Heart Failure and Associated Conditions
VerifiedAdded on 2021/04/21
|14
|4275
|75
AI Summary
This assignment focuses on various studies and research related to heart failure, covering topics such as predictors of new-onset heart failure, glucose and obesity's impact on heart health, low-density lipoprotein cholesterol's effect on coronary heart disease, and more. It also touches upon arrhythmias in heart failure and the importance of fluid management in patients with chronic heart failure.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Running head:CLINICAL CARE
Student Name:
Jaspreet kaur
SID:
100554931
Student e-Mail Address:
prabhjaspreet001@gmail.com
Contact Number:
0406303876
Subject: NSG2101, Clinical Care-A Group: C
Assessment Topic:
M.G, 68 years old/female/CHF, (part-A)
Lecturer: Virginia Plummer Word Count: 1611
Due Date: Sunday 15th April 2018
(23.59hrs) Date Submitted: 11/03/2018
Plagiarism, like cheating and collusion, is when you are dishonest about the source of
information that you include in your work. When you have academic honesty you do not
plagiarise, cheat or collude and you respect copyright.
Plagiarism is the taking, and representing as your own, material or ideas which has been
prepared or written by another person.
Cheating is when you wilfully deceive, or assist others to deceive, the development of
your work for assessment. This may be in exams, assignments or other forms of
assessment.
Collusion is a form of cheating in which you have copied the work of another, or worked
closely with others, in developing work that you present as your own.
Cheating and collusion are intentional acts to deceive and have serious consequences. This also
applies to plagiarism; however, plagiarism sometimes can be unintentional, but this will still incur
serious penalties. It is important that you, the student, are fully aware of what plagiarism is and
how to avoid it.
Student Declaration:
1. I have used the Institutes referencing guide
http://www.holmesglen.edu.au/services/learning_commons_library/research_tools/
referencing_guide
2. I am aware that penalties exist for plagiarism, cheating and unauthorised collusion with
other students, or external consultants.
3. I am aware that if I do not comply with copyright laws that I am being dishonest and will be
Student Name:
Jaspreet kaur
SID:
100554931
Student e-Mail Address:
prabhjaspreet001@gmail.com
Contact Number:
0406303876
Subject: NSG2101, Clinical Care-A Group: C
Assessment Topic:
M.G, 68 years old/female/CHF, (part-A)
Lecturer: Virginia Plummer Word Count: 1611
Due Date: Sunday 15th April 2018
(23.59hrs) Date Submitted: 11/03/2018
Plagiarism, like cheating and collusion, is when you are dishonest about the source of
information that you include in your work. When you have academic honesty you do not
plagiarise, cheat or collude and you respect copyright.
Plagiarism is the taking, and representing as your own, material or ideas which has been
prepared or written by another person.
Cheating is when you wilfully deceive, or assist others to deceive, the development of
your work for assessment. This may be in exams, assignments or other forms of
assessment.
Collusion is a form of cheating in which you have copied the work of another, or worked
closely with others, in developing work that you present as your own.
Cheating and collusion are intentional acts to deceive and have serious consequences. This also
applies to plagiarism; however, plagiarism sometimes can be unintentional, but this will still incur
serious penalties. It is important that you, the student, are fully aware of what plagiarism is and
how to avoid it.
Student Declaration:
1. I have used the Institutes referencing guide
http://www.holmesglen.edu.au/services/learning_commons_library/research_tools/
referencing_guide
2. I am aware that penalties exist for plagiarism, cheating and unauthorised collusion with
other students, or external consultants.
3. I am aware that if I do not comply with copyright laws that I am being dishonest and will be
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1CLINICAL CARE
penalised.
4. Before submitting this assignment, I have used the referencing guide; Turnitin & EndNote
Web
5. I am aware of the requirements covering style and layout standards as described in my
course outline
6. I have retained a copy of this assignment
I have read the above and make the following declaration:
I declare the above statements to be true.
*************All students MUST sign this declaration *******************************
Please commence your Assignment on the next page.
penalised.
4. Before submitting this assignment, I have used the referencing guide; Turnitin & EndNote
Web
5. I am aware of the requirements covering style and layout standards as described in my
course outline
6. I have retained a copy of this assignment
I have read the above and make the following declaration:
I declare the above statements to be true.
*************All students MUST sign this declaration *******************************
Please commence your Assignment on the next page.
2CLINICAL CARE
Introduction
Clinical reasoning is the process by which the care providers are to collect cues or patient information, process the collected information, point out the patient problems or situation,
plan and correspondingly implement appropriate interventions, assess the outcomes, and successively reflect on the entire nursing process. The clinical reasoning cycle is a notable
framework that allows nurses to demonstrate problem solving, clinical judgment, clinical reasoning and decision-making skills. The present paper is based on the case study of M.G, a 68-
year-old female patient whose chief diagnosisis congestive heart failure (CCF). A concept map is provided for the case study and each of steps 1-3 of the clinical reasoning cycle is
explained. The purpose is to highlight the physiology presented in the case study.
Introduction
Clinical reasoning is the process by which the care providers are to collect cues or patient information, process the collected information, point out the patient problems or situation,
plan and correspondingly implement appropriate interventions, assess the outcomes, and successively reflect on the entire nursing process. The clinical reasoning cycle is a notable
framework that allows nurses to demonstrate problem solving, clinical judgment, clinical reasoning and decision-making skills. The present paper is based on the case study of M.G, a 68-
year-old female patient whose chief diagnosisis congestive heart failure (CCF). A concept map is provided for the case study and each of steps 1-3 of the clinical reasoning cycle is
explained. The purpose is to highlight the physiology presented in the case study.
