NURBN 2012 - Betsy Case Study: Nursing Practice 3 Report
VerifiedAdded on 2023/01/19
|10
|3051
|26
Report
AI Summary
This report provides a comprehensive analysis of the Betsy case study, focusing on a patient presenting with potential acute coronary syndrome. The introduction sets the stage for exploring the rationale behind ECG testing, followed by a detailed examination of the pathophysiology of angina, including unstable and stable angina, STEMI, and NSTEMI. The report identifies specific risk factors relevant to Betsy's case, excluding age and gender, and analyzes the ECG results, interpreting findings such as inverted T waves and ST elevation. Central findings leading to an ACS diagnosis are discussed, along with the mechanisms of action, nursing considerations, and side effects of various drugs like GTN, diltiazem, and pravastatin. Furthermore, it explains the roles of aspirin, ticagrelor, and morphine in managing cardiac patients, including potential benefits and drawbacks. The report concludes by addressing the link between increased risks of depression and chronic illness, providing a holistic view of the patient's condition and care. The analysis is well-supported by current research and literature using APA referencing.

Running head: BETSY CASE STUDY
1
Betsy case study
Student’s Name
University
1
Betsy case study
Student’s Name
University
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BETSY CASE STUDY
2
Betsy case study
Introduction
The acute coronary syndrome is one of the challenges in old age since as people grow
older, the complication of heart problem keeps on increasing. This means that patients who are
presented to the hospital with this condition have to be verified to determine the nature of the
condition that they have (Osler, et al., 2016). Patients with a heart problem can develop different
conditions that are associated with the problem like angina which is measured through ECG.
Question 1: Rationale for ECG
ECG is a simple test for checking the electoral activity and the rhythm of the heart
through assessing the sensors attached on the skin to detect electoral activity each time the heart
beats. This means that through measuring electoral activity, irregular heartbeat and any other
complications associated with the heart to develop early interventions (James, et al., 2015). Thus
the reason why this test was ordered is to develop an early diagnosis of any heart attack that may
be in progress despite the fact that Betsy was not feeling any chest pain. The fact that she is
feeling shortness of breath is a red flag for the test so that practitioners can be adequately
prepared for any challenge that may arise from the condition of the patient.
Question 2
2a. The pathophysiology of angina
Chest heaviness or angina is a result of shortness of breath that makes it difficult for the
patient to breathe well. This is due to the reduced amount of blood that reaches the heart thus
reducing the amount of oxygen that the heart receives which in turn damages the endothelium
(Kumar & Cannon, 2011). Thus cholesterol, fats, and lipoprotein accumulate in the arteries
which leads to the formation of fatty acids in the artery that produces an extracellular matrix that
2
Betsy case study
Introduction
The acute coronary syndrome is one of the challenges in old age since as people grow
older, the complication of heart problem keeps on increasing. This means that patients who are
presented to the hospital with this condition have to be verified to determine the nature of the
condition that they have (Osler, et al., 2016). Patients with a heart problem can develop different
conditions that are associated with the problem like angina which is measured through ECG.
Question 1: Rationale for ECG
ECG is a simple test for checking the electoral activity and the rhythm of the heart
through assessing the sensors attached on the skin to detect electoral activity each time the heart
beats. This means that through measuring electoral activity, irregular heartbeat and any other
complications associated with the heart to develop early interventions (James, et al., 2015). Thus
the reason why this test was ordered is to develop an early diagnosis of any heart attack that may
be in progress despite the fact that Betsy was not feeling any chest pain. The fact that she is
feeling shortness of breath is a red flag for the test so that practitioners can be adequately
prepared for any challenge that may arise from the condition of the patient.
Question 2
2a. The pathophysiology of angina
Chest heaviness or angina is a result of shortness of breath that makes it difficult for the
patient to breathe well. This is due to the reduced amount of blood that reaches the heart thus
reducing the amount of oxygen that the heart receives which in turn damages the endothelium
(Kumar & Cannon, 2011). Thus cholesterol, fats, and lipoprotein accumulate in the arteries
which leads to the formation of fatty acids in the artery that produces an extracellular matrix that
BETSY CASE STUDY
3
forms atherosclerotic plaque that makes the luminal space narrow. Unstable angina or acute
coronary syndrome is characterized by unexpected pain that mostly occurs when one is resting
due to reduced blood flow from coronary arteries that lead to building up of fats that may rupture
causing injury or sometimes lead to blood clotting that eventually blocks the flow of blood. On
the other hand, stable angina pathophysiology is similar to unstable angina since it is also based
on a lack of enough blood flow due to narrowed and blocked arteries (Cheung & Li, 2012). It is
characterized by squeezing and uncomfortable pressure in the center of the chest but this can
extend to discomfort in the jaw, shoulder or neck. The difference with stable angina is that it is
predictable and it is easy for the patient to monitor the signs. In most cases, the signs arise as a
result of physical activity that leads to the need for more blood in the heart.
According to Babu, Haneef, Joseph, & Noone (2010) STEMI pathophysiology is based
on the buildup of fats and blocking of arteries which leads to what is called a classic heart attack.
