Schizophrenia and Bipolar Disorder: A Comparative Analysis
VerifiedAdded on 2020/10/04
|13
|3617
|168
AI Summary
This assignment provides a comprehensive comparison of schizophrenia and bipolar disorder, including an overview of each condition, risk factors, symptoms, diagnosis, and treatment options. It also discusses the importance of engaging patients and relatives in decision-making to promote dignity. The assignment includes research studies on the topic, as well as online resources for further information.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Comprehensive Case study
review of a patient's
experience: Mental Illness
review of a patient's
experience: Mental Illness
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
TABLE OF CONTENTS
PRESENTATION ...........................................................................................................................1
PHYSICAL ASSESSMENT ..........................................................................................................1
MENTAL/EMOTIONAL ASSESSMENT ....................................................................................2
BIOGRAPHICAL HISTORY ........................................................................................................2
PAST PHYSICAL AND MENTAL HEALTH HISTORY ...........................................................3
COLLABORATIVE/CORROBORATIVE HISTORY ..................................................................4
DIAGNOSIS ...................................................................................................................................4
COMMON INTERVENTIONS AND RECOVERY PLAN ..........................................................6
ENGAGEMENT .............................................................................................................................7
REFLECTION.................................................................................................................................7
REFERENCES................................................................................................................................9
PRESENTATION ...........................................................................................................................1
PHYSICAL ASSESSMENT ..........................................................................................................1
MENTAL/EMOTIONAL ASSESSMENT ....................................................................................2
BIOGRAPHICAL HISTORY ........................................................................................................2
PAST PHYSICAL AND MENTAL HEALTH HISTORY ...........................................................3
COLLABORATIVE/CORROBORATIVE HISTORY ..................................................................4
DIAGNOSIS ...................................................................................................................................4
COMMON INTERVENTIONS AND RECOVERY PLAN ..........................................................6
ENGAGEMENT .............................................................................................................................7
REFLECTION.................................................................................................................................7
REFERENCES................................................................................................................................9
PRESENTATION
When human brain is affected by some serious disorders then respective individual is
said to be suffering from mental illness. In the present case study, the mental illness of Dora
(pseudo name generated due to ethical considerations) a 22 year old girl, will be discussed in
depth. She is suffering from schizophrenia- a severe mental condition that highlights the
abnormalities in social behaviour of the person. Her family recognised that Dora was depicting
quite an unusual behaviour with her friends and family members. She complained of listening
sounds that do not exist and visualise situations which actually did not happen (hallucinations).
These were indications that forced her family to seek medical consultations.
Dora's mother reported that she has been noticing changes/symptoms in her behaviour in
the past 2 months. On the other hand, Dora herself accounted that she started visualising things
since 6 months. The patient was followed-up quite quickly after the initial check-up. The follow-
up involved consultation with a psychiatrist for about a week. In case the occurrence of delusions
and hallucinations increase, the patient has to be immediately hospitalised (Bortolon,
Capdevielle and Raffard, 2015).
PHYSICAL ASSESSMENT
Before the doctor prescribes any sort of tests or medicines, there is a physical assessment
conducted (Khademvatan and Yousefi, 2014). For Dora, this assessment included general check-
up of the vitals which included blood pressure, weight, eye movements and pulse rate. The
involuntary movements of body and diverging actions, repetitive motions, check up of twitches
and tics are some of the parameters that are considered during the physical examination (Rasic
and et.al., 2014). The doctor identified that Dora blinked her eyes very less while swung her leg
in a pendulum motion continuously. It was also recognised that Dora's weight was normal but
she kept her head tilted towards one direction as if continuously listening to some other person's
talks.
The physical assessment conducted by medical practitioner describes very abnormal
social behaviour of the patient. Physical abnormalities portray that patient's mental state is not
stable and there are some mental barriers which are causing the patient to behave in such a
mysterious manner (Physical Exam for Schizophrenia, 2015).
1
When human brain is affected by some serious disorders then respective individual is
said to be suffering from mental illness. In the present case study, the mental illness of Dora
(pseudo name generated due to ethical considerations) a 22 year old girl, will be discussed in
depth. She is suffering from schizophrenia- a severe mental condition that highlights the
abnormalities in social behaviour of the person. Her family recognised that Dora was depicting
quite an unusual behaviour with her friends and family members. She complained of listening
sounds that do not exist and visualise situations which actually did not happen (hallucinations).
These were indications that forced her family to seek medical consultations.
Dora's mother reported that she has been noticing changes/symptoms in her behaviour in
the past 2 months. On the other hand, Dora herself accounted that she started visualising things
since 6 months. The patient was followed-up quite quickly after the initial check-up. The follow-
up involved consultation with a psychiatrist for about a week. In case the occurrence of delusions
and hallucinations increase, the patient has to be immediately hospitalised (Bortolon,
Capdevielle and Raffard, 2015).
