Mechanical versus manual chest compressions for cardiac arrest: a systematic review and meta-analysis
Added on 2023-06-15
10 Pages6758 Words122 Views
O R I G I N A L R E S E A R C H Open Access
Mechanical versus manual chest
compressions for cardiac arrest: a
systematic review and meta-analysis
Hui Li 1†, Dongping Wang 2†, Yi Yu1
, Xiang Zhao1 and Xiaoli Jing 1*
Abstract
Background: The aim of this paper was to conduct a systematic review of the published literatures comparing the
use of mechanical chest compression device and manual chest compression during cardiac arrest (CA) with respect
to short-term survival outcomes and neurological function.
Methods: Databases including MEDLINE, EMBASE, Web of Science and the ClinicalTrials.gov registry were
systematically searched. Further references were gathered from cross-references from articles by handsearch. The
inclusion criteria for this review must be human prospective controlled studies of adult CA. Random effects models
were used to assess the risk ratios and 95 % confidence intervals for return of spontaneous circulation (ROSC),
survival to admission and discharge, and neurological function.
Results: Twelve trials (9 out-of-hospital and 3 in-hospital studies), involving 11,162 participants, were included in
the review. The results of this meta-analysis indicated no differences were found in Cerebral Performance Category
(CPC) scores, survival to hospital admission and survival to discharge between manual cardiopulmonary
resuscitation (CPR) and mechanical CPR for out-of-hospital CA (OHCA) patients. The data on achieving ROSC in both
of in-hospital and out-of-hospital setting suggested poor application of the mechanical device (RR 0.71, [95 % CI,
0.53, 0.97] and 0.87 [95 % CI, 0.81, 0.94], respectively). OHCA patients receiving manual resuscitation were more
likely to attain ROSC compared with load-distributing bands chest compression device (RR 0.88, [95 % CI, 0.80,
0.96]). The in-hospital studies suggested increased relative harm with mechanical compressions for ratio of survival
to hospital discharge (RR 0.54, [95 % CI 0.29, 0.98]). However, the results were not statistically significant between
different kinds of mechanical chest compression devices and manual resuscitation in survival to admission,
discharge and CPC scores for OHCA patients and survival to discharge for in-hospital CA patients.
Conclusions: The ability to achieve ROSC with mechanical devise was inferior to manual chest compression during
resuscitation. The use of mechanical chest compression cannot be recommended as a replacement for manual CPR,
but rather a supplemental treatment in an overall strategy for treating CA patients.
Keywords: Cardiac arrest, Cardiopulmonary resuscitation, Device, Meta-analysis
* Correspondence: jing-xl@163.com
†Equal contributors
1
Department of Emergency, The First Affiliated Hospital of Sun Yat-Sen
University, 58 Zhongshan 2nd Road, Guangzhou, Guangdong 510080, China
Full list of author information is available at the end of the article
© 2016 Li et al. Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International
License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any
medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative
Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://
creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Li et al. Scandinavian Journal of Trauma, Resuscitation
and Emergency Medicine (2016) 24:10
DOI 10.1186/s13049-016-0202-y
Mechanical versus manual chest
compressions for cardiac arrest: a
systematic review and meta-analysis
Hui Li 1†, Dongping Wang 2†, Yi Yu1
, Xiang Zhao1 and Xiaoli Jing 1*
Abstract
Background: The aim of this paper was to conduct a systematic review of the published literatures comparing the
use of mechanical chest compression device and manual chest compression during cardiac arrest (CA) with respect
to short-term survival outcomes and neurological function.
Methods: Databases including MEDLINE, EMBASE, Web of Science and the ClinicalTrials.gov registry were
systematically searched. Further references were gathered from cross-references from articles by handsearch. The
inclusion criteria for this review must be human prospective controlled studies of adult CA. Random effects models
were used to assess the risk ratios and 95 % confidence intervals for return of spontaneous circulation (ROSC),
survival to admission and discharge, and neurological function.
