Case Study: Assessment and Nursing Care for Mrs. Sue Jackson's Stroke
VerifiedAdded on 2022/08/26
|16
|4732
|14
Case Study
AI Summary
This case study analyzes the presentation of a 51-year-old woman, Mrs. Sue Jackson, experiencing an ischemic stroke. The analysis begins with the pathophysiology of stroke, detailing the mechanisms of ischemic cascade, the impact of hyperglycemia, and the role of factors like hypertension and atherosclerosis. The assessment section emphasizes the use of the FAST tool, vital signs, and the ROISER scale for diagnosis. The study then explores the priorities of nursing care, including the need for immediate hospital admission, MRI scans, and the potential for thrombolysis treatment within a specific timeframe. The case study highlights the importance of oxygen supplementation, insulin therapy, and antiplatelet medications. It also covers thrombectomy, temperature management, and anticoagulation treatments. The document underscores the significance of NICE guidelines in stroke management, emphasizing the roles of trained healthcare staff, neuroradiological support, and the importance of blood pressure control. The case study concludes by discussing various treatment options and nursing interventions, providing a comprehensive overview of stroke management in a clinical setting.

Running Head: Nursing
Case Study Analysis
Name of the Student
Name of the University
Authors Note
Case Study Analysis
Name of the Student
Name of the University
Authors Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1Case Study Analysis
Pathophysiology
Stroke is occurred in the brain due to poor blood circulation to the brain. Different
factors are responsible for stroke such as high blood pressure, hypoglycaemia, cardiac
abnormalities and high level of cholesterol. Primarily hypertension, atherosclerosis related to
coronary artery disease, hyperlipidaemia and dyslipidaemia are factors for the ischemic
stroke. Stroke might be happened in brain as the passage in the artery becomes narrow for
different reasons for example hypertension, atherosclerosis, high level of cholesterol and
blood clots. Cerebro-arterial system is damaged due to the lipid deposition and blockages in
the artery. Blood clots in heart often travel to the brain and block the blood circulation
pathways. Due to hypertension, some blood vessels are ruptured in brain and as a result entire
blood circulation of brain gets disturbed. The ischemic attack in brain is dependent upon
the ischemic cascade pathway. The brain tissues stop the functions if they do not get
oxygen for at least 60 to 90 seconds due to infractions and emboli. The infraction occurs
due to death of the tissues by de-oxygenation(Li, & Yang, 2017). On the other hand,
atherosclerosis disrupts the blood flow to the brain as the depositions and parts of the
deposition narrow down the space in lumen following the reduction in the blood flow. The
embolic infraction occurs due to formation of emboli in the circulatory system. emboli
influence the anaerobic metabolism in the region of brain tissues(Khoshnamet al., 2017).
Due to the anaerobic metabolism, ATP production get disrupted and lactic acid production
get increased. This lactic acid destroysthe acid-base balance in the body, specially in the
circulatory systems of brain and as a result ischemia occurs. The part of brain where
ischemia occurs is called penumbra. Due to depletion of oxygen and glucose in brain, ATP
cannot execute the energy production processes (such as ion pumping) which are important
for the survival of the tissues(Samaryet al., 2016).ATP reduction leads to the release
ofglutamate in the extra-cellular space. This condition lower the ion gradient and process a
Pathophysiology
Stroke is occurred in the brain due to poor blood circulation to the brain. Different
factors are responsible for stroke such as high blood pressure, hypoglycaemia, cardiac
abnormalities and high level of cholesterol. Primarily hypertension, atherosclerosis related to
coronary artery disease, hyperlipidaemia and dyslipidaemia are factors for the ischemic
stroke. Stroke might be happened in brain as the passage in the artery becomes narrow for
different reasons for example hypertension, atherosclerosis, high level of cholesterol and
blood clots. Cerebro-arterial system is damaged due to the lipid deposition and blockages in
the artery. Blood clots in heart often travel to the brain and block the blood circulation
pathways. Due to hypertension, some blood vessels are ruptured in brain and as a result entire
blood circulation of brain gets disturbed. The ischemic attack in brain is dependent upon
the ischemic cascade pathway. The brain tissues stop the functions if they do not get
oxygen for at least 60 to 90 seconds due to infractions and emboli. The infraction occurs
due to death of the tissues by de-oxygenation(Li, & Yang, 2017). On the other hand,
atherosclerosis disrupts the blood flow to the brain as the depositions and parts of the
deposition narrow down the space in lumen following the reduction in the blood flow. The
embolic infraction occurs due to formation of emboli in the circulatory system. emboli
influence the anaerobic metabolism in the region of brain tissues(Khoshnamet al., 2017).
