Assignment on Childhood Obesity in Queensland
VerifiedAdded on 2022/09/10
|1
|2109
|20
Presentation
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
CHILDHOOD OBESITY IN QUEENSLAND
IMPACT, KEY AREAS OF CONCERN AND ACTION PLAN
CHILDHOOD OBESITY IN QUEENSLAND
About one in four children (5–17 years) in Australia are the sufferers of
childhood obesity. Proportions of obesity and combined overweight and
obesity are higher in aboriginal children compared with non-Aboriginal
children at several ages, especially in the region of rural Queensland. In
2012–13, 30% of Indigenous Queenslander children aged 5–17 years were
estimated to be overweight or obese, amongst which 17% were overweight
and 13% were obese. As per 2016 data, 1 in 14 aboriginal children is obese
as compared to about 1 in 50 three decades ago. It is projected that by
2026, there will be altogether 250,000 overweight and obese children
(Health.qld.gov.au, 2020).
IMPACTS OF OVERWEIGHT AND OBESITY
Childhood overweight or obesity has several effects at the individual, community, and population levels in rural Queensland
(McDermott et al., 2009).
• Prolonged health conditions are more tenacious in obese individuals, both at an early age and in those who go on to become
obese or overweight as adults. The outcome of childhood obesity includes a greater risk of breathing difficulties, poor bone
health, hypertension, insulin resistance, and early indicators of cardiovascular disease. Obese adults who were overweight as
adolescents have larger levels of weight-induced health issues and a higher risk of mortality than adults who developed
obesity only in adulthood. Childhood obesity is related to increased morbidity and mortality in adults from cardiovascular
diseases regardless of their weight in matured ages. Childhood obesity also contributes to financial burden at the population
level of Queensland, where more than 35% of the hospital costs are associated with obesity-related illnesses. Obese and
overweight children in Queensland also suffer from bullying, peer pressure, low self-esteem, and body image issues.
Overweight adolescents are also vulnerable to become socially isolated than teenagers of healthy weight
• Impact on an individual Queenslander child-
• Overweight and obesity in childhood is an intricate health concern with the involvement of multiple social, ecological, and
biological aspects contributing to the increase in weight. It is associated with both short and long term serious ill health.
Hypertension, type 2 diabetes mellitus, cardiovascular complications, and transition into adulthood exerts a substantial
impression on optimal health and wellbeing. The psychological, emotional, and cognitive health of a child may also get
disrupted by hurting their quality of life, self-esteem, and body image.
• Impact on the community-
• Poor nutrition, physical inactivity, tobacco smoking and alcohol misuse are four major risk factors that affect all the school-
going children in Queensland. Subsequently, these lead to shortened life expectancy in this generation of children, as they are
more likely to be the victim of obesity-induced diseases.
• Impact on population-
• The direct and indirect effects of obesity have adverse health consequences that reduce the quality of life. It leads to a
negative economic outcome for the entire population. The most recent financial cost analysis in 2015 found that the costs
associated with obesity were estimated at $1.72 billion in Queensland. Loss of wellbeing and early death because of obesity
cost the economy around $9.5 billion in Queensland. The aggregate financial cost of obesity in Queensland stood at
$11.2billion in 2015.
KEY AREAS OF CHANGE REQUIRED:
• Increasing the number of public health policies that address the childhood obesity concern among aboriginal children
• Eliminating the social and health disparities that exist through implementing appropriate strategies
• Increased consumption of energy-dense foods that are low on nutrients, such as ready-to-eat meals high in fat or sugar or sodas and aerated drinks having empty calories and little
intake of vegetables and fruit.
• A sedentary lifestyle pattern and low levels of physical activity induces an obesogenic environment and amplifies the risk of getting obesity-related health issues
• The risk of a child becoming obese or overweight develops from poor nutritional habits during pregnancy. Such deficit in maternal nutrition gives rise to accompanying comorbidities
such as metabolic syndrome, insulin resistance, dyslipidemia and hypertension.
• Easy availability of energy-dense foods and rapid accessibility to ‘fast’ or ‘junk’ foods, as they are often economically priced. These foods provide excessive calories, saturated fats,
refined sugars and salt, and very less beneficial nutrients. The frequent presence of convenience food and drinks at school tuck-shops, community sporting clubs and workplaces is
also an area of concern.
