Report: Type 2 Diabetes - Assessment, Complications, and Control
VerifiedAdded on 2019/12/04
|8
|2896
|212
Report
AI Summary
This report delves into Type 2 diabetes, exploring key areas for initial assessment, diagnostic tests, and the differences between Type 1 and Type 2 diabetes. It outlines the causes and pathophysiology of both types, followed by a discussion of macrovascular (heart disease, peripheral arterial disease) and microvascular complications (retinopathy, nephropathy, neuropathy). The report details tests used to screen for these microvascular complications and assesses ongoing levels of glycemic control, including self-monitoring blood glucose and HbA1c tests. Finally, it examines pharmacological strategies for improving glycemic control in patients with Type 2 diabetes. The report is contributed by a student and available on Desklib, a platform offering AI-based study tools for students.
Diabetes
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Table of Contents
INTRODUCTION ...............................................................................................................................3
Q 1 Key areas for initial assessment ...............................................................................................3
Test to confirm the diagnosis of Diabetes........................................................................................3
Q 2 Description of Type 1 and Type 2 Diabetes..............................................................................4
Difference in clinical presentation of type 1 and type 2 diabetes....................................................5
Q 3 Two macro-vascular and three microvascular complications of diabetes.................................5
Test used to screen three microvascular complications...................................................................6
Q 4 Assess the ongoing levels of glycaemic control in patient with diabetes type 2 .....................7
Pharmacological strategies for improving glycaemic controls........................................................7
CONCLUSION....................................................................................................................................7
REFERENCES.....................................................................................................................................9
INTRODUCTION ...............................................................................................................................3
Q 1 Key areas for initial assessment ...............................................................................................3
Test to confirm the diagnosis of Diabetes........................................................................................3
Q 2 Description of Type 1 and Type 2 Diabetes..............................................................................4
Difference in clinical presentation of type 1 and type 2 diabetes....................................................5
Q 3 Two macro-vascular and three microvascular complications of diabetes.................................5
Test used to screen three microvascular complications...................................................................6
Q 4 Assess the ongoing levels of glycaemic control in patient with diabetes type 2 .....................7
Pharmacological strategies for improving glycaemic controls........................................................7
CONCLUSION....................................................................................................................................7
REFERENCES.....................................................................................................................................9
INTRODUCTION
Diabetes mellitus or type 2 is a disorder that is characterized by increase in blood sugar
levels, resistance in insulin and lack of insulin in body (Armstrong, Harskamp and Armstrong,
2013). Common symptoms of diabetes mellitus 2 are increase in thirst level, frequency of urination
and unreasoning loss in body weight of an individual. Other symptoms include increased hunger,
feeling of fatigue and tiredness throughout the day and long time for healing of injuries. These
symptoms can be controlled but the adversities due to this metabolic disorder has long term
complication on a person. Long term complications in case of type 2 diabetes may include
cardiovascular disorders, strokes, retinopathy, nephrological disorders and blindness in some cases
(Aschner, Horton and Skyler, 2010).
The overall report will be based on type 2 diabetes that is caused due to obesity and lack of
physical activity. The study will discuss key areas which are required for initial assessment. The
report will also discuss test required to diagnose diabetes in patients. Further, causes and
pathophysiology of both type 1 and type 2 diabetes will be explored. Lastly the report will include
two macro and micro complications associated with diabetes.
Q 1 Key areas for initial assessment
Jazminder has recently visited a surgical department and is concerned that she may
encounter diabetes because her sister has been diagnosed with diabetes and she has increased risk of
developing the same condition. There are several key areas that needs to be assessed concerning
diabetes.
For confirming whether Jazminder has diabetes or not it is very necessary to carry different
types of test so that results inferred from them can justify whether diabetes is present or not
(Asija, 2014).
Urine sample will be collected which is the initial criteria for assessment of presence of
diabetes. On normal evaluation urine samples do not contain glucose levels but if Jazminder
has encountered diabetes then the urine samples will detect the presence of glucose in it.
Further if urine samples have detected glucose then a specialised blood test is performed that
confirms the presence of diabetes. The test is generally known as glycated haemoglobin
(HbA1c) which measures the glucose levels of previous months also (Boström and et.al,
2014).