Here the heart is damaged due to complete or near rapture of the coronary artery that makes the
heart weak and increases the complications of the heart. This means that STEMI is a ruptured
plaque that results from blocking of arteries. NSTEMI is a minor complication of the heart that is
based on blocked or obstructed coronary artery causing partial obstruction the major artery. This
means that NSTEMI has lesser effects on the heart. From the four conditions what is common in
all of them is the fact that they are all related to blockage of arteries which leads to reduced
blood flow. However, the nature of the complication depends on the signs and symptoms that the
patient is feeling.
2b. Risk factors specific to Betsy (not including age or gender) that increase her risk of
Acute Coronary Syndrome
Hypertension and type 2 Diabetes Mellitus
3
forms atherosclerotic plaque that makes the luminal space narrow. Unstable angina or acute
coronary syndrome is characterized by unexpected pain that mostly occurs when one is resting
due to reduced blood flow from coronary arteries that lead to building up of fats that may rupture
causing injury or sometimes lead to blood clotting that eventually blocks the flow of blood. On
the other hand, stable angina pathophysiology is similar to unstable angina since it is also based
on a lack of enough blood flow due to narrowed and blocked arteries (Cheung & Li, 2012). It is
characterized by squeezing and uncomfortable pressure in the center of the chest but this can
extend to discomfort in the jaw, shoulder or neck. The difference with stable angina is that it is
predictable and it is easy for the patient to monitor the signs. In most cases, the signs arise as a
result of physical activity that leads to the need for more blood in the heart.
According to Babu, Haneef, Joseph, & Noone (2010) STEMI pathophysiology is based
on the buildup of fats and blocking of arteries which leads to what is called a classic heart attack.
Here the heart is damaged due to complete or near rapture of the coronary artery that makes the
heart weak and increases the complications of the heart. This means that STEMI is a ruptured
plaque that results from blocking of arteries. NSTEMI is a minor complication of the heart that is
based on blocked or obstructed coronary artery causing partial obstruction the major artery. This
means that NSTEMI has lesser effects on the heart. From the four conditions what is common in
all of them is the fact that they are all related to blockage of arteries which leads to reduced
blood flow. However, the nature of the complication depends on the signs and symptoms that the
patient is feeling.
2b. Risk factors specific to Betsy (not including age or gender) that increase her risk of
Acute Coronary Syndrome
Hypertension and type 2 Diabetes Mellitus
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BETSY CASE STUDY
4
3. ECG analysis
From the ECG Betsy has a normal heart rate, rhythm, PR/P wave. This means that she
does not present a higher risk of an attack based on the fact that QTc is normal and the ST/T
analysis shows an inverted T wave I, II, III and Avf, the V4-V5.ST elevation in Avr>1mm. My
interpretation of these results we can assume that the patient may be having an inferolateral
NSTEMI due to the t-wave inversion that can be described as fitting within an anatomical
territory and there could be an ischemic chest pain that is developing slowly thus the reason why
Betsy has not reported any angina. Further, Begg (2016) adds that from the ST elevation in aVR.
suggests that the left main occlusion may be affected which calls for the need to analyze the
results further with a cardiologist so that Percutaneous coronary intervention can be planned.
This will address the challenge being faced by the patient by ensuring that the narrowed arteries
are treated.
Question 4: Central findings that potentially lead to a diagnosis of Acute Coronary
Syndrome
Acute coronary syndromes describe the blockage of arteries that reduces blood supply to
the heart. The condition ranges from unstable angina to irreversible cell death that makes the
patient feel the signs. In most cases, ECG tests are used to measure electromagnetic
abnormalities in the patient and determine the onset or the presence of this problem. From the
signs that Betsy presents one finding that shows she may be having this problem is the T-wave
tenting or inversion. In normal ECG measures, the wave is supposed to be in the same direction
as the QRS and is asymmetric with the first half moving slowly (Jheeta, Narayan, & Krasemann,
2014). Thus Betsy presents an inverted lead of aVR which shows that there is a problem with her
heart. The second sign is the ST-segment elevation which is associated with the rapture of an
4
3. ECG analysis
From the ECG Betsy has a normal heart rate, rhythm, PR/P wave. This means that she
does not present a higher risk of an attack based on the fact that QTc is normal and the ST/T
analysis shows an inverted T wave I, II, III and Avf, the V4-V5.ST elevation in Avr>1mm. My
interpretation of these results we can assume that the patient may be having an inferolateral
NSTEMI due to the t-wave inversion that can be described as fitting within an anatomical
territory and there could be an ischemic chest pain that is developing slowly thus the reason why
Betsy has not reported any angina. Further, Begg (2016) adds that from the ST elevation in aVR.
suggests that the left main occlusion may be affected which calls for the need to analyze the
results further with a cardiologist so that Percutaneous coronary intervention can be planned.
This will address the challenge being faced by the patient by ensuring that the narrowed arteries
are treated.
