Case Study: Ms Jane Green
VerifiedAdded on 2023/04/20
|10
|2044
|145
AI Summary
This case study analyzes the condition of Ms Jane Green after a car accident, including normal and abnormal data, interpretation, and nursing diagnoses.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: CASE STUDY
Ms Jane Green
Name of the Student
Name of the University
Author Note
Ms Jane Green
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1CASE STUDY
Student number:
CNA253 AT2 Scenario: Miss Jane Green
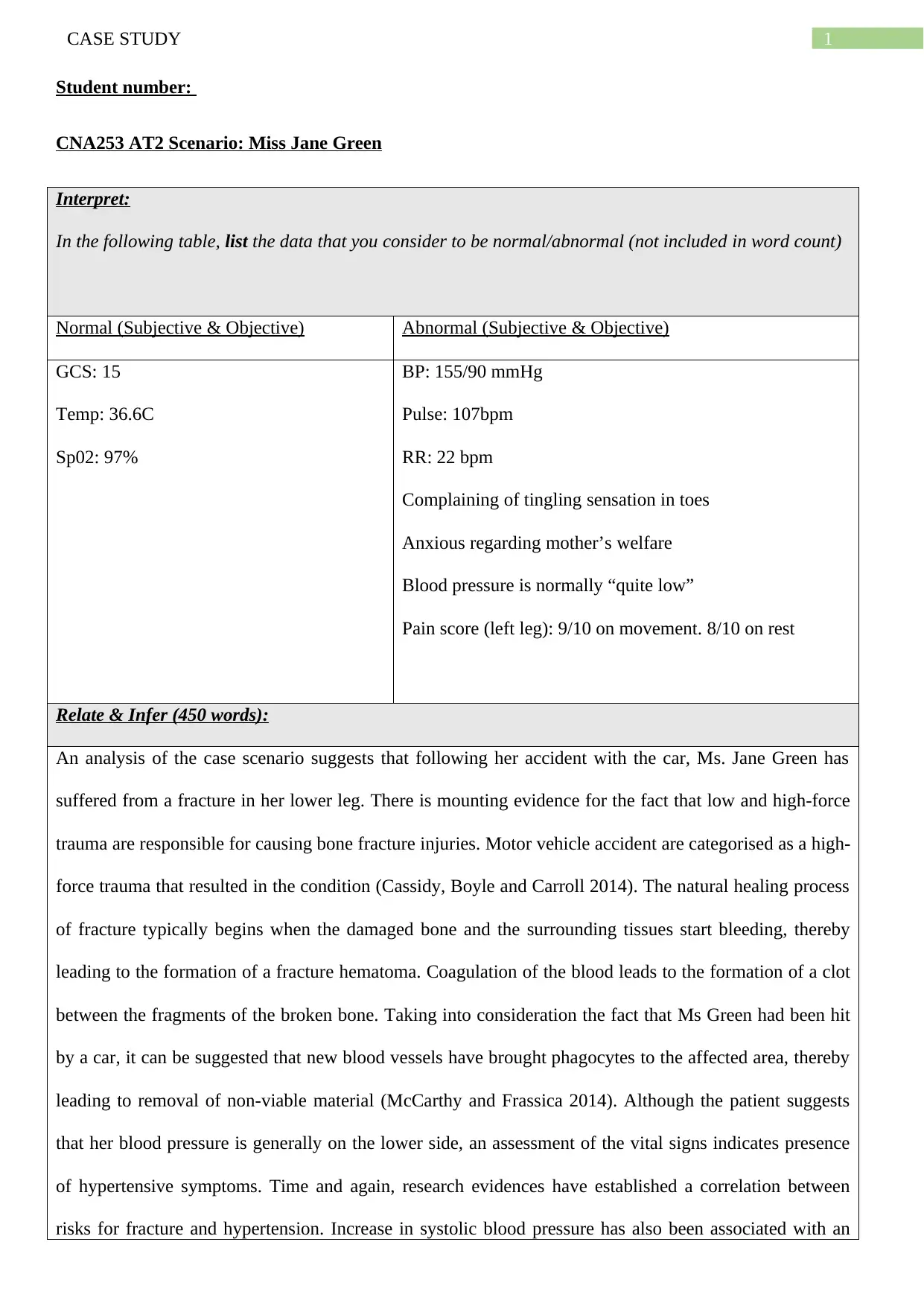
Interpret:
In the following table, list the data that you consider to be normal/abnormal (not included in word count)
Normal (Subjective & Objective) Abnormal (Subjective & Objective)
GCS: 15
Temp: 36.6C
Sp02: 97%
BP: 155/90 mmHg
Pulse: 107bpm
RR: 22 bpm
Complaining of tingling sensation in toes
Anxious regarding mother’s welfare
Blood pressure is normally “quite low”
Pain score (left leg): 9/10 on movement. 8/10 on rest
Relate & Infer (450 words):
An analysis of the case scenario suggests that following her accident with the car, Ms. Jane Green has
suffered from a fracture in her lower leg. There is mounting evidence for the fact that low and high-force
trauma are responsible for causing bone fracture injuries. Motor vehicle accident are categorised as a high-
force trauma that resulted in the condition (Cassidy, Boyle and Carroll 2014). The natural healing process
of fracture typically begins when the damaged bone and the surrounding tissues start bleeding, thereby
leading to the formation of a fracture hematoma. Coagulation of the blood leads to the formation of a clot
between the fragments of the broken bone. Taking into consideration the fact that Ms Green had been hit
by a car, it can be suggested that new blood vessels have brought phagocytes to the affected area, thereby
leading to removal of non-viable material (McCarthy and Frassica 2014). Although the patient suggests
that her blood pressure is generally on the lower side, an assessment of the vital signs indicates presence
of hypertensive symptoms. Time and again, research evidences have established a correlation between
risks for fracture and hypertension. Increase in systolic blood pressure has also been associated with an
Student number:
CNA253 AT2 Scenario: Miss Jane Green
Interpret:
In the following table, list the data that you consider to be normal/abnormal (not included in word count)
Normal (Subjective & Objective) Abnormal (Subjective & Objective)
GCS: 15
Temp: 36.6C
Sp02: 97%
BP: 155/90 mmHg
Pulse: 107bpm
RR: 22 bpm
Complaining of tingling sensation in toes
Anxious regarding mother’s welfare
Blood pressure is normally “quite low”
Pain score (left leg): 9/10 on movement. 8/10 on rest
Relate & Infer (450 words):
An analysis of the case scenario suggests that following her accident with the car, Ms. Jane Green has