Test to confirm the diagnosis of Diabetes.
Based on the current guidelines and there are several tests that will confirm diagnosis of
diabetes in Jazminder. Test are discussed below.
Random blood sugar test: In this type of blood testing a blood sample is recorded at a random time
Diabetes mellitus or type 2 is a disorder that is characterized by increase in blood sugar
levels, resistance in insulin and lack of insulin in body (Armstrong, Harskamp and Armstrong,
2013). Common symptoms of diabetes mellitus 2 are increase in thirst level, frequency of urination
and unreasoning loss in body weight of an individual. Other symptoms include increased hunger,
feeling of fatigue and tiredness throughout the day and long time for healing of injuries. These
symptoms can be controlled but the adversities due to this metabolic disorder has long term
complication on a person. Long term complications in case of type 2 diabetes may include
cardiovascular disorders, strokes, retinopathy, nephrological disorders and blindness in some cases
(Aschner, Horton and Skyler, 2010).
The overall report will be based on type 2 diabetes that is caused due to obesity and lack of
physical activity. The study will discuss key areas which are required for initial assessment. The
report will also discuss test required to diagnose diabetes in patients. Further, causes and
pathophysiology of both type 1 and type 2 diabetes will be explored. Lastly the report will include
two macro and micro complications associated with diabetes.
Q 1 Key areas for initial assessment
Jazminder has recently visited a surgical department and is concerned that she may
encounter diabetes because her sister has been diagnosed with diabetes and she has increased risk of
developing the same condition. There are several key areas that needs to be assessed concerning
diabetes.
For confirming whether Jazminder has diabetes or not it is very necessary to carry different
types of test so that results inferred from them can justify whether diabetes is present or not
(Asija, 2014).
Urine sample will be collected which is the initial criteria for assessment of presence of
diabetes. On normal evaluation urine samples do not contain glucose levels but if Jazminder
has encountered diabetes then the urine samples will detect the presence of glucose in it.
Further if urine samples have detected glucose then a specialised blood test is performed that
confirms the presence of diabetes. The test is generally known as glycated haemoglobin
(HbA1c) which measures the glucose levels of previous months also (Boström and et.al,
2014).
Test to confirm the diagnosis of Diabetes.
Based on the current guidelines and there are several tests that will confirm diagnosis of
diabetes in Jazminder. Test are discussed below.
Random blood sugar test: In this type of blood testing a blood sample is recorded at a random time
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
irrespective of when the patient took her last meal (Buijsse and et.al, 2011). If random sample
detects level of 200 milligrams per decilitre (mg/dL) or 11.1 millimoles per liter (mmol/L) then it is
suggested that Jazminder is suffering from diabetes.
Fasting blood sugar test: A blood sample is taken after the fasting process of overnight. If the
blood records a minimum of 100 mg/dL (5.6 mmol/L) then it is considered to be normal. If it
records 100 to 125 mg/dL (5.6 to 6.9 mmol/L) then she can be pre-diabetic but it records more than
126 mg/dL (7 mmol/L) then it is considered that she is suffering from diabetes (Carnethon and et.al,
2012).
Oral glucose tolerance test: Blood sugar levels after fasting and intake of sugary liquid is tested
for next two hours. If the reading is less than (7.8 mmol/L) then it is normal. If it is 200 mg/dL (11.1
mmol/L) or more than this value then the patient is suffering from diabetes (Armstrong, Harskamp
and Armstrong, 2013).
Q 2 Description of Type 1 and Type 2 Diabetes.
Type 1 Diabetes
Type 1 diabetes is generally caused when a person's immune system destroys the cells of
pancreas known as beta cells (Chalishajar and Stanford, 2014). These beta cells are responsible for
the production of insulin in the body. The main purpose of insulin is to transfer glucose into
different tissues of the organ so that it is utilised in the form of fuel from tissues. If there is no
production of insulin then the glucose which is present in the body will not be utilised in the form of
energy from the cells. All the glucose then starts accumulating in blood which causes high content
of sugar in blood. There are several causes which are responsible for a person developing type 1
diabetes. They are discussed below.
Inadequate supply of insulin in the body
Taking diet more as compared to normal (Chary, Greiner, Bowers and Rohloff, 2012).