PHYSICAL ASSESSMENT
Before the doctor prescribes any sort of tests or medicines, there is a physical assessment
conducted (Khademvatan and Yousefi, 2014). For Dora, this assessment included general check-
up of the vitals which included blood pressure, weight, eye movements and pulse rate. The
involuntary movements of body and diverging actions, repetitive motions, check up of twitches
and tics are some of the parameters that are considered during the physical examination (Rasic
and et.al., 2014). The doctor identified that Dora blinked her eyes very less while swung her leg
in a pendulum motion continuously. It was also recognised that Dora's weight was normal but
she kept her head tilted towards one direction as if continuously listening to some other person's
talks.
The physical assessment conducted by medical practitioner describes very abnormal
social behaviour of the patient. Physical abnormalities portray that patient's mental state is not
stable and there are some mental barriers which are causing the patient to behave in such a
mysterious manner (Physical Exam for Schizophrenia, 2015).
1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
MENTAL/EMOTIONAL ASSESSMENT
The state of healthiness is a combination of physical, mental and emotional well-being
(Demjaha, MacCabe and Murray, 2012). Dora's condition was not well as per the physical
examination. The psychiatrist performed mental/emotional assessment for getting an overview
regarding the internal situation. This mental examination was witnessed by Dora's parents also.
The attributes that were assessed include appearance, changes in mood, thinking styles,
reasoning in different situations, behaviour and lastly memory (Baker and et.al., 2014). The
abilities of patient to express herself are also tested (Schizophrenia, 2017). The psychiatrist
conducted verbal and written test on the scale of aforementioned parameters.
From this mental/emotional assessment, the psychiatrist inferred that Dora was
experiencing severe difficulty in thinking and managing her emotions. She was quite confused
when asked about herself talking with an invisible person, etc. In the initial stage of test, she was
reluctant to talk and interact with the doctor but later on she communicated that her “friend”
(hallucinations that are not real) stated to initiate a conversation. Dora stated that her friend is
here to protect her from the upcoming danger that might kill her. These statements reflected
towards a risk or threat of danger to her own life which is hypothetical for others but realistic for
Dora. Schizophrenic patients have been reported to kill themselves just to safeguard themselves
from such kind of assumed deaths (Larsson and et.al., 2013). These symptoms led the doctor to
indicate that Dora was suffering from incurable disease i.e. schizophrenia.
BIOGRAPHICAL HISTORY
The biographical history depicts a patient's overall history from childhood to the present
state. This helps in providing appropriate interventions to the patients that are suffering from
mental illness like schizophrenia (Correll and et.al., 2015). Dora's early childhood was very
natural and just similar to that of normal kids till the age of 14. her father died in a brutal mishap
when he was coming to pick her up. This situation had a deep scar over Dora's emotional health.
She withdrew from her friends and had restricted conversations with her mother. This particular
attribute is a severe indication towards the onset of a mental illness (Whitton, Treadway and
Pizzagalli, 2015). Dora's school performance declined and the initial stages of adolescent also led
to depression and loneliness. There was no inclusion of drugs and alcohol in her lifestyle. But her
mother was quite worried regarding her behaviour with other family members because it was
quite harsh and storming.
2
The state of healthiness is a combination of physical, mental and emotional well-being
(Demjaha, MacCabe and Murray, 2012). Dora's condition was not well as per the physical
examination. The psychiatrist performed mental/emotional assessment for getting an overview
regarding the internal situation. This mental examination was witnessed by Dora's parents also.
The attributes that were assessed include appearance, changes in mood, thinking styles,
reasoning in different situations, behaviour and lastly memory (Baker and et.al., 2014). The
abilities of patient to express herself are also tested (Schizophrenia, 2017). The psychiatrist
conducted verbal and written test on the scale of aforementioned parameters.
From this mental/emotional assessment, the psychiatrist inferred that Dora was
experiencing severe difficulty in thinking and managing her emotions. She was quite confused
when asked about herself talking with an invisible person, etc. In the initial stage of test, she was
reluctant to talk and interact with the doctor but later on she communicated that her “friend”
(hallucinations that are not real) stated to initiate a conversation. Dora stated that her friend is
here to protect her from the upcoming danger that might kill her. These statements reflected
towards a risk or threat of danger to her own life which is hypothetical for others but realistic for
Dora. Schizophrenic patients have been reported to kill themselves just to safeguard themselves
from such kind of assumed deaths (Larsson and et.al., 2013). These symptoms led the doctor to
indicate that Dora was suffering from incurable disease i.e. schizophrenia.
BIOGRAPHICAL HISTORY
The biographical history depicts a patient's overall history from childhood to the present
state. This helps in providing appropriate interventions to the patients that are suffering from
mental illness like schizophrenia (Correll and et.al., 2015). Dora's early childhood was very
natural and just similar to that of normal kids till the age of 14. her father died in a brutal mishap
when he was coming to pick her up. This situation had a deep scar over Dora's emotional health.
She withdrew from her friends and had restricted conversations with her mother. This particular
attribute is a severe indication towards the onset of a mental illness (Whitton, Treadway and
Pizzagalli, 2015). Dora's school performance declined and the initial stages of adolescent also led
to depression and loneliness. There was no inclusion of drugs and alcohol in her lifestyle. But her
mother was quite worried regarding her behaviour with other family members because it was
quite harsh and storming.