suffered from a fracture in her lower leg. There is mounting evidence for the fact that low and high-force
trauma are responsible for causing bone fracture injuries. Motor vehicle accident are categorised as a high-
force trauma that resulted in the condition (Cassidy, Boyle and Carroll 2014). The natural healing process
of fracture typically begins when the damaged bone and the surrounding tissues start bleeding, thereby
leading to the formation of a fracture hematoma. Coagulation of the blood leads to the formation of a clot
between the fragments of the broken bone. Taking into consideration the fact that Ms Green had been hit
by a car, it can be suggested that new blood vessels have brought phagocytes to the affected area, thereby
leading to removal of non-viable material (McCarthy and Frassica 2014). Although the patient suggests
that her blood pressure is generally on the lower side, an assessment of the vital signs indicates presence
of hypertensive symptoms. Time and again, research evidences have established a correlation between
risks for fracture and hypertension. Increase in systolic blood pressure has also been associated with an
2CASE STUDY
improvement in survival rates of patients having hypotension (Yang et al. 2014). Blood pressure
commonly increases after an accident due to massive internal bleeding and damage to the internal organs.
Hence, the hypovolemic shock caused due to car accident was responsible for severe loss of fluids and
blood, which elevated the pressure. Motor vehicle accidents are also associated with acute respiratory
failure. Although the normal range for respiratory rate in healthy adults is 12-18 breaths/min. However,
the increased respiratory rate in the patient can be explained as the onset of tachypnea that led to shallow
and rapid breathing. This condition can be accredited to disruption of balance between oxygen and carbon
dioxide in the human body. It is commonly found that patients who have suffered from motor vehicle
accidents, are subjected to chest trauma that increases their respiratory distress and lead to laboured
breathing (Chen et al. 2014).
In addition, while the normal pulse rate for adults ranges between 60-100 beats/min, presence of 107 pulse
rate in Ms Green can be termed as tachycardia that is manifested by an abnormal beating of the upper and
lower chambers of the heart. The high-force trauma resulted in a disruption in the electrical impulses that
control the functioning of the heart. In addition, presence of pain can be associated with tissue injury at the
legs that occurred due to activation of nerve fibres and peripheral pain receptors (Sommer 2016). The
sensation of pain is a kind of normal response to the injury. Severity of pain can be accredited to chronic
sensitisation of nociceptors that contribute to persistent pain in the patient.
