Scenario 2- Mr Clive Jenkins: A retired navy engineer with a history of Congestive Cardiac Failure
6 Pages2438 Words420 Views
Added on 2020-05-28
About This Document
Gather new information (patient assessment): Upon undertaking a further assessment of Mr Jenkins you obtain the following new information: Vital Signs RR: 24 Sp02: 94% on 2lt via nasal prongs Temp: afebrile HR: 112bpm BP: 150/90 Mr Jenkins appears ‘pleasantly confused’ as you speak to him where you notice he becomes short of breath as he attempts to reposition himself in bed and is reluctant to get up as he feels so tired. The patient also
Scenario 2- Mr Clive Jenkins: A retired navy engineer with a history of Congestive Cardiac Failure
Added on 2020-05-28
ShareRelated Documents
CNA255: Scenario 2- Mr Clive Jenkins Consider the patient situationMr Clive Jenkins is a 78 year old retired navy engineer with a history of Congestive Cardiac Failure after suffering a severe myocardial infarction 2 years ago that affected both ventricles. Since that time, Mr Jenkins has recently been diagnosed with Dementia and as a result, it has been difficult for him to sustain the necessary life-style adjustments required to prevent exacerbations of his condition. This has resulted in several admissions to hospital for management and review of his congestive heart failure. For this admission, Mr Jenkins was referred to hospital by his GP after recently gaining weight (currently 95kg) since his last visit the week prior. The time now is 0800 and you have just come on for your morning shift. Mr Jenkins has been on the ward for only two hours after spending the 18 hours in emergency waiting for a bed to become available.Collect CuesReview:Please refer to documentation provided via the MyLO site.Gather new information (patient assessment):Upon undertaking a further assessment of Mr Jenkins you obtain the following new information:Vital SignsRR: 24Sp02: 94% on 2lt via nasal prongsTemp: afebrileHR: 112bpm BP: 150/90Mr Jenkins appears ‘pleasantly confused’ as you speak to him where you notice he becomes short of breath as he attempts to reposition himself in bed and is reluctant to get up as he feels so tired. You also note he has already drunk the 1 litre jug of water provided to him when he arrived.Other informationBGL within normal rangeGCS 14 (confused)Peripheral pulses difficult to palpate