Prevalence of stress conditions if a person is not on usual diet
Intake of medicines which increases the level of sugar in blood such as sleeping pills and
decongestants. Change in hormonal levels due to adolescence.
Type 2 Diabetes
Type 2 diabetes is also caused due to imbalance in production of insulin from pancreatic
cells known as islet cells. It is also called insulin resistance because the body is able to make insulin
but is not able to utilise it from the body (Evans and et.al, 2013). At the initial level pancreatic cells
are able to make adequate amount of insulin but due to hormonal imbalance body cannot use it in
the form of energy. There are several causes that leads to type 2 diabetes in patients. They are
detects level of 200 milligrams per decilitre (mg/dL) or 11.1 millimoles per liter (mmol/L) then it is
suggested that Jazminder is suffering from diabetes.
Fasting blood sugar test: A blood sample is taken after the fasting process of overnight. If the
blood records a minimum of 100 mg/dL (5.6 mmol/L) then it is considered to be normal. If it
records 100 to 125 mg/dL (5.6 to 6.9 mmol/L) then she can be pre-diabetic but it records more than
126 mg/dL (7 mmol/L) then it is considered that she is suffering from diabetes (Carnethon and et.al,
2012).
Oral glucose tolerance test: Blood sugar levels after fasting and intake of sugary liquid is tested
for next two hours. If the reading is less than (7.8 mmol/L) then it is normal. If it is 200 mg/dL (11.1
mmol/L) or more than this value then the patient is suffering from diabetes (Armstrong, Harskamp
and Armstrong, 2013).
Q 2 Description of Type 1 and Type 2 Diabetes.
Type 1 Diabetes
Type 1 diabetes is generally caused when a person's immune system destroys the cells of
pancreas known as beta cells (Chalishajar and Stanford, 2014). These beta cells are responsible for
the production of insulin in the body. The main purpose of insulin is to transfer glucose into
different tissues of the organ so that it is utilised in the form of fuel from tissues. If there is no
production of insulin then the glucose which is present in the body will not be utilised in the form of
energy from the cells. All the glucose then starts accumulating in blood which causes high content
of sugar in blood. There are several causes which are responsible for a person developing type 1
diabetes. They are discussed below.
Inadequate supply of insulin in the body
Taking diet more as compared to normal (Chary, Greiner, Bowers and Rohloff, 2012).
Prevalence of stress conditions if a person is not on usual diet
Intake of medicines which increases the level of sugar in blood such as sleeping pills and
decongestants. Change in hormonal levels due to adolescence.
Type 2 Diabetes
Type 2 diabetes is also caused due to imbalance in production of insulin from pancreatic
cells known as islet cells. It is also called insulin resistance because the body is able to make insulin
but is not able to utilise it from the body (Evans and et.al, 2013). At the initial level pancreatic cells
are able to make adequate amount of insulin but due to hormonal imbalance body cannot use it in
the form of energy. There are several causes that leads to type 2 diabetes in patients. They are
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
discussed below.
Genetic factors
Body weight, obesity and lack of physical activity
Metabolic syndrome (Ginter and Simko, 2013)
Excess of glucose production from liver
Improper communication and signalling between cells
Breakdown of beta cells due to high production of blood glucose levels.