• Socioeconomically deprived children and adolescents who live in hostile conditions, and face unsupportive behavior from the surroundings indulge in obesogenic activities and hardly
get exposed to a healthy lifestyle
• The inadequacy of the indigenous childhood obesity prevention programs in recognizing the potential social and economic elements, and not only the individual factors that contribute to
childhood obesity.
• School issues that elevate the level of stress and induce binge eating pattern in children
•
ACTION PLAN TO BE TAKEN
• All the children of Queensland, especially the indigenous ones, are growing up in an obesogenic environment that
encourages weight gain and obesity. Instead of focusing on a single intervention to address the rising obesity epidemic,
a whole of government approach is vital to mitigate childhood obesity and to treat children who are already overweight or
obese.
• Childhood overweight and obesity can only be tackled by a collective group of allies and shareholders from the domain
of health and beyond. Key stakeholders will vary depending on the specific health setting and has to be based on a local
level. This may require the participation of community group representatives, shoppers, patrons, private enterprises,
child care and health services, schools, primary care providers, sports organizations, and different governmental levels.
• The necessary action to address the childhood obesity burden among Aboriginal children should take an approach of
empowering the indigenous communities and eliminating the current health and social inequalities. Governments must
work collaboratively with Aboriginal communities to cultivate and implement strategies and policies that adequately
address inequities witnessed in childhood obesity and other ailments. Through this approach, a sincere co-designing of
public health promotional activities and obesity prevention curriculums must be ensured, which effectively supports the
expansion, valuation, and potential scaling up of programs established for and by Aboriginal communities.
• To ensure the effectiveness of the interventions targeting aboriginal childhood obesity, there should be government
commitment towards implementation work, aboriginal leadership policies, and developing relevant programs.
Governments need to adopt a two-way approach to accomplish this by sharing power and control with aboriginal
communities. There is also a need for the indigenous people and organizations to define the success parameters of a
program and lead the ongoing estimation.
• Management of the childhood obesity epidemic also requires the assimilation of evidence-based services along with
strong assurance, promise, and actively engaging with the community, government, and health professionals.
• Capabilities of the health professionals should be improved and enhanced in preventing and managing childhood
obesity, with the focus on education, training, and supply of up to date and factual resources and reliable tools.
• Multiple formats of prevention and treatment programs must be implemented, which are flexible, scalable, and easily
accessible to the healthcare workers and consumers equally.
• The various stages of the lifespan, such as preconception, pregnancy, infancy, and childhood, should be considered
while planning the action plan, with critically addressing each time period of the life-course, to ensure the success of the
programs.
BIBLIOGRAPHY
• Alsharairi, N. A. (2018). Current government actions and potential policy options for reducing obesity in
Queensland schools. Children, 5(2), 18.
• Cameron, C. M., Shibl, R., McClure, R. J., Ng, S. K., & Hills, A. P. (2014). Maternal pregravid body mass
index and child hospital admissions in the first 5 years of life: results from an Australian birth cohort.
International journal of obesity, 38(10), 1268-1274.
• Clemens, S. L., & Lincoln, D. J. (2018). Where children play most: physical activity levels of school
children across four settings and policy implications. Australian and New Zealand journal of public health,
42(6), 575-581.
• Croyden, D. L., Vidgen, H. A., Esdaile, E., Hernandez, E., Magarey, A., Moores, C. J., & Daniels, L. (2018).
A narrative account of implementation lessons learnt from the dissemination of an up-scaled state-wide
child obesity management program in Australia: PEACH™(Parenting, Eating and Activity for Child Health)
Queensland. BMC public health, 18(1), 347.
• Growinggoodhabits.health.qld.gov.au. (2020). Retrieved 5 April 2020, from
https://www.growinggoodhabits.health.qld.gov.au/wp-content/uploads/PDF/health-professionals/An-integrat
ed-approach-for-tackling-childhood-overweight-and-obesity-in-Queensland-overview.pdf
• Health.qld.gov.au. (2015). Retrieved 4 April 2020, from
https://www.health.qld.gov.au/__data/assets/pdf_file/0020/441092/qcs-pp-1507-young.pdf
• Health.qld.gov.au. (2020). Retrieved 4 April 2020, from
https://www.health.qld.gov.au/__data/assets/pdf_file/0018/641331/health-disparities-in-queensland-childre
n.pdf
• Huse, O., Hettiarachchi, J., Gearon, E., Nichols, M., Allender, S., & Peeters, A. (2018). Obesity in Australia.
