A Review of Automatic and Manual CPR Devices in Mechanical Engineering
VerifiedAdded on 2023/06/15
|14
|11785
|493
Literature Review
AI Summary
This literature review examines both automatic and manual devices used in cardiopulmonary resuscitation (CPR). It highlights that while early recognition and high-quality CPR are crucial for survival after cardiac arrest, the effectiveness of manual CPR is often compromised by rescuer fatigue. Automatic devices have been developed to address this issue, either by mimicking manual techniques or using entirely different principles to generate hemodynamic effects. The review categorizes these devices based on actuation method, applied force, working space, and positioning time. Although many studies have not proven automatic devices to be more effective than manual compressions, ongoing advancements in technology and clinical research are continuously improving their potential. The article also discusses the technical features, effectiveness, positioning speed, and versatility of various CPR devices, considering their use in specific situations like patient transportation and during percutaneous coronary interventions.
SpecialIssue Article
Advances in MechanicalEngineering
2018, Vol. 10(1) 1–14
Ó The Author(s) 2018
DOI: 10.1177/1687814017748749
journals.sagepub.com/home/ade
Automatic and manual devices for
cardiopulmonary resuscitation: A
review
Carlo Remino1 , Manuela Baronio2, Nicola Pellegrini1 ,
Francesco Aggogeri1 and Riccardo Adamini1
Abstract
Rate of survivalwithout any neurologicalconsequence after cardiac arrest is driven not only by early recognition b
also by high-quality cardiopulmonary resuscitation.Because the effectiveness of the manualcardiopulmonary resusci-
tation is usually impaired by rescuers’fatigue,devices have been devised to improve it by appliances or ergonomi
solutions.However,some devices are thought to replace the manualresuscitation altogether,either mimicking its
action or generating hemodynamic effects with working principles which are entirely different.This article reviews
such devices,both manualand automatic.They are mainly classified by actuation method,applied force,working
space,and positioning time.Most ofthe trials and meta-analyses have not demonstrated that chest compressio
given with automatic devices are more effective than those given manually.However,advances in clinicalresearch
and technology,with an improved understanding ofthe organizationalimplications oftheir use,are constantly
improving the effectiveness of such devices.
Keywords
Cardiac arrest, cardiopulmonary resuscitation, automatic devices, interposed abdominal compression.
Date received: 27 July 2017; accepted: 13 November 2017
Handling Editor: Liyuan Sheng
Introduction
Cardiac arrest is a sudden diminution of heart activity
which impairs the effective pumping ofblood. More
than 420,000 people suffer an out-of-hospitalcardiac
arrest in the United States every year, and the
American Heart Association (AHA) estimates that this
numberwill increase in the nextyears.1 In the last
50 years, research has steadily improved cardiopulmon-
ary resuscitation (CPR),but there is stillmuch to do,
since survival rates remain low. The effectiveness of the
CPR depends on many factors,where the promptness
and the quality of the resuscitation procedure are the
mostimportant.All the optimalparametersof such
procedure,like execution timing,chestcompression
rate, and chest compression frequency are stated in the
AHA guidelines.2
Automatic CPR devices have been devised to solve
some problems that reduce the effectiveness of the man-
ual CPR. The first of these problems,probably the
most important,is the fatigue that rescuers experience
during CPR. In fact, the human chesthas a viscous
damping that dissipates part of the energy applied dur-
ing the massage, so that energy has to be continuously
supplied by the rescuer.3–5Over time, fatigue sets in and
1Department of Mechanical and Industrial Engineering, University of
Brescia, Brescia, Italy
2Fondazione Poliambulanza Hospital, Brescia, Italy
Corresponding author:
Carlo Remino, Department of Mechanical and Industrial Engineering,
University of Brescia, Via Branze 38, 25123 Brescia, Italy.
Email: carlo.remino@unibs.it
Creative Commons CC BY: This article is distributed under the terms of the Creative Commons Attribution 4.0 License
(http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work w
further permission provided the originalwork is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us
open-access-at-sage).
Advances in MechanicalEngineering
2018, Vol. 10(1) 1–14
Ó The Author(s) 2018
DOI: 10.1177/1687814017748749
journals.sagepub.com/home/ade
Automatic and manual devices for
cardiopulmonary resuscitation: A
review
Carlo Remino1 , Manuela Baronio2, Nicola Pellegrini1 ,
Francesco Aggogeri1 and Riccardo Adamini1
Abstract
Rate of survivalwithout any neurologicalconsequence after cardiac arrest is driven not only by early recognition b
also by high-quality cardiopulmonary resuscitation.Because the effectiveness of the manualcardiopulmonary resusci-
tation is usually impaired by rescuers’fatigue,devices have been devised to improve it by appliances or ergonomi
solutions.However,some devices are thought to replace the manualresuscitation altogether,either mimicking its
action or generating hemodynamic effects with working principles which are entirely different.This article reviews
such devices,both manualand automatic.They are mainly classified by actuation method,applied force,working
space,and positioning time.Most ofthe trials and meta-analyses have not demonstrated that chest compressio
given with automatic devices are more effective than those given manually.However,advances in clinicalresearch
and technology,with an improved understanding ofthe organizationalimplications oftheir use,are constantly
improving the effectiveness of such devices.
Keywords
Cardiac arrest, cardiopulmonary resuscitation, automatic devices, interposed abdominal compression.
Date received: 27 July 2017; accepted: 13 November 2017
Handling Editor: Liyuan Sheng
Introduction
Cardiac arrest is a sudden diminution of heart activity
which impairs the effective pumping ofblood. More
than 420,000 people suffer an out-of-hospitalcardiac
arrest in the United States every year, and the
American Heart Association (AHA) estimates that this
numberwill increase in the nextyears.1 In the last
50 years, research has steadily improved cardiopulmon-
ary resuscitation (CPR),but there is stillmuch to do,
since survival rates remain low. The effectiveness of the
CPR depends on many factors,where the promptness
and the quality of the resuscitation procedure are the
mostimportant.All the optimalparametersof such
procedure,like execution timing,chestcompression
rate, and chest compression frequency are stated in the
AHA guidelines.2
Automatic CPR devices have been devised to solve
some problems that reduce the effectiveness of the man-
ual CPR. The first of these problems,probably the
most important,is the fatigue that rescuers experience
during CPR. In fact, the human chesthas a viscous
damping that dissipates part of the energy applied dur-
ing the massage, so that energy has to be continuously
supplied by the rescuer.3–5Over time, fatigue sets in and
1Department of Mechanical and Industrial Engineering, University of
Brescia, Brescia, Italy
2Fondazione Poliambulanza Hospital, Brescia, Italy
Corresponding author:
Carlo Remino, Department of Mechanical and Industrial Engineering,
University of Brescia, Via Branze 38, 25123 Brescia, Italy.
Email: carlo.remino@unibs.it
Creative Commons CC BY: This article is distributed under the terms of the Creative Commons Attribution 4.0 License
(http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work w
further permission provided the originalwork is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us
open-access-at-sage).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
lowers the effectiveness ofthe massage.6–9 Therefore,
rescuersneed to change frequently,interrupting the
massageand consequently reducing stillfurtherthe
effectivenessof the resuscitation.10,11 On the other
hand, automatic devices do not suffer fatigue at all and
can also continue to massage during defibrillation or
other complementary operations.12 In addition, if a
rigid stretcher is used during the transportation of the
patient from the scene to the ambulance,the massage
can continue uninterrupted all the time.
However,because no evidence has been shown that
automatic devices improve the outcome ofCPR, the
AHA does not recommendtheir routine use.
Nevertheless, such devices are a viable alternative when
high-quality manualcompressionsare challenging or
dangerousby the provider.2 This article reviewsthe
devices for CPR, which can be just adjuncts to manual
CPR, for example providing prompts to the rescuer or
improving theeffectof the chestcompressions,or
devices aimed at replacing completely the manual CPR.
After a brief description of each device,their technical
features will be summarized and compared. Then, their
effectiveness will be evaluated confronting the results of
meta-analyses,trials,and smallerstudies,considering
not only clinicaloutcomes but also the ability to per-
form high-quality CPR in specific situations,such as
during patienttransportation,percutaneouscoronary
intervention,or diagnostic imaging.Finally,more spe-
cific issues will be addressed in the section ‘‘Discussion.’’
Most of these issues are technical, but we will consider
features and properties thatinfluence the three main
requirements that,in our opinion, an automatic device
for CPR should have:effectiveness,fast positioning,
and versatility.
CPR devices
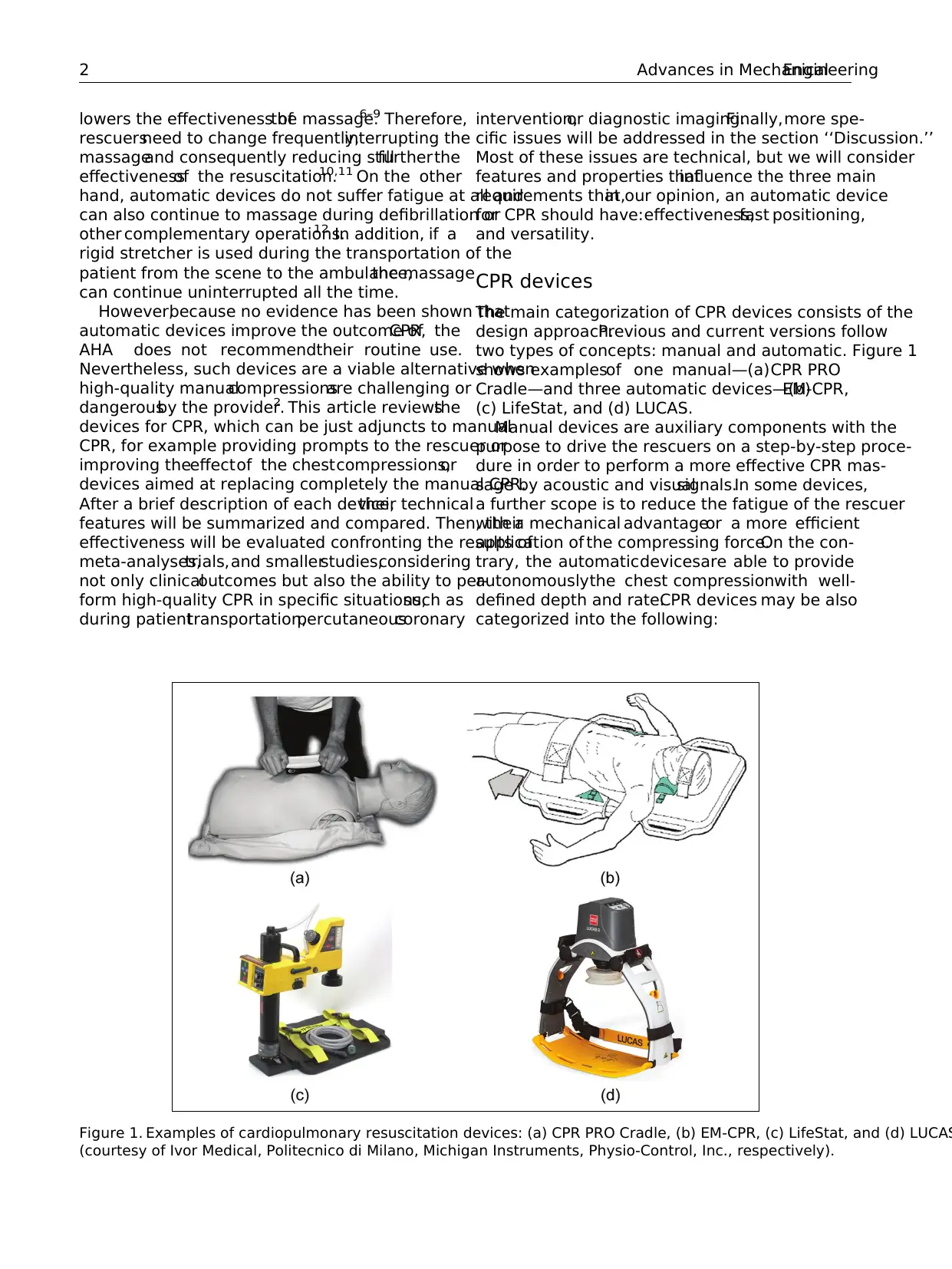
The main categorization of CPR devices consists of the
design approach.Previous and current versions follow
two types of concepts: manual and automatic. Figure 1
shows examplesof one manual—(a)CPR PRO
Cradle—and three automatic devices—(b)EM-CPR,
(c) LifeStat, and (d) LUCAS.
Manual devices are auxiliary components with the
purpose to drive the rescuers on a step-by-step proce-
dure in order to perform a more effective CPR mas-
sage by acoustic and visualsignals.In some devices,
a further scope is to reduce the fatigue of the rescuer
with a mechanical advantageor a more efficient
application of the compressing force.On the con-
trary, the automaticdevicesare able to provide
autonomouslythe chest compressionwith well-
defined depth and rate.CPR devices may be also
categorized into the following:
Figure 1. Examples of cardiopulmonary resuscitation devices: (a) CPR PRO Cradle, (b) EM-CPR, (c) LifeStat, and (d) LUCAS
(courtesy of Ivor Medical, Politecnico di Milano, Michigan Instruments, Physio-Control, Inc., respectively).
2 Advances in MechanicalEngineering
rescuersneed to change frequently,interrupting the
massageand consequently reducing stillfurtherthe
effectivenessof the resuscitation.10,11 On the other
hand, automatic devices do not suffer fatigue at all and
can also continue to massage during defibrillation or
other complementary operations.12 In addition, if a
rigid stretcher is used during the transportation of the
patient from the scene to the ambulance,the massage
can continue uninterrupted all the time.
However,because no evidence has been shown that
automatic devices improve the outcome ofCPR, the
AHA does not recommendtheir routine use.
Nevertheless, such devices are a viable alternative when
high-quality manualcompressionsare challenging or
dangerousby the provider.2 This article reviewsthe
devices for CPR, which can be just adjuncts to manual
CPR, for example providing prompts to the rescuer or
improving theeffectof the chestcompressions,or
devices aimed at replacing completely the manual CPR.
After a brief description of each device,their technical
features will be summarized and compared. Then, their
effectiveness will be evaluated confronting the results of
meta-analyses,trials,and smallerstudies,considering
not only clinicaloutcomes but also the ability to per-
form high-quality CPR in specific situations,such as
during patienttransportation,percutaneouscoronary
intervention,or diagnostic imaging.Finally,more spe-
cific issues will be addressed in the section ‘‘Discussion.’’
Most of these issues are technical, but we will consider
features and properties thatinfluence the three main
requirements that,in our opinion, an automatic device
for CPR should have:effectiveness,fast positioning,
and versatility.
CPR devices
The main categorization of CPR devices consists of the
design approach.Previous and current versions follow
two types of concepts: manual and automatic. Figure 1
shows examplesof one manual—(a)CPR PRO
Cradle—and three automatic devices—(b)EM-CPR,
(c) LifeStat, and (d) LUCAS.
Manual devices are auxiliary components with the
purpose to drive the rescuers on a step-by-step proce-
dure in order to perform a more effective CPR mas-
sage by acoustic and visualsignals.In some devices,
a further scope is to reduce the fatigue of the rescuer
with a mechanical advantageor a more efficient
application of the compressing force.On the con-
trary, the automaticdevicesare able to provide
autonomouslythe chest compressionwith well-
defined depth and rate.CPR devices may be also
categorized into the following:
Figure 1. Examples of cardiopulmonary resuscitation devices: (a) CPR PRO Cradle, (b) EM-CPR, (c) LifeStat, and (d) LUCAS
(courtesy of Ivor Medical, Politecnico di Milano, Michigan Instruments, Physio-Control, Inc., respectively).
2 Advances in MechanicalEngineering
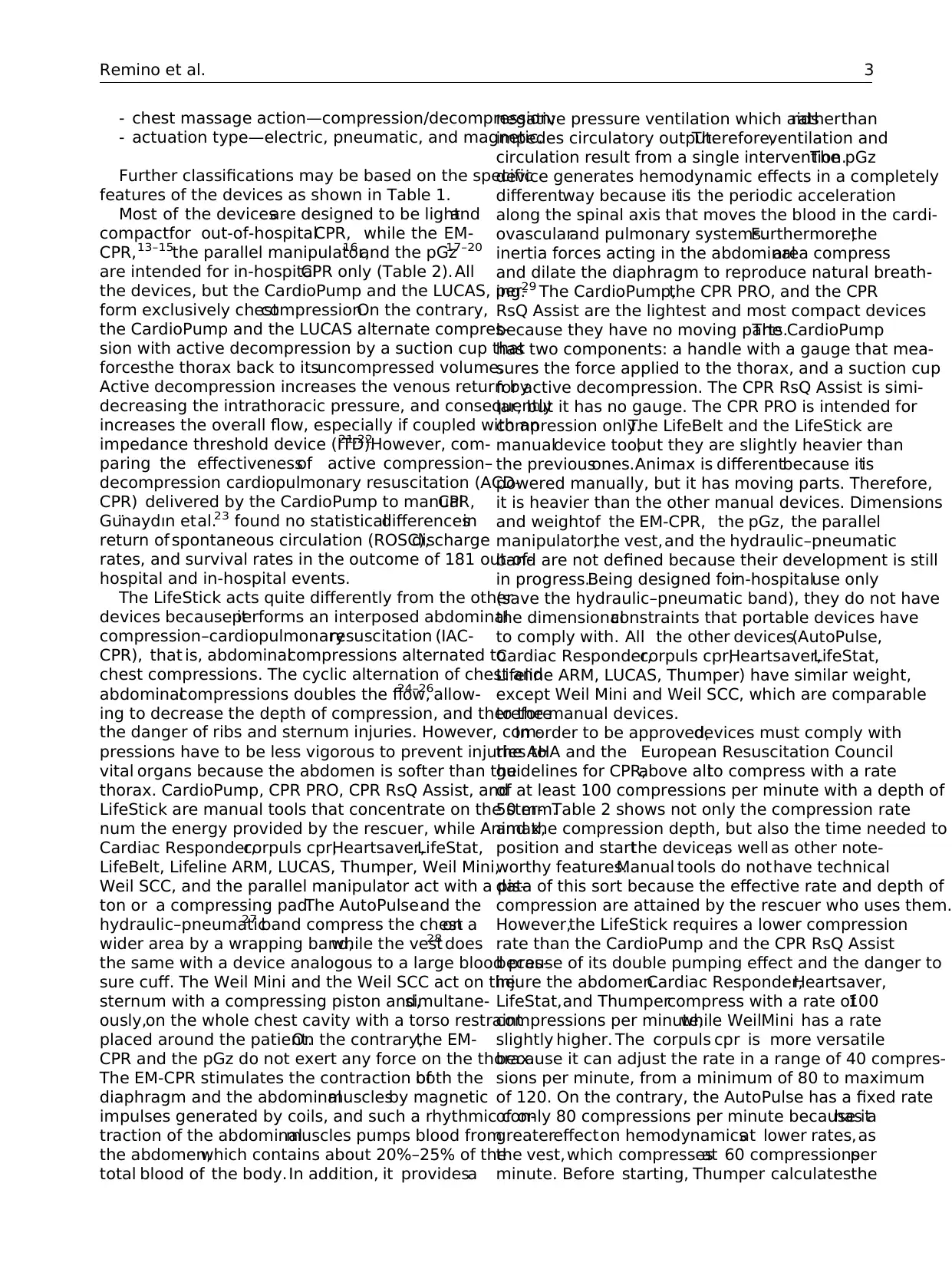
- chest massage action—compression/decompression;
- actuation type—electric, pneumatic, and magnetic.
