Advanced Pathophysiology & Pharmacology Report: Case Study Analysis
VerifiedAdded on 2021/05/31
|15
|3522
|31
Report
AI Summary
This report delves into the advanced pathophysiology and pharmacology of chronic obstructive pulmonary disorder (COPD) and pneumonia, focusing on a case study involving a patient named Robert. It examines the pathophysiology of COPD, including the roles of chronic bronchitis and emphysema, and the exacerbation factors such as smoking and occupational exposure. The report also explores the pathophysiology of pneumonia, differentiating between community-acquired and healthcare-associated types. Furthermore, it provides a detailed analysis of various pharmacological interventions, including Salbutamol, Budesonide, Tiotropium, Levofloxacin, Moxifloxacin, and Ceftriaxone, discussing their mechanisms of action, contraindications, side effects, and nursing considerations. The report also touches upon the psychosocial aspects of managing chronic disorders in elderly patients. Overall, the report provides a comprehensive overview of the diseases and the pharmacological treatments.

Running head: ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
Advanced Pathophysiology & Pharmacology
Name of the student:
Name of the university:
Author note:
Advanced Pathophysiology & Pharmacology
Name of the student:
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
Table of Contents
Pathophysiology:.............................................................................................................................2
Pathophysiology of COPD:.........................................................................................................2
Exacerbation of the COPD:.........................................................................................................3
Pathophysiology of pneumonia:..................................................................................................4
Pharmacology..................................................................................................................................5
Salbutamol:..................................................................................................................................5
Budesonide or fomoterol fumarate dehydrate (symbicort):.........................................................6
Tiotropium:..................................................................................................................................6
Levoflaxone:................................................................................................................................7
Moxifloxacin:..............................................................................................................................8
Ceftriaxone:.................................................................................................................................8
Psychosocial:...................................................................................................................................9
References:....................................................................................................................................11
Table of Contents
Pathophysiology:.............................................................................................................................2
Pathophysiology of COPD:.........................................................................................................2
Exacerbation of the COPD:.........................................................................................................3
Pathophysiology of pneumonia:..................................................................................................4
Pharmacology..................................................................................................................................5
Salbutamol:..................................................................................................................................5
Budesonide or fomoterol fumarate dehydrate (symbicort):.........................................................6
Tiotropium:..................................................................................................................................6
Levoflaxone:................................................................................................................................7
Moxifloxacin:..............................................................................................................................8
Ceftriaxone:.................................................................................................................................8
Psychosocial:...................................................................................................................................9
References:....................................................................................................................................11
2ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
Pathophysiology:
Pathophysiology of COPD:
COPD or chronic obstructive pulmonary disorder is a life-threatening respiratory disorder
which can be considered as an umbrella terms that encompasses to key diseases, chronic
bronchitis and emphysema. Emphysema is the abnormal permanent enlargement of the alveoli t
facilitated by the destruction of alveolar wall without Fibrosis. The damage to the alveolar walls
leads to lack of elasticity of the wall fibers of alveoli and destroys the exhalation stability of the
patient leading to chronic emphysema (Agusti, 2014). Chronic Bronchitis can be characterized
by inflammation of the bronchial tubes and facilitated by hypersecretion of mucus. In order to
better understand the pathophysiology of this particular disease the most prevailing contributing
factor has to be discussed. According to the case study, Robert had developed chronic
obstructive pulmonary disorder 18 months before having the acute exacerbation and being
admitted to the ICU. His past medical history reveals that he has been active chain-smoker for
the past 40 years of his life. According to the Albert et al. (2011), COPD is a progressive and
eventually debilitating lung disease and tobacco addiction is one of the most prominent triggers
leading to manifestation and exacerbation of this disease. Smoke triggers damage and breakdown
of the alveolar wall fibres and heightens the risk of chronic obstructive pulmonary disorder and
bronchitis, several folds. The smoke stiffness the air sacs seconds and destroys the alveolar walls
actresses over secretion of mucus as well due to prolonged exposure (Bischoff et al., 2011).
Hence for Robert, the COPD can be considered to be manifested largely due to the smoking and
as he had not stopped smoking even after being diagnosed with this particular respiratory
disorder it also facilitated to the exacerbation. Robert had been working in his own chicken farm,
Pathophysiology:
Pathophysiology of COPD:
COPD or chronic obstructive pulmonary disorder is a life-threatening respiratory disorder
which can be considered as an umbrella terms that encompasses to key diseases, chronic
bronchitis and emphysema. Emphysema is the abnormal permanent enlargement of the alveoli t
facilitated by the destruction of alveolar wall without Fibrosis. The damage to the alveolar walls
leads to lack of elasticity of the wall fibers of alveoli and destroys the exhalation stability of the
patient leading to chronic emphysema (Agusti, 2014). Chronic Bronchitis can be characterized
by inflammation of the bronchial tubes and facilitated by hypersecretion of mucus. In order to
better understand the pathophysiology of this particular disease the most prevailing contributing
factor has to be discussed. According to the case study, Robert had developed chronic
obstructive pulmonary disorder 18 months before having the acute exacerbation and being
admitted to the ICU. His past medical history reveals that he has been active chain-smoker for
the past 40 years of his life. According to the Albert et al. (2011), COPD is a progressive and
eventually debilitating lung disease and tobacco addiction is one of the most prominent triggers
leading to manifestation and exacerbation of this disease. Smoke triggers damage and breakdown
of the alveolar wall fibres and heightens the risk of chronic obstructive pulmonary disorder and
bronchitis, several folds. The smoke stiffness the air sacs seconds and destroys the alveolar walls
actresses over secretion of mucus as well due to prolonged exposure (Bischoff et al., 2011).