2
The absence of a sibling also led to increase in these mental conditions. The high school
performance was quite average and Dora somehow managed to get a degree in Arts with
literature as the specialisation. There were no spiritual practises conducted by her mother and
herself. However, her paternal grandmother is said to have schizophrenia. There was a
probability of transfer of this genetic defect to the next generations which can be witnessed in
Dora. The age time period from 19-21 was very smooth for both Dora and her mother. She did
not indulge in any sort of violent activity which may harm herself or any other person. But after
her disturbed sexual relationship with her senior in the college, the onset of past metal issues
was witnessed. The occurrence of hallucinations increased and this further led to development of
inner anxiety and highly disturbed social behaviour.
PAST PHYSICAL AND MENTAL HEALTH HISTORY
The consultation of primary health care doctor by the patient includes accumulation of
information relating with the medical history. Dora's history depicts following facts:
Inability in sleeping.
Loss of appetite in some situations and over eating in some.
Dora did not feel good when asked about friends or family members.
She had experienced death of her father at an early age and also had a disturbed
relationship with her boyfriend during college.
Had been hospitalised once for 5 days due to acute jaundice.
No exposure to drugs and alcohols.
Paternal grandmother had schizophrenia.
Severe hallucinations from 6 months.
Hears whispering sounds and visualises a “friend” who is same as the age of Dora and a
male.
Dora often experiences that she is in danger and somebody will harm her.
Continuous talking to herself.
Often gets confused when asked about day and night or the present time.
No operations or surgeries have been experienced by the patient till date.
Schizophrenia is often confused with depression and anxiety (Jónsdóttir and et.al., 2013).
The health practitioner has to perform respective question answer sessions so that in-depth
history of the patient is acquired and then necessary conclusions can be made. The biographical
3
performance was quite average and Dora somehow managed to get a degree in Arts with
literature as the specialisation. There were no spiritual practises conducted by her mother and
herself. However, her paternal grandmother is said to have schizophrenia. There was a
probability of transfer of this genetic defect to the next generations which can be witnessed in
Dora. The age time period from 19-21 was very smooth for both Dora and her mother. She did
not indulge in any sort of violent activity which may harm herself or any other person. But after
her disturbed sexual relationship with her senior in the college, the onset of past metal issues
was witnessed. The occurrence of hallucinations increased and this further led to development of
inner anxiety and highly disturbed social behaviour.
PAST PHYSICAL AND MENTAL HEALTH HISTORY
The consultation of primary health care doctor by the patient includes accumulation of
information relating with the medical history. Dora's history depicts following facts:
Inability in sleeping.
Loss of appetite in some situations and over eating in some.
Dora did not feel good when asked about friends or family members.
She had experienced death of her father at an early age and also had a disturbed
relationship with her boyfriend during college.
Had been hospitalised once for 5 days due to acute jaundice.
No exposure to drugs and alcohols.
Paternal grandmother had schizophrenia.
Severe hallucinations from 6 months.
Hears whispering sounds and visualises a “friend” who is same as the age of Dora and a
male.
Dora often experiences that she is in danger and somebody will harm her.
Continuous talking to herself.
Often gets confused when asked about day and night or the present time.
No operations or surgeries have been experienced by the patient till date.
Schizophrenia is often confused with depression and anxiety (Jónsdóttir and et.al., 2013).
The health practitioner has to perform respective question answer sessions so that in-depth
history of the patient is acquired and then necessary conclusions can be made. The biographical
3
history of Dora presents that her hospitalisation experience is only one in number but she has
been subjected to mentally ill conditions throughout major part of her life. The presence of
schizophrenia is prevalent in her genes because her paternal grandmother also experienced the
same. Physical relationships were not so productive or soothing for Dora's conditions. She had
been emotionally disturbed because of her father's death and boyfriend's abusive behaviour. All
these conditions indicate her probability of getting diagnosed with schizophrenia.
COLLABORATIVE/CORROBORATIVE HISTORY
The collaborative and corroborative evidences or history help in reaching a conclusion
whether proposed doubt is appropriate or not (Demjaha, MacCabe and Murray, 2012). The
collaborative history was confirmed by collection of findings of both psychiatrist and the
primary health practitioner in Dora's case. The primary doctor was family doctor for Dora since
her childhood. Hence, familiarity with patient's conditions is quite high. The assessments
conducted by both these practitioners led to similar conclusions that there is a prevalence of
mental illness for Dora. She is experiencing severe schizophrenia because of her increasing
hallucinations and minimal interaction with people in the social set up.
To support this claim, the medical practitioners recognised existence of loneliness and
talking to herself in adulthood were primary conditions. Further, she experienced hallucinations
at a stronger level which was confirmed in her description of a male friend who stays with her
throughout the day and everywhere. Her physical structure is quite shabby in appearance and she
twitches continuously. These symptoms and biographical history are the evidences of
corroborative history which depict and strengthen the fact that Dora is not a patient of severe
depression or anxiety but schizophrenia.