Further classifications may be based on the specific
features of the devices as shown in Table 1.
Most of the devicesare designed to be lightand
compactfor out-of-hospitalCPR, while the EM-
CPR, 13–15the parallel manipulator,16 and the pGz17–20
are intended for in-hospitalCPR only (Table 2). All
the devices, but the CardioPump and the LUCAS, per-
form exclusively chestcompression.On the contrary,
the CardioPump and the LUCAS alternate compres-
sion with active decompression by a suction cup that
forcesthe thorax back to itsuncompressed volume.
Active decompression increases the venous return by
decreasing the intrathoracic pressure, and consequently
increases the overall flow, especially if coupled with an
impedance threshold device (ITD).21,22However, com-
paring the effectivenessof active compression–
decompression cardiopulmonary resuscitation (ACD-
CPR) delivered by the CardioPump to manualCPR,
Gu¨naydın etal.23 found no statisticaldifferencesin
return of spontaneous circulation (ROSC),discharge
rates, and survival rates in the outcome of 181 out-of-
hospital and in-hospital events.
The LifeStick acts quite differently from the other
devices because itperforms an interposed abdominal
compression–cardiopulmonaryresuscitation (IAC-
CPR), that is, abdominalcompressions alternated to
chest compressions. The cyclic alternation of chest and
abdominalcompressions doubles the flow,24–26allow-
ing to decrease the depth of compression, and therefore
the danger of ribs and sternum injuries. However, com-
pressions have to be less vigorous to prevent injuries to
vital organs because the abdomen is softer than the
thorax. CardioPump, CPR PRO, CPR RsQ Assist, and
LifeStick are manual tools that concentrate on the ster-
num the energy provided by the rescuer, while Animax,
Cardiac Responder,corpuls cpr,Heartsaver,LifeStat,
LifeBelt, Lifeline ARM, LUCAS, Thumper, Weil Mini,
Weil SCC, and the parallel manipulator act with a pis-
ton or a compressing pad.The AutoPulseand the
hydraulic–pneumatic27 band compress the cheston a
wider area by a wrapping band,while the vest28 does
the same with a device analogous to a large blood pres-
sure cuff. The Weil Mini and the Weil SCC act on the
sternum with a compressing piston and,simultane-
ously,on the whole chest cavity with a torso restraint
placed around the patient.On the contrary,the EM-
CPR and the pGz do not exert any force on the thorax.
The EM-CPR stimulates the contraction ofboth the
diaphragm and the abdominalmusclesby magnetic
impulses generated by coils, and such a rhythmic con-
traction of the abdominalmuscles pumps blood from
the abdomen,which contains about 20%–25% of the
total blood of the body.In addition, it providesa
negative pressure ventilation which aidsratherthan
impedes circulatory output.Therefore,ventilation and
circulation result from a single intervention.The pGz
device generates hemodynamic effects in a completely
differentway because itis the periodic acceleration
along the spinal axis that moves the blood in the cardi-
ovascularand pulmonary systems.Furthermore,the
inertia forces acting in the abdominalarea compress
and dilate the diaphragm to reproduce natural breath-
ing.29 The CardioPump,the CPR PRO, and the CPR
RsQ Assist are the lightest and most compact devices
because they have no moving parts.The CardioPump
has two components: a handle with a gauge that mea-
sures the force applied to the thorax, and a suction cup
for active decompression. The CPR RsQ Assist is simi-
lar, but it has no gauge. The CPR PRO is intended for
compression only.The LifeBelt and the LifeStick are
manualdevice too,but they are slightly heavier than
the previousones.Animax is differentbecause itis
powered manually, but it has moving parts. Therefore,
it is heavier than the other manual devices. Dimensions
and weightof the EM-CPR, the pGz, the parallel
manipulator,the vest,and the hydraulic–pneumatic
band are not defined because their development is still
in progress.Being designed forin-hospitaluse only
(save the hydraulic–pneumatic band), they do not have
the dimensionalconstraints that portable devices have
to comply with. All the other devices(AutoPulse,
Cardiac Responder,corpuls cpr,Heartsaver,LifeStat,
Lifeline ARM, LUCAS, Thumper) have similar weight,
except Weil Mini and Weil SCC, which are comparable
to the manual devices.
In order to be approved,devices must comply with
the AHA and the European Resuscitation Council
guidelines for CPR,above allto compress with a rate
of at least 100 compressions per minute with a depth of
50 mm.Table 2 shows not only the compression rate
and the compression depth, but also the time needed to
position and startthe device,as well as other note-
worthy features.Manual tools do nothave technical
data of this sort because the effective rate and depth of
compression are attained by the rescuer who uses them.
However,the LifeStick requires a lower compression
rate than the CardioPump and the CPR RsQ Assist
because of its double pumping effect and the danger to
injure the abdomen.Cardiac Responder,Heartsaver,
LifeStat,and Thumpercompress with a rate of100
compressions per minute,while WeilMini has a rate
slightly higher. The corpuls cpr is more versatile
because it can adjust the rate in a range of 40 compres-
sions per minute, from a minimum of 80 to maximum
of 120. On the contrary, the AutoPulse has a fixed rate
of only 80 compressions per minute because ithas a
greatereffecton hemodynamicsat lower rates,as
the vest,which compressesat 60 compressionsper
minute. Before starting, Thumper calculatesthe
Remino et al. 3
- actuation type—electric, pneumatic, and magnetic.
Further classifications may be based on the specific
features of the devices as shown in Table 1.
Most of the devicesare designed to be lightand
compactfor out-of-hospitalCPR, while the EM-
CPR, 13–15the parallel manipulator,16 and the pGz17–20
are intended for in-hospitalCPR only (Table 2). All
the devices, but the CardioPump and the LUCAS, per-
form exclusively chestcompression.On the contrary,
the CardioPump and the LUCAS alternate compres-
sion with active decompression by a suction cup that
forcesthe thorax back to itsuncompressed volume.
Active decompression increases the venous return by
decreasing the intrathoracic pressure, and consequently
increases the overall flow, especially if coupled with an
impedance threshold device (ITD).21,22However, com-
paring the effectivenessof active compression–
decompression cardiopulmonary resuscitation (ACD-
CPR) delivered by the CardioPump to manualCPR,
Gu¨naydın etal.23 found no statisticaldifferencesin
return of spontaneous circulation (ROSC),discharge
rates, and survival rates in the outcome of 181 out-of-
hospital and in-hospital events.
The LifeStick acts quite differently from the other
devices because itperforms an interposed abdominal
compression–cardiopulmonaryresuscitation (IAC-
CPR), that is, abdominalcompressions alternated to
chest compressions. The cyclic alternation of chest and
abdominalcompressions doubles the flow,24–26allow-
ing to decrease the depth of compression, and therefore
the danger of ribs and sternum injuries. However, com-
pressions have to be less vigorous to prevent injuries to
vital organs because the abdomen is softer than the
thorax. CardioPump, CPR PRO, CPR RsQ Assist, and
LifeStick are manual tools that concentrate on the ster-
num the energy provided by the rescuer, while Animax,
Cardiac Responder,corpuls cpr,Heartsaver,LifeStat,
LifeBelt, Lifeline ARM, LUCAS, Thumper, Weil Mini,
Weil SCC, and the parallel manipulator act with a pis-
ton or a compressing pad.The AutoPulseand the
hydraulic–pneumatic27 band compress the cheston a
wider area by a wrapping band,while the vest28 does
the same with a device analogous to a large blood pres-
sure cuff. The Weil Mini and the Weil SCC act on the
sternum with a compressing piston and,simultane-
ously,on the whole chest cavity with a torso restraint
placed around the patient.On the contrary,the EM-
CPR and the pGz do not exert any force on the thorax.
The EM-CPR stimulates the contraction ofboth the
diaphragm and the abdominalmusclesby magnetic
impulses generated by coils, and such a rhythmic con-
traction of the abdominalmuscles pumps blood from
the abdomen,which contains about 20%–25% of the
total blood of the body.In addition, it providesa
negative pressure ventilation which aidsratherthan
impedes circulatory output.Therefore,ventilation and
circulation result from a single intervention.The pGz
device generates hemodynamic effects in a completely
differentway because itis the periodic acceleration
along the spinal axis that moves the blood in the cardi-
ovascularand pulmonary systems.Furthermore,the
inertia forces acting in the abdominalarea compress
and dilate the diaphragm to reproduce natural breath-
ing.29 The CardioPump,the CPR PRO, and the CPR
RsQ Assist are the lightest and most compact devices
because they have no moving parts.The CardioPump
has two components: a handle with a gauge that mea-
sures the force applied to the thorax, and a suction cup
for active decompression. The CPR RsQ Assist is simi-
lar, but it has no gauge. The CPR PRO is intended for
compression only.The LifeBelt and the LifeStick are
manualdevice too,but they are slightly heavier than
the previousones.Animax is differentbecause itis
powered manually, but it has moving parts. Therefore,
it is heavier than the other manual devices. Dimensions
and weightof the EM-CPR, the pGz, the parallel
manipulator,the vest,and the hydraulic–pneumatic
band are not defined because their development is still
in progress.Being designed forin-hospitaluse only
(save the hydraulic–pneumatic band), they do not have
the dimensionalconstraints that portable devices have
to comply with. All the other devices(AutoPulse,
Cardiac Responder,corpuls cpr,Heartsaver,LifeStat,
Lifeline ARM, LUCAS, Thumper) have similar weight,
except Weil Mini and Weil SCC, which are comparable
to the manual devices.
In order to be approved,devices must comply with
the AHA and the European Resuscitation Council
guidelines for CPR,above allto compress with a rate
of at least 100 compressions per minute with a depth of
50 mm.Table 2 shows not only the compression rate
and the compression depth, but also the time needed to
position and startthe device,as well as other note-
worthy features.Manual tools do nothave technical
data of this sort because the effective rate and depth of
compression are attained by the rescuer who uses them.
However,the LifeStick requires a lower compression
rate than the CardioPump and the CPR RsQ Assist
because of its double pumping effect and the danger to
injure the abdomen.Cardiac Responder,Heartsaver,
LifeStat,and Thumpercompress with a rate of100
compressions per minute,while WeilMini has a rate
slightly higher. The corpuls cpr is more versatile
because it can adjust the rate in a range of 40 compres-
sions per minute, from a minimum of 80 to maximum
of 120. On the contrary, the AutoPulse has a fixed rate
of only 80 compressions per minute because ithas a
greatereffecton hemodynamicsat lower rates,as
the vest,which compressesat 60 compressionsper
minute. Before starting, Thumper calculatesthe
Remino et al. 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
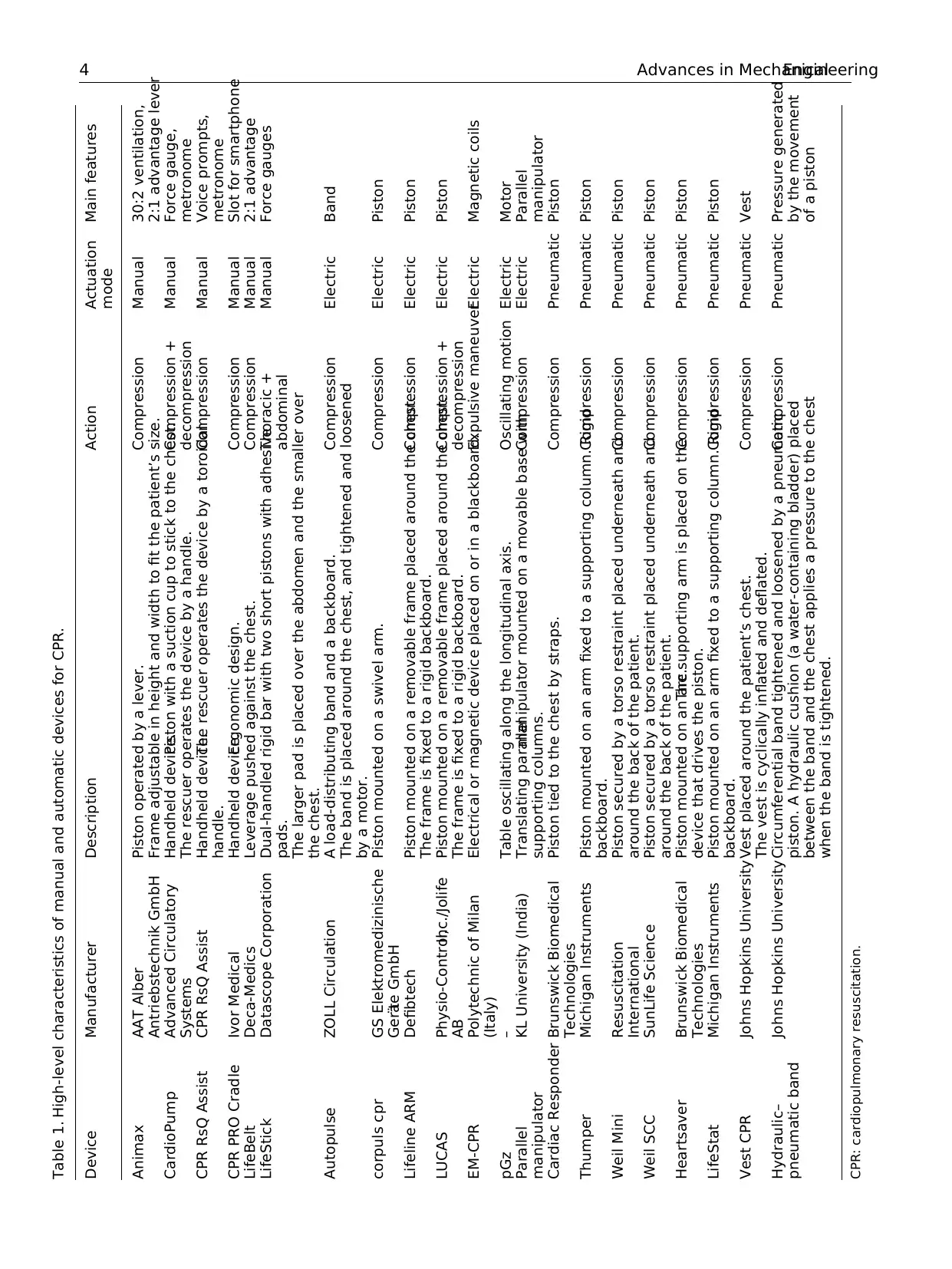
Table 1. High-level characteristics of manual and automatic devices for CPR.
Device Manufacturer Description Action Actuation
mode
Main features
Animax AAT Alber
Antriebstechnik GmbH
Piston operated by a lever.
Frame adjustable in height and width to fit the patient’s size.
Compression Manual 30:2 ventilation,
2:1 advantage lever
CardioPump Advanced Circulatory
Systems
Handheld device.Piston with a suction cup to stick to the chest.
The rescuer operates the device by a handle.
Compression +
decompression
Manual Force gauge,
metronome
CPR RsQ Assist CPR RsQ Assist Handheld device.The rescuer operates the device by a toroidal
handle.
Compression Manual Voice prompts,
metronome
CPR PRO Cradle Ivor Medical Handheld device.Ergonomic design. Compression Manual Slot for smartphone
LifeBelt Deca-Medics Leverage pushed against the chest. Compression Manual 2:1 advantage
LifeStick Datascope Corporation Dual-handled rigid bar with two short pistons with adhesive
pads.
The larger pad is placed over the abdomen and the smaller over
the chest.
Thoracic +
abdominal
Manual Force gauges
Autopulse ZOLL Circulation A load-distributing band and a backboard.
The band is placed around the chest, and tightened and loosened
by a motor.
Compression Electric Band
corpuls cpr GS Elektromedizinische
Gera¨te GmbH
Piston mounted on a swivel arm. Compression Electric Piston
Lifeline ARM Defibtech Piston mounted on a removable frame placed around the chest.
The frame is fixed to a rigid backboard.
Compression Electric Piston
LUCAS Physio-Control,Inc./Jolife
AB
Piston mounted on a removable frame placed around the chest.
The frame is fixed to a rigid backboard.