Hence for Robert, the COPD can be considered to be manifested largely due to the smoking and
as he had not stopped smoking even after being diagnosed with this particular respiratory
disorder it also facilitated to the exacerbation. Robert had been working in his own chicken farm,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
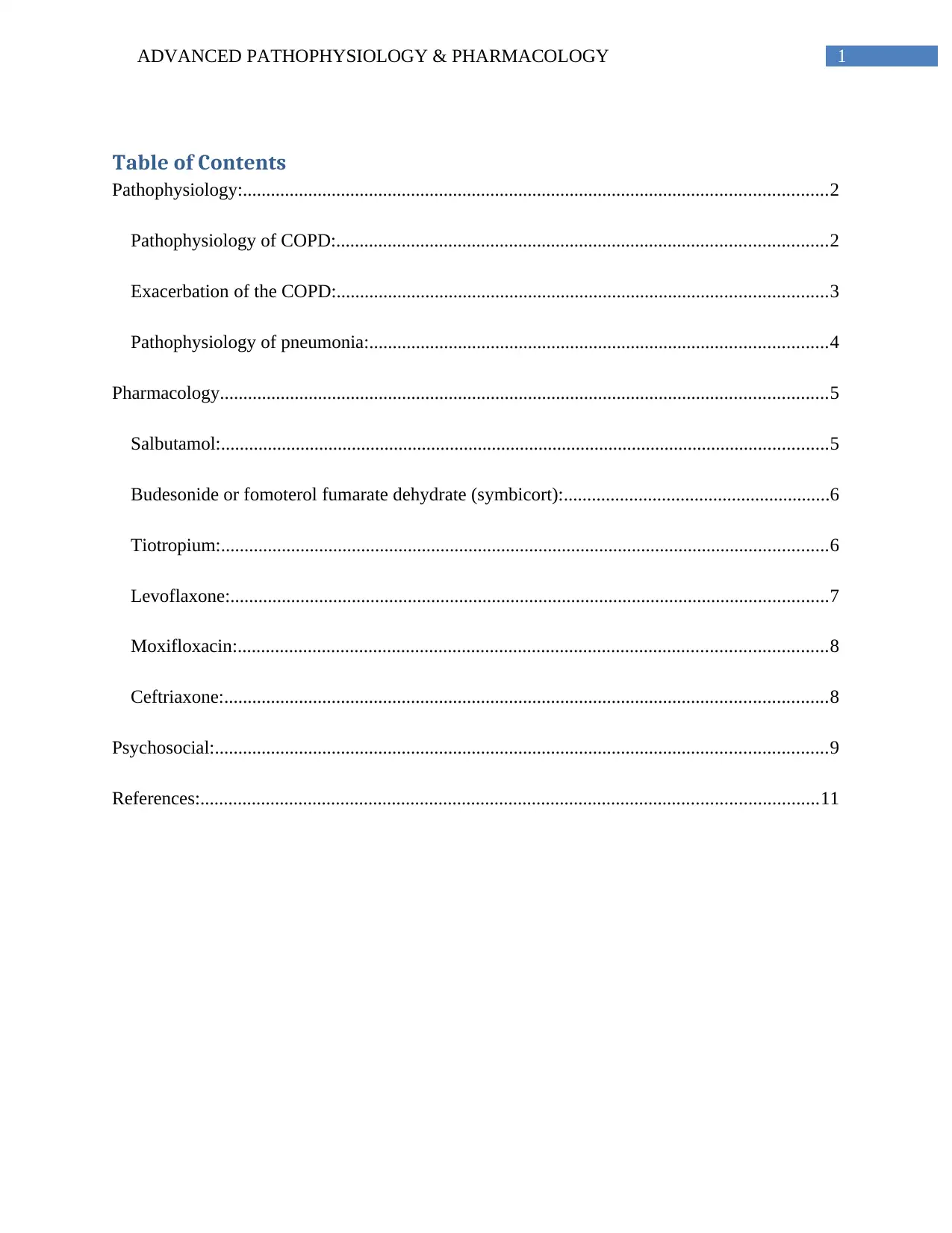
the prolonged occupational exposure to poultry dust could also have contributed to damaging his
respiratory system and facilitating the COPD (Almagro et al., 2012).
(Erb-Downward et al., 2011)
Exacerbation of the COPD:
An exacerbation can be defined as the event that causes deteriorating changes in the
disease progression threatening the life and safety of the patient going through the disease. In
case of COPD, acute exacerbation can be caused by many factors such as a secondary infection,
environmental pollutant triggers, etc (Erb-Downward et al., 2011). The clinical manifestation of
acute exacerbation of chronic obstructive pulmonary disorders includes excessive and severe
wheezing, severe and prolonged episodes of shortness of breath or dyspnea, changes in the
quantity and colour of the sputum. Considering the case study, the most important contributing
factor to the exacerbation that the patient suffers from can be the community acquired
pneumonia. According to the Han et al. (2010), infection leads to 75% of the acute exacerbations
of CPD and it is the leading cause for fatalities associated with this respiratory disorder as well.
the prolonged occupational exposure to poultry dust could also have contributed to damaging his
respiratory system and facilitating the COPD (Almagro et al., 2012).
