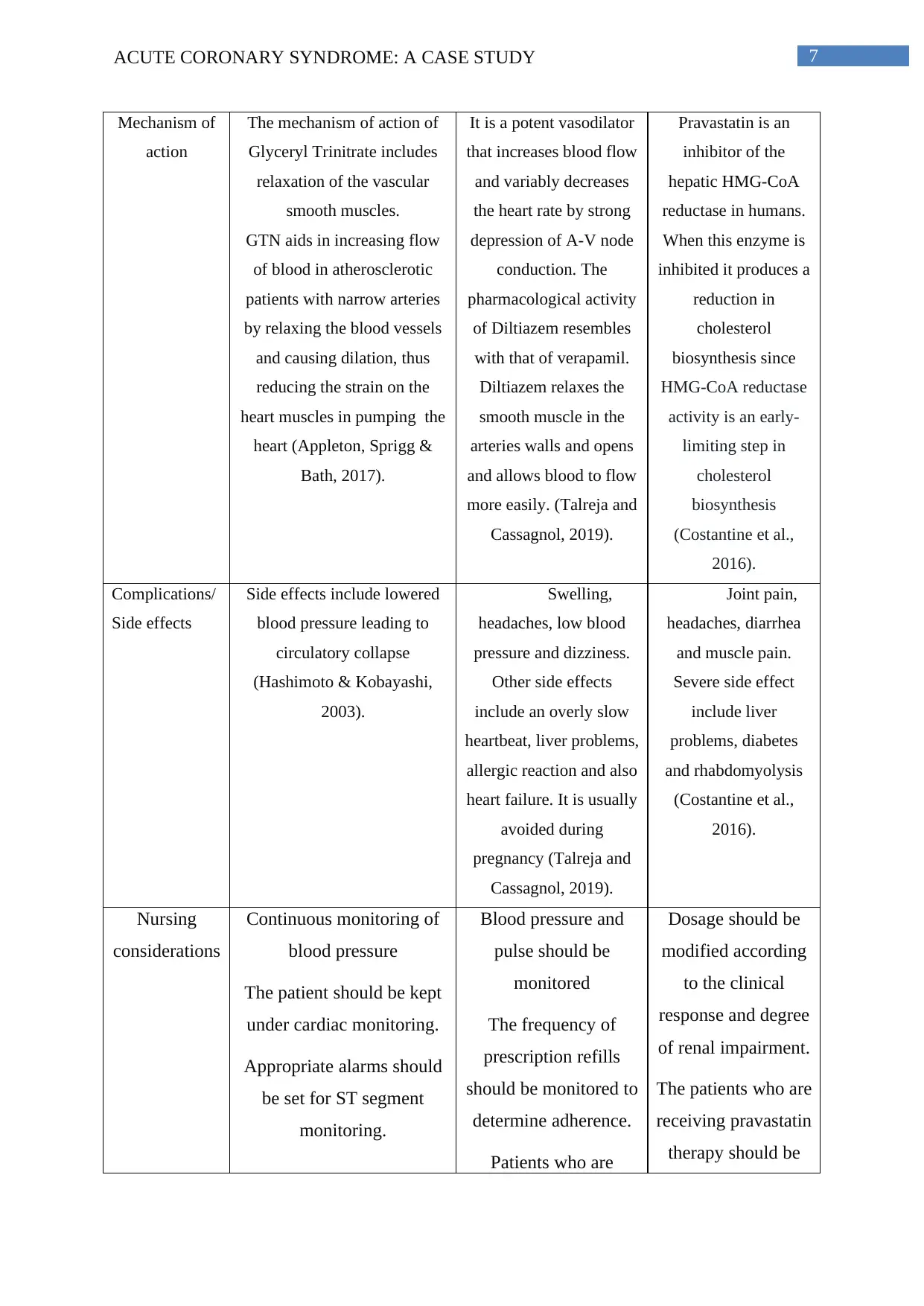
7ACUTE CORONARY SYNDROME: A CASE STUDY
Mechanism of
action
The mechanism of action of
Glyceryl Trinitrate includes
relaxation of the vascular
smooth muscles.
GTN aids in increasing flow
of blood in atherosclerotic
patients with narrow arteries
by relaxing the blood vessels
and causing dilation, thus
reducing the strain on the
heart muscles in pumping the
heart (Appleton, Sprigg &
Bath, 2017).
It is a potent vasodilator
that increases blood flow
and variably decreases
the heart rate by strong
depression of A-V node
conduction. The
pharmacological activity
of Diltiazem resembles
with that of verapamil.
Diltiazem relaxes the
smooth muscle in the
arteries walls and opens
and allows blood to flow
more easily. (Talreja and
Cassagnol, 2019).
Pravastatin is an
inhibitor of the
hepatic HMG-CoA
reductase in humans.
When this enzyme is
inhibited it produces a
reduction in
cholesterol
biosynthesis since
HMG-CoA reductase
activity is an early-
limiting step in
cholesterol
biosynthesis
(Costantine et al.,
2016).
