Community Health And Diseases Australia Discussion 2022
VerifiedAdded on 2022/08/25
|7
|1376
|14
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: COMMUNITY HEALTH AND DISEASE: OBESITY PREVENTION
COMMUNITY HEALTH AND DISEASE: OBESITY PREVENTION IN CHILDREN AND
YOUTH
Name of the Student:
Name of the University:
Author note:
COMMUNITY HEALTH AND DISEASE: OBESITY PREVENTION IN CHILDREN AND
YOUTH
Name of the Student:
Name of the University:
Author note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

1COMMUNITY HEALTH AND DISEASE: OBESITY PREVENTION
Introduction
Approximately 24% of children and youth aged 5 to 14 years were found to be
overweight and obese in Australia during 2017 to 2018 (Australian Institute of Health and
Welfare, 2018). The following paper briefly expounds upon key components of a health
promotion program.
Discussion
Interventions
One intervention will involve nutritional educational and assessment sessions concerning
balanced diet consumption and healthy weight comprising of parents, children and youth. This is
because the consumption of high fat, sugar and sodium beverages and foods have been linked to
lack of health literacy. Childhood obesity has been linked to eating patterns followed by parents
(Demir & Bektas, 2017). The next strategies will comprise of practical demonstrations where
children, youth and parents will be involved in healthy cooking sessions, nutritional label
interpretation and cost effective, nutritious food selection. This is because consumption of high
fat, sugar and sodium beverages and foods has been linked to misinterpretation of labels,
convenience, less knowledge on healthy cooking and consumption of inexpensive, energy dense
foods in low income group families (Jarpe-Ratner et al., 2016). Lastly, exercise interventions
will include both parents, youth and children since obesity has been linked to increased sedentary
lifestyles (Ham et al., 2016). Weekly counseling feedback sessions will be included for
motivation since obesity has been linked to poor psychological outcomes (Barlow et al., 2018).
Introduction
Approximately 24% of children and youth aged 5 to 14 years were found to be
overweight and obese in Australia during 2017 to 2018 (Australian Institute of Health and
Welfare, 2018). The following paper briefly expounds upon key components of a health
promotion program.
Discussion
Interventions
One intervention will involve nutritional educational and assessment sessions concerning
balanced diet consumption and healthy weight comprising of parents, children and youth. This is
because the consumption of high fat, sugar and sodium beverages and foods have been linked to
lack of health literacy. Childhood obesity has been linked to eating patterns followed by parents
(Demir & Bektas, 2017). The next strategies will comprise of practical demonstrations where
children, youth and parents will be involved in healthy cooking sessions, nutritional label
interpretation and cost effective, nutritious food selection. This is because consumption of high
fat, sugar and sodium beverages and foods has been linked to misinterpretation of labels,
convenience, less knowledge on healthy cooking and consumption of inexpensive, energy dense
foods in low income group families (Jarpe-Ratner et al., 2016). Lastly, exercise interventions
will include both parents, youth and children since obesity has been linked to increased sedentary
lifestyles (Ham et al., 2016). Weekly counseling feedback sessions will be included for
motivation since obesity has been linked to poor psychological outcomes (Barlow et al., 2018).

2COMMUNITY HEALTH AND DISEASE: OBESITY PREVENTION
Health Promotion
Primary care health promotion will be addressed via educational and assessment sessions such as
practitioners and nurses educating parents, children and youth on balanced diet intake along with
weight measurement. Secondary health promotion will be addressed using specialist services
where nutritionists, fitness experts and counselors will demonstrate practical sessions of healthy
cooking, food selection, exercise and label interpretation to parents, youth and children (Daniels,
2019).
Intervention Phases
1. Planning: Planning will comprise of first assessing the demographics of obese children
and youth in the locality using patient records across schools, gyms, community health
clinics and weight loss centers. Children and youth with Body Mass Index (BMI) above
24.9 kg/m2 along with their parents will be recruited based on informed consent.
2. Community Engagement: Both parents of the children and youth will be included
together in educational sessions before as well as during the study along with practical
sessions of cooking, food selection, exercise and label interpretation to improved parent-
youth interaction and healthier home environments.
3. Implementation: The educational and assessment interventions will comprise of the first
phase of implementation for a period of 1 week, followed by second phase of practical
sessions of cooking, food selection, and exercise and label interpretation for the next 3
weeks.
4. Management: The interventions will be managed by supervision and weekly follow ups
by counselors, nurses, practitioners, dieticians and fitness experts.
Health Promotion
Primary care health promotion will be addressed via educational and assessment sessions such as
practitioners and nurses educating parents, children and youth on balanced diet intake along with
weight measurement. Secondary health promotion will be addressed using specialist services
where nutritionists, fitness experts and counselors will demonstrate practical sessions of healthy
cooking, food selection, exercise and label interpretation to parents, youth and children (Daniels,
2019).