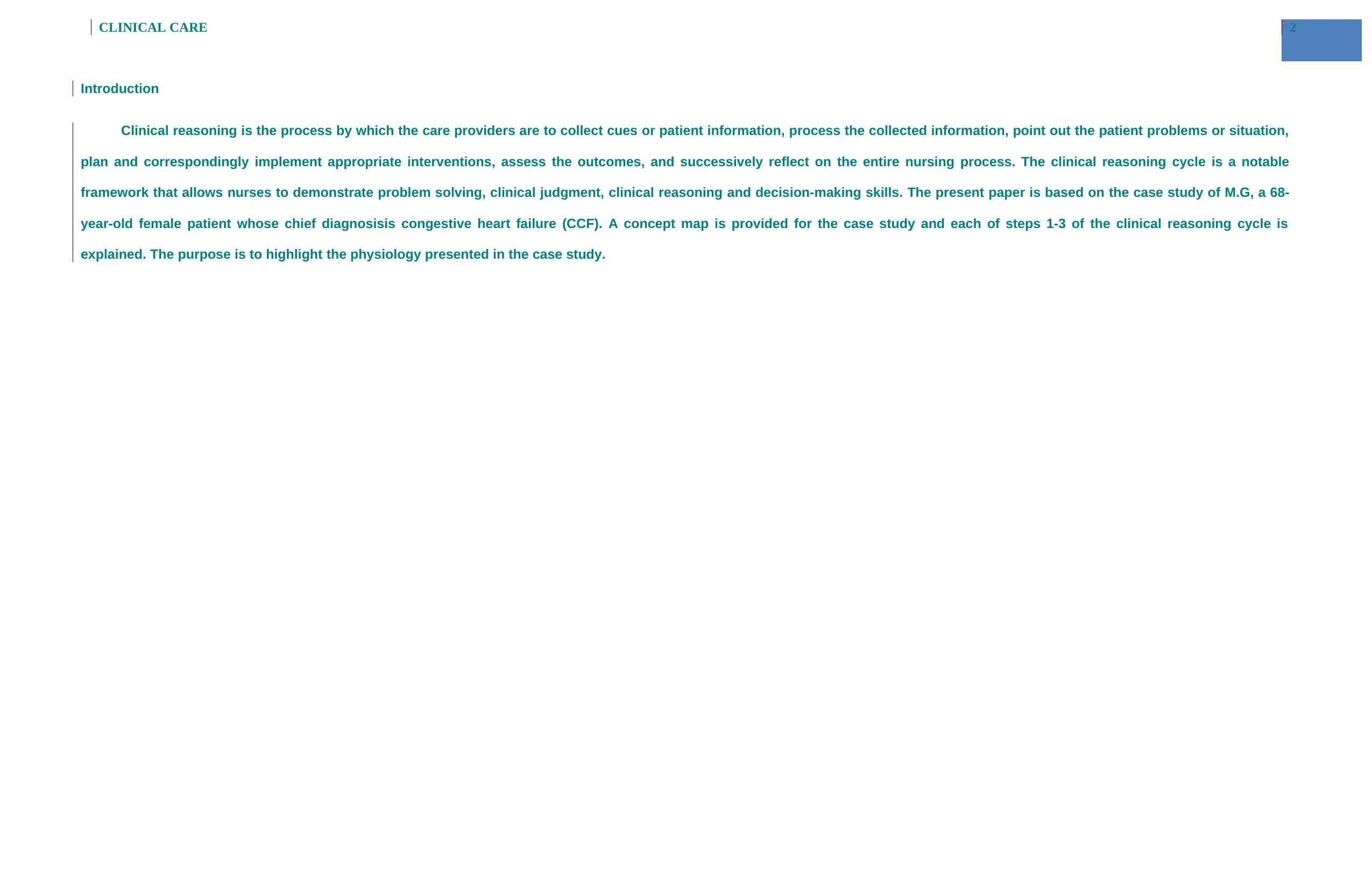
3CLINICAL CARE
CUES
Discharged from the hospital 11days back after diagnosis of congestive
heart failure, shortness of breath and poor mobility due to swelling of legs,
non-adherence to the fluids and salt intake restrictions, Newly Diagnosis-
Atrial Fibrillation.
Hx: - Hypertension, acute myocardial infarction x 4 years, chronic renal
failure, Diabetes type-2, hyperlipidaemia (high cholesterol),
cholecystectomy, hysterectomy. Pulse-122/min, irregular, BP-160/100, R/R-
26/min, Temp-37.3 Celsius, sat. O2-93% on room air.
Risk Factors
Diabetes type-2
Chronic renal failure
Hypertension
Hyperlipidaemia
History of Acute myocardial infarction
Strong family history
M.G, 68 years old/female
Admitted with Congestive heart failure
Married for 45 years
2 children and 6 grandchildren.
CUES
Discharged from the hospital 11days back after diagnosis of congestive
heart failure, shortness of breath and poor mobility due to swelling of legs,
non-adherence to the fluids and salt intake restrictions, Newly Diagnosis-
Atrial Fibrillation.
Hx: - Hypertension, acute myocardial infarction x 4 years, chronic renal
failure, Diabetes type-2, hyperlipidaemia (high cholesterol),
cholecystectomy, hysterectomy. Pulse-122/min, irregular, BP-160/100, R/R-
26/min, Temp-37.3 Celsius, sat. O2-93% on room air.
Risk Factors
Diabetes type-2
Chronic renal failure
Hypertension
Hyperlipidaemia
History of Acute myocardial infarction
Strong family history
M.G, 68 years old/female
Admitted with Congestive heart failure
Married for 45 years
2 children and 6 grandchildren.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4CLINICAL CARE
Medications
Captopril 25mg daily (ACE-inhibitors)- To control high blood pressure by
relaxing blood vessels pressure to work more efficiently.
Enalapril 5mg (ACE-inhibitors)- for heart failure
Hydrochlorothiazide 25mg (diuretics)- To treat oedema, accumulation of
Signs and symptoms
Short of Breath -due to leakage of fluid into lungs.
Swelling of legs- due to build-up of fluid in lower body parts and kidney
failure.
Difficulty in mobility- due to swelling of legs.
Complications
Atrial Fibrillation- Abnormal heart rhythm due to high potassium level (mild
hyperkalaemia). AF leads to clot formation in vein, called vein thrombosis, that clot can
travel to lungs can cause pulmonary embolism and may travel to brain leads to stroke.
Kidney Failure- due to lack of blood supply and kidneys won’t able to remove sufficient
wastes from your blood.
Respiratory failure (pulmonary congestion)- due to build-up of fluids in lungs.
Anaemia and liver damage- due to lack of RBC’s that supply oxygen to body’s tissues and
accumulation of fluid in body.
Pathophysiology
Congestive heart failure (CHF)- ventricles are incapable of pumping
blood to the body in sufficient volume. It causes accumulation of fluid
in lungs and other body parts that leads to short of breath and oedema
od legs.
Rapid and irregular heart beat- weakened heart tries to beat faster to
M.G, 68 years old/ female
Married for 45 years
2 children and 6 grandchildren.
Medications
Captopril 25mg daily (ACE-inhibitors)- To control high blood pressure by
relaxing blood vessels pressure to work more efficiently.
Enalapril 5mg (ACE-inhibitors)- for heart failure
Hydrochlorothiazide 25mg (diuretics)- To treat oedema, accumulation of
Signs and symptoms
Short of Breath -due to leakage of fluid into lungs.
Swelling of legs- due to build-up of fluid in lower body parts and kidney
failure.
Difficulty in mobility- due to swelling of legs.
Complications
Atrial Fibrillation- Abnormal heart rhythm due to high potassium level (mild
hyperkalaemia). AF leads to clot formation in vein, called vein thrombosis, that clot can
travel to lungs can cause pulmonary embolism and may travel to brain leads to stroke.
Kidney Failure- due to lack of blood supply and kidneys won’t able to remove sufficient
wastes from your blood.
Respiratory failure (pulmonary congestion)- due to build-up of fluids in lungs.