Complications/
Side effects
Side effects include lowered
blood pressure leading to
circulatory collapse
(Hashimoto & Kobayashi,
2003).
Swelling,
headaches, low blood
pressure and dizziness.
Other side effects
include an overly slow
heartbeat, liver problems,
allergic reaction and also
heart failure. It is usually
avoided during
pregnancy (Talreja and
Cassagnol, 2019).
Joint pain,
headaches, diarrhea
and muscle pain.
Severe side effect
include liver
problems, diabetes
and rhabdomyolysis
(Costantine et al.,
2016).
Nursing
considerations
Continuous monitoring of
blood pressure
The patient should be kept
under cardiac monitoring.
Appropriate alarms should
be set for ST segment
monitoring.
Blood pressure and
pulse should be
monitored
The frequency of
prescription refills
should be monitored to
determine adherence.
Patients who are
Dosage should be
modified according
to the clinical
response and degree
of renal impairment.
The patients who are
receiving pravastatin
therapy should be
Mechanism of
action
The mechanism of action of
Glyceryl Trinitrate includes
relaxation of the vascular
smooth muscles.
GTN aids in increasing flow
of blood in atherosclerotic
patients with narrow arteries
by relaxing the blood vessels
and causing dilation, thus
reducing the strain on the
heart muscles in pumping the
heart (Appleton, Sprigg &
Bath, 2017).
It is a potent vasodilator
that increases blood flow
and variably decreases
the heart rate by strong
depression of A-V node
conduction. The
pharmacological activity
of Diltiazem resembles
with that of verapamil.
Diltiazem relaxes the
smooth muscle in the
arteries walls and opens
and allows blood to flow
more easily. (Talreja and
Cassagnol, 2019).
Pravastatin is an
inhibitor of the
hepatic HMG-CoA
reductase in humans.
When this enzyme is
inhibited it produces a
reduction in
cholesterol
biosynthesis since
HMG-CoA reductase
activity is an early-
limiting step in
cholesterol
biosynthesis
(Costantine et al.,
2016).
Complications/
Side effects
Side effects include lowered
blood pressure leading to
circulatory collapse
(Hashimoto & Kobayashi,
2003).
Swelling,
headaches, low blood
pressure and dizziness.
Other side effects
include an overly slow
heartbeat, liver problems,
allergic reaction and also
heart failure. It is usually
avoided during
pregnancy (Talreja and
Cassagnol, 2019).
Joint pain,
headaches, diarrhea
and muscle pain.
Severe side effect
include liver
problems, diabetes
and rhabdomyolysis
(Costantine et al.,
2016).
Nursing
considerations
Continuous monitoring of
blood pressure
The patient should be kept
under cardiac monitoring.
Appropriate alarms should
be set for ST segment
monitoring.
Blood pressure and
pulse should be
monitored
The frequency of
prescription refills
should be monitored to
determine adherence.
Patients who are
Dosage should be
modified according
to the clinical
response and degree
of renal impairment.
The patients who are
receiving pravastatin
therapy should be
8ACUTE CORONARY SYNDROME: A CASE STUDY
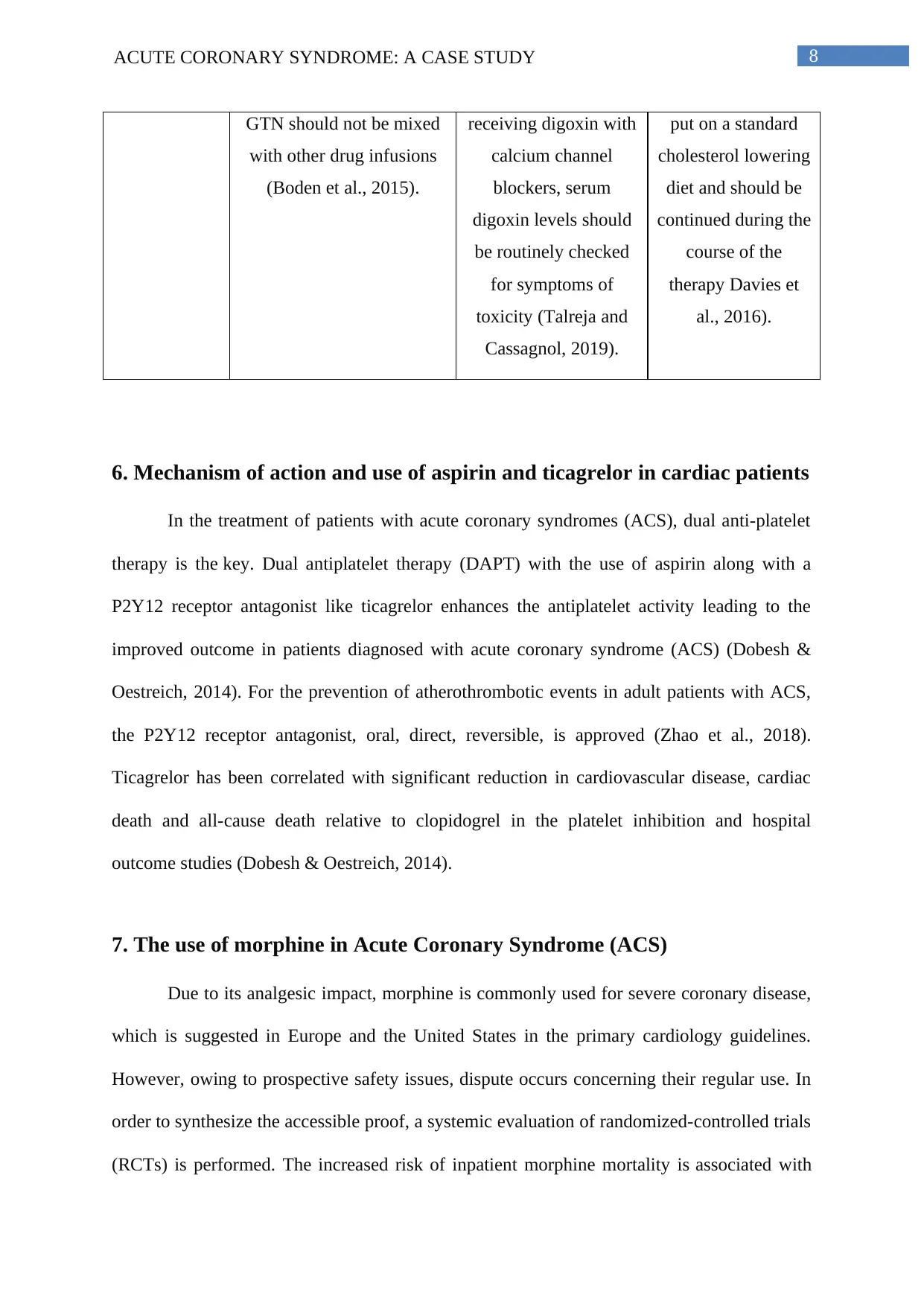
GTN should not be mixed