Results: Twelve trials (9 out-of-hospital and 3 in-hospital studies), involving 11,162 participants, were included in
the review. The results of this meta-analysis indicated no differences were found in Cerebral Performance Category
(CPC) scores, survival to hospital admission and survival to discharge between manual cardiopulmonary
resuscitation (CPR) and mechanical CPR for out-of-hospital CA (OHCA) patients. The data on achieving ROSC in both
of in-hospital and out-of-hospital setting suggested poor application of the mechanical device (RR 0.71, [95 % CI,
0.53, 0.97] and 0.87 [95 % CI, 0.81, 0.94], respectively). OHCA patients receiving manual resuscitation were more
likely to attain ROSC compared with load-distributing bands chest compression device (RR 0.88, [95 % CI, 0.80,
0.96]). The in-hospital studies suggested increased relative harm with mechanical compressions for ratio of survival
to hospital discharge (RR 0.54, [95 % CI 0.29, 0.98]). However, the results were not statistically significant between
different kinds of mechanical chest compression devices and manual resuscitation in survival to admission,
discharge and CPC scores for OHCA patients and survival to discharge for in-hospital CA patients.
Conclusions: The ability to achieve ROSC with mechanical devise was inferior to manual chest compression during
resuscitation. The use of mechanical chest compression cannot be recommended as a replacement for manual CPR,
but rather a supplemental treatment in an overall strategy for treating CA patients.
Keywords: Cardiac arrest, Cardiopulmonary resuscitation, Device, Meta-analysis
* Correspondence: jing-xl@163.com
†Equal contributors
1
Department of Emergency, The First Affiliated Hospital of Sun Yat-Sen
University, 58 Zhongshan 2nd Road, Guangzhou, Guangdong 510080, China
Full list of author information is available at the end of the article
© 2016 Li et al. Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International
License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any
medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative
Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://
creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Li et al. Scandinavian Journal of Trauma, Resuscitation
and Emergency Medicine (2016) 24:10
DOI 10.1186/s13049-016-0202-y
Background
Sudden cardiac arrest (CA) occurs when someone’s
heart stops beating unexpectedly. Minimally interrupted,
regular and appropriate cardiopulmonary resuscitation
(CPR) can keep blood flowing to the victim’s vital organs
while the heart is not pumping [1–4]. Unfortunately, even
healthcare professionals have difficulty in performing
effective CPR persistently, especially in a moving vehicle
and in situations of prolonged cardiac arrest [5–8]. Chest-
compressions often are too shallow, hands-off time is too
long, chest compression rate is less than 90/min, and
rescuers fatigue over time [9–12].
Machines have been developed to take over this chest
pumping action using pneumatically driven or load-dis-
tributing bands (LDBs) mechanisms, because the machines
do not pause or get tired, and deliver uninterrupted chest-
compressions with a predefined depth and rate [13]. Some
studies using those machines for chest compressions have
shown that they could achieve intrathoracic pressures
higher, improve coronary and systemic perfusion pressures
and flows compared with manual CPR in animal models
and in a small number of terminally ill patients [14–16].
Some data from human observational studies suggested
that mechanical chest compressions might be superior to
manual chest compressions in cardiac arrest [16–19]. A
few recent meta-analyses could not eliminate all the
doubts at this regards because of the paucity of data avail-
able and the presence of confounding factors [20–22]. We
aimed to investigate which method of chest compression
(applying the traditional manual compression vs. using a
machine) would result in more lives saved.
Methods
Types of studies
A meta-analysis was performed to compare any type of
mechanical chest compression device with manual chest
compression in the management of patients suffered
from CA in out-of-hospital and in-hospital settings.
Human prospective randomized controlled studies com-
paring compressions delivered via any type of powered,
automatic mechanical compression device versus man-
ual compression were considered for inclusion. Studies
explicitly including patients with CA caused by drown-
ing, hypothermia and toxic substances were excluded.
Types of outcome measures
The primary outcome for this meta-analysis was return of
spontaneous circulation (ROSC) defined as spontaneous
palpable pulse. Secondary outcomes included survival to
hospital admission for out-of-hospital cardiac arrest
(OHCA) patients only, survival to hospital discharge and
good neurological outcome after hospital discharge, with
Cerebral Performance Category (CPC) scores one or two
for both in-hospital and out-of-hospital patients.