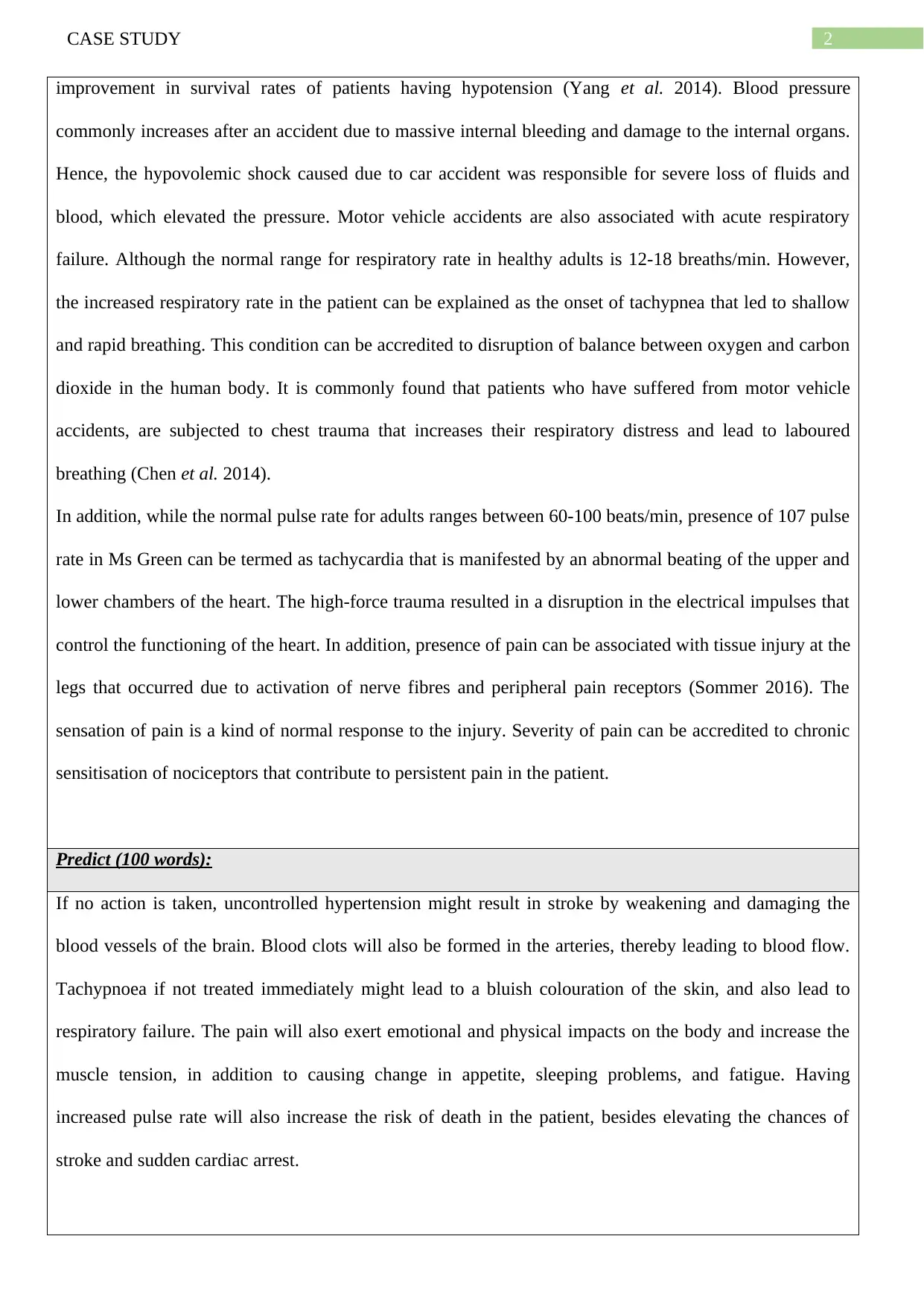
Predict (100 words):
If no action is taken, uncontrolled hypertension might result in stroke by weakening and damaging the
blood vessels of the brain. Blood clots will also be formed in the arteries, thereby leading to blood flow.
Tachypnoea if not treated immediately might lead to a bluish colouration of the skin, and also lead to
respiratory failure. The pain will also exert emotional and physical impacts on the body and increase the
muscle tension, in addition to causing change in appetite, sleeping problems, and fatigue. Having
increased pulse rate will also increase the risk of death in the patient, besides elevating the chances of
stroke and sudden cardiac arrest.
improvement in survival rates of patients having hypotension (Yang et al. 2014). Blood pressure
commonly increases after an accident due to massive internal bleeding and damage to the internal organs.
Hence, the hypovolemic shock caused due to car accident was responsible for severe loss of fluids and
blood, which elevated the pressure. Motor vehicle accidents are also associated with acute respiratory
failure. Although the normal range for respiratory rate in healthy adults is 12-18 breaths/min. However,
the increased respiratory rate in the patient can be explained as the onset of tachypnea that led to shallow
and rapid breathing. This condition can be accredited to disruption of balance between oxygen and carbon
dioxide in the human body. It is commonly found that patients who have suffered from motor vehicle
accidents, are subjected to chest trauma that increases their respiratory distress and lead to laboured
breathing (Chen et al. 2014).
