Practice Portfolio of Evidence PART B: Clinical Encounter Analysis
Analyzing a clinical encounter and applying clinical reasoning skills in nursing practice.
6 Pages1996 Words230 Views
Added on 2023-05-29
About This Document
Read about a clinical encounter analysis of a patient post-surgery in ICU. Learn about the nursing problems, goals, and actions taken to resolve them. Desklib provides evidence-based literature to support the discussion.
Practice Portfolio of Evidence PART B: Clinical Encounter Analysis
Analyzing a clinical encounter and applying clinical reasoning skills in nursing practice.
Added on 2023-05-29
ShareRelated Documents
Becoming a RN: Practice consolidation
Practice Portfolio of Evidence PART B: Clinical Encounter Analysis
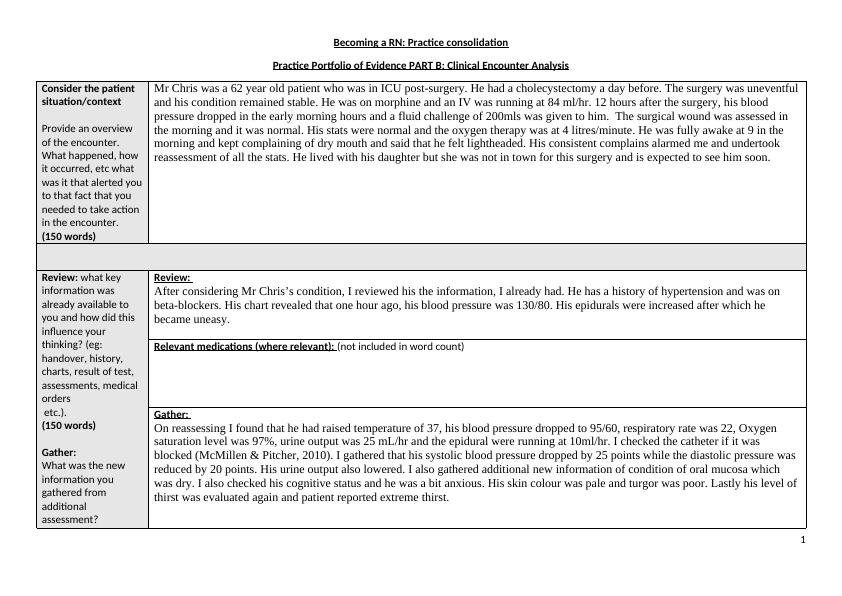
Consider the patient
situation/context
Provide an overview
of the encounter.
What happened, how
it occurred, etc what
was it that alerted you
to that fact that you
needed to take action
in the encounter.
(150 words)
Mr Chris was a 62 year old patient who was in ICU post-surgery. He had a cholecystectomy a day before. The surgery was uneventful
and his condition remained stable. He was on morphine and an IV was running at 84 ml/hr. 12 hours after the surgery, his blood
pressure dropped in the early morning hours and a fluid challenge of 200mls was given to him. The surgical wound was assessed in
the morning and it was normal. His stats were normal and the oxygen therapy was at 4 litres/minute. He was fully awake at 9 in the
morning and kept complaining of dry mouth and said that he felt lightheaded. His consistent complains alarmed me and undertook
reassessment of all the stats. He lived with his daughter but she was not in town for this surgery and is expected to see him soon.
Review: what key
information was
already available to
you and how did this
influence your
thinking? (eg:
handover, history,
charts, result of test,
assessments, medical
orders
etc.).
(150 words)
Gather:
What was the new
information you
gathered from
additional
assessment?
Review:
After considering Mr Chris’s condition, I reviewed his the information, I already had. He has a history of hypertension and was on
beta-blockers. His chart revealed that one hour ago, his blood pressure was 130/80. His epidurals were increased after which he
became uneasy.
Relevant medications (where relevant): (not included in word count)
Gather:
On reassessing I found that he had raised temperature of 37, his blood pressure dropped to 95/60, respiratory rate was 22, Oxygen
saturation level was 97%, urine output was 25 mL/hr and the epidural were running at 10ml/hr. I checked the catheter if it was
blocked (McMillen & Pitcher, 2010). I gathered that his systolic blood pressure dropped by 25 points while the diastolic pressure was
reduced by 20 points. His urine output also lowered. I also gathered additional new information of condition of oral mucosa which
was dry. I also checked his cognitive status and he was a bit anxious. His skin colour was pale and turgor was poor. Lastly his level of
thirst was evaluated again and patient reported extreme thirst.
