Pathophysiology and Pharmacology Applied to Nursing
VerifiedAdded on 2023/04/10
|12
|2572
|447
AI Summary
This study material explores the pathophysiology and pharmacology applied to nursing, focusing on acute coronary syndrome, angina, risk factors, ECG interpretation, and medication considerations. It provides a comprehensive understanding of the topic.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: ACUTE CORONARY SYNDROME 1
PATHOPHYSIOLOGY AND PHARMACOLOGY APPLIED TO NURSING
Student’s Name
Institutional Affiliation
Course
Instructor
Date
PATHOPHYSIOLOGY AND PHARMACOLOGY APPLIED TO NURSING
Student’s Name
Institutional Affiliation
Course
Instructor
Date
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

ACUTE CORONARY SYNDROME 2
Introduction
The paper will respond to the given questions with reference to the case study of
Betsy Blogger who is 72 years with complains of shortness of breath and nauseas in the
surgical ward. She also has uncomplicated fixation of the right tubula and the fibula fracture
for a period of two period. The patient has a past medical history of Coronary Heart Disease,
Coronary Artery Bypass Graft (CAGs), Hypertension, Chronic Obstructive Pulmonary
Disease (COPD), and Type 2 Diabetes. The current medication regimens for the patient
include Aspirin, endone, diltiazem, paracetamol, enoxaparin, GTN spray, salbutamol,
pravastatin, metformin, and Spiriva 2 puffs. With reference to the case scenario of Betsy, the
paper will provide a rationale for the request of the ECG, describe the underlying
pathophysiology of angina with regard to the causes, outcomes, and progression and the risk
factors associated with the increased risk of the development of Acute Coronary Syndrome to
the patient.
Thirdly, the paper with analyze and interpret Betsy’s ECG which was taken while
experiencing shortness of breath and nausea. Fourthly, the paper will discuss three central
findings that may indicate Acute Coronary Syndrome and discuss the GTN, pravastatin, and
diltiazem medications including their groups, mechanisms of action, side effects and
complications, and the nursing considerations. Lastly, the paper will discuss the use of and
mechanism of action of ticagrelor and aspirin in a patient with cardiac problems, use of
morphine in the Acute Coronary Syndrome, and an elaboration of the linkage between high
risk of depression in patients with chronic illnesses such as Coronary Heart Disease.
Question 1: Interpretation of Betsy’s ECG without shortness of breath and nausea
The ECG shows ST segment depression, Q waves, and T wave inversion which whose rate
and rhythm are slightly irregular compared to when the patient is experiencing shortness of
breath and nausea.
Introduction
The paper will respond to the given questions with reference to the case study of
Betsy Blogger who is 72 years with complains of shortness of breath and nauseas in the
surgical ward. She also has uncomplicated fixation of the right tubula and the fibula fracture
for a period of two period. The patient has a past medical history of Coronary Heart Disease,
Coronary Artery Bypass Graft (CAGs), Hypertension, Chronic Obstructive Pulmonary
Disease (COPD), and Type 2 Diabetes. The current medication regimens for the patient
include Aspirin, endone, diltiazem, paracetamol, enoxaparin, GTN spray, salbutamol,
pravastatin, metformin, and Spiriva 2 puffs. With reference to the case scenario of Betsy, the
paper will provide a rationale for the request of the ECG, describe the underlying
pathophysiology of angina with regard to the causes, outcomes, and progression and the risk
factors associated with the increased risk of the development of Acute Coronary Syndrome to
the patient.
Thirdly, the paper with analyze and interpret Betsy’s ECG which was taken while
experiencing shortness of breath and nausea. Fourthly, the paper will discuss three central
findings that may indicate Acute Coronary Syndrome and discuss the GTN, pravastatin, and
diltiazem medications including their groups, mechanisms of action, side effects and
complications, and the nursing considerations. Lastly, the paper will discuss the use of and
mechanism of action of ticagrelor and aspirin in a patient with cardiac problems, use of
morphine in the Acute Coronary Syndrome, and an elaboration of the linkage between high
risk of depression in patients with chronic illnesses such as Coronary Heart Disease.
Question 1: Interpretation of Betsy’s ECG without shortness of breath and nausea
The ECG shows ST segment depression, Q waves, and T wave inversion which whose rate
and rhythm are slightly irregular compared to when the patient is experiencing shortness of
breath and nausea.

ACUTE CORONARY SYNDROME 3
Question 2a: Pathophysiology of Angina
Angina is a chest pain which results from reduced flow of blood to the heart. It is one
of the primary symptoms of Coronary Artery Disease. It may also be referred as angina
pectoris which is always described as the pressure, squeezing, heaviness, pain, or tightness of
the chest. The primary cause of angina is myocardial ischemia which is caused by the
mismatch between the oxygen demand and myocardial blood supply or flow. The restriction
of the myocardial flow of blood results from the atherosclerotic narrowing of the epicardial
coronary artery, although vasoconstriction or abnormal vasodilation caused by impairment of
the endothelia functioning are also essential pathophysiological mechanisms behind the
development of angina (Ambrose, & Singh, 2015).