Due to the anaerobic metabolism, ATP production get disrupted and lactic acid production
get increased. This lactic acid destroysthe acid-base balance in the body, specially in the
circulatory systems of brain and as a result ischemia occurs. The part of brain where
ischemia occurs is called penumbra. Due to depletion of oxygen and glucose in brain, ATP
cannot execute the energy production processes (such as ion pumping) which are important
for the survival of the tissues(Samaryet al., 2016).ATP reduction leads to the release
ofglutamate in the extra-cellular space. This condition lower the ion gradient and process a
2Case Study Analysis
calcium influx which destroys the functionalities of mitochondria by the process of
programmed cell death. Due to ischemia, the oxygen levels gets disturbed and the free
oxygen radicals are produced. The radicals react to the elements in the extracellular or
cellular elements of the blood vessels. The antioxidants neuroprotectants ( uric
acid and NXY-059) do not act on the brain cells but in the endothelium. The free radicals
affect the cells and initiate the cell death cascades with the reference of redox signalling. In
this case study the patient had chronic hyperglycemia or high blood glucose level. High
blood glucose level leads to elevated cell apoptosis due to the calcium imbalance and
aggravates cytochrome c outflow into the cytosol. Hyperglycaemia will lead to pentose
phosphate pathway which produces NADPH(Chenet al., 2016). The hyperglycaemia
increase vasoconstriction with the decreased level of nitric oxide production and induced
level of NO elimination. High blood sugar level increases ROS(Reactive Oxygen Species)
which interact with the Nitrogen oxides to generate peroxy-nitrite and this interaction
reduces bioavailability of NO(Reshiet al.,2017). The reduced bioavailability of NO leads to
vasoconstriction and poor condition of perfusion. Thus ischemia occurs in the brain cells.
Different parts of body become impaired due to the occurrence of the ischemic stroke for
an example aphasia, dysphagia, cognitive impairment and paralysis.
Assessment and the priorities of nursing care
In this case study ,Mrs Sue Jackson is a 51 year old lady and was suspected to be
affected by ischemic stroke or attack. The lady collapsed after feeling light headed and
having headache. Her husband thought that the headache was due to not taking Metformin for
blood glucose level control. The person who is suspected to have an ischemic stroke
should be assessed with the help of FAST assessment tool. Full form of “FAST” is Facial
drooping , Arm weakness, Speech impairment, and Time. The term Facial drooping denotes
if any deformities (any side of the face is deformed or hard to move) can be observed in the
calcium influx which destroys the functionalities of mitochondria by the process of
programmed cell death. Due to ischemia, the oxygen levels gets disturbed and the free
oxygen radicals are produced. The radicals react to the elements in the extracellular or
cellular elements of the blood vessels. The antioxidants neuroprotectants ( uric
acid and NXY-059) do not act on the brain cells but in the endothelium. The free radicals
affect the cells and initiate the cell death cascades with the reference of redox signalling. In
this case study the patient had chronic hyperglycemia or high blood glucose level. High
blood glucose level leads to elevated cell apoptosis due to the calcium imbalance and
aggravates cytochrome c outflow into the cytosol. Hyperglycaemia will lead to pentose
phosphate pathway which produces NADPH(Chenet al., 2016). The hyperglycaemia
increase vasoconstriction with the decreased level of nitric oxide production and induced
level of NO elimination. High blood sugar level increases ROS(Reactive Oxygen Species)
which interact with the Nitrogen oxides to generate peroxy-nitrite and this interaction
reduces bioavailability of NO(Reshiet al.,2017). The reduced bioavailability of NO leads to
vasoconstriction and poor condition of perfusion. Thus ischemia occurs in the brain cells.
Different parts of body become impaired due to the occurrence of the ischemic stroke for
an example aphasia, dysphagia, cognitive impairment and paralysis.
Assessment and the priorities of nursing care
In this case study ,Mrs Sue Jackson is a 51 year old lady and was suspected to be
affected by ischemic stroke or attack. The lady collapsed after feeling light headed and
having headache. Her husband thought that the headache was due to not taking Metformin for
blood glucose level control. The person who is suspected to have an ischemic stroke
should be assessed with the help of FAST assessment tool. Full form of “FAST” is Facial
drooping , Arm weakness, Speech impairment, and Time. The term Facial drooping denotes
if any deformities (any side of the face is deformed or hard to move) can be observed in the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3Case Study Analysis
face of the patient(Wolterset al., 2018). Arm weakness means if the patient feels
difficulties in moving hands and limbs, the patient will have the arm weakness as per
FAST.If the patient’s speech is become slurry or she/ he cannot talk properly , the patient
is having difficulties in the producing speech. At last “Time” means if the patient is showing
any of the above-discussed symptoms , emergency services should be called and the
patient should be hospitalised immediately. It is not clear whether the paramedics or Mrs
Jackson assessed her with the help of FAST assessment.