Anaemia and liver damage- due to lack of RBC’s that supply oxygen to body’s tissues and
accumulation of fluid in body.
Pathophysiology
Congestive heart failure (CHF)- ventricles are incapable of pumping
blood to the body in sufficient volume. It causes accumulation of fluid
in lungs and other body parts that leads to short of breath and oedema
od legs.
Rapid and irregular heart beat- weakened heart tries to beat faster to
M.G, 68 years old/ female
Married for 45 years
2 children and 6 grandchildren.
5CLINICAL CARE
M.G, 68 years old/female married
for 45 years, 2 children and 6
grandchildren
Laboratory tests
Potassium chloride-5.3mEq/L, (mild hyperkalaemia) (normal value- 3.5mEq/L -5.0mEq/L),Glucose-11.2mmoL (normal range-4-6mmoL)
Creatinine-4.5mg/dl(normal value-0.6-1.2 mg/dl), Sodium-145mEq/L.
BUN-4.3 dl(normal value-7-20mg/dl), Chloride-100mEq/L,
Magnesium-1.9mEq/L,Bicarbonates-27mEq/L.
Chest X-rays-cardiomegaly and consolidation, Radiology shows- pulmonary congestion.
On auscultation- crepitations sounds present due to accumulation of fluid in lungs.
On palpation- Apical pulse (on midclavicular line + 5th intercostal space) found fast and thready.
ECG shows Atrial Fibrillation.
complete the need of body- what is the relevant arrhythmia?.
M.G, 68 years old/female married
for 45 years, 2 children and 6
grandchildren
Laboratory tests
Potassium chloride-5.3mEq/L, (mild hyperkalaemia) (normal value- 3.5mEq/L -5.0mEq/L),Glucose-11.2mmoL (normal range-4-6mmoL)
Creatinine-4.5mg/dl(normal value-0.6-1.2 mg/dl), Sodium-145mEq/L.
BUN-4.3 dl(normal value-7-20mg/dl), Chloride-100mEq/L,
Magnesium-1.9mEq/L,Bicarbonates-27mEq/L.
Chest X-rays-cardiomegaly and consolidation, Radiology shows- pulmonary congestion.
On auscultation- crepitations sounds present due to accumulation of fluid in lungs.
On palpation- Apical pulse (on midclavicular line + 5th intercostal space) found fast and thready.
ECG shows Atrial Fibrillation.
complete the need of body- what is the relevant arrhythmia?.
6CLINICAL CARE
Patho physiology of congestive heart failure
CHF
Steps 1-3 of clinical reasoning cycle applied to the case study
Step 1 – Consider the patient- need to give a summary to the patient’s condition here
MG is a 68 year old female who has been admitted to the emergency department with congestive heart failure (CHF). The main symptoms highlighted by her which has lead to her
immediate admission include shortness in breadth, swelling or fluid accumulation in the hips. Accoridng to M.G, her legs have become as big as tree trunk and she is unable to move.
Moreover, she has gained 5 kgs of weight recently. She also has previous reported cases of chronic renal failure, type 2 diabetes mellitus, hyperlipidemia, HT and AMI (4 years ago). She
also displayed pink skin colour along with fast apical pulse followed by atrial fibrillation, high BP, pulmonary congestion (Scott & Winters, 2015). CHF is defined as a condition where the
muscles of the heat get weakened and thus fail to pump adequate blood to the different parts of the body. CHF can also be defines as the state of heart in which abnormal circulatory
congestion exists that eventually results in heart failure. CHF has different types and this include low output heart failure, high-output heart failure along with right ventricular failure. Low
output heart failure can be further subdivided into systolic heart failure and diastolic heart failure. In CHF, overall the structure of the heart changes due to volume overload and this result in
valvular dysfunction and thus making heart unable to pump adequate blood to the different parts of the body. This leads to the generation of diabetes, severe lung disease, fluid retention,
hyperthyroidism along with abnormal heart rhythms. Fluid retention causes pulmonary edema which increases the systemic pressure and thereby nearing the chances of heart attack. Due
to abnormal structure of the heart like cardiomegally, there occurs stretching of the heart muscles thereby causing cardiac dilation and as a result, mainly the left ventricular side fails to
function normally leading to disruption in the equilibrium in the normal end diastolic volume and thereby increasing the risk of heart disease (Scott & Winters, 2015).
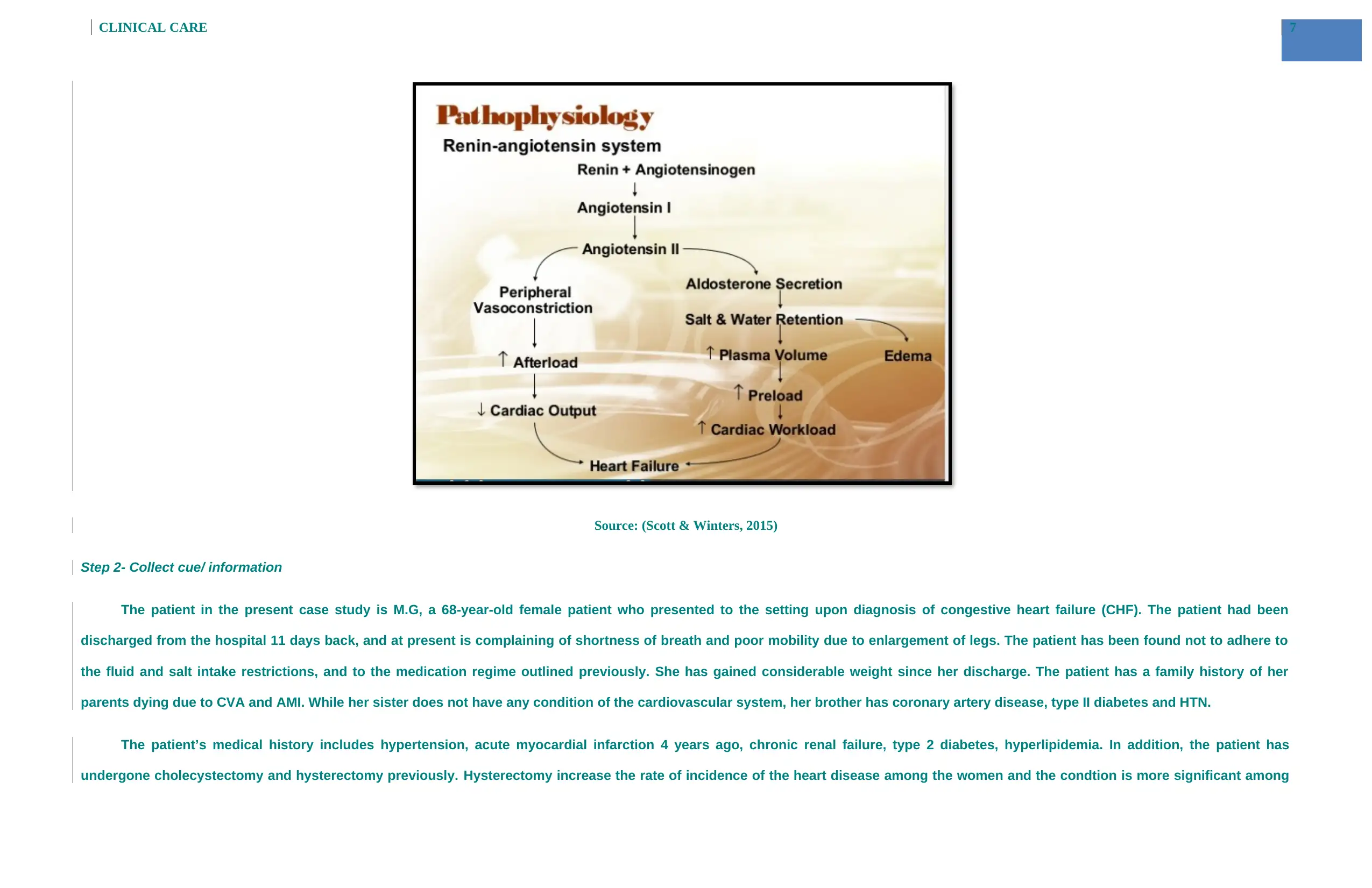
The pathophysiology of CHF can also be explained under the guidance of the renin-angiostensin system.