Some of the risk factors of angina include obesity, diabetes, stress physical inactivity,
hypertension, older age, positive history of heart disease in the family, high levels of
cholesterol in blood, and tobacco use either smoking, chewing or prolonged exposure to
passive smoking. The heart rate is one of the major determinants of myocardial ischemia
which principally results from the reduction of diastolic perfusion and increased myocardial
demand for oxygen (Palombo, & Kozakova, 2016).
One of the major symptoms of angina include chest discomfort or pain which is
possibly described as squeezing, pressure, fullness or burning. Other symptoms include
fatigue, nauseas, shortness of breath, dizziness, sweating, and painful neck, arms, jaw, back,
or shoulder which accompany chest pain. Stable angina results from exertion and is relieved
by resting (Thiruvoipati, Kielhorn, & Armstrong, 2015).
Unstable angina is considered as a medical emergency since it occurs unexpectedly
even when the patient is resting and its severe lasting for about 30 minutes above. Unstable
angina may not relieve with the use of medication or rest and its might be signal of heart
Question 2a: Pathophysiology of Angina
Angina is a chest pain which results from reduced flow of blood to the heart. It is one
of the primary symptoms of Coronary Artery Disease. It may also be referred as angina
pectoris which is always described as the pressure, squeezing, heaviness, pain, or tightness of
the chest. The primary cause of angina is myocardial ischemia which is caused by the
mismatch between the oxygen demand and myocardial blood supply or flow. The restriction
of the myocardial flow of blood results from the atherosclerotic narrowing of the epicardial
coronary artery, although vasoconstriction or abnormal vasodilation caused by impairment of
the endothelia functioning are also essential pathophysiological mechanisms behind the
development of angina (Ambrose, & Singh, 2015).
Some of the risk factors of angina include obesity, diabetes, stress physical inactivity,
hypertension, older age, positive history of heart disease in the family, high levels of
cholesterol in blood, and tobacco use either smoking, chewing or prolonged exposure to
passive smoking. The heart rate is one of the major determinants of myocardial ischemia
which principally results from the reduction of diastolic perfusion and increased myocardial
demand for oxygen (Palombo, & Kozakova, 2016).
One of the major symptoms of angina include chest discomfort or pain which is
possibly described as squeezing, pressure, fullness or burning. Other symptoms include
fatigue, nauseas, shortness of breath, dizziness, sweating, and painful neck, arms, jaw, back,
or shoulder which accompany chest pain. Stable angina results from exertion and is relieved
by resting (Thiruvoipati, Kielhorn, & Armstrong, 2015).
Unstable angina is considered as a medical emergency since it occurs unexpectedly
even when the patient is resting and its severe lasting for about 30 minutes above. Unstable
angina may not relieve with the use of medication or rest and its might be signal of heart

ACUTE CORONARY SYNDROME 4
attack. In unstable angina, the fatty deposits in the blood vessels rupture or a clot forms thus
blocking or reducing the flow via the narrowed artery. Consequently, this severely and
suddenly decreases the blood flow to the patient’s heart muscles resulting in chest pain
(Nelson et al., 2015).
The nonSTEMI type of angina results from partial occlusion of the coronary
artery by a thrombus resulting in the reduction of coronary flow of blood which
consequently results in subendocardial ischemia. On the other hand, STEMI angina is
caused a complete obstruction of the coronary artery by a thrombus which completely
stops the coronary flow of blood causing transmural ischemia. The hallmark for all is
chest pain but it is more severe in STEMI compare to unstable angina and nonSTEMI
(Handler, Coghlan, & Brown, 2018).
Ischemia in both STEMI and nonSTEMI are associated with necrosis while the
unstable does not present with necrosis. Angina progresses from unstable angina which is
potentially reversible to the irreversible phase of cell death secondary to myocardial
infarction which is either nonSTEMI or STEMI. If left untreated, the outcome of angina is
negative since it results in life-threatening complications and conditions such as heart failure,
arrhythmias, and heart attack (Douglas et al., 2015).
Question 2b: Two risk factors specific to the case scenario of Betsy that increase her
risk of Acute Coronary Syndrome
1) History of hypertension and Type 2 diabetes
2) Past history of Coronary Artery Bypass Graft and Coronary Artery Disease
Question 3: Interpretation of Betsy’s ECG while experiencing shortness of breath and
nausea
attack. In unstable angina, the fatty deposits in the blood vessels rupture or a clot forms thus
blocking or reducing the flow via the narrowed artery. Consequently, this severely and
suddenly decreases the blood flow to the patient’s heart muscles resulting in chest pain
(Nelson et al., 2015).
The nonSTEMI type of angina results from partial occlusion of the coronary
artery by a thrombus resulting in the reduction of coronary flow of blood which
consequently results in subendocardial ischemia. On the other hand, STEMI angina is
caused a complete obstruction of the coronary artery by a thrombus which completely
stops the coronary flow of blood causing transmural ischemia. The hallmark for all is
chest pain but it is more severe in STEMI compare to unstable angina and nonSTEMI
(Handler, Coghlan, & Brown, 2018).
Ischemia in both STEMI and nonSTEMI are associated with necrosis while the
unstable does not present with necrosis. Angina progresses from unstable angina which is
potentially reversible to the irreversible phase of cell death secondary to myocardial
infarction which is either nonSTEMI or STEMI. If left untreated, the outcome of angina is
negative since it results in life-threatening complications and conditions such as heart failure,
arrhythmias, and heart attack (Douglas et al., 2015).
