Cormac's Case Study: Holistic Assessment, Care Plan, and Recovery-Oriented Nursing Care
VerifiedAdded on 2023/06/05
|11
|2867
|246
AI Summary
This case study explores Cormac's mental health assessment, care plan, and recovery-oriented nursing care. It covers therapeutic engagement, cultural safety, and more.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Nursing
Student’s name:
Institutional:
0
Student’s name:
Institutional:
0
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CORMAC’S CASE STUDY
PART 1: Holistic assessment and planning
1.1. MENTAL STATUS ASSESMENT
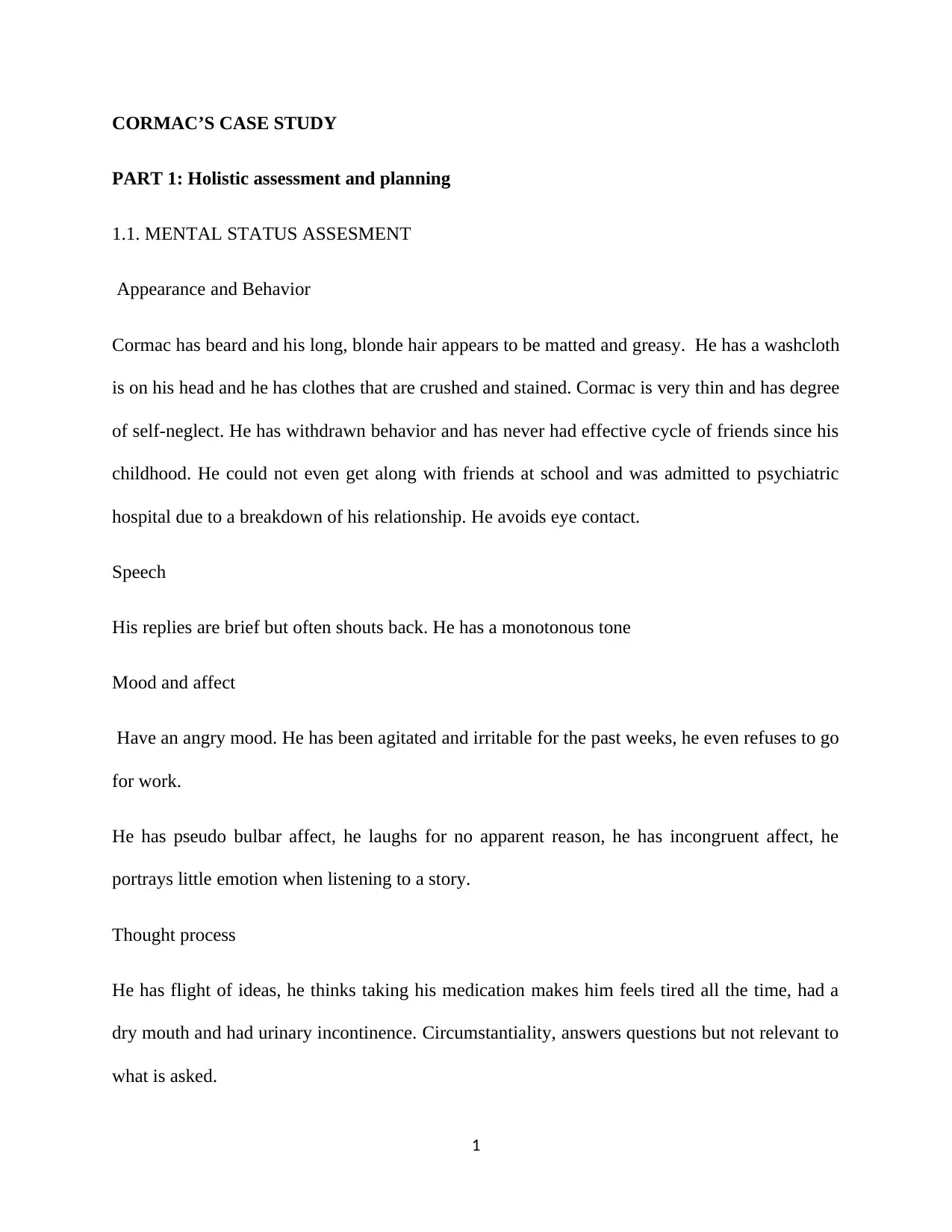
Appearance and Behavior
Cormac has beard and his long, blonde hair appears to be matted and greasy. He has a washcloth
is on his head and he has clothes that are crushed and stained. Cormac is very thin and has degree
of self-neglect. He has withdrawn behavior and has never had effective cycle of friends since his
childhood. He could not even get along with friends at school and was admitted to psychiatric
hospital due to a breakdown of his relationship. He avoids eye contact.
Speech
His replies are brief but often shouts back. He has a monotonous tone
Mood and affect
Have an angry mood. He has been agitated and irritable for the past weeks, he even refuses to go
for work.
He has pseudo bulbar affect, he laughs for no apparent reason, he has incongruent affect, he
portrays little emotion when listening to a story.
Thought process
He has flight of ideas, he thinks taking his medication makes him feels tired all the time, had a
dry mouth and had urinary incontinence. Circumstantiality, answers questions but not relevant to
what is asked.