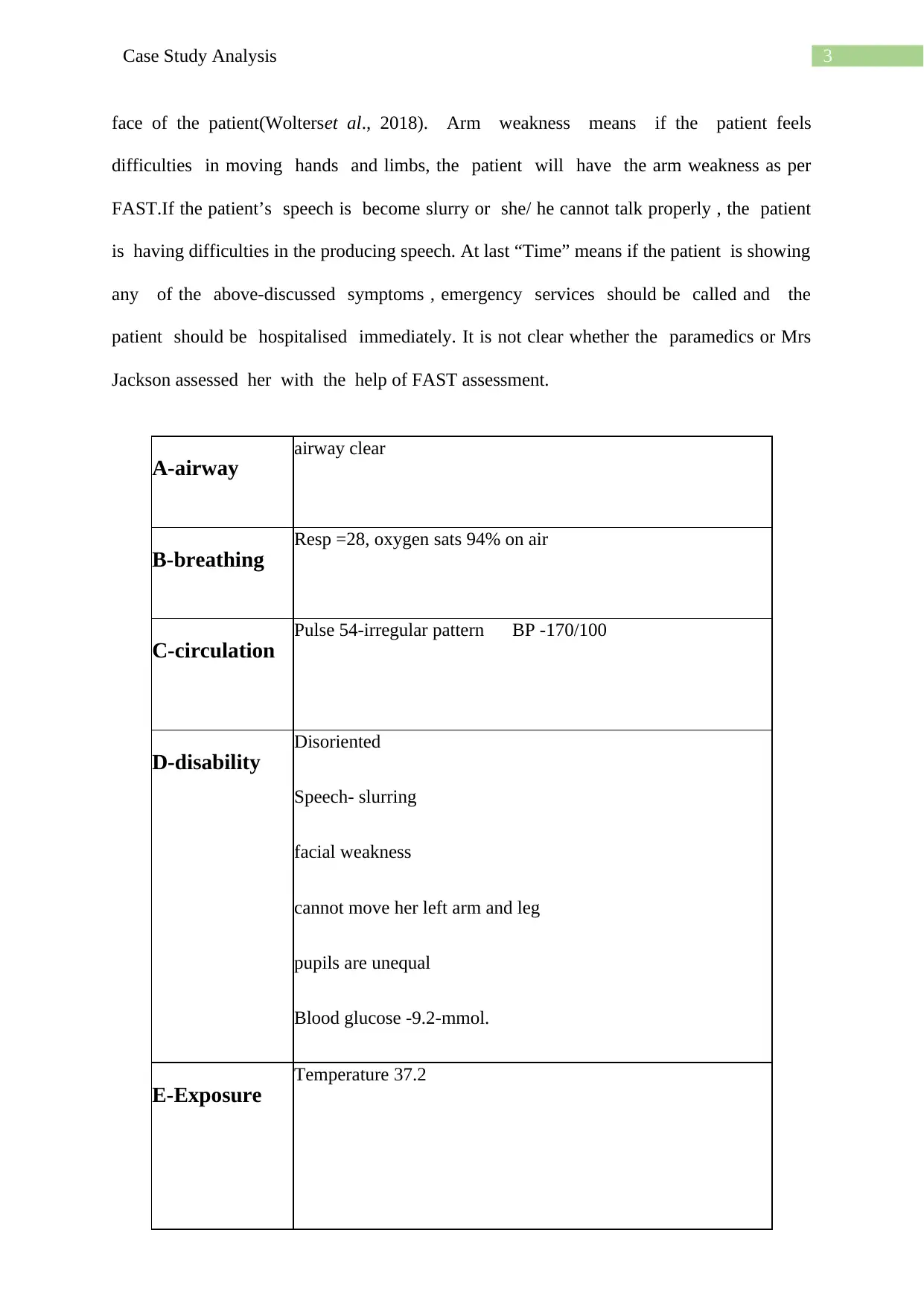
A-airway airway clear
B-breathing Resp =28, oxygen sats 94% on air
C-circulation Pulse 54-irregular pattern BP -170/100
D-disability Disoriented
Speech- slurring
facial weakness
cannot move her left arm and leg
pupils are unequal
Blood glucose -9.2-mmol.
E-Exposure Temperature 37.2
face of the patient(Wolterset al., 2018). Arm weakness means if the patient feels
difficulties in moving hands and limbs, the patient will have the arm weakness as per
FAST.If the patient’s speech is become slurry or she/ he cannot talk properly , the patient
is having difficulties in the producing speech. At last “Time” means if the patient is showing
any of the above-discussed symptoms , emergency services should be called and the
patient should be hospitalised immediately. It is not clear whether the paramedics or Mrs
Jackson assessed her with the help of FAST assessment.
A-airway airway clear
B-breathing Resp =28, oxygen sats 94% on air
C-circulation Pulse 54-irregular pattern BP -170/100
D-disability Disoriented
Speech- slurring
facial weakness
cannot move her left arm and leg
pupils are unequal
Blood glucose -9.2-mmol.