Obesity research & clinical practice, 12(1), 29-39.
• Ingram, L., Brumpton, K., & Kitchener, S. CHILDHOOD OBESITY IN RURAL QUEENSLAND: HOW BIG IS
THE PROBLEM?.
• Lee, A., & Minniecon, D. L. (2014). Healthy start: Closing the gap on Indigenous childhood obesity. The
Conversation, (16).
• Love, P., & Vidgen, H. (2016). Policy and practice in managing childhood obesity: Implementation case
studies in Queensland and NSW.
• McDermott, R., Campbell, S., Li, M., & McCulloch, B. (2009). The health and nutrition of young indigenous
women in north Queensland–intergenerational implications of poor food quality, obesity, diabetes, tobacco
smoking and alcohol use. Public health nutrition, 12(11), 2143-2149.
• Mihrshahi, S., Vaughan, L., Fa’avale, N., Weliange, S. D. S., Manu-Sione, I., & Schubert, L. (2017).
Evaluation of the Good Start Program: a healthy eating and physical activity intervention for Maori and
Pacific Islander children living in Queensland, Australia. BMC public health, 17(1), 77.
• Sanders, R. H., Han, A., Baker, J. S., & Cobley, S. (2015). Childhood obesity and its physical and
psychological co-morbidities: a systematic review of Australian children and adolescents. European journal
of pediatrics, 174(6), 715-746.
• Thurber, K., Boxall, A. M., & Partel, K. (2014). Overweight and obesity among Indigenous children:
individual and social determinants. Canberra: Deeble Institute.
•
Vidgen, H. A., Love, P. V., Wutzke, S. E., Daniels, L. A., Rissel, C. E., Innes-Hughes, C., & Baur, L. A.
(2018). A description of health care system factors in the implementation of universal weight management
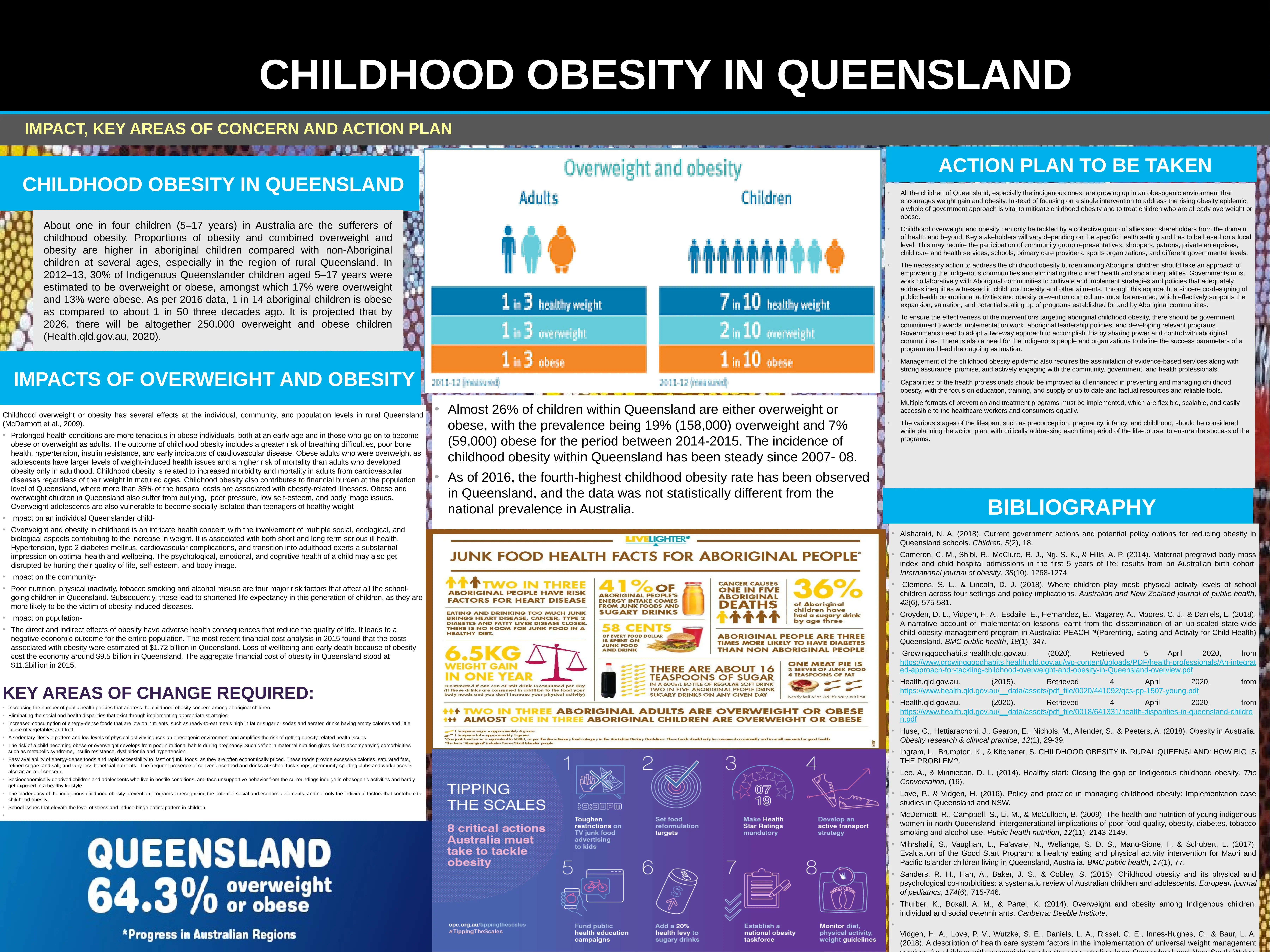
• Almost 26% of children within Queensland are either overweight or
obese, with the prevalence being 19% (158,000) overweight and 7%
(59,000) obese for the period between 2014-2015. The incidence of
childhood obesity within Queensland has been steady since 2007- 08.
• As of 2016, the fourth-highest childhood obesity rate has been observed
in Queensland, and the data was not statistically different from the
national prevalence in Australia.
IMPACT, KEY AREAS OF CONCERN AND ACTION PLAN
CHILDHOOD OBESITY IN QUEENSLAND
About one in four children (5–17 years) in Australia are the sufferers of
childhood obesity. Proportions of obesity and combined overweight and
obesity are higher in aboriginal children compared with non-Aboriginal