Patho physiology of congestive heart failure
CHF
Steps 1-3 of clinical reasoning cycle applied to the case study
Step 1 – Consider the patient- need to give a summary to the patient’s condition here
MG is a 68 year old female who has been admitted to the emergency department with congestive heart failure (CHF). The main symptoms highlighted by her which has lead to her
immediate admission include shortness in breadth, swelling or fluid accumulation in the hips. Accoridng to M.G, her legs have become as big as tree trunk and she is unable to move.
Moreover, she has gained 5 kgs of weight recently. She also has previous reported cases of chronic renal failure, type 2 diabetes mellitus, hyperlipidemia, HT and AMI (4 years ago). She
also displayed pink skin colour along with fast apical pulse followed by atrial fibrillation, high BP, pulmonary congestion (Scott & Winters, 2015). CHF is defined as a condition where the
muscles of the heat get weakened and thus fail to pump adequate blood to the different parts of the body. CHF can also be defines as the state of heart in which abnormal circulatory
congestion exists that eventually results in heart failure. CHF has different types and this include low output heart failure, high-output heart failure along with right ventricular failure. Low
output heart failure can be further subdivided into systolic heart failure and diastolic heart failure. In CHF, overall the structure of the heart changes due to volume overload and this result in
valvular dysfunction and thus making heart unable to pump adequate blood to the different parts of the body. This leads to the generation of diabetes, severe lung disease, fluid retention,
hyperthyroidism along with abnormal heart rhythms. Fluid retention causes pulmonary edema which increases the systemic pressure and thereby nearing the chances of heart attack. Due
to abnormal structure of the heart like cardiomegally, there occurs stretching of the heart muscles thereby causing cardiac dilation and as a result, mainly the left ventricular side fails to
function normally leading to disruption in the equilibrium in the normal end diastolic volume and thereby increasing the risk of heart disease (Scott & Winters, 2015).
The pathophysiology of CHF can also be explained under the guidance of the renin-angiostensin system.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CLINICAL CARE
Source: (Scott & Winters, 2015)
Step 2- Collect cue/ information
The patient in the present case study is M.G, a 68-year-old female patient who presented to the setting upon diagnosis of congestive heart failure (CHF). The patient had been
discharged from the hospital 11 days back, and at present is complaining of shortness of breath and poor mobility due to enlargement of legs. The patient has been found not to adhere to
the fluid and salt intake restrictions, and to the medication regime outlined previously. She has gained considerable weight since her discharge. The patient has a family history of her
parents dying due to CVA and AMI. While her sister does not have any condition of the cardiovascular system, her brother has coronary artery disease, type II diabetes and HTN.
The patient’s medical history includes hypertension, acute myocardial infarction 4 years ago, chronic renal failure, type 2 diabetes, hyperlipidemia. In addition, the patient has
undergone cholecystectomy and hysterectomy previously. Hysterectomy increase the rate of incidence of the heart disease among the women and the condtion is more significant among
Source: (Scott & Winters, 2015)
Step 2- Collect cue/ information
The patient in the present case study is M.G, a 68-year-old female patient who presented to the setting upon diagnosis of congestive heart failure (CHF). The patient had been
discharged from the hospital 11 days back, and at present is complaining of shortness of breath and poor mobility due to enlargement of legs. The patient has been found not to adhere to
the fluid and salt intake restrictions, and to the medication regime outlined previously. She has gained considerable weight since her discharge. The patient has a family history of her
parents dying due to CVA and AMI. While her sister does not have any condition of the cardiovascular system, her brother has coronary artery disease, type II diabetes and HTN.
The patient’s medical history includes hypertension, acute myocardial infarction 4 years ago, chronic renal failure, type 2 diabetes, hyperlipidemia. In addition, the patient has
undergone cholecystectomy and hysterectomy previously. Hysterectomy increase the rate of incidence of the heart disease among the women and the condtion is more significant among
8CLINICAL CARE
the population who are undergoing hormone replacement therapy after hysterectomy ( (Wild, et al., 2013). Moreover, there is also a inter linkage between the gall bladder disease and heart
disease (Chavez-Tapia, et al., 2012). Chavez-Tapi et al. (2012) highlighted that cholecystectomy increases the metabolic risk factor behind the development of cardio vascular disease like
CHF. The present vital signs of the patient are P 122 irregular; BP 160/100, RR 26, T 37.3 C, O2 Sat- 93% on room air. Chest examination shows widespread consolidation and cardiomegaly.
Widespread crepitations are found on chest auscultation. The patient is newly diagnosed with Atrial Fibrillation. Edema is present with pink skin color. Further, apical pulse is thready and
fast. Radiology results indicate pulmonary congestion. The laboratory test results report potassium 5.3 mEq/L, sodium 145 mEq/L, chloride 100 mEq/L, bicarbonate 27 mEq/L, glucose 11.2
mmol, creatinine 4.5 mg/dL, BUN 4.3 mg/dL, magnesium 1.9 mEq/L. Among the blood parameters, abnormality is detected in the glucose and creatinine as they are beyond the normal limits.
According to Chavez-Tapia, Castro-Gastelum, Sánchez-Lara and Méndez-Sánchez (2012), high level of blood glucose increases the risk of developing both type 1 or type 2 diabetes mellitus.
Increase in the level of risk of diabetes mellitus increases the risk of developing heart disease like congestive heart failure (Chavez-Tapia, Castro-Gastelum, Sánchez-Lara, & Méndez-
Sánchez, 2012).