DIAGNOSIS
Unlike other biological disorders or diseases that can be diagnosed by conducting
laboratory tests or technical examinations, schizophrenia doesn't have a particular test. Medical
practitioners have to rely on certain criteria for the diagnosis of this mental illness. The various
assessments like physical examination, psychiatric evaluations and screenings, MRI and CT scan
tests are helpful in gathering evidences for the detection of right disease (Vöhringer and et.al.,
2013). The primary doctor listed a series of tests like blood test, sugar, quantification of alcohol
4
been subjected to mentally ill conditions throughout major part of her life. The presence of
schizophrenia is prevalent in her genes because her paternal grandmother also experienced the
same. Physical relationships were not so productive or soothing for Dora's conditions. She had
been emotionally disturbed because of her father's death and boyfriend's abusive behaviour. All
these conditions indicate her probability of getting diagnosed with schizophrenia.
COLLABORATIVE/CORROBORATIVE HISTORY
The collaborative and corroborative evidences or history help in reaching a conclusion
whether proposed doubt is appropriate or not (Demjaha, MacCabe and Murray, 2012). The
collaborative history was confirmed by collection of findings of both psychiatrist and the
primary health practitioner in Dora's case. The primary doctor was family doctor for Dora since
her childhood. Hence, familiarity with patient's conditions is quite high. The assessments
conducted by both these practitioners led to similar conclusions that there is a prevalence of
mental illness for Dora. She is experiencing severe schizophrenia because of her increasing
hallucinations and minimal interaction with people in the social set up.
To support this claim, the medical practitioners recognised existence of loneliness and
talking to herself in adulthood were primary conditions. Further, she experienced hallucinations
at a stronger level which was confirmed in her description of a male friend who stays with her
throughout the day and everywhere. Her physical structure is quite shabby in appearance and she
twitches continuously. These symptoms and biographical history are the evidences of
corroborative history which depict and strengthen the fact that Dora is not a patient of severe
depression or anxiety but schizophrenia.
DIAGNOSIS
Unlike other biological disorders or diseases that can be diagnosed by conducting
laboratory tests or technical examinations, schizophrenia doesn't have a particular test. Medical
practitioners have to rely on certain criteria for the diagnosis of this mental illness. The various
assessments like physical examination, psychiatric evaluations and screenings, MRI and CT scan
tests are helpful in gathering evidences for the detection of right disease (Vöhringer and et.al.,
2013). The primary doctor listed a series of tests like blood test, sugar, quantification of alcohol
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
and drugs, MRI scan and electrocardiogram readings. These were a part of the physical
examination for diagnosis.
The psychiatrist consultation included mental examination of patient for substantiating
the level of mental illness that is visible in Dora's behaviour. The diagnosis also included
consultations from family members and the close friends of patient (Sasayama and et.al., 2013).
Their opinions and reviews helped in acquiring knowledge regarding stimulation of the disorder
in sufferer. The criteria for diagnosis of the mental illness is produced in the DSM-5 i.e.
Diagnostic and Statistical Manual of Mental Disorders (Raffa and et.al., 2012). It is a manual
published by APA i.e. American Psychiatric Association for consultation by the doctors and
healthcare practitioners in the field of mental disorders.
About 1.1 % of the entire population that is categorised in the adult category i.e. above 18
years of age is said to be suffering from schizophrenia (About Schizophrenia, 2014). This is also
known as the prevalence rate. The Australian researches have inferred over the fact that people
suffering from this mental illness can experience either a no disability state or experience major
disabilities and disorders in assistance (Schizophrenia – Diagnosis, 2017). The age group 15 to
30 is considered to be more vulnerable in onset of this illness. The risk factors associated with
people developing this illness include a family history and indulging in drugs that alter mental
balance (About Schizophrenia, 2014). Teenagers are highly subjected to drugs which are also
known as psychoactive or psychotropic because they fluctuate the mental balance. Furthermore,
the complications experienced by mother in pregnancy also leads to development of such a
disease (Whitton, Treadway and Pizzagalli, 2015).
The predisposing factors linked with the development of schizophrenia in general
audience include presence of schizophrenic genes in parents or the family history (Baker and
et.al., 2014). If there are more number of blood relatives with this illness then next generation is
highly vulnerable simultaneously. Additionally, the socio-cultural aspects associated with life of
a person are also contributing to the mental disharmony. This further inclines them to become
schizophrenic and seek medical intervention (Schizophrenia – Diagnosis, 2017). Psychological
disturbances caused to a person's mental orientation also lead to occurrence of this disease. In
Dora's situation, loss of her father had a tragic impact over her psychological balance.
The common co-morbidities linked with schizophrenia include development of pre-
existing symptoms like depression and anxiety (Rasic and et.al., 2014). There is also an increase
5
examination for diagnosis.
The psychiatrist consultation included mental examination of patient for substantiating
the level of mental illness that is visible in Dora's behaviour. The diagnosis also included
consultations from family members and the close friends of patient (Sasayama and et.al., 2013).
Their opinions and reviews helped in acquiring knowledge regarding stimulation of the disorder
in sufferer. The criteria for diagnosis of the mental illness is produced in the DSM-5 i.e.
