Educational Booklet: Sulfonylureas for Type 2 Diabetes Mellitus
VerifiedAdded on 2022/09/18
|11
|2436
|24
Report
AI Summary
This educational booklet provides a comprehensive overview of sulfonylureas, a class of anti-diabetic drugs used in the treatment of Type 2 Diabetes Mellitus (T2DM). The booklet begins by explaining the pathophysiology of T2DM, focusing on impaired insulin secretion, insulin resistance, and the dysfunction of pancreatic beta cells. It then describes the mode of action of sulfonylureas, emphasizing their role in stimulating insulin secretion and their interaction with specific receptors in pancreatic beta cells. The booklet also details the indications for sulfonylurea use, contraindications, potential drug interactions, and adverse effects such as hypoglycemia and weight gain. The route of administration, therapeutic outcomes, and the importance of monitoring blood glucose levels are also discussed. References from various research papers are also included to support the content.

Running head: EDUCATIONAL BOOKLET
Educational Booklet
Name of the Student
Name of the University
Author Note
Educational Booklet
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EDUCATIONAL BOOKLET 1
Introduction
Sulfonylureas is an anti-diabetic drug that is used for the treatment of Type 2 Diabetes
Mellitus (T2DM) among the older adults. Despite the presence of the large number of the
anti-diabetic drug in the market, sulfonylureas are regarded as one of the potent drug for the
treatment of T2DM (Kalra et al., 2018). The following educational booklet will highlight the
pathophysiology of T2DM followed by the mode of action of this medication in order to
overcome hyperglycaemic condition of T2DM in relation to the disease pathophysiology. The
educational booklet will also provide necessary details about the medication side-effects,
interactions, contradictions and implications.
Pathophysiology of the disorder: Type 2 Diabetes Mellitus (T2DM)
Normal Pathophysiology of T2DM
Impaired secretion of insulin and development of resistance towards insulin contribute
to development of the complex pathological condition of T2DM. Impaired insulin secretion
leads to decrease in the glucose responsiveness. Impaired glucose tolerance (IGT) is mainly
induced through decrease in the level of glucose-responsive during the early phase of the
insulin secretion and decrease in the additional insulin secretion that is produced after meals
(Postprandial hyperglycemia) (Zaccardi et al., 2016). Impaired insulin secretion is
progressive condition and this leads to the development of glucose toxicity and lipo-toxicity.
Insulin resistance is defined as a condition under which the insulin fails to exert the sufficient
action that is proportional to the amount of glucose present in the blood. Insulin resistance
and high glucose concentration hamper several organs like liver, kidneys and muscles. The
development of insulin resistance is multifactorial as it has both genetic and environmental
influence. The dysfunction of the beta-cells of the Islet of Langerhans present in the pancreas
leads to inappropriate secretion of insulin in response to glucose and thus developing
Introduction
Sulfonylureas is an anti-diabetic drug that is used for the treatment of Type 2 Diabetes
Mellitus (T2DM) among the older adults. Despite the presence of the large number of the
anti-diabetic drug in the market, sulfonylureas are regarded as one of the potent drug for the
treatment of T2DM (Kalra et al., 2018). The following educational booklet will highlight the
pathophysiology of T2DM followed by the mode of action of this medication in order to
overcome hyperglycaemic condition of T2DM in relation to the disease pathophysiology. The
educational booklet will also provide necessary details about the medication side-effects,
interactions, contradictions and implications.
Pathophysiology of the disorder: Type 2 Diabetes Mellitus (T2DM)
Normal Pathophysiology of T2DM
Impaired secretion of insulin and development of resistance towards insulin contribute
to development of the complex pathological condition of T2DM. Impaired insulin secretion
leads to decrease in the glucose responsiveness. Impaired glucose tolerance (IGT) is mainly
induced through decrease in the level of glucose-responsive during the early phase of the
insulin secretion and decrease in the additional insulin secretion that is produced after meals
(Postprandial hyperglycemia) (Zaccardi et al., 2016). Impaired insulin secretion is
progressive condition and this leads to the development of glucose toxicity and lipo-toxicity.