Question 4: Central findings that potentially lead to a diagnosis of Acute Coronary
Syndrome
Acute coronary syndromes describe the blockage of arteries that reduces blood supply to
the heart. The condition ranges from unstable angina to irreversible cell death that makes the
patient feel the signs. In most cases, ECG tests are used to measure electromagnetic
abnormalities in the patient and determine the onset or the presence of this problem. From the
signs that Betsy presents one finding that shows she may be having this problem is the T-wave
tenting or inversion. In normal ECG measures, the wave is supposed to be in the same direction
as the QRS and is asymmetric with the first half moving slowly (Jheeta, Narayan, & Krasemann,
2014). Thus Betsy presents an inverted lead of aVR which shows that there is a problem with her
heart. The second sign is the ST-segment elevation which is associated with the rapture of an
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BETSY CASE STUDY
5
unstable atheroma plaque which may be due to occlusion of an epicardial artery. Thus the results
show that Betsy has signs of the acute coronary syndrome. The last sign that Betsy shows is
angina pectoris or chest discomfort that has been witnessed by the patient especially when she
came from the bathroom. This is due to the myocardial oxygen demand and supply to the heart
which shows the signs of the acute coronary syndrome.
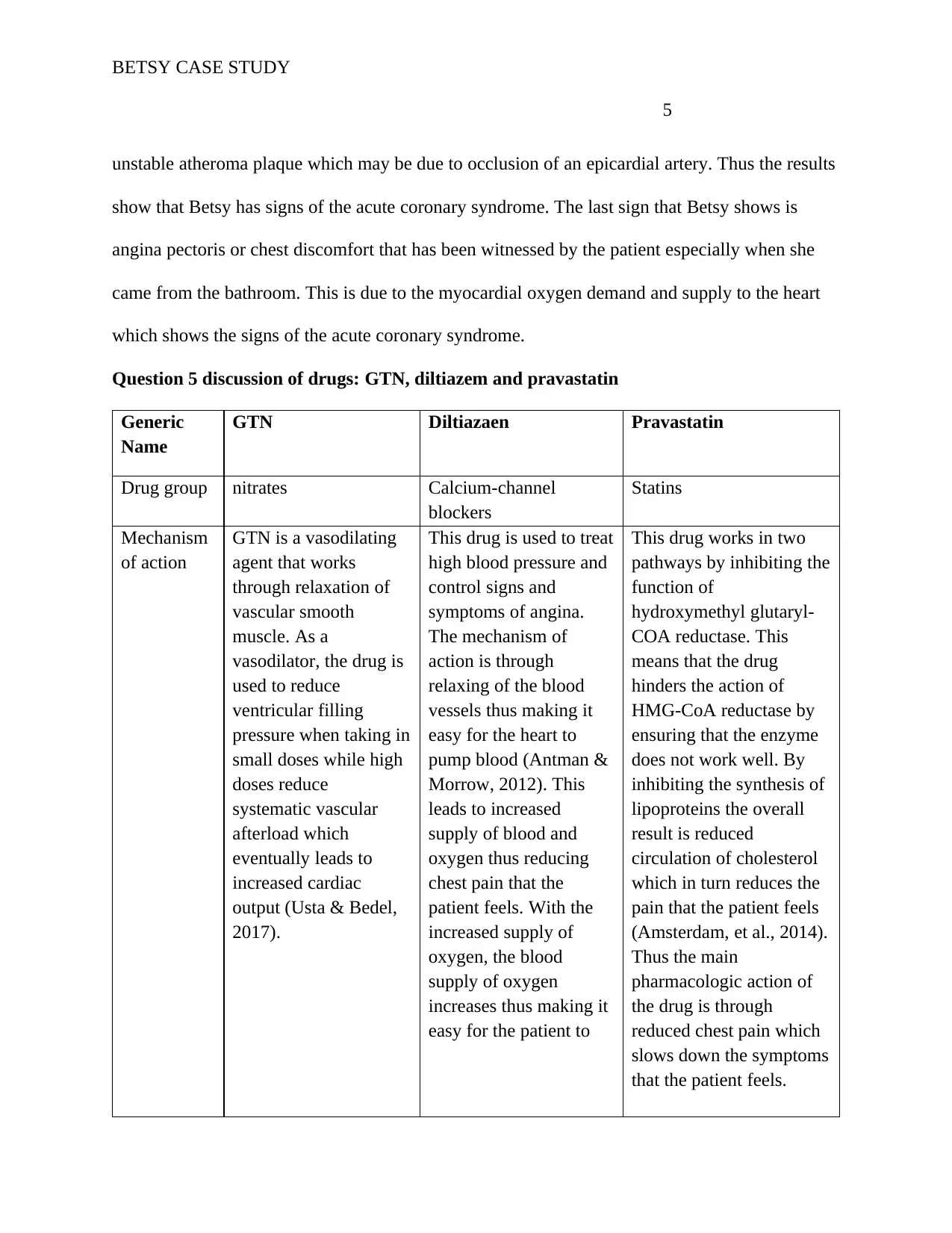
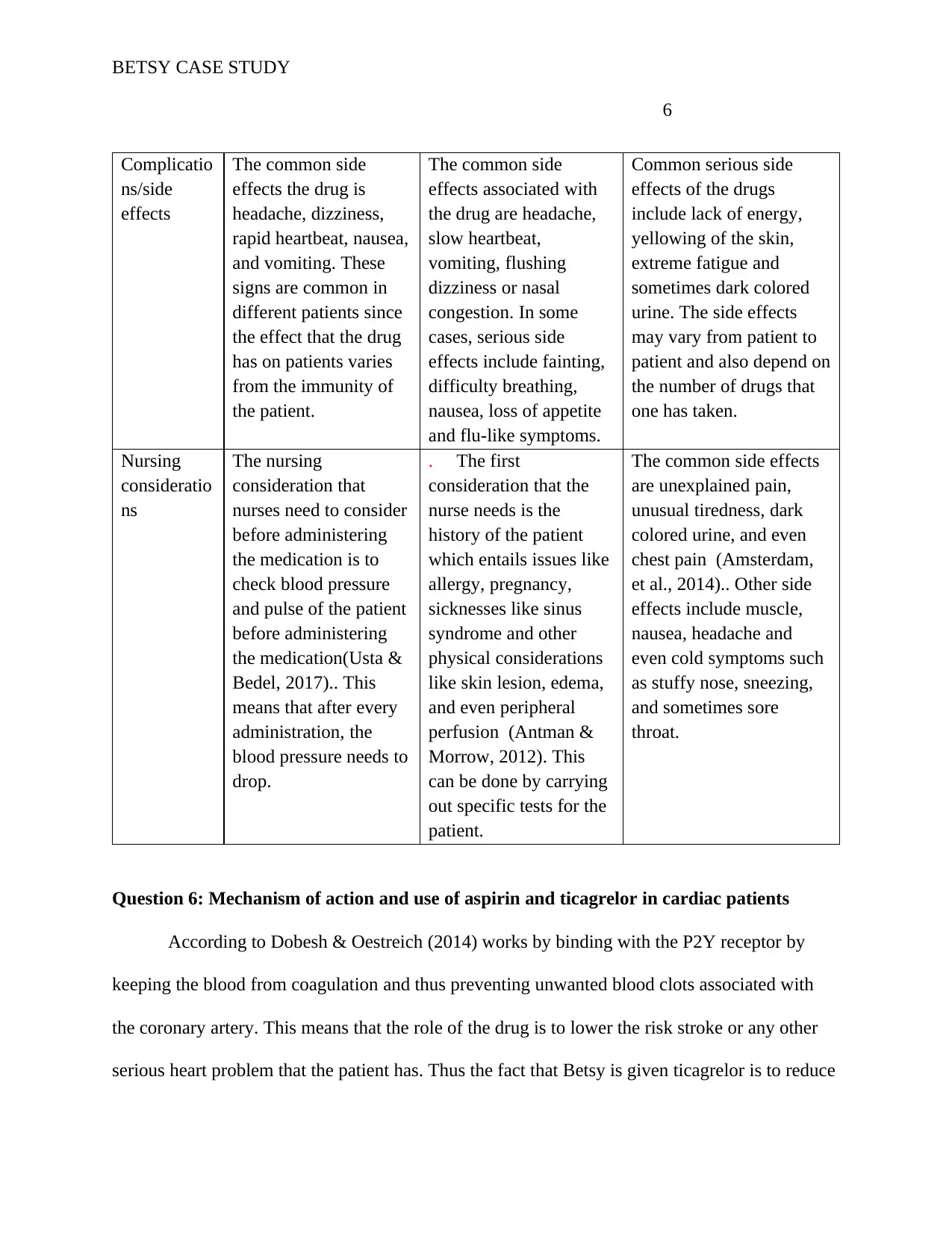
Question 5 discussion of drugs: GTN, diltiazem and pravastatin
Generic
Name
GTN Diltiazaen Pravastatin
Drug group nitrates Calcium-channel
blockers
Statins
Mechanism
of action
GTN is a vasodilating
agent that works
through relaxation of
vascular smooth
muscle. As a
vasodilator, the drug is
used to reduce
ventricular filling
pressure when taking in
small doses while high
doses reduce
systematic vascular
afterload which