children at several ages, especially in the region of rural Queensland. In
2012–13, 30% of Indigenous Queenslander children aged 5–17 years were
estimated to be overweight or obese, amongst which 17% were overweight
and 13% were obese. As per 2016 data, 1 in 14 aboriginal children is obese
as compared to about 1 in 50 three decades ago. It is projected that by
2026, there will be altogether 250,000 overweight and obese children
(Health.qld.gov.au, 2020).
IMPACTS OF OVERWEIGHT AND OBESITY
Childhood overweight or obesity has several effects at the individual, community, and population levels in rural Queensland
(McDermott et al., 2009).
• Prolonged health conditions are more tenacious in obese individuals, both at an early age and in those who go on to become
obese or overweight as adults. The outcome of childhood obesity includes a greater risk of breathing difficulties, poor bone
health, hypertension, insulin resistance, and early indicators of cardiovascular disease. Obese adults who were overweight as
adolescents have larger levels of weight-induced health issues and a higher risk of mortality than adults who developed
obesity only in adulthood. Childhood obesity is related to increased morbidity and mortality in adults from cardiovascular
diseases regardless of their weight in matured ages. Childhood obesity also contributes to financial burden at the population
level of Queensland, where more than 35% of the hospital costs are associated with obesity-related illnesses. Obese and
overweight children in Queensland also suffer from bullying, peer pressure, low self-esteem, and body image issues.
Overweight adolescents are also vulnerable to become socially isolated than teenagers of healthy weight
• Impact on an individual Queenslander child-
• Overweight and obesity in childhood is an intricate health concern with the involvement of multiple social, ecological, and
biological aspects contributing to the increase in weight. It is associated with both short and long term serious ill health.
Hypertension, type 2 diabetes mellitus, cardiovascular complications, and transition into adulthood exerts a substantial
impression on optimal health and wellbeing. The psychological, emotional, and cognitive health of a child may also get
disrupted by hurting their quality of life, self-esteem, and body image.