Step 3- Process information
The patient’s primary diagnosis is congestive heart failure (CHF) which is a chronic progressive condition affecting the pumping action of the heart muscles. In CHF there is
accumulation of fluid around the heart due to the underlying causes. According to Pellicori, Kaur and Clark (2015), the development of peripheral oedema among the patients with CHF leads
to the excess of fluid accumulation. As the cardiac output begins to decline, there occurs an imbalance in the renal function . This imbalance in the renal function is reported by the kidneys
with the increase in the production of renin. Increase in renin leads to an increase in the production of aldosterone which is followed by sodium and water retention.CHF develops when the
ventricles become larger and thicker and are incapable of pumping blood to the body in sufficient volume (Pellicori, Kaur, & Clark, 2015). Accumulation of fluid prevents the normal supply
and the transport of the blood coming from the venous system and this leads to lack of adequate blood supply in the lungs, abdomen, liver and parts of lower body (Oikonomou, Tousoulis,
Siasos, Zaromitidou, Papavassiliou, & Stefanadis, 2011). The patient has been complaining of shortness of breath and enlarged legs. In the case of left-sided CHF, the left ventricle does not
pump blood adequately to the body and fluid (blood) backs up and leaks into the lungs causing shortness of breath . Moreover, inability of the heart to pump adequate blood to the other
parts of the body due to fluid accumulation causes lack of oxygen supply in the body which is again manifested in the form of shortness of breath (Bressler, et al., 2011). Left-sided heart
failure usually leads to right-sided heart failure. In Right heart failure, the rightventricle cannot pump blood properly to the lungs to be replenished with oxygen. Blood and fluid may back up
in the veins that deliver blood to the heart. This can cause fluid to leak into tissues and organs (Bressler, et al., 2011). The main symptoms are pulmonary edema and shortness of breath
the population who are undergoing hormone replacement therapy after hysterectomy ( (Wild, et al., 2013). Moreover, there is also a inter linkage between the gall bladder disease and heart
disease (Chavez-Tapia, et al., 2012). Chavez-Tapi et al. (2012) highlighted that cholecystectomy increases the metabolic risk factor behind the development of cardio vascular disease like
CHF. The present vital signs of the patient are P 122 irregular; BP 160/100, RR 26, T 37.3 C, O2 Sat- 93% on room air. Chest examination shows widespread consolidation and cardiomegaly.
Widespread crepitations are found on chest auscultation. The patient is newly diagnosed with Atrial Fibrillation. Edema is present with pink skin color. Further, apical pulse is thready and
fast. Radiology results indicate pulmonary congestion. The laboratory test results report potassium 5.3 mEq/L, sodium 145 mEq/L, chloride 100 mEq/L, bicarbonate 27 mEq/L, glucose 11.2
mmol, creatinine 4.5 mg/dL, BUN 4.3 mg/dL, magnesium 1.9 mEq/L. Among the blood parameters, abnormality is detected in the glucose and creatinine as they are beyond the normal limits.
According to Chavez-Tapia, Castro-Gastelum, Sánchez-Lara and Méndez-Sánchez (2012), high level of blood glucose increases the risk of developing both type 1 or type 2 diabetes mellitus.
Increase in the level of risk of diabetes mellitus increases the risk of developing heart disease like congestive heart failure (Chavez-Tapia, Castro-Gastelum, Sánchez-Lara, & Méndez-
Sánchez, 2012).
Step 3- Process information
The patient’s primary diagnosis is congestive heart failure (CHF) which is a chronic progressive condition affecting the pumping action of the heart muscles. In CHF there is
accumulation of fluid around the heart due to the underlying causes. According to Pellicori, Kaur and Clark (2015), the development of peripheral oedema among the patients with CHF leads
to the excess of fluid accumulation. As the cardiac output begins to decline, there occurs an imbalance in the renal function . This imbalance in the renal function is reported by the kidneys
with the increase in the production of renin. Increase in renin leads to an increase in the production of aldosterone which is followed by sodium and water retention.CHF develops when the
ventricles become larger and thicker and are incapable of pumping blood to the body in sufficient volume (Pellicori, Kaur, & Clark, 2015). Accumulation of fluid prevents the normal supply
and the transport of the blood coming from the venous system and this leads to lack of adequate blood supply in the lungs, abdomen, liver and parts of lower body (Oikonomou, Tousoulis,
Siasos, Zaromitidou, Papavassiliou, & Stefanadis, 2011). The patient has been complaining of shortness of breath and enlarged legs. In the case of left-sided CHF, the left ventricle does not
pump blood adequately to the body and fluid (blood) backs up and leaks into the lungs causing shortness of breath . Moreover, inability of the heart to pump adequate blood to the other
parts of the body due to fluid accumulation causes lack of oxygen supply in the body which is again manifested in the form of shortness of breath (Bressler, et al., 2011). Left-sided heart
failure usually leads to right-sided heart failure. In Right heart failure, the rightventricle cannot pump blood properly to the lungs to be replenished with oxygen. Blood and fluid may back up
in the veins that deliver blood to the heart. This can cause fluid to leak into tissues and organs (Bressler, et al., 2011). The main symptoms are pulmonary edema and shortness of breath
9CLINICAL CARE
due to the fluid accumulation in the lungs. Increase of weight by 5 kg is indicative of body swelling due to fluid accumulation. In this case study, M.G is suffering from high rate of fluid
retention as evident from the tree trunk sized legs. She has also reported that dur massive swelling and fluid retention in her leg, she is unable to walk. Hypervolemia or fluid retention is
frequently regarded as the stimulus for the decompensate acute heart failure. It also leads towards the considerable weight gain followed by the hospitalization (Albert, 2012).
The patient has a medical history of type II diabetes, coronary artery disease that is acute myocardial infarction, and HTN, all of which are important risk factors of CHF. When the
patient’s blood pressure is higher than the normal value, CHF is common, due to increased pressure in arteries and heart started to pumping forcefully. Coronary artery diseases are also a
contributor to CHF. Cholesterol and other fatty substances block the coronary arteries, leading to atherosclerosis. As a result, blood flow is restricted in the body. While CHF is mostly due
to heart-related conditions, other conditions, such as diabetes and obesity, can lead to CHF (Horwich & Fonarow, 2010). Obesity cast an adverse effect on the left ventricular structure of the
heart along with hampering the diastolic and systolic function. Thus the hamper in the equilibrium as imposed by obesity increase the risk of heart failure and hypertension which ultimately
leads to CHF (Lavie, Alpert, Arena, Mehra, Milani, & Ventura, 2013). In the domain of diabetes, it can be said that patients with high level of blood glucose level of are suffering from type 1
and type 2 diabetes suffers from high risk of developing microvascular and macrovascular complications and this increases the risk of developing cardiac complications which is leading
towards congestive heart failure (McMurray, Gerstein, Holman, & Pfeffer, 2014). Further, the patient has not adhered to the fluid and salt intake restrictions following her previous hospital
admission. This has aggravated the symptoms related to CHF. Salt and fluid restriction is recommended for those individuals living with CHF in global guidelines, since a pool of scientific
evidence supporting it is strong (Fabrício, Gentil, Amato, Marques, & Schwartzmann, 2016). Restrictions of dietary sodium are a common and modifiable precipitant of admissions due to
HF. High consumption of sodium is a primary modifiable factor for promotion of hypertension. Excess salt consumption leads retention of water, worsening the fluid build up that happens
in the case of heart failure (Doukky, et al., 2016).