1
PART 1: Holistic assessment and planning
1.1. MENTAL STATUS ASSESMENT
Appearance and Behavior
Cormac has beard and his long, blonde hair appears to be matted and greasy. He has a washcloth
is on his head and he has clothes that are crushed and stained. Cormac is very thin and has degree
of self-neglect. He has withdrawn behavior and has never had effective cycle of friends since his
childhood. He could not even get along with friends at school and was admitted to psychiatric
hospital due to a breakdown of his relationship. He avoids eye contact.
Speech
His replies are brief but often shouts back. He has a monotonous tone
Mood and affect
Have an angry mood. He has been agitated and irritable for the past weeks, he even refuses to go
for work.
He has pseudo bulbar affect, he laughs for no apparent reason, he has incongruent affect, he
portrays little emotion when listening to a story.
Thought process
He has flight of ideas, he thinks taking his medication makes him feels tired all the time, had a
dry mouth and had urinary incontinence. Circumstantiality, answers questions but not relevant to
what is asked.
1
Thought content
He has delusions, he spends time scrutinizing videos because he thinks his manager has been
recording all his conversations when doing business to catch him making mistakes, that certain
brand of equipment’s has recordings of the conversation he held with spy agency, and that he has
ability to send and receive messages from God through his recordings.
Perception.
He has hallucinations. He hears strange voices that are real talking about hi, his lips move
silently and even turns his head as if he is speaking to someone.
Cognition
He is conscious and well oriented to time, place and person. He however does not pay attention
or concentrate for a long span. He stands up to look out of the window often. He started studying
electronics after high school but dropped out because he could not finish work. His judgement
seems to be poor because he advises customers to buy some products and leave others since it
contains his conversations.
Insight
He is not aware that he’s sick, he tells the parents that there is nothing wrong with him, he
refuses to take medications because he thinks he is okay and that the drugs make him terrible.
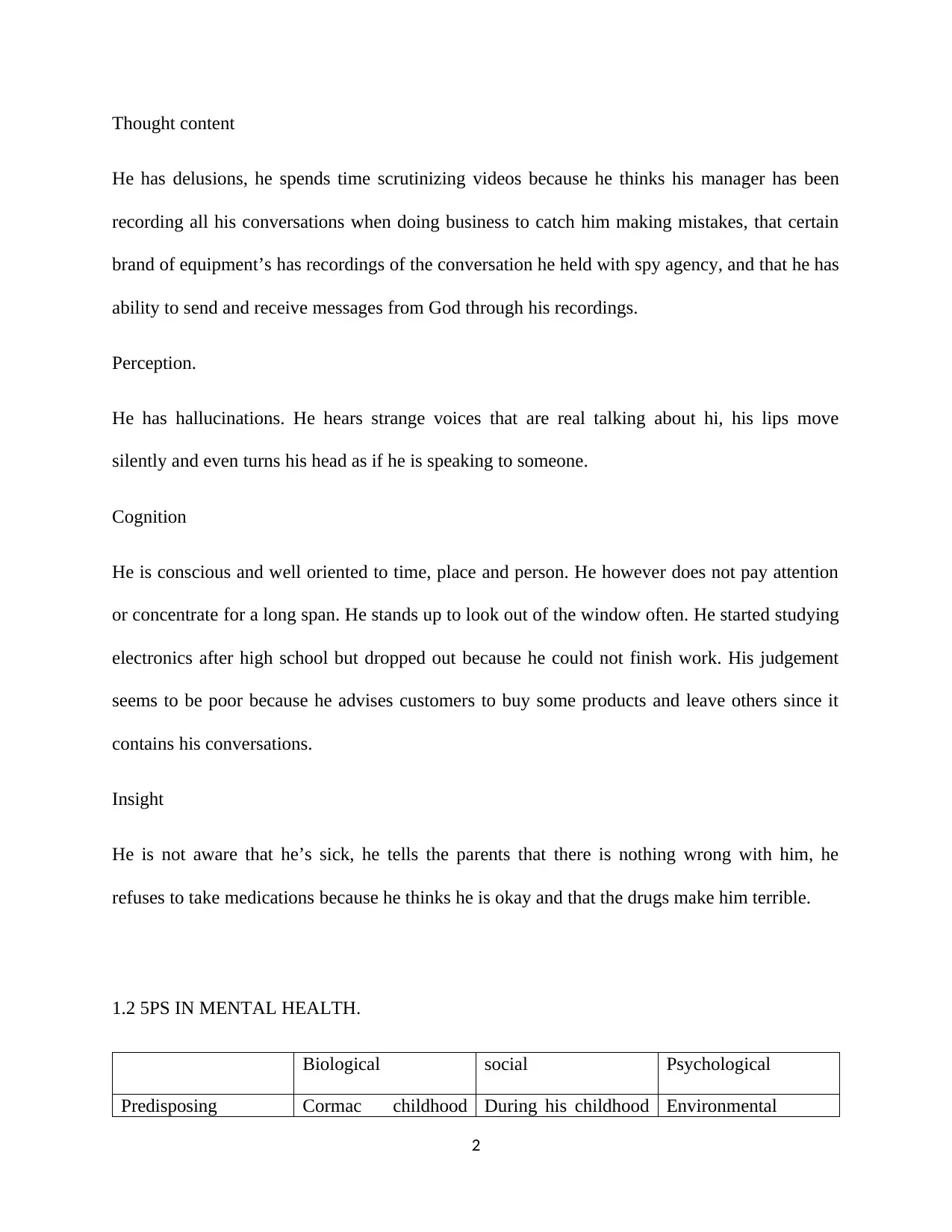
1.2 5PS IN MENTAL HEALTH.