(Erb-Downward et al., 2011)
Exacerbation of the COPD:
An exacerbation can be defined as the event that causes deteriorating changes in the
disease progression threatening the life and safety of the patient going through the disease. In
case of COPD, acute exacerbation can be caused by many factors such as a secondary infection,
environmental pollutant triggers, etc (Erb-Downward et al., 2011). The clinical manifestation of
acute exacerbation of chronic obstructive pulmonary disorders includes excessive and severe
wheezing, severe and prolonged episodes of shortness of breath or dyspnea, changes in the
quantity and colour of the sputum. Considering the case study, the most important contributing
factor to the exacerbation that the patient suffers from can be the community acquired
pneumonia. According to the Han et al. (2010), infection leads to 75% of the acute exacerbations
of CPD and it is the leading cause for fatalities associated with this respiratory disorder as well.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
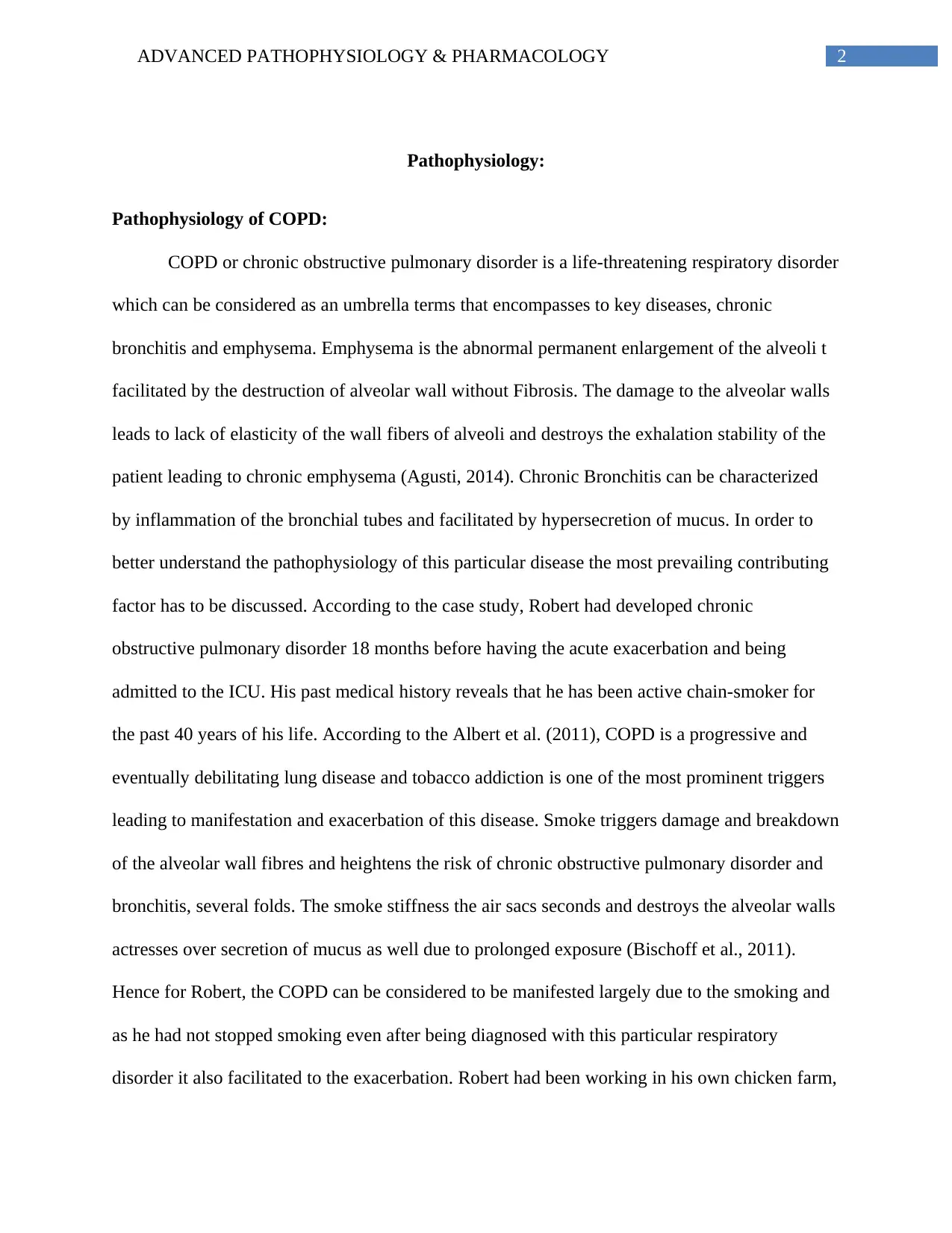
In case of Robert as well, the infection provoked the over secretion of mucus further and
contributed to further blocking of the airways which eventually let two acute exacerbation and
resulted in accessories in acute shortness of breath in the patient. The prolonged effect of
smoking cannot be ignored in this scenario as well. It has to be mentioned that the patient had
been an active smoker for the past 40 years and he had made 5 attempts to quit already but had
not been successful. Continuing to smoke even after being diagnosed with chronic obstructive
pulmonary disorder 18 months ago can also be a constituting factor to the acute exacerbation
Robert suffered from in the case scenario (Giske & Hedlund, 2010).