Question 2b: Two risk factors specific to the case scenario of Betsy that increase her
risk of Acute Coronary Syndrome
1) History of hypertension and Type 2 diabetes
2) Past history of Coronary Artery Bypass Graft and Coronary Artery Disease
Question 3: Interpretation of Betsy’s ECG while experiencing shortness of breath and
nausea
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
ACUTE CORONARY SYNDROME 5
The ECG reveals depression of the ST segment, inversion of T wave, and Q waves
which shows high likelihood of myocardial infarction to the patient. Abnormalities like
arterial fibrillation, ventricular hypertrophy, and pacing artifacts may bring out ischemic
signs on the ECG. The rate of the ECG is reduced with an irregular rhythm and presence of P
waves which are irregular indicating possibility of Acute Coronary Syndrome to the patient.
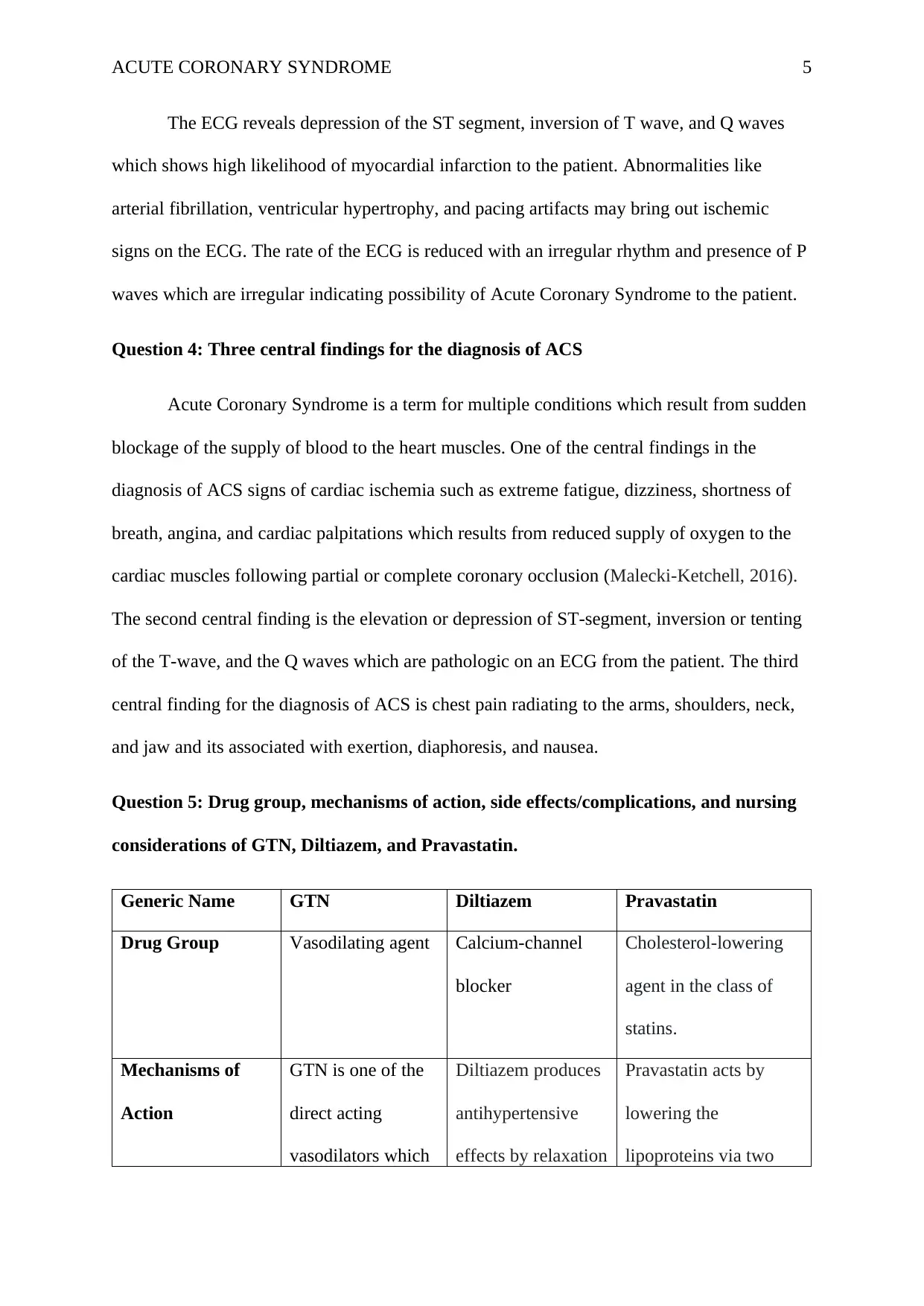
Question 4: Three central findings for the diagnosis of ACS
Acute Coronary Syndrome is a term for multiple conditions which result from sudden
blockage of the supply of blood to the heart muscles. One of the central findings in the
diagnosis of ACS signs of cardiac ischemia such as extreme fatigue, dizziness, shortness of
breath, angina, and cardiac palpitations which results from reduced supply of oxygen to the
cardiac muscles following partial or complete coronary occlusion (Malecki-Ketchell, 2016).