Electronic searches
A search strategy was pursued, using the following search
terms: “mechanical”, “manual”, “chest compression” and
“cardiopulmonary resuscitation”. Searches were conducted
in MEDLINE (1946 to 31 August 2015), EMBASE (1950
to 31 August 2015), Web of Science (including web of
science Core Collection, current content connect, BIOSIS
Previews, Chinese Science Citation Database and SciELO
Citation Index, from the start to 31 August 2015) and the
ClinicalTrials.gov registry (on 31 August 2015). We hand-
searched bibliographies of included papers. The search
was inclusive of studies in any language.
Data collection and analysis
Data selection and data extracted were performed
among pairs of independent reviewers, and the results
were confirmed by a third review author. Discrepancies
were discussed and adjudicated by the team consensus.
In reporting the results of this systematic review, the au-
thors have followed the recommended guidelines from
the Quality of Reporting of Meta-Analysis (QUOROM)
Statement.
Statistical analyses
Data were checked and entered into the Stata 12.0 (Stata
Corp., College Station, TX) database for further analysis.
Using a random-effects model, we calculated the risk
ratios (RR) and 95 % confidence intervals (CI) for ROSC,
arrival to hospital with a spontaneous palpable pulse,
survival at discharge and CPC score. The presence of
heterogeneity between trials was assessed using the I2
statistics. Funnel plots and Egger’s regression test were
used to assess the potential for reporting bias.
Results
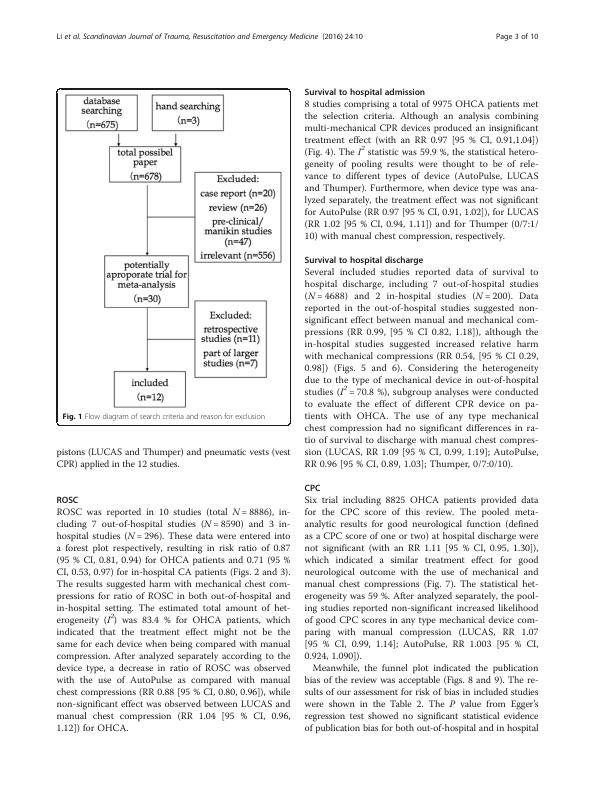
Results of the search
In the original review, the comprehensive search identi-
fied 678 citations (MEDLINE 118, EMBASE 94, Web of
Science 444, clinicaltrials.gov 19, handsearch of references
of included papers 3). Two independent review authors
reviewed 678 citations by titles; possible citations were
selected for review by abstract. After review by abstract,
potential relevant were identified and reviewed by full
article. After exclusion, 12 studies were found meeting the
inclusion criteria, included 9 out-of-hospital studies and 3
in-hospital studies [23–34]. The process was detailed in a
PRISMA flow diagram (Fig. 1). Trial characteristics were
summarized in the Table 1. Eleven of the articles were
published in English and one was Chinese, comprising
data from eight countries. Six studies were multiple-
center trials, whereas the others were conducted in one
single center. Three different mechanisms of mechanical
chest compression devices including LDBs (AutoPulse),
Li et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2016) 24:10 Page 2 of 10
Sudden cardiac arrest (CA) occurs when someone’s
heart stops beating unexpectedly. Minimally interrupted,
regular and appropriate cardiopulmonary resuscitation
(CPR) can keep blood flowing to the victim’s vital organs
while the heart is not pumping [1–4]. Unfortunately, even
healthcare professionals have difficulty in performing
effective CPR persistently, especially in a moving vehicle
and in situations of prolonged cardiac arrest [5–8]. Chest-
compressions often are too shallow, hands-off time is too
long, chest compression rate is less than 90/min, and
rescuers fatigue over time [9–12].