Compression +
decompression
Electric Piston
EM-CPR Polytechnic of Milan
(Italy)
Electrical or magnetic device placed on or in a blackboard.Expulsive maneuverElectric Magnetic coils
pGz – Table oscillating along the longitudinal axis. Oscillating motion Electric Motor
Parallel
manipulator
KL University (India) Translating parallelmanipulator mounted on a movable base with
supporting columns.
Compression Electric Parallel
manipulator
Cardiac Responder Brunswick Biomedical
Technologies
Piston tied to the chest by straps. Compression Pneumatic Piston
Thumper Michigan Instruments Piston mounted on an arm fixed to a supporting column. Rigid
backboard.
Compression Pneumatic Piston
Weil Mini Resuscitation
International
Piston secured by a torso restraint placed underneath and
around the back of the patient.
Compression Pneumatic Piston
Weil SCC SunLife Science Piston secured by a torso restraint placed underneath and
around the back of the patient.
Compression Pneumatic Piston
Heartsaver Brunswick Biomedical
Technologies
Piston mounted on an arc.The supporting arm is placed on the
device that drives the piston.
Compression Pneumatic Piston
LifeStat Michigan Instruments Piston mounted on an arm fixed to a supporting column. Rigid
backboard.
Compression Pneumatic Piston
Vest CPR Johns Hopkins UniversityVest placed around the patient’s chest.
The vest is cyclically inflated and deflated.
Compression Pneumatic Vest
Hydraulic–
pneumatic band
Johns Hopkins UniversityCircumferential band tightened and loosened by a pneumatic
piston. A hydraulic cushion (a water-containing bladder) placed
between the band and the chest applies a pressure to the chest
when the band is tightened.
Compression Pneumatic Pressure generated
by the movement
of a piston
CPR: cardiopulmonary resuscitation.
4 Advances in MechanicalEngineering
Device Manufacturer Description Action Actuation
mode
Main features
Animax AAT Alber
Antriebstechnik GmbH
Piston operated by a lever.
Frame adjustable in height and width to fit the patient’s size.
Compression Manual 30:2 ventilation,
2:1 advantage lever
CardioPump Advanced Circulatory
Systems
Handheld device.Piston with a suction cup to stick to the chest.
The rescuer operates the device by a handle.
Compression +
decompression
Manual Force gauge,
metronome
CPR RsQ Assist CPR RsQ Assist Handheld device.The rescuer operates the device by a toroidal
handle.
Compression Manual Voice prompts,
metronome
CPR PRO Cradle Ivor Medical Handheld device.Ergonomic design. Compression Manual Slot for smartphone
LifeBelt Deca-Medics Leverage pushed against the chest. Compression Manual 2:1 advantage
LifeStick Datascope Corporation Dual-handled rigid bar with two short pistons with adhesive
pads.
The larger pad is placed over the abdomen and the smaller over
the chest.
Thoracic +
abdominal
Manual Force gauges
Autopulse ZOLL Circulation A load-distributing band and a backboard.
The band is placed around the chest, and tightened and loosened
by a motor.
Compression Electric Band
corpuls cpr GS Elektromedizinische
Gera¨te GmbH
Piston mounted on a swivel arm. Compression Electric Piston
Lifeline ARM Defibtech Piston mounted on a removable frame placed around the chest.
The frame is fixed to a rigid backboard.
Compression Electric Piston
LUCAS Physio-Control,Inc./Jolife
AB
Piston mounted on a removable frame placed around the chest.
The frame is fixed to a rigid backboard.
Compression +
decompression
Electric Piston
EM-CPR Polytechnic of Milan
(Italy)
Electrical or magnetic device placed on or in a blackboard.Expulsive maneuverElectric Magnetic coils
pGz – Table oscillating along the longitudinal axis. Oscillating motion Electric Motor
Parallel
manipulator
KL University (India) Translating parallelmanipulator mounted on a movable base with
supporting columns.
Compression Electric Parallel
manipulator
Cardiac Responder Brunswick Biomedical
Technologies
Piston tied to the chest by straps. Compression Pneumatic Piston
Thumper Michigan Instruments Piston mounted on an arm fixed to a supporting column. Rigid
backboard.
Compression Pneumatic Piston
Weil Mini Resuscitation
International
Piston secured by a torso restraint placed underneath and
around the back of the patient.
Compression Pneumatic Piston
Weil SCC SunLife Science Piston secured by a torso restraint placed underneath and
around the back of the patient.
Compression Pneumatic Piston
Heartsaver Brunswick Biomedical
Technologies
Piston mounted on an arc.The supporting arm is placed on the
device that drives the piston.
Compression Pneumatic Piston
LifeStat Michigan Instruments Piston mounted on an arm fixed to a supporting column. Rigid
backboard.
Compression Pneumatic Piston
Vest CPR Johns Hopkins UniversityVest placed around the patient’s chest.
The vest is cyclically inflated and deflated.
Compression Pneumatic Vest
Hydraulic–
pneumatic band
Johns Hopkins UniversityCircumferential band tightened and loosened by a pneumatic
piston. A hydraulic cushion (a water-containing bladder) placed
between the band and the chest applies a pressure to the chest
when the band is tightened.
Compression Pneumatic Pressure generated
by the movement
of a piston
CPR: cardiopulmonary resuscitation.
4 Advances in MechanicalEngineering
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
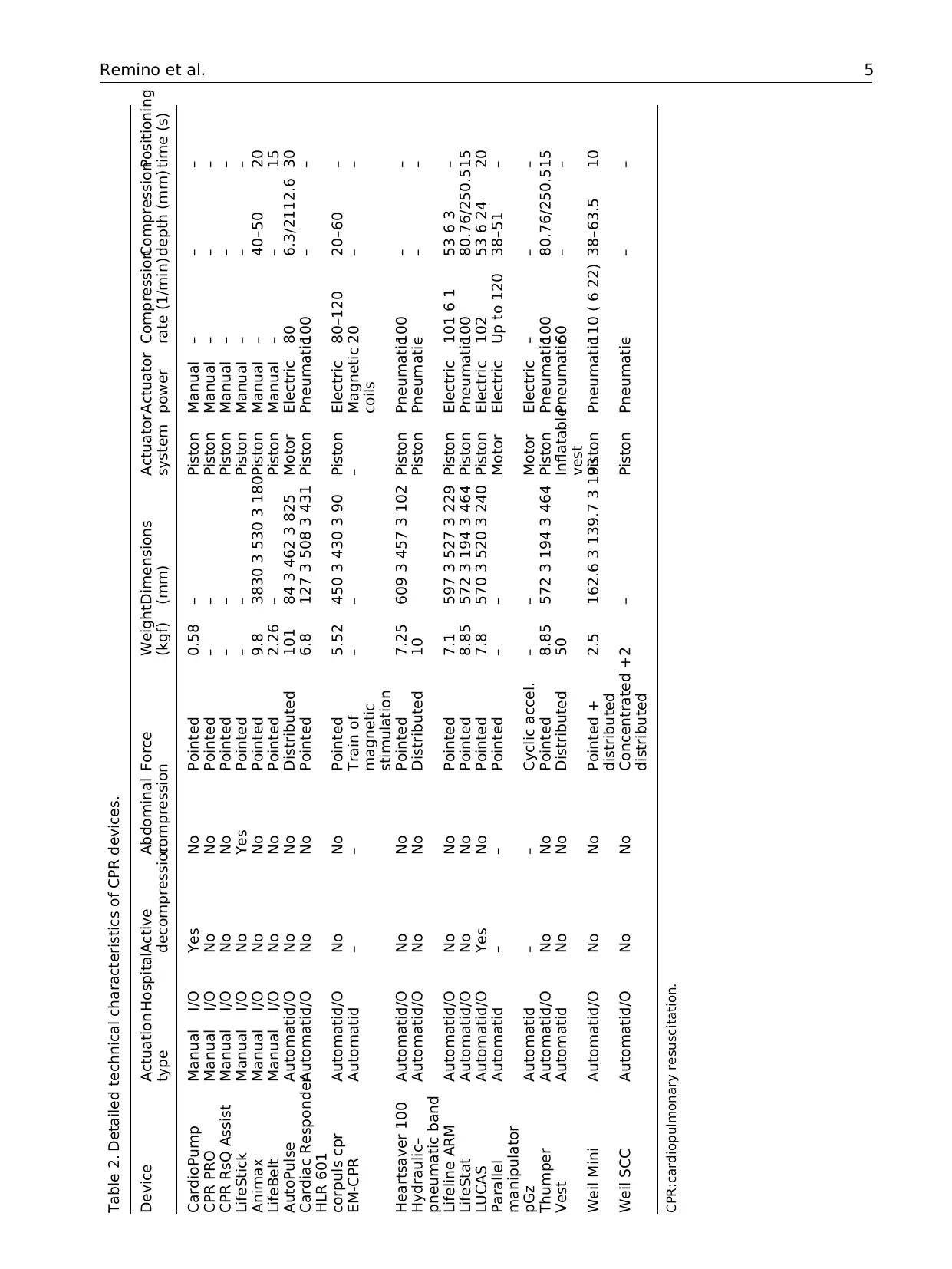
Table 2. Detailed technical characteristics of CPR devices.
Device Actuation
type
HospitalActive
decompression
Abdominal
compression
Force Weight
(kgf)
Dimensions
(mm)
Actuator
system
Actuator
power
Compression
rate (1/min)
Compression
depth (mm)
Positioning
time (s)
CardioPump Manual I/O Yes No Pointed 0.58 – Piston Manual – – –
CPR PRO Manual I/O No No Pointed – – Piston Manual – – –
CPR RsQ Assist Manual I/O No No Pointed – – Piston Manual – – –
LifeStick Manual I/O No Yes Pointed – – Piston Manual – – –
Animax Manual I/O No No Pointed 9.8 3830 3 530 3 180Piston Manual – 40–50 20
LifeBelt Manual I/O No No Pointed 2.26 – Piston Manual – – 15
AutoPulse AutomaticI/O No No Distributed 101 84 3 462 3 825 Motor Electric 80 6.3/2112.6 30
Cardiac Responder
HLR 601
AutomaticI/O No No Pointed 6.8 127 3 508 3 431 Piston Pneumatic100 – –
corpuls cpr AutomaticI/O No No Pointed 5.52 450 3 430 3 90 Piston Electric 80–120 20–60 –
EM-CPR AutomaticI – – Train of
magnetic
stimulation
– – – Magnetic
coils
20 – –
Heartsaver 100 AutomaticI/O No No Pointed 7.25 609 3 457 3 102 Piston Pneumatic100 – –
Hydraulic–
pneumatic band
AutomaticI/O No No Distributed 10 Piston Pneumatic– – –
Lifeline ARM AutomaticI/O No No Pointed 7.1 597 3 527 3 229 Piston Electric 101 6 1 53 6 3 –
LifeStat AutomaticI/O No No Pointed 8.85 572 3 194 3 464 Piston Pneumatic100 80.76/250.515
LUCAS AutomaticI/O Yes No Pointed 7.8 570 3 520 3 240 Piston Electric 102 53 6 24 20
Parallel
manipulator
AutomaticI – – Pointed – – Motor Electric Up to 120 38–51 –
pGz AutomaticI – – Cyclic accel. – – Motor Electric – – –
Thumper AutomaticI/O No No Pointed 8.85 572 3 194 3 464 Piston Pneumatic100 80.76/250.515
Vest AutomaticI No No Distributed 50 Inflatable
vest
Pneumatic60 – –
Weil Mini AutomaticI/O No No Pointed +
distributed
2.5 162.6 3 139.7 3 193Piston Pneumatic110 ( 6 22) 38–63.5 10
Weil SCC AutomaticI/O No No Concentrated +
distributed
2 – Piston Pneumatic– – –
CPR:cardiopulmonary resuscitation.
Remino et al. 5
Device Actuation
type
HospitalActive
decompression
Abdominal
compression
Force Weight
(kgf)
Dimensions
(mm)
Actuator
system
Actuator
power
Compression
rate (1/min)
Compression
depth (mm)
Positioning
time (s)
CardioPump Manual I/O Yes No Pointed 0.58 – Piston Manual – – –
CPR PRO Manual I/O No No Pointed – – Piston Manual – – –
CPR RsQ Assist Manual I/O No No Pointed – – Piston Manual – – –
LifeStick Manual I/O No Yes Pointed – – Piston Manual – – –
Animax Manual I/O No No Pointed 9.8 3830 3 530 3 180Piston Manual – 40–50 20
LifeBelt Manual I/O No No Pointed 2.26 – Piston Manual – – 15
AutoPulse AutomaticI/O No No Distributed 101 84 3 462 3 825 Motor Electric 80 6.3/2112.6 30
Cardiac Responder
HLR 601
AutomaticI/O No No Pointed 6.8 127 3 508 3 431 Piston Pneumatic100 – –
corpuls cpr AutomaticI/O No No Pointed 5.52 450 3 430 3 90 Piston Electric 80–120 20–60 –
EM-CPR AutomaticI – – Train of
magnetic
stimulation
– – – Magnetic
coils
20 – –
Heartsaver 100 AutomaticI/O No No Pointed 7.25 609 3 457 3 102 Piston Pneumatic100 – –
Hydraulic–
pneumatic band
AutomaticI/O No No Distributed 10 Piston Pneumatic– – –
Lifeline ARM AutomaticI/O No No Pointed 7.1 597 3 527 3 229 Piston Electric 101 6 1 53 6 3 –
LifeStat AutomaticI/O No No Pointed 8.85 572 3 194 3 464 Piston Pneumatic100 80.76/250.515
LUCAS AutomaticI/O Yes No Pointed 7.8 570 3 520 3 240 Piston Electric 102 53 6 24 20
Parallel
manipulator
AutomaticI – – Pointed – – Motor Electric Up to 120 38–51 –
pGz AutomaticI – – Cyclic accel. – – Motor Electric – – –
Thumper AutomaticI/O No No Pointed 8.85 572 3 194 3 464 Piston Pneumatic100 80.76/250.515
Vest AutomaticI No No Distributed 50 Inflatable
vest
Pneumatic60 – –
Weil Mini AutomaticI/O No No Pointed +
distributed
2.5 162.6 3 139.7 3 193Piston Pneumatic110 ( 6 22) 38–63.5 10
Weil SCC AutomaticI/O No No Concentrated +
distributed
2 – Piston Pneumatic– – –
CPR:cardiopulmonary resuscitation.
Remino et al. 5

anterior–posterior chestdiameter to deliver the right
sternum deflection.Similarly,the AutoPulseadjusts
automatically the band to the patient’s chest and, mea-
suring its circumference,calibratesthe compression
depth.Therefore,the depth at which the two devices
compress is relative to the dimension of the patient. All
the other devices compress with an absolute depth that
can often be adjusted to the dimension of the chest.
An essentialrequirementfor a successfuldevice is
the positioning time because CPR has to start as early
as possible to be effective: according to the manufactur-
ers, this time variesfrom a minimum of 10 s(Weil
Mini) to a maximum of 30 s (AutoPulse).
The effectiveness of the automatic devices
Devices are used when they are effective.Therefore,
there are two main questions to be answered about the
devices for CPR. The first is: are they at least as effec-
tive as the manual CPR? Whatever the answer, the next
question is: what are the factors that influence their per-
formance? Answering to the first question is necessary
to decide if such devices are useful, in general or in spe-
cific situations, while answering to the latter question is
a prerequisite condition to devise solutions that increase
their effectiveness,even ifthe performance is already
satisfactory. The following sections summarize the find-
ings of published studies that are usefulto answer the
two previous questions.
Is the automatic CPR effective?
Despiteautomaticdevicesdeliverhigh-quality chest
compressions,there is no consensuswhetherthey
improve the outcome of CPR.To compare AutoPulse
CPR with manual CPR in out-of-hospital cardiac
arrests, Hallstrom et al.30carried out a multicenter, ran-
domized trial, with 554 patients in the treatment group
and 517 patients in the controlgroup.They found no
difference in survival to 4 h after the emergency call, but
mechanicalCPR was associated with worseperfor-
mance than manualCPR both in survivalto hospital
discharge (5.8% vs 9.9%, p = 0.06 after adjustment for
covariates and clustering)and neurologicaloutcomes
(3.1% vs 7.5%, p = 0.006). The Circulation Improving
Resuscitation Care (CIRC)trial in the study ofWik
et al.31 was a randomized, unblended, controlled group
sequentialtrial, where AutoPulse CPR wasadmini-
strated to 2099 patientsand manualCPR to 2132
patients. Comparing mechanical CPR to manual CPR,
sustained ROSC was 28.6% versus 32.3%,24-h sur-
vivalwas 21.8% versus 25.0%,and hospitaldischarge
was 9.4% versus 11.0%. The LINC trial of Rubertsson
et al.32 was a multicenterrandomized clinicaltrial
aimed to determinewhether defibrillationduring
ongoing mechanicalcompressions would improve 4-h
survivalcompared with manualCPR. A total of 1300
patients received mechanicalchestcompressions with
LUCAS combined with defibrillation during ongoing
compressions,while 1289 patientsreceived manual
CPR according to the guidelines. There was no signifi-
cant difference in 4-h survival, and almost all the survi-
vors in both groups (99% mechanical vs 94% manual)
had good neurologicaloutcomesby 6 months(8.5%
mechanicalvs 7.6% manual).PARAMEDIC 33,34was
another large trial. It was a pragmatic,cluster-
randomized open-label trial, enrolling adults with out-
of-hospital cardiac arrest as the previous trials. A total
of 985 out of 1652 patients received mechanicalCPR
with LUCAS, while 2819 received manualCPR. The
findings showed that 30-day survival was similar in the
two groups: 6% LUCAS versus 7% manual.