E-Exposure Temperature 37.2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4Case Study Analysis
This assessment can help in diagnosis of sudden neurological occurrence outside
the hospital. The paramedics or the nurse should exclude hypoglycaemia during the primary
assessment but here the patient had hyperglycaemia. Therefore the condition of
hypoglycaemia would not be counted. Patients who admitted to the hospital with the
condition of stroke should be undergone the assessment of ROISER (Recognition of Stroke
In the Emergency Room)(Sibson, 2017). The scale helps in the assessment of the Loss of
consciousness, seizure activity, asymmetric weakness in face , arm and leg, speech
disturbance and visual field defect. Moreover NICE has published a medical innovative
technology which briefs for theCerebrotech Visor for detecting stroke(pathways.nice.org.uk,
2020). The recognition method can involve some other assessment such as NIH stroke table
where patient’s consciousness and LOC(Loss Of Consciousness) level can be determined
with particular scoring methods. The patient with stroke symptoms should be admitted to
the specialist acute stroke unit to prevent any further deterioration in the patient’s health
scenario. The admission is important as this is the first step to provide quality treatment
service as per the quality standards of the NICE guideline. The person with stroke
syndrome will be referred to the MRI section for imaging. The MRI helps in understanding
the patient’s internal haemorrhage and if any lesions formed due to the blood clot and
rupture in the blood vessels. After performing MRI the process of Thrombolysis should be
held for a correct diagnosis and also for the betterment of the patient(Sreedharanet al.,2019).
The process of the patient should give oxygen supplement as the oxygen saturation has
dropped below the rate of 95% . Mrs Jacksonshould give the Proper insulin therapy to
manage the blood glucose level of body. Thrombolysis is with alteplase is a treatment for a
patient with acute ischaemic stroke. This treatment of Thrombolysis usually applied to the
patient as early as possible within 4-4.5 hours of onset of stroke symptoms. In this treatment
if there is any intracranial haemorrhage is happened or if there is a chance of the
This assessment can help in diagnosis of sudden neurological occurrence outside
the hospital. The paramedics or the nurse should exclude hypoglycaemia during the primary
assessment but here the patient had hyperglycaemia. Therefore the condition of
hypoglycaemia would not be counted. Patients who admitted to the hospital with the
condition of stroke should be undergone the assessment of ROISER (Recognition of Stroke
In the Emergency Room)(Sibson, 2017). The scale helps in the assessment of the Loss of
consciousness, seizure activity, asymmetric weakness in face , arm and leg, speech
disturbance and visual field defect. Moreover NICE has published a medical innovative
technology which briefs for theCerebrotech Visor for detecting stroke(pathways.nice.org.uk,
2020). The recognition method can involve some other assessment such as NIH stroke table
where patient’s consciousness and LOC(Loss Of Consciousness) level can be determined
with particular scoring methods. The patient with stroke symptoms should be admitted to
the specialist acute stroke unit to prevent any further deterioration in the patient’s health
scenario. The admission is important as this is the first step to provide quality treatment
service as per the quality standards of the NICE guideline. The person with stroke
syndrome will be referred to the MRI section for imaging. The MRI helps in understanding
the patient’s internal haemorrhage and if any lesions formed due to the blood clot and
rupture in the blood vessels. After performing MRI the process of Thrombolysis should be
held for a correct diagnosis and also for the betterment of the patient(Sreedharanet al.,2019).
The process of the patient should give oxygen supplement as the oxygen saturation has
dropped below the rate of 95% . Mrs Jacksonshould give the Proper insulin therapy to
manage the blood glucose level of body. Thrombolysis is with alteplase is a treatment for a
patient with acute ischaemic stroke. This treatment of Thrombolysis usually applied to the
patient as early as possible within 4-4.5 hours of onset of stroke symptoms. In this treatment
if there is any intracranial haemorrhage is happened or if there is a chance of the
5Case Study Analysis
haemorrhage, this has been excluded by the appropriate techniques of imaging. The process
of Thrombolysis based diagnosis can be performed only with the help of proper trained
healthcare staffs and should have a well-organised stroke management and services
(Thomallaet al., 2018). The trained healthcare associates should be involved in delivering
thrombolysis and for monitoring the process to identify any complications associated with
thrombolysis. The nursing staffs with proper management skills are also involved in the
treatment of acute ischaemic stroke and thrombolysis to provide level 1 and level 2 care to
the patient. The trained staffs should be involved in this treatment also for the accurate
imaging and re-imaging process and for the interpretation of those images towards the
patient’s family (pathways.nice.org.uk, 2020.). The staffs of emergency care department can
also be involved in this process of thrombolysis treatment if they have the required training
and management skills. The ischaemic stroke management is also be performed and managed
with the with the support of neuroradiological staffs and stroke physicians. The catheter-
directed thrombolysis is a minimally invasive treatment procedure in which the abnormal
blood clots are dissolved in the blood vessels by the insertion of a dissolving drug into the
blood veins through a certain part of the patient’s body (usually through the leg). The x-ray
imaging helps the physician to see the flow of drug and the inspection remains until it reaches