Biological social Psychological
Predisposing Cormac childhood During his childhood Environmental
2
He has delusions, he spends time scrutinizing videos because he thinks his manager has been
recording all his conversations when doing business to catch him making mistakes, that certain
brand of equipment’s has recordings of the conversation he held with spy agency, and that he has
ability to send and receive messages from God through his recordings.
Perception.
He has hallucinations. He hears strange voices that are real talking about hi, his lips move
silently and even turns his head as if he is speaking to someone.
Cognition
He is conscious and well oriented to time, place and person. He however does not pay attention
or concentrate for a long span. He stands up to look out of the window often. He started studying
electronics after high school but dropped out because he could not finish work. His judgement
seems to be poor because he advises customers to buy some products and leave others since it
contains his conversations.
Insight
He is not aware that he’s sick, he tells the parents that there is nothing wrong with him, he
refuses to take medications because he thinks he is okay and that the drugs make him terrible.
1.2 5PS IN MENTAL HEALTH.
Biological social Psychological
Predisposing Cormac childhood During his childhood Environmental
2
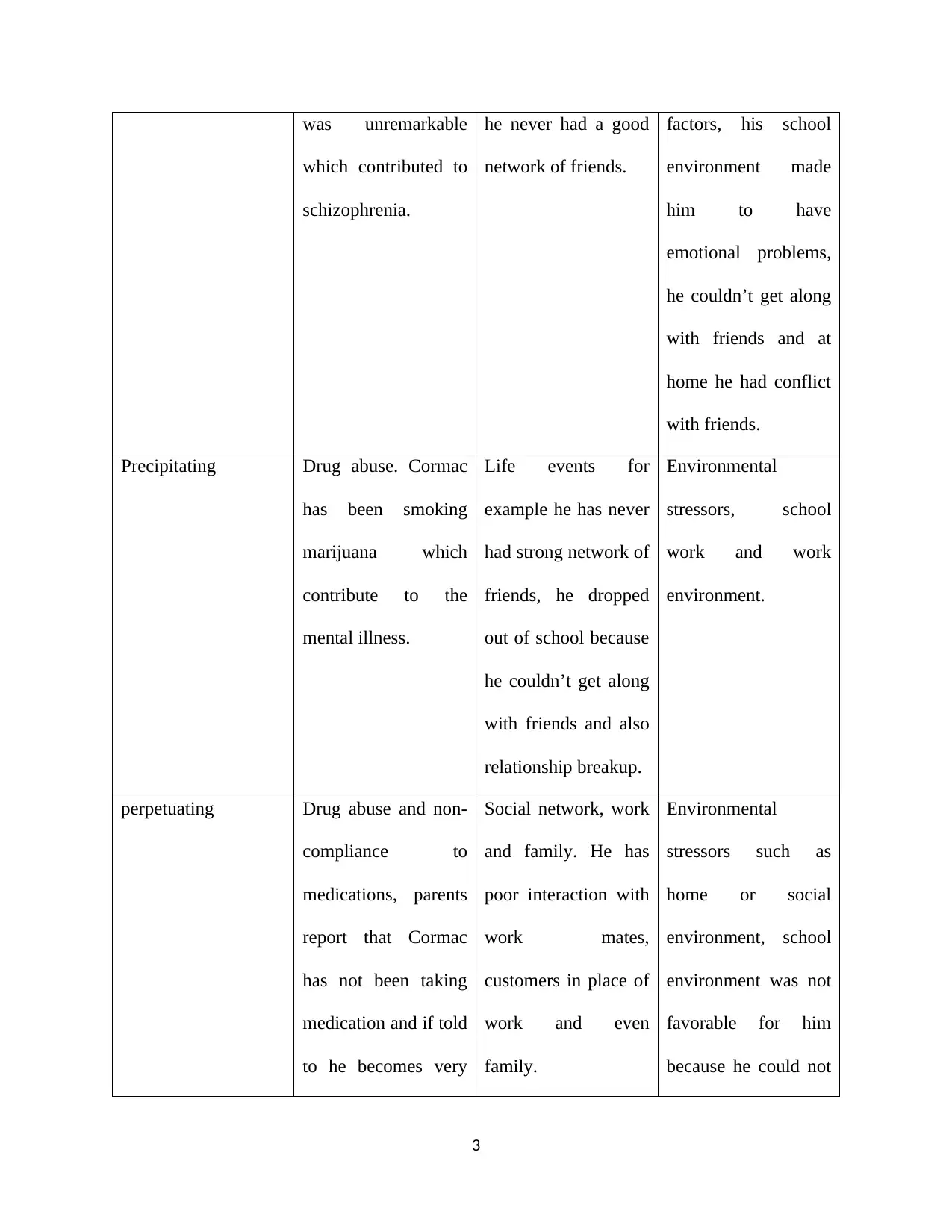
was unremarkable
which contributed to
schizophrenia.
he never had a good
network of friends.
factors, his school
environment made
him to have
emotional problems,
he couldn’t get along
with friends and at
home he had conflict
with friends.