Diagnostic and Statistical Manual of Mental Disorders (Raffa and et.al., 2012). It is a manual
published by APA i.e. American Psychiatric Association for consultation by the doctors and
healthcare practitioners in the field of mental disorders.
About 1.1 % of the entire population that is categorised in the adult category i.e. above 18
years of age is said to be suffering from schizophrenia (About Schizophrenia, 2014). This is also
known as the prevalence rate. The Australian researches have inferred over the fact that people
suffering from this mental illness can experience either a no disability state or experience major
disabilities and disorders in assistance (Schizophrenia – Diagnosis, 2017). The age group 15 to
30 is considered to be more vulnerable in onset of this illness. The risk factors associated with
people developing this illness include a family history and indulging in drugs that alter mental
balance (About Schizophrenia, 2014). Teenagers are highly subjected to drugs which are also
known as psychoactive or psychotropic because they fluctuate the mental balance. Furthermore,
the complications experienced by mother in pregnancy also leads to development of such a
disease (Whitton, Treadway and Pizzagalli, 2015).
The predisposing factors linked with the development of schizophrenia in general
audience include presence of schizophrenic genes in parents or the family history (Baker and
et.al., 2014). If there are more number of blood relatives with this illness then next generation is
highly vulnerable simultaneously. Additionally, the socio-cultural aspects associated with life of
a person are also contributing to the mental disharmony. This further inclines them to become
schizophrenic and seek medical intervention (Schizophrenia – Diagnosis, 2017). Psychological
disturbances caused to a person's mental orientation also lead to occurrence of this disease. In
Dora's situation, loss of her father had a tragic impact over her psychological balance.
The common co-morbidities linked with schizophrenia include development of pre-
existing symptoms like depression and anxiety (Rasic and et.al., 2014). There is also an increase
5

in the psychiatric co-morbidities of this disease which is further increased by consequent abusive
activities. This implies that there are chances that the patient might harm him/herself.
COMMON INTERVENTIONS AND RECOVERY PLAN
The common interventions that are provided to patients with schizophrenia for reducing
their pain and suffering include use of antipsychotics which are specialised tranquillisers given
to patients when their physical behaviour goes out of control (Everybody matters 3: engaging
patients and relatives in decision making to promote dignity, 2010). These are termed as
pharmacological interventions. A care program is launched in which the service providers
address the basic needs and requirements of patient and appoint a professional care provider to
look after each and every need of the patient with keen monitoring (Schizophrenia, 2017). The
psychological treatment includes therapeutic measures which engage arts, family and cognitive
behaviour therapy.
Dora is receiving psychological intervention with her mother's support and strict
supervision of her psychiatrist. Since, she is not involved with drugs and alcohol, there is a scope
of improvement. In case of violent behaviour or situation of harming herself, Dora shall be
provided antipsychotics. Currently, there are no medications provided to the patient which
directly implies that there are no side-effects. The multidisciplinary team active in providing care
to the patient have certain roles in providing the intervention without any barrier. These are
depicted as follows: Doctor has to prescribe right treatment according to mental conditions of Dora. Nurse monitors the patient continuously and restricts activities that can increase the
potentiality of schizophrenia. Support Group must look after the fact that every patient whose is being treated with this
disease doesn't get subjected to abuse or exploitation in any manner.
Community organisation should provide support to Dora and her family in a way that
socio-cultural barriers do not hinder her treatment.
Following recovery plan has been developed for Dora:
Goals: To improve Dora's mental condition and reduce impact of schizophrenia.
Activities: The entire treatment is divided into following activities:
Activity 1 Recognising different positions and places
6
activities. This implies that there are chances that the patient might harm him/herself.
COMMON INTERVENTIONS AND RECOVERY PLAN
The common interventions that are provided to patients with schizophrenia for reducing
their pain and suffering include use of antipsychotics which are specialised tranquillisers given
to patients when their physical behaviour goes out of control (Everybody matters 3: engaging
patients and relatives in decision making to promote dignity, 2010). These are termed as
pharmacological interventions. A care program is launched in which the service providers
address the basic needs and requirements of patient and appoint a professional care provider to
look after each and every need of the patient with keen monitoring (Schizophrenia, 2017). The
psychological treatment includes therapeutic measures which engage arts, family and cognitive
behaviour therapy.
Dora is receiving psychological intervention with her mother's support and strict
supervision of her psychiatrist. Since, she is not involved with drugs and alcohol, there is a scope
of improvement. In case of violent behaviour or situation of harming herself, Dora shall be
provided antipsychotics. Currently, there are no medications provided to the patient which
directly implies that there are no side-effects. The multidisciplinary team active in providing care
to the patient have certain roles in providing the intervention without any barrier. These are
depicted as follows: Doctor has to prescribe right treatment according to mental conditions of Dora. Nurse monitors the patient continuously and restricts activities that can increase the
potentiality of schizophrenia. Support Group must look after the fact that every patient whose is being treated with this
disease doesn't get subjected to abuse or exploitation in any manner.
Community organisation should provide support to Dora and her family in a way that
socio-cultural barriers do not hinder her treatment.