In addition, while the normal pulse rate for adults ranges between 60-100 beats/min, presence of 107 pulse
rate in Ms Green can be termed as tachycardia that is manifested by an abnormal beating of the upper and
lower chambers of the heart. The high-force trauma resulted in a disruption in the electrical impulses that
control the functioning of the heart. In addition, presence of pain can be associated with tissue injury at the
legs that occurred due to activation of nerve fibres and peripheral pain receptors (Sommer 2016). The
sensation of pain is a kind of normal response to the injury. Severity of pain can be accredited to chronic
sensitisation of nociceptors that contribute to persistent pain in the patient.
Predict (100 words):
If no action is taken, uncontrolled hypertension might result in stroke by weakening and damaging the
blood vessels of the brain. Blood clots will also be formed in the arteries, thereby leading to blood flow.
Tachypnoea if not treated immediately might lead to a bluish colouration of the skin, and also lead to
respiratory failure. The pain will also exert emotional and physical impacts on the body and increase the
muscle tension, in addition to causing change in appetite, sleeping problems, and fatigue. Having
increased pulse rate will also increase the risk of death in the patient, besides elevating the chances of
stroke and sudden cardiac arrest.
3CASE STUDY
Develop, Articulate and Prioritise Nursing Diagnoses – at least 3 (not included in word count)
To reduce pain severity
To restore blood pressure
To restore breathing
To restore pulse rate
Goals, Actions and Evaluation 2 highest priority diagnoses only (450 words)
Diagnosis 1 Goal/s Related actions Rationale Evaluate
outcomes
Numeric rating
scale
To lower
his pain
severity
scores
near or
below 3
Conduct a
comprehensive
assessment
Administer
morphine
Use non-
pharmacological
methods like
music therapy
and relaxation
exercises
Assessment is the
initial step in pain
management and will
help in ensuring the
Ms Green is offered
effective pain relief
services
Morphine is the
mainstay in pain
medication and will
act on the central
nervous system, by
interacting with
the μ–δ-opioid (Mu-
Delta) receptor
heteromer.
Activation of the
receptor will result in
Pain scores
between 1-
3 after 24
hours
Develop, Articulate and Prioritise Nursing Diagnoses – at least 3 (not included in word count)
To reduce pain severity
To restore blood pressure
To restore breathing
To restore pulse rate
Goals, Actions and Evaluation 2 highest priority diagnoses only (450 words)
Diagnosis 1 Goal/s Related actions Rationale Evaluate
outcomes
Numeric rating
scale
To lower
his pain
severity
scores
near or
below 3
Conduct a
comprehensive
assessment
Administer
morphine
Use non-
pharmacological
methods like
music therapy
and relaxation
exercises
Assessment is the
initial step in pain
management and will
help in ensuring the
Ms Green is offered
effective pain relief
services
Morphine is the
mainstay in pain
medication and will
act on the central
nervous system, by
interacting with
the μ–δ-opioid (Mu-
Delta) receptor
heteromer.
Activation of the
receptor will result in
Pain scores
between 1-
3 after 24
hours
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4CASE STUDY
onset of analgesia
and will provide
relief from pain
(Kapur, Lala and
Shaw 2014).
Music therapy will
also provide sensory
stimulation and
evoke responses in
the patient, thus
lowering the pain she
feels (Korhan et al.
2014).