All thesestudiesshowed thatchestcompression
delivered by automatic devices is as effective as that
delivered byhigh-qualitymanual CPR, but meta-
analyses and reviews did notfind sufficientevidence
that mechanical devices are so beneficial to recommend
their widespread use.Gateset al.35 reviewed rando-
mized controlled trialsand cluster-randomized trials
that compared mechanicalCPR (LUCAS and
AutoPulse)with manualCPR in out-of-hospitalcar-
diac arrests.They included in their meta-analysis five
trials which enrolled over 10,000 patients.30–33,36
Differences between the studies may have introduced
heterogeneity into the meta-analysis,but the randomi-
zation methods appeared to be adequate in all the stud-
ies. The resultsdid not show advantagesin using
mechanicaldevices for survival, both to discharge and
with good neurologicaloutcome.The same was true
for ROSC, but the effects ofthe two devices seemed
different.Westfallet al.37 conducted anothermeta-
analysis, but concentrating on ROSC. They selected 12
investigations(reported in 6 journalarticles30,36,38–41
and 6 abstracts)enrolling 6538 patients.The ROSC
events were 1824. Like the previous meta-analysis, they
found that LUCAS and AutoPulse had different effec-
tiveness: LUCAS had an effect similar to manual CPR,
while AutoPulse had significantlygreaterodds of
ROSC. Therefore,unlike the previous meta-analysis,
they concluded thatboth mechanicaldeviceshad,
together,higher odds ofROSC compared to manual
CPR. The updated review of Brooks et al.42 analyzed
six trials with a totalof 1166 patients.Despite such
studies lacked clinical homogeneity and overall quality,
the authors concluded that there was no evidence that
mechanicalCPR is more beneficialor harmfulthan
manual CPR. Bonnes et al.43 reached a similar conclu-
sion afterhaving analyzed 20 studies,5 randomized
controlled trials,and 15 studies with non-randomized
design,for a total of 21,363 patients.Couper et al.44
carried out a review and meta-analysis to ascertain the
effectivenessof automated devicesduring in-hospital
6 Advances in MechanicalEngineering
sternum deflection.Similarly,the AutoPulseadjusts
automatically the band to the patient’s chest and, mea-
suring its circumference,calibratesthe compression
depth.Therefore,the depth at which the two devices
compress is relative to the dimension of the patient. All
the other devices compress with an absolute depth that
can often be adjusted to the dimension of the chest.
An essentialrequirementfor a successfuldevice is
the positioning time because CPR has to start as early
as possible to be effective: according to the manufactur-
ers, this time variesfrom a minimum of 10 s(Weil
Mini) to a maximum of 30 s (AutoPulse).
The effectiveness of the automatic devices
Devices are used when they are effective.Therefore,
there are two main questions to be answered about the
devices for CPR. The first is: are they at least as effec-
tive as the manual CPR? Whatever the answer, the next
question is: what are the factors that influence their per-
formance? Answering to the first question is necessary
to decide if such devices are useful, in general or in spe-
cific situations, while answering to the latter question is
a prerequisite condition to devise solutions that increase
their effectiveness,even ifthe performance is already
satisfactory. The following sections summarize the find-
ings of published studies that are usefulto answer the
two previous questions.
Is the automatic CPR effective?
Despiteautomaticdevicesdeliverhigh-quality chest
compressions,there is no consensuswhetherthey
improve the outcome of CPR.To compare AutoPulse
CPR with manual CPR in out-of-hospital cardiac
arrests, Hallstrom et al.30carried out a multicenter, ran-
domized trial, with 554 patients in the treatment group
and 517 patients in the controlgroup.They found no
difference in survival to 4 h after the emergency call, but
mechanicalCPR was associated with worseperfor-
mance than manualCPR both in survivalto hospital
discharge (5.8% vs 9.9%, p = 0.06 after adjustment for
covariates and clustering)and neurologicaloutcomes
(3.1% vs 7.5%, p = 0.006). The Circulation Improving
Resuscitation Care (CIRC)trial in the study ofWik
et al.31 was a randomized, unblended, controlled group
sequentialtrial, where AutoPulse CPR wasadmini-
strated to 2099 patientsand manualCPR to 2132
patients. Comparing mechanical CPR to manual CPR,
sustained ROSC was 28.6% versus 32.3%,24-h sur-
vivalwas 21.8% versus 25.0%,and hospitaldischarge
was 9.4% versus 11.0%. The LINC trial of Rubertsson
et al.32 was a multicenterrandomized clinicaltrial
aimed to determinewhether defibrillationduring
ongoing mechanicalcompressions would improve 4-h
survivalcompared with manualCPR. A total of 1300
patients received mechanicalchestcompressions with
LUCAS combined with defibrillation during ongoing
compressions,while 1289 patientsreceived manual
CPR according to the guidelines. There was no signifi-
cant difference in 4-h survival, and almost all the survi-
vors in both groups (99% mechanical vs 94% manual)
had good neurologicaloutcomesby 6 months(8.5%
mechanicalvs 7.6% manual).PARAMEDIC 33,34was
another large trial. It was a pragmatic,cluster-
randomized open-label trial, enrolling adults with out-
of-hospital cardiac arrest as the previous trials. A total
of 985 out of 1652 patients received mechanicalCPR
with LUCAS, while 2819 received manualCPR. The
findings showed that 30-day survival was similar in the
two groups: 6% LUCAS versus 7% manual.
All thesestudiesshowed thatchestcompression
delivered by automatic devices is as effective as that
delivered byhigh-qualitymanual CPR, but meta-
analyses and reviews did notfind sufficientevidence
that mechanical devices are so beneficial to recommend
their widespread use.Gateset al.35 reviewed rando-
mized controlled trialsand cluster-randomized trials
that compared mechanicalCPR (LUCAS and
AutoPulse)with manualCPR in out-of-hospitalcar-
diac arrests.They included in their meta-analysis five
trials which enrolled over 10,000 patients.30–33,36
Differences between the studies may have introduced
heterogeneity into the meta-analysis,but the randomi-
zation methods appeared to be adequate in all the stud-
ies. The resultsdid not show advantagesin using
mechanicaldevices for survival, both to discharge and
with good neurologicaloutcome.The same was true
for ROSC, but the effects ofthe two devices seemed
different.Westfallet al.37 conducted anothermeta-
analysis, but concentrating on ROSC. They selected 12
investigations(reported in 6 journalarticles30,36,38–41
and 6 abstracts)enrolling 6538 patients.The ROSC
events were 1824. Like the previous meta-analysis, they
found that LUCAS and AutoPulse had different effec-
tiveness: LUCAS had an effect similar to manual CPR,
while AutoPulse had significantlygreaterodds of
ROSC. Therefore,unlike the previous meta-analysis,
they concluded thatboth mechanicaldeviceshad,
together,higher odds ofROSC compared to manual
CPR. The updated review of Brooks et al.42 analyzed
six trials with a totalof 1166 patients.Despite such
studies lacked clinical homogeneity and overall quality,
the authors concluded that there was no evidence that
mechanicalCPR is more beneficialor harmfulthan
manual CPR. Bonnes et al.43 reached a similar conclu-
sion afterhaving analyzed 20 studies,5 randomized
controlled trials,and 15 studies with non-randomized
design,for a total of 21,363 patients.Couper et al.44
carried out a review and meta-analysis to ascertain the
effectivenessof automated devicesduring in-hospital
6 Advances in MechanicalEngineering
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
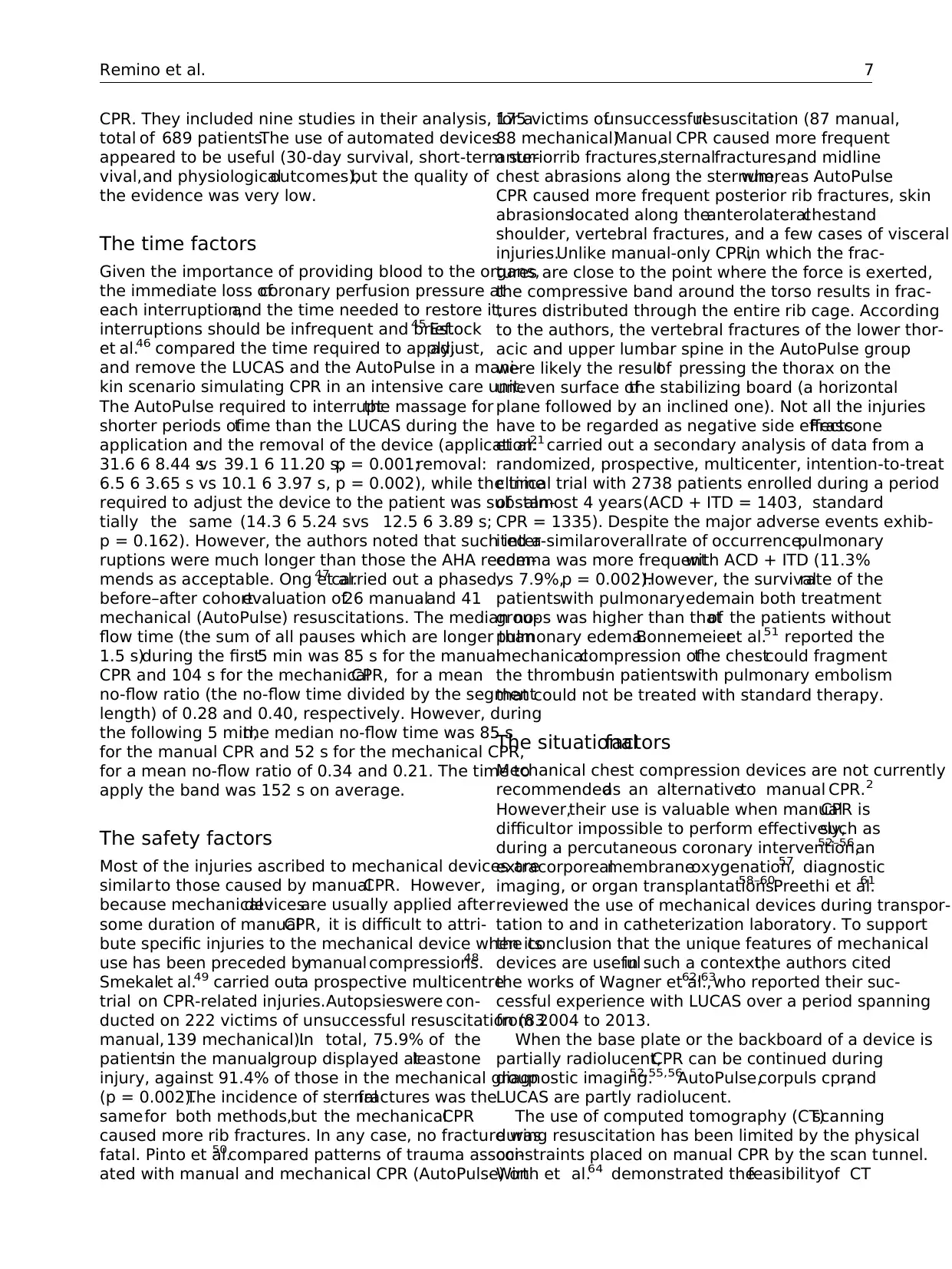
CPR. They included nine studies in their analysis, for a
total of 689 patients.The use of automated devices
appeared to be useful (30-day survival, short-term sur-
vival,and physiologicaloutcomes),but the quality of
the evidence was very low.
The time factors
Given the importance of providing blood to the organs,
the immediate loss ofcoronary perfusion pressure at
each interruption,and the time needed to restore it,
interruptions should be infrequent and brief.45 Estock
et al.46 compared the time required to apply,adjust,
and remove the LUCAS and the AutoPulse in a mani-
kin scenario simulating CPR in an intensive care unit.
The AutoPulse required to interruptthe massage for
shorter periods oftime than the LUCAS during the
application and the removal of the device (application:
31.6 6 8.44 svs 39.1 6 11.20 s,p = 0.001;removal:
6.5 6 3.65 s vs 10.1 6 3.97 s, p = 0.002), while the time
required to adjust the device to the patient was substan-
tially the same (14.3 6 5.24 svs 12.5 6 3.89 s;
p = 0.162). However, the authors noted that such inter-
ruptions were much longer than those the AHA recom-
mends as acceptable. Ong et al.47 carried out a phased,
before–after cohortevaluation of26 manualand 41
mechanical (AutoPulse) resuscitations. The median no-
flow time (the sum of all pauses which are longer than
1.5 s)during the first5 min was 85 s for the manual
CPR and 104 s for the mechanicalCPR, for a mean
no-flow ratio (the no-flow time divided by the segment
length) of 0.28 and 0.40, respectively. However, during
the following 5 min,the median no-flow time was 85 s
for the manual CPR and 52 s for the mechanical CPR,
for a mean no-flow ratio of 0.34 and 0.21. The time to
apply the band was 152 s on average.
The safety factors
Most of the injuries ascribed to mechanical devices are
similar to those caused by manualCPR. However,
because mechanicaldevicesare usually applied after
some duration of manualCPR, it is difficult to attri-
bute specific injuries to the mechanical device when its
use has been preceded bymanual compressions.48
Smekalet al.49 carried outa prospective multicentre
trial on CPR-related injuries.Autopsieswere con-
ducted on 222 victims of unsuccessful resuscitation (83
manual, 139 mechanical).In total, 75.9% of the
patientsin the manualgroup displayed atleastone
injury, against 91.4% of those in the mechanical group
(p = 0.002).The incidence of sternalfractures was the
samefor both methods,but the mechanicalCPR
caused more rib fractures. In any case, no fracture was
fatal. Pinto et al.50compared patterns of trauma associ-
ated with manual and mechanical CPR (AutoPulse) on
175 victims ofunsuccessfulresuscitation (87 manual,
88 mechanical).Manual CPR caused more frequent
anteriorrib fractures,sternalfractures,and midline
chest abrasions along the sternum,whereas AutoPulse
CPR caused more frequent posterior rib fractures, skin
abrasionslocated along theanterolateralchestand
shoulder, vertebral fractures, and a few cases of visceral
injuries.Unlike manual-only CPR,in which the frac-
tures are close to the point where the force is exerted,
the compressive band around the torso results in frac-
tures distributed through the entire rib cage. According
to the authors, the vertebral fractures of the lower thor-
acic and upper lumbar spine in the AutoPulse group
were likely the resultof pressing the thorax on the
uneven surface ofthe stabilizing board (a horizontal
plane followed by an inclined one). Not all the injuries
have to be regarded as negative side effects.Frascone
et al.21 carried out a secondary analysis of data from a
randomized, prospective, multicenter, intention-to-treat
clinical trial with 2738 patients enrolled during a period
of almost 4 years(ACD + ITD = 1403, standard
CPR = 1335). Despite the major adverse events exhib-
ited a similaroverallrate of occurrence,pulmonary
edema was more frequentwith ACD + ITD (11.3%
vs 7.9%,p = 0.002).However, the survivalrate of the
patientswith pulmonaryedemain both treatment
groups was higher than thatof the patients without
pulmonary edema.Bonnemeieret al.51 reported the
mechanicalcompression ofthe chestcould fragment
the thrombusin patientswith pulmonary embolism
that could not be treated with standard therapy.
The situationalfactors
Mechanical chest compression devices are not currently
recommendedas an alternativeto manual CPR. 2
However,their use is valuable when manualCPR is
difficultor impossible to perform effectively,such as
during a percutaneous coronary intervention,52–56an
extracorporealmembraneoxygenation,57 diagnostic
imaging, or organ transplantations.58–60Preethi et al.61
reviewed the use of mechanical devices during transpor-
tation to and in catheterization laboratory. To support
the conclusion that the unique features of mechanical
devices are usefulin such a context,the authors cited
the works of Wagner et al.,62,63
who reported their suc-
cessful experience with LUCAS over a period spanning
from 2004 to 2013.
When the base plate or the backboard of a device is
partially radiolucent,CPR can be continued during
diagnostic imaging.52,55,56
AutoPulse,corpuls cpr,and
LUCAS are partly radiolucent.
The use of computed tomography (CT)scanning
during resuscitation has been limited by the physical
constraints placed on manual CPR by the scan tunnel.
Wirth et al.64 demonstrated thefeasibilityof CT
Remino et al. 7
total of 689 patients.The use of automated devices
appeared to be useful (30-day survival, short-term sur-
vival,and physiologicaloutcomes),but the quality of
the evidence was very low.
The time factors
Given the importance of providing blood to the organs,
the immediate loss ofcoronary perfusion pressure at
each interruption,and the time needed to restore it,
interruptions should be infrequent and brief.45 Estock
et al.46 compared the time required to apply,adjust,
and remove the LUCAS and the AutoPulse in a mani-
kin scenario simulating CPR in an intensive care unit.
The AutoPulse required to interruptthe massage for
shorter periods oftime than the LUCAS during the
application and the removal of the device (application:
31.6 6 8.44 svs 39.1 6 11.20 s,p = 0.001;removal:
6.5 6 3.65 s vs 10.1 6 3.97 s, p = 0.002), while the time
required to adjust the device to the patient was substan-
tially the same (14.3 6 5.24 svs 12.5 6 3.89 s;
p = 0.162). However, the authors noted that such inter-
ruptions were much longer than those the AHA recom-
mends as acceptable. Ong et al.47 carried out a phased,
before–after cohortevaluation of26 manualand 41
mechanical (AutoPulse) resuscitations. The median no-
flow time (the sum of all pauses which are longer than
1.5 s)during the first5 min was 85 s for the manual
CPR and 104 s for the mechanicalCPR, for a mean
no-flow ratio (the no-flow time divided by the segment
length) of 0.28 and 0.40, respectively. However, during
the following 5 min,the median no-flow time was 85 s
for the manual CPR and 52 s for the mechanical CPR,
for a mean no-flow ratio of 0.34 and 0.21. The time to
apply the band was 152 s on average.