with other drug infusions
(Boden et al., 2015).
receiving digoxin with
calcium channel
blockers, serum
digoxin levels should
be routinely checked
for symptoms of
toxicity (Talreja and
Cassagnol, 2019).
put on a standard
cholesterol lowering
diet and should be
continued during the
course of the
therapy Davies et
al., 2016).
6. Mechanism of action and use of aspirin and ticagrelor in cardiac patients
In the treatment of patients with acute coronary syndromes (ACS), dual anti-platelet
therapy is the key. Dual antiplatelet therapy (DAPT) with the use of aspirin along with a
P2Y12 receptor antagonist like ticagrelor enhances the antiplatelet activity leading to the
improved outcome in patients diagnosed with acute coronary syndrome (ACS) (Dobesh &
Oestreich, 2014). For the prevention of atherothrombotic events in adult patients with ACS,
the P2Y12 receptor antagonist, oral, direct, reversible, is approved (Zhao et al., 2018).
Ticagrelor has been correlated with significant reduction in cardiovascular disease, cardiac
death and all-cause death relative to clopidogrel in the platelet inhibition and hospital
outcome studies (Dobesh & Oestreich, 2014).
7. The use of morphine in Acute Coronary Syndrome (ACS)
Due to its analgesic impact, morphine is commonly used for severe coronary disease,
which is suggested in Europe and the United States in the primary cardiology guidelines.
However, owing to prospective safety issues, dispute occurs concerning their regular use. In
order to synthesize the accessible proof, a systemic evaluation of randomized-controlled trials
(RCTs) is performed. The increased risk of inpatient morphine mortality is associated with
GTN should not be mixed
with other drug infusions
(Boden et al., 2015).
receiving digoxin with
calcium channel
blockers, serum
digoxin levels should
be routinely checked
for symptoms of
toxicity (Talreja and
Cassagnol, 2019).
put on a standard
cholesterol lowering
diet and should be
continued during the
course of the
therapy Davies et
al., 2016).
6. Mechanism of action and use of aspirin and ticagrelor in cardiac patients
In the treatment of patients with acute coronary syndromes (ACS), dual anti-platelet
therapy is the key. Dual antiplatelet therapy (DAPT) with the use of aspirin along with a
P2Y12 receptor antagonist like ticagrelor enhances the antiplatelet activity leading to the
improved outcome in patients diagnosed with acute coronary syndrome (ACS) (Dobesh &
Oestreich, 2014). For the prevention of atherothrombotic events in adult patients with ACS,
the P2Y12 receptor antagonist, oral, direct, reversible, is approved (Zhao et al., 2018).
Ticagrelor has been correlated with significant reduction in cardiovascular disease, cardiac
death and all-cause death relative to clopidogrel in the platelet inhibition and hospital
outcome studies (Dobesh & Oestreich, 2014).
7. The use of morphine in Acute Coronary Syndrome (ACS)
Due to its analgesic impact, morphine is commonly used for severe coronary disease,
which is suggested in Europe and the United States in the primary cardiology guidelines.