due to presence of pitting oedema in both feet. Evident rash noted on left leg. Capillary return < 5 seconds.Current weight 97kg.Raised JVPPassing urine in bottle.Abdomen soft and non-tender. Bowel sounds present.Recall:Recall and apply your existing knowledge to the above situation to ensure you have a broad understanding of what is/may be occurring before proceeding with the rest of the cycle (self-directed)
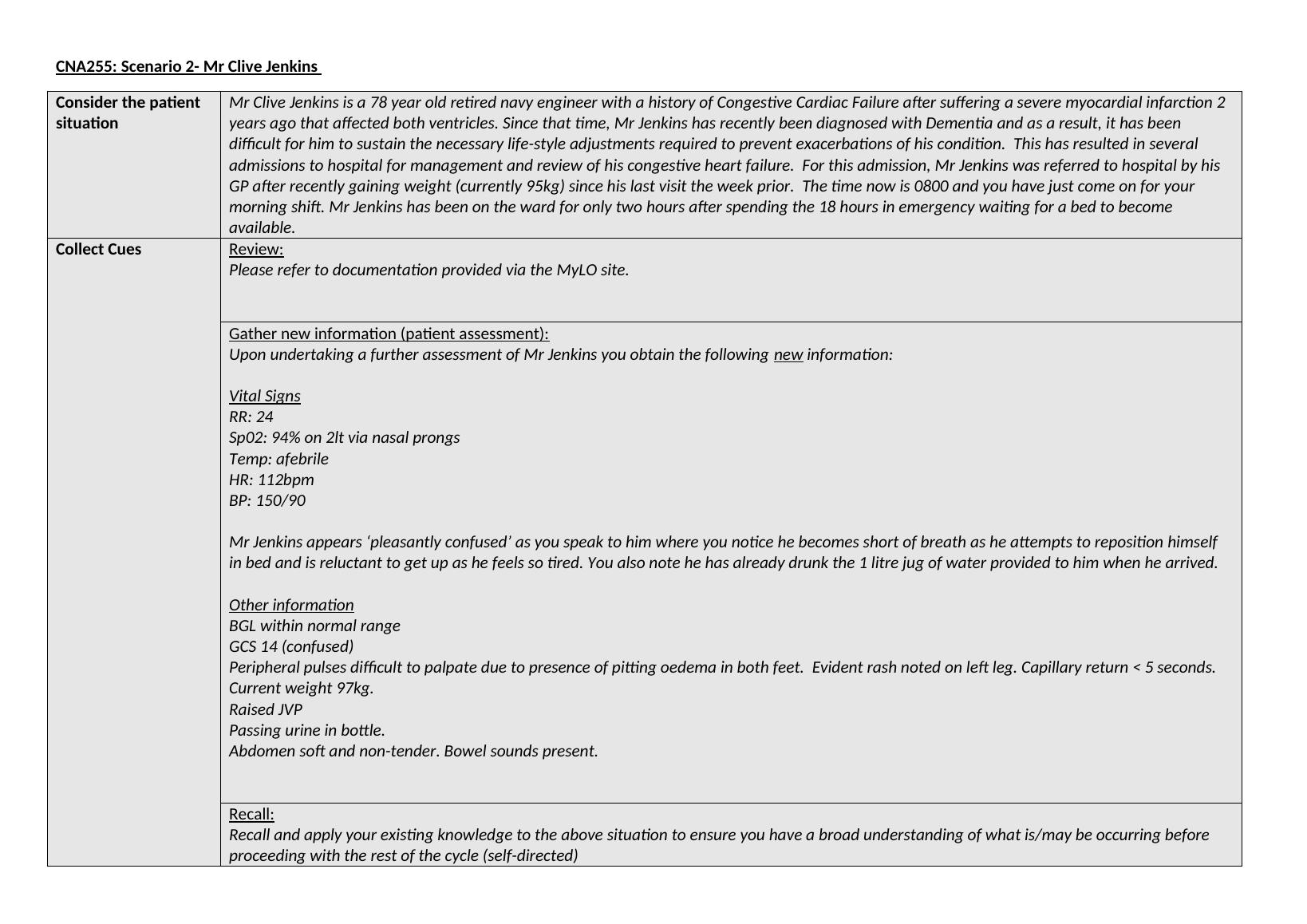
Process InformationInterpret:List the data that you consider to be normal/abnormal below (not included in word count)NormalAbnormalOn assessment of the clinical symptoms presented by the patient,the observations were noted down by the nursing professional. Thepatient depicted a respiratory rate of 24 whereas the normalrespiratory rate should be between 25 -40 breaths per minute. Thepartial pressure of oxygen depicted by the patient was 94% withthe help of nasal prongs. The patient did not show any signs offeverThe patient recorded a heart beat rate of 112 per minute.Additionally, the patient recorded a high blood pressure of150/90 and appeared confused.The high rate of heart beat along with high bloodpressure could be attributed to the insufficient pumping by theheart.Relate & Infer:Relate the two most significant abnormal findings to the underlying physiology/pathophysiology to justify why it is considered abnormal in this context. Based on your interpretation of all the information/cues presented, form an overall opinion on what may be happening and justify your answer (400 words).Some of the other clinical symptoms expressed by Mr. Jenkins were also considered to analyse the detailed health condition presentedby the patient. Further analysis showed that the blood glucose level of the patient were within normal limits. Oedema was found to bepresent on both feet of the patient. Rashes were also found to be present in the left leg of the patient. The patient also depicted raisedjugular blood pressure and was put on type IV oral administration along furesomide to treat build up of tissue fluid accumulation andramipril to relax muscles around small arteries, which can help in revival of the pumping capacity of the heart.The three main clinical symptoms expressed in the patient were development of oedema, sinus tachycardia and mentalconfustion. As mentioned by Hunter and Arthur (2016), congestive