eventually leads to
increased cardiac
output (Usta & Bedel,
2017).
This drug is used to treat
high blood pressure and
control signs and
symptoms of angina.
The mechanism of
action is through
relaxing of the blood
vessels thus making it
easy for the heart to
pump blood (Antman &
Morrow, 2012). This
leads to increased
supply of blood and
oxygen thus reducing
chest pain that the
patient feels. With the
increased supply of
oxygen, the blood
supply of oxygen
increases thus making it
easy for the patient to
This drug works in two
pathways by inhibiting the
function of
hydroxymethyl glutaryl-
COA reductase. This
means that the drug
hinders the action of
HMG-CoA reductase by
ensuring that the enzyme
does not work well. By
inhibiting the synthesis of
lipoproteins the overall
result is reduced
circulation of cholesterol
which in turn reduces the
pain that the patient feels
(Amsterdam, et al., 2014).
Thus the main
pharmacologic action of
the drug is through
reduced chest pain which
slows down the symptoms
that the patient feels.
5
unstable atheroma plaque which may be due to occlusion of an epicardial artery. Thus the results
show that Betsy has signs of the acute coronary syndrome. The last sign that Betsy shows is
angina pectoris or chest discomfort that has been witnessed by the patient especially when she
came from the bathroom. This is due to the myocardial oxygen demand and supply to the heart
which shows the signs of the acute coronary syndrome.
Question 5 discussion of drugs: GTN, diltiazem and pravastatin
Generic
Name
GTN Diltiazaen Pravastatin
Drug group nitrates Calcium-channel
blockers
Statins
Mechanism
of action
GTN is a vasodilating
agent that works
through relaxation of
vascular smooth
muscle. As a
vasodilator, the drug is
used to reduce
ventricular filling
pressure when taking in
small doses while high
doses reduce
systematic vascular
afterload which
eventually leads to
increased cardiac
output (Usta & Bedel,
2017).