The second central finding is the elevation or depression of ST-segment, inversion or tenting
of the T-wave, and the Q waves which are pathologic on an ECG from the patient. The third
central finding for the diagnosis of ACS is chest pain radiating to the arms, shoulders, neck,
and jaw and its associated with exertion, diaphoresis, and nausea.
Question 5: Drug group, mechanisms of action, side effects/complications, and nursing
considerations of GTN, Diltiazem, and Pravastatin.
Generic Name GTN Diltiazem Pravastatin
Drug Group Vasodilating agent Calcium-channel
blocker
Cholesterol-lowering
agent in the class of
statins.
Mechanisms of
Action
GTN is one of the
direct acting
vasodilators which
Diltiazem produces
antihypertensive
effects by relaxation
Pravastatin acts by
lowering the
lipoproteins via two
The ECG reveals depression of the ST segment, inversion of T wave, and Q waves
which shows high likelihood of myocardial infarction to the patient. Abnormalities like
arterial fibrillation, ventricular hypertrophy, and pacing artifacts may bring out ischemic
signs on the ECG. The rate of the ECG is reduced with an irregular rhythm and presence of P
waves which are irregular indicating possibility of Acute Coronary Syndrome to the patient.
Question 4: Three central findings for the diagnosis of ACS
Acute Coronary Syndrome is a term for multiple conditions which result from sudden
blockage of the supply of blood to the heart muscles. One of the central findings in the
diagnosis of ACS signs of cardiac ischemia such as extreme fatigue, dizziness, shortness of
breath, angina, and cardiac palpitations which results from reduced supply of oxygen to the
cardiac muscles following partial or complete coronary occlusion (Malecki-Ketchell, 2016).
The second central finding is the elevation or depression of ST-segment, inversion or tenting
of the T-wave, and the Q waves which are pathologic on an ECG from the patient. The third
central finding for the diagnosis of ACS is chest pain radiating to the arms, shoulders, neck,
and jaw and its associated with exertion, diaphoresis, and nausea.
Question 5: Drug group, mechanisms of action, side effects/complications, and nursing
considerations of GTN, Diltiazem, and Pravastatin.
Generic Name GTN Diltiazem Pravastatin
Drug Group Vasodilating agent Calcium-channel
blocker
Cholesterol-lowering
agent in the class of
statins.
Mechanisms of
Action
GTN is one of the
direct acting
vasodilators which
Diltiazem produces
antihypertensive
effects by relaxation
Pravastatin acts by
lowering the
lipoproteins via two

ACUTE CORONARY SYNDROME 6
is administered to
reduce pressure of
ventricular filling
or preload in small
doses. It is given in
high doses to
reduce systemic
vascular resistance,
the afterload
(Sawhney et al.,
2018). GTN acts
by reducing the
pulmonary vascular
resistance by
relaxing the smooth
muscles. The
dilation of the
capillary beds
including the large
veins enhances
peripheral blood
pooling thus
decreasing the
venous return to the
patient’s heart. This
of the vascular
smooth muscles
resulting in the
decrease in the
peripheral vascular
resistance. It also
reduces the demand
of oxygen by the
cardiac muscles by
reducing the
systemic blood
pressure and heart
rate at the maximal
and submaximal
workloads. It is a
potent dilator for
the coronary
arteries, both
subendocardial and
epicardial (Leopold,
2015).
pathways. It acts in the
major pathway to
inhibit the functioning
of the
hydroxymethylglutaryl-
CoA reductase
(Sawhney et al., 2018).
Sterically, pravastatin
acts as a reversible
competitive inhibitor to
hinder the action of the
HMG-CoA reductase
through occupation of
the active site of
enzymes. While in the
liver, the enzyme
converts the HMG-
CoA to a mevalonate in
rate-limiting step of
biosynthesis
cholesterol pathway. It
inhibits the process of
synthesis of the Low-
Density Lipoproteins.
The reductions increase
is administered to
reduce pressure of
ventricular filling
or preload in small
doses. It is given in
high doses to
reduce systemic
vascular resistance,
the afterload
(Sawhney et al.,
2018). GTN acts
by reducing the
pulmonary vascular
resistance by
relaxing the smooth
muscles. The
dilation of the
capillary beds
including the large
veins enhances
peripheral blood
pooling thus
decreasing the
venous return to the
patient’s heart. This
of the vascular
smooth muscles
resulting in the
decrease in the
peripheral vascular
resistance. It also
reduces the demand
of oxygen by the
cardiac muscles by
reducing the
systemic blood
pressure and heart
rate at the maximal
and submaximal
workloads. It is a
potent dilator for
the coronary
arteries, both
subendocardial and
epicardial (Leopold,
2015).
pathways. It acts in the
major pathway to
inhibit the functioning
of the
hydroxymethylglutaryl-
CoA reductase
(Sawhney et al., 2018).
Sterically, pravastatin
acts as a reversible
competitive inhibitor to
hinder the action of the
HMG-CoA reductase
through occupation of
the active site of
enzymes. While in the
liver, the enzyme
converts the HMG-
CoA to a mevalonate in
rate-limiting step of
biosynthesis
cholesterol pathway. It
inhibits the process of
synthesis of the Low-
Density Lipoproteins.