Machines have been developed to take over this chest
pumping action using pneumatically driven or load-dis-
tributing bands (LDBs) mechanisms, because the machines
do not pause or get tired, and deliver uninterrupted chest-
compressions with a predefined depth and rate [13]. Some
studies using those machines for chest compressions have
shown that they could achieve intrathoracic pressures
higher, improve coronary and systemic perfusion pressures
and flows compared with manual CPR in animal models
and in a small number of terminally ill patients [14–16].
Some data from human observational studies suggested
that mechanical chest compressions might be superior to
manual chest compressions in cardiac arrest [16–19]. A
few recent meta-analyses could not eliminate all the
doubts at this regards because of the paucity of data avail-
able and the presence of confounding factors [20–22]. We
aimed to investigate which method of chest compression
(applying the traditional manual compression vs. using a
machine) would result in more lives saved.
Methods
Types of studies
A meta-analysis was performed to compare any type of
mechanical chest compression device with manual chest
compression in the management of patients suffered
from CA in out-of-hospital and in-hospital settings.
Human prospective randomized controlled studies com-
paring compressions delivered via any type of powered,
automatic mechanical compression device versus man-
ual compression were considered for inclusion. Studies
explicitly including patients with CA caused by drown-
ing, hypothermia and toxic substances were excluded.
Types of outcome measures
The primary outcome for this meta-analysis was return of
spontaneous circulation (ROSC) defined as spontaneous
palpable pulse. Secondary outcomes included survival to
hospital admission for out-of-hospital cardiac arrest
(OHCA) patients only, survival to hospital discharge and
good neurological outcome after hospital discharge, with
Cerebral Performance Category (CPC) scores one or two
for both in-hospital and out-of-hospital patients.
Electronic searches
A search strategy was pursued, using the following search
terms: “mechanical”, “manual”, “chest compression” and
“cardiopulmonary resuscitation”. Searches were conducted
in MEDLINE (1946 to 31 August 2015), EMBASE (1950
to 31 August 2015), Web of Science (including web of
science Core Collection, current content connect, BIOSIS
Previews, Chinese Science Citation Database and SciELO
Citation Index, from the start to 31 August 2015) and the
ClinicalTrials.gov registry (on 31 August 2015). We hand-
searched bibliographies of included papers. The search
was inclusive of studies in any language.
Data collection and analysis
Data selection and data extracted were performed
among pairs of independent reviewers, and the results
were confirmed by a third review author. Discrepancies
were discussed and adjudicated by the team consensus.
In reporting the results of this systematic review, the au-
thors have followed the recommended guidelines from
the Quality of Reporting of Meta-Analysis (QUOROM)
Statement.
Statistical analyses
Data were checked and entered into the Stata 12.0 (Stata
Corp., College Station, TX) database for further analysis.
Using a random-effects model, we calculated the risk
ratios (RR) and 95 % confidence intervals (CI) for ROSC,
arrival to hospital with a spontaneous palpable pulse,
survival at discharge and CPC score. The presence of
heterogeneity between trials was assessed using the I2
statistics. Funnel plots and Egger’s regression test were
used to assess the potential for reporting bias.
Results
Results of the search
In the original review, the comprehensive search identi-
fied 678 citations (MEDLINE 118, EMBASE 94, Web of
Science 444, clinicaltrials.gov 19, handsearch of references
of included papers 3). Two independent review authors
reviewed 678 citations by titles; possible citations were
selected for review by abstract. After review by abstract,
potential relevant were identified and reviewed by full
article. After exclusion, 12 studies were found meeting the
inclusion criteria, included 9 out-of-hospital studies and 3
in-hospital studies [23–34]. The process was detailed in a
PRISMA flow diagram (Fig. 1). Trial characteristics were
summarized in the Table 1. Eleven of the articles were
published in English and one was Chinese, comprising
data from eight countries. Six studies were multiple-
center trials, whereas the others were conducted in one
single center. Three different mechanisms of mechanical
chest compression devices including LDBs (AutoPulse),
Li et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2016) 24:10 Page 2 of 10

pistons (LUCAS and Thumper) and pneumatic vests (vest
CPR) applied in the 12 studies.