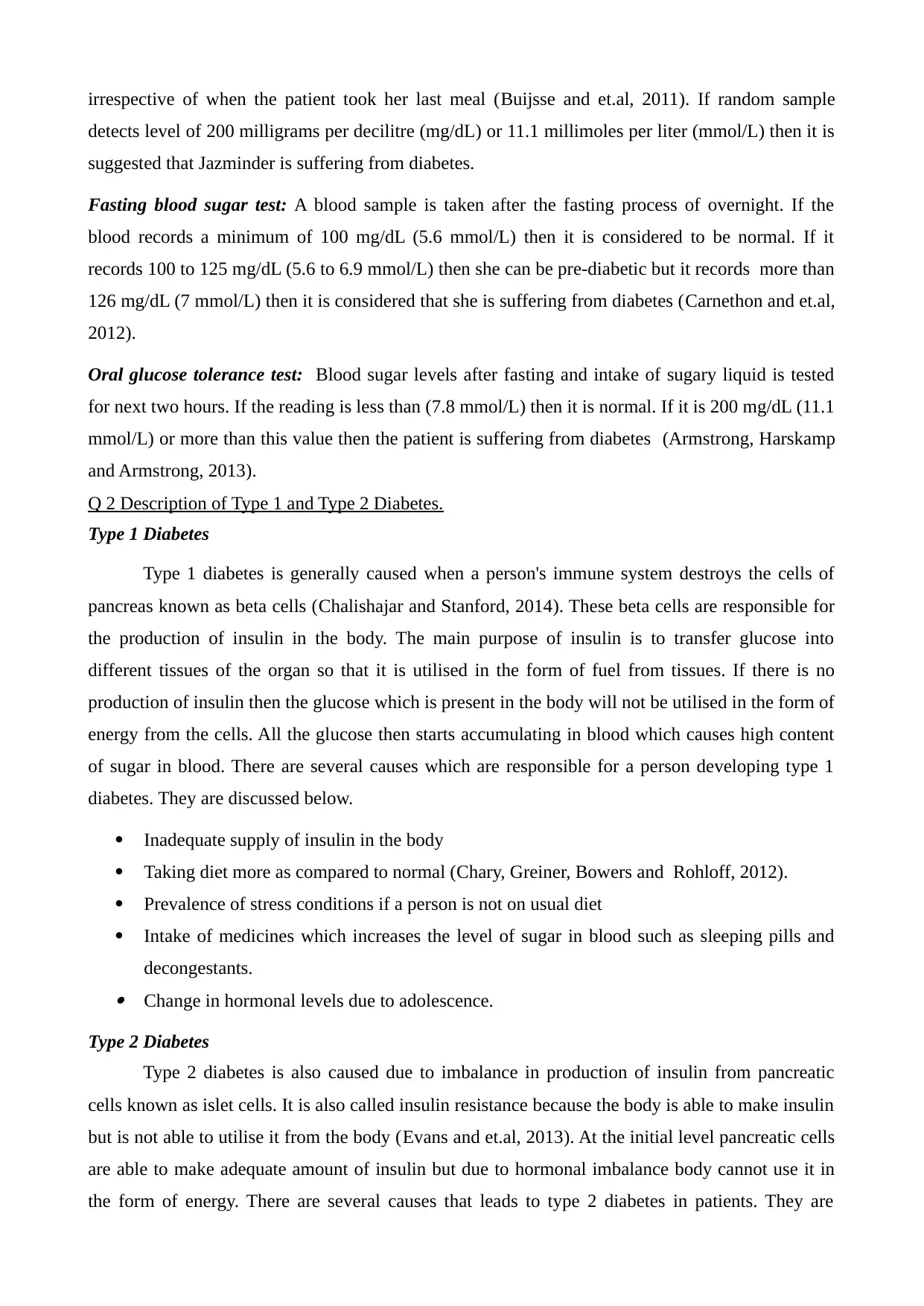
Difference in clinical presentation of type 1 and type 2 diabetes.
There are various difference in type 1 and type 2 diabetes. All differences are discussed
below.
Type 1 Diabetes Type 2 Diabetes
Type 1 diabetes is a autoimmune disorder that
results in damage of pancreatic cells known as
beta cells
Type 2 diabetes is different from type 1 diabetes
and is not considered as autoimmune disorder.
This is generally known as insulin resistant
diabetes (Hayes and et.al, 2013).
This is generally diagnosed in children due to
hormonal imbalance (Polonsky and Fisher,
2013)
This is diagnosed in individuals who are 30
years or more than that.
In this type of diabetes the ketone levels in urine
is more than normal and the condition is known
as ketoacidosis.
It is often related to high levels of sugar in blood
and cholesterol (Schaupp and et.al, 2015).
Insulin injections and pumps are usually used to
treat type 1 diabetes (Chary, Greiner, Bowers
and Rohloff, 2012).
No medications are prescribed at initial levels.
This type of diabetes cannot be controlled
without taking diabetes.
Sometimes it is possible to control without
medications but in severe cases it is necessary to
take medications to control it (Armstrong,
Harskamp and Armstrong, 2013).