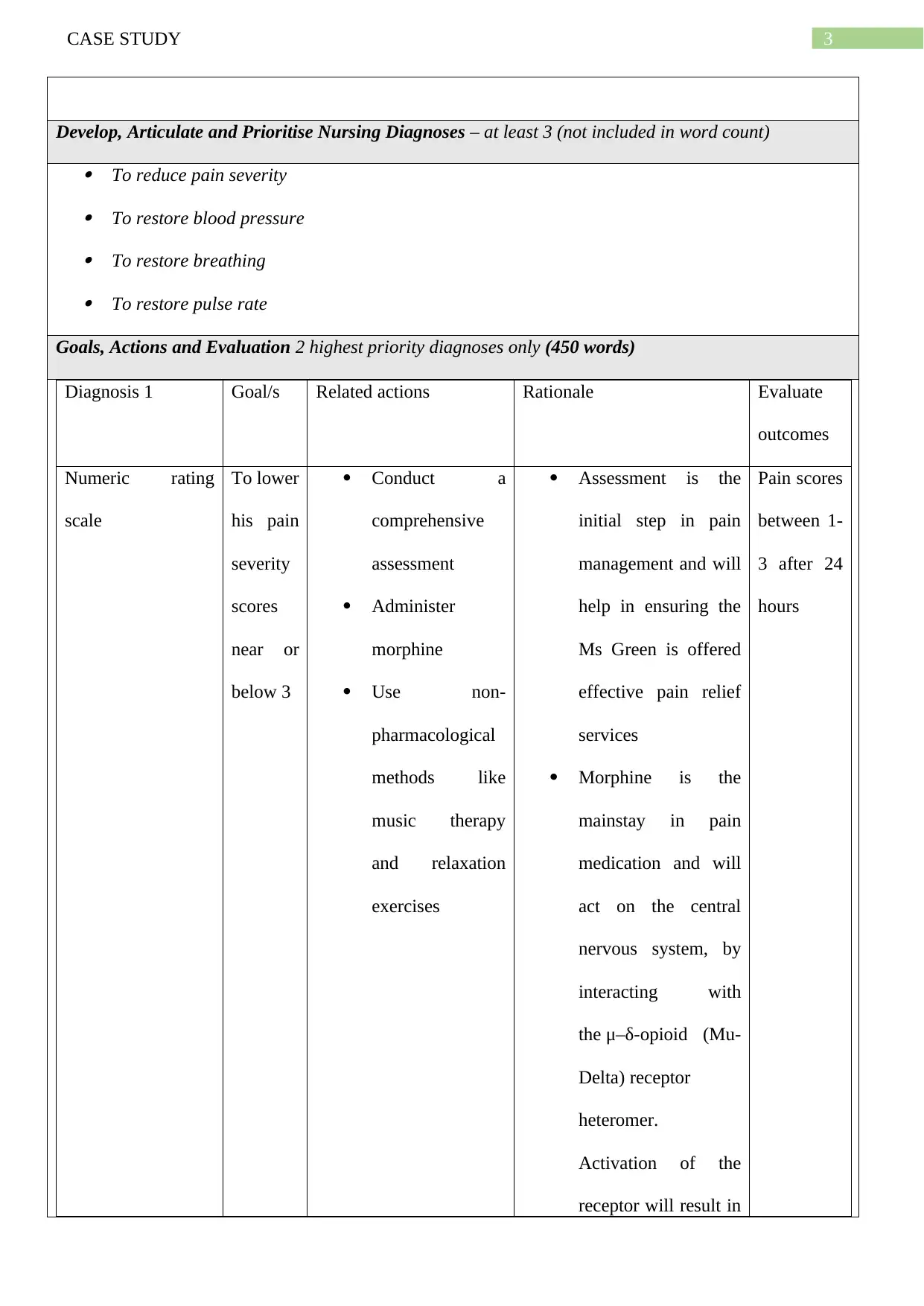
Heart rate monitor To lower
pulse
rate to
60-100
bpm
Limit the intake
of sodium and
fluids
Auscultate heart
sounds
Administer
vasodilators
Fluid and sodium
restriction will
reduce demand on
heart and
extracellular fluid
volume (Lin et al.
2014).
It will help to detect
crackles in lung.
Vasodilators will
dilate the blood
vessels and allow
easy flow of blood
(Mar and Raj 2014).
Pulse rate
will get
restored to
60-100
bpm
onset of analgesia
and will provide
relief from pain
(Kapur, Lala and
Shaw 2014).
Music therapy will
also provide sensory
stimulation and
evoke responses in
the patient, thus
lowering the pain she
feels (Korhan et al.
2014).
Heart rate monitor To lower
pulse
rate to
60-100
bpm
Limit the intake
of sodium and
fluids
Auscultate heart
sounds
Administer
vasodilators
Fluid and sodium
restriction will
reduce demand on
heart and
extracellular fluid
volume (Lin et al.
2014).
It will help to detect
crackles in lung.
Vasodilators will
dilate the blood
vessels and allow
easy flow of blood
(Mar and Raj 2014).