the blood clots. Thrombolysis process is usually recommended for the permanent deletion of
the blood clots in veins which are responsible for the severe stroke, damaging tissues and loss
of organs. After the tip of the catheter reaches the clot, the clot-dissolving drug is infused
through the catheter. The bolus infusion is neede as it prevent the oxygen flow towards brain
and causes cell damage or stroke. In most cases the clots usually dissolves within one or two
days. The whole procedure is monitored through special x-rays and ultrasound scans. The
images also help the physicians to determine if the vein-wall is narrow or damaged, making
prone to more clots in future. If there is a chance of this type of damage occurrence, an
haemorrhage, this has been excluded by the appropriate techniques of imaging. The process
of Thrombolysis based diagnosis can be performed only with the help of proper trained
healthcare staffs and should have a well-organised stroke management and services
(Thomallaet al., 2018). The trained healthcare associates should be involved in delivering
thrombolysis and for monitoring the process to identify any complications associated with
thrombolysis. The nursing staffs with proper management skills are also involved in the
treatment of acute ischaemic stroke and thrombolysis to provide level 1 and level 2 care to
the patient. The trained staffs should be involved in this treatment also for the accurate
imaging and re-imaging process and for the interpretation of those images towards the
patient’s family (pathways.nice.org.uk, 2020.). The staffs of emergency care department can
also be involved in this process of thrombolysis treatment if they have the required training
and management skills. The ischaemic stroke management is also be performed and managed
with the with the support of neuroradiological staffs and stroke physicians. The catheter-
directed thrombolysis is a minimally invasive treatment procedure in which the abnormal
blood clots are dissolved in the blood vessels by the insertion of a dissolving drug into the
blood veins through a certain part of the patient’s body (usually through the leg). The x-ray
imaging helps the physician to see the flow of drug and the inspection remains until it reaches
the blood clots. Thrombolysis process is usually recommended for the permanent deletion of
the blood clots in veins which are responsible for the severe stroke, damaging tissues and loss
of organs. After the tip of the catheter reaches the clot, the clot-dissolving drug is infused
through the catheter. The bolus infusion is neede as it prevent the oxygen flow towards brain
and causes cell damage or stroke. In most cases the clots usually dissolves within one or two
days. The whole procedure is monitored through special x-rays and ultrasound scans. The
images also help the physicians to determine if the vein-wall is narrow or damaged, making
prone to more clots in future. If there is a chance of this type of damage occurrence, an
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6Case Study Analysis
additional procedure may be needed, such as a balloon angioplasty or a small mesh stent
placement into the vein to avoid further clotting. Here, the Consultant attends and discusses
the option of thrombolysis as a treatment for Mrs Jackson. The patient provides informed
consent, a bolus is given and the infusion is commenced. Mrs Jackson is transferred to the
acute stroke ward and receives close supervision and further assessments.
In the ischaemic stroke cases the aspirin or antiplatelet treatments are also
recommended for the reduction of the risks of further clotting in blood veins. This type of
medication usually prevents the platelets from sticking to each other and forming further
blood clots. This therapy is applied on the patient after 24 hours of thrombolysis treatment.
Approximately 22% chances of stroke can be reduced by the anti-platelet therapy as it can
diminish the amount of clot formation (Mas et al., 2017). In first-line antiplatelet therapy
Aspirin 300mg is administered maintaining a daily course. Clopidogrel should be
administered in case the patient is not tolerant to Aspirin (Pan et al., 2017). If the patient is
dysphasic the medication should be given through the suppository or enteral tube. After the
enduring antithrombotic treatment process, the antiplatelet medication should be specified for
a two-week term after the performance of AIS. Thrombectomy is actually a mechanical
process of clot recuperation which is a straight clot elimination therapy of the crassamentum
via angiography. This process is indicated for the patient’s large artery occlusion due to
stroke(Alberset al, 2018). Thisshould be performed by the nurses within 6 hours of
admission , the thrombectomy monitored by the help of CTA and MRA . If the patient has
defective proximal anterior circulation , thrombectomy is done. If the patient got less
than 3 in mRS or more than 5 in NIHSS, the paitient should be referred to the
thrombectomy. The nurses should use clot retrieval process by the help of angiography. The
Patient has shown that he body temperature is more than 36 C. the nurses should maintain
the body temperature between 33 to 36C. The temperature should be ,monitored with the
additional procedure may be needed, such as a balloon angioplasty or a small mesh stent
placement into the vein to avoid further clotting. Here, the Consultant attends and discusses
the option of thrombolysis as a treatment for Mrs Jackson. The patient provides informed
consent, a bolus is given and the infusion is commenced. Mrs Jackson is transferred to the
acute stroke ward and receives close supervision and further assessments.
In the ischaemic stroke cases the aspirin or antiplatelet treatments are also
recommended for the reduction of the risks of further clotting in blood veins. This type of
medication usually prevents the platelets from sticking to each other and forming further
blood clots. This therapy is applied on the patient after 24 hours of thrombolysis treatment.