This drug is used to treat
high blood pressure and
control signs and
symptoms of angina.
The mechanism of
action is through
relaxing of the blood
vessels thus making it
easy for the heart to
pump blood (Antman &
Morrow, 2012). This
leads to increased
supply of blood and
oxygen thus reducing
chest pain that the
patient feels. With the
increased supply of
oxygen, the blood
supply of oxygen
increases thus making it
easy for the patient to
This drug works in two
pathways by inhibiting the
function of
hydroxymethyl glutaryl-
COA reductase. This
means that the drug
hinders the action of
HMG-CoA reductase by
ensuring that the enzyme
does not work well. By
inhibiting the synthesis of
lipoproteins the overall
result is reduced
circulation of cholesterol
which in turn reduces the
pain that the patient feels
(Amsterdam, et al., 2014).
Thus the main
pharmacologic action of
the drug is through
reduced chest pain which
slows down the symptoms
that the patient feels.
BETSY CASE STUDY
6
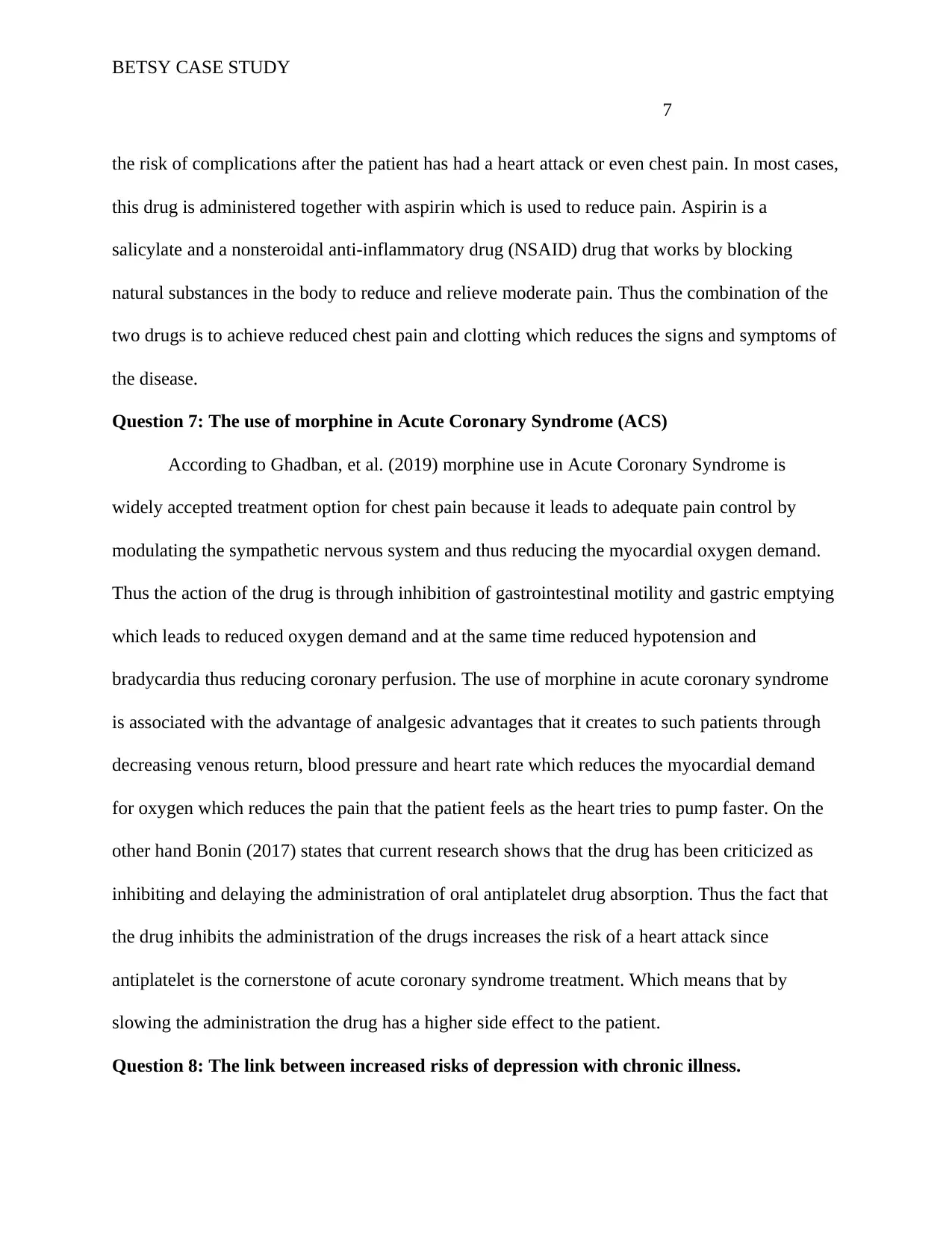
Complicatio
ns/side
effects
The common side
effects the drug is
headache, dizziness,
rapid heartbeat, nausea,
and vomiting. These
signs are common in
different patients since
the effect that the drug
has on patients varies
from the immunity of
the patient.