The lifetime risk for development of CHF doubles with blood pressure more than 160/100 (Ettehad, et al., 2016). In the present case, the patient has a BP of 160/100 and PR 122.Rapid
and irregular heartbeat is a common condition associated with CHF. There are mainly four types of arrhthmia common cardiac complications and this includes extra beats, supraventricular
tachycardias, ventricular arrhythmias and bradyarrhythmias. Among this ventricular arrhythmias (VA) along with arterial fibrilation is associated with CHF (Lip, et al., 2015). Lip et al. (2015)
have further opined that VA increases the risk of development of concurrent co-morbidities like electrolyte imbalance, obstructure sleep apnoea, catecholamine excess, hypoxaemia, renal
and heaptic dysfunction. All these add on towards the development of the CHF. The weakened heart tries to beat faster for sending more blood through your system, leading to irregular
heartbeat (Morton, Fontaine, & Hudak, 2017). The patient’s RR 26 is also abnormal, and patients with CHF often develop breathing abnormalities (Garde, Sörnmo, Jané, & Giraldo, 2010).
Chest examination of the patient indicates Cardiomegaly, a condition of the heart in which it is enlarged. Enlargement of heart or cardiomegally is not a condition but it is defined as a
symptom of an underlying problem that forces the heart to work for a longer period of time than in normal conditions. Hypertension is highlighted as the main reason behind the
due to the fluid accumulation in the lungs. Increase of weight by 5 kg is indicative of body swelling due to fluid accumulation. In this case study, M.G is suffering from high rate of fluid
retention as evident from the tree trunk sized legs. She has also reported that dur massive swelling and fluid retention in her leg, she is unable to walk. Hypervolemia or fluid retention is
frequently regarded as the stimulus for the decompensate acute heart failure. It also leads towards the considerable weight gain followed by the hospitalization (Albert, 2012).
The patient has a medical history of type II diabetes, coronary artery disease that is acute myocardial infarction, and HTN, all of which are important risk factors of CHF. When the
patient’s blood pressure is higher than the normal value, CHF is common, due to increased pressure in arteries and heart started to pumping forcefully. Coronary artery diseases are also a
contributor to CHF. Cholesterol and other fatty substances block the coronary arteries, leading to atherosclerosis. As a result, blood flow is restricted in the body. While CHF is mostly due
to heart-related conditions, other conditions, such as diabetes and obesity, can lead to CHF (Horwich & Fonarow, 2010). Obesity cast an adverse effect on the left ventricular structure of the
heart along with hampering the diastolic and systolic function. Thus the hamper in the equilibrium as imposed by obesity increase the risk of heart failure and hypertension which ultimately
leads to CHF (Lavie, Alpert, Arena, Mehra, Milani, & Ventura, 2013). In the domain of diabetes, it can be said that patients with high level of blood glucose level of are suffering from type 1
and type 2 diabetes suffers from high risk of developing microvascular and macrovascular complications and this increases the risk of developing cardiac complications which is leading
towards congestive heart failure (McMurray, Gerstein, Holman, & Pfeffer, 2014). Further, the patient has not adhered to the fluid and salt intake restrictions following her previous hospital
admission. This has aggravated the symptoms related to CHF. Salt and fluid restriction is recommended for those individuals living with CHF in global guidelines, since a pool of scientific
evidence supporting it is strong (Fabrício, Gentil, Amato, Marques, & Schwartzmann, 2016). Restrictions of dietary sodium are a common and modifiable precipitant of admissions due to
HF. High consumption of sodium is a primary modifiable factor for promotion of hypertension. Excess salt consumption leads retention of water, worsening the fluid build up that happens
in the case of heart failure (Doukky, et al., 2016).
The lifetime risk for development of CHF doubles with blood pressure more than 160/100 (Ettehad, et al., 2016). In the present case, the patient has a BP of 160/100 and PR 122.Rapid
and irregular heartbeat is a common condition associated with CHF. There are mainly four types of arrhthmia common cardiac complications and this includes extra beats, supraventricular
tachycardias, ventricular arrhythmias and bradyarrhythmias. Among this ventricular arrhythmias (VA) along with arterial fibrilation is associated with CHF (Lip, et al., 2015). Lip et al. (2015)
have further opined that VA increases the risk of development of concurrent co-morbidities like electrolyte imbalance, obstructure sleep apnoea, catecholamine excess, hypoxaemia, renal
and heaptic dysfunction. All these add on towards the development of the CHF. The weakened heart tries to beat faster for sending more blood through your system, leading to irregular
heartbeat (Morton, Fontaine, & Hudak, 2017). The patient’s RR 26 is also abnormal, and patients with CHF often develop breathing abnormalities (Garde, Sörnmo, Jané, & Giraldo, 2010).
Chest examination of the patient indicates Cardiomegaly, a condition of the heart in which it is enlarged. Enlargement of heart or cardiomegally is not a condition but it is defined as a
symptom of an underlying problem that forces the heart to work for a longer period of time than in normal conditions. Hypertension is highlighted as the main reason behind the
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10CLINICAL CARE
cardiomegally in case of MG and under this condition; the heart fails to pump adequate blood to the different parts of the body and thereby causing increase in the oxygen deficiency along
with shortness of breath (Ho, et al., 2012). This condition has a strong association with CHF, and the risk factors for the same include diabetes and hypertension. Examining the blood serum
chemistry report it can be stated that the glucose level at11.2 mmol and creatinine level at 4.5 mg/dL are above reference range. While the normal value of creatinine is 1.0-2.0 mg/dL, the
normal value for glucose is 4.0 to 6.0mmol/L for fasting state (Lindblad, Eickhoff, Forslund, Isaksson, & Gustafsson, 2015).This indicates chronic renal failure and poorly managed diabetes
due to irregular medications. Familial hyperlipidemia can be stated as another risk for developing CHR as it increase the concentration of low density lipoprotein (LDL) long with
apolipoprotein B (Imes & Austin, 2013).