1
Practice Portfolio of Evidence PART B: Clinical Encounter Analysis
Consider the patient
situation/context
Provide an overview
of the encounter.
What happened, how
it occurred, etc what
was it that alerted you
to that fact that you
needed to take action
in the encounter.
(150 words)
Mr Chris was a 62 year old patient who was in ICU post-surgery. He had a cholecystectomy a day before. The surgery was uneventful
and his condition remained stable. He was on morphine and an IV was running at 84 ml/hr. 12 hours after the surgery, his blood
pressure dropped in the early morning hours and a fluid challenge of 200mls was given to him. The surgical wound was assessed in
the morning and it was normal. His stats were normal and the oxygen therapy was at 4 litres/minute. He was fully awake at 9 in the
morning and kept complaining of dry mouth and said that he felt lightheaded. His consistent complains alarmed me and undertook
reassessment of all the stats. He lived with his daughter but she was not in town for this surgery and is expected to see him soon.
Review: what key
information was
already available to
you and how did this
influence your
thinking? (eg:
handover, history,
charts, result of test,
assessments, medical
orders
etc.).
(150 words)
Gather:
What was the new
information you
gathered from
additional
assessment?
Review:
After considering Mr Chris’s condition, I reviewed his the information, I already had. He has a history of hypertension and was on
beta-blockers. His chart revealed that one hour ago, his blood pressure was 130/80. His epidurals were increased after which he
became uneasy.
Relevant medications (where relevant): (not included in word count)
Gather:
On reassessing I found that he had raised temperature of 37, his blood pressure dropped to 95/60, respiratory rate was 22, Oxygen
saturation level was 97%, urine output was 25 mL/hr and the epidural were running at 10ml/hr. I checked the catheter if it was
blocked (McMillen & Pitcher, 2010). I gathered that his systolic blood pressure dropped by 25 points while the diastolic pressure was
reduced by 20 points. His urine output also lowered. I also gathered additional new information of condition of oral mucosa which
was dry. I also checked his cognitive status and he was a bit anxious. His skin colour was pale and turgor was poor. Lastly his level of
thirst was evaluated again and patient reported extreme thirst.
1
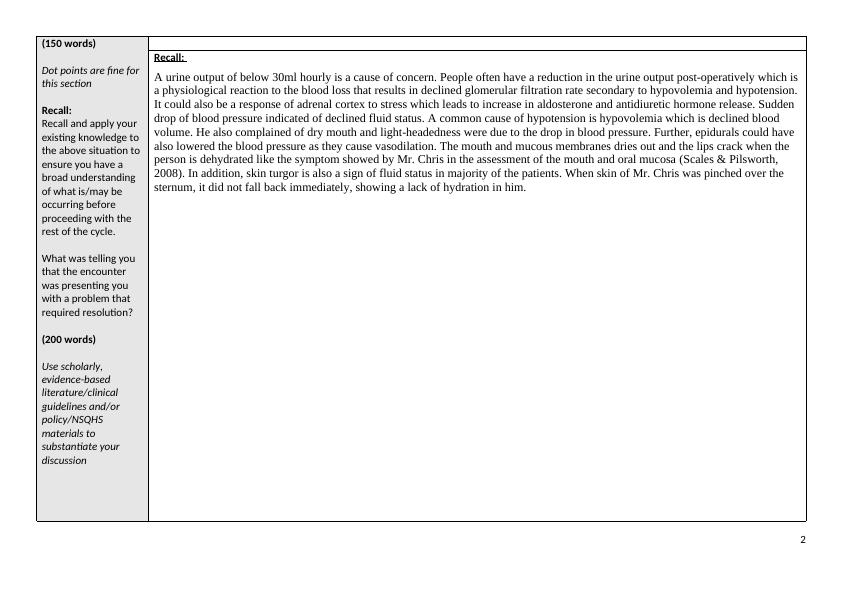
(150 words)
Dot points are fine for
this section
Recall:
Recall and apply your
existing knowledge to
the above situation to
ensure you have a
broad understanding
of what is/may be
occurring before
proceeding with the
rest of the cycle.