The safety factors
Most of the injuries ascribed to mechanical devices are
similar to those caused by manualCPR. However,
because mechanicaldevicesare usually applied after
some duration of manualCPR, it is difficult to attri-
bute specific injuries to the mechanical device when its
use has been preceded bymanual compressions.48
Smekalet al.49 carried outa prospective multicentre
trial on CPR-related injuries.Autopsieswere con-
ducted on 222 victims of unsuccessful resuscitation (83
manual, 139 mechanical).In total, 75.9% of the
patientsin the manualgroup displayed atleastone
injury, against 91.4% of those in the mechanical group
(p = 0.002).The incidence of sternalfractures was the
samefor both methods,but the mechanicalCPR
caused more rib fractures. In any case, no fracture was
fatal. Pinto et al.50compared patterns of trauma associ-
ated with manual and mechanical CPR (AutoPulse) on
175 victims ofunsuccessfulresuscitation (87 manual,
88 mechanical).Manual CPR caused more frequent
anteriorrib fractures,sternalfractures,and midline
chest abrasions along the sternum,whereas AutoPulse
CPR caused more frequent posterior rib fractures, skin
abrasionslocated along theanterolateralchestand
shoulder, vertebral fractures, and a few cases of visceral
injuries.Unlike manual-only CPR,in which the frac-
tures are close to the point where the force is exerted,
the compressive band around the torso results in frac-
tures distributed through the entire rib cage. According
to the authors, the vertebral fractures of the lower thor-
acic and upper lumbar spine in the AutoPulse group
were likely the resultof pressing the thorax on the
uneven surface ofthe stabilizing board (a horizontal
plane followed by an inclined one). Not all the injuries
have to be regarded as negative side effects.Frascone
et al.21 carried out a secondary analysis of data from a
randomized, prospective, multicenter, intention-to-treat
clinical trial with 2738 patients enrolled during a period
of almost 4 years(ACD + ITD = 1403, standard
CPR = 1335). Despite the major adverse events exhib-
ited a similaroverallrate of occurrence,pulmonary
edema was more frequentwith ACD + ITD (11.3%
vs 7.9%,p = 0.002).However, the survivalrate of the
patientswith pulmonaryedemain both treatment
groups was higher than thatof the patients without
pulmonary edema.Bonnemeieret al.51 reported the
mechanicalcompression ofthe chestcould fragment
the thrombusin patientswith pulmonary embolism
that could not be treated with standard therapy.
The situationalfactors
Mechanical chest compression devices are not currently
recommendedas an alternativeto manual CPR. 2
However,their use is valuable when manualCPR is
difficultor impossible to perform effectively,such as
during a percutaneous coronary intervention,52–56an
extracorporealmembraneoxygenation,57 diagnostic
imaging, or organ transplantations.58–60Preethi et al.61
reviewed the use of mechanical devices during transpor-
tation to and in catheterization laboratory. To support
the conclusion that the unique features of mechanical
devices are usefulin such a context,the authors cited
the works of Wagner et al.,62,63
who reported their suc-
cessful experience with LUCAS over a period spanning
from 2004 to 2013.
When the base plate or the backboard of a device is
partially radiolucent,CPR can be continued during
diagnostic imaging.52,55,56
AutoPulse,corpuls cpr,and
LUCAS are partly radiolucent.
The use of computed tomography (CT)scanning
during resuscitation has been limited by the physical
constraints placed on manual CPR by the scan tunnel.
Wirth et al.64 demonstrated thefeasibilityof CT
Remino et al. 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
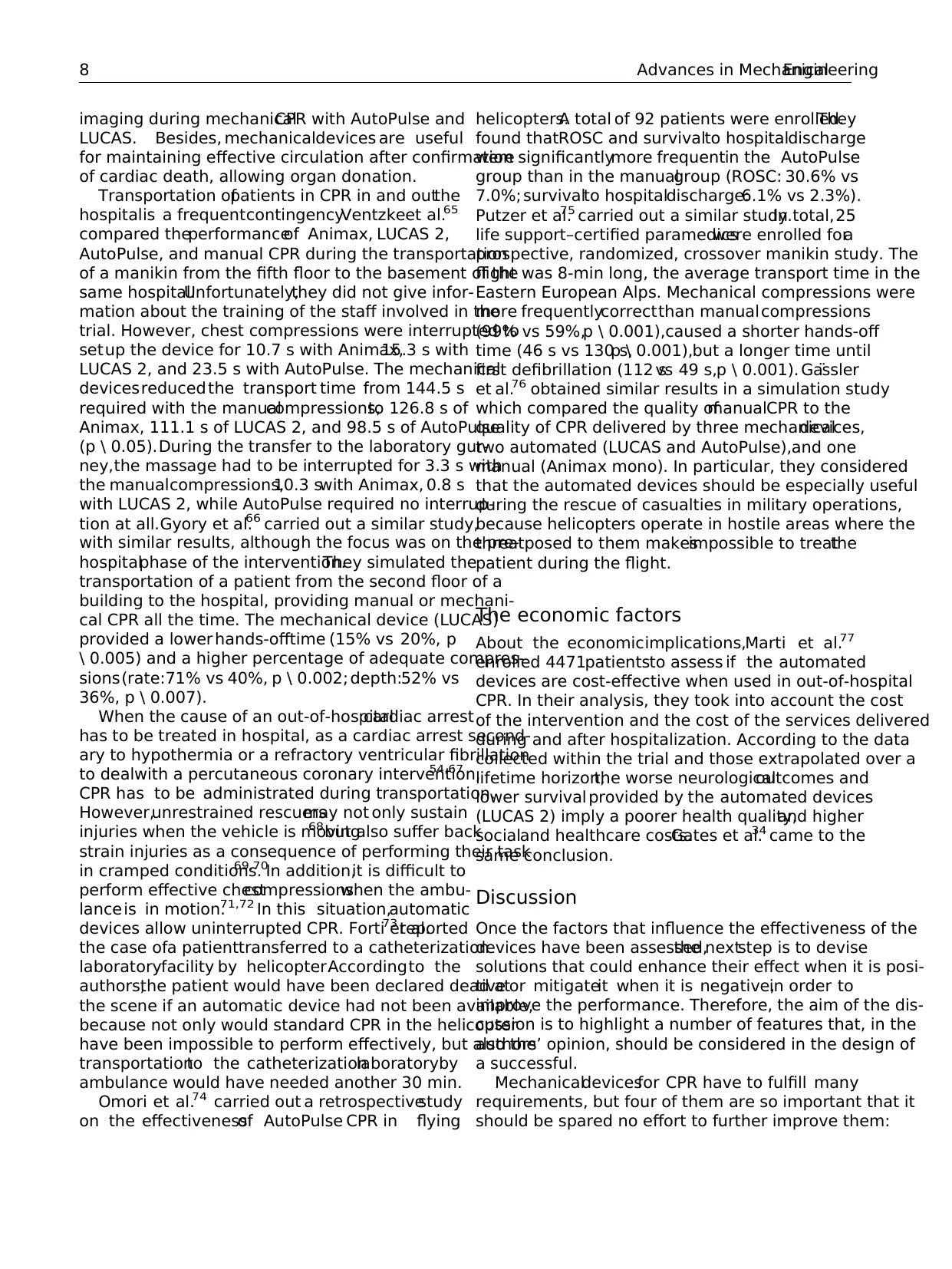
imaging during mechanicalCPR with AutoPulse and
LUCAS. Besides, mechanicaldevices are useful
for maintaining effective circulation after confirmation
of cardiac death, allowing organ donation.
Transportation ofpatients in CPR in and outthe
hospitalis a frequentcontingency.Ventzkeet al.65
compared theperformanceof Animax, LUCAS 2,
AutoPulse, and manual CPR during the transportation
of a manikin from the fifth floor to the basement of the
same hospital.Unfortunately,they did not give infor-
mation about the training of the staff involved in the
trial. However, chest compressions were interrupted to
setup the device for 10.7 s with Animax,15.3 s with
LUCAS 2, and 23.5 s with AutoPulse. The mechanical
devicesreduced the transport time from 144.5 s
required with the manualcompressions,to 126.8 s of
Animax, 111.1 s of LUCAS 2, and 98.5 s of AutoPulse
(p \ 0.05).During the transfer to the laboratory gur-
ney,the massage had to be interrupted for 3.3 s with
the manualcompressions,10.3 swith Animax, 0.8 s
with LUCAS 2, while AutoPulse required no interrup-
tion at all.Gyory et al.66 carried out a similar study,
with similar results, although the focus was on the pre-
hospitalphase of the intervention.They simulated the
transportation of a patient from the second floor of a
building to the hospital, providing manual or mechani-
cal CPR all the time. The mechanical device (LUCAS)
provided a lower hands-offtime (15% vs 20%, p
\ 0.005) and a higher percentage of adequate compres-
sions(rate:71% vs 40%, p \ 0.002; depth:52% vs
36%, p \ 0.007).
When the cause of an out-of-hospitalcardiac arrest
has to be treated in hospital, as a cardiac arrest second-
ary to hypothermia or a refractory ventricular fibrillation
to dealwith a percutaneous coronary intervention,54,67
CPR has to be administrated during transportation.
However,unrestrained rescuersmay not only sustain
injuries when the vehicle is moving68but also suffer back
strain injuries as a consequence of performing their task
in cramped conditions.69,70In addition,it is difficult to
perform effective chestcompressionswhen the ambu-
lance is in motion.71,72 In this situation,automatic
devices allow uninterrupted CPR. Forti et al.73 reported
the case ofa patienttransferred to a catheterization
laboratoryfacility by helicopter.Accordingto the
authors,the patient would have been declared dead at
the scene if an automatic device had not been available,
because not only would standard CPR in the helicopter
have been impossible to perform effectively, but also the
transportationto the catheterizationlaboratoryby
ambulance would have needed another 30 min.
Omori et al.74 carried out a retrospectivestudy
on the effectivenessof AutoPulse CPR in flying
helicopters.A total of 92 patients were enrolled.They
found thatROSC and survivalto hospitaldischarge
were significantlymore frequentin the AutoPulse
group than in the manualgroup (ROSC: 30.6% vs
7.0%; survivalto hospitaldischarge:6.1% vs 2.3%).
Putzer et al.75 carried out a similar study.In total,25
life support–certified paramedicswere enrolled fora
prospective, randomized, crossover manikin study. The
flight was 8-min long, the average transport time in the
Eastern European Alps. Mechanical compressions were
more frequentlycorrectthan manualcompressions
(99% vs 59%,p \ 0.001),caused a shorter hands-off
time (46 s vs 130 s,p \ 0.001),but a longer time until
first defibrillation (112 svs 49 s,p \ 0.001). Ga¨ssler
et al.76 obtained similar results in a simulation study
which compared the quality ofmanualCPR to the
quality of CPR delivered by three mechanicaldevices,
two automated (LUCAS and AutoPulse),and one
manual (Animax mono). In particular, they considered
that the automated devices should be especially useful
during the rescue of casualties in military operations,
because helicopters operate in hostile areas where the
threatposed to them makesimpossible to treatthe
patient during the flight.
The economic factors
About the economicimplications,Marti et al.77
enrolled 4471patientsto assess if the automated
devices are cost-effective when used in out-of-hospital
CPR. In their analysis, they took into account the cost
of the intervention and the cost of the services delivered
during and after hospitalization. According to the data
collected within the trial and those extrapolated over a
lifetime horizon,the worse neurologicaloutcomes and
lower survival provided by the automated devices
(LUCAS 2) imply a poorer health quality,and higher
socialand healthcare costs.Gates et al.34 came to the
same conclusion.
Discussion
Once the factors that influence the effectiveness of the
devices have been assessed,the nextstep is to devise
solutions that could enhance their effect when it is posi-
tive or mitigateit when it is negative,in order to
improve the performance. Therefore, the aim of the dis-
cussion is to highlight a number of features that, in the
authors’ opinion, should be considered in the design of
a successful.
Mechanicaldevicesfor CPR have to fulfill many
requirements, but four of them are so important that it
should be spared no effort to further improve them:
8 Advances in MechanicalEngineering
LUCAS. Besides, mechanicaldevices are useful
for maintaining effective circulation after confirmation
of cardiac death, allowing organ donation.
Transportation ofpatients in CPR in and outthe
hospitalis a frequentcontingency.Ventzkeet al.65
compared theperformanceof Animax, LUCAS 2,
AutoPulse, and manual CPR during the transportation
of a manikin from the fifth floor to the basement of the
same hospital.Unfortunately,they did not give infor-
mation about the training of the staff involved in the
trial. However, chest compressions were interrupted to
setup the device for 10.7 s with Animax,15.3 s with
LUCAS 2, and 23.5 s with AutoPulse. The mechanical
devicesreduced the transport time from 144.5 s
required with the manualcompressions,to 126.8 s of
Animax, 111.1 s of LUCAS 2, and 98.5 s of AutoPulse
(p \ 0.05).During the transfer to the laboratory gur-
ney,the massage had to be interrupted for 3.3 s with
the manualcompressions,10.3 swith Animax, 0.8 s
with LUCAS 2, while AutoPulse required no interrup-
tion at all.Gyory et al.66 carried out a similar study,
with similar results, although the focus was on the pre-
hospitalphase of the intervention.They simulated the
transportation of a patient from the second floor of a
building to the hospital, providing manual or mechani-
cal CPR all the time. The mechanical device (LUCAS)
provided a lower hands-offtime (15% vs 20%, p
\ 0.005) and a higher percentage of adequate compres-
sions(rate:71% vs 40%, p \ 0.002; depth:52% vs
36%, p \ 0.007).
When the cause of an out-of-hospitalcardiac arrest
has to be treated in hospital, as a cardiac arrest second-
ary to hypothermia or a refractory ventricular fibrillation
to dealwith a percutaneous coronary intervention,54,67
CPR has to be administrated during transportation.
However,unrestrained rescuersmay not only sustain
injuries when the vehicle is moving68but also suffer back
strain injuries as a consequence of performing their task
in cramped conditions.69,70In addition,it is difficult to
perform effective chestcompressionswhen the ambu-
lance is in motion.71,72 In this situation,automatic
devices allow uninterrupted CPR. Forti et al.73 reported
the case ofa patienttransferred to a catheterization
laboratoryfacility by helicopter.Accordingto the
authors,the patient would have been declared dead at
the scene if an automatic device had not been available,
because not only would standard CPR in the helicopter
have been impossible to perform effectively, but also the
transportationto the catheterizationlaboratoryby
ambulance would have needed another 30 min.
Omori et al.74 carried out a retrospectivestudy
on the effectivenessof AutoPulse CPR in flying
helicopters.A total of 92 patients were enrolled.They
found thatROSC and survivalto hospitaldischarge
were significantlymore frequentin the AutoPulse
group than in the manualgroup (ROSC: 30.6% vs
7.0%; survivalto hospitaldischarge:6.1% vs 2.3%).
Putzer et al.75 carried out a similar study.In total,25
life support–certified paramedicswere enrolled fora
prospective, randomized, crossover manikin study. The
flight was 8-min long, the average transport time in the
Eastern European Alps. Mechanical compressions were
more frequentlycorrectthan manualcompressions
(99% vs 59%,p \ 0.001),caused a shorter hands-off
time (46 s vs 130 s,p \ 0.001),but a longer time until
first defibrillation (112 svs 49 s,p \ 0.001). Ga¨ssler
et al.76 obtained similar results in a simulation study
which compared the quality ofmanualCPR to the
quality of CPR delivered by three mechanicaldevices,
two automated (LUCAS and AutoPulse),and one
manual (Animax mono). In particular, they considered
that the automated devices should be especially useful
during the rescue of casualties in military operations,
because helicopters operate in hostile areas where the
threatposed to them makesimpossible to treatthe
patient during the flight.
The economic factors
About the economicimplications,Marti et al.77
enrolled 4471patientsto assess if the automated
devices are cost-effective when used in out-of-hospital
CPR. In their analysis, they took into account the cost
of the intervention and the cost of the services delivered
during and after hospitalization. According to the data
collected within the trial and those extrapolated over a
lifetime horizon,the worse neurologicaloutcomes and
lower survival provided by the automated devices
(LUCAS 2) imply a poorer health quality,and higher
socialand healthcare costs.Gates et al.34 came to the
same conclusion.
Discussion
Once the factors that influence the effectiveness of the
devices have been assessed,the nextstep is to devise
solutions that could enhance their effect when it is posi-
tive or mitigateit when it is negative,in order to
improve the performance. Therefore, the aim of the dis-
cussion is to highlight a number of features that, in the
authors’ opinion, should be considered in the design of
a successful.