The patient has recently been diagnosed with Atrial fibrillation which is the irregular and rapid heart rate in individuals, increasing the risk of heart failure stroke, and other heart-
related complications (Kirchhof, Benussi, Kotecha, Ahlsson, & Atar, 2016).Atrial fibrillation and congestive heart failure are known to be morbid conditions sharing common risk factors and
these two conditions frequently coexist. Research indicates that each of the two conditions predisposes to the other, increasing the risk for mortality.
Step 4- Identify problems
Processing of the collected information about the patient has helped in highlighting the patient problems aligned to which nursing interventions are to be given. In the present case,
the main patient problems/issues are shortness of breath, poorly managed diabetes, hypertension, renal failure and improper salt and fluid intake.
cardiomegally in case of MG and under this condition; the heart fails to pump adequate blood to the different parts of the body and thereby causing increase in the oxygen deficiency along
with shortness of breath (Ho, et al., 2012). This condition has a strong association with CHF, and the risk factors for the same include diabetes and hypertension. Examining the blood serum
chemistry report it can be stated that the glucose level at11.2 mmol and creatinine level at 4.5 mg/dL are above reference range. While the normal value of creatinine is 1.0-2.0 mg/dL, the
normal value for glucose is 4.0 to 6.0mmol/L for fasting state (Lindblad, Eickhoff, Forslund, Isaksson, & Gustafsson, 2015).This indicates chronic renal failure and poorly managed diabetes
due to irregular medications. Familial hyperlipidemia can be stated as another risk for developing CHR as it increase the concentration of low density lipoprotein (LDL) long with
apolipoprotein B (Imes & Austin, 2013).
The patient has recently been diagnosed with Atrial fibrillation which is the irregular and rapid heart rate in individuals, increasing the risk of heart failure stroke, and other heart-
related complications (Kirchhof, Benussi, Kotecha, Ahlsson, & Atar, 2016).Atrial fibrillation and congestive heart failure are known to be morbid conditions sharing common risk factors and
these two conditions frequently coexist. Research indicates that each of the two conditions predisposes to the other, increasing the risk for mortality.
Step 4- Identify problems
Processing of the collected information about the patient has helped in highlighting the patient problems aligned to which nursing interventions are to be given. In the present case,
the main patient problems/issues are shortness of breath, poorly managed diabetes, hypertension, renal failure and improper salt and fluid intake.
11CLINICAL CARE
References
Albert, N. M. (2012). Fluid management strategies in heart failure. Critical care nurse , 32(2), 20-32.
Bressler, J., Knopman, D. S., Sharrett, A. R., Gottesman, F., R., Penman, A., et al. (2011). Incident heart failure and cognitive decline: the Atherosclerosis Risk in Communities Study. Journal of cardiac failure ,
23 (1), 47-55.
Chavez-Tapia, N. C., Kinney-Novelo, I. M., Sifuentes-Rentería, S. E., Torres-Zavala, M., Castro-Gastelum, G., Sánchez-Lara, K. .., et al. (2012). Association between cholecystectomy for gallstone disease and risk
factors for cardiovascular disease. Ann Hepatol , 11(1), 85-89.
Chavez-Tapia, N. C.-N.-R.-Z., Castro-Gastelum, G., Sánchez-Lara, K. .., & Méndez-Sánchez, N. (2012). Association between cholecystectomy for gallstone disease and risk factors for cardiovascular disease. Ann
Hepatol , 11(1), 85-89.
Crowley, M. J., Diamantidis, C. J., McDuffie, J. R., Cameron, C. B., Stanifer, J. W., Mock, C. K., et al. (2017). Clinical outcomes of metformin use in populations with chronic kidney disease, congestive heart
failure, or chronic liver disease: a systematic review. . Annals of internal medicine , 166 (3), 191-200.
Doukky, R., Avery, E., Mangla, A., Collado, F. M., Ibrahim, Z., Poulin, M. F., et al. (2016). Impact of dietary sodium restriction on heart failure outcomes. . JACC: Heart Failure , 4 (1), 24-35.
Ettehad, D., Emdin, C. A., Kiran, A., Anderson, S. G., Callender, T., Emberson, J., et al. (2016). Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-
analysis. The Lancet , 387 (10022), 957-967.
Fabrício, C. G., Gentil, J. R., Amato, C. A., Marques, F., & Schwartzmann, P. V. (2016). Prospective, Randomised and Blinded Clinical Study Testing Two Levels of Dietary Sodium Intake in Patients with Acute
Decompensated Heart Failure. Journal of Cardiac Failure , 22 (8), 55.
Garde, A., Sörnmo, L., Jané, R., & Giraldo, B. F. (2010). Breathing Pattern Characterization in Chronic Heart Failure Patients Using the Respiratory Flow Signal. Annals of biomedical engineering , 3572-3580.
Hall, J. E. (2015). Guyton and Hall textbook of medical physiology e-Book. Elsevier Health Sciences.
References
Albert, N. M. (2012). Fluid management strategies in heart failure. Critical care nurse , 32(2), 20-32.
Bressler, J., Knopman, D. S., Sharrett, A. R., Gottesman, F., R., Penman, A., et al. (2011). Incident heart failure and cognitive decline: the Atherosclerosis Risk in Communities Study. Journal of cardiac failure ,
23 (1), 47-55.
Chavez-Tapia, N. C., Kinney-Novelo, I. M., Sifuentes-Rentería, S. E., Torres-Zavala, M., Castro-Gastelum, G., Sánchez-Lara, K. .., et al. (2012). Association between cholecystectomy for gallstone disease and risk
factors for cardiovascular disease. Ann Hepatol , 11(1), 85-89.
Chavez-Tapia, N. C.-N.-R.-Z., Castro-Gastelum, G., Sánchez-Lara, K. .., & Méndez-Sánchez, N. (2012). Association between cholecystectomy for gallstone disease and risk factors for cardiovascular disease. Ann
Hepatol , 11(1), 85-89.
Crowley, M. J., Diamantidis, C. J., McDuffie, J. R., Cameron, C. B., Stanifer, J. W., Mock, C. K., et al. (2017). Clinical outcomes of metformin use in populations with chronic kidney disease, congestive heart
failure, or chronic liver disease: a systematic review. . Annals of internal medicine , 166 (3), 191-200.
Doukky, R., Avery, E., Mangla, A., Collado, F. M., Ibrahim, Z., Poulin, M. F., et al. (2016). Impact of dietary sodium restriction on heart failure outcomes. . JACC: Heart Failure , 4 (1), 24-35.
Ettehad, D., Emdin, C. A., Kiran, A., Anderson, S. G., Callender, T., Emberson, J., et al. (2016). Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-
analysis. The Lancet , 387 (10022), 957-967.
Fabrício, C. G., Gentil, J. R., Amato, C. A., Marques, F., & Schwartzmann, P. V. (2016). Prospective, Randomised and Blinded Clinical Study Testing Two Levels of Dietary Sodium Intake in Patients with Acute
Decompensated Heart Failure. Journal of Cardiac Failure , 22 (8), 55.