(Almagro et al., 2012)
Pathophysiology of pneumonia:
Pneumonia is infectious disease caused by Streptococcus pneumoniae that results in
inflammation of the alveolar sac and triggers overproduction of mucus for the blocking the
airways of the patient. The manifestation of the disease is facilitated by the entry of pathogens
through the aspiration procedure after which the pathogen in which the lung parenchyma and
In case of Robert as well, the infection provoked the over secretion of mucus further and
contributed to further blocking of the airways which eventually let two acute exacerbation and
resulted in accessories in acute shortness of breath in the patient. The prolonged effect of
smoking cannot be ignored in this scenario as well. It has to be mentioned that the patient had
been an active smoker for the past 40 years and he had made 5 attempts to quit already but had
not been successful. Continuing to smoke even after being diagnosed with chronic obstructive
pulmonary disorder 18 months ago can also be a constituting factor to the acute exacerbation
Robert suffered from in the case scenario (Giske & Hedlund, 2010).
(Almagro et al., 2012)
Pathophysiology of pneumonia:
Pneumonia is infectious disease caused by Streptococcus pneumoniae that results in
inflammation of the alveolar sac and triggers overproduction of mucus for the blocking the
airways of the patient. The manifestation of the disease is facilitated by the entry of pathogens
through the aspiration procedure after which the pathogen in which the lung parenchyma and
5ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
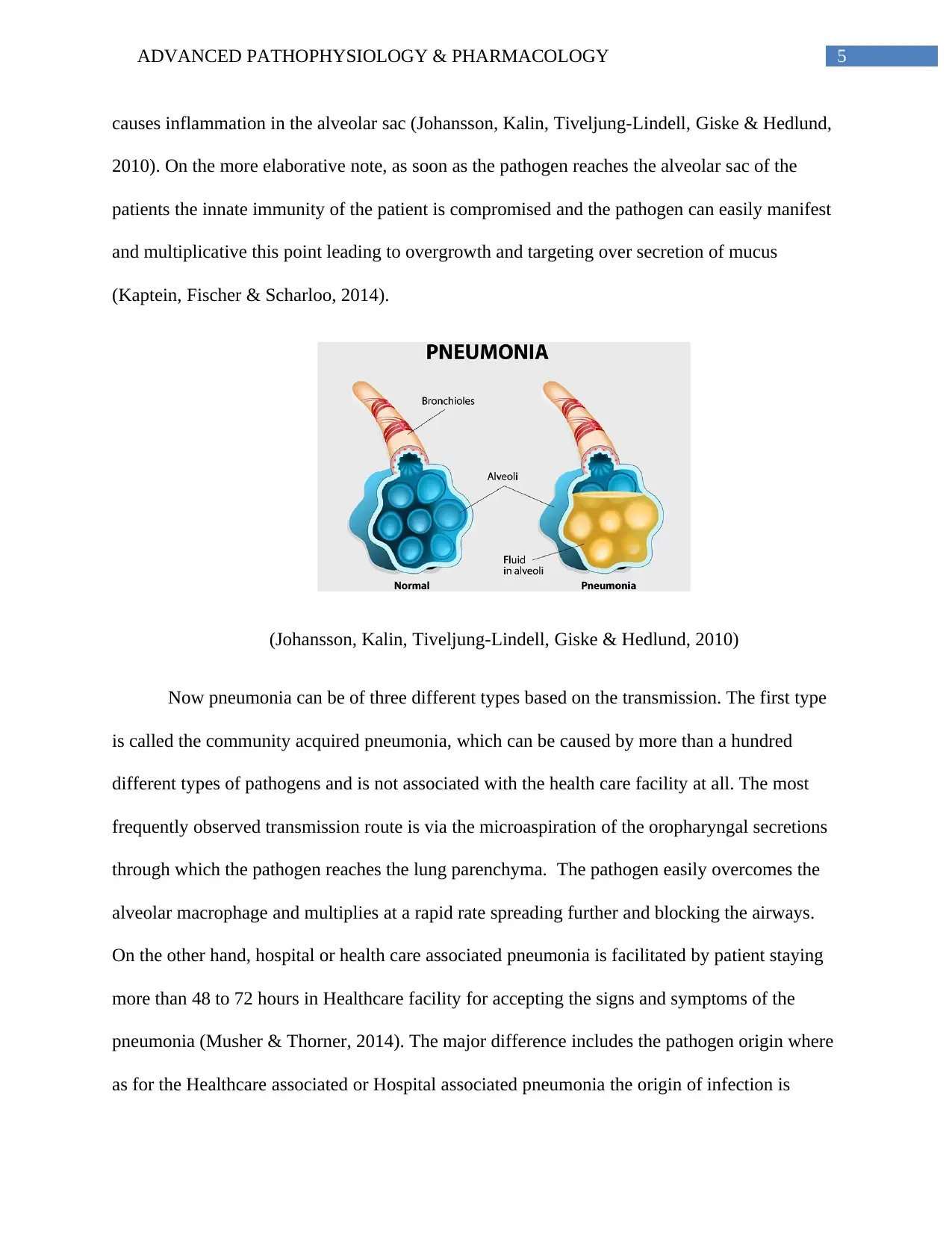
causes inflammation in the alveolar sac (Johansson, Kalin, Tiveljung-Lindell, Giske & Hedlund,
2010). On the more elaborative note, as soon as the pathogen reaches the alveolar sac of the
patients the innate immunity of the patient is compromised and the pathogen can easily manifest
and multiplicative this point leading to overgrowth and targeting over secretion of mucus
(Kaptein, Fischer & Scharloo, 2014).