What was telling you
that the encounter
was presenting you
with a problem that
required resolution?
(200 words)
Use scholarly,
evidence-based
literature/clinical
guidelines and/or
policy/NSQHS
materials to
substantiate your
discussion
Recall:
A urine output of below 30ml hourly is a cause of concern. People often have a reduction in the urine output post-operatively which is
a physiological reaction to the blood loss that results in declined glomerular filtration rate secondary to hypovolemia and hypotension.
It could also be a response of adrenal cortex to stress which leads to increase in aldosterone and antidiuretic hormone release. Sudden
drop of blood pressure indicated of declined fluid status. A common cause of hypotension is hypovolemia which is declined blood
volume. He also complained of dry mouth and light-headedness were due to the drop in blood pressure. Further, epidurals could have
also lowered the blood pressure as they cause vasodilation. The mouth and mucous membranes dries out and the lips crack when the
person is dehydrated like the symptom showed by Mr. Chris in the assessment of the mouth and oral mucosa (Scales & Pilsworth,
2008). In addition, skin turgor is also a sign of fluid status in majority of the patients. When skin of Mr. Chris was pinched over the
sternum, it did not fall back immediately, showing a lack of hydration in him.
2
Dot points are fine for
this section
Recall:
Recall and apply your
existing knowledge to
the above situation to
ensure you have a
broad understanding
of what is/may be
occurring before
proceeding with the
rest of the cycle.
What was telling you
that the encounter
was presenting you
with a problem that
required resolution?
(200 words)
Use scholarly,
evidence-based
literature/clinical
guidelines and/or
policy/NSQHS
materials to
substantiate your
discussion
Recall:
A urine output of below 30ml hourly is a cause of concern. People often have a reduction in the urine output post-operatively which is
a physiological reaction to the blood loss that results in declined glomerular filtration rate secondary to hypovolemia and hypotension.
It could also be a response of adrenal cortex to stress which leads to increase in aldosterone and antidiuretic hormone release. Sudden
drop of blood pressure indicated of declined fluid status. A common cause of hypotension is hypovolemia which is declined blood
volume. He also complained of dry mouth and light-headedness were due to the drop in blood pressure. Further, epidurals could have
also lowered the blood pressure as they cause vasodilation. The mouth and mucous membranes dries out and the lips crack when the
person is dehydrated like the symptom showed by Mr. Chris in the assessment of the mouth and oral mucosa (Scales & Pilsworth,
2008). In addition, skin turgor is also a sign of fluid status in majority of the patients. When skin of Mr. Chris was pinched over the
sternum, it did not fall back immediately, showing a lack of hydration in him.
2
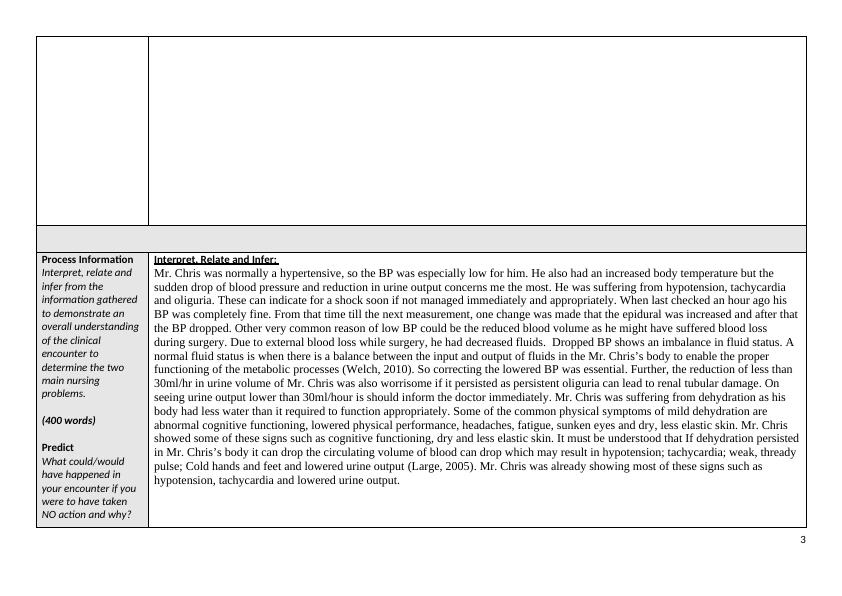
Process Information
Interpret, relate and
infer from the
information gathered
to demonstrate an
overall understanding
of the clinical
encounter to
determine the two
main nursing
problems.