Pulse rate
will get
restored to
60-100
bpm
5CASE STUDY
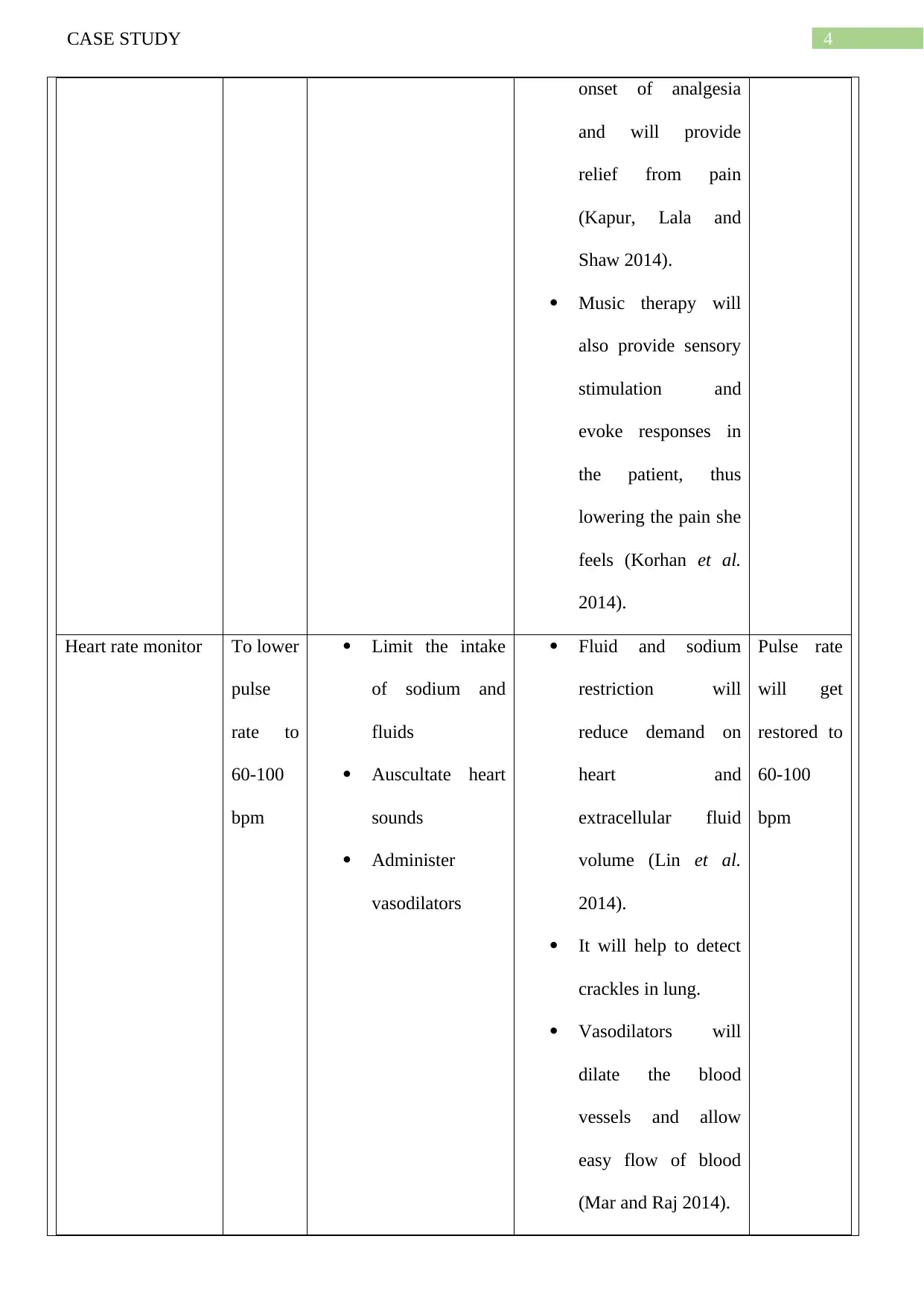
Sphygmomanomete
r
To lower
the
blood
pressure
near
120/80
mm Hg
Monitor and
assess blood
pressure after
every hour
Administration of
blood pressure
lowering agents
like thiazide
diuretics
Administering
adrenergic
antagonists
Auscultating
breathing sound
and heart tone
Maintaining
activity
restrictions
Comparison of blood
pressure will provide
a detailed picture of
vascular involvement
Chlorothiazide and
indapamide are first-
line medications that
will potentiate action
of other
antihypertensive
medications by
bringing about
diuresis, a decrease
in plasma volume
and lowering of
cardiac output
(Musini et al. 2014).
Propranol and
acebutolol will lower
peripheral resistance
and reduce cardiac
output, besides
suppressing renin
release (Phillips et al.
2015).
Prevalence of
S4 heart sound is due
The patient
will report
reduction
in blood
pressure
within 24
hours.
Sphygmomanomete
r
To lower
the
blood
pressure
near
120/80
mm Hg
Monitor and
assess blood
pressure after
every hour
Administration of
blood pressure
lowering agents
like thiazide
diuretics
Administering
adrenergic
antagonists
Auscultating
breathing sound
and heart tone
Maintaining
activity
restrictions
Comparison of blood
pressure will provide
a detailed picture of
vascular involvement
Chlorothiazide and
indapamide are first-
line medications that
will potentiate action
of other
antihypertensive
medications by
bringing about
diuresis, a decrease
in plasma volume
and lowering of
cardiac output
(Musini et al. 2014).
Propranol and
acebutolol will lower
peripheral resistance
and reduce cardiac
output, besides
suppressing renin
release (Phillips et al.
2015).