Q 3 Two macro-vascular and three microvascular complications of diabetes
Macro-vascular complications of diabetes
Macro-vascular complications are those disease that are caused due to disruption of large
Genetic factors
Body weight, obesity and lack of physical activity
Metabolic syndrome (Ginter and Simko, 2013)
Excess of glucose production from liver
Improper communication and signalling between cells
Breakdown of beta cells due to high production of blood glucose levels.
Difference in clinical presentation of type 1 and type 2 diabetes.
There are various difference in type 1 and type 2 diabetes. All differences are discussed
below.
Type 1 Diabetes Type 2 Diabetes
Type 1 diabetes is a autoimmune disorder that
results in damage of pancreatic cells known as
beta cells
Type 2 diabetes is different from type 1 diabetes
and is not considered as autoimmune disorder.
This is generally known as insulin resistant
diabetes (Hayes and et.al, 2013).
This is generally diagnosed in children due to
hormonal imbalance (Polonsky and Fisher,
2013)
This is diagnosed in individuals who are 30
years or more than that.
In this type of diabetes the ketone levels in urine
is more than normal and the condition is known
as ketoacidosis.
It is often related to high levels of sugar in blood
and cholesterol (Schaupp and et.al, 2015).
Insulin injections and pumps are usually used to
treat type 1 diabetes (Chary, Greiner, Bowers
and Rohloff, 2012).
No medications are prescribed at initial levels.
This type of diabetes cannot be controlled
without taking diabetes.
Sometimes it is possible to control without
medications but in severe cases it is necessary to
take medications to control it (Armstrong,
Harskamp and Armstrong, 2013).
Q 3 Two macro-vascular and three microvascular complications of diabetes
Macro-vascular complications of diabetes
Macro-vascular complications are those disease that are caused due to disruption of large
blood vessels. These complications can occur in any part of the body depending upon the signs and
symptoms. There are several factors that contribute towards the macro-vascular complications.
These are high levels of blood sugar, insulin resistance in the body, high cholesterol and increase in
blood pressure of the body (Aschner, Horton and Skyler, 2010). Generally it is noted that micro-
vascular complications do not occur in all the patients but due to reasons like tissue resistance to
damage and inherited life factors complications may arise. For example if a person who has
encountered diabetes is habitual to smoking then there are increased chances that they he/she will
develop heart diseases (Asija, 2014). Major macro-vascular complications in diabetes are as
follows.
Heart disease: Heart diseases include strokes and heart attacks which are considered to be macro-
vascular complications in case of diabetes. If a person who is suffering from diabetes is diabetic
neuropathy then there are less chances that they suffer from heart problems.
Peripheral arterial disease: This is also a type of macro-vascular disorder which leads to narrowing
or blockage of arteries that is followed by poor blood flow in arms and legs of a person (Boström
and et.al, 2014). Due to insufficient supply of blood in arms and legs a person is not able to walk
properly and may experience painful cramps.
Micro-vascular complications
Micro-vascular complications in diabetes can be broadly defined as long term effects which
affects small blood vessels in the body. Based on classification three micro-vascular complications
have been discussed below.
Retinopathy: Retinopathy is also divided into two main types such as non-proliferative retinopathy
and proliferative retinopathy (Buijsse and et.al, 2011).
Diabetic nepropathy: It can be defined as presence of protein in urea which is greater than 0.5 g/day
Neuropathy: This complication is result of failure of nerve function in the body. It mainly affects
sensory and motor neuron of the body.
Test used to screen three microvascular complications
Retinopathy: Diabetic retinopathy is one of the micro-vascular complications that is diagnosed with
the help of dilated eye exam. In this process a drop is placed inside the eyes which helps in dilation
of the pupil more easily (Carnethon and et.al, 2012). In the examination, the physician test for
abnormal blood vessels that are present in the eyes, swelling and fatty deposits in the retina of the
eye. If normal eye drop testing do not show significant results than doctors suggest fluorescein
angiography and optical coherence tomography. If a person is having retinal detachment and
abnormalities in optic nerve then the individual is suffering from diabetes retinopathy.
Diabetic nephropathy: Diabetic nephropathy can be easily diagnosed by checking protein in urine
which is responsible for damaging kidney. Through urine test protein can be detected. If a urine
symptoms. There are several factors that contribute towards the macro-vascular complications.