However, owing to prospective safety issues, dispute occurs concerning their regular use. In
order to synthesize the accessible proof, a systemic evaluation of randomized-controlled trials
(RCTs) is performed. The increased risk of inpatient morphine mortality is associated with
9ACUTE CORONARY SYNDROME: A CASE STUDY
morphines and the antiplatelet effect of P 2Y12 inhibitors is reduced during the first hour of
ACS and the bias risk associated with this measure is considered to be low (Kubica et al.,
2016). The triggering of opioid receptor in the myentereic plexus reduces gut motility and
secretion, inhibiting drug activity which is targeted to the P2Y12 protein, and reduces its
absorption and bioavailability. In addition, the effects on opioid receptors in myentereic
plexus reduce the motility and secretion of the intestines. Morphine is furthermore renowned
for its prometic and antiperistaltic impacts that can further reduce antiplatelet intake (Kubica
et al., 2016). Morphine is also associated with increased risk in mortality and morphine
decreases the antiplatelet effect of P2Y12 inhibitors such as ticagrelor which might be used in
patients with acute coronary syndrome as a treatment (Duarte et al., 2019).
8. Increased risk of depression with chronic illness
Depression is a crucial negative prognostic indicator for many important chronic
diseases, including heart disease, stroke, cancer and diabetes and the rate of diagnosis of
depression is increasing (Lagraauw, Kuiper & Bot, 2015). Depressions and chronic disorders
have a bi-directional liaison and progression of chronic disorders have severe impact on the
emotional and psychological well being of the individual (Voinov, Richie & Bailey, 2013).
In the post-myocardial patient, 23% suffer from major depressive disorders and 35%–45%
from other chronic symptoms. Morbidity and death in patients with cardiac illness and
anxiety are considerably greater than in patients with non-depressed cardiac illness (NIMH,
2019). The risk factor for mortality coincides with other severe threat variables, like
myocardial infarction or right ventricular dysfunction. Depression also increases disability
and the use of medical aid in people with coronary artery disease, which leads to a
considerable economic and medical public health strain (Voinov, Richie & Bailey, 2013).
morphines and the antiplatelet effect of P 2Y12 inhibitors is reduced during the first hour of
ACS and the bias risk associated with this measure is considered to be low (Kubica et al.,
2016). The triggering of opioid receptor in the myentereic plexus reduces gut motility and
secretion, inhibiting drug activity which is targeted to the P2Y12 protein, and reduces its
absorption and bioavailability. In addition, the effects on opioid receptors in myentereic
plexus reduce the motility and secretion of the intestines. Morphine is furthermore renowned
for its prometic and antiperistaltic impacts that can further reduce antiplatelet intake (Kubica
et al., 2016). Morphine is also associated with increased risk in mortality and morphine
decreases the antiplatelet effect of P2Y12 inhibitors such as ticagrelor which might be used in
patients with acute coronary syndrome as a treatment (Duarte et al., 2019).
8. Increased risk of depression with chronic illness
Depression is a crucial negative prognostic indicator for many important chronic
diseases, including heart disease, stroke, cancer and diabetes and the rate of diagnosis of
depression is increasing (Lagraauw, Kuiper & Bot, 2015). Depressions and chronic disorders
have a bi-directional liaison and progression of chronic disorders have severe impact on the
emotional and psychological well being of the individual (Voinov, Richie & Bailey, 2013).
In the post-myocardial patient, 23% suffer from major depressive disorders and 35%–45%
from other chronic symptoms. Morbidity and death in patients with cardiac illness and
anxiety are considerably greater than in patients with non-depressed cardiac illness (NIMH,
2019). The risk factor for mortality coincides with other severe threat variables, like
myocardial infarction or right ventricular dysfunction. Depression also increases disability
and the use of medical aid in people with coronary artery disease, which leads to a
considerable economic and medical public health strain (Voinov, Richie & Bailey, 2013).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10ACUTE CORONARY SYNDROME: A CASE STUDY
Conclusion
To summarize, the patient, 72 years old Betsy Blogger admitted in the surgical ward
had an uncomplicated fixation of right tibula and fibula fracture but two days following the
surgery, she complained of nausea and shortness of breath along with heart rate of 90, blood
pressure of 145/85 and 94% O2 saturation. She had a past medical history of coronary heart
disease, chronic obstructive pulmonary disease, three coronary artery bypass Graft over the
last eight years, hypertension and type 2 diabetes mellitus. The ECG revealed STEMI with
elevated ST waves which suggested total blockage of the coronary artery leading to the heart
attack. Lack of chest pain can be attributed to the camouflage of pain by the pain medications
prescribed to her post surgery for pain management. Therefore, it can be concluded that
hyperglycemia, hypertension along with chronic obstructive pulmonary disease might be the
reason contributing to the detrimental status of her heart leading to acute coronary syndrome.