heart failure is one of the most important causes of peripheraloedema. It is activated by a series of humoral and neurohumoral mechanisms that promotes sodium and water absorption by kidneysand results in expansion of extracellular fluid resulting the swelling of hands and feet. The increased jugular vein pressure could alsopromote fluid extravasation. The oedema is characterised by increased movement of fluid from the intravascular to the interstitialspace. It activates the renin-angiotensin-aldosterone- vasopressin (ADH) system resulting in renal sodium retention. As mentioned byMebazaaet al. (2015), combination of diuretics and vasodilators has been seen to relieve the formation of oedema to a greater extent.Additionally, the patient also showed clinical symptoms of sinus tachycardia where an abnormal heart beat rate was noted inthe patient. The patient expressed heart rate of 112 beats per minute which was much above the normal heart rate of 72 beats perminute. It could be attributed to the condition of sinus tachycardia present in the patient. The sinus tachycardia is a condition, whicharises as a result of the inability of the SA node to effectively transmit impulses. As mentioned by Platzet al. (2015), thedevelopment of the condition could be attributed to the fall in arterial blood pressure. In here, the patient suffered from myocardialinfarction twice over which affected the pumping capacity of his ventricles. It is associated with increased sympathetic tone and mayresult in restlessness and confusion within the patient. As argued by Gorter and de Boer (2018), the sinus tachycardia can occur inmoist of the conditions without any deep seated clinical cause and mostly settles down with proper rest. However, here the patient had
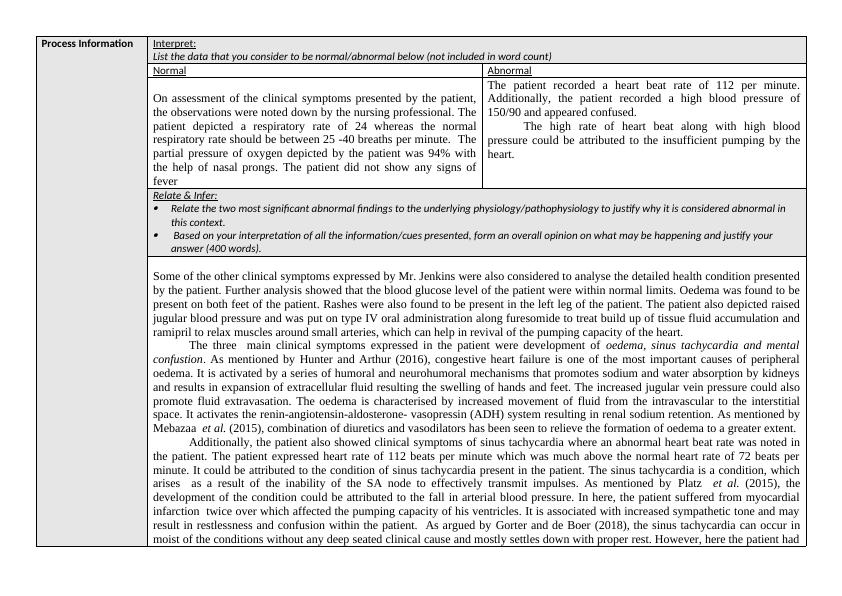
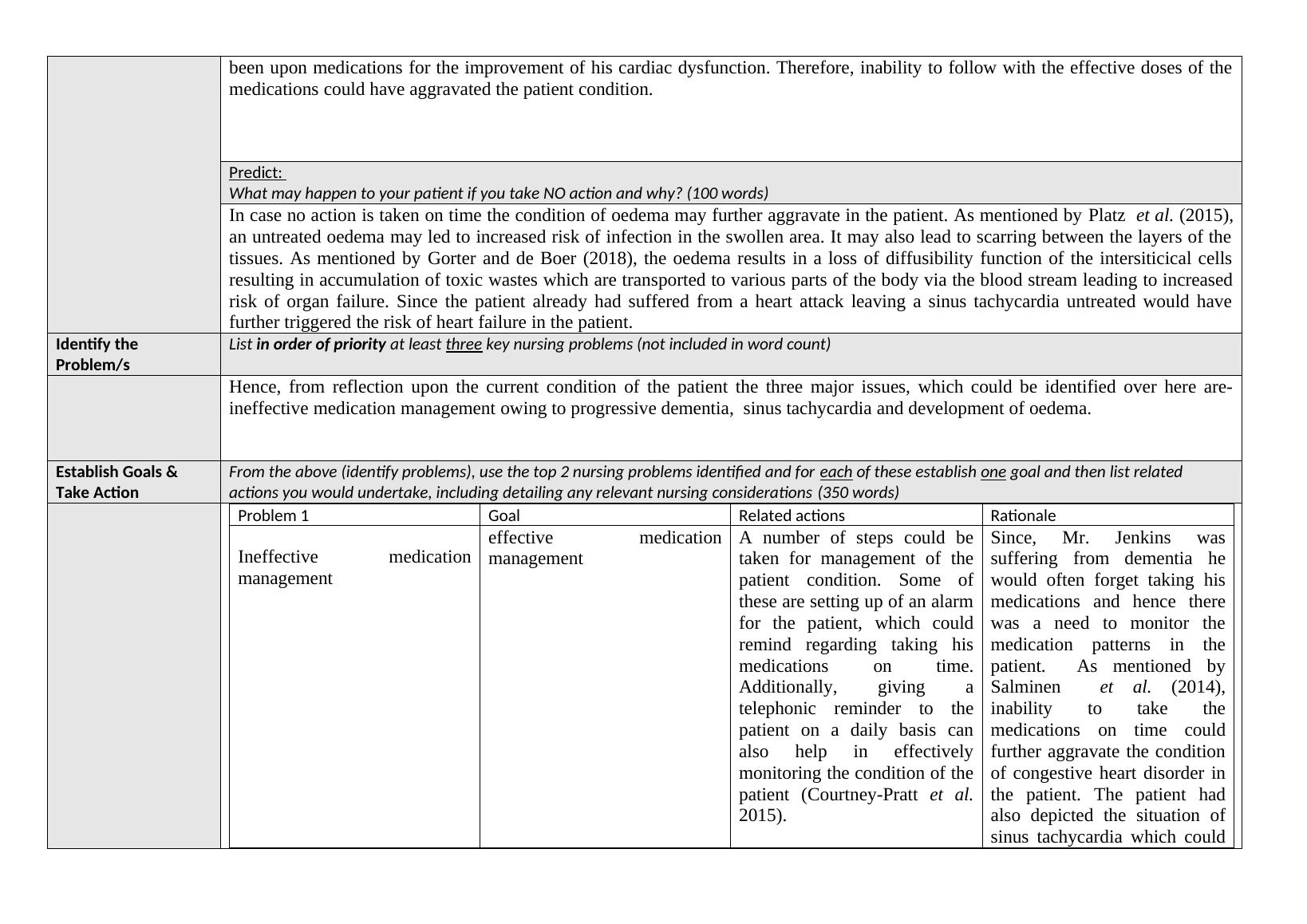
been upon medications for the improvement of his cardiac dysfunction. Therefore, inability to follow with the effective doses of themedications could have aggravated the patient condition. Predict: What may happen to your patient if you take NO action and why? (100 words)In case no action is taken on time the condition of oedema may further aggravate in the patient. As mentioned by Platzet al. (2015),an untreated oedema may led to increased risk of infection in the swollen area. It may also lead to scarring between