Prevalence of
S4 heart sound is due
The patient
will report
reduction
in blood
pressure
within 24
hours.
6CASE STUDY
to atrial hypertrophy.
Hearing S3 sound will
indicate the onset of
pulmonary
congestion
Reducing tension and
stress that affects
blood pressure will
also prove effective
in lowering
hypertension. She
will be ensured about
the safety and
wellbeing of her
mother.
Pneumography Restore
breathin
g
Place the patient
with adequate
body alignment
for maximising
the breathing
pattern
Encouraging
deep sustained
breaths by usage
of incentive
spirometer and
demonstrating
Making the patient
sit in fowler position
will enhance
oxygenation and
maximise expansion
of the chest, by
triggering relaxation
of the abdominal
muscle tension
(Costa, Almeida and
Ribeiro 2015).
These techniques will
Respirator
y rate will
get
restored to
12-18
breaths/mi
n
to atrial hypertrophy.
Hearing S3 sound will
indicate the onset of
pulmonary
congestion
Reducing tension and
stress that affects
blood pressure will
also prove effective
in lowering
hypertension. She
will be ensured about
the safety and
wellbeing of her
mother.
Pneumography Restore
breathin
g
Place the patient
with adequate
body alignment
for maximising
the breathing
pattern
Encouraging
deep sustained
breaths by usage
of incentive
spirometer and
demonstrating
Making the patient
sit in fowler position
will enhance
oxygenation and
maximise expansion
of the chest, by
triggering relaxation
of the abdominal
muscle tension
(Costa, Almeida and
Ribeiro 2015).
These techniques will
Respirator
y rate will
get
restored to
12-18
breaths/mi
n
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CASE STUDY
slow inhalation
Administering
respiratory
medications
Administering
supplementary
oxygen therapy
Providing patient
education on
proper coughing,
breathing and
splinting methods
allow deep
inspiration and
increase oxygenation.
Controlled breathing
will also prevent air
trapping in the
patient
Beta-adrenergic
agonist medications
will lead to the
relaxation of smooth
muscle airways and
result in
bronchodilation of
the air passages
(Spina 2014).
Oxygen therapy
through nasal prongs
will deliver the
oxygen that is
required by the
patient for an
effective breathing
and will prevent
alveolar hypoxia
(Hofmann et al.
2017).
slow inhalation
Administering
respiratory
medications
Administering
supplementary
oxygen therapy
Providing patient
education on
proper coughing,
breathing and
splinting methods
allow deep
inspiration and
increase oxygenation.
Controlled breathing
will also prevent air
trapping in the
patient
Beta-adrenergic
agonist medications
will lead to the
relaxation of smooth
muscle airways and
result in
bronchodilation of
the air passages
(Spina 2014).
Oxygen therapy
through nasal prongs
will deliver the
oxygen that is
required by the
patient for an
effective breathing
and will prevent
alveolar hypoxia
(Hofmann et al.
2017).
8CASE STUDY
Patient education will
permit adequate
mobilisation of the
respiratory secretions
Reference list:
Cassidy, J.D., Boyle, E. and Carroll, L.J., 2014. Population-based, inception cohort study of the incidence,
course, and prognosis of mild traumatic brain injury after motor vehicle collisions. Archives of physical
medicine and rehabilitation, 95(3), pp.S278-S285.
Chen, J.M., Lv, J., Ma, K. and Yan, J., 2014. Assessment of internal mammary artery injury after blunt
chest trauma: a literature review. Journal of Zhejiang University SCIENCE B, 15(10), pp.864-869.
Costa, R., Almeida, N. and Ribeiro, F., 2015. Body position influences the maximum inspiratory and
expiratory mouth pressures of young healthy subjects. Physiotherapy, 101(2), pp.239-241.
Hofmann, R., James, S.K., Jernberg, T., Lindahl, B., Erlinge, D., Witt, N., Arefalk, G., Frick, M.,
Alfredsson, J., Nilsson, L. and Ravn-Fischer, A., 2017. Oxygen therapy in suspected acute myocardial
infarction. New England Journal of Medicine, 377(13), pp.1240-1249.
Kapur, B.M., Lala, P.K. and Shaw, J.L., 2014. Pharmacogenetics of chronic pain management. Clinical
biochemistry, 47(13-14), pp.1169-1187.
Korhan, E.A., Uyar, M., Eyigör, C., Yönt, G.H., Çelik, S. and Khorshıd, L., 2014. The effects of music
therapy on pain in patients with neuropathic pain. Pain Management Nursing, 15(1), pp.306-314.
Lin, J., Han, Z., Li, X., Ochs, T., Zhao, J., Zhang, X., Yang, J., Liu, P., Xiong, Z., Gai, Y. and Tang, C.,
2014. Risk factors for postural tachycardia syndrome in children and adolescents. PLoS One, 9(12),
p.e113625.