The common side
effects associated with
the drug are headache,
slow heartbeat,
vomiting, flushing
dizziness or nasal
congestion. In some
cases, serious side
effects include fainting,
difficulty breathing,
nausea, loss of appetite
and flu-like symptoms.
Common serious side
effects of the drugs
include lack of energy,
yellowing of the skin,
extreme fatigue and
sometimes dark colored
urine. The side effects
may vary from patient to
patient and also depend on
the number of drugs that
one has taken.
Nursing
consideratio
ns
The nursing
consideration that
nurses need to consider
before administering
the medication is to
check blood pressure
and pulse of the patient
before administering
the medication(Usta &
Bedel, 2017).. This
means that after every
administration, the
blood pressure needs to
drop.
. The first
consideration that the
nurse needs is the
history of the patient
which entails issues like
allergy, pregnancy,
sicknesses like sinus
syndrome and other
physical considerations
like skin lesion, edema,
and even peripheral
perfusion (Antman &
Morrow, 2012). This
can be done by carrying
out specific tests for the
patient.
The common side effects
are unexplained pain,
unusual tiredness, dark
colored urine, and even
chest pain (Amsterdam,
et al., 2014).. Other side
effects include muscle,
nausea, headache and
even cold symptoms such
as stuffy nose, sneezing,
and sometimes sore
throat.
Question 6: Mechanism of action and use of aspirin and ticagrelor in cardiac patients
According to Dobesh & Oestreich (2014) works by binding with the P2Y receptor by
keeping the blood from coagulation and thus preventing unwanted blood clots associated with
the coronary artery. This means that the role of the drug is to lower the risk stroke or any other
serious heart problem that the patient has. Thus the fact that Betsy is given ticagrelor is to reduce
6
Complicatio
ns/side
effects
The common side
effects the drug is
headache, dizziness,
rapid heartbeat, nausea,
and vomiting. These
signs are common in
different patients since
the effect that the drug
has on patients varies
from the immunity of
the patient.
The common side
effects associated with
the drug are headache,
slow heartbeat,
vomiting, flushing
dizziness or nasal
congestion. In some
cases, serious side
effects include fainting,
difficulty breathing,
nausea, loss of appetite
and flu-like symptoms.
Common serious side
effects of the drugs
include lack of energy,
yellowing of the skin,
extreme fatigue and
sometimes dark colored
urine. The side effects
may vary from patient to
patient and also depend on
the number of drugs that
one has taken.
Nursing
consideratio
ns
The nursing
consideration that
nurses need to consider
before administering
the medication is to
check blood pressure
and pulse of the patient
before administering
the medication(Usta &
Bedel, 2017).. This
means that after every
administration, the
blood pressure needs to
drop.
. The first
consideration that the
nurse needs is the
history of the patient
which entails issues like
allergy, pregnancy,
sicknesses like sinus
syndrome and other
physical considerations
like skin lesion, edema,
and even peripheral
perfusion (Antman &
Morrow, 2012). This
can be done by carrying
out specific tests for the
patient.
The common side effects
are unexplained pain,
unusual tiredness, dark
colored urine, and even
chest pain (Amsterdam,
et al., 2014).. Other side
effects include muscle,
nausea, headache and
even cold symptoms such
as stuffy nose, sneezing,
and sometimes sore
throat.
Question 6: Mechanism of action and use of aspirin and ticagrelor in cardiac patients
According to Dobesh & Oestreich (2014) works by binding with the P2Y receptor by
keeping the blood from coagulation and thus preventing unwanted blood clots associated with
the coronary artery. This means that the role of the drug is to lower the risk stroke or any other
serious heart problem that the patient has. Thus the fact that Betsy is given ticagrelor is to reduce
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BETSY CASE STUDY
7
the risk of complications after the patient has had a heart attack or even chest pain. In most cases,
this drug is administered together with aspirin which is used to reduce pain. Aspirin is a
salicylate and a nonsteroidal anti-inflammatory drug (NSAID) drug that works by blocking
natural substances in the body to reduce and relieve moderate pain. Thus the combination of the
two drugs is to achieve reduced chest pain and clotting which reduces the signs and symptoms of
the disease.
Question 7: The use of morphine in Acute Coronary Syndrome (ACS)
According to Ghadban, et al. (2019) morphine use in Acute Coronary Syndrome is
widely accepted treatment option for chest pain because it leads to adequate pain control by
modulating the sympathetic nervous system and thus reducing the myocardial oxygen demand.
Thus the action of the drug is through inhibition of gastrointestinal motility and gastric emptying
which leads to reduced oxygen demand and at the same time reduced hypotension and
bradycardia thus reducing coronary perfusion. The use of morphine in acute coronary syndrome
is associated with the advantage of analgesic advantages that it creates to such patients through
decreasing venous return, blood pressure and heart rate which reduces the myocardial demand
for oxygen which reduces the pain that the patient feels as the heart tries to pump faster. On the
other hand Bonin (2017) states that current research shows that the drug has been criticized as
inhibiting and delaying the administration of oral antiplatelet drug absorption. Thus the fact that
the drug inhibits the administration of the drugs increases the risk of a heart attack since
antiplatelet is the cornerstone of acute coronary syndrome treatment. Which means that by
slowing the administration the drug has a higher side effect to the patient.
Question 8: The link between increased risks of depression with chronic illness.
