Acute Tubular Necrosis: Risk Factors, Aetiology, Pathophysiology, Clinical Manifestations, Diagnostic Tests, and Treatment
VerifiedAI Summary
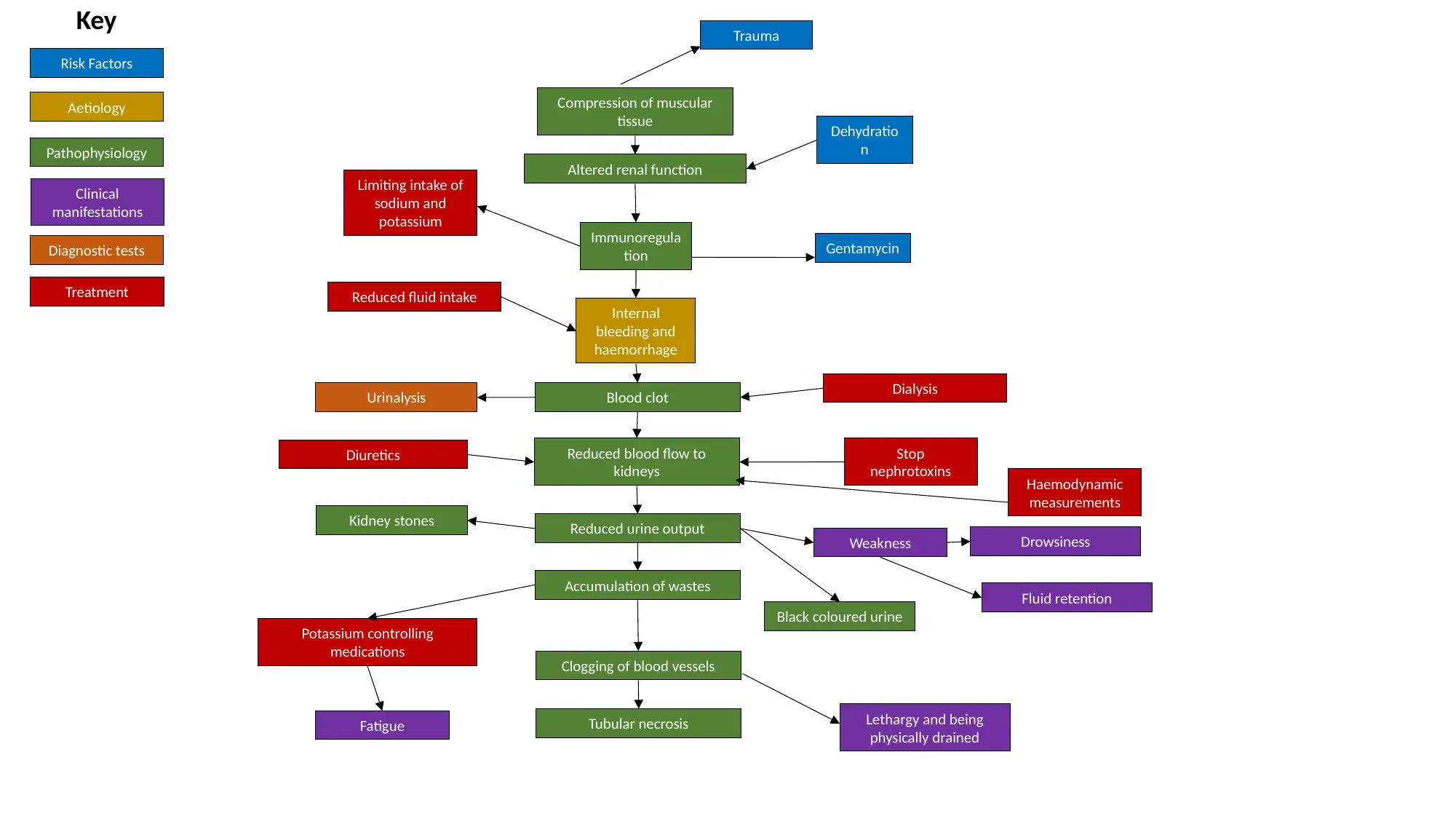
Acute tubular necrosis encompasses a medical condition where there occurs death of the tubular epithelial cells present in the renal tubules. This condition is concomitant with acute kidney injury. Some of the risk factor that contribute to the onset of kidney injury include advanced age, diabetes, radiocontrast, trauma, haemorrhage, and sepsis, overdose of drugs and disease of the connective tissue. Following suspicion of acute tubular necrosis, a range of diagnostic tests were performed in the patient that are given below: Urinalysis, CT scan, Biopsy, Creatinine urine test. Gentamycin antibiotic is commonly used for the prevention of bacterial infections, in combination with other antibiotics. Higher dose of the drug have been found directly responsible for nephrotoxicity.
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)