Conclusion
To summarize, the patient, 72 years old Betsy Blogger admitted in the surgical ward
had an uncomplicated fixation of right tibula and fibula fracture but two days following the
surgery, she complained of nausea and shortness of breath along with heart rate of 90, blood
pressure of 145/85 and 94% O2 saturation. She had a past medical history of coronary heart
disease, chronic obstructive pulmonary disease, three coronary artery bypass Graft over the
last eight years, hypertension and type 2 diabetes mellitus. The ECG revealed STEMI with
elevated ST waves which suggested total blockage of the coronary artery leading to the heart
attack. Lack of chest pain can be attributed to the camouflage of pain by the pain medications
prescribed to her post surgery for pain management. Therefore, it can be concluded that
hyperglycemia, hypertension along with chronic obstructive pulmonary disease might be the
reason contributing to the detrimental status of her heart leading to acute coronary syndrome.
11ACUTE CORONARY SYNDROME: A CASE STUDY
References
Appleton, J. P., Sprigg, N., & Bath, P. M. (2017). Therapeutic potential of transdermal
glyceryl trinitrate in the management of acute stroke. CNS drugs, 31(1), 1-9.
Boden, W. E., Padala, S. K., Cabral, K. P., Buschmann, I. R., & Sidhu, M. S. (2015). Role of
short-acting nitroglycerin in the management of ischemic heart disease. Drug design,
development and therapy, 9, 4793.
Brown, D. L., & Redberg, R. F. (2018). Last nail in the coffin for PCI in stable angina?. The
Lancet, 391(10115), 3-4.
Cohen, B. E., Edmondson, D., &Kronish, I. M. (2015). State of the art review: depression,
stress, anxiety, and cardiovascular disease. American journal of hypertension, 28(11),
1295-1302.
Costantine, M., Cleary, K., Hebert, M., Ahmed, M., Brown, L., Ren, Z., Easterling, T., Haas,
D., Haneline, L., Caritis, S., Venkataramanan, R., West, H., D’Alton, M. and
Hankins, G. (2016). Safety and pharmacokinetics of pravastatin used for the
prevention of preeclampsia in high-risk pregnant women: a pilot randomized
controlled trial. American Journal of Obstetrics and Gynecology, 214(6), pp.720.e1-
720.e17.
Davies, J. T., Delfino, S. F., Feinberg, C. E., Johnson, M. F., Nappi, V. L., Olinger, J. T., ...
& Swanson, H. I. (2016). Current and emerging uses of statins in clinical therapeutics:
a review. Lipid insights, 9, LPI-S37450.
References
Appleton, J. P., Sprigg, N., & Bath, P. M. (2017). Therapeutic potential of transdermal
glyceryl trinitrate in the management of acute stroke. CNS drugs, 31(1), 1-9.
Boden, W. E., Padala, S. K., Cabral, K. P., Buschmann, I. R., & Sidhu, M. S. (2015). Role of
short-acting nitroglycerin in the management of ischemic heart disease. Drug design,
development and therapy, 9, 4793.
Brown, D. L., & Redberg, R. F. (2018). Last nail in the coffin for PCI in stable angina?. The
Lancet, 391(10115), 3-4.
Cohen, B. E., Edmondson, D., &Kronish, I. M. (2015). State of the art review: depression,
stress, anxiety, and cardiovascular disease. American journal of hypertension, 28(11),
1295-1302.
Costantine, M., Cleary, K., Hebert, M., Ahmed, M., Brown, L., Ren, Z., Easterling, T., Haas,
D., Haneline, L., Caritis, S., Venkataramanan, R., West, H., D’Alton, M. and
Hankins, G. (2016). Safety and pharmacokinetics of pravastatin used for the
prevention of preeclampsia in high-risk pregnant women: a pilot randomized
controlled trial. American Journal of Obstetrics and Gynecology, 214(6), pp.720.e1-
720.e17.
Davies, J. T., Delfino, S. F., Feinberg, C. E., Johnson, M. F., Nappi, V. L., Olinger, J. T., ...
& Swanson, H. I. (2016). Current and emerging uses of statins in clinical therapeutics:
a review. Lipid insights, 9, LPI-S37450.
12ACUTE CORONARY SYNDROME: A CASE STUDY
Dobesh, P., &Oestreich, J. (2014). Ticagrelor: Pharmacokinetics, Pharmacodynamics,
Clinical Efficacy, and Safety. Pharmacotherapy: The Journal of Human
Pharmacology and Drug Therapy, 34(10), 1077-1090. doi:10.1002/phar.1477
Duarte, G. S., Nunes-Ferreira, A., Rodrigues, F. B., Pinto, F. J., Ferreira, J. J., Costa, J., &
Caldeira, D. (2019). Morphine in acute coronary syndrome: systematic review and
meta-analysis. BMJ open, 9(3), e025232.
EPSTEIN, S. E., Redwood, D. R., Goldstein, R. E., Beiser, G. D., Rosing, D. R., Glancy, D.
L., ... & Stinson, E. B. (1971). Angina pectoris: pathophysiology, evaluation, and
treatment. Annals of Internal Medicine, 75(2), 263-296.