The reductions increase

ACUTE CORONARY SYNDROME 7
helps in the
reduction of end
diastolic and left
ventricular
pressure. The
venous and arterial
effects of the GTN
reduces
consumption of
oxygen by the
cardiac muscles
(Leopold, 2015).
the receptor of cellular
LDL thus increasing
the uptake of LDL and
reducing its levels in
the bloodstream.
Generally, the
mechanism reduces the
circulating LDL and
cholesterol in the blood
(Leopold, 2015).
Side effects/
complications
Tachycardia,
Hypotension,
Bradycardia,
Muscle twitching,
decreased partial
pressure of oxygen
(Katzung, 2017).
Hypotension,
dizziness,
bradycardia,
flushing (Katzung,
2017).
joint pain, headaches
diarrhea, muscle pains,
nausea, liver problems,
rhabdomyolysis,
diabetes (Katzung,
2017).
Nursing
Considerations
Careful and close
monitoring of the
patient’s CVP,
systemic blood
pressure, heart
rhythm and rate,
Close monitoring of
the patient’s blood
pressure to prevent
hypotension
Close monitoring
and measuring of
Assessing the patient
for signs of renal and
hepatic impairment
since it’s a
contraindication.
Checking the patient
helps in the
reduction of end
diastolic and left
ventricular
pressure. The
venous and arterial
effects of the GTN
reduces
consumption of
oxygen by the
cardiac muscles
(Leopold, 2015).
the receptor of cellular
LDL thus increasing
the uptake of LDL and
reducing its levels in
the bloodstream.
Generally, the
mechanism reduces the
circulating LDL and
cholesterol in the blood
(Leopold, 2015).
Side effects/
complications
Tachycardia,
Hypotension,
Bradycardia,
Muscle twitching,
decreased partial
pressure of oxygen
(Katzung, 2017).
Hypotension,
dizziness,
bradycardia,
flushing (Katzung,
2017).
joint pain, headaches
diarrhea, muscle pains,
nausea, liver problems,
rhabdomyolysis,
diabetes (Katzung,
2017).
Nursing
Considerations
Careful and close
monitoring of the
patient’s CVP,
systemic blood
pressure, heart
rhythm and rate,
Close monitoring of
the patient’s blood
pressure to prevent
hypotension
Close monitoring
and measuring of
Assessing the patient
for signs of renal and
hepatic impairment
since it’s a
contraindication.
Checking the patient
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE CORONARY SYNDROME 8
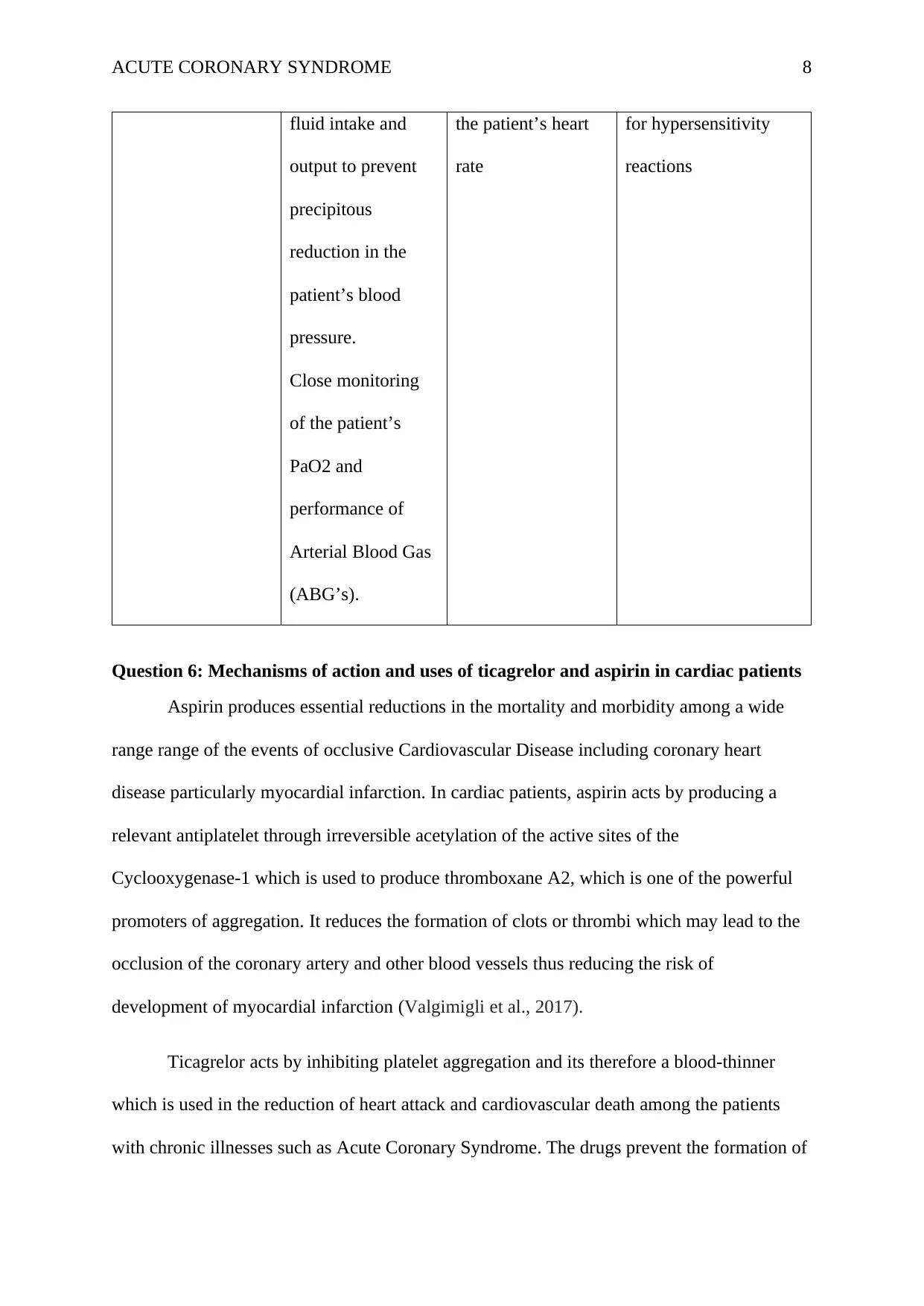
fluid intake and
output to prevent
precipitous
reduction in the
patient’s blood
pressure.
