Case Study: Systolic Heart Failure and Atrial Fibrillation
VerifiedAdded on 2021/02/19
|12
|1881
|16
Report
AI Summary
This report presents a comprehensive analysis of a case study involving a patient diagnosed with systolic heart failure and atrial fibrillation. The report delves into the pathogenesis of the condition, highlighting the role of atrial fibrillation, age, and hypertension in exacerbating heart failure symptoms such as breathlessness and irregular heartbeats. It also examines the importance of monitoring SpO2 levels and pulse rate as key nursing strategies. Furthermore, the report discusses the pharmacological actions of Lasix and GTN, two common medications used in the treatment of heart failure, explaining their mechanisms of action and therapeutic benefits. The report concludes by emphasizing the significance of both pharmacological interventions and nursing priorities in providing effective care for patients with heart failure. The case study underscores the need for swift responses and appropriate medications to manage and control heart failure exacerbations, particularly in patients with atrial fibrillation.
Concept Map and Guided
question response
question response
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TABLE OF CONTENT
INTRODUCTION...........................................................................................................................1
QUESTION 1...................................................................................................................................1
Pathogenesis of systolic heart failure...........................................................................................1
QUESTION 2 ..................................................................................................................................3
Priority nursing strategy for patient.............................................................................................3
QUESTION 3 ..................................................................................................................................4
Pharmacological actions of Lasix and GTN ...............................................................................4
.....................................................................................................................................................4
CONCLUSION ...............................................................................................................................4
REFERENCES................................................................................................................................5
INTRODUCTION...........................................................................................................................1
QUESTION 1...................................................................................................................................1
Pathogenesis of systolic heart failure...........................................................................................1
QUESTION 2 ..................................................................................................................................3
Priority nursing strategy for patient.............................................................................................3
QUESTION 3 ..................................................................................................................................4
Pharmacological actions of Lasix and GTN ...............................................................................4
.....................................................................................................................................................4
CONCLUSION ...............................................................................................................................4
REFERENCES................................................................................................................................5
INTRODUCTION
Atrial fibrillation is one of the most emerging cause for the development of systolic heart
failure which is responsible for significant mortality and morbidity. The report will provide
analysis of case study of patient named Mrs Brown who has been diagnosed with the acute
exacerbation of heart failure. It will discuss the pathogenesis and nursing strategy for the care
management of patient. The study will also describe the drug actions of common drugs which are
given to patients of systolic heart failure.
QUESTION 1
Pathogenesis of systolic heart failure
Atrial fibrillation (AF) is also called arrhythmia and is known as the condition in which
irregular or abnormal heart rhythms are observed. One of the factor which enhances the risk for
the development of AF is age . Mrs Brown is 78 years old and also has past records of heart
failure. Thus, the symptoms such as irregular heart beats, breathlessness, chest pressure or pain
are visible among the patients of AF. According to Hulkower & Aiken, (2015) atrial fibrillation
can be considered as the first symptom of complication likes heart failure, blood clot or strokes.
It has been observed high blood pressure for long duration can add to increased vulnerabilities of
AF and heart issues.
Mrs Brown also had blood pressure readings as 170/95 mm/Hg which indicates the
hypertension. Due to hypertension her breathlessness and dyspnoea becomes more critical. With
the AF both the heart chambers does not work in synchronization and thus heart beats
abnormally or at higher rates than the normal (Spiesshoefer & et.al., 2019) . Without
synchronization between heart chambers due to AF, lower heart chamber does not pump
sufficient blood to other organs and lungs which give rise to risk such as blood clot or the
excessive burden on heart muscles causing heart failure. Park & et.al., (2016) stated that
uneven breathing due to AF makes the symptoms of systolic heart failure even worse. Atrial
fibrillation is caused when sinus node produces electrical messages in less coordinated way
which makes atria twitch or the irregular pulse rate. Due to this reason the pulse rate monitoring
is also considered as important aspect in nursing strategy and diagnosis. The pulse rate of Mrs
Brown was diagnosed as very high which resulted in breathing shortness. The insufficient supply
to other organs and breathlessness can be monitored by saturated oxygen level in the blood
(SpO2). In the given case study patient has very low value of 85% SpO2.