Ford, T. J., Corcoran, D., & Berry, C. (2018). Stable coronary syndromes: pathophysiology,
diagnostic advances and therapeutic need. Heart, 104(4), 284-292.
Franchi, F., &Angiolillo, D. J. (2015). Novel antiplatelet agents in acute coronary syndrome.
Nature Reviews Cardiology, 12(1), 30.
Gorlin, R. (1965). Pathophysiology of cardiac pain. Circulation, 32(1), 138-148.
Hashimoto, S., & Kobayashi, A. (2003). Clinical pharmacokinetics and pharmacodynamics
of glyceryl trinitrate and its metabolites. Clinical pharmacokinetics, 42(3), 205-221.
Kaski, J. C. (2016). Stable Angina Pectoris: Definition, Clinical Presentation and
Pathophysiologic Mechanisms. In Essentials in Stable Angina Pectoris (pp. 15-35).
Springer, Cham.
Koh, K. K., Lim, S., Choi, H., Lee, Y., Han, S. H., Lee, K., ... & Quon, M. J. (2013).
Combination pravastatin and valsartan treatment has additive beneficial effects to
simultaneously improve both metabolic and cardiovascular phenotypes beyond that of
Dobesh, P., &Oestreich, J. (2014). Ticagrelor: Pharmacokinetics, Pharmacodynamics,
Clinical Efficacy, and Safety. Pharmacotherapy: The Journal of Human
Pharmacology and Drug Therapy, 34(10), 1077-1090. doi:10.1002/phar.1477
Duarte, G. S., Nunes-Ferreira, A., Rodrigues, F. B., Pinto, F. J., Ferreira, J. J., Costa, J., &
Caldeira, D. (2019). Morphine in acute coronary syndrome: systematic review and
meta-analysis. BMJ open, 9(3), e025232.
EPSTEIN, S. E., Redwood, D. R., Goldstein, R. E., Beiser, G. D., Rosing, D. R., Glancy, D.
L., ... & Stinson, E. B. (1971). Angina pectoris: pathophysiology, evaluation, and
treatment. Annals of Internal Medicine, 75(2), 263-296.
Ford, T. J., Corcoran, D., & Berry, C. (2018). Stable coronary syndromes: pathophysiology,
diagnostic advances and therapeutic need. Heart, 104(4), 284-292.
Franchi, F., &Angiolillo, D. J. (2015). Novel antiplatelet agents in acute coronary syndrome.
Nature Reviews Cardiology, 12(1), 30.
Gorlin, R. (1965). Pathophysiology of cardiac pain. Circulation, 32(1), 138-148.
Hashimoto, S., & Kobayashi, A. (2003). Clinical pharmacokinetics and pharmacodynamics
of glyceryl trinitrate and its metabolites. Clinical pharmacokinetics, 42(3), 205-221.
Kaski, J. C. (2016). Stable Angina Pectoris: Definition, Clinical Presentation and
Pathophysiologic Mechanisms. In Essentials in Stable Angina Pectoris (pp. 15-35).
Springer, Cham.
Koh, K. K., Lim, S., Choi, H., Lee, Y., Han, S. H., Lee, K., ... & Quon, M. J. (2013).
Combination pravastatin and valsartan treatment has additive beneficial effects to
simultaneously improve both metabolic and cardiovascular phenotypes beyond that of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13ACUTE CORONARY SYNDROME: A CASE STUDY
monotherapy with either drug in patients with primary hypercholesterolemia.
Diabetes, 62(10), 3547-3552.
Kopeć, G., Waligora, M., Pacia, M., Chmielak, W., Stępień, A., Janiec, S., ... & Podolec, P.
(2018). Electrocardiogram reading: a randomized study comparing 2 e-learning
methods for medical students. Polish archives of internal medicine, 128(2), 98-104.
Kubica, J., Kubica, A., Jilma, B., Adamski, P., Hobl, E. L., Navarese, E. P., ...&Gurbel, P. A.
(2016). Impact of morphine on antiplatelet effects of oral P2Y12 receptor inhibitors.
International journal of cardiology, 215, 201-208.
Lagraauw, H. M., Kuiper, J., & Bot, I. (2015). Acute and chronic psychological stress as risk
factors for cardiovascular disease: Insights gained from epidemiological, clinical and
experimental studies. Brain, behavior, and immunity, 50, 18-30.
Marinescu, M. A., Löffler, A. I., Ouellette, M., Smith, L., Kramer, C. M., & Bourque, J. M.
(2015). Coronary microvascular dysfunction, microvascular angina, and treatment
strategies. JACC: Cardiovascular Imaging, 8(2), 210-220.
Milosevic, A., Vasiljevic-Pokrajcic, Z., Milasinovic, D., Marinkovic, J., Vukcevic, V.,
Stefanovic, B., ... & Stankovic, G. (2016). Immediate versus delayed invasive
intervention for non-STEMI patients: the RIDDLE-NSTEMI study. JACC:
Cardiovascular Interventions, 9(6), 541-549.
NIMH 2019 Chronic Illness & Mental Health. (2019). Nimh.nih.gov.