Close monitoring
of the patient’s
PaO2 and
performance of
Arterial Blood Gas
(ABG’s).
the patient’s heart
rate
for hypersensitivity
reactions
Question 6: Mechanisms of action and uses of ticagrelor and aspirin in cardiac patients
Aspirin produces essential reductions in the mortality and morbidity among a wide
range range of the events of occlusive Cardiovascular Disease including coronary heart
disease particularly myocardial infarction. In cardiac patients, aspirin acts by producing a
relevant antiplatelet through irreversible acetylation of the active sites of the
Cyclooxygenase-1 which is used to produce thromboxane A2, which is one of the powerful
promoters of aggregation. It reduces the formation of clots or thrombi which may lead to the
occlusion of the coronary artery and other blood vessels thus reducing the risk of
development of myocardial infarction (Valgimigli et al., 2017).
Ticagrelor acts by inhibiting platelet aggregation and its therefore a blood-thinner
which is used in the reduction of heart attack and cardiovascular death among the patients
with chronic illnesses such as Acute Coronary Syndrome. The drugs prevent the formation of
fluid intake and
output to prevent
precipitous
reduction in the
patient’s blood
pressure.
Close monitoring
of the patient’s
PaO2 and
performance of
Arterial Blood Gas
(ABG’s).
the patient’s heart
rate
for hypersensitivity
reactions
Question 6: Mechanisms of action and uses of ticagrelor and aspirin in cardiac patients
Aspirin produces essential reductions in the mortality and morbidity among a wide
range range of the events of occlusive Cardiovascular Disease including coronary heart
disease particularly myocardial infarction. In cardiac patients, aspirin acts by producing a
relevant antiplatelet through irreversible acetylation of the active sites of the
Cyclooxygenase-1 which is used to produce thromboxane A2, which is one of the powerful
promoters of aggregation. It reduces the formation of clots or thrombi which may lead to the
occlusion of the coronary artery and other blood vessels thus reducing the risk of
development of myocardial infarction (Valgimigli et al., 2017).
Ticagrelor acts by inhibiting platelet aggregation and its therefore a blood-thinner
which is used in the reduction of heart attack and cardiovascular death among the patients
with chronic illnesses such as Acute Coronary Syndrome. The drugs prevent the formation of

ACUTE CORONARY SYNDROME 9
blood clots thus maintaining smooth blood flow thus reducing the risk of the development of
other cardiovascular events. In cardiac patients, a combination of aspirin and ticagrelor are
used in the prevention of heart attack among patients with cardiac problems like unstable
angina and heart attack especially after Coronary Artery Bypass Graft (Franchi et al., 2015).
Question 7: Use of morphine n Acute Coronary Syndrome (ACS) including its benefits
and controversies
In patients with Acute Coronary Syndrome, morphine is used for the relieve of the
symptoms and pain control. It decreases the oxygen demand of the cardiac muscles through
vasodilation, anxiolysis, and reduced pulse rate and blood pressure via elevated vagal tone
(Katzung, 2017). Despite these benefits of morphine to the patients with ACS, there are
problems which are associated with the use of morphine thus making it more controversial.
Morphine has multiple physical effects including dilated pupils, inattention, slurred speech,
nodding off, shallow breathing, apathy, hallucinations, and itchy skin (Parodi et al., 2015).
Question 8: Connection between increased risk of depression and Coronary Heart
Disease (CHD) to Betsy
CHD and depression have a bidirectional relation whereby CHD can lead to
depression while depression is regarded as one of the risk factors for the development of
CHD and its complications. CHD presents with emotional and psychological trauma since the
patient’s may feel hopeless based on her health condition (Sin, Yaffe, & Whooley,2015).