Mar, P.L. and Raj, S.R., 2014. Neuronal and hormonal perturbations in postural tachycardia
syndrome. Frontiers in physiology, 5, p.220.
McCarthy, E.F. and Frassica, F.J., 2014. Pathology of bone and joint disorders: with clinical and
radiographic correlation. Cambridge University Press.
Musini, V.M., Nazer, M., Bassett, K. and Wright, J.M., 2014. Blood pressure‐lowering efficacy of
Patient education will
permit adequate
mobilisation of the
respiratory secretions
Reference list:
Cassidy, J.D., Boyle, E. and Carroll, L.J., 2014. Population-based, inception cohort study of the incidence,
course, and prognosis of mild traumatic brain injury after motor vehicle collisions. Archives of physical
medicine and rehabilitation, 95(3), pp.S278-S285.
Chen, J.M., Lv, J., Ma, K. and Yan, J., 2014. Assessment of internal mammary artery injury after blunt
chest trauma: a literature review. Journal of Zhejiang University SCIENCE B, 15(10), pp.864-869.
Costa, R., Almeida, N. and Ribeiro, F., 2015. Body position influences the maximum inspiratory and
expiratory mouth pressures of young healthy subjects. Physiotherapy, 101(2), pp.239-241.
Hofmann, R., James, S.K., Jernberg, T., Lindahl, B., Erlinge, D., Witt, N., Arefalk, G., Frick, M.,
Alfredsson, J., Nilsson, L. and Ravn-Fischer, A., 2017. Oxygen therapy in suspected acute myocardial
infarction. New England Journal of Medicine, 377(13), pp.1240-1249.
Kapur, B.M., Lala, P.K. and Shaw, J.L., 2014. Pharmacogenetics of chronic pain management. Clinical
biochemistry, 47(13-14), pp.1169-1187.
Korhan, E.A., Uyar, M., Eyigör, C., Yönt, G.H., Çelik, S. and Khorshıd, L., 2014. The effects of music
therapy on pain in patients with neuropathic pain. Pain Management Nursing, 15(1), pp.306-314.
Lin, J., Han, Z., Li, X., Ochs, T., Zhao, J., Zhang, X., Yang, J., Liu, P., Xiong, Z., Gai, Y. and Tang, C.,
2014. Risk factors for postural tachycardia syndrome in children and adolescents. PLoS One, 9(12),
p.e113625.
Mar, P.L. and Raj, S.R., 2014. Neuronal and hormonal perturbations in postural tachycardia
syndrome. Frontiers in physiology, 5, p.220.
McCarthy, E.F. and Frassica, F.J., 2014. Pathology of bone and joint disorders: with clinical and
radiographic correlation. Cambridge University Press.
Musini, V.M., Nazer, M., Bassett, K. and Wright, J.M., 2014. Blood pressure‐lowering efficacy of
9CASE STUDY
monotherapy with thiazide diuretics for primary hypertension. Cochrane Database of Systematic Reviews,
(5).
Phillips, A.A., Elliott, S.L., Zheng, M.M. and Krassioukov, A.V., 2015. Selective alpha adrenergic
antagonist reduces severity of transient hypertension during sexual stimulation after spinal cord
injury. Journal of neurotrauma, 32(6), pp.392-396.
Sommer, C., 2016. Exploring pain pathophysiology in patients. Science, 354(6312), pp.588-592.
Spina, D., 2014. Current and novel bronchodilators in respiratory disease. Current opinion in pulmonary
medicine, 20(1), pp.73-86.
Yang, S., Nguyen, N.D., Center, J.R., Eisman, J.A. and Nguyen, T.V., 2014. Association between
hypertension and fragility fracture: a longitudinal study. Osteoporosis International, 25(1), pp.97-103.
monotherapy with thiazide diuretics for primary hypertension. Cochrane Database of Systematic Reviews,
(5).
Phillips, A.A., Elliott, S.L., Zheng, M.M. and Krassioukov, A.V., 2015. Selective alpha adrenergic
antagonist reduces severity of transient hypertension during sexual stimulation after spinal cord
injury. Journal of neurotrauma, 32(6), pp.392-396.
Sommer, C., 2016. Exploring pain pathophysiology in patients. Science, 354(6312), pp.588-592.
Spina, D., 2014. Current and novel bronchodilators in respiratory disease. Current opinion in pulmonary
medicine, 20(1), pp.73-86.
Yang, S., Nguyen, N.D., Center, J.R., Eisman, J.A. and Nguyen, T.V., 2014. Association between
hypertension and fragility fracture: a longitudinal study. Osteoporosis International, 25(1), pp.97-103.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