Ohman, E. M. (2016). Chronic stable angina. New England Journal of Medicine, 374(12),
1167-1176.
monotherapy with either drug in patients with primary hypercholesterolemia.
Diabetes, 62(10), 3547-3552.
Kopeć, G., Waligora, M., Pacia, M., Chmielak, W., Stępień, A., Janiec, S., ... & Podolec, P.
(2018). Electrocardiogram reading: a randomized study comparing 2 e-learning
methods for medical students. Polish archives of internal medicine, 128(2), 98-104.
Kubica, J., Kubica, A., Jilma, B., Adamski, P., Hobl, E. L., Navarese, E. P., ...&Gurbel, P. A.
(2016). Impact of morphine on antiplatelet effects of oral P2Y12 receptor inhibitors.
International journal of cardiology, 215, 201-208.
Lagraauw, H. M., Kuiper, J., & Bot, I. (2015). Acute and chronic psychological stress as risk
factors for cardiovascular disease: Insights gained from epidemiological, clinical and
experimental studies. Brain, behavior, and immunity, 50, 18-30.
Marinescu, M. A., Löffler, A. I., Ouellette, M., Smith, L., Kramer, C. M., & Bourque, J. M.
(2015). Coronary microvascular dysfunction, microvascular angina, and treatment
strategies. JACC: Cardiovascular Imaging, 8(2), 210-220.
Milosevic, A., Vasiljevic-Pokrajcic, Z., Milasinovic, D., Marinkovic, J., Vukcevic, V.,
Stefanovic, B., ... & Stankovic, G. (2016). Immediate versus delayed invasive
intervention for non-STEMI patients: the RIDDLE-NSTEMI study. JACC:
Cardiovascular Interventions, 9(6), 541-549.
NIMH 2019 Chronic Illness & Mental Health. (2019). Nimh.nih.gov.
Ohman, E. M. (2016). Chronic stable angina. New England Journal of Medicine, 374(12),
1167-1176.
14ACUTE CORONARY SYNDROME: A CASE STUDY
Patel, N. B., &Zeltser, R. (2018). Angina, Unstable. In StatPearls [Internet]. StatPearls
Publishing.
Penzel, T., Kantelhardt, J. W., Bartsch, R. P., Riedl, M., Kraemer, J. F., Wessel, N., ... &
Schöbel, C. (2016). Modulations of heart rate, ECG, and cardio-respiratory coupling
observed in polysomnography. Frontiers in physiology, 7, 460.
Pollack Jr, C. V., & Riese, V. G. (2019). Acute Coronary Syndrome: Unstable Angina.
In Differential Diagnosis of Cardiopulmonary Disease (pp. 73-96). Springer, Cham.
Rothnie, K. J., Smeeth, L., Pearce, N., Herrett, E., Timmis, A., Hemingway, H., ... & Quint, J.
K. (2016). Predicting mortality after acute coronary syndromes in people with chronic
obstructive pulmonary disease. Heart, 102(18), 1442-1448.
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., & Lucia, A. (2016). Epidemiology of
coronary heart disease and acute coronary syndrome. Annals of translational
medicine, 4(13).
Sandoval, Y., Apple, F. S., & Smith, S. W. (2018). High-sensitivity cardiac troponin assays
and unstable angina. European Heart Journal: Acute Cardiovascular Care, 7(2), 120-
128.
Sepahvand, E., Jalai, R., Mirzaei, M., & Jahromi, M. K. (2015). Association between short
sleep and body mass index, hypertension among acute coronary syndrome patients in
coronary care unit. Global journal of health science, 7(3), 134.
Talreja, O. and Cassagnol, M. (2019). Diltiazem. [online] Ncbi.nlm.nih.gov. Available at:
https://www.ncbi.nlm.nih.gov/books/NBK532937/ [Accessed 20 Jul. 2019].
Patel, N. B., &Zeltser, R. (2018). Angina, Unstable. In StatPearls [Internet]. StatPearls
Publishing.
Penzel, T., Kantelhardt, J. W., Bartsch, R. P., Riedl, M., Kraemer, J. F., Wessel, N., ... &
Schöbel, C. (2016). Modulations of heart rate, ECG, and cardio-respiratory coupling
observed in polysomnography. Frontiers in physiology, 7, 460.
Pollack Jr, C. V., & Riese, V. G. (2019). Acute Coronary Syndrome: Unstable Angina.
In Differential Diagnosis of Cardiopulmonary Disease (pp. 73-96). Springer, Cham.
Rothnie, K. J., Smeeth, L., Pearce, N., Herrett, E., Timmis, A., Hemingway, H., ... & Quint, J.
K. (2016). Predicting mortality after acute coronary syndromes in people with chronic
obstructive pulmonary disease. Heart, 102(18), 1442-1448.
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., & Lucia, A. (2016). Epidemiology of
coronary heart disease and acute coronary syndrome. Annals of translational
medicine, 4(13).