Approximately 22% chances of stroke can be reduced by the anti-platelet therapy as it can
diminish the amount of clot formation (Mas et al., 2017). In first-line antiplatelet therapy
Aspirin 300mg is administered maintaining a daily course. Clopidogrel should be
administered in case the patient is not tolerant to Aspirin (Pan et al., 2017). If the patient is
dysphasic the medication should be given through the suppository or enteral tube. After the
enduring antithrombotic treatment process, the antiplatelet medication should be specified for
a two-week term after the performance of AIS. Thrombectomy is actually a mechanical
process of clot recuperation which is a straight clot elimination therapy of the crassamentum
via angiography. This process is indicated for the patient’s large artery occlusion due to
stroke(Alberset al, 2018). Thisshould be performed by the nurses within 6 hours of
admission , the thrombectomy monitored by the help of CTA and MRA . If the patient has
defective proximal anterior circulation , thrombectomy is done. If the patient got less
than 3 in mRS or more than 5 in NIHSS, the paitient should be referred to the
thrombectomy. The nurses should use clot retrieval process by the help of angiography. The
Patient has shown that he body temperature is more than 36 C. the nurses should maintain
the body temperature between 33 to 36C. The temperature should be ,monitored with the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7Case Study Analysis
help of internal probe which is connected to cooling device. after cooling the nurse
should monitor the cardiovascular functionality. Intubation and sedation will be suggested
if needed by the patient. Neuromuscular blockersmight be suggested to the patient as
drugs for emergency. Hypothermia aims to reduce further secondary brain damage. Nurses
should provide anticoagulation treatment to Mrs Jackson for treating the cerebral venous
thrombosis or proximal deep vein thrombosis .If the patient has the situation of atrial
fibrillation , the patient must be treated with the help of warfarin . This medication will
help in preventing coagulation as well as hypertension. Blood pressure control is one of
the most important factor for preventing the stroke . As per the NICE guidelines the
patient’s blood pressure was 170/100 mmHg which is less than 185/110 mmHg . Therefore,
she is considered to have intravenous thrombolysis(McManusand Liebeskind, 2016.). The
antihypertensive therapy will after detecting stroke of the patient by AIS. Antihypertensive
medication will be administered to the patient(Georgianouet al., 2018). The swallow screen
assessment will done after the arrival of the patient in the acute emergency ward for
stroke. If the patient is suspected to have thrombolysis, nasogastric tube should be used for
feeding the patient within 24 hours of admission. Assessment and reassessment should
beperformed by proper health professionals.If the patient have dysphagia, the tube is used
to continue nutrition and hydration with oral nutritional supplementation to avoid
aspiration pneumonia. Nurses should check the BMI and nutritional quality of the patient
with the help of assessment tools like MUST. Statin treatment will be required by the patient
within 48 hours of admission . Decompressivehemicraniectomy should be performed
within the 48 hours if 1 or more than one criteria is matched with NIHSS and 50% infarct
can be observed in middle cerebral artery territory. This process need the consent of patient
and her family.. Before that to investigate the hypertensive effects on the patient, carotid
stenosis will be suggested the stroke is non disabling in nature.
help of internal probe which is connected to cooling device. after cooling the nurse
should monitor the cardiovascular functionality. Intubation and sedation will be suggested
if needed by the patient. Neuromuscular blockersmight be suggested to the patient as
drugs for emergency. Hypothermia aims to reduce further secondary brain damage. Nurses
should provide anticoagulation treatment to Mrs Jackson for treating the cerebral venous
thrombosis or proximal deep vein thrombosis .If the patient has the situation of atrial
fibrillation , the patient must be treated with the help of warfarin . This medication will
help in preventing coagulation as well as hypertension. Blood pressure control is one of
the most important factor for preventing the stroke . As per the NICE guidelines the
patient’s blood pressure was 170/100 mmHg which is less than 185/110 mmHg . Therefore,
she is considered to have intravenous thrombolysis(McManusand Liebeskind, 2016.). The
antihypertensive therapy will after detecting stroke of the patient by AIS. Antihypertensive
medication will be administered to the patient(Georgianouet al., 2018). The swallow screen
assessment will done after the arrival of the patient in the acute emergency ward for
stroke. If the patient is suspected to have thrombolysis, nasogastric tube should be used for
feeding the patient within 24 hours of admission. Assessment and reassessment should
beperformed by proper health professionals.If the patient have dysphagia, the tube is used
to continue nutrition and hydration with oral nutritional supplementation to avoid
aspiration pneumonia. Nurses should check the BMI and nutritional quality of the patient
with the help of assessment tools like MUST. Statin treatment will be required by the patient
within 48 hours of admission . Decompressivehemicraniectomy should be performed
within the 48 hours if 1 or more than one criteria is matched with NIHSS and 50% infarct
can be observed in middle cerebral artery territory. This process need the consent of patient
and her family.. Before that to investigate the hypertensive effects on the patient, carotid
stenosis will be suggested the stroke is non disabling in nature.