• Impact on the community-
• Poor nutrition, physical inactivity, tobacco smoking and alcohol misuse are four major risk factors that affect all the school-
going children in Queensland. Subsequently, these lead to shortened life expectancy in this generation of children, as they are
more likely to be the victim of obesity-induced diseases.
• Impact on population-
• The direct and indirect effects of obesity have adverse health consequences that reduce the quality of life. It leads to a
negative economic outcome for the entire population. The most recent financial cost analysis in 2015 found that the costs
associated with obesity were estimated at $1.72 billion in Queensland. Loss of wellbeing and early death because of obesity
cost the economy around $9.5 billion in Queensland. The aggregate financial cost of obesity in Queensland stood at
$11.2billion in 2015.
KEY AREAS OF CHANGE REQUIRED:
• Increasing the number of public health policies that address the childhood obesity concern among aboriginal children
• Eliminating the social and health disparities that exist through implementing appropriate strategies
• Increased consumption of energy-dense foods that are low on nutrients, such as ready-to-eat meals high in fat or sugar or sodas and aerated drinks having empty calories and little
intake of vegetables and fruit.
• A sedentary lifestyle pattern and low levels of physical activity induces an obesogenic environment and amplifies the risk of getting obesity-related health issues
• The risk of a child becoming obese or overweight develops from poor nutritional habits during pregnancy. Such deficit in maternal nutrition gives rise to accompanying comorbidities
such as metabolic syndrome, insulin resistance, dyslipidemia and hypertension.
• Easy availability of energy-dense foods and rapid accessibility to ‘fast’ or ‘junk’ foods, as they are often economically priced. These foods provide excessive calories, saturated fats,
refined sugars and salt, and very less beneficial nutrients. The frequent presence of convenience food and drinks at school tuck-shops, community sporting clubs and workplaces is
also an area of concern.
• Socioeconomically deprived children and adolescents who live in hostile conditions, and face unsupportive behavior from the surroundings indulge in obesogenic activities and hardly
get exposed to a healthy lifestyle
• The inadequacy of the indigenous childhood obesity prevention programs in recognizing the potential social and economic elements, and not only the individual factors that contribute to
childhood obesity.
• School issues that elevate the level of stress and induce binge eating pattern in children
•
ACTION PLAN TO BE TAKEN
• All the children of Queensland, especially the indigenous ones, are growing up in an obesogenic environment that
encourages weight gain and obesity. Instead of focusing on a single intervention to address the rising obesity epidemic,
a whole of government approach is vital to mitigate childhood obesity and to treat children who are already overweight or
obese.
• Childhood overweight and obesity can only be tackled by a collective group of allies and shareholders from the domain
of health and beyond. Key stakeholders will vary depending on the specific health setting and has to be based on a local
level. This may require the participation of community group representatives, shoppers, patrons, private enterprises,
child care and health services, schools, primary care providers, sports organizations, and different governmental levels.
• The necessary action to address the childhood obesity burden among Aboriginal children should take an approach of
empowering the indigenous communities and eliminating the current health and social inequalities. Governments must
work collaboratively with Aboriginal communities to cultivate and implement strategies and policies that adequately
address inequities witnessed in childhood obesity and other ailments. Through this approach, a sincere co-designing of
public health promotional activities and obesity prevention curriculums must be ensured, which effectively supports the
expansion, valuation, and potential scaling up of programs established for and by Aboriginal communities.
• To ensure the effectiveness of the interventions targeting aboriginal childhood obesity, there should be government
commitment towards implementation work, aboriginal leadership policies, and developing relevant programs.
Governments need to adopt a two-way approach to accomplish this by sharing power and control with aboriginal
communities. There is also a need for the indigenous people and organizations to define the success parameters of a
program and lead the ongoing estimation.
• Management of the childhood obesity epidemic also requires the assimilation of evidence-based services along with
strong assurance, promise, and actively engaging with the community, government, and health professionals.
• Capabilities of the health professionals should be improved and enhanced in preventing and managing childhood
obesity, with the focus on education, training, and supply of up to date and factual resources and reliable tools.
• Multiple formats of prevention and treatment programs must be implemented, which are flexible, scalable, and easily
accessible to the healthcare workers and consumers equally.