1
Atrial fibrillation is one of the most emerging cause for the development of systolic heart
failure which is responsible for significant mortality and morbidity. The report will provide
analysis of case study of patient named Mrs Brown who has been diagnosed with the acute
exacerbation of heart failure. It will discuss the pathogenesis and nursing strategy for the care
management of patient. The study will also describe the drug actions of common drugs which are
given to patients of systolic heart failure.
QUESTION 1
Pathogenesis of systolic heart failure
Atrial fibrillation (AF) is also called arrhythmia and is known as the condition in which
irregular or abnormal heart rhythms are observed. One of the factor which enhances the risk for
the development of AF is age . Mrs Brown is 78 years old and also has past records of heart
failure. Thus, the symptoms such as irregular heart beats, breathlessness, chest pressure or pain
are visible among the patients of AF. According to Hulkower & Aiken, (2015) atrial fibrillation
can be considered as the first symptom of complication likes heart failure, blood clot or strokes.
It has been observed high blood pressure for long duration can add to increased vulnerabilities of
AF and heart issues.
Mrs Brown also had blood pressure readings as 170/95 mm/Hg which indicates the
hypertension. Due to hypertension her breathlessness and dyspnoea becomes more critical. With
the AF both the heart chambers does not work in synchronization and thus heart beats
abnormally or at higher rates than the normal (Spiesshoefer & et.al., 2019) . Without
synchronization between heart chambers due to AF, lower heart chamber does not pump
sufficient blood to other organs and lungs which give rise to risk such as blood clot or the
excessive burden on heart muscles causing heart failure. Park & et.al., (2016) stated that
uneven breathing due to AF makes the symptoms of systolic heart failure even worse. Atrial
fibrillation is caused when sinus node produces electrical messages in less coordinated way
which makes atria twitch or the irregular pulse rate. Due to this reason the pulse rate monitoring
is also considered as important aspect in nursing strategy and diagnosis. The pulse rate of Mrs
Brown was diagnosed as very high which resulted in breathing shortness. The insufficient supply
to other organs and breathlessness can be monitored by saturated oxygen level in the blood