Mechanicaldevicesfor CPR have to fulfill many
requirements, but four of them are so important that it
should be spared no effort to further improve them:
8 Advances in MechanicalEngineering
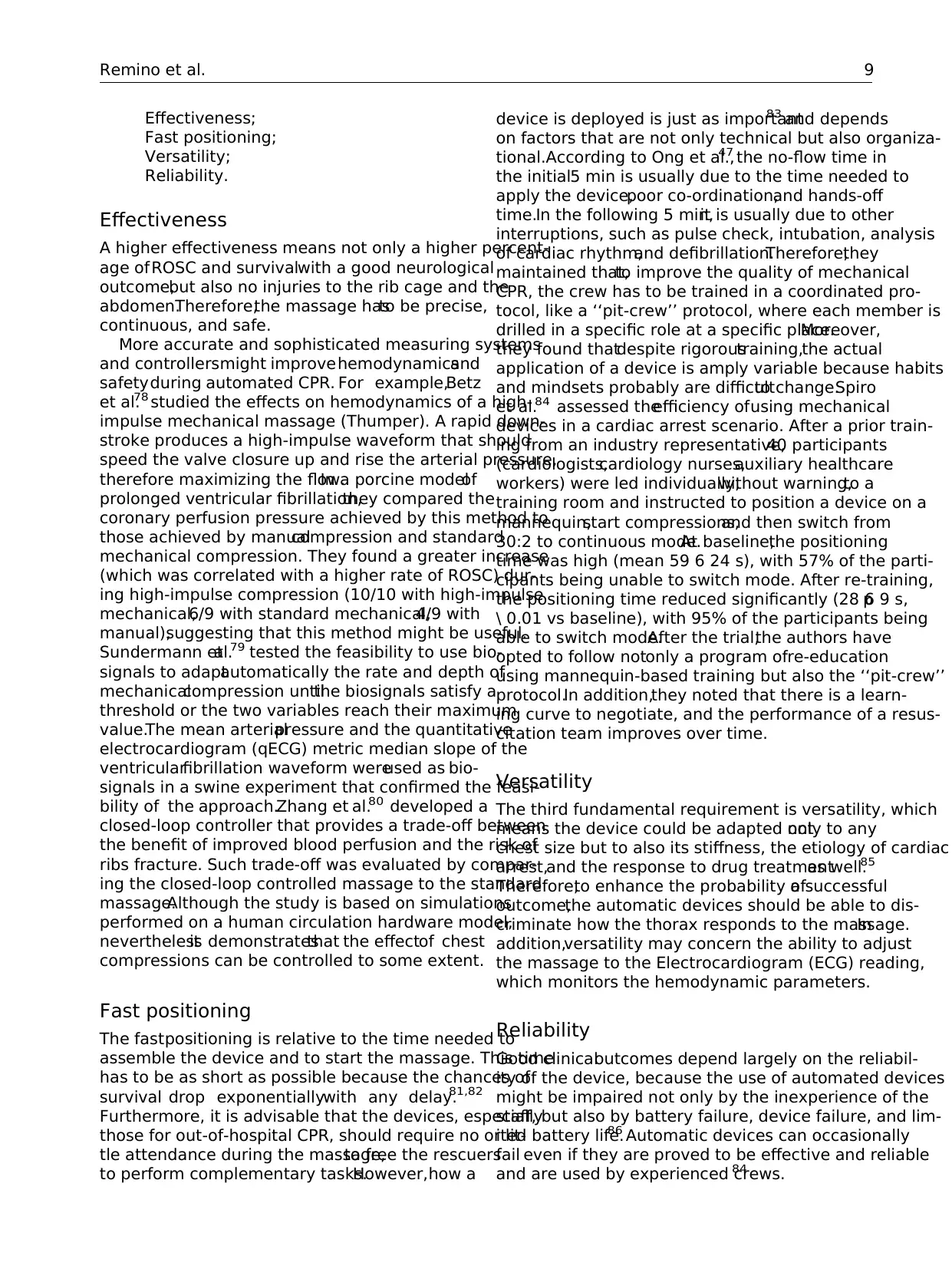
Effectiveness;
Fast positioning;
Versatility;
Reliability.
Effectiveness
A higher effectiveness means not only a higher percent-
age of ROSC and survivalwith a good neurological
outcome,but also no injuries to the rib cage and the
abdomen.Therefore,the massage hasto be precise,
continuous, and safe.
More accurate and sophisticated measuring systems
and controllersmight improvehemodynamicsand
safetyduring automated CPR. For example,Betz
et al.78 studied the effects on hemodynamics of a high-
impulse mechanical massage (Thumper). A rapid down-
stroke produces a high-impulse waveform that should
speed the valve closure up and rise the arterial pressure,
therefore maximizing the flow.In a porcine modelof
prolonged ventricular fibrillation,they compared the
coronary perfusion pressure achieved by this method to
those achieved by manualcompression and standard
mechanical compression. They found a greater increase
(which was correlated with a higher rate of ROSC) dur-
ing high-impulse compression (10/10 with high-impulse
mechanical,6/9 with standard mechanical,4/9 with
manual),suggesting that this method might be useful.
Sundermann etal.79 tested the feasibility to use bio-
signals to adaptautomatically the rate and depth of
mechanicalcompression untilthe biosignals satisfy a
threshold or the two variables reach their maximum
value.The mean arterialpressure and the quantitative
electrocardiogram (qECG) metric median slope of the
ventricularfibrillation waveform wereused as bio-
signals in a swine experiment that confirmed the feasi-
bility of the approach.Zhang et al.80 developed a
closed-loop controller that provides a trade-off between
the benefit of improved blood perfusion and the risk of
ribs fracture. Such trade-off was evaluated by compar-
ing the closed-loop controlled massage to the standard
massage.Although the study is based on simulations
performed on a human circulation hardware model,
neverthelessit demonstratesthat the effectof chest
compressions can be controlled to some extent.
Fast positioning
The fastpositioning is relative to the time needed to
assemble the device and to start the massage. This time
has to be as short as possible because the chances of
survival drop exponentiallywith any delay.81,82
Furthermore, it is advisable that the devices, especially
those for out-of-hospital CPR, should require no or lit-
tle attendance during the massage,to free the rescuers
to perform complementary tasks.However,how a
device is deployed is just as important83 and depends
on factors that are not only technical but also organiza-
tional.According to Ong et al.,47 the no-flow time in
the initial5 min is usually due to the time needed to
apply the device,poor co-ordination,and hands-off
time.In the following 5 min,it is usually due to other
interruptions, such as pulse check, intubation, analysis
of cardiac rhythm,and defibrillation.Therefore,they
maintained that,to improve the quality of mechanical
CPR, the crew has to be trained in a coordinated pro-
tocol, like a ‘‘pit-crew’’ protocol, where each member is
drilled in a specific role at a specific place.Moreover,
they found thatdespite rigoroustraining,the actual
application of a device is amply variable because habits
and mindsets probably are difficultto change.Spiro
et al.84 assessed theefficiency ofusing mechanical
devices in a cardiac arrest scenario. After a prior train-
ing from an industry representative,40 participants
(cardiologists,cardiology nurses,auxiliary healthcare
workers) were led individually,without warning,to a
training room and instructed to position a device on a
mannequin,start compressions,and then switch from
30:2 to continuous mode.At baseline,the positioning
time was high (mean 59 6 24 s), with 57% of the parti-
cipants being unable to switch mode. After re-training,
the positioning time reduced significantly (28 6 9 s,p
\ 0.01 vs baseline), with 95% of the participants being
able to switch mode.After the trial,the authors have
opted to follow notonly a program ofre-education
using mannequin-based training but also the ‘‘pit-crew’’
protocol.In addition,they noted that there is a learn-
ing curve to negotiate, and the performance of a resus-
citation team improves over time.
Versatility
The third fundamental requirement is versatility, which
means the device could be adapted notonly to any
chest size but to also its stiffness, the etiology of cardiac
arrest,and the response to drug treatmentas well.85
Therefore,to enhance the probability ofa successful
outcome,the automatic devices should be able to dis-
criminate how the thorax responds to the massage.In
addition,versatility may concern the ability to adjust
the massage to the Electrocardiogram (ECG) reading,
which monitors the hemodynamic parameters.
Reliability
Good clinicaloutcomes depend largely on the reliabil-
ity of the device, because the use of automated devices
might be impaired not only by the inexperience of the
staff, but also by battery failure, device failure, and lim-
ited battery life.86 Automatic devices can occasionally
fail even if they are proved to be effective and reliable
and are used by experienced crews.84
Remino et al. 9
Fast positioning;
Versatility;
Reliability.
Effectiveness
A higher effectiveness means not only a higher percent-
age of ROSC and survivalwith a good neurological
outcome,but also no injuries to the rib cage and the
abdomen.Therefore,the massage hasto be precise,
continuous, and safe.
More accurate and sophisticated measuring systems
and controllersmight improvehemodynamicsand
safetyduring automated CPR. For example,Betz
et al.78 studied the effects on hemodynamics of a high-
impulse mechanical massage (Thumper). A rapid down-
stroke produces a high-impulse waveform that should
speed the valve closure up and rise the arterial pressure,
therefore maximizing the flow.In a porcine modelof
prolonged ventricular fibrillation,they compared the
coronary perfusion pressure achieved by this method to
those achieved by manualcompression and standard
mechanical compression. They found a greater increase
(which was correlated with a higher rate of ROSC) dur-
ing high-impulse compression (10/10 with high-impulse
mechanical,6/9 with standard mechanical,4/9 with
manual),suggesting that this method might be useful.
Sundermann etal.79 tested the feasibility to use bio-
signals to adaptautomatically the rate and depth of
mechanicalcompression untilthe biosignals satisfy a
threshold or the two variables reach their maximum
value.The mean arterialpressure and the quantitative
electrocardiogram (qECG) metric median slope of the
ventricularfibrillation waveform wereused as bio-
signals in a swine experiment that confirmed the feasi-
bility of the approach.Zhang et al.80 developed a
closed-loop controller that provides a trade-off between
the benefit of improved blood perfusion and the risk of
ribs fracture. Such trade-off was evaluated by compar-
ing the closed-loop controlled massage to the standard
massage.Although the study is based on simulations
performed on a human circulation hardware model,
neverthelessit demonstratesthat the effectof chest
compressions can be controlled to some extent.
Fast positioning
The fastpositioning is relative to the time needed to
assemble the device and to start the massage. This time
has to be as short as possible because the chances of
survival drop exponentiallywith any delay.81,82
Furthermore, it is advisable that the devices, especially
those for out-of-hospital CPR, should require no or lit-
tle attendance during the massage,to free the rescuers
to perform complementary tasks.However,how a
device is deployed is just as important83 and depends
on factors that are not only technical but also organiza-
tional.According to Ong et al.,47 the no-flow time in
the initial5 min is usually due to the time needed to
apply the device,poor co-ordination,and hands-off
time.In the following 5 min,it is usually due to other
interruptions, such as pulse check, intubation, analysis
of cardiac rhythm,and defibrillation.Therefore,they
maintained that,to improve the quality of mechanical
CPR, the crew has to be trained in a coordinated pro-
tocol, like a ‘‘pit-crew’’ protocol, where each member is
drilled in a specific role at a specific place.Moreover,
they found thatdespite rigoroustraining,the actual
application of a device is amply variable because habits
and mindsets probably are difficultto change.Spiro
et al.84 assessed theefficiency ofusing mechanical
devices in a cardiac arrest scenario. After a prior train-
ing from an industry representative,40 participants
(cardiologists,cardiology nurses,auxiliary healthcare
workers) were led individually,without warning,to a
training room and instructed to position a device on a
mannequin,start compressions,and then switch from
30:2 to continuous mode.At baseline,the positioning
time was high (mean 59 6 24 s), with 57% of the parti-
cipants being unable to switch mode. After re-training,
the positioning time reduced significantly (28 6 9 s,p
\ 0.01 vs baseline), with 95% of the participants being
able to switch mode.After the trial,the authors have
opted to follow notonly a program ofre-education
using mannequin-based training but also the ‘‘pit-crew’’
protocol.In addition,they noted that there is a learn-
ing curve to negotiate, and the performance of a resus-
citation team improves over time.
Versatility
The third fundamental requirement is versatility, which
means the device could be adapted notonly to any
chest size but to also its stiffness, the etiology of cardiac
arrest,and the response to drug treatmentas well.85
Therefore,to enhance the probability ofa successful
outcome,the automatic devices should be able to dis-
criminate how the thorax responds to the massage.In
addition,versatility may concern the ability to adjust
the massage to the Electrocardiogram (ECG) reading,
which monitors the hemodynamic parameters.
Reliability
Good clinicaloutcomes depend largely on the reliabil-
ity of the device, because the use of automated devices
might be impaired not only by the inexperience of the
staff, but also by battery failure, device failure, and lim-
ited battery life.86 Automatic devices can occasionally
fail even if they are proved to be effective and reliable
and are used by experienced crews.84
Remino et al. 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
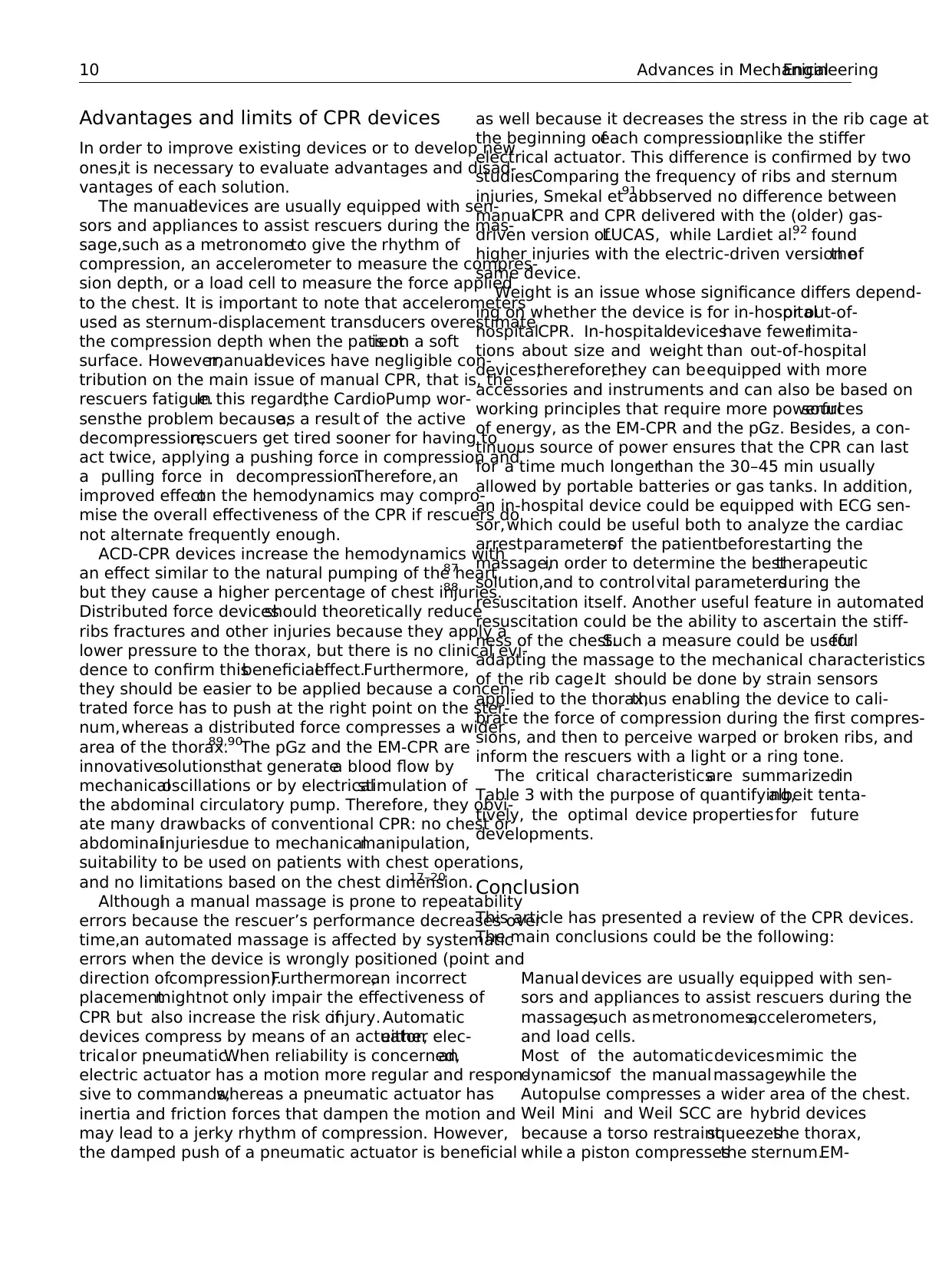
Advantages and limits of CPR devices
In order to improve existing devices or to develop new
ones,it is necessary to evaluate advantages and disad-
vantages of each solution.
The manualdevices are usually equipped with sen-
sors and appliances to assist rescuers during the mas-
sage,such as a metronometo give the rhythm of
compression, an accelerometer to measure the compres-
sion depth, or a load cell to measure the force applied
to the chest. It is important to note that accelerometers
used as sternum-displacement transducers overestimate
the compression depth when the patientis on a soft
surface. However,manualdevices have negligible con-
tribution on the main issue of manual CPR, that is, the
rescuers fatigue.In this regard,the CardioPump wor-
sensthe problem because,as a result of the active
decompression,rescuers get tired sooner for having to
act twice, applying a pushing force in compression and
a pulling force in decompression.Therefore,an
improved effecton the hemodynamics may compro-
mise the overall effectiveness of the CPR if rescuers do
not alternate frequently enough.
ACD-CPR devices increase the hemodynamics with
an effect similar to the natural pumping of the heart,87
but they cause a higher percentage of chest injuries.88
Distributed force devicesshould theoretically reduce
ribs fractures and other injuries because they apply a
lower pressure to the thorax, but there is no clinical evi-
dence to confirm thisbeneficialeffect.Furthermore,
they should be easier to be applied because a concen-
trated force has to push at the right point on the ster-
num,whereas a distributed force compresses a wider
area of the thorax.89,90The pGz and the EM-CPR are
innovativesolutionsthat generatea blood flow by
mechanicaloscillations or by electricalstimulation of
the abdominal circulatory pump. Therefore, they obvi-
ate many drawbacks of conventional CPR: no chest or
abdominalinjuriesdue to mechanicalmanipulation,
suitability to be used on patients with chest operations,
and no limitations based on the chest dimension.17–20
Although a manual massage is prone to repeatability
errors because the rescuer’s performance decreases over
time,an automated massage is affected by systematic
errors when the device is wrongly positioned (point and
direction ofcompression).Furthermore,an incorrect
placementmightnot only impair the effectiveness of
CPR but also increase the risk ofinjury. Automatic
devices compress by means of an actuator,either elec-
tricalor pneumatic.When reliability is concerned,an
electric actuator has a motion more regular and respon-
sive to commands,whereas a pneumatic actuator has
inertia and friction forces that dampen the motion and
may lead to a jerky rhythm of compression. However,
the damped push of a pneumatic actuator is beneficial
as well because it decreases the stress in the rib cage at
the beginning ofeach compression,unlike the stiffer
electrical actuator. This difference is confirmed by two
studies.Comparing the frequency of ribs and sternum
injuries, Smekal et al.91 observed no difference between
manualCPR and CPR delivered with the (older) gas-
driven version ofLUCAS, while Lardiet al.92 found
higher injuries with the electric-driven version ofthe
same device.