Precipitating Drug abuse. Cormac
has been smoking
marijuana which
contribute to the
mental illness.
Life events for
example he has never
had strong network of
friends, he dropped
out of school because
he couldn’t get along
with friends and also
relationship breakup.
Environmental
stressors, school
work and work
environment.
perpetuating Drug abuse and non-
compliance to
medications, parents
report that Cormac
has not been taking
medication and if told
to he becomes very
Social network, work
and family. He has
poor interaction with
work mates,
customers in place of
work and even
family.
Environmental
stressors such as
home or social
environment, school
environment was not
favorable for him
because he could not
3
which contributed to
schizophrenia.
he never had a good
network of friends.
factors, his school
environment made
him to have
emotional problems,
he couldn’t get along
with friends and at
home he had conflict
with friends.
Precipitating Drug abuse. Cormac
has been smoking
marijuana which
contribute to the
mental illness.
Life events for
example he has never
had strong network of
friends, he dropped
out of school because
he couldn’t get along
with friends and also
relationship breakup.
Environmental
stressors, school
work and work
environment.
perpetuating Drug abuse and non-
compliance to
medications, parents
report that Cormac
has not been taking
medication and if told
to he becomes very
Social network, work
and family. He has
poor interaction with
work mates,
customers in place of
work and even
family.
Environmental
stressors such as
home or social
environment, school
environment was not
favorable for him
because he could not
3
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
hostile. get along with friends
and his had
unremarkable
childhood.
Protective Medications, they act
directly on to
biological mechanism
that caused his
condition, for
example monoamine
oxidase inhibitors.
Training on social
skills, social
adjustment, and
social cognition
(Spence, Zubrick, &
Lawrence, 2017).
Cognitive behavioral
therapy and cognition
training.
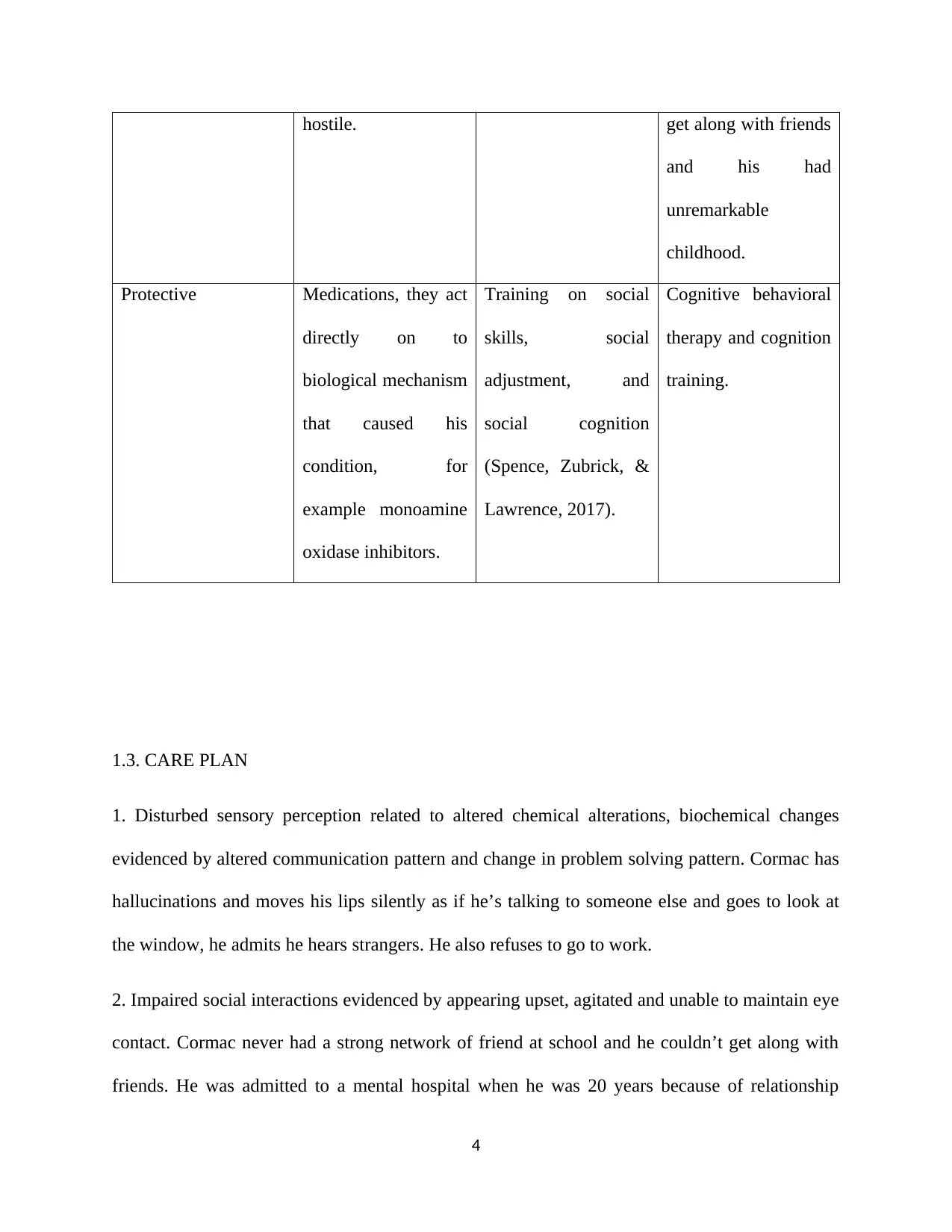
1.3. CARE PLAN
1. Disturbed sensory perception related to altered chemical alterations, biochemical changes
evidenced by altered communication pattern and change in problem solving pattern. Cormac has
hallucinations and moves his lips silently as if he’s talking to someone else and goes to look at
the window, he admits he hears strangers. He also refuses to go to work.