This may result in the development of depression. The patient has been put on multiple
medication regimens and it might be technical for her to adhere to all of them since they
might be psychologically traumatizing. The health conditions and the past medical history of
the patient are one of the key contributors to the patient’s lack of happiness and comfort in
life which increases the risk of development of depression (Dickens, 2015).
blood clots thus maintaining smooth blood flow thus reducing the risk of the development of
other cardiovascular events. In cardiac patients, a combination of aspirin and ticagrelor are
used in the prevention of heart attack among patients with cardiac problems like unstable
angina and heart attack especially after Coronary Artery Bypass Graft (Franchi et al., 2015).
Question 7: Use of morphine n Acute Coronary Syndrome (ACS) including its benefits
and controversies
In patients with Acute Coronary Syndrome, morphine is used for the relieve of the
symptoms and pain control. It decreases the oxygen demand of the cardiac muscles through
vasodilation, anxiolysis, and reduced pulse rate and blood pressure via elevated vagal tone
(Katzung, 2017). Despite these benefits of morphine to the patients with ACS, there are
problems which are associated with the use of morphine thus making it more controversial.
Morphine has multiple physical effects including dilated pupils, inattention, slurred speech,
nodding off, shallow breathing, apathy, hallucinations, and itchy skin (Parodi et al., 2015).
Question 8: Connection between increased risk of depression and Coronary Heart
Disease (CHD) to Betsy
CHD and depression have a bidirectional relation whereby CHD can lead to
depression while depression is regarded as one of the risk factors for the development of
CHD and its complications. CHD presents with emotional and psychological trauma since the
patient’s may feel hopeless based on her health condition (Sin, Yaffe, & Whooley,2015).
This may result in the development of depression. The patient has been put on multiple
medication regimens and it might be technical for her to adhere to all of them since they
might be psychologically traumatizing. The health conditions and the past medical history of
the patient are one of the key contributors to the patient’s lack of happiness and comfort in
life which increases the risk of development of depression (Dickens, 2015).

ACUTE CORONARY SYNDROME 10
Conclusion
With regard to the case study, the paper has provided an interpretation of the patient’s
ECG and the underlying pathophysiology of angina including its progress and outcomes. The
paper has discussed the mechanisms of action, drug group, side effects, and nursing
considerations for various drugs including GTN, pravastatin, and diltiazem. Other
medications that have been discussed with regard to the cardiac patients include aspirin,
morphine, and ticagrelor. The paper has also discussed the connection between Coronary
Heart Disease and depression since the patient seems to have an increased risk of depression.
References
Conclusion
With regard to the case study, the paper has provided an interpretation of the patient’s
ECG and the underlying pathophysiology of angina including its progress and outcomes. The
paper has discussed the mechanisms of action, drug group, side effects, and nursing
considerations for various drugs including GTN, pravastatin, and diltiazem. Other
medications that have been discussed with regard to the cardiac patients include aspirin,
morphine, and ticagrelor. The paper has also discussed the connection between Coronary
Heart Disease and depression since the patient seems to have an increased risk of depression.
References
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

ACUTE CORONARY SYNDROME 11
Ambrose, J. A., & Singh, M. (2015). Pathophysiology of coronary artery disease leading to
acute coronary syndromes. F1000prime reports, 7.
Dickens, C. (2015). Depression in people with coronary heart disease: prognostic significance
and mechanisms. Current cardiology reports, 17(10), 83.
Douglas, P. S., Hoffmann, U., Patel, M. R., Mark, D. B., Al-Khalidi, H. R., Cavanaugh, B., ...
& Khan, M. A. (2015). Outcomes of anatomical versus functional testing for coronary
artery disease. New England Journal of Medicine, 372(14), 1291-1300.
Franchi, F., Rollini, F., Cho, J. R., Bhatti, M., DeGroat, C., Ferrante, E., ... & Zenni, M. M.
(2015). Impact of escalating loading dose regimens of ticagrelor in patients with ST-
segment elevation myocardial infarction undergoing primary percutaneous coronary
intervention: results of a prospective randomized pharmacokinetic and
pharmacodynamic investigation. JACC: Cardiovascular Interventions, 8(11), 1457-
1467.
Handler, C., Coghlan, G., & Brown, N. (2018). Angina. In Management of Cardiac
Problems in Primary Care (pp. 92-121). CRC Press.
Katzung, B. G. (2017). Basic and clinical pharmacology. McGraw-Hill Education.
Leopold, J. A. (2015). Antioxidants and coronary artery disease: from pathophysiology to
preventive therapy. Coronary artery disease, 26(2), 176.
Malecki-Ketchell, A. (2016). Acute coronary syndrome. Nursing the Acutely Ill Adult:
Priorities in Assessment and Management. Second edition. Palgrave Macmillan,
London, 140-184.
Ambrose, J. A., & Singh, M. (2015). Pathophysiology of coronary artery disease leading to
acute coronary syndromes. F1000prime reports, 7.
Dickens, C. (2015). Depression in people with coronary heart disease: prognostic significance
and mechanisms. Current cardiology reports, 17(10), 83.
Douglas, P. S., Hoffmann, U., Patel, M. R., Mark, D. B., Al-Khalidi, H. R., Cavanaugh, B., ...
& Khan, M. A. (2015). Outcomes of anatomical versus functional testing for coronary
artery disease. New England Journal of Medicine, 372(14), 1291-1300.