Intervention Phases
1. Planning: Planning will comprise of first assessing the demographics of obese children
and youth in the locality using patient records across schools, gyms, community health
clinics and weight loss centers. Children and youth with Body Mass Index (BMI) above
24.9 kg/m2 along with their parents will be recruited based on informed consent.
2. Community Engagement: Both parents of the children and youth will be included
together in educational sessions before as well as during the study along with practical
sessions of cooking, food selection, exercise and label interpretation to improved parent-
youth interaction and healthier home environments.
3. Implementation: The educational and assessment interventions will comprise of the first
phase of implementation for a period of 1 week, followed by second phase of practical
sessions of cooking, food selection, and exercise and label interpretation for the next 3
weeks.
4. Management: The interventions will be managed by supervision and weekly follow ups
by counselors, nurses, practitioners, dieticians and fitness experts.

3COMMUNITY HEALTH AND DISEASE: OBESITY PREVENTION
5. Evaluation: Measurements of BMI will be taken before and after the program, where
greater reduction in these values to normal range of 18 to 24 kg/m2 will indicate success.
Weekly follow ups will be taken where feedback from parents, children and youth giving
feedback to counselors will indicate program participant compliance and motivation.
6. Recommendations: A post intervention will comprise of all stakeholders and
participants discussion on results, program experiences and how these interventions can
be used for future (Ek et al., 2019; Hammersley et al., 2019).
Table 1: Timeline
Activity 1st week 2nd week 3rd week 4th week 5th week 6th week
Participant
Recruitment
Educational
Sessions
Assessments
Cooking
sessions
Label
Interpretation
Food selection
demonstration
Exercise
session
Counseling
sessions
Table 2: Stakeholders
Interventions Stakeholders Function
BMI assessment Nurses Measure participant’s BMI
Educational session Practitioners, nurses Educate participants on
healthy weight, balanced diet
intake
Practical sessions Dieticians
Fitness Experts
Educate participants on
nutritional label
interpretation, healthy
5. Evaluation: Measurements of BMI will be taken before and after the program, where
greater reduction in these values to normal range of 18 to 24 kg/m2 will indicate success.
Weekly follow ups will be taken where feedback from parents, children and youth giving
feedback to counselors will indicate program participant compliance and motivation.
6. Recommendations: A post intervention will comprise of all stakeholders and
participants discussion on results, program experiences and how these interventions can
be used for future (Ek et al., 2019; Hammersley et al., 2019).
Table 1: Timeline
Activity 1st week 2nd week 3rd week 4th week 5th week 6th week
Participant
Recruitment
Educational
Sessions
Assessments
Cooking
sessions
Label
Interpretation
Food selection
demonstration
Exercise
session
Counseling
sessions
Table 2: Stakeholders
Interventions Stakeholders Function
BMI assessment Nurses Measure participant’s BMI
Educational session Practitioners, nurses Educate participants on
healthy weight, balanced diet
intake
Practical sessions Dieticians
Fitness Experts
Educate participants on
nutritional label
interpretation, healthy
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4COMMUNITY HEALTH AND DISEASE: OBESITY PREVENTION
cooking and food selection
Conduct moderate exercise
sessions of 2.5 hours per
week involving parents,
youth, children.