2. Impaired social interactions evidenced by appearing upset, agitated and unable to maintain eye
contact. Cormac never had a strong network of friend at school and he couldn’t get along with
friends. He was admitted to a mental hospital when he was 20 years because of relationship
4
and his had
unremarkable
childhood.
Protective Medications, they act
directly on to
biological mechanism
that caused his
condition, for
example monoamine
oxidase inhibitors.
Training on social
skills, social
adjustment, and
social cognition
(Spence, Zubrick, &
Lawrence, 2017).
Cognitive behavioral
therapy and cognition
training.
1.3. CARE PLAN
1. Disturbed sensory perception related to altered chemical alterations, biochemical changes
evidenced by altered communication pattern and change in problem solving pattern. Cormac has
hallucinations and moves his lips silently as if he’s talking to someone else and goes to look at
the window, he admits he hears strangers. He also refuses to go to work.
2. Impaired social interactions evidenced by appearing upset, agitated and unable to maintain eye
contact. Cormac never had a strong network of friend at school and he couldn’t get along with
friends. He was admitted to a mental hospital when he was 20 years because of relationship
4
breakdown and he has also been behaving strangely with customers at work, he chooses for them
the brand of equipment to buy and not to buy.
INTERVENTIONS
1. Accept the fact that the voices are real but explain to Cormac that you do not hear them; refer
as “your voices” (Rogers, 2012). This makes client to cast doubts. Intervene with one on one or
seclusion when necessary. Intervene before anxiety begins, if he is out of control then use of
chemical can implemented (Carhuff, 2017). Adhere to easy, basic and reality based topics of
conversations. This help him to focus on one idea at a go. Moreover, try to explain to him the
consequences of his choices; for examples, the impact of him not going to work
2. Ensure the patient is taking drugs and even asses if medication have reached therapeutic
levels, most of the positive symptoms of schizophrenia will subside with medications which
facilitate interactions (Evans, 2017). Since the patient is very withdrawn, a one on one activities
with someone should be planned, this will help him learn to feel safe and he may even gradually
participate in a group therapy. Engage the client with other clients in social interactions and
activities such as games, this will help client to feel part of the group and that he is wanted.
1.4. CLINICAL HANDOVER
Identity; my name is-. from school of nursing. Cormac, 24 years, diagnosed with schizophrenia,
has withdrawn behavior, never had a strong network of friends since childhood, couldn’t get
along with friends at school. He has long, blonde, greasy and matted hair and his clothes are
crushed and stained. The patient has monotonous tone and monosyllabic pressure of speech, he is
hostile and shouts at parents when asked to take medications. He has an angry mood and has
been irritable for the past weeks, unable to concentrate and remain seated for long and often gets
5
the brand of equipment to buy and not to buy.
INTERVENTIONS
1. Accept the fact that the voices are real but explain to Cormac that you do not hear them; refer
as “your voices” (Rogers, 2012). This makes client to cast doubts. Intervene with one on one or
seclusion when necessary. Intervene before anxiety begins, if he is out of control then use of
chemical can implemented (Carhuff, 2017). Adhere to easy, basic and reality based topics of
conversations. This help him to focus on one idea at a go. Moreover, try to explain to him the
consequences of his choices; for examples, the impact of him not going to work
2. Ensure the patient is taking drugs and even asses if medication have reached therapeutic
levels, most of the positive symptoms of schizophrenia will subside with medications which
facilitate interactions (Evans, 2017). Since the patient is very withdrawn, a one on one activities
with someone should be planned, this will help him learn to feel safe and he may even gradually
participate in a group therapy. Engage the client with other clients in social interactions and
activities such as games, this will help client to feel part of the group and that he is wanted.