8Case Study Analysis
Mrs Jackson is a patient of hyperglycemia. In A-E assessment; respiratory rate and
blood pressure is high. The interventions are discussed in above discussion. She was feeling
light headed and acute headache before she collapsed. Socially she is active as she is a
working woman. She works as an accountant in her husband's farm. She takes care of her
children and her mother who is a dementia patient. Excessive hard work and stress might
affect her health. Psychological health is also affected as she takes care of a mother who is a
dementia patient.
The effect of Mrs Jackson's illness will affect the family biological psychological and
socially. Biological e she will not be able to you as active as she was before the stroke. This
will definitely effect of psychological health of her and the family members also
After having stroke Mrs Jackson will feel social isolation or emotional distance from
the family. She might feel loneliness and depression as her cognition and speech will be
affected. Her activity will definitely affected by the histamine stroke which will be obstacle
for her daily activities. Her family members specially the children and her mother will get
affected psychologically as she was the only person who took care of them(Cheng et al.,
2016). Her husband also feel very lonely and he might we suffered from depression. To uplift
the spirit of the family the nurse should take stations with the children and old mother. One or
more support workers should be appointed to take care of dementia patient and the children.
Mr Jackson should be trained for giving medication to his wife.
He should help her in the rehabilitation process by giving support in physical therapy
and household chores. The nurse should counsel him regular basis so that positivity and
optimism will be e present always in him. The nurse would take psychological examination
assess(MMSE- mini mental state examination) the mental state of the family(Lestariet al.,
2017). Psychologist or mental health nurse should give counselling and CBT(cognitive
Mrs Jackson is a patient of hyperglycemia. In A-E assessment; respiratory rate and
blood pressure is high. The interventions are discussed in above discussion. She was feeling
light headed and acute headache before she collapsed. Socially she is active as she is a
working woman. She works as an accountant in her husband's farm. She takes care of her
children and her mother who is a dementia patient. Excessive hard work and stress might
affect her health. Psychological health is also affected as she takes care of a mother who is a
dementia patient.
The effect of Mrs Jackson's illness will affect the family biological psychological and
socially. Biological e she will not be able to you as active as she was before the stroke. This
will definitely effect of psychological health of her and the family members also
After having stroke Mrs Jackson will feel social isolation or emotional distance from
the family. She might feel loneliness and depression as her cognition and speech will be
affected. Her activity will definitely affected by the histamine stroke which will be obstacle
for her daily activities. Her family members specially the children and her mother will get
affected psychologically as she was the only person who took care of them(Cheng et al.,
2016). Her husband also feel very lonely and he might we suffered from depression. To uplift
the spirit of the family the nurse should take stations with the children and old mother. One or
more support workers should be appointed to take care of dementia patient and the children.
Mr Jackson should be trained for giving medication to his wife.
He should help her in the rehabilitation process by giving support in physical therapy
and household chores. The nurse should counsel him regular basis so that positivity and
optimism will be e present always in him. The nurse would take psychological examination
assess(MMSE- mini mental state examination) the mental state of the family(Lestariet al.,
2017). Psychologist or mental health nurse should give counselling and CBT(cognitive
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9Case Study Analysis
behavioural therapy) for preventing him from any kind of addiction due to depression. The
family relationship may be improve interpersonal therapies. Regular sessions and counselling
will help to improve spirituality and the positivity among the family members.Non-verbal
communication like hand gestures, touch, proximity will be the part of therapeutic
management if there are speech issues ( which is normal after stroke) in the patient.If
memory impairment can be observed in the patient ,nutritional therapy, sleep, rest and
memory tracking exercises will be provided to her as interventions. Psychotherapists and
psychoanalysts will intervene cognitive behavioural therapy to improve cognitionof the
patient.
Impact of acute illness on the patient and family
The nurse will involve multidisciplinary team in the rehabilitation of Mrs Jackson.
Physician physiotherapist occupational therapist.Nurses and the rehabilitation assistant
should maintain legal and ethical guidelines without conflict. To serve the dementia patient
the support worker might find difficulty with reference to the old patient’s personal and
cultural values and beliefs. Speech Language therapist, clinical psychologist, rehabilitation
assistance ,social workers should be involved in the rehabilitation of the patient(Horton,
Laneand Shiggins, 2016).Conflict with family members should be resolved by involvement
of psychologist or negotiators as patience well-being is the most important for both nurse and
the family. The nurse will convince the family member to involve in different therapies
which will be a long-term part of Mrs Jackson's life. Without the help of the family and Mr
Jackson the nurse cannot treat the patient alone. Therefore Mr Jackson will be taught how to
assess the vital signs such as blood pressure temperature Glucose level pulse rate to regular
assessment. Nursing staff should ensure that access to other services like continents advice
dietetics electronic aids, psychiatry,orthoptics, orthotics, pharmacy should be involved.