Following recovery plan has been developed for Dora:
Goals: To improve Dora's mental condition and reduce impact of schizophrenia.
Activities: The entire treatment is divided into following activities:
Activity 1 Recognising different positions and places
6
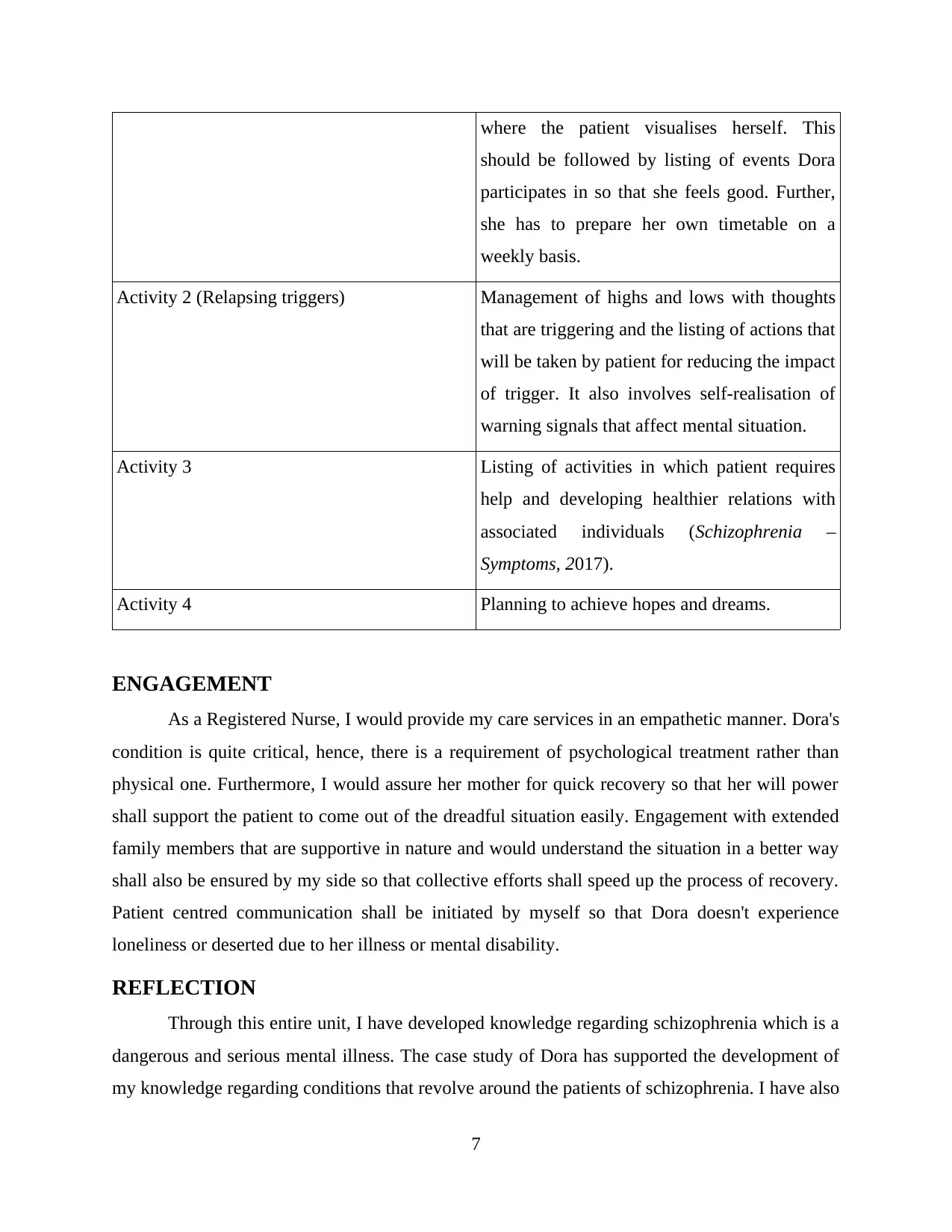
where the patient visualises herself. This
should be followed by listing of events Dora
participates in so that she feels good. Further,
she has to prepare her own timetable on a
weekly basis.
Activity 2 (Relapsing triggers) Management of highs and lows with thoughts
that are triggering and the listing of actions that
will be taken by patient for reducing the impact
of trigger. It also involves self-realisation of
warning signals that affect mental situation.
Activity 3 Listing of activities in which patient requires
help and developing healthier relations with
associated individuals (Schizophrenia –
Symptoms, 2017).
Activity 4 Planning to achieve hopes and dreams.
ENGAGEMENT
As a Registered Nurse, I would provide my care services in an empathetic manner. Dora's
condition is quite critical, hence, there is a requirement of psychological treatment rather than
physical one. Furthermore, I would assure her mother for quick recovery so that her will power
shall support the patient to come out of the dreadful situation easily. Engagement with extended
family members that are supportive in nature and would understand the situation in a better way
shall also be ensured by my side so that collective efforts shall speed up the process of recovery.
Patient centred communication shall be initiated by myself so that Dora doesn't experience
loneliness or deserted due to her illness or mental disability.