These are high levels of blood sugar, insulin resistance in the body, high cholesterol and increase in
blood pressure of the body (Aschner, Horton and Skyler, 2010). Generally it is noted that micro-
vascular complications do not occur in all the patients but due to reasons like tissue resistance to
damage and inherited life factors complications may arise. For example if a person who has
encountered diabetes is habitual to smoking then there are increased chances that they he/she will
develop heart diseases (Asija, 2014). Major macro-vascular complications in diabetes are as
follows.
Heart disease: Heart diseases include strokes and heart attacks which are considered to be macro-
vascular complications in case of diabetes. If a person who is suffering from diabetes is diabetic
neuropathy then there are less chances that they suffer from heart problems.
Peripheral arterial disease: This is also a type of macro-vascular disorder which leads to narrowing
or blockage of arteries that is followed by poor blood flow in arms and legs of a person (Boström
and et.al, 2014). Due to insufficient supply of blood in arms and legs a person is not able to walk
properly and may experience painful cramps.
Micro-vascular complications
Micro-vascular complications in diabetes can be broadly defined as long term effects which
affects small blood vessels in the body. Based on classification three micro-vascular complications
have been discussed below.
Retinopathy: Retinopathy is also divided into two main types such as non-proliferative retinopathy
and proliferative retinopathy (Buijsse and et.al, 2011).
Diabetic nepropathy: It can be defined as presence of protein in urea which is greater than 0.5 g/day
Neuropathy: This complication is result of failure of nerve function in the body. It mainly affects
sensory and motor neuron of the body.
Test used to screen three microvascular complications
Retinopathy: Diabetic retinopathy is one of the micro-vascular complications that is diagnosed with
the help of dilated eye exam. In this process a drop is placed inside the eyes which helps in dilation
of the pupil more easily (Carnethon and et.al, 2012). In the examination, the physician test for
abnormal blood vessels that are present in the eyes, swelling and fatty deposits in the retina of the
eye. If normal eye drop testing do not show significant results than doctors suggest fluorescein
angiography and optical coherence tomography. If a person is having retinal detachment and
abnormalities in optic nerve then the individual is suffering from diabetes retinopathy.
Diabetic nephropathy: Diabetic nephropathy can be easily diagnosed by checking protein in urine
which is responsible for damaging kidney. Through urine test protein can be detected. If a urine
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
sample measures protein content in it then the patient is suffering from diabetic nepropathy
(Chalishajar and Stanford, 2014).
Neuropathy: Diabetic neuropathy is largely based on symptoms and can be detected through
physical and medical examination. Electromyographic technique can be helpful in detecting
diabetic neuropathy in patients who are suffering from diabetes.
Q 4 Assess the ongoing levels of glycaemic control in patient with diabetes type 2
The measurement of haemoglobin levels is one of the most appropriate way for assessing
the glycaemic control levels in patients suffering from type 2 diabetes (Chary, Greiner, Bowers and
Rohloff, 2012). Glycaemic control is defined as a medical term that is used to refer to blood sugar
levels in a person who has encountered diabetes mellitus. Glycaemic control can be assessed in two
different ways which are described below.
Self monitoring blood glucose levels:Based on research and studies it has been proved that regular
monitoring of glucose levels with the help of meters is likely to improve the outcomes and control
in type 2 diabetes.
HbA1c test: This test is helpful in measuring glycated haemoglobin levels associated with the total
levels of haemoglobin. In non diabetic patients the level of HbA1c is 4-6% whereas if the
glycaemic level is below 6.5% then it is said that it is controlled with efficiency (Evans and et.al,
2013).
Pharmacological strategies for improving glycaemic controls
There are many pharmacological strategies that can be adopted so that glycaemic levels in
type 2 diabetes is controlled and maintained to normal levels (Ginter and Simko, 2013). Metformin
is 1st line order drug which is used to treat or control the glycaemic levels in diabetes 2. The
mechanism of action is based on large amount of disposal of peripheral glucose which is followed
by decrease in insulin resistance to the body. The effects of Metformin are irrespective of age,
gender and weight of the body (Polonsky and Fisher, 2013).