ROSC
ROSC was reported in 10 studies (total N = 8886), in-
cluding 7 out-of-hospital studies (N = 8590) and 3 in-
hospital studies (N = 296). These data were entered into
a forest plot respectively, resulting in risk ratio of 0.87
(95 % CI, 0.81, 0.94) for OHCA patients and 0.71 (95 %
CI, 0.53, 0.97) for in-hospital CA patients (Figs. 2 and 3).
The results suggested harm with mechanical chest com-
pressions for ratio of ROSC in both out-of-hospital and
in-hospital setting. The estimated total amount of het-
erogeneity (I 2) was 83.4 % for OHCA patients, which
indicated that the treatment effect might not be the
same for each device when being compared with manual
compression. After analyzed separately according to the
device type, a decrease in ratio of ROSC was observed
with the use of AutoPulse as compared with manual
chest compressions (RR 0.88 [95 % CI, 0.80, 0.96]), while
non-significant effect was observed between LUCAS and
manual chest compression (RR 1.04 [95 % CI, 0.96,
1.12]) for OHCA.
Survival to hospital admission
8 studies comprising a total of 9975 OHCA patients met
the selection criteria. Although an analysis combining
multi-mechanical CPR devices produced an insignificant
treatment effect (with an RR 0.97 [95 % CI, 0.91,1.04])
(Fig. 4). The I2 statistic was 59.9 %, the statistical hetero-
geneity of pooling results were thought to be of rele-
vance to different types of device (AutoPulse, LUCAS
and Thumper). Furthermore, when device type was ana-
lyzed separately, the treatment effect was not significant
for AutoPulse (RR 0.97 [95 % CI, 0.91, 1.02]), for LUCAS
(RR 1.02 [95 % CI, 0.94, 1.11]) and for Thumper (0/7:1/
10) with manual chest compression, respectively.
Survival to hospital discharge
Several included studies reported data of survival to
hospital discharge, including 7 out-of-hospital studies
(N = 4688) and 2 in-hospital studies (N = 200). Data
reported in the out-of-hospital studies suggested non-
significant effect between manual and mechanical com-
pressions (RR 0.99, [95 % CI 0.82, 1.18]), although the
in-hospital studies suggested increased relative harm
with mechanical compressions (RR 0.54, [95 % CI 0.29,
0.98]) (Figs. 5 and 6). Considering the heterogeneity
due to the type of mechanical device in out-of-hospital
studies (I 2 = 70.8 %), subgroup analyses were conducted
to evaluate the effect of different CPR device on pa-
tients with OHCA. The use of any type mechanical
chest compression had no significant differences in ra-
tio of survival to discharge with manual chest compres-
sion (LUCAS, RR 1.09 [95 % CI, 0.99, 1.19]; AutoPulse,
RR 0.96 [95 % CI, 0.89, 1.03]; Thumper, 0/7:0/10).
CPC
Six trial including 8825 OHCA patients provided data
for the CPC score of this review. The pooled meta-
analytic results for good neurological function (defined
as a CPC score of one or two) at hospital discharge were
not significant (with an RR 1.11 [95 % CI, 0.95, 1.30]),
which indicated a similar treatment effect for good
neurological outcome with the use of mechanical and
manual chest compressions (Fig. 7). The statistical het-
erogeneity was 59 %. After analyzed separately, the pool-
ing studies reported non-significant increased likelihood
of good CPC scores in any type mechanical device com-
paring with manual compression (LUCAS, RR 1.07
[95 % CI, 0.99, 1.14]; AutoPulse, RR 1.003 [95 % CI,
0.924, 1.090]).
Meanwhile, the funnel plot indicated the publication
bias of the review was acceptable (Figs. 8 and 9). The re-
sults of our assessment for risk of bias in included studies
were shown in the Table 2. The P value from Egger’s
regression test showed no significant statistical evidence
of publication bias for both out-of-hospital and in hospital
Fig. 1 Flow diagram of search criteria and reason for exclusion
Li et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2016) 24:10 Page 3 of 10
CPR) applied in the 12 studies.
ROSC
ROSC was reported in 10 studies (total N = 8886), in-
cluding 7 out-of-hospital studies (N = 8590) and 3 in-
hospital studies (N = 296). These data were entered into
a forest plot respectively, resulting in risk ratio of 0.87
(95 % CI, 0.81, 0.94) for OHCA patients and 0.71 (95 %
CI, 0.53, 0.97) for in-hospital CA patients (Figs. 2 and 3).