Weekly follow up sessions Counselors Motivate participants and
obtain subjective feedback
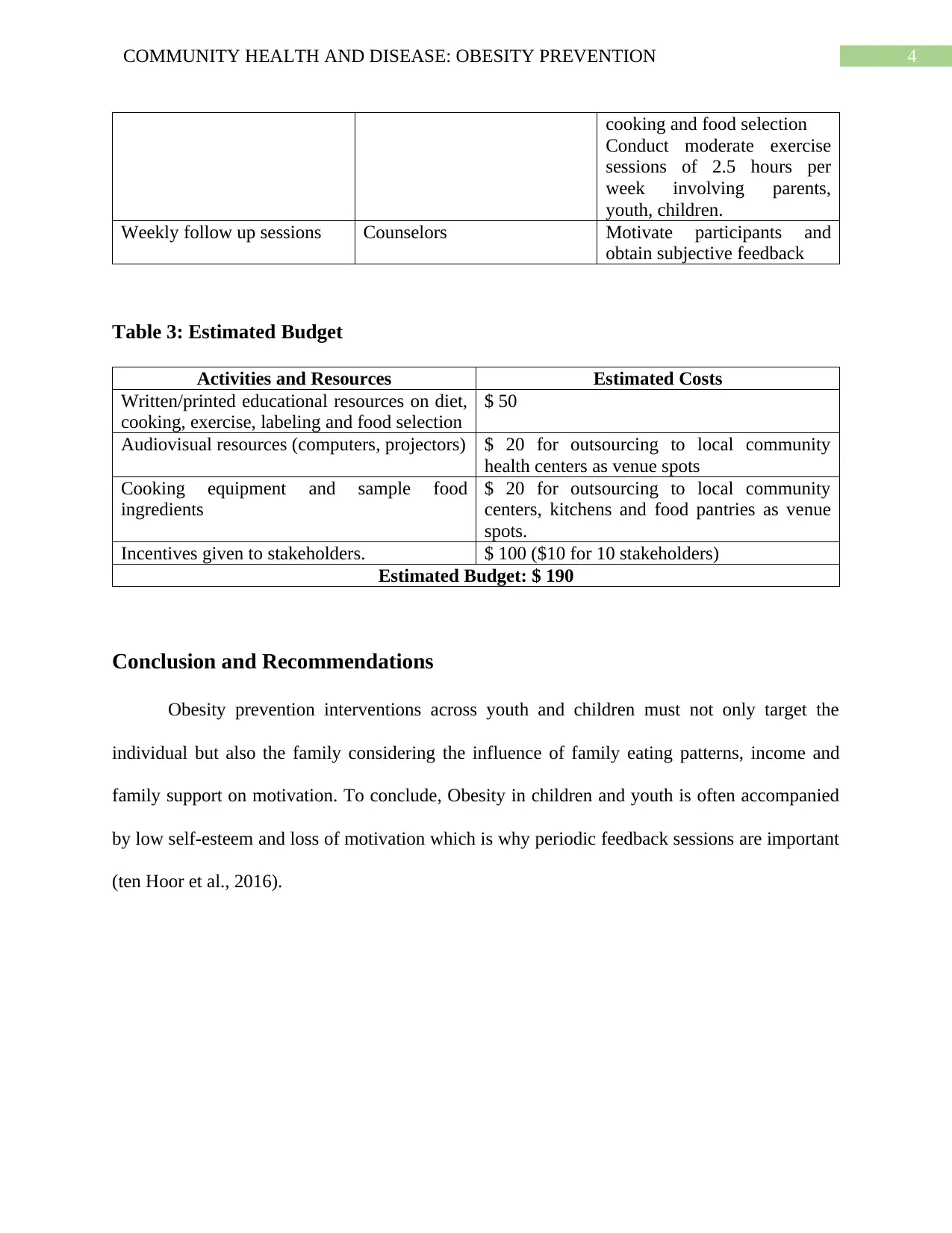
Table 3: Estimated Budget
Activities and Resources Estimated Costs
Written/printed educational resources on diet,
cooking, exercise, labeling and food selection
$ 50
Audiovisual resources (computers, projectors) $ 20 for outsourcing to local community
health centers as venue spots
Cooking equipment and sample food
ingredients
$ 20 for outsourcing to local community
centers, kitchens and food pantries as venue
spots.
Incentives given to stakeholders. $ 100 ($10 for 10 stakeholders)
Estimated Budget: $ 190
Conclusion and Recommendations
Obesity prevention interventions across youth and children must not only target the
individual but also the family considering the influence of family eating patterns, income and
family support on motivation. To conclude, Obesity in children and youth is often accompanied
by low self-esteem and loss of motivation which is why periodic feedback sessions are important
(ten Hoor et al., 2016).
cooking and food selection
Conduct moderate exercise
sessions of 2.5 hours per
week involving parents,
youth, children.
Weekly follow up sessions Counselors Motivate participants and
obtain subjective feedback
Table 3: Estimated Budget
Activities and Resources Estimated Costs
Written/printed educational resources on diet,
cooking, exercise, labeling and food selection
$ 50
Audiovisual resources (computers, projectors) $ 20 for outsourcing to local community
health centers as venue spots
Cooking equipment and sample food
ingredients
$ 20 for outsourcing to local community
centers, kitchens and food pantries as venue
spots.
Incentives given to stakeholders. $ 100 ($10 for 10 stakeholders)
Estimated Budget: $ 190
Conclusion and Recommendations
Obesity prevention interventions across youth and children must not only target the
individual but also the family considering the influence of family eating patterns, income and
family support on motivation. To conclude, Obesity in children and youth is often accompanied
by low self-esteem and loss of motivation which is why periodic feedback sessions are important
(ten Hoor et al., 2016).