the layers of thetissues. As mentioned by Gorter and de Boer (2018), the oedema results in a loss of diffusibility function of the intersiticical cellsresulting in accumulation of toxic wastes which are transported to various parts of the body via the blood stream leading to increasedrisk of organ failure. Since the patient already had suffered from a heart attack leaving a sinus tachycardia untreated would havefurther triggered the risk of heart failure in the patient.Identify the Problem/sList in order of priority at least three key nursing problems (not included in word count)Hence, from reflection upon the current condition of the patient the three major issues, which could be identified over here are-ineffective medication management owing to progressive dementia, sinus tachycardia and development of oedema. Establish Goals & Take ActionFrom the above (identify problems), use the top 2 nursing problems identified and for each of these establish one goal and then list related actions you would undertake, including detailing any relevant nursing considerations (350 words)Problem 1GoalRelated actionsRationaleIneffective medicationmanagementeffectivemedicationmanagementA number of steps could betaken for management of thepatient condition. Some ofthese are setting up of an alarmfor the patient, which couldremind regarding taking hismedications on time.Additionally, giving atelephonic reminder to thepatient on a daily basis canalso help in effectivelymonitoring the condition of thepatient (Courtney-Pratt et al.2015). Since, Mr. Jenkins wassuffering from dementia hewould often forget taking hismedications and hence therewas a need to monitor themedication patterns in thepatient. As mentioned bySalminenet al. (2014),inability to take themedications on time couldfurther aggravate the conditionof congestive heart disorder inthe patient. The patient hadalso depicted the situation ofsinus tachycardia which could
End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Interpret, Relate & Infer: Mr. Clive Jenkins Case Studylg...
|4
|1901
|85
Nursing Case Study Question 2022lg...
|12
|3166
|20
Comparative Essay on Maintenance of Oxygen Levelslg...
|6
|1574
|301
Assessment of a Patient with Breathing Difficulty and Chest Painlg...
|9
|1883
|31
Health Alterationlg...
|12
|2630
|424
Essential Nursing Care: Foundational Skillslg...
|9
|2504
|80