Weight is an issue whose significance differs depend-
ing on whether the device is for in-hospitalor out-of-
hospitalCPR. In-hospitaldeviceshave fewerlimita-
tions about size and weight than out-of-hospital
devices;therefore,they can beequipped with more
accessories and instruments and can also be based on
working principles that require more powerfulsources
of energy, as the EM-CPR and the pGz. Besides, a con-
tinuous source of power ensures that the CPR can last
for a time much longerthan the 30–45 min usually
allowed by portable batteries or gas tanks. In addition,
an in-hospital device could be equipped with ECG sen-
sor,which could be useful both to analyze the cardiac
arrestparametersof the patientbeforestarting the
massage,in order to determine the besttherapeutic
solution,and to controlvital parametersduring the
resuscitation itself. Another useful feature in automated
resuscitation could be the ability to ascertain the stiff-
ness of the chest.Such a measure could be usefulfor
adapting the massage to the mechanical characteristics
of the rib cage.It should be done by strain sensors
applied to the thorax,thus enabling the device to cali-
brate the force of compression during the first compres-
sions, and then to perceive warped or broken ribs, and
inform the rescuers with a light or a ring tone.
The critical characteristicsare summarizedin
Table 3 with the purpose of quantifying,albeit tenta-
tively, the optimal device propertiesfor future
developments.
Conclusion
This article has presented a review of the CPR devices.
The main conclusions could be the following:
Manual devices are usually equipped with sen-
sors and appliances to assist rescuers during the
massage,such asmetronomes,accelerometers,
and load cells.
Most of the automaticdevicesmimic the
dynamicsof the manualmassage,while the
Autopulse compresses a wider area of the chest.
Weil Mini and Weil SCC are hybrid devices
because a torso restraintsqueezesthe thorax,
while a piston compressesthe sternum.EM-
10 Advances in MechanicalEngineering
In order to improve existing devices or to develop new
ones,it is necessary to evaluate advantages and disad-
vantages of each solution.
The manualdevices are usually equipped with sen-
sors and appliances to assist rescuers during the mas-
sage,such as a metronometo give the rhythm of
compression, an accelerometer to measure the compres-
sion depth, or a load cell to measure the force applied
to the chest. It is important to note that accelerometers
used as sternum-displacement transducers overestimate
the compression depth when the patientis on a soft
surface. However,manualdevices have negligible con-
tribution on the main issue of manual CPR, that is, the
rescuers fatigue.In this regard,the CardioPump wor-
sensthe problem because,as a result of the active
decompression,rescuers get tired sooner for having to
act twice, applying a pushing force in compression and
a pulling force in decompression.Therefore,an
improved effecton the hemodynamics may compro-
mise the overall effectiveness of the CPR if rescuers do
not alternate frequently enough.
ACD-CPR devices increase the hemodynamics with
an effect similar to the natural pumping of the heart,87
but they cause a higher percentage of chest injuries.88
Distributed force devicesshould theoretically reduce
ribs fractures and other injuries because they apply a
lower pressure to the thorax, but there is no clinical evi-
dence to confirm thisbeneficialeffect.Furthermore,
they should be easier to be applied because a concen-
trated force has to push at the right point on the ster-
num,whereas a distributed force compresses a wider
area of the thorax.89,90The pGz and the EM-CPR are
innovativesolutionsthat generatea blood flow by
mechanicaloscillations or by electricalstimulation of
the abdominal circulatory pump. Therefore, they obvi-
ate many drawbacks of conventional CPR: no chest or
abdominalinjuriesdue to mechanicalmanipulation,
suitability to be used on patients with chest operations,
and no limitations based on the chest dimension.17–20
Although a manual massage is prone to repeatability
errors because the rescuer’s performance decreases over
time,an automated massage is affected by systematic
errors when the device is wrongly positioned (point and
direction ofcompression).Furthermore,an incorrect
placementmightnot only impair the effectiveness of
CPR but also increase the risk ofinjury. Automatic
devices compress by means of an actuator,either elec-
tricalor pneumatic.When reliability is concerned,an
electric actuator has a motion more regular and respon-
sive to commands,whereas a pneumatic actuator has
inertia and friction forces that dampen the motion and
may lead to a jerky rhythm of compression. However,
the damped push of a pneumatic actuator is beneficial
as well because it decreases the stress in the rib cage at
the beginning ofeach compression,unlike the stiffer
electrical actuator. This difference is confirmed by two
studies.Comparing the frequency of ribs and sternum
injuries, Smekal et al.91 observed no difference between
manualCPR and CPR delivered with the (older) gas-
driven version ofLUCAS, while Lardiet al.92 found
higher injuries with the electric-driven version ofthe
same device.
Weight is an issue whose significance differs depend-
ing on whether the device is for in-hospitalor out-of-
hospitalCPR. In-hospitaldeviceshave fewerlimita-
tions about size and weight than out-of-hospital
devices;therefore,they can beequipped with more
accessories and instruments and can also be based on
working principles that require more powerfulsources
of energy, as the EM-CPR and the pGz. Besides, a con-
tinuous source of power ensures that the CPR can last
for a time much longerthan the 30–45 min usually
allowed by portable batteries or gas tanks. In addition,
an in-hospital device could be equipped with ECG sen-
sor,which could be useful both to analyze the cardiac
arrestparametersof the patientbeforestarting the
massage,in order to determine the besttherapeutic
solution,and to controlvital parametersduring the
resuscitation itself. Another useful feature in automated
resuscitation could be the ability to ascertain the stiff-
ness of the chest.Such a measure could be usefulfor
adapting the massage to the mechanical characteristics
of the rib cage.It should be done by strain sensors
applied to the thorax,thus enabling the device to cali-
brate the force of compression during the first compres-
sions, and then to perceive warped or broken ribs, and
inform the rescuers with a light or a ring tone.
The critical characteristicsare summarizedin
Table 3 with the purpose of quantifying,albeit tenta-
tively, the optimal device propertiesfor future
developments.
Conclusion
This article has presented a review of the CPR devices.
The main conclusions could be the following:
Manual devices are usually equipped with sen-
sors and appliances to assist rescuers during the
massage,such asmetronomes,accelerometers,
and load cells.
Most of the automaticdevicesmimic the
dynamicsof the manualmassage,while the
Autopulse compresses a wider area of the chest.
Weil Mini and Weil SCC are hybrid devices
because a torso restraintsqueezesthe thorax,
while a piston compressesthe sternum.EM-
10 Advances in MechanicalEngineering
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
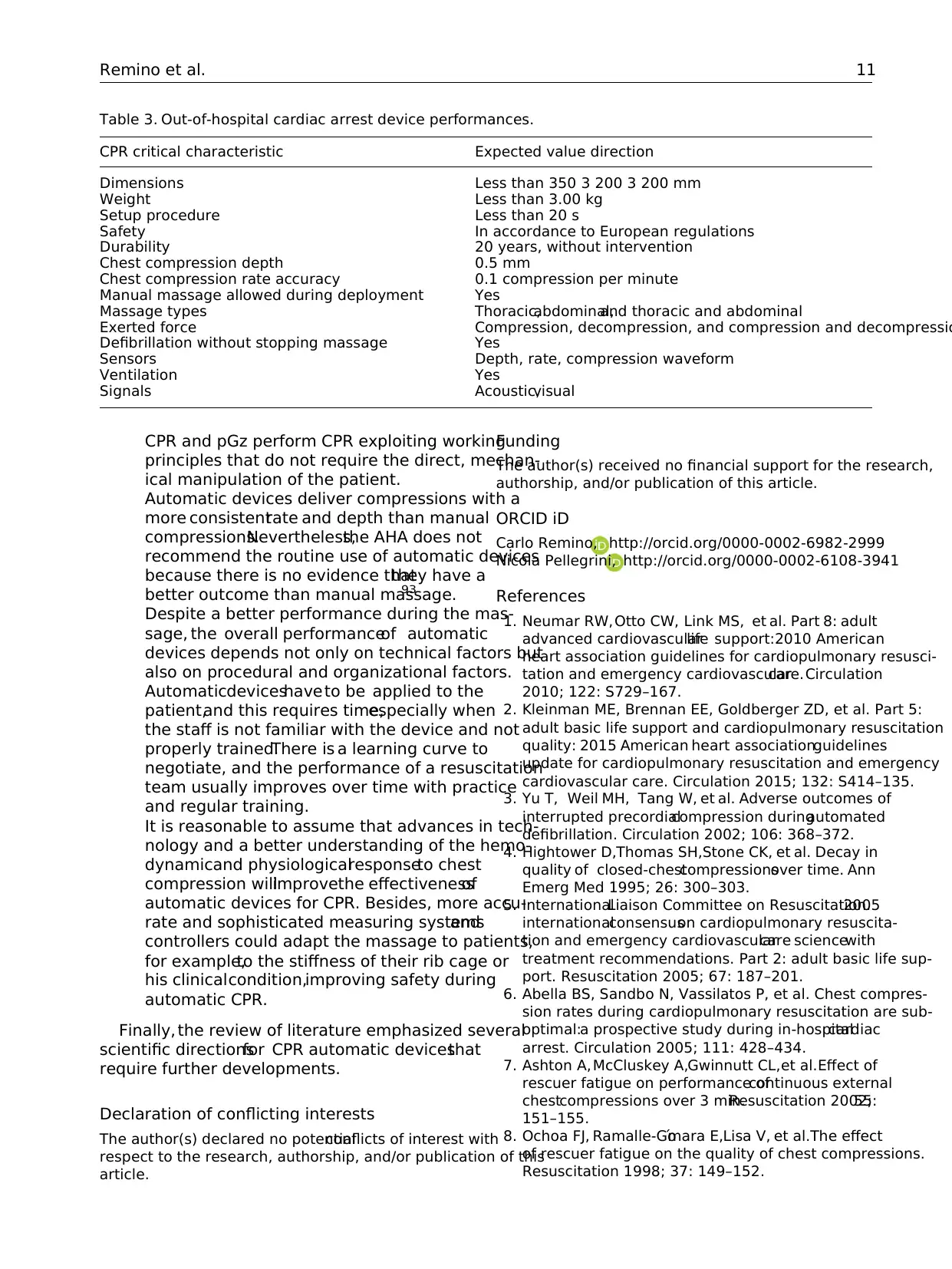
CPR and pGz perform CPR exploiting working
principles that do not require the direct, mechan-
ical manipulation of the patient.
Automatic devices deliver compressions with a
more consistentrate and depth than manual
compressions.Nevertheless,the AHA does not
recommend the routine use of automatic devices
because there is no evidence thatthey have a
better outcome than manual massage.93
Despite a better performance during the mas-
sage, the overall performanceof automatic
devices depends not only on technical factors but
also on procedural and organizational factors.
Automaticdeviceshave to be applied to the
patient,and this requires time,especially when
the staff is not familiar with the device and not
properly trained.There is a learning curve to
negotiate, and the performance of a resuscitation
team usually improves over time with practice
and regular training.
It is reasonable to assume that advances in tech-
nology and a better understanding of the hemo-
dynamicand physiologicalresponseto chest
compression willimprovethe effectivenessof
automatic devices for CPR. Besides, more accu-
rate and sophisticated measuring systemsand
controllers could adapt the massage to patients,
for example,to the stiffness of their rib cage or
his clinicalcondition,improving safety during
automatic CPR.
Finally, the review of literature emphasized several
scientific directionsfor CPR automatic devicesthat
require further developments.
Declaration of conflicting interests
The author(s) declared no potentialconflicts of interest with
respect to the research, authorship, and/or publication of this
article.
Funding
The author(s) received no financial support for the research,
authorship, and/or publication of this article.
ORCID iD
Carlo Remino, http://orcid.org/0000-0002-6982-2999
Nicola Pellegrini, http://orcid.org/0000-0002-6108-3941
References
1. Neumar RW,Otto CW, Link MS, et al. Part 8: adult
advanced cardiovascularlife support:2010 American
heart association guidelines for cardiopulmonary resusci-
tation and emergency cardiovascularcare.Circulation
2010; 122: S729–167.
2. Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5:
adult basic life support and cardiopulmonary resuscitation
quality: 2015 American heart associationguidelines
update for cardiopulmonary resuscitation and emergency
cardiovascular care. Circulation 2015; 132: S414–135.
3. Yu T, Weil MH, Tang W, et al. Adverse outcomes of
interrupted precordialcompression duringautomated
defibrillation. Circulation 2002; 106: 368–372.
4. Hightower D,Thomas SH,Stone CK, et al. Decay in
quality of closed-chestcompressionsover time. Ann
Emerg Med 1995; 26: 300–303.
5. InternationalLiaison Committee on Resuscitation.2005
internationalconsensuson cardiopulmonary resuscita-
tion and emergency cardiovascularcare sciencewith
treatment recommendations. Part 2: adult basic life sup-
port. Resuscitation 2005; 67: 187–201.
6. Abella BS, Sandbo N, Vassilatos P, et al. Chest compres-
sion rates during cardiopulmonary resuscitation are sub-
optimal:a prospective study during in-hospitalcardiac
arrest. Circulation 2005; 111: 428–434.
7. Ashton A, McCluskey A,Gwinnutt CL,et al.Effect of
rescuer fatigue on performance ofcontinuous external
chestcompressions over 3 min.Resuscitation 2002;55:
151–155.
8. Ochoa FJ, Ramalle-Go´mara E,Lisa V, et al.The effect
of rescuer fatigue on the quality of chest compressions.
Resuscitation 1998; 37: 149–152.
Table 3. Out-of-hospital cardiac arrest device performances.
CPR critical characteristic Expected value direction
Dimensions Less than 350 3 200 3 200 mm
Weight Less than 3.00 kg
Setup procedure Less than 20 s
Safety In accordance to European regulations
Durability 20 years, without intervention
Chest compression depth 0.5 mm
Chest compression rate accuracy 0.1 compression per minute
Manual massage allowed during deployment Yes
Massage types Thoracic,abdominal,and thoracic and abdominal
Exerted force Compression, decompression, and compression and decompressio
Defibrillation without stopping massage Yes
Sensors Depth, rate, compression waveform
Ventilation Yes
Signals Acoustic,visual
Remino et al. 11
principles that do not require the direct, mechan-
ical manipulation of the patient.
Automatic devices deliver compressions with a
more consistentrate and depth than manual
compressions.Nevertheless,the AHA does not
recommend the routine use of automatic devices
because there is no evidence thatthey have a
better outcome than manual massage.93
Despite a better performance during the mas-
sage, the overall performanceof automatic
devices depends not only on technical factors but
also on procedural and organizational factors.
Automaticdeviceshave to be applied to the
patient,and this requires time,especially when
the staff is not familiar with the device and not
properly trained.There is a learning curve to
negotiate, and the performance of a resuscitation
team usually improves over time with practice
and regular training.
It is reasonable to assume that advances in tech-
nology and a better understanding of the hemo-
dynamicand physiologicalresponseto chest
compression willimprovethe effectivenessof
automatic devices for CPR. Besides, more accu-
rate and sophisticated measuring systemsand
controllers could adapt the massage to patients,
for example,to the stiffness of their rib cage or
his clinicalcondition,improving safety during
automatic CPR.
Finally, the review of literature emphasized several
scientific directionsfor CPR automatic devicesthat
require further developments.
Declaration of conflicting interests
The author(s) declared no potentialconflicts of interest with
respect to the research, authorship, and/or publication of this
article.
Funding
The author(s) received no financial support for the research,
authorship, and/or publication of this article.
ORCID iD
Carlo Remino, http://orcid.org/0000-0002-6982-2999
Nicola Pellegrini, http://orcid.org/0000-0002-6108-3941
References
1. Neumar RW,Otto CW, Link MS, et al. Part 8: adult
advanced cardiovascularlife support:2010 American
heart association guidelines for cardiopulmonary resusci-
tation and emergency cardiovascularcare.Circulation
2010; 122: S729–167.
2. Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5:
adult basic life support and cardiopulmonary resuscitation
quality: 2015 American heart associationguidelines
update for cardiopulmonary resuscitation and emergency
cardiovascular care. Circulation 2015; 132: S414–135.
3. Yu T, Weil MH, Tang W, et al. Adverse outcomes of
interrupted precordialcompression duringautomated
defibrillation. Circulation 2002; 106: 368–372.
4. Hightower D,Thomas SH,Stone CK, et al. Decay in
quality of closed-chestcompressionsover time. Ann
Emerg Med 1995; 26: 300–303.
5. InternationalLiaison Committee on Resuscitation.2005
internationalconsensuson cardiopulmonary resuscita-
tion and emergency cardiovascularcare sciencewith
treatment recommendations. Part 2: adult basic life sup-
port. Resuscitation 2005; 67: 187–201.
6. Abella BS, Sandbo N, Vassilatos P, et al. Chest compres-
sion rates during cardiopulmonary resuscitation are sub-
optimal:a prospective study during in-hospitalcardiac
arrest. Circulation 2005; 111: 428–434.
7. Ashton A, McCluskey A,Gwinnutt CL,et al.Effect of
rescuer fatigue on performance ofcontinuous external
chestcompressions over 3 min.Resuscitation 2002;55:
151–155.
8. Ochoa FJ, Ramalle-Go´mara E,Lisa V, et al.The effect
of rescuer fatigue on the quality of chest compressions.
Resuscitation 1998; 37: 149–152.
Table 3. Out-of-hospital cardiac arrest device performances.