(Johansson, Kalin, Tiveljung-Lindell, Giske & Hedlund, 2010)
Now pneumonia can be of three different types based on the transmission. The first type
is called the community acquired pneumonia, which can be caused by more than a hundred
different types of pathogens and is not associated with the health care facility at all. The most
frequently observed transmission route is via the microaspiration of the oropharyngal secretions
through which the pathogen reaches the lung parenchyma. The pathogen easily overcomes the
alveolar macrophage and multiplies at a rapid rate spreading further and blocking the airways.
On the other hand, hospital or health care associated pneumonia is facilitated by patient staying
more than 48 to 72 hours in Healthcare facility for accepting the signs and symptoms of the
pneumonia (Musher & Thorner, 2014). The major difference includes the pathogen origin where
as for the Healthcare associated or Hospital associated pneumonia the origin of infection is
causes inflammation in the alveolar sac (Johansson, Kalin, Tiveljung-Lindell, Giske & Hedlund,
2010). On the more elaborative note, as soon as the pathogen reaches the alveolar sac of the
patients the innate immunity of the patient is compromised and the pathogen can easily manifest
and multiplicative this point leading to overgrowth and targeting over secretion of mucus
(Kaptein, Fischer & Scharloo, 2014).
(Johansson, Kalin, Tiveljung-Lindell, Giske & Hedlund, 2010)
Now pneumonia can be of three different types based on the transmission. The first type
is called the community acquired pneumonia, which can be caused by more than a hundred
different types of pathogens and is not associated with the health care facility at all. The most
frequently observed transmission route is via the microaspiration of the oropharyngal secretions
through which the pathogen reaches the lung parenchyma. The pathogen easily overcomes the
alveolar macrophage and multiplies at a rapid rate spreading further and blocking the airways.
On the other hand, hospital or health care associated pneumonia is facilitated by patient staying
more than 48 to 72 hours in Healthcare facility for accepting the signs and symptoms of the
pneumonia (Musher & Thorner, 2014). The major difference includes the pathogen origin where
as for the Healthcare associated or Hospital associated pneumonia the origin of infection is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
bacterial rather than being viral and the microbial strain is often antibiotic resistant. Similarly in
case of healthcare associated pneumonia, the infection is facilitated by staying for a program
time of period in a community care in patient setting where the transmission on it is also
antibiotic resistant strains (Martin-Loeches et al., 2010).
Pharmacology
Salbutamol:
This is a beta 2 andrenergic receptor stimulator which performs bronchodilation in COPD. The
mechanism of action is by activating the adenylyl cyclase channel of the patient that triggers
overproduction of cyclic AMP. The increase in the concentration of cyclic AMP activates the
protein kinase which relaxes the bronchial tube and facilitates better air passage through the
airways and reduces airway resistance. The contraindication includes hypersensitivity reactions
such as urticaria, angioedema, rash and preexisting cardiac tachyarrhythmias as well. The side
effects are fine tremor, enhanced nervousness, palpitations, tachycardia, headache, muscle
cramps, hyperkalemia, and paradoxical bronchospasms. The nursing consideration for Robert
while administering salbutamol should be checking if he has any hypersensitivity to the
medication or if there are any tremors or palpitation. The nurse will have to be conscious about
arrhythmia, hypertension, hypothyroidism, convulsive disorders, and if the patient has been
taking any tricyclic antidepressants as well. The patient will have to be educated regarding the
side effects of this medication and regarding the dosage (Postma et al., 2015).
Budesonide or fomoterol fumarate dehydrate (symbicort):
It is the combination of two active components, budesonide which is a corticosteroid and
formoterol fumarate dihydrate which is a selective Beta 2 agonist. The mechanism of action of
bacterial rather than being viral and the microbial strain is often antibiotic resistant. Similarly in
case of healthcare associated pneumonia, the infection is facilitated by staying for a program
time of period in a community care in patient setting where the transmission on it is also
antibiotic resistant strains (Martin-Loeches et al., 2010).
Pharmacology
Salbutamol:
This is a beta 2 andrenergic receptor stimulator which performs bronchodilation in COPD. The
mechanism of action is by activating the adenylyl cyclase channel of the patient that triggers
overproduction of cyclic AMP. The increase in the concentration of cyclic AMP activates the
protein kinase which relaxes the bronchial tube and facilitates better air passage through the
airways and reduces airway resistance. The contraindication includes hypersensitivity reactions
such as urticaria, angioedema, rash and preexisting cardiac tachyarrhythmias as well. The side
effects are fine tremor, enhanced nervousness, palpitations, tachycardia, headache, muscle
cramps, hyperkalemia, and paradoxical bronchospasms. The nursing consideration for Robert
while administering salbutamol should be checking if he has any hypersensitivity to the
medication or if there are any tremors or palpitation. The nurse will have to be conscious about
arrhythmia, hypertension, hypothyroidism, convulsive disorders, and if the patient has been
taking any tricyclic antidepressants as well. The patient will have to be educated regarding the
side effects of this medication and regarding the dosage (Postma et al., 2015).