7
the risk of complications after the patient has had a heart attack or even chest pain. In most cases,
this drug is administered together with aspirin which is used to reduce pain. Aspirin is a
salicylate and a nonsteroidal anti-inflammatory drug (NSAID) drug that works by blocking
natural substances in the body to reduce and relieve moderate pain. Thus the combination of the
two drugs is to achieve reduced chest pain and clotting which reduces the signs and symptoms of
the disease.
Question 7: The use of morphine in Acute Coronary Syndrome (ACS)
According to Ghadban, et al. (2019) morphine use in Acute Coronary Syndrome is
widely accepted treatment option for chest pain because it leads to adequate pain control by
modulating the sympathetic nervous system and thus reducing the myocardial oxygen demand.
Thus the action of the drug is through inhibition of gastrointestinal motility and gastric emptying
which leads to reduced oxygen demand and at the same time reduced hypotension and
bradycardia thus reducing coronary perfusion. The use of morphine in acute coronary syndrome
is associated with the advantage of analgesic advantages that it creates to such patients through
decreasing venous return, blood pressure and heart rate which reduces the myocardial demand
for oxygen which reduces the pain that the patient feels as the heart tries to pump faster. On the
other hand Bonin (2017) states that current research shows that the drug has been criticized as
inhibiting and delaying the administration of oral antiplatelet drug absorption. Thus the fact that
the drug inhibits the administration of the drugs increases the risk of a heart attack since
antiplatelet is the cornerstone of acute coronary syndrome treatment. Which means that by
slowing the administration the drug has a higher side effect to the patient.
Question 8: The link between increased risks of depression with chronic illness.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BETSY CASE STUDY
8
Figueiredo, Silva, Pereira, & Oliveira (2017) study reported that there are higher
increases in depression are associated with the diagnosis of acute coronary syndrome due to the
fear of the effects of the condition. Thus most patients develop depression syndromes when
diagnosed with the condition which becomes one of the factors for the mortality rate of the
people with the acute coronary syndrome. The fact that the condition is manageable means that
depression increases the effects of the disease, repeated attacks and even the response to
medication. Thus there is a need to address the issue of depression in these population.
Conclusion
The acute coronary syndrome is one of the challenges that older people experience due to defects
in their arterial system from the accumulation of fatty acids thus leading to the blockage and
narrowing of arteries making it difficult for the heart to receive in blood circulation thus the need
for the increased heartbeat. Therefore, the acute coronary syndrome is associated with many
challenges that patients have to be assisted to manage the condition thus making it easy for the
symptoms to be managed and reduce the fatal effects of the condition.
8
Figueiredo, Silva, Pereira, & Oliveira (2017) study reported that there are higher
increases in depression are associated with the diagnosis of acute coronary syndrome due to the
fear of the effects of the condition. Thus most patients develop depression syndromes when
diagnosed with the condition which becomes one of the factors for the mortality rate of the
people with the acute coronary syndrome. The fact that the condition is manageable means that
depression increases the effects of the disease, repeated attacks and even the response to
medication. Thus there is a need to address the issue of depression in these population.
Conclusion
The acute coronary syndrome is one of the challenges that older people experience due to defects
in their arterial system from the accumulation of fatty acids thus leading to the blockage and
narrowing of arteries making it difficult for the heart to receive in blood circulation thus the need
for the increased heartbeat. Therefore, the acute coronary syndrome is associated with many
challenges that patients have to be assisted to manage the condition thus making it easy for the
symptoms to be managed and reduce the fatal effects of the condition.
BETSY CASE STUDY
9
References
Amsterdam, E. A., Wenger, N. K., Brindis, R. G., Casey, D. E., Ganiats, T. G., Holmes, D. R., . .
. Zieman, S. J. (2014). 2014 AHA/ACC Guideline for the Management of Patients With
Non-ST-Elevation Acute Coronary Syndromes: A Report of the American College of
Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation,
25(10), 2354–2394.
Antman, E., & Morrow, D. (2012). Chapter 55. ST-segment elevation myocardial infarction:
Management. In B. RO, M. DL, Z. DP, & L. P, . Braunwald's heart disease: A textbook
of cardiovascular medicine (pp. 1111–1178). New York: Wiley.
Babu, A. S., Haneef, M., Joseph, A. N., & Noone, M. S. (2010). Risk Factors Among Patients
with Acute Coronary Syndrome in Rural Kerala. 35(2), 364–365.
Begg, G. (2016). Electrocardiogram interpretation and arrhythmia management: a primary and
secondary care survey. British Journal of General Practice, 66(246), 291-296.
Bonin, M., Mewton, N., Roubille, F., Morel, O., Cayla, G., Angoulvant, D., . . . Guerin, P.
(2017). Effect and Safety of Morphine Use in Acute Anterior ST-Segment Elevation
Myocardial Infarction. Journal of the American Heart Association, 10(6), 1-10.
Cheung, B. M., & Li, C. (2012). Diabetes and Hypertension: Is There a Common Metabolic
Pathway? Current Atheroclerosis Reports, 14(2), 160-166.
Dobesh, P. P., & Oestreich, J. H. (2014). Ticagrelor: Pharmacokinetics, Pharmacodynamics,
Clinical Efficacy, and Safety. Pharmacotherapy, 34(10), 1-10.