Franchi, F., Rollini, F., Cho, J. R., Bhatti, M., DeGroat, C., Ferrante, E., ... & Zenni, M. M.
(2015). Impact of escalating loading dose regimens of ticagrelor in patients with ST-
segment elevation myocardial infarction undergoing primary percutaneous coronary
intervention: results of a prospective randomized pharmacokinetic and
pharmacodynamic investigation. JACC: Cardiovascular Interventions, 8(11), 1457-
1467.
Handler, C., Coghlan, G., & Brown, N. (2018). Angina. In Management of Cardiac
Problems in Primary Care (pp. 92-121). CRC Press.
Katzung, B. G. (2017). Basic and clinical pharmacology. McGraw-Hill Education.
Leopold, J. A. (2015). Antioxidants and coronary artery disease: from pathophysiology to
preventive therapy. Coronary artery disease, 26(2), 176.
Malecki-Ketchell, A. (2016). Acute coronary syndrome. Nursing the Acutely Ill Adult:
Priorities in Assessment and Management. Second edition. Palgrave Macmillan,
London, 140-184.
ACUTE CORONARY SYNDROME 12
Nelson, C. P., Hamby, S. E., Saleheen, D., Hopewell, J. C., Zeng, L., Assimes, T. L., ... &
Anand, S. (2015). Genetically determined height and coronary artery disease. New
England Journal of Medicine, 372(17), 1608-1618.
Palombo, C., & Kozakova, M. (2016). Arterial stiffness, atherosclerosis and cardiovascular
risk: pathophysiologic mechanisms and emerging clinical indications. Vascular
pharmacology, 77, 1-7.
Parodi, G., Bellandi, B., Xanthopoulou, I., Capranzano, P., Capodanno, D., Valenti, R., ... &
Alexopoulos, D. (2015). Morphine is associated with a delayed activity of oral
antiplatelet agents in patients with ST-elevation acute myocardial infarction
undergoing primary percutaneous coronary intervention. Circulation: Cardiovascular
Interventions, 8(1), e001593.
Sawhney, J. P. S., Kahali, D., Desai, B., Kumar, S. K., Vishvanathan, M., & Rastogi, V.
(2018). The role of optimal medical therapy in patients with stable coronary artery
disease. Journal of Clinical and Preventive Cardiology, 7(2), 60.
Sin, N. L., Yaffe, K., & Whooley, M. A. (2015). Depressive symptoms, cardiovascular
disease severity, and functional status in older adults with coronary heart disease: the
heart and soul study. Journal of the American Geriatrics Society, 63(1), 8-15.
Thiruvoipati, T., Kielhorn, C. E., & Armstrong, E. J. (2015). Peripheral artery disease in
patients with diabetes: Epidemiology, mechanisms, and outcomes. World journal of
diabetes, 6(7), 961.
Valgimigli, M., Bueno, H., Byrne, R. A., Collet, J. P., Costa, F., Jeppsson, A., ... &
Montalescot, G. (2017). 2017 ESC focused update on dual antiplatelet therapy in
coronary artery disease developed in collaboration with EACTS. European journal of
cardio-thoracic surgery, 53(1), 34-78.
Nelson, C. P., Hamby, S. E., Saleheen, D., Hopewell, J. C., Zeng, L., Assimes, T. L., ... &
Anand, S. (2015). Genetically determined height and coronary artery disease. New
England Journal of Medicine, 372(17), 1608-1618.
Palombo, C., & Kozakova, M. (2016). Arterial stiffness, atherosclerosis and cardiovascular
risk: pathophysiologic mechanisms and emerging clinical indications. Vascular
pharmacology, 77, 1-7.
Parodi, G., Bellandi, B., Xanthopoulou, I., Capranzano, P., Capodanno, D., Valenti, R., ... &
Alexopoulos, D. (2015). Morphine is associated with a delayed activity of oral
antiplatelet agents in patients with ST-elevation acute myocardial infarction
undergoing primary percutaneous coronary intervention. Circulation: Cardiovascular
Interventions, 8(1), e001593.
Sawhney, J. P. S., Kahali, D., Desai, B., Kumar, S. K., Vishvanathan, M., & Rastogi, V.
(2018). The role of optimal medical therapy in patients with stable coronary artery
disease. Journal of Clinical and Preventive Cardiology, 7(2), 60.
Sin, N. L., Yaffe, K., & Whooley, M. A. (2015). Depressive symptoms, cardiovascular
disease severity, and functional status in older adults with coronary heart disease: the
heart and soul study. Journal of the American Geriatrics Society, 63(1), 8-15.
Thiruvoipati, T., Kielhorn, C. E., & Armstrong, E. J. (2015). Peripheral artery disease in
patients with diabetes: Epidemiology, mechanisms, and outcomes. World journal of
diabetes, 6(7), 961.
Valgimigli, M., Bueno, H., Byrne, R. A., Collet, J. P., Costa, F., Jeppsson, A., ... &
Montalescot, G. (2017). 2017 ESC focused update on dual antiplatelet therapy in
coronary artery disease developed in collaboration with EACTS. European journal of
cardio-thoracic surgery, 53(1), 34-78.
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