The results suggested harm with mechanical chest com-
pressions for ratio of ROSC in both out-of-hospital and
in-hospital setting. The estimated total amount of het-
erogeneity (I 2) was 83.4 % for OHCA patients, which
indicated that the treatment effect might not be the
same for each device when being compared with manual
compression. After analyzed separately according to the
device type, a decrease in ratio of ROSC was observed
with the use of AutoPulse as compared with manual
chest compressions (RR 0.88 [95 % CI, 0.80, 0.96]), while
non-significant effect was observed between LUCAS and
manual chest compression (RR 1.04 [95 % CI, 0.96,
1.12]) for OHCA.
Survival to hospital admission
8 studies comprising a total of 9975 OHCA patients met
the selection criteria. Although an analysis combining
multi-mechanical CPR devices produced an insignificant
treatment effect (with an RR 0.97 [95 % CI, 0.91,1.04])
(Fig. 4). The I2 statistic was 59.9 %, the statistical hetero-
geneity of pooling results were thought to be of rele-
vance to different types of device (AutoPulse, LUCAS
and Thumper). Furthermore, when device type was ana-
lyzed separately, the treatment effect was not significant
for AutoPulse (RR 0.97 [95 % CI, 0.91, 1.02]), for LUCAS
(RR 1.02 [95 % CI, 0.94, 1.11]) and for Thumper (0/7:1/
10) with manual chest compression, respectively.
Survival to hospital discharge
Several included studies reported data of survival to
hospital discharge, including 7 out-of-hospital studies
(N = 4688) and 2 in-hospital studies (N = 200). Data
reported in the out-of-hospital studies suggested non-
significant effect between manual and mechanical com-
pressions (RR 0.99, [95 % CI 0.82, 1.18]), although the
in-hospital studies suggested increased relative harm
with mechanical compressions (RR 0.54, [95 % CI 0.29,
0.98]) (Figs. 5 and 6). Considering the heterogeneity
due to the type of mechanical device in out-of-hospital
studies (I 2 = 70.8 %), subgroup analyses were conducted
to evaluate the effect of different CPR device on pa-
tients with OHCA. The use of any type mechanical
chest compression had no significant differences in ra-
tio of survival to discharge with manual chest compres-
sion (LUCAS, RR 1.09 [95 % CI, 0.99, 1.19]; AutoPulse,
RR 0.96 [95 % CI, 0.89, 1.03]; Thumper, 0/7:0/10).
CPC
Six trial including 8825 OHCA patients provided data
for the CPC score of this review. The pooled meta-
analytic results for good neurological function (defined
as a CPC score of one or two) at hospital discharge were
not significant (with an RR 1.11 [95 % CI, 0.95, 1.30]),
which indicated a similar treatment effect for good
neurological outcome with the use of mechanical and
manual chest compressions (Fig. 7). The statistical het-
erogeneity was 59 %. After analyzed separately, the pool-
ing studies reported non-significant increased likelihood
of good CPC scores in any type mechanical device com-
paring with manual compression (LUCAS, RR 1.07
[95 % CI, 0.99, 1.14]; AutoPulse, RR 1.003 [95 % CI,
0.924, 1.090]).
Meanwhile, the funnel plot indicated the publication
bias of the review was acceptable (Figs. 8 and 9). The re-
sults of our assessment for risk of bias in included studies
were shown in the Table 2. The P value from Egger’s
regression test showed no significant statistical evidence
of publication bias for both out-of-hospital and in hospital
Fig. 1 Flow diagram of search criteria and reason for exclusion
Li et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2016) 24:10 Page 3 of 10
End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Automatic and manual devices for cardiopulmonary resuscitation: A reviewlg...
|14
|11785
|493
Mechanical versus manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled triallg...
|12
|11588
|127
Safety with Mechanical Chest Compressions in CPR: Clinical studies with the LUCAS™ devicelg...
|70
|21472
|64
Evidence Based Research Nursinglg...
|11
|2847
|61
LUCAS-2 Mechanical CPR in Front-Line Emergency Response Vehicles: A Medical Case Studylg...
|6
|1491
|265
Percutaneous noncoronary interventions during continuous mechanical chest compression with the LUCAS-2 devicelg...
|4
|1909
|361