(400 words)
Predict
What could/would
have happened in
your encounter if you
were to have taken
NO action and why?
Interpret, Relate and Infer:
Mr. Chris was normally a hypertensive, so the BP was especially low for him. He also had an increased body temperature but the
sudden drop of blood pressure and reduction in urine output concerns me the most. He was suffering from hypotension, tachycardia
and oliguria. These can indicate for a shock soon if not managed immediately and appropriately. When last checked an hour ago his
BP was completely fine. From that time till the next measurement, one change was made that the epidural was increased and after that
the BP dropped. Other very common reason of low BP could be the reduced blood volume as he might have suffered blood loss
during surgery. Due to external blood loss while surgery, he had decreased fluids. Dropped BP shows an imbalance in fluid status. A
normal fluid status is when there is a balance between the input and output of fluids in the Mr. Chris’s body to enable the proper
functioning of the metabolic processes (Welch, 2010). So correcting the lowered BP was essential. Further, the reduction of less than
30ml/hr in urine volume of Mr. Chris was also worrisome if it persisted as persistent oliguria can lead to renal tubular damage. On
seeing urine output lower than 30ml/hour is should inform the doctor immediately. Mr. Chris was suffering from dehydration as his
body had less water than it required to function appropriately. Some of the common physical symptoms of mild dehydration are
abnormal cognitive functioning, lowered physical performance, headaches, fatigue, sunken eyes and dry, less elastic skin. Mr. Chris
showed some of these signs such as cognitive functioning, dry and less elastic skin. It must be understood that If dehydration persisted
in Mr. Chris’s body it can drop the circulating volume of blood can drop which may result in hypotension; tachycardia; weak, thready
pulse; Cold hands and feet and lowered urine output (Large, 2005). Mr. Chris was already showing most of these signs such as
hypotension, tachycardia and lowered urine output.
3
Interpret, relate and
infer from the
information gathered
to demonstrate an
overall understanding
of the clinical
encounter to
determine the two
main nursing
problems.
(400 words)
Predict
What could/would
have happened in
your encounter if you
were to have taken
NO action and why?
Interpret, Relate and Infer:
Mr. Chris was normally a hypertensive, so the BP was especially low for him. He also had an increased body temperature but the
sudden drop of blood pressure and reduction in urine output concerns me the most. He was suffering from hypotension, tachycardia
and oliguria. These can indicate for a shock soon if not managed immediately and appropriately. When last checked an hour ago his
BP was completely fine. From that time till the next measurement, one change was made that the epidural was increased and after that
the BP dropped. Other very common reason of low BP could be the reduced blood volume as he might have suffered blood loss
during surgery. Due to external blood loss while surgery, he had decreased fluids. Dropped BP shows an imbalance in fluid status. A
normal fluid status is when there is a balance between the input and output of fluids in the Mr. Chris’s body to enable the proper
functioning of the metabolic processes (Welch, 2010). So correcting the lowered BP was essential. Further, the reduction of less than
30ml/hr in urine volume of Mr. Chris was also worrisome if it persisted as persistent oliguria can lead to renal tubular damage. On
seeing urine output lower than 30ml/hour is should inform the doctor immediately. Mr. Chris was suffering from dehydration as his
body had less water than it required to function appropriately. Some of the common physical symptoms of mild dehydration are
abnormal cognitive functioning, lowered physical performance, headaches, fatigue, sunken eyes and dry, less elastic skin. Mr. Chris
showed some of these signs such as cognitive functioning, dry and less elastic skin. It must be understood that If dehydration persisted
in Mr. Chris’s body it can drop the circulating volume of blood can drop which may result in hypotension; tachycardia; weak, thready
pulse; Cold hands and feet and lowered urine output (Large, 2005). Mr. Chris was already showing most of these signs such as
hypotension, tachycardia and lowered urine output.
3
End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Treatment in Patients with Rectal Cancerlg...
|12
|3108
|36
CNA344 | Clinical Encounter Analysislg...
|8
|2769
|17
Scenario 2- Mr Clive Jenkins: A retired navy engineer with a history of Congestive Cardiac Failurelg...
|6
|2438
|420