CPR critical characteristic Expected value direction
Dimensions Less than 350 3 200 3 200 mm
Weight Less than 3.00 kg
Setup procedure Less than 20 s
Safety In accordance to European regulations
Durability 20 years, without intervention
Chest compression depth 0.5 mm
Chest compression rate accuracy 0.1 compression per minute
Manual massage allowed during deployment Yes
Massage types Thoracic,abdominal,and thoracic and abdominal
Exerted force Compression, decompression, and compression and decompressio
Defibrillation without stopping massage Yes
Sensors Depth, rate, compression waveform
Ventilation Yes
Signals Acoustic,visual
Remino et al. 11
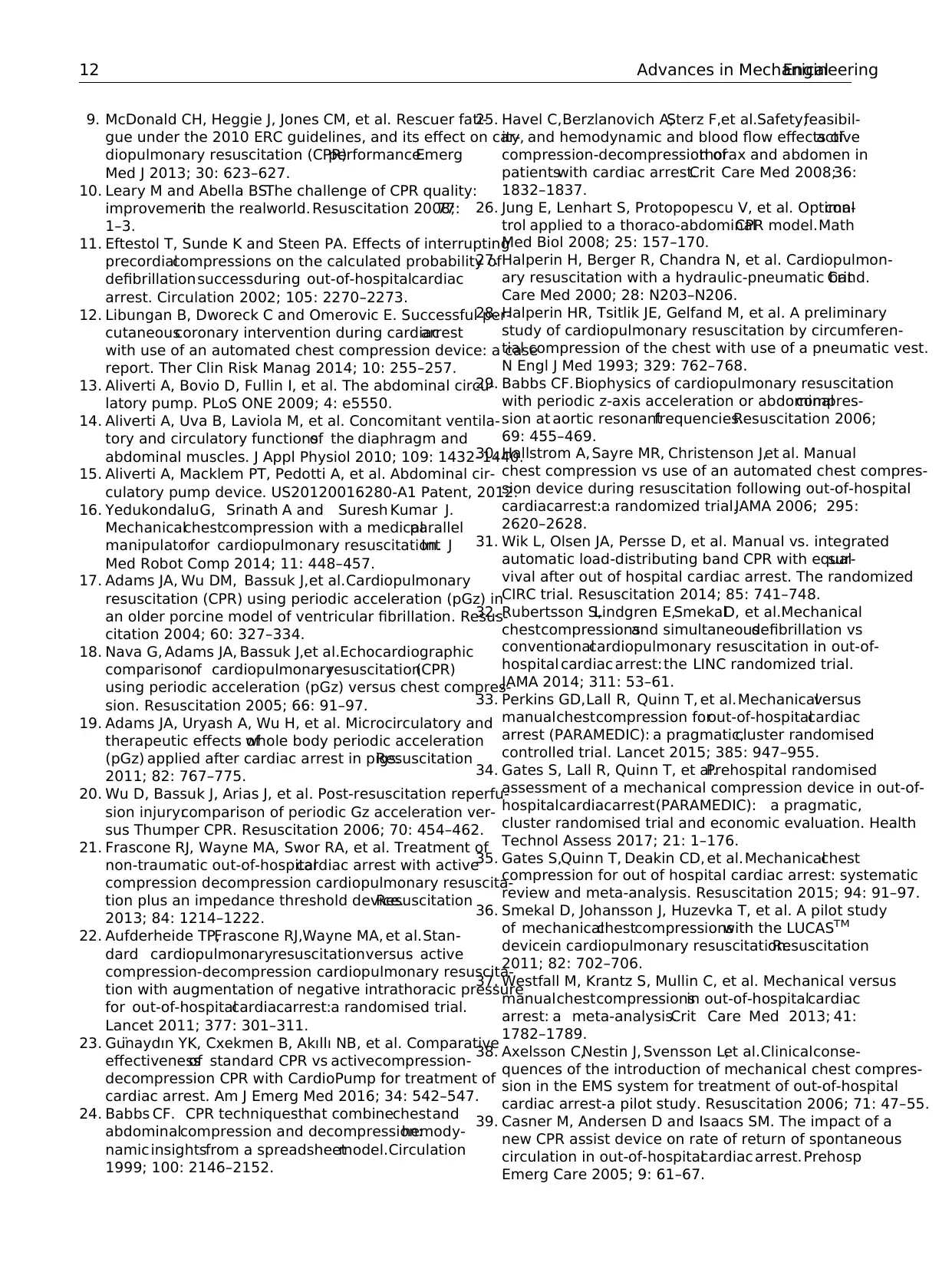
9. McDonald CH, Heggie J, Jones CM, et al. Rescuer fati-
gue under the 2010 ERC guidelines, and its effect on car-
diopulmonary resuscitation (CPR)performance.Emerg
Med J 2013; 30: 623–627.
10. Leary M and Abella BS.The challenge of CPR quality:
improvementin the realworld. Resuscitation 2008;77:
1–3.
11. Eftestol T, Sunde K and Steen PA. Effects of interrupting
precordialcompressions on the calculated probability of
defibrillationsuccessduring out-of-hospitalcardiac
arrest. Circulation 2002; 105: 2270–2273.
12. Libungan B, Dworeck C and Omerovic E. Successful per-
cutaneouscoronary intervention during cardiacarrest
with use of an automated chest compression device: a case
report. Ther Clin Risk Manag 2014; 10: 255–257.
13. Aliverti A, Bovio D, Fullin I, et al. The abdominal circu-
latory pump. PLoS ONE 2009; 4: e5550.
14. Aliverti A, Uva B, Laviola M, et al. Concomitant ventila-
tory and circulatory functionsof the diaphragm and
abdominal muscles. J Appl Physiol 2010; 109: 1432–1440.
15. Aliverti A, Macklem PT, Pedotti A, et al. Abdominal cir-
culatory pump device. US20120016280-A1 Patent, 2012.
16. YedukondaluG, Srinath A and Suresh Kumar J.
Mechanicalchestcompression with a medicalparallel
manipulatorfor cardiopulmonary resuscitation.Int J
Med Robot Comp 2014; 11: 448–457.
17. Adams JA, Wu DM, Bassuk J,et al.Cardiopulmonary
resuscitation (CPR) using periodic acceleration (pGz) in
an older porcine model of ventricular fibrillation. Resus-
citation 2004; 60: 327–334.
18. Nava G, Adams JA, Bassuk J,et al.Echocardiographic
comparisonof cardiopulmonaryresuscitation(CPR)
using periodic acceleration (pGz) versus chest compres-
sion. Resuscitation 2005; 66: 91–97.
19. Adams JA, Uryash A, Wu H, et al. Microcirculatory and
therapeutic effects ofwhole body periodic acceleration
(pGz) applied after cardiac arrest in pigs.Resuscitation
2011; 82: 767–775.
20. Wu D, Bassuk J, Arias J, et al. Post-resuscitation reperfu-
sion injury:comparison of periodic Gz acceleration ver-
sus Thumper CPR. Resuscitation 2006; 70: 454–462.
21. Frascone RJ, Wayne MA, Swor RA, et al. Treatment of
non-traumatic out-of-hospitalcardiac arrest with active
compression decompression cardiopulmonary resuscita-
tion plus an impedance threshold device.Resuscitation
2013; 84: 1214–1222.
22. Aufderheide TP,Frascone RJ,Wayne MA, et al.Stan-
dard cardiopulmonaryresuscitationversus active
compression-decompression cardiopulmonary resuscita-
tion with augmentation of negative intrathoracic pressure
for out-of-hospitalcardiacarrest:a randomised trial.
Lancet 2011; 377: 301–311.
23. Gu¨naydın YK, Cxekmen B, Akıllı NB, et al. Comparative
effectivenessof standard CPR vs activecompression-
decompression CPR with CardioPump for treatment of
cardiac arrest. Am J Emerg Med 2016; 34: 542–547.
24. Babbs CF. CPR techniquesthat combinechestand
abdominalcompression and decompression:hemody-
namic insightsfrom a spreadsheetmodel.Circulation
1999; 100: 2146–2152.
25. Havel C,Berzlanovich A,Sterz F,et al.Safety,feasibil-
ity, and hemodynamic and blood flow effects ofactive
compression-decompression ofthorax and abdomen in
patientswith cardiac arrest.Crit Care Med 2008;36:
1832–1837.
26. Jung E, Lenhart S, Protopopescu V, et al. Optimalcon-
trol applied to a thoraco-abdominalCPR model.Math
Med Biol 2008; 25: 157–170.
27. Halperin H, Berger R, Chandra N, et al. Cardiopulmon-
ary resuscitation with a hydraulic-pneumatic band.Crit
Care Med 2000; 28: N203–N206.
28. Halperin HR, Tsitlik JE, Gelfand M, et al. A preliminary
study of cardiopulmonary resuscitation by circumferen-
tial compression of the chest with use of a pneumatic vest.
N Engl J Med 1993; 329: 762–768.
29. Babbs CF.Biophysics of cardiopulmonary resuscitation
with periodic z-axis acceleration or abdominalcompres-
sion at aortic resonantfrequencies.Resuscitation 2006;
69: 455–469.
30. Hallstrom A, Sayre MR, Christenson J,et al. Manual
chest compression vs use of an automated chest compres-
sion device during resuscitation following out-of-hospital
cardiacarrest:a randomized trial.JAMA 2006; 295:
2620–2628.
31. Wik L, Olsen JA, Persse D, et al. Manual vs. integrated
automatic load-distributing band CPR with equalsur-
vival after out of hospital cardiac arrest. The randomized
CIRC trial. Resuscitation 2014; 85: 741–748.
32. Rubertsson S,Lindgren E,SmekalD, et al.Mechanical
chestcompressionsand simultaneousdefibrillation vs
conventionalcardiopulmonary resuscitation in out-of-
hospital cardiac arrest:the LINC randomized trial.
JAMA 2014; 311: 53–61.
33. Perkins GD,Lall R, Quinn T, et al.Mechanicalversus
manualchestcompression forout-of-hospitalcardiac
arrest (PARAMEDIC): a pragmatic,cluster randomised
controlled trial. Lancet 2015; 385: 947–955.
34. Gates S, Lall R, Quinn T, et al.Prehospital randomised
assessment of a mechanical compression device in out-of-
hospitalcardiacarrest(PARAMEDIC): a pragmatic,
cluster randomised trial and economic evaluation. Health
Technol Assess 2017; 21: 1–176.
35. Gates S,Quinn T, Deakin CD, et al.Mechanicalchest
compression for out of hospital cardiac arrest: systematic
review and meta-analysis. Resuscitation 2015; 94: 91–97.
36. Smekal D, Johansson J, Huzevka T, et al. A pilot study
of mechanicalchestcompressionswith the LUCASTM
devicein cardiopulmonary resuscitation.Resuscitation
2011; 82: 702–706.
37. Westfall M, Krantz S, Mullin C, et al. Mechanical versus
manualchestcompressionsin out-of-hospitalcardiac
arrest: a meta-analysis.Crit Care Med 2013; 41:
1782–1789.
38. Axelsson C,Nestin J, Svensson L,et al.Clinicalconse-
quences of the introduction of mechanical chest compres-
sion in the EMS system for treatment of out-of-hospital
cardiac arrest-a pilot study. Resuscitation 2006; 71: 47–55.
39. Casner M, Andersen D and Isaacs SM. The impact of a
new CPR assist device on rate of return of spontaneous
circulation in out-of-hospitalcardiac arrest. Prehosp
Emerg Care 2005; 9: 61–67.
12 Advances in MechanicalEngineering
gue under the 2010 ERC guidelines, and its effect on car-
diopulmonary resuscitation (CPR)performance.Emerg
Med J 2013; 30: 623–627.
10. Leary M and Abella BS.The challenge of CPR quality:
improvementin the realworld. Resuscitation 2008;77:
1–3.
11. Eftestol T, Sunde K and Steen PA. Effects of interrupting
precordialcompressions on the calculated probability of
defibrillationsuccessduring out-of-hospitalcardiac
arrest. Circulation 2002; 105: 2270–2273.
12. Libungan B, Dworeck C and Omerovic E. Successful per-
cutaneouscoronary intervention during cardiacarrest
with use of an automated chest compression device: a case
report. Ther Clin Risk Manag 2014; 10: 255–257.
13. Aliverti A, Bovio D, Fullin I, et al. The abdominal circu-
latory pump. PLoS ONE 2009; 4: e5550.
14. Aliverti A, Uva B, Laviola M, et al. Concomitant ventila-
tory and circulatory functionsof the diaphragm and
abdominal muscles. J Appl Physiol 2010; 109: 1432–1440.
15. Aliverti A, Macklem PT, Pedotti A, et al. Abdominal cir-
culatory pump device. US20120016280-A1 Patent, 2012.
16. YedukondaluG, Srinath A and Suresh Kumar J.
Mechanicalchestcompression with a medicalparallel
manipulatorfor cardiopulmonary resuscitation.Int J
Med Robot Comp 2014; 11: 448–457.
17. Adams JA, Wu DM, Bassuk J,et al.Cardiopulmonary
resuscitation (CPR) using periodic acceleration (pGz) in
an older porcine model of ventricular fibrillation. Resus-
citation 2004; 60: 327–334.
18. Nava G, Adams JA, Bassuk J,et al.Echocardiographic
comparisonof cardiopulmonaryresuscitation(CPR)
using periodic acceleration (pGz) versus chest compres-
sion. Resuscitation 2005; 66: 91–97.
19. Adams JA, Uryash A, Wu H, et al. Microcirculatory and
therapeutic effects ofwhole body periodic acceleration
(pGz) applied after cardiac arrest in pigs.Resuscitation
2011; 82: 767–775.
20. Wu D, Bassuk J, Arias J, et al. Post-resuscitation reperfu-
sion injury:comparison of periodic Gz acceleration ver-
sus Thumper CPR. Resuscitation 2006; 70: 454–462.
21. Frascone RJ, Wayne MA, Swor RA, et al. Treatment of
non-traumatic out-of-hospitalcardiac arrest with active
compression decompression cardiopulmonary resuscita-
tion plus an impedance threshold device.Resuscitation
2013; 84: 1214–1222.
22. Aufderheide TP,Frascone RJ,Wayne MA, et al.Stan-
dard cardiopulmonaryresuscitationversus active
compression-decompression cardiopulmonary resuscita-
tion with augmentation of negative intrathoracic pressure
for out-of-hospitalcardiacarrest:a randomised trial.
Lancet 2011; 377: 301–311.
23. Gu¨naydın YK, Cxekmen B, Akıllı NB, et al. Comparative
effectivenessof standard CPR vs activecompression-
decompression CPR with CardioPump for treatment of
cardiac arrest. Am J Emerg Med 2016; 34: 542–547.
24. Babbs CF. CPR techniquesthat combinechestand
abdominalcompression and decompression:hemody-
namic insightsfrom a spreadsheetmodel.Circulation
1999; 100: 2146–2152.
25. Havel C,Berzlanovich A,Sterz F,et al.Safety,feasibil-
ity, and hemodynamic and blood flow effects ofactive
compression-decompression ofthorax and abdomen in
patientswith cardiac arrest.Crit Care Med 2008;36:
1832–1837.
26. Jung E, Lenhart S, Protopopescu V, et al. Optimalcon-
trol applied to a thoraco-abdominalCPR model.Math
Med Biol 2008; 25: 157–170.
27. Halperin H, Berger R, Chandra N, et al. Cardiopulmon-
ary resuscitation with a hydraulic-pneumatic band.Crit
Care Med 2000; 28: N203–N206.
28. Halperin HR, Tsitlik JE, Gelfand M, et al. A preliminary
study of cardiopulmonary resuscitation by circumferen-
tial compression of the chest with use of a pneumatic vest.
N Engl J Med 1993; 329: 762–768.
29. Babbs CF.Biophysics of cardiopulmonary resuscitation
with periodic z-axis acceleration or abdominalcompres-
sion at aortic resonantfrequencies.Resuscitation 2006;
69: 455–469.
30. Hallstrom A, Sayre MR, Christenson J,et al. Manual
chest compression vs use of an automated chest compres-
sion device during resuscitation following out-of-hospital
cardiacarrest:a randomized trial.JAMA 2006; 295:
2620–2628.
31. Wik L, Olsen JA, Persse D, et al. Manual vs. integrated
automatic load-distributing band CPR with equalsur-
vival after out of hospital cardiac arrest. The randomized
CIRC trial. Resuscitation 2014; 85: 741–748.
32. Rubertsson S,Lindgren E,SmekalD, et al.Mechanical
chestcompressionsand simultaneousdefibrillation vs
conventionalcardiopulmonary resuscitation in out-of-
hospital cardiac arrest:the LINC randomized trial.
JAMA 2014; 311: 53–61.
33. Perkins GD,Lall R, Quinn T, et al.Mechanicalversus
manualchestcompression forout-of-hospitalcardiac
arrest (PARAMEDIC): a pragmatic,cluster randomised
controlled trial. Lancet 2015; 385: 947–955.
34. Gates S, Lall R, Quinn T, et al.Prehospital randomised
assessment of a mechanical compression device in out-of-
hospitalcardiacarrest(PARAMEDIC): a pragmatic,
cluster randomised trial and economic evaluation. Health
Technol Assess 2017; 21: 1–176.
35. Gates S,Quinn T, Deakin CD, et al.Mechanicalchest
compression for out of hospital cardiac arrest: systematic
review and meta-analysis. Resuscitation 2015; 94: 91–97.
36. Smekal D, Johansson J, Huzevka T, et al. A pilot study
of mechanicalchestcompressionswith the LUCASTM
devicein cardiopulmonary resuscitation.Resuscitation
2011; 82: 702–706.
37. Westfall M, Krantz S, Mullin C, et al. Mechanical versus
manualchestcompressionsin out-of-hospitalcardiac
arrest: a meta-analysis.Crit Care Med 2013; 41:
1782–1789.
38. Axelsson C,Nestin J, Svensson L,et al.Clinicalconse-
quences of the introduction of mechanical chest compres-
sion in the EMS system for treatment of out-of-hospital
cardiac arrest-a pilot study. Resuscitation 2006; 71: 47–55.
39. Casner M, Andersen D and Isaacs SM. The impact of a
new CPR assist device on rate of return of spontaneous
circulation in out-of-hospitalcardiac arrest. Prehosp
Emerg Care 2005; 9: 61–67.
12 Advances in MechanicalEngineering
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