1.4. CLINICAL HANDOVER
Identity; my name is-. from school of nursing. Cormac, 24 years, diagnosed with schizophrenia,
has withdrawn behavior, never had a strong network of friends since childhood, couldn’t get
along with friends at school. He has long, blonde, greasy and matted hair and his clothes are
crushed and stained. The patient has monotonous tone and monosyllabic pressure of speech, he is
hostile and shouts at parents when asked to take medications. He has an angry mood and has
been irritable for the past weeks, unable to concentrate and remain seated for long and often gets
5
up to look at the window. He has flight of ideas and thinks taking medication makes him feels
tired all the time. He has delusion, he believes his boss has been taping all the conversations with
the customers to catch him with mistake. He hallucinates and hears strange voices which are real.
he has religious delusions, he believes he can send and receive messages from God through the
radio and television.
PART 2: Therapeutic engagement and clinical interpretation
2.1 Therapeutic relationship
Developing a therapeutic relationship with a patient is one of the key elements that contributes
greatly to the wellness of a patient (Unhjem, Vatne, & Hem, 2018). It is a key determinant of the
positive results for people with mental health disorders irrespective of the kind of therapy used
(Sucala et.al, 2012). This is why it is important to develop a therapeutic relationship with
Cormac. The patient is the only one who can perfectly describe his experiences since he is the
one going through it and a therapeutic relationship will help the nurse to get him describe the
experience well. To develop such a relationship with Cormac there are some key factors to
consider. First, empathy should be embrace (Erskine, Moursund, & Trautmann, 2013). This is
the act of being able to identify with the feelings, thoughts or his emotional state (Edward,
Hercelinskyj, & Giandinoto, J2017). Being empathic will enable Cormac to express his and also
provide an appropriate environment in which he can feel safe sharing his feelings. I should also
engage with him in a genuine manner and be non-judgmental. This means that I should not at
any point try to lie to Cormac or judge him in any way, either concerning his feelings or his
actions. Judging him may create a negative impact and will even restrain him from opening up
more. Another factor to consider is confidentiality (Greenberg, 2014. Cormac should be assured
6
tired all the time. He has delusion, he believes his boss has been taping all the conversations with
the customers to catch him with mistake. He hallucinates and hears strange voices which are real.
he has religious delusions, he believes he can send and receive messages from God through the
radio and television.
PART 2: Therapeutic engagement and clinical interpretation
2.1 Therapeutic relationship
Developing a therapeutic relationship with a patient is one of the key elements that contributes
greatly to the wellness of a patient (Unhjem, Vatne, & Hem, 2018). It is a key determinant of the
positive results for people with mental health disorders irrespective of the kind of therapy used
(Sucala et.al, 2012). This is why it is important to develop a therapeutic relationship with
Cormac. The patient is the only one who can perfectly describe his experiences since he is the
one going through it and a therapeutic relationship will help the nurse to get him describe the
experience well. To develop such a relationship with Cormac there are some key factors to
consider. First, empathy should be embrace (Erskine, Moursund, & Trautmann, 2013). This is
the act of being able to identify with the feelings, thoughts or his emotional state (Edward,
Hercelinskyj, & Giandinoto, J2017). Being empathic will enable Cormac to express his and also
provide an appropriate environment in which he can feel safe sharing his feelings. I should also
engage with him in a genuine manner and be non-judgmental. This means that I should not at
any point try to lie to Cormac or judge him in any way, either concerning his feelings or his
actions. Judging him may create a negative impact and will even restrain him from opening up
more. Another factor to consider is confidentiality (Greenberg, 2014. Cormac should be assured
6
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
that all that he is going to say will not in any way exposed to other people. This may also involve
ensuring that privacy is maintain while engaging in a discussion with him by selecting a place
where other people cannot hear the conversation. Probing will also help to guide Cormac
examine his feelings. Most importantly, warmth and safety must also be enhanced throughout the
conversation (Australian College of Mental Health Nurses, 2010).
2.2 Cultural safety
The first step to ensure that that culturally safe health care is delivered to Cormac is ensuring
self-awareness by realizing and acknowledging the fact that he differs from the nurse both in
beliefs and practices, for example in age, occupation, religion, ethnic origin and even disability
(Best, 2014). Cormac state and believes that he receives messages from God through radio and
television. This is a clear indication that he believes in God and therefore this must be considered
when delivering care to him. The principle to be applied in this scenario is that cultural safety
aims to enhance or improve the health of an individual. This is why the interventions stated
above was geared towards improving his health status despite the fact that he differs culturally
(Usher, Mills, West, & Power, 2017).
2.3 Recovery-oriented Nursing Care
Health care workers plays a major role in the recovery of patients, however, it is important to
note that health care staff do not possess the key to recovery but instead it is the mental health
patients who do (Sini, Munro, Taylor, & Griffiths, 2015). Therefore, considering the
interventions aimed at improving Cormac’s mental health status, I only do the facilitation
towards achieving recovery. This can only be achieved by learning his disorder and being able to
define what can be done with the resources available. Cormac’s recovery is also achieved
7
ensuring that privacy is maintain while engaging in a discussion with him by selecting a place
where other people cannot hear the conversation. Probing will also help to guide Cormac
examine his feelings. Most importantly, warmth and safety must also be enhanced throughout the
conversation (Australian College of Mental Health Nurses, 2010).