(SpO2). In the given case study patient has very low value of 85% SpO2.
1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
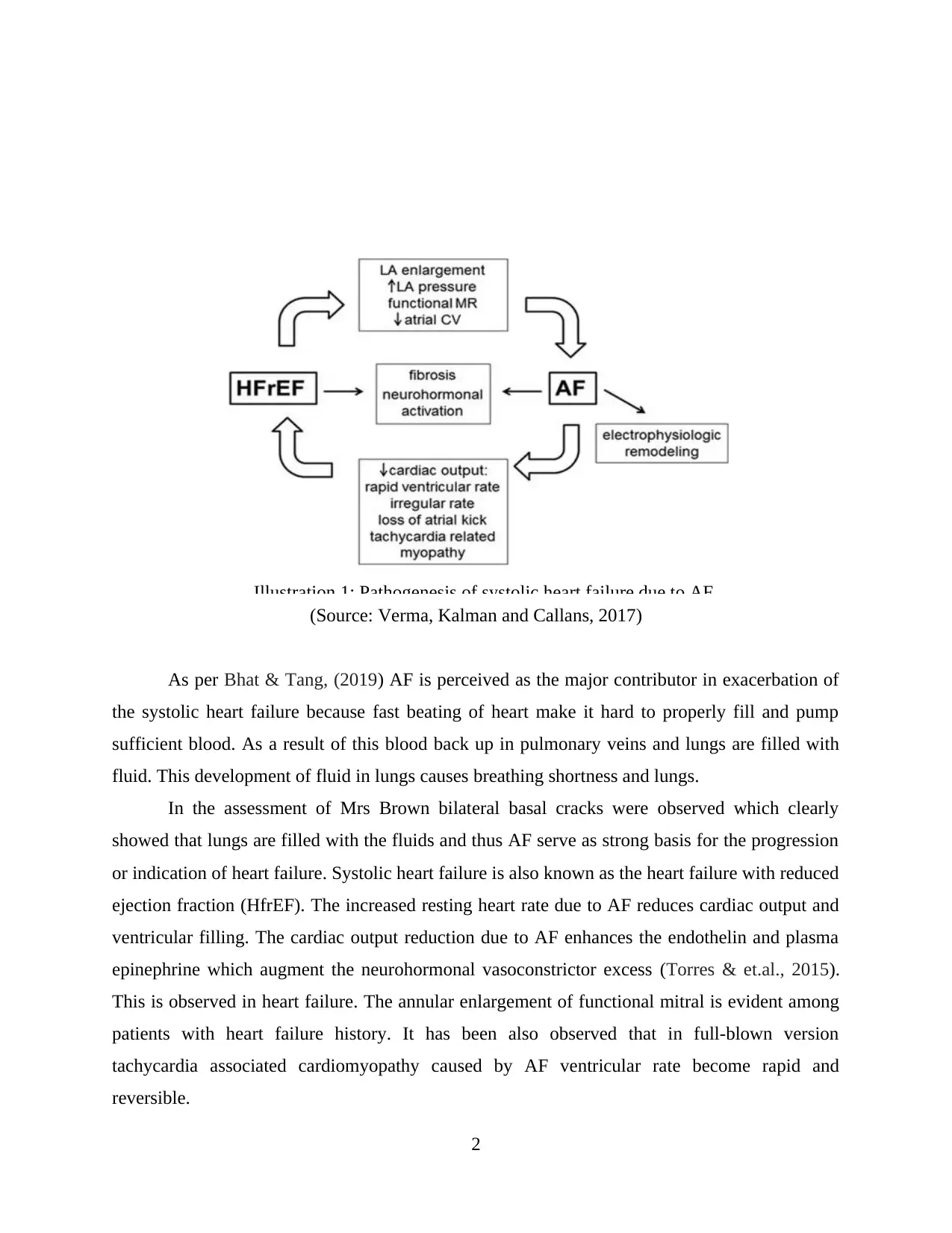
(Source: Verma, Kalman and Callans, 2017)
As per Bhat & Tang, (2019) AF is perceived as the major contributor in exacerbation of
the systolic heart failure because fast beating of heart make it hard to properly fill and pump
sufficient blood. As a result of this blood back up in pulmonary veins and lungs are filled with
fluid. This development of fluid in lungs causes breathing shortness and lungs.
In the assessment of Mrs Brown bilateral basal cracks were observed which clearly
showed that lungs are filled with the fluids and thus AF serve as strong basis for the progression
or indication of heart failure. Systolic heart failure is also known as the heart failure with reduced
ejection fraction (HfrEF). The increased resting heart rate due to AF reduces cardiac output and
ventricular filling. The cardiac output reduction due to AF enhances the endothelin and plasma
epinephrine which augment the neurohormonal vasoconstrictor excess (Torres & et.al., 2015).
This is observed in heart failure. The annular enlargement of functional mitral is evident among
patients with heart failure history. It has been also observed that in full-blown version
tachycardia associated cardiomyopathy caused by AF ventricular rate become rapid and
reversible.
2
Illustration 1: Pathogenesis of systolic heart failure due to AF
As per Bhat & Tang, (2019) AF is perceived as the major contributor in exacerbation of
the systolic heart failure because fast beating of heart make it hard to properly fill and pump
sufficient blood. As a result of this blood back up in pulmonary veins and lungs are filled with
fluid. This development of fluid in lungs causes breathing shortness and lungs.
In the assessment of Mrs Brown bilateral basal cracks were observed which clearly
showed that lungs are filled with the fluids and thus AF serve as strong basis for the progression
or indication of heart failure. Systolic heart failure is also known as the heart failure with reduced
ejection fraction (HfrEF). The increased resting heart rate due to AF reduces cardiac output and
ventricular filling. The cardiac output reduction due to AF enhances the endothelin and plasma
epinephrine which augment the neurohormonal vasoconstrictor excess (Torres & et.al., 2015).