Budesonide or fomoterol fumarate dehydrate (symbicort):
It is the combination of two active components, budesonide which is a corticosteroid and
formoterol fumarate dihydrate which is a selective Beta 2 agonist. The mechanism of action of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
this medication is by reducing the inflammation of the airways of Robert and relaxing the
bronchial tubes. The contraindications include any allergic hypersensitivity reaction probability
in the patient and this particular medication it is not useful or beneficial in case of acute
exacerbation event. Side effects include body pain, cough, difficulty breathing, fever, headache,
muscle ache, chills, sneezing, sore throat, fatigue, stuffy or runny nose, and tightness of the
chest. In case of Robert the two nursing considerations for administration of this medication will
include hypersensitivity reaction and possibility of secondary infection requiring intensive
measures where this medication can resolve to decrement ill effects rather than positive effects.
Patient education for this medication will be the possible side effects and not to take this
particular medication in case of acute bronchospasm events. This medication also leads to
exceeding wheezing, the patient will also be educated to seek medical attention immediately in
case of acute asthmatic attack (File et al., 2010).
Tiotropium:
It is a long acting 24 hour anticholinergic, a very common medication used in chronic
obstructive pulmonary disorder. This is a muscarinic receptor agonist, which targets mainly M3
muscarinic receptors that are located in the bronchial airways and facilitate smooth muscle
relaxation and causes a bronchodilatory effect. The side effects are dry mouth and dizziness
along with renal problem such as difficulty in union eating and painful urination. This
medication is contraindicated for patients with closed angle glaucoma, blockage of urinary
bladder, enlarged prostate, chronic kidney diseases, anticholinergic quaternary allergies, and
allergies to ipratorium analogues (Barrera et al., 2016). The nursing consideration is halting
administration in case of angioedema and monitoring for anticholinergic effects in the patient.
Patient education for this medication includes educating the patient not to let the medication
this medication is by reducing the inflammation of the airways of Robert and relaxing the
bronchial tubes. The contraindications include any allergic hypersensitivity reaction probability
in the patient and this particular medication it is not useful or beneficial in case of acute
exacerbation event. Side effects include body pain, cough, difficulty breathing, fever, headache,
muscle ache, chills, sneezing, sore throat, fatigue, stuffy or runny nose, and tightness of the
chest. In case of Robert the two nursing considerations for administration of this medication will
include hypersensitivity reaction and possibility of secondary infection requiring intensive
measures where this medication can resolve to decrement ill effects rather than positive effects.
Patient education for this medication will be the possible side effects and not to take this
particular medication in case of acute bronchospasm events. This medication also leads to
exceeding wheezing, the patient will also be educated to seek medical attention immediately in
case of acute asthmatic attack (File et al., 2010).
Tiotropium:
It is a long acting 24 hour anticholinergic, a very common medication used in chronic
obstructive pulmonary disorder. This is a muscarinic receptor agonist, which targets mainly M3
muscarinic receptors that are located in the bronchial airways and facilitate smooth muscle
relaxation and causes a bronchodilatory effect. The side effects are dry mouth and dizziness
along with renal problem such as difficulty in union eating and painful urination. This
medication is contraindicated for patients with closed angle glaucoma, blockage of urinary
bladder, enlarged prostate, chronic kidney diseases, anticholinergic quaternary allergies, and
allergies to ipratorium analogues (Barrera et al., 2016). The nursing consideration is halting
administration in case of angioedema and monitoring for anticholinergic effects in the patient.
Patient education for this medication includes educating the patient not to let the medication
8ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
contact the eyes, educating him regarding this medication being once daily maintenance
treatment, withholding the drug and seeking immediate medical attention in case of swelling
around the face mouth or neck.
The physician has replaced budesonamide injection with tiotropium because researchers
are of the opinion that budosonamide leads to secondary infection of pneumonia and it is not
very useful for severe exercise session of chronic obstructive pulmonary disorders. As Robert
have already been suffering with community acquired pneumonia continuing this would have
been extremely harmful for him hence the doctor changed it for a much more effective
bronchodilator tiotropium.
Medication for pneumonia:
Levoflaxone:
It is a quinolone antibiotic, a very common antibiotic used for community acquired
pneumonia only of bacterial origin. The mechanism of action is facilitated by its bacteriocidal
activity that inhibits the growth of bacteria. The side effects of this medication include nausea,
diarrhea, headache, dizziness, lightheadedness, and sleeping problems (Musher & Thorner,
2014). The contraindications include hypersensitivity reaction, diabetes, and renal disorders.
While administering the medication the nurse will have to run medication should very slowly to
avoid any stinging that Robert may feel. The patient will have to be educated about possible side
effects of this medication and the patient should also be encouraged to take vitamin supplements
while taking this particular antibiotic as it can lead to nutrition deficiency and weakness.
contact the eyes, educating him regarding this medication being once daily maintenance
treatment, withholding the drug and seeking immediate medical attention in case of swelling
around the face mouth or neck.