2.2 Cultural safety
The first step to ensure that that culturally safe health care is delivered to Cormac is ensuring
self-awareness by realizing and acknowledging the fact that he differs from the nurse both in
beliefs and practices, for example in age, occupation, religion, ethnic origin and even disability
(Best, 2014). Cormac state and believes that he receives messages from God through radio and
television. This is a clear indication that he believes in God and therefore this must be considered
when delivering care to him. The principle to be applied in this scenario is that cultural safety
aims to enhance or improve the health of an individual. This is why the interventions stated
above was geared towards improving his health status despite the fact that he differs culturally
(Usher, Mills, West, & Power, 2017).
2.3 Recovery-oriented Nursing Care
Health care workers plays a major role in the recovery of patients, however, it is important to
note that health care staff do not possess the key to recovery but instead it is the mental health
patients who do (Sini, Munro, Taylor, & Griffiths, 2015). Therefore, considering the
interventions aimed at improving Cormac’s mental health status, I only do the facilitation
towards achieving recovery. This can only be achieved by learning his disorder and being able to
define what can be done with the resources available. Cormac’s recovery is also achieved
7
through therapeutic relationship which enables the nurse to develop a more personal relationship
with him. It is through this interaction that the nurse can get to give hope to him to enable him
depend on himself with only help from others and not entirely count on others. Recovery may
occur and clinical manifestation recur again. Therefore, as a nurse I have to lead Cormac towards
achieving personal identity, that is a sense of self that is even past diagnostic label. The
individual should however recognize as much as possible that they are at the Centre of the care
that is given to them. Recovery may not be all about cure but letting the individual get to live a
meaningful life that is purposeful and satisfying. The ability to be able to make choices and be
valued as an important member of the community (Slade, 2010). As a nurse I should also not
only be keen in the curative process of Cormac but also I should focus more on the whole life of
Cormac by working with him even beyond hospital care to helping him in his career to be able to
realize his goals, hopes and dreams (Slade, Teesson, & Burgess, 2013). The attitude and dignity
of a nurse towards a patient recovery is also very important (Pope, 2012). A nurse should truthful
and respectful to the client. As for Cormac this means that I would be sensitive to her values,
culture and belief and tell him the truth in all matters.
8
with him. It is through this interaction that the nurse can get to give hope to him to enable him
depend on himself with only help from others and not entirely count on others. Recovery may
occur and clinical manifestation recur again. Therefore, as a nurse I have to lead Cormac towards
achieving personal identity, that is a sense of self that is even past diagnostic label. The
individual should however recognize as much as possible that they are at the Centre of the care
that is given to them. Recovery may not be all about cure but letting the individual get to live a
meaningful life that is purposeful and satisfying. The ability to be able to make choices and be
valued as an important member of the community (Slade, 2010). As a nurse I should also not
only be keen in the curative process of Cormac but also I should focus more on the whole life of
Cormac by working with him even beyond hospital care to helping him in his career to be able to
realize his goals, hopes and dreams (Slade, Teesson, & Burgess, 2013). The attitude and dignity
of a nurse towards a patient recovery is also very important (Pope, 2012). A nurse should truthful
and respectful to the client. As for Cormac this means that I would be sensitive to her values,
culture and belief and tell him the truth in all matters.
8
References
Australian College of Mental Health Nurses (2010) Standards of Practice in Mental Health
Nursing, Australian College of Mental Health Nurses,
http://www.acmhn.org/publications/standards-of-practice (accessed 10/10/2018)
Barlow, D. H. (Ed.). (2014). Clinical handbook of psychological disorders: A step-by-step
treatment manual. Guilford publications.
Best, O. (2014). The cultural safety journey: an Australian nursing context. In Yatdjuligin
aboriginal and Torres strait islander nursing and midwifery care (pp. 51-73).
Cambridge, Melbourne, Australia.
Carkhuff, R. (2017). Toward effective counseling and psychotherapy: Training and practice.
Routledge.
Downes, C., Gill, A., Doyle, L., Morrissey, J., & Higgins, A. (2016). Survey of mental health
nurses’ attitudes towards risk assessment, risk assessment tools and positive risk. Journal
of Psychiatric and Mental Health Nursing, 23(3-4), 188–197. doi:10.1111/jpm.12299
Edward, K. l., Hercelinskyj, G., & Giandinoto, J. A. (2017). Emotional labour in mental health
nursing: An integrative systematic review. International Journal of Mental Health
Nursing, 26(3), 215-225. doi:doi:10.1111/inm.12330
Erskine, R., Moursund, J., & Trautmann, R. (2013). Beyond empathy: A therapy of contact-in
relationships. Routledge.
Evans, K. (2017). Schizophrenia and psychotic disorders, in K. Evans; D. Nizette and A. O'Brien
(eds.), Psychiatric and mental health nursing, (pp. 341-369). Chatswood: Elsevier.
Greenberg, L. (2014). The therapeutic relationship in emotion-focused
therapy. Psychotherapy, 51(3), 350.