Sandoval, Y., Apple, F. S., & Smith, S. W. (2018). High-sensitivity cardiac troponin assays
and unstable angina. European Heart Journal: Acute Cardiovascular Care, 7(2), 120-
128.
Sepahvand, E., Jalai, R., Mirzaei, M., & Jahromi, M. K. (2015). Association between short
sleep and body mass index, hypertension among acute coronary syndrome patients in
coronary care unit. Global journal of health science, 7(3), 134.
Talreja, O. and Cassagnol, M. (2019). Diltiazem. [online] Ncbi.nlm.nih.gov. Available at:
https://www.ncbi.nlm.nih.gov/books/NBK532937/ [Accessed 20 Jul. 2019].
15ACUTE CORONARY SYNDROME: A CASE STUDY
Tran, H. V., Gore, J. M., Darling, C. E., Ash, A. S., Kiefe, C. I., & Goldberg, R. J. (2018).
Hyperglycemia and risk of ventricular tachycardia among patients hospitalized with
acute myocardial infarction. Cardiovascular diabetology, 17(1), 136.
Verheye, S., Jolicœur, E. M., Behan, M. W., Pettersson, T., Sainsbury, P., Hill, J., ... & De
Silva, R. (2015). Efficacy of a device to narrow the coronary sinus in refractory
angina. New England Journal of Medicine, 372(6), 519-527.
Voinov, B., Richie, W., & Bailey, R. (2013). Depression and Chronic Diseases. The Primary
Care Companion For CNS Disorders. doi:10.4088/pcc.12r01468
White, W. B., Kupfer, S., Zannad, F., Mehta, C. R., Wilson, C. A., Lei, L., ... & Bergenstal,
R. M. (2016). Cardiovascular mortality in patients with type 2 diabetes and recent
acute coronary syndromes from the EXAMINE trial. Diabetes Care, 39(7), 1267-
1273.
Yellon, D. M., Ackbarkhan, A. K., Balgobin, V., Bulluck, H., Deelchand, A., Dhuny, M.
R., ... & Kowlessur, S. (2015). Remote ischemic conditioning reduces myocardial
infarct size in STEMI patients treated by thrombolysis. Journal of the American
College of Cardiology, 65(25), 2764-2765.
Zègre-Hemsey, J., Garvey, J., & Carey, M. (2016). Cardiac Monitoring in the Emergency
Department. Critical Care Nursing Clinics of North America, 28(3), 331-345.
doi:10.1016/j.cnc.2016.04.009
Zhao, Q., Zhu, Y., Xu, Z., Cheng, Z., Mei, J., Chen, X., & Wang, X. (2018). Effect of
Ticagrelor Plus Aspirin, Ticagrelor Alone, or Aspirin Alone on Saphenous Vein Graft
Patency 1 Year After Coronary Artery Bypass Grafting. JAMA, 319(16), 1677.
doi:10.1001/jama.2018.3197
Tran, H. V., Gore, J. M., Darling, C. E., Ash, A. S., Kiefe, C. I., & Goldberg, R. J. (2018).
Hyperglycemia and risk of ventricular tachycardia among patients hospitalized with
acute myocardial infarction. Cardiovascular diabetology, 17(1), 136.
Verheye, S., Jolicœur, E. M., Behan, M. W., Pettersson, T., Sainsbury, P., Hill, J., ... & De
Silva, R. (2015). Efficacy of a device to narrow the coronary sinus in refractory
angina. New England Journal of Medicine, 372(6), 519-527.
Voinov, B., Richie, W., & Bailey, R. (2013). Depression and Chronic Diseases. The Primary
Care Companion For CNS Disorders. doi:10.4088/pcc.12r01468
White, W. B., Kupfer, S., Zannad, F., Mehta, C. R., Wilson, C. A., Lei, L., ... & Bergenstal,
R. M. (2016). Cardiovascular mortality in patients with type 2 diabetes and recent
acute coronary syndromes from the EXAMINE trial. Diabetes Care, 39(7), 1267-
1273.
Yellon, D. M., Ackbarkhan, A. K., Balgobin, V., Bulluck, H., Deelchand, A., Dhuny, M.
R., ... & Kowlessur, S. (2015). Remote ischemic conditioning reduces myocardial
infarct size in STEMI patients treated by thrombolysis. Journal of the American
College of Cardiology, 65(25), 2764-2765.
Zègre-Hemsey, J., Garvey, J., & Carey, M. (2016). Cardiac Monitoring in the Emergency
Department. Critical Care Nursing Clinics of North America, 28(3), 331-345.
doi:10.1016/j.cnc.2016.04.009
Zhao, Q., Zhu, Y., Xu, Z., Cheng, Z., Mei, J., Chen, X., & Wang, X. (2018). Effect of
Ticagrelor Plus Aspirin, Ticagrelor Alone, or Aspirin Alone on Saphenous Vein Graft
Patency 1 Year After Coronary Artery Bypass Grafting. JAMA, 319(16), 1677.
doi:10.1001/jama.2018.3197
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

16ACUTE CORONARY SYNDROME: A CASE STUDY
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