The physician has replaced budesonamide injection with tiotropium because researchers
are of the opinion that budosonamide leads to secondary infection of pneumonia and it is not
very useful for severe exercise session of chronic obstructive pulmonary disorders. As Robert
have already been suffering with community acquired pneumonia continuing this would have
been extremely harmful for him hence the doctor changed it for a much more effective
bronchodilator tiotropium.
Medication for pneumonia:
Levoflaxone:
It is a quinolone antibiotic, a very common antibiotic used for community acquired
pneumonia only of bacterial origin. The mechanism of action is facilitated by its bacteriocidal
activity that inhibits the growth of bacteria. The side effects of this medication include nausea,
diarrhea, headache, dizziness, lightheadedness, and sleeping problems (Musher & Thorner,
2014). The contraindications include hypersensitivity reaction, diabetes, and renal disorders.
While administering the medication the nurse will have to run medication should very slowly to
avoid any stinging that Robert may feel. The patient will have to be educated about possible side
effects of this medication and the patient should also be encouraged to take vitamin supplements
while taking this particular antibiotic as it can lead to nutrition deficiency and weakness.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
Moxifloxacin:
It is another common antibiotic used to treat community acquired pneumonia and the
mechanism of action of this medication is facilitated by bacteriocidal activity. It is also a
quilonone antibiotic. The side effects of this kind of medication are also nausea, diarrhea,
dizziness, lightheadedness, headache, weakness, and insomnia. This medication is
contraindicated against any hypersensitivity reaction to quilonone derivatives, and this
medication is also contraindicated against diabetes cardiac problems hepatic diseases depression
nervous system diseases convulsions and seizures (Davydow, Hough, Levine, Langa &
Iwashyna, 2013). The nursing consideration for this medication will be to check if Robert has
any hypersensitivity reaction to quilonone derivatives and if patient has had a history of taking
blood thinners and Strontium until recently. Patient education will be for side effects of this
medication and possible drug interactions.
Ceftriaxone:
This particular medication is a cefalosporine which is a very common medication used
for elderly patients like Robert to treat bacterial infection such as pneumonia and its mechanism
of action is also bactericidal. Possible Side Effects that Robert may experience after taking his
medication includes bronchospasm, diarrhoea, nausea and vomiting (Barrera et al., 2016). This
medication is contraindicated for calcium ceftriaxone interaction or any hypersensitivity or
allergic reaction to it. While administering this medication the nurse will have to ensure that
Robert does not have bronchospasm or sudden shortness of breath and he does not develop any
allergic reaction. He will need to be educated regarding the possible precautions to take and the
possible side effects and along with that Robert will also needed to be educated to seek attention
if any adverse reaction develops.
Moxifloxacin:
It is another common antibiotic used to treat community acquired pneumonia and the
mechanism of action of this medication is facilitated by bacteriocidal activity. It is also a
quilonone antibiotic. The side effects of this kind of medication are also nausea, diarrhea,
dizziness, lightheadedness, headache, weakness, and insomnia. This medication is
contraindicated against any hypersensitivity reaction to quilonone derivatives, and this
medication is also contraindicated against diabetes cardiac problems hepatic diseases depression
nervous system diseases convulsions and seizures (Davydow, Hough, Levine, Langa &
Iwashyna, 2013). The nursing consideration for this medication will be to check if Robert has
any hypersensitivity reaction to quilonone derivatives and if patient has had a history of taking
blood thinners and Strontium until recently. Patient education will be for side effects of this
medication and possible drug interactions.
Ceftriaxone:
This particular medication is a cefalosporine which is a very common medication used
for elderly patients like Robert to treat bacterial infection such as pneumonia and its mechanism
of action is also bactericidal. Possible Side Effects that Robert may experience after taking his
medication includes bronchospasm, diarrhoea, nausea and vomiting (Barrera et al., 2016). This
medication is contraindicated for calcium ceftriaxone interaction or any hypersensitivity or
allergic reaction to it. While administering this medication the nurse will have to ensure that
Robert does not have bronchospasm or sudden shortness of breath and he does not develop any
allergic reaction. He will need to be educated regarding the possible precautions to take and the
possible side effects and along with that Robert will also needed to be educated to seek attention
if any adverse reaction develops.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
Psychosocial:
Elderly patient population with chronic disorders have been reported to be twice as likely
to suffer from depression in psychiatric impairments. In this case Robert had been suffering from
two chronic health conditions, COPD and pneumonia and these health conditions are associated
with various restrictions and suffering which could have a negative impact at his psyche
(Davydow, Hough, Levine, Langa & Iwashyna, 2013). Robert has stated that he is anxious about
how his prolonged hospitalization would affect his wife as she would be left all alone and
devastated to see him suffering. Hence, the anxiety and stress can also lead to detrimental impact
on the psychological state of the patient.
In this case, the nursing professional will have to establish and therapeutic relationship
with the patient and engage him effective communication to help him feel better and understand
the depth of the psychological troubles he might have. According to the NMBA practice
standards, therapeutic relationship provides the patient with communicational comfort and a
sense of being valued which enhances their emotional and spiritual health and helps them share
their grievances effectively. The nurse will have to commence the patient on psychotherapies
like cognitive behavioral therapy and mindfulness based therapies with collaboration with
psychotherapists to help him cope with stress, anxiety and depression (Hynninen, Bjerke,
Pallesen, Bakke & Nordhus, 2010). His wife must be included in the entire care planning
procedure so that she is not anxious and so that Robert is not distressed with thoughts of how his
wife is coping.