This is observed in heart failure. The annular enlargement of functional mitral is evident among
patients with heart failure history. It has been also observed that in full-blown version
tachycardia associated cardiomyopathy caused by AF ventricular rate become rapid and
reversible.
2
Illustration 1: Pathogenesis of systolic heart failure due to AF
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
QUESTION 2
Priority nursing strategy for patient
The use of effective nursing strategies or the methods assist in managing the health
condition of the patient. The two most prioritized nursing strategies which must be used for Mrs
Brown are as follows:
Nursing strategy 1: The first nursing strategy for the patient is to monitor the oxygen saturation
level so that additional pressure on the blood supply actions can be reduced and systolic heart
failure can be managed.
Rationale and evaluation: With the regular breathlessness and bilateral basal crackles SpO2 level
of patient is 85% (low). It makes it difficult for the patient to perform normal breathing due to
reduction in cardiac output. The atrial fibrillation also makes it hard for the patient to breath with
normal rate and thus due to inadequate oxygen level distal tissues are not supplied with
oxygenated blood. The monitoring of SpO2 level is mandatory as it helps in alleviating activity
intolerance symptoms (Stewart & et.al., 2015). Since patient has heart failure history she may
show modest reduction in the value of SpO2. The nursing strategy will result in reducing the
dyspneic events. It will be helpful for the patient in improving respiratory status and breathing
actions.
Nursing strategy 2: Another priority nursing strategy is to regularly monitor the pulse rate, heart
rhythm and blood pressure so that through suitable medications and control activities heart
failure risk can be controlled and avoided.
Rationale and evaluation:
Mrs Brown has abnormalities in respiratory rate (24 breaths / min) along with high blood
pressure and heart rate. The suggested nursing strategy of monitoring is vital as Tachycardia
enhances the heart rate. The patient is diagnosed with exacerbating systolic heart failure. Atrial
fibrillation acts as potential risk for the heart failure and dysrhythmias. In the early onset of heart
failure the blood pressure of patient is increased thus monitoring of these factors can assist in
regulating the symptoms and severity of heart failure. The monitoring of these factors is helpful
in minimizing the other heart failure complications such as stroke and breathlessness.
The implementation of this nursing strategy also assist in suitable medication so that
heart rhythm and pulse rate can be managed and additional pressure on the ventricular muscles
3
Priority nursing strategy for patient
The use of effective nursing strategies or the methods assist in managing the health
condition of the patient. The two most prioritized nursing strategies which must be used for Mrs
Brown are as follows:
Nursing strategy 1: The first nursing strategy for the patient is to monitor the oxygen saturation
level so that additional pressure on the blood supply actions can be reduced and systolic heart
failure can be managed.
Rationale and evaluation: With the regular breathlessness and bilateral basal crackles SpO2 level
of patient is 85% (low). It makes it difficult for the patient to perform normal breathing due to
reduction in cardiac output. The atrial fibrillation also makes it hard for the patient to breath with
normal rate and thus due to inadequate oxygen level distal tissues are not supplied with
oxygenated blood. The monitoring of SpO2 level is mandatory as it helps in alleviating activity
intolerance symptoms (Stewart & et.al., 2015). Since patient has heart failure history she may
show modest reduction in the value of SpO2. The nursing strategy will result in reducing the
dyspneic events. It will be helpful for the patient in improving respiratory status and breathing
actions.
Nursing strategy 2: Another priority nursing strategy is to regularly monitor the pulse rate, heart
rhythm and blood pressure so that through suitable medications and control activities heart
failure risk can be controlled and avoided.
Rationale and evaluation:
Mrs Brown has abnormalities in respiratory rate (24 breaths / min) along with high blood
pressure and heart rate. The suggested nursing strategy of monitoring is vital as Tachycardia
enhances the heart rate. The patient is diagnosed with exacerbating systolic heart failure. Atrial
fibrillation acts as potential risk for the heart failure and dysrhythmias. In the early onset of heart
failure the blood pressure of patient is increased thus monitoring of these factors can assist in
regulating the symptoms and severity of heart failure. The monitoring of these factors is helpful
in minimizing the other heart failure complications such as stroke and breathlessness.