REFLECTION
Through this entire unit, I have developed knowledge regarding schizophrenia which is a
dangerous and serious mental illness. The case study of Dora has supported the development of
my knowledge regarding conditions that revolve around the patients of schizophrenia. I have also
7
should be followed by listing of events Dora
participates in so that she feels good. Further,
she has to prepare her own timetable on a
weekly basis.
Activity 2 (Relapsing triggers) Management of highs and lows with thoughts
that are triggering and the listing of actions that
will be taken by patient for reducing the impact
of trigger. It also involves self-realisation of
warning signals that affect mental situation.
Activity 3 Listing of activities in which patient requires
help and developing healthier relations with
associated individuals (Schizophrenia –
Symptoms, 2017).
Activity 4 Planning to achieve hopes and dreams.
ENGAGEMENT
As a Registered Nurse, I would provide my care services in an empathetic manner. Dora's
condition is quite critical, hence, there is a requirement of psychological treatment rather than
physical one. Furthermore, I would assure her mother for quick recovery so that her will power
shall support the patient to come out of the dreadful situation easily. Engagement with extended
family members that are supportive in nature and would understand the situation in a better way
shall also be ensured by my side so that collective efforts shall speed up the process of recovery.
Patient centred communication shall be initiated by myself so that Dora doesn't experience
loneliness or deserted due to her illness or mental disability.
REFLECTION
Through this entire unit, I have developed knowledge regarding schizophrenia which is a
dangerous and serious mental illness. The case study of Dora has supported the development of
my knowledge regarding conditions that revolve around the patients of schizophrenia. I have also
7
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

acquired a skill to provide intervention and tackle a patient that has certain type of psychological
disturbances. Being a Registered nurse, it is my prime responsibility to ensure that both family
and the patient are not in a state of trauma due to the unhealthy atmosphere. Lastly, I would like
to infer that the production of recovery plan and implementation of basic diagnostic knowledge
helps in reducing the trigger factors which can reverse the recovery process. This aspect has been
acquired by myself through this assessment.
8
disturbances. Being a Registered nurse, it is my prime responsibility to ensure that both family
and the patient are not in a state of trauma due to the unhealthy atmosphere. Lastly, I would like
to infer that the production of recovery plan and implementation of basic diagnostic knowledge
helps in reducing the trigger factors which can reverse the recovery process. This aspect has been
acquired by myself through this assessment.
8
REFERENCES
Books and Journals
Baker, J. T. & et.al., (2014). Disruption of cortical association networks in schizophrenia and
psychotic bipolar disorder. JAMA psychiatry, 71(2), 109-118.
Bortolon, C., Capdevielle, D., & Raffard, S. (2015). Face recognition in schizophrenia disorder:
A comprehensive review of behavioral, neuroimaging and neurophysiological
studies. Neuroscience & Biobehavioral Reviews, 53, 79-107.
Correll, C. U. & et.al., (2015). Effects of antipsychotics, antidepressants and mood stabilizers on
risk for physical diseases in people with schizophrenia, depression and bipolar
disorder. World Psychiatry, 14(2), 119-136.
Demjaha, A., MacCabe, J. H., & Murray, R. M. (2012). How genes and environmental factors
determine the different neurodevelopmental trajectories of schizophrenia and bipolar
disorder. Schizophrenia bulletin, 38(2), 209-214.
Jónsdóttir, H. & et.al., (2013). Predictors of medication adherence in patients with schizophrenia
and bipolar disorder. Acta Psychiatrica Scandinavica, 127(1), 23-33.
Khademvatan, S., & Yousefi, E. (2014). Investigation of anti-Toxocara and anti-Toxoplasma
antibodies in patients with schizophrenia disorder. Schizophrenia research and
treatment, 2014.
Larsson, H. & et.al., (2013). Risk of bipolar disorder and schizophrenia in relatives of people
with attention-deficit hyperactivity disorder. The British Journal of Psychiatry, 203(2),
103-106.
Raffa, M. & et.al., (2012). Reduced antioxidant defense systems in schizophrenia and bipolar I
disorder. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 39(2), 371-
375.
Rasic, D. & et.al., (2014). Risk of mental illness in offspring of parents with schizophrenia,
bipolar disorder, and major depressive disorder: a meta-analysis of family high-risk
studies. Schizophrenia bulletin, 40(1), 28-38.
Sasayama, D. & et.al., (2013). Increased cerebrospinal fluid interleukin-6 levels in patients with
schizophrenia and those with major depressive disorder. Journal of psychiatric
research, 47(3), 401-406.
Vöhringer, P. A. & et.al., (2013). Cognitive impairment in bipolar disorder and schizophrenia: a
systematic review. Frontiers in psychiatry, 4, 87.
Whitton, A. E., Treadway, M. T., & Pizzagalli, D. A. (2015). Reward processing dysfunction in
major depression, bipolar disorder and schizophrenia. Current opinion in psychiatry, 28(1),
7.