Another pharmacological treatment for controlling glycaemic levels in the body is through
Sulphonylureas (Sus) which is only used when there are presence of severe contraindications or
complexities in Metformin. It increases the release of insulin so that it can be readily utilised by
body organs (Schaupp and et.al, 2015).
CONCLUSION
The overall report was based a case study in which a patient has developed risk of
encountering diabetes due to her family and medical history. Different aspects of diabetes have
been discussed in the study.
(Chalishajar and Stanford, 2014).
Neuropathy: Diabetic neuropathy is largely based on symptoms and can be detected through
physical and medical examination. Electromyographic technique can be helpful in detecting
diabetic neuropathy in patients who are suffering from diabetes.
Q 4 Assess the ongoing levels of glycaemic control in patient with diabetes type 2
The measurement of haemoglobin levels is one of the most appropriate way for assessing
the glycaemic control levels in patients suffering from type 2 diabetes (Chary, Greiner, Bowers and
Rohloff, 2012). Glycaemic control is defined as a medical term that is used to refer to blood sugar
levels in a person who has encountered diabetes mellitus. Glycaemic control can be assessed in two
different ways which are described below.
Self monitoring blood glucose levels:Based on research and studies it has been proved that regular
monitoring of glucose levels with the help of meters is likely to improve the outcomes and control
in type 2 diabetes.
HbA1c test: This test is helpful in measuring glycated haemoglobin levels associated with the total
levels of haemoglobin. In non diabetic patients the level of HbA1c is 4-6% whereas if the
glycaemic level is below 6.5% then it is said that it is controlled with efficiency (Evans and et.al,
2013).
Pharmacological strategies for improving glycaemic controls
There are many pharmacological strategies that can be adopted so that glycaemic levels in
type 2 diabetes is controlled and maintained to normal levels (Ginter and Simko, 2013). Metformin
is 1st line order drug which is used to treat or control the glycaemic levels in diabetes 2. The
mechanism of action is based on large amount of disposal of peripheral glucose which is followed
by decrease in insulin resistance to the body. The effects of Metformin are irrespective of age,
gender and weight of the body (Polonsky and Fisher, 2013).
Another pharmacological treatment for controlling glycaemic levels in the body is through
Sulphonylureas (Sus) which is only used when there are presence of severe contraindications or
complexities in Metformin. It increases the release of insulin so that it can be readily utilised by
body organs (Schaupp and et.al, 2015).
CONCLUSION
The overall report was based a case study in which a patient has developed risk of
encountering diabetes due to her family and medical history. Different aspects of diabetes have
been discussed in the study.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
REFERENCES
Books and Journals
Armstrong, A.W., Harskamp, C.T. and Armstrong, E.J., 2013. Psoriasis and the risk of diabetes
mellitus: a systematic review and meta-analysis. JAMA dermatology. 149(1). pp.84-91.
Aschner, P., Horton, E., and Skyler, J. S., 2010. Practical steps to improving the management of
type 1 diabetes: recommendations from the Global Partnership for Effective Diabetes
Management. International Journal of Clinical Practice. 64(3). Pp. 305- 315.
Asija, R., 2014. Herbal plants used in treatment of diabeties mellitus: an updated review. Journal of
drug discovery and therapeutics. 2(24).
Boström, E. and et.al., 2014. Interaction between diabetes specialist nurses and patients during
group sessions about self-management in type 2 diabetes. Patient Education and
Counseling. 94(2). Pp.187-192.
Buijsse, B. and et.al., 2011. Risk assessment tools for identifying individuals at risk of developing
type 2 diabetes. Am J Epidemiol. 33. Pp.46–62.
Carnethon, M. R. and et.al. 2012. Association of weight status with mortality in adults with incident
diabetes. JAMA. 308. Pp.581–90.
Chalishajar, D.D. and Stanford, C.A.C., 2014. Mathematical Analysis of Insulin-Glucose Feedback
System of Diabeties. International Journal of Engineering. 5(02). p.8269.
Chary, C., Greiner, M., Bowers, C. and Rohloff, P., 2012. Determining adult type 2 diabetes-related
health care needs in an indigenous population from rural Guatemala: a mixed-methods
preliminary study. BMC Health Services Research. 12(476).