The implementation of this nursing strategy also assist in suitable medication so that
heart rhythm and pulse rate can be managed and additional pressure on the ventricular muscles
3
can be controlled (Mebazaa & et.al., 2015). Variation or the high value of pulse rate also
indicates the deteriorating aspects of cardiac output. Thus, the strategy is beneficial in improving
the cardiac output and to improve the dyspnoea and to control the heart failure event on time.
QUESTION 3
Pharmacological actions of Lasix and GTN
Glyceryl trinitrate (GTN) is used fro the treatment of high blood pressure, heart failure as
well as chest pain while furosemide (Lasix) is provided to patient for treatment of fluid built in
lungs due to heart failure and other cardiac and kidney diseases. The action of mechanisms of
both of these drugs provided to Mrs Brown is as follows:
Lasix: The action mechanism for this diuretic drug inhibits luminal sodium, potassium and
chlorine cotransporter within loop of Henle limb. The Na-K-Cl are lost in urine by binding to
chloride transport channel (Yıldırım & et.al., 2017). Thus, it improve dyspnoea and
haemodynamic parameter due to congestion and is beneficial for chronic heart failure.
GTN: It relaxes vascular smooth muscles and lowers the end diastolic and left ventricular
pressure. Its higher dose also lowers systemic vascular resistance (López-Sainz & et.al., 2019).
This combined action enhances cardiac output in heart failure. This vasodilatation agent reduces
systolic, arterial and diastolic pressure to maintain coronary perfusion.
CONCLUSION
It can be concluded from the report that along with the pharmacological interventions
nurses must also identify the nursing priorities so that suitable care can be provided to the
patient. It has been also observed that for the patients with atrial fibrillation there are high
vulnerabilities of heart failure thus professionals must give quick response and medications to
manage and control the heart failure exacerbation.
4
indicates the deteriorating aspects of cardiac output. Thus, the strategy is beneficial in improving
the cardiac output and to improve the dyspnoea and to control the heart failure event on time.
QUESTION 3
Pharmacological actions of Lasix and GTN
Glyceryl trinitrate (GTN) is used fro the treatment of high blood pressure, heart failure as
well as chest pain while furosemide (Lasix) is provided to patient for treatment of fluid built in
lungs due to heart failure and other cardiac and kidney diseases. The action of mechanisms of
both of these drugs provided to Mrs Brown is as follows:
Lasix: The action mechanism for this diuretic drug inhibits luminal sodium, potassium and
chlorine cotransporter within loop of Henle limb. The Na-K-Cl are lost in urine by binding to
chloride transport channel (Yıldırım & et.al., 2017). Thus, it improve dyspnoea and
haemodynamic parameter due to congestion and is beneficial for chronic heart failure.
GTN: It relaxes vascular smooth muscles and lowers the end diastolic and left ventricular
pressure. Its higher dose also lowers systemic vascular resistance (López-Sainz & et.al., 2019).
This combined action enhances cardiac output in heart failure. This vasodilatation agent reduces
systolic, arterial and diastolic pressure to maintain coronary perfusion.
CONCLUSION
It can be concluded from the report that along with the pharmacological interventions
nurses must also identify the nursing priorities so that suitable care can be provided to the
patient. It has been also observed that for the patients with atrial fibrillation there are high
vulnerabilities of heart failure thus professionals must give quick response and medications to
manage and control the heart failure exacerbation.
4
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
REFERENCES
Books and Journals
Bhat, P., & Tang, W. W. (2019). Biomarkers to Assess and Guide the Management of Heart
Failure. In Biomarkers in Cardiovascular Disease (pp. 97-108). Elsevier.
Hulkower, S. D., & Aiken, B. A. (2015). What is the best beta-blocker for systolic heart failure?.
López-Sainz, Á. & et.al., (2019). Prevalence of cardiac amyloidosis among elderly patients with
systolic heart failure or conduction disorders. Amyloid, 1-8.