Assess the patient condition in orientation positioning, shallowing, transfer continence,
behavioural therapy) for preventing him from any kind of addiction due to depression. The
family relationship may be improve interpersonal therapies. Regular sessions and counselling
will help to improve spirituality and the positivity among the family members.Non-verbal
communication like hand gestures, touch, proximity will be the part of therapeutic
management if there are speech issues ( which is normal after stroke) in the patient.If
memory impairment can be observed in the patient ,nutritional therapy, sleep, rest and
memory tracking exercises will be provided to her as interventions. Psychotherapists and
psychoanalysts will intervene cognitive behavioural therapy to improve cognitionof the
patient.
Impact of acute illness on the patient and family
The nurse will involve multidisciplinary team in the rehabilitation of Mrs Jackson.
Physician physiotherapist occupational therapist.Nurses and the rehabilitation assistant
should maintain legal and ethical guidelines without conflict. To serve the dementia patient
the support worker might find difficulty with reference to the old patient’s personal and
cultural values and beliefs. Speech Language therapist, clinical psychologist, rehabilitation
assistance ,social workers should be involved in the rehabilitation of the patient(Horton,
Laneand Shiggins, 2016).Conflict with family members should be resolved by involvement
of psychologist or negotiators as patience well-being is the most important for both nurse and
the family. The nurse will convince the family member to involve in different therapies
which will be a long-term part of Mrs Jackson's life. Without the help of the family and Mr
Jackson the nurse cannot treat the patient alone. Therefore Mr Jackson will be taught how to
assess the vital signs such as blood pressure temperature Glucose level pulse rate to regular
assessment. Nursing staff should ensure that access to other services like continents advice
dietetics electronic aids, psychiatry,orthoptics, orthotics, pharmacy should be involved.
Assess the patient condition in orientation positioning, shallowing, transfer continence,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10Case Study Analysis
pressure areas, communication and nutritional status for goal settings and planning the
rehabilitation. Therapies like cognitive functioning, communication therapy, emotional
functioning, self-care,shallowing andvisionassessmnet will be involved as per the intensity
of the stroke rehabilitation(pathways.nice.org.uk/pathways, 2020). Physiotherapy well
consider fitness training and strength training as per the patient condition. Upper Limb and
lower limb repeated movements are also included in the therapy(dos Santos et al., 2019). The
patient will transfer from acute care to the community health care. Rehabilitation process
should ensure that the person will continue her occupation and long-term support throughout
her life. In these activities the family must play a major role. In emotional functioning
training the family should be supported and educated by the care givers as per their
psychological needs as per the time and different settings.The rehabilitation assistant will kill
the patient to dress one handed and how to use the electronic devices which support bathing
dressing and doing other regular activities. The restorative strategies might be included and
supported by the team members. Self-care training and guidelines might be tot to the family
members also as per the situations therefore they will not be affected by other diseases.
Different orthoptic assessment and eye movement therapy should be given to the
person(Rowe, 2019). Shallowing therapy and assessment with exercises and postural advices
will be given to the person(Bath, Lee and Everton, 2018).Lack of training and will affect the
family members as well as the patient to deal with the situation we stop the nurses should
understand emotional and social requirement daily Lifestyle might be affected divisibility of
Mrs Jackson. Agitation, aggression and depression can be observed in the family members
emotional isolation should not be taken place in this situation. To normalise and regularise
the family life regular counselling and emotional support should be given to the person’s
family. By proper support training and maintaining the guidelines will help the patient and
the family member overcome the situation.
pressure areas, communication and nutritional status for goal settings and planning the
rehabilitation. Therapies like cognitive functioning, communication therapy, emotional
functioning, self-care,shallowing andvisionassessmnet will be involved as per the intensity
of the stroke rehabilitation(pathways.nice.org.uk/pathways, 2020). Physiotherapy well
consider fitness training and strength training as per the patient condition. Upper Limb and
lower limb repeated movements are also included in the therapy(dos Santos et al., 2019). The
patient will transfer from acute care to the community health care. Rehabilitation process
should ensure that the person will continue her occupation and long-term support throughout
her life. In these activities the family must play a major role. In emotional functioning
training the family should be supported and educated by the care givers as per their
psychological needs as per the time and different settings.The rehabilitation assistant will kill
the patient to dress one handed and how to use the electronic devices which support bathing
dressing and doing other regular activities. The restorative strategies might be included and
supported by the team members. Self-care training and guidelines might be tot to the family
members also as per the situations therefore they will not be affected by other diseases.
Different orthoptic assessment and eye movement therapy should be given to the
person(Rowe, 2019). Shallowing therapy and assessment with exercises and postural advices
will be given to the person(Bath, Lee and Everton, 2018).Lack of training and will affect the
family members as well as the patient to deal with the situation we stop the nurses should
understand emotional and social requirement daily Lifestyle might be affected divisibility of
Mrs Jackson. Agitation, aggression and depression can be observed in the family members
emotional isolation should not be taken place in this situation. To normalise and regularise
the family life regular counselling and emotional support should be given to the person’s
family. By proper support training and maintaining the guidelines will help the patient and
the family member overcome the situation.

11Case Study Analysis
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