5COMMUNITY HEALTH AND DISEASE: OBESITY PREVENTION
References
Australian Institute of Health and Welfare. (2018). Australia's children, Overweight and obesity -
Australian Institute of Health and Welfare. Retrieved 20 April 2020, from
https://www.aihw.gov.au/reports/children-youth/australias-children/contents/health/
overweight-and-obesity.
Barlow, S. E., Salahuddin, M., Butte, N. F., Hoelscher, D. M., & Pont, S. J. (2018). Improvement
in primary care provider self-efficacy and use of patient-centered counseling to address
child overweight and obesity after practice-based changes: Texas Childhood Obesity
Research Demonstration study. Childhood Obesity, 14(8), 518-527.
Daniels, L. A. (2019). A Life-Course Model of Obesity: Primary and Secondary Interventions to
Prevent Childhood Obesity. Multidisciplinary Digital Publishing Institute
Proceedings, 8(1), 59.
Demir, D., & Bektas, M. (2017). The effect of childrens' eating behaviors and parental feeding
style on childhood obesity. Eating behaviors, 26, 137-142.
Ek, A., Chamberlain, K. L., Sorjonen, K., Hammar, U., Malek, M. E., Sandvik, P., ... &
Ejderhamn, J. (2019). A parent treatment program for preschoolers with obesity: a
randomized controlled trial. Pediatrics, 144(2), e20183457.
Ham, O. K., Sung, K. M., Lee, B. G., Choi, H. W., & Im, E. O. (2016). Transtheoretical model
based exercise counseling combined with music skipping rope exercise on childhood
obesity. Asian nursing research, 10(2), 116-122.
References
Australian Institute of Health and Welfare. (2018). Australia's children, Overweight and obesity -
Australian Institute of Health and Welfare. Retrieved 20 April 2020, from
https://www.aihw.gov.au/reports/children-youth/australias-children/contents/health/
overweight-and-obesity.
Barlow, S. E., Salahuddin, M., Butte, N. F., Hoelscher, D. M., & Pont, S. J. (2018). Improvement
in primary care provider self-efficacy and use of patient-centered counseling to address
child overweight and obesity after practice-based changes: Texas Childhood Obesity
Research Demonstration study. Childhood Obesity, 14(8), 518-527.
Daniels, L. A. (2019). A Life-Course Model of Obesity: Primary and Secondary Interventions to
Prevent Childhood Obesity. Multidisciplinary Digital Publishing Institute
Proceedings, 8(1), 59.
Demir, D., & Bektas, M. (2017). The effect of childrens' eating behaviors and parental feeding
style on childhood obesity. Eating behaviors, 26, 137-142.
Ek, A., Chamberlain, K. L., Sorjonen, K., Hammar, U., Malek, M. E., Sandvik, P., ... &
Ejderhamn, J. (2019). A parent treatment program for preschoolers with obesity: a
randomized controlled trial. Pediatrics, 144(2), e20183457.
Ham, O. K., Sung, K. M., Lee, B. G., Choi, H. W., & Im, E. O. (2016). Transtheoretical model
based exercise counseling combined with music skipping rope exercise on childhood
obesity. Asian nursing research, 10(2), 116-122.

6COMMUNITY HEALTH AND DISEASE: OBESITY PREVENTION
Hammersley, M. L., Okely, A. D., Batterham, M. J., & Jones, R. A. (2019). An internet-based
childhood obesity prevention program (Time2bHealthy) for parents of preschool-aged
children: randomized controlled trial. Journal of medical Internet research, 21(2),
e11964.
Jarpe-Ratner, E., Folkens, S., Sharma, S., Daro, D., & Edens, N. K. (2016). An experiential
cooking and nutrition education program increases cooking self-efficacy and vegetable
consumption in children in grades 3–8. Journal of nutrition education and
behavior, 48(10), 697-705.
ten Hoor, G., Sleddens, E., Gillison, F., Horodyska, K., Luszczynska, A., & Kok, G. (2016).
Parental influences on childhood obesity. European Health Psychologist, 18(S), 409.
Hammersley, M. L., Okely, A. D., Batterham, M. J., & Jones, R. A. (2019). An internet-based
childhood obesity prevention program (Time2bHealthy) for parents of preschool-aged
children: randomized controlled trial. Journal of medical Internet research, 21(2),
e11964.
Jarpe-Ratner, E., Folkens, S., Sharma, S., Daro, D., & Edens, N. K. (2016). An experiential
cooking and nutrition education program increases cooking self-efficacy and vegetable
consumption in children in grades 3–8. Journal of nutrition education and
behavior, 48(10), 697-705.
ten Hoor, G., Sleddens, E., Gillison, F., Horodyska, K., Luszczynska, A., & Kok, G. (2016).
Parental influences on childhood obesity. European Health Psychologist, 18(S), 409.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