Psychosocial:
Elderly patient population with chronic disorders have been reported to be twice as likely
to suffer from depression in psychiatric impairments. In this case Robert had been suffering from
two chronic health conditions, COPD and pneumonia and these health conditions are associated
with various restrictions and suffering which could have a negative impact at his psyche
(Davydow, Hough, Levine, Langa & Iwashyna, 2013). Robert has stated that he is anxious about
how his prolonged hospitalization would affect his wife as she would be left all alone and
devastated to see him suffering. Hence, the anxiety and stress can also lead to detrimental impact
on the psychological state of the patient.
In this case, the nursing professional will have to establish and therapeutic relationship
with the patient and engage him effective communication to help him feel better and understand
the depth of the psychological troubles he might have. According to the NMBA practice
standards, therapeutic relationship provides the patient with communicational comfort and a
sense of being valued which enhances their emotional and spiritual health and helps them share
their grievances effectively. The nurse will have to commence the patient on psychotherapies
like cognitive behavioral therapy and mindfulness based therapies with collaboration with
psychotherapists to help him cope with stress, anxiety and depression (Hynninen, Bjerke,
Pallesen, Bakke & Nordhus, 2010). His wife must be included in the entire care planning
procedure so that she is not anxious and so that Robert is not distressed with thoughts of how his
wife is coping.
11ADVANCED PATHOPHYSIOLOGY & PHARMACOLOGY
References:
Agusti, A. (2014). The path to personalised medicine in COPD. Thorax, vol 69(9), pp 857-864.
doi: 10.1136/thoraxjnl-2014-205507
Agustí, A., Edwards, L. D., Rennard, S. I., MacNee, W., Tal-Singer, R., Miller, B. E., ... & Crim,
C. (2012). Persistent systemic inflammation is associated with poor clinical outcomes in
COPD: a novel phenotype. PloS one, vol 7(5), e37483. Retrieved from
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0037483
Albert, R. K., Connett, J., Bailey, W. C., Casaburi, R., Cooper Jr, J. A. D., Criner, G. J., ... &
Make, B. (2011). Azithromycin for prevention of exacerbations of COPD. New England
Journal of Medicine, 365(8), pp 689-698. doi: 10.1056/NEJMoa1104623.
Almagro, P., Cabrera, F. J., Diez, J., Boixeda, R., Ortiz, M. B. A., Murio, C., & Soriano, J. B.
(2012). Comorbidities and short-term prognosis in patients hospitalized for acute
exacerbation of COPD: the EPOC en Servicios de medicina interna (ESMI)
study. Chest, vol 142(5), pp 1126-1133. Retrieved from
http://journal.chestnet.org/article/S0012-3692(12)60613-8/abstract
Barrera, C. M., Mykietiuk, A., Metev, H., Nitu, M. F., Karimjee, N., Doreski, P. A., ... & Van
Rensburg, D. J. (2016). Efficacy and safety of oral solithromycin versus oral
moxifloxacin for treatment of community-acquired bacterial pneumonia: a global,
double-blind, multicentre, randomised, active-controlled, non-inferiority trial
(SOLITAIRE-ORAL). The Lancet Infectious Diseases, 16(4), 421-430.
doi.org/10.1016/S1473-3099(16)00017-7
References:
Agusti, A. (2014). The path to personalised medicine in COPD. Thorax, vol 69(9), pp 857-864.
doi: 10.1136/thoraxjnl-2014-205507
Agustí, A., Edwards, L. D., Rennard, S. I., MacNee, W., Tal-Singer, R., Miller, B. E., ... & Crim,
C. (2012). Persistent systemic inflammation is associated with poor clinical outcomes in
COPD: a novel phenotype. PloS one, vol 7(5), e37483. Retrieved from
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0037483
Albert, R. K., Connett, J., Bailey, W. C., Casaburi, R., Cooper Jr, J. A. D., Criner, G. J., ... &
Make, B. (2011). Azithromycin for prevention of exacerbations of COPD. New England
Journal of Medicine, 365(8), pp 689-698. doi: 10.1056/NEJMoa1104623.
Almagro, P., Cabrera, F. J., Diez, J., Boixeda, R., Ortiz, M. B. A., Murio, C., & Soriano, J. B.
(2012). Comorbidities and short-term prognosis in patients hospitalized for acute
exacerbation of COPD: the EPOC en Servicios de medicina interna (ESMI)
study. Chest, vol 142(5), pp 1126-1133. Retrieved from
http://journal.chestnet.org/article/S0012-3692(12)60613-8/abstract
Barrera, C. M., Mykietiuk, A., Metev, H., Nitu, M. F., Karimjee, N., Doreski, P. A., ... & Van
Rensburg, D. J. (2016). Efficacy and safety of oral solithromycin versus oral
moxifloxacin for treatment of community-acquired bacterial pneumonia: a global,
double-blind, multicentre, randomised, active-controlled, non-inferiority trial
(SOLITAIRE-ORAL). The Lancet Infectious Diseases, 16(4), 421-430.
doi.org/10.1016/S1473-3099(16)00017-7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