9
Australian College of Mental Health Nurses (2010) Standards of Practice in Mental Health
Nursing, Australian College of Mental Health Nurses,
http://www.acmhn.org/publications/standards-of-practice (accessed 10/10/2018)
Barlow, D. H. (Ed.). (2014). Clinical handbook of psychological disorders: A step-by-step
treatment manual. Guilford publications.
Best, O. (2014). The cultural safety journey: an Australian nursing context. In Yatdjuligin
aboriginal and Torres strait islander nursing and midwifery care (pp. 51-73).
Cambridge, Melbourne, Australia.
Carkhuff, R. (2017). Toward effective counseling and psychotherapy: Training and practice.
Routledge.
Downes, C., Gill, A., Doyle, L., Morrissey, J., & Higgins, A. (2016). Survey of mental health
nurses’ attitudes towards risk assessment, risk assessment tools and positive risk. Journal
of Psychiatric and Mental Health Nursing, 23(3-4), 188–197. doi:10.1111/jpm.12299
Edward, K. l., Hercelinskyj, G., & Giandinoto, J. A. (2017). Emotional labour in mental health
nursing: An integrative systematic review. International Journal of Mental Health
Nursing, 26(3), 215-225. doi:doi:10.1111/inm.12330
Erskine, R., Moursund, J., & Trautmann, R. (2013). Beyond empathy: A therapy of contact-in
relationships. Routledge.
Evans, K. (2017). Schizophrenia and psychotic disorders, in K. Evans; D. Nizette and A. O'Brien
(eds.), Psychiatric and mental health nursing, (pp. 341-369). Chatswood: Elsevier.
Greenberg, L. (2014). The therapeutic relationship in emotion-focused
therapy. Psychotherapy, 51(3), 350.
9
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Pope, T. (2012). How person-centred care can improve nurses' attitudes to hospitalised older
patients. Nursing Older People (through 2013), 24(1), 32.
Rogers, C. (2012). Client Centred Therapy (New Ed). Hachette UK.
Sini, J., Munro, I., Taylor, B., & Griffiths, D. (2015). Mental health recovery: A review of the
peer reviewed literature. Collegian 24, 53–61
Slade, M. (2010). Mental illness and well-being: the central importance of positive psychology
and recovery approaches. BMC health services research, 10(1), 26.
Slade, J., Teesson, W., & Burgess, P. (2013). The mental health of Australians 2: report on the
2007 National Survey of Mental Health and Wellbeing.
Spence, S., Zubrick, S. & Lawrence, D. (2017). A profile of social, separation and generalized
anxiety disorders in an Australian nationally representative sample of children and
adolescents: Prevalence, comorbidity and correlates, Australian & New Zealand Journal
of Psychiatry, 52, (29) 5, pp. 446 – 460. https://doi.org/10.1177/0004867417741981
Sucala, M., Schnur, J. B., Constantino, M. J., Miller, S. J., Brackman, E. H., & Montgomery, G.
H. (2012). The therapeutic relationship in e-therapy for mental health: a systematic
review. Journal of medical Internet research, 14(4).
Unhjem, J. V., Vatne, S., & Hem, M. H. (2018). Transforming nurse–patient relationships—A
qualitative study of nurse self‐disclosure in mental health care. Journal of Clinical
Nursing, 27(5-6), e798-e807. doi:doi:10.1111/jocn.14191
Usher, K., Mills, J., West, R., & Power, T. (2017). CULTURAL SAFETY IN NURSING AND
MIDWIFERY. Contexts of Nursing: An Introduction, 337.
10
patients. Nursing Older People (through 2013), 24(1), 32.
Rogers, C. (2012). Client Centred Therapy (New Ed). Hachette UK.
Sini, J., Munro, I., Taylor, B., & Griffiths, D. (2015). Mental health recovery: A review of the
peer reviewed literature. Collegian 24, 53–61
Slade, M. (2010). Mental illness and well-being: the central importance of positive psychology
and recovery approaches. BMC health services research, 10(1), 26.
Slade, J., Teesson, W., & Burgess, P. (2013). The mental health of Australians 2: report on the
2007 National Survey of Mental Health and Wellbeing.
Spence, S., Zubrick, S. & Lawrence, D. (2017). A profile of social, separation and generalized
anxiety disorders in an Australian nationally representative sample of children and
adolescents: Prevalence, comorbidity and correlates, Australian & New Zealand Journal
of Psychiatry, 52, (29) 5, pp. 446 – 460. https://doi.org/10.1177/0004867417741981
Sucala, M., Schnur, J. B., Constantino, M. J., Miller, S. J., Brackman, E. H., & Montgomery, G.
H. (2012). The therapeutic relationship in e-therapy for mental health: a systematic
review. Journal of medical Internet research, 14(4).
Unhjem, J. V., Vatne, S., & Hem, M. H. (2018). Transforming nurse–patient relationships—A
qualitative study of nurse self‐disclosure in mental health care. Journal of Clinical
Nursing, 27(5-6), e798-e807. doi:doi:10.1111/jocn.14191
Usher, K., Mills, J., West, R., & Power, T. (2017). CULTURAL SAFETY IN NURSING AND
MIDWIFERY. Contexts of Nursing: An Introduction, 337.
10
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