Figueiredo, J. H., Silva, N. A., Pereira, B. d., & Oliveira, G. M. (2017). Major Depression and
Acute Coronary Syndrome-Related Factors. Brazilian Cardiology Archives, 108(3), 217–
9
References
Amsterdam, E. A., Wenger, N. K., Brindis, R. G., Casey, D. E., Ganiats, T. G., Holmes, D. R., . .
. Zieman, S. J. (2014). 2014 AHA/ACC Guideline for the Management of Patients With
Non-ST-Elevation Acute Coronary Syndromes: A Report of the American College of
Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation,
25(10), 2354–2394.
Antman, E., & Morrow, D. (2012). Chapter 55. ST-segment elevation myocardial infarction:
Management. In B. RO, M. DL, Z. DP, & L. P, . Braunwald's heart disease: A textbook
of cardiovascular medicine (pp. 1111–1178). New York: Wiley.
Babu, A. S., Haneef, M., Joseph, A. N., & Noone, M. S. (2010). Risk Factors Among Patients
with Acute Coronary Syndrome in Rural Kerala. 35(2), 364–365.
Begg, G. (2016). Electrocardiogram interpretation and arrhythmia management: a primary and
secondary care survey. British Journal of General Practice, 66(246), 291-296.
Bonin, M., Mewton, N., Roubille, F., Morel, O., Cayla, G., Angoulvant, D., . . . Guerin, P.
(2017). Effect and Safety of Morphine Use in Acute Anterior ST-Segment Elevation
Myocardial Infarction. Journal of the American Heart Association, 10(6), 1-10.
Cheung, B. M., & Li, C. (2012). Diabetes and Hypertension: Is There a Common Metabolic
Pathway? Current Atheroclerosis Reports, 14(2), 160-166.
Dobesh, P. P., & Oestreich, J. H. (2014). Ticagrelor: Pharmacokinetics, Pharmacodynamics,
Clinical Efficacy, and Safety. Pharmacotherapy, 34(10), 1-10.
Figueiredo, J. H., Silva, N. A., Pereira, B. d., & Oliveira, G. M. (2017). Major Depression and
Acute Coronary Syndrome-Related Factors. Brazilian Cardiology Archives, 108(3), 217–
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BETSY CASE STUDY
10
227.
Ghadban, R., Enezate, T., Payne, J., Allaham, H., Halawa, A., Fong, H. K., . . . Aggarwal, K.
(2019). The safety of morphine use in acute coronary syndrome: a meta-analysis. Heart
Asia, 11(1).
James, S., Murphy, T., Waterhouse, D., Gallagher, J., O’Connell, E., & D Barton4, K. M. (2015).
22 Role of 12-lead electrocardiography in predicting heart failure in the community.
Heart, 101(5), 1-10.
Jheeta, J., Narayan, O., & Krasemann, T. (2014). Accuracy in interpreting the paediatric ECG: a
UK-wide study and the need for improvement. Archives of Disease in Childhood, 99(7),
646-648.
Kumar, A., & Christopher P. Cannon. (2011). Acute Coronary Syndromes: Diagnosis and
Management, Part I. Mayo Clinic Proceedings, 84(10), 917-938.
Osler, M., Mårtensson, S., Wium-Andersen, I. K., Andersen, E. P., Sara, T., Marie, C., &
Jørgensen, K. W.-A. (2016). Depression After First Hospital Admission for Acute
Coronary Syndrome: A Study of Time of Onset and Impact on Survival. American
Journal of Epidemiology, 183(3), 218-226.
Usta, C., & Bedel, A. (2017). Update on pharmacological treatment of acute coronary syndrome
without persistent ST segment elevation myocardial infarction in the elderly. Journal of
Geriatric Cardiology, 14(7), 457-464.
10
227.
Ghadban, R., Enezate, T., Payne, J., Allaham, H., Halawa, A., Fong, H. K., . . . Aggarwal, K.
(2019). The safety of morphine use in acute coronary syndrome: a meta-analysis. Heart
Asia, 11(1).
James, S., Murphy, T., Waterhouse, D., Gallagher, J., O’Connell, E., & D Barton4, K. M. (2015).
22 Role of 12-lead electrocardiography in predicting heart failure in the community.
Heart, 101(5), 1-10.
Jheeta, J., Narayan, O., & Krasemann, T. (2014). Accuracy in interpreting the paediatric ECG: a
UK-wide study and the need for improvement. Archives of Disease in Childhood, 99(7),
646-648.
Kumar, A., & Christopher P. Cannon. (2011). Acute Coronary Syndromes: Diagnosis and
Management, Part I. Mayo Clinic Proceedings, 84(10), 917-938.
Osler, M., Mårtensson, S., Wium-Andersen, I. K., Andersen, E. P., Sara, T., Marie, C., &
Jørgensen, K. W.-A. (2016). Depression After First Hospital Admission for Acute
Coronary Syndrome: A Study of Time of Onset and Impact on Survival. American
Journal of Epidemiology, 183(3), 218-226.
Usta, C., & Bedel, A. (2017). Update on pharmacological treatment of acute coronary syndrome
without persistent ST segment elevation myocardial infarction in the elderly. Journal of
Geriatric Cardiology, 14(7), 457-464.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