Garde, A., Sörnmo, L., Jané, R., & Giraldo, B. F. (2010). Breathing Pattern Characterization in Chronic Heart Failure Patients Using the Respiratory Flow Signal. Annals of biomedical engineering , 3572-3580.
Hall, J. E. (2015). Guyton and Hall textbook of medical physiology e-Book. Elsevier Health Sciences.
12CLINICAL CARE
Ho, J. E., Lyass, A., Lee, D. S., Vasan, R. S., Kannel, W. B., Larson, M. G., et al. (2012). Predictors of new-onset heart failure: differences in preserved versus reduced ejection fraction. Circulation: Heart Failure ,
112.
Horwich, T. B., & Fonarow, G. C. (2010). Glucose, obesity, metabolic syndrome, and diabetes: relevance to incidence of heart failure. Journal of the American College of Cardiology , 283-293.
Imes, C. C., & Austin, M. A. (2013). Low-density lipoprotein cholesterol, apolipoprotein B, and risk of coronary heart disease: from familial hyperlipidemia to genomics. Biological research for nursing , 15(3),
292-308.
Kirchhof, P., Benussi, S., Kotecha, D., Ahlsson, A., & Atar, D. .. (2016). ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. EP Europace , 18 (11), 1609-1678.
Koeppen, B. M. (2017). Berne and Levy Physiology E-Book. Elsevier Health Sciences.
Lavie, C. J., Alpert, M. A., Arena, R., Mehra, M. R., Milani, R. V., & Ventura, H. O. (2013). mpact of obesity and the obesity paradox on prevalence and prognosis in heart failure. JACC: Heart Failure , 1(2), 93-
102.
Lindblad, F., Eickhoff, M., Forslund, A. H., Isaksson, J., & Gustafsson. (2015). Fasting blood glucose and HbA1c in children with ADHD. Psychiatry research , 226 (2), 515-516.
Lip, G. Y., Heinzel, F. R., Gaita, F., Juanatey, J. R., Le Heuzey, J. Y., Potpara, T. .., et al. (2015). European heart rhythm association/heart failure association joint consensus document on arrhythmias in heart
failure, endorsed by the Heart rhythm society and the Asia Pacific heart rhythm society. EP Europace , 18(1), 12-36.
McMurray, J. J., Gerstein, H. C., Holman, R. R., & Pfeffer, M. A. (2014). Heart failure: a cardiovascular outcome in diabetes that can no longer be ignored. The Lancet Diabetes & Endocrinology , 2(10), 843-851.
Morton, P. G., Fontaine, D., & Hudak, C. M. (2017). Critical care nursing: a holistic approach. Lippincott Williams & Wilkins.
Oikonomou, E., Tousoulis, D., Siasos, G., Zaromitidou, M. A., Papavassiliou, A. G., & Stefanadis, C. H. (2011). The role of inflammation in heart failure: new therapeutic approaches. . Hellenic J Cardiol , 30-40.
Pellicori, P., Kaur, K., & Clark, A. L. (2015). Fluid management in patients with chronic heart failure. Cardiac failure review , 1(2), 90.
Scott, M. C., & Winters, M. E. (2015). Congestive heart failure. Emergency Medicine Clinics , 33(3), 553-562.
Wild, R. A., Wu, C., Curb, J. D., Martin, L. W., Phillips, L., Stefanick, M. .., et al. (2013). Coronary heart disease events in the Women's Health Initiative hormone trials: effect modification by metabolic
syndrome: A nested case-control study within the Women's Health Initiative randomized clinical trials. Menopause. Newyork , 20(3), 254-260.
Ho, J. E., Lyass, A., Lee, D. S., Vasan, R. S., Kannel, W. B., Larson, M. G., et al. (2012). Predictors of new-onset heart failure: differences in preserved versus reduced ejection fraction. Circulation: Heart Failure ,
112.
Horwich, T. B., & Fonarow, G. C. (2010). Glucose, obesity, metabolic syndrome, and diabetes: relevance to incidence of heart failure. Journal of the American College of Cardiology , 283-293.
Imes, C. C., & Austin, M. A. (2013). Low-density lipoprotein cholesterol, apolipoprotein B, and risk of coronary heart disease: from familial hyperlipidemia to genomics. Biological research for nursing , 15(3),
292-308.
Kirchhof, P., Benussi, S., Kotecha, D., Ahlsson, A., & Atar, D. .. (2016). ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. EP Europace , 18 (11), 1609-1678.
Koeppen, B. M. (2017). Berne and Levy Physiology E-Book. Elsevier Health Sciences.
Lavie, C. J., Alpert, M. A., Arena, R., Mehra, M. R., Milani, R. V., & Ventura, H. O. (2013). mpact of obesity and the obesity paradox on prevalence and prognosis in heart failure. JACC: Heart Failure , 1(2), 93-
102.
Lindblad, F., Eickhoff, M., Forslund, A. H., Isaksson, J., & Gustafsson. (2015). Fasting blood glucose and HbA1c in children with ADHD. Psychiatry research , 226 (2), 515-516.
Lip, G. Y., Heinzel, F. R., Gaita, F., Juanatey, J. R., Le Heuzey, J. Y., Potpara, T. .., et al. (2015). European heart rhythm association/heart failure association joint consensus document on arrhythmias in heart
failure, endorsed by the Heart rhythm society and the Asia Pacific heart rhythm society. EP Europace , 18(1), 12-36.
McMurray, J. J., Gerstein, H. C., Holman, R. R., & Pfeffer, M. A. (2014). Heart failure: a cardiovascular outcome in diabetes that can no longer be ignored. The Lancet Diabetes & Endocrinology , 2(10), 843-851.
Morton, P. G., Fontaine, D., & Hudak, C. M. (2017). Critical care nursing: a holistic approach. Lippincott Williams & Wilkins.
Oikonomou, E., Tousoulis, D., Siasos, G., Zaromitidou, M. A., Papavassiliou, A. G., & Stefanadis, C. H. (2011). The role of inflammation in heart failure: new therapeutic approaches. . Hellenic J Cardiol , 30-40.
Pellicori, P., Kaur, K., & Clark, A. L. (2015). Fluid management in patients with chronic heart failure. Cardiac failure review , 1(2), 90.
Scott, M. C., & Winters, M. E. (2015). Congestive heart failure. Emergency Medicine Clinics , 33(3), 553-562.
Wild, R. A., Wu, C., Curb, J. D., Martin, L. W., Phillips, L., Stefanick, M. .., et al. (2013). Coronary heart disease events in the Women's Health Initiative hormone trials: effect modification by metabolic
syndrome: A nested case-control study within the Women's Health Initiative randomized clinical trials. Menopause. Newyork , 20(3), 254-260.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

13CLINICAL CARE
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