• The various stages of the lifespan, such as preconception, pregnancy, infancy, and childhood, should be considered
while planning the action plan, with critically addressing each time period of the life-course, to ensure the success of the
programs.
BIBLIOGRAPHY
• Alsharairi, N. A. (2018). Current government actions and potential policy options for reducing obesity in
Queensland schools. Children, 5(2), 18.
• Cameron, C. M., Shibl, R., McClure, R. J., Ng, S. K., & Hills, A. P. (2014). Maternal pregravid body mass
index and child hospital admissions in the first 5 years of life: results from an Australian birth cohort.
International journal of obesity, 38(10), 1268-1274.
• Clemens, S. L., & Lincoln, D. J. (2018). Where children play most: physical activity levels of school
children across four settings and policy implications. Australian and New Zealand journal of public health,
42(6), 575-581.
• Croyden, D. L., Vidgen, H. A., Esdaile, E., Hernandez, E., Magarey, A., Moores, C. J., & Daniels, L. (2018).
A narrative account of implementation lessons learnt from the dissemination of an up-scaled state-wide
child obesity management program in Australia: PEACH™(Parenting, Eating and Activity for Child Health)
Queensland. BMC public health, 18(1), 347.
• Growinggoodhabits.health.qld.gov.au. (2020). Retrieved 5 April 2020, from
https://www.growinggoodhabits.health.qld.gov.au/wp-content/uploads/PDF/health-professionals/An-integrat
ed-approach-for-tackling-childhood-overweight-and-obesity-in-Queensland-overview.pdf
• Health.qld.gov.au. (2015). Retrieved 4 April 2020, from
https://www.health.qld.gov.au/__data/assets/pdf_file/0020/441092/qcs-pp-1507-young.pdf
• Health.qld.gov.au. (2020). Retrieved 4 April 2020, from
https://www.health.qld.gov.au/__data/assets/pdf_file/0018/641331/health-disparities-in-queensland-childre
n.pdf
• Huse, O., Hettiarachchi, J., Gearon, E., Nichols, M., Allender, S., & Peeters, A. (2018). Obesity in Australia.
Obesity research & clinical practice, 12(1), 29-39.
• Ingram, L., Brumpton, K., & Kitchener, S. CHILDHOOD OBESITY IN RURAL QUEENSLAND: HOW BIG IS
THE PROBLEM?.
• Lee, A., & Minniecon, D. L. (2014). Healthy start: Closing the gap on Indigenous childhood obesity. The
Conversation, (16).
• Love, P., & Vidgen, H. (2016). Policy and practice in managing childhood obesity: Implementation case
studies in Queensland and NSW.
• McDermott, R., Campbell, S., Li, M., & McCulloch, B. (2009). The health and nutrition of young indigenous
women in north Queensland–intergenerational implications of poor food quality, obesity, diabetes, tobacco
smoking and alcohol use. Public health nutrition, 12(11), 2143-2149.
• Mihrshahi, S., Vaughan, L., Fa’avale, N., Weliange, S. D. S., Manu-Sione, I., & Schubert, L. (2017).
Evaluation of the Good Start Program: a healthy eating and physical activity intervention for Maori and
Pacific Islander children living in Queensland, Australia. BMC public health, 17(1), 77.
• Sanders, R. H., Han, A., Baker, J. S., & Cobley, S. (2015). Childhood obesity and its physical and
psychological co-morbidities: a systematic review of Australian children and adolescents. European journal
of pediatrics, 174(6), 715-746.
• Thurber, K., Boxall, A. M., & Partel, K. (2014). Overweight and obesity among Indigenous children:
individual and social determinants. Canberra: Deeble Institute.
•
Vidgen, H. A., Love, P. V., Wutzke, S. E., Daniels, L. A., Rissel, C. E., Innes-Hughes, C., & Baur, L. A.
(2018). A description of health care system factors in the implementation of universal weight management
• Almost 26% of children within Queensland are either overweight or
obese, with the prevalence being 19% (158,000) overweight and 7%
(59,000) obese for the period between 2014-2015. The incidence of
childhood obesity within Queensland has been steady since 2007- 08.
• As of 2016, the fourth-highest childhood obesity rate has been observed
in Queensland, and the data was not statistically different from the
national prevalence in Australia.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1 out of 1
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