Evans, J.M. and et.al., 2013. Self-monitoring among non-insulin treated patients with type 2
diabetes mellitus: patients’ behavioural responses to readings and associations with glycaemic
control. Diabetes research and clinical practice. 100(2). pp.235-242.
Ginter, E. and Simko, V., 2013. Type 2 diabetes mellitus, pandemic in 21st century. Springer New
York.
Hayes, A.J. and et.al., 2013. UKPDS outcomes model 2: a new version of a model to simulate
lifetime health outcomes of patients with type 2 diabetes mellitus using data from the 30 year
United Kingdom Prospective Diabetes Study: UKPDS 82. Diabetologia. 56(9). pp.1925-1933.
Polonsky, W.H. and Fisher, L., 2013. Self-Monitoring of Blood Glucose in Noninsulin-Using Type
2 Diabetic Patients Right answer, but wrong question: self-monitoring of blood glucose can be
clinically valuable for noninsulin users. Diabetes Care. 36(1). pp.179-182.
Schaupp, L. and et.al., 2015. Taking a closer look—continuous glucose monitoring in non-critically
ill hospitalized patients with type 2 diabetes mellitus under basal-bolus insulin therapy.
Diabetes technology & therapeutics. 17(9). pp.611-618.
Books and Journals
Armstrong, A.W., Harskamp, C.T. and Armstrong, E.J., 2013. Psoriasis and the risk of diabetes
mellitus: a systematic review and meta-analysis. JAMA dermatology. 149(1). pp.84-91.
Aschner, P., Horton, E., and Skyler, J. S., 2010. Practical steps to improving the management of
type 1 diabetes: recommendations from the Global Partnership for Effective Diabetes
Management. International Journal of Clinical Practice. 64(3). Pp. 305- 315.
Asija, R., 2014. Herbal plants used in treatment of diabeties mellitus: an updated review. Journal of
drug discovery and therapeutics. 2(24).
Boström, E. and et.al., 2014. Interaction between diabetes specialist nurses and patients during
group sessions about self-management in type 2 diabetes. Patient Education and
Counseling. 94(2). Pp.187-192.
Buijsse, B. and et.al., 2011. Risk assessment tools for identifying individuals at risk of developing
type 2 diabetes. Am J Epidemiol. 33. Pp.46–62.
Carnethon, M. R. and et.al. 2012. Association of weight status with mortality in adults with incident
diabetes. JAMA. 308. Pp.581–90.
Chalishajar, D.D. and Stanford, C.A.C., 2014. Mathematical Analysis of Insulin-Glucose Feedback
System of Diabeties. International Journal of Engineering. 5(02). p.8269.
Chary, C., Greiner, M., Bowers, C. and Rohloff, P., 2012. Determining adult type 2 diabetes-related
health care needs in an indigenous population from rural Guatemala: a mixed-methods
preliminary study. BMC Health Services Research. 12(476).
Evans, J.M. and et.al., 2013. Self-monitoring among non-insulin treated patients with type 2
diabetes mellitus: patients’ behavioural responses to readings and associations with glycaemic
control. Diabetes research and clinical practice. 100(2). pp.235-242.
Ginter, E. and Simko, V., 2013. Type 2 diabetes mellitus, pandemic in 21st century. Springer New
York.
Hayes, A.J. and et.al., 2013. UKPDS outcomes model 2: a new version of a model to simulate
lifetime health outcomes of patients with type 2 diabetes mellitus using data from the 30 year
United Kingdom Prospective Diabetes Study: UKPDS 82. Diabetologia. 56(9). pp.1925-1933.
Polonsky, W.H. and Fisher, L., 2013. Self-Monitoring of Blood Glucose in Noninsulin-Using Type
2 Diabetic Patients Right answer, but wrong question: self-monitoring of blood glucose can be
clinically valuable for noninsulin users. Diabetes Care. 36(1). pp.179-182.
Schaupp, L. and et.al., 2015. Taking a closer look—continuous glucose monitoring in non-critically
ill hospitalized patients with type 2 diabetes mellitus under basal-bolus insulin therapy.
Diabetes technology & therapeutics. 17(9). pp.611-618.
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