Online
Everybody matters 3: engaging patients and relatives in decision making to promote dignity
(2010). [Online]. Available Through:<https://www.nursingtimes.net/roles/nurse-
managers/everybody-matters-3-engaging-patients-and-relatives-in-decision-making-to-
promote-dignity-/5015609.article>. [Accessed on 9th June, 2017].
Physical Exam for Schizophrenia (2015). [Online]. Available
Through:<http://www.webmd.com/schizophrenia/physical-exam-for-schizophrenia>.
[Accessed on 9th June, 2017].
9
Books and Journals
Baker, J. T. & et.al., (2014). Disruption of cortical association networks in schizophrenia and
psychotic bipolar disorder. JAMA psychiatry, 71(2), 109-118.
Bortolon, C., Capdevielle, D., & Raffard, S. (2015). Face recognition in schizophrenia disorder:
A comprehensive review of behavioral, neuroimaging and neurophysiological
studies. Neuroscience & Biobehavioral Reviews, 53, 79-107.
Correll, C. U. & et.al., (2015). Effects of antipsychotics, antidepressants and mood stabilizers on
risk for physical diseases in people with schizophrenia, depression and bipolar
disorder. World Psychiatry, 14(2), 119-136.
Demjaha, A., MacCabe, J. H., & Murray, R. M. (2012). How genes and environmental factors
determine the different neurodevelopmental trajectories of schizophrenia and bipolar
disorder. Schizophrenia bulletin, 38(2), 209-214.
Jónsdóttir, H. & et.al., (2013). Predictors of medication adherence in patients with schizophrenia
and bipolar disorder. Acta Psychiatrica Scandinavica, 127(1), 23-33.
Khademvatan, S., & Yousefi, E. (2014). Investigation of anti-Toxocara and anti-Toxoplasma
antibodies in patients with schizophrenia disorder. Schizophrenia research and
treatment, 2014.
Larsson, H. & et.al., (2013). Risk of bipolar disorder and schizophrenia in relatives of people
with attention-deficit hyperactivity disorder. The British Journal of Psychiatry, 203(2),
103-106.
Raffa, M. & et.al., (2012). Reduced antioxidant defense systems in schizophrenia and bipolar I
disorder. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 39(2), 371-
375.
Rasic, D. & et.al., (2014). Risk of mental illness in offspring of parents with schizophrenia,
bipolar disorder, and major depressive disorder: a meta-analysis of family high-risk
studies. Schizophrenia bulletin, 40(1), 28-38.
Sasayama, D. & et.al., (2013). Increased cerebrospinal fluid interleukin-6 levels in patients with
schizophrenia and those with major depressive disorder. Journal of psychiatric
research, 47(3), 401-406.
Vöhringer, P. A. & et.al., (2013). Cognitive impairment in bipolar disorder and schizophrenia: a
systematic review. Frontiers in psychiatry, 4, 87.
Whitton, A. E., Treadway, M. T., & Pizzagalli, D. A. (2015). Reward processing dysfunction in
major depression, bipolar disorder and schizophrenia. Current opinion in psychiatry, 28(1),
7.
Online
Everybody matters 3: engaging patients and relatives in decision making to promote dignity
(2010). [Online]. Available Through:<https://www.nursingtimes.net/roles/nurse-
managers/everybody-matters-3-engaging-patients-and-relatives-in-decision-making-to-
promote-dignity-/5015609.article>. [Accessed on 9th June, 2017].
Physical Exam for Schizophrenia (2015). [Online]. Available
Through:<http://www.webmd.com/schizophrenia/physical-exam-for-schizophrenia>.
[Accessed on 9th June, 2017].
9
Schizophrenia – Diagnosis (2017). [Online]. Available
Through:<http://www.nhs.uk/conditions/Schizophrenia/Pages/Diagnosis.aspx>. [Accessed
on 9th June, 2017].
Schizophrenia – Symptoms (2017). [Online]. Available
Through:<http://www.nhs.uk/Conditions/Schizophrenia/Pages/Symptoms.aspx>.
[Accessed on 9th June, 2017].
Schizophrenia (2017). [Online]. Available
Through:<http://bestpractice.bmj.com/best-practice/monograph/406/follow-up/
recommendations.html>. [Accessed on 9th June, 2017].
About Schizophrenia. (2014). [Online]. Available
Through:<http://www.schizophreniaresearch.org.au/schizophrenia/about-schizophrenia/>.
[Accessed on 9th June, 2017].
10
Through:<http://www.nhs.uk/conditions/Schizophrenia/Pages/Diagnosis.aspx>. [Accessed
on 9th June, 2017].
Schizophrenia – Symptoms (2017). [Online]. Available
Through:<http://www.nhs.uk/Conditions/Schizophrenia/Pages/Symptoms.aspx>.
[Accessed on 9th June, 2017].
Schizophrenia (2017). [Online]. Available
Through:<http://bestpractice.bmj.com/best-practice/monograph/406/follow-up/
recommendations.html>. [Accessed on 9th June, 2017].
About Schizophrenia. (2014). [Online]. Available
Through:<http://www.schizophreniaresearch.org.au/schizophrenia/about-schizophrenia/>.
[Accessed on 9th June, 2017].
10
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