Mebazaa, A. & et.al., (2015). Recommendations on pre‐hospital & early hospital management of
acute heart failure: a consensus paper from the Heart Failure Association of the European
Society of Cardiology, the European Society of Emergency Medicine and the Society of
Academic Emergency Medicine. European journal of heart failure. 17(6). 544-558.
Park, J. J. & et.al., (2016). Renal function, serum sodium level, and outcomes in hospitalized
systolic heart failure patients: An analysis of the COAST study. Medicine. 95(25).
Spiesshoefer, J. & et.al., (2019). APAP therapy does not improve impaired sleep quality and
sympatho-vagal balance: a randomized trial in patients with obstructive sleep apnea and
systolic heart failure. Sleep and Breathing, 1-9.
Stewart, S. & et.al., (2015). Impact of a nurse‐led home and clinic‐based secondary prevention
programme to prevent progressive cardiac dysfunction in high‐risk individuals: the
Nurse‐led Intervention for Less Chronic Heart Failure (NIL‐CHF) randomized controlled
study. European journal of heart failure. 17(6). 620-630.
Torres, D. J. R. & et.al., (2015). Multidisciplinary Approach for a Patient with Advanced Heart
Failure: A Case Report. J Cardiol. 3(1). 1041.
Yıldırım, E. & et.al., (2017). The evaluation of the clinical utility of urocortin 1 and
adrenomedullin versus proBNP in systolic heart failure. Anatolian journal of
cardiology. 17(3). 184.
Online
Verma, A., Kalman, J., & Callans, D., (2017). Treatment of Patients With Atrial Fibrillation and
Heart Failure With Reduced Ejection Fraction. [Online]. Accessed through
<https://www.ahajournals.org/doi/full/10.1161/circulationaha.116.026054>
5
Books and Journals
Bhat, P., & Tang, W. W. (2019). Biomarkers to Assess and Guide the Management of Heart
Failure. In Biomarkers in Cardiovascular Disease (pp. 97-108). Elsevier.
Hulkower, S. D., & Aiken, B. A. (2015). What is the best beta-blocker for systolic heart failure?.
López-Sainz, Á. & et.al., (2019). Prevalence of cardiac amyloidosis among elderly patients with
systolic heart failure or conduction disorders. Amyloid, 1-8.
Mebazaa, A. & et.al., (2015). Recommendations on pre‐hospital & early hospital management of
acute heart failure: a consensus paper from the Heart Failure Association of the European
Society of Cardiology, the European Society of Emergency Medicine and the Society of
Academic Emergency Medicine. European journal of heart failure. 17(6). 544-558.
Park, J. J. & et.al., (2016). Renal function, serum sodium level, and outcomes in hospitalized
systolic heart failure patients: An analysis of the COAST study. Medicine. 95(25).
Spiesshoefer, J. & et.al., (2019). APAP therapy does not improve impaired sleep quality and
sympatho-vagal balance: a randomized trial in patients with obstructive sleep apnea and
systolic heart failure. Sleep and Breathing, 1-9.
Stewart, S. & et.al., (2015). Impact of a nurse‐led home and clinic‐based secondary prevention
programme to prevent progressive cardiac dysfunction in high‐risk individuals: the
Nurse‐led Intervention for Less Chronic Heart Failure (NIL‐CHF) randomized controlled
study. European journal of heart failure. 17(6). 620-630.
Torres, D. J. R. & et.al., (2015). Multidisciplinary Approach for a Patient with Advanced Heart
Failure: A Case Report. J Cardiol. 3(1). 1041.
Yıldırım, E. & et.al., (2017). The evaluation of the clinical utility of urocortin 1 and
adrenomedullin versus proBNP in systolic heart failure. Anatolian journal of
cardiology. 17(3). 184.
Online
Verma, A., Kalman, J., & Callans, D., (2017). Treatment of Patients With Atrial Fibrillation and
Heart Failure With Reduced Ejection Fraction. [Online]. Accessed through
<https://www.ahajournals.org/doi/full/10.1161/circulationaha.116.026054>
5
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

6

7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

8
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

9

10
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