Insulin resistance is defined as a condition under which the insulin fails to exert the sufficient
action that is proportional to the amount of glucose present in the blood. Insulin resistance
and high glucose concentration hamper several organs like liver, kidneys and muscles. The
development of insulin resistance is multifactorial as it has both genetic and environmental
influence. The dysfunction of the beta-cells of the Islet of Langerhans present in the pancreas
leads to inappropriate secretion of insulin in response to glucose and thus developing
EDUCATIONAL BOOKLET 2
hyperglycaemic condition. Presence of obesity along with visceral adiposity for a prolong
period of time increase the level of internal inflammation and this in turn creates de-
sensitization by hampering the sensitivity of the glucose-re-uptake receptors and thereby
developing insulin resistance even under the high concentration of glucose in the blood and
insulin in the plasma. Other factors that promote insulin resistance and subsequent generation
of insulin resistance include presence of ectopic fat storage syndrome, presence of high
adipose tissues in the endocrine organs and high concentration of the non-esterified fatty
acids (Zaccardi et al., 2016).
Dysfunction of pancreatic beta cell
Chronic insulin resistance is regarded as the main pathophysiology of T2DM (Shehata
et al., 2017). Chronic insulin resistance develops when the pancreatic beta cells are unable to
produce insulin to compensate the glucose content in the blood (Shehata et al., 2017). The
worsening of the T2DM condition occurs due to dysfunction of the pancreatic beta cells to
produce insulin followed by the development of insulin resistance in the body under the
action of the Pancreatic Derived Factor (PANDER). Thus insulin resistance, the hepatic cell
fails to re-uptake glucose from the blood leading to the development of T2DM (Shehata et
al., 2017).
PANDER is a 235 amino-acid protein. It is secreted from the pancreatic beta and
alpha cells (MarElia et al., 2018). This protein is involved in regulating the secretary process
of insulin and glucose homeostasis (MarElia et al., 2018). Under hypergycemic action, the
PANDER protein involves negative action on the Islet cells and thus reducing the insulin
secretion and increasing the hyperglycaemic condition further. The concentration of
PANDER is elevated as highlighted in the serum of the diabetic patients and thus it is
concluded that beta-cell dysfunction play an important role in the glycemic control of the
diabetic patient. In obese adolescents, the dysfunction of beta cells plays an importance role
hyperglycaemic condition. Presence of obesity along with visceral adiposity for a prolong
period of time increase the level of internal inflammation and this in turn creates de-
sensitization by hampering the sensitivity of the glucose-re-uptake receptors and thereby
developing insulin resistance even under the high concentration of glucose in the blood and
insulin in the plasma. Other factors that promote insulin resistance and subsequent generation
of insulin resistance include presence of ectopic fat storage syndrome, presence of high
adipose tissues in the endocrine organs and high concentration of the non-esterified fatty
acids (Zaccardi et al., 2016).
Dysfunction of pancreatic beta cell
Chronic insulin resistance is regarded as the main pathophysiology of T2DM (Shehata
et al., 2017). Chronic insulin resistance develops when the pancreatic beta cells are unable to
produce insulin to compensate the glucose content in the blood (Shehata et al., 2017). The
worsening of the T2DM condition occurs due to dysfunction of the pancreatic beta cells to
produce insulin followed by the development of insulin resistance in the body under the
action of the Pancreatic Derived Factor (PANDER). Thus insulin resistance, the hepatic cell
fails to re-uptake glucose from the blood leading to the development of T2DM (Shehata et
al., 2017).
PANDER is a 235 amino-acid protein. It is secreted from the pancreatic beta and
alpha cells (MarElia et al., 2018). This protein is involved in regulating the secretary process
of insulin and glucose homeostasis (MarElia et al., 2018). Under hypergycemic action, the
PANDER protein involves negative action on the Islet cells and thus reducing the insulin
secretion and increasing the hyperglycaemic condition further. The concentration of
PANDER is elevated as highlighted in the serum of the diabetic patients and thus it is
concluded that beta-cell dysfunction play an important role in the glycemic control of the
diabetic patient. In obese adolescents, the dysfunction of beta cells plays an importance role
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EDUCATIONAL BOOKLET 3
in predicting the disease progression during the later stages of life (MarElia et al., 2018).
Ageing is also associated with the development of the beta-cell dysfunction and thus the
chances of developing Type 2 Diabetes mellitus are higher among the older adults (MarElia
et al., 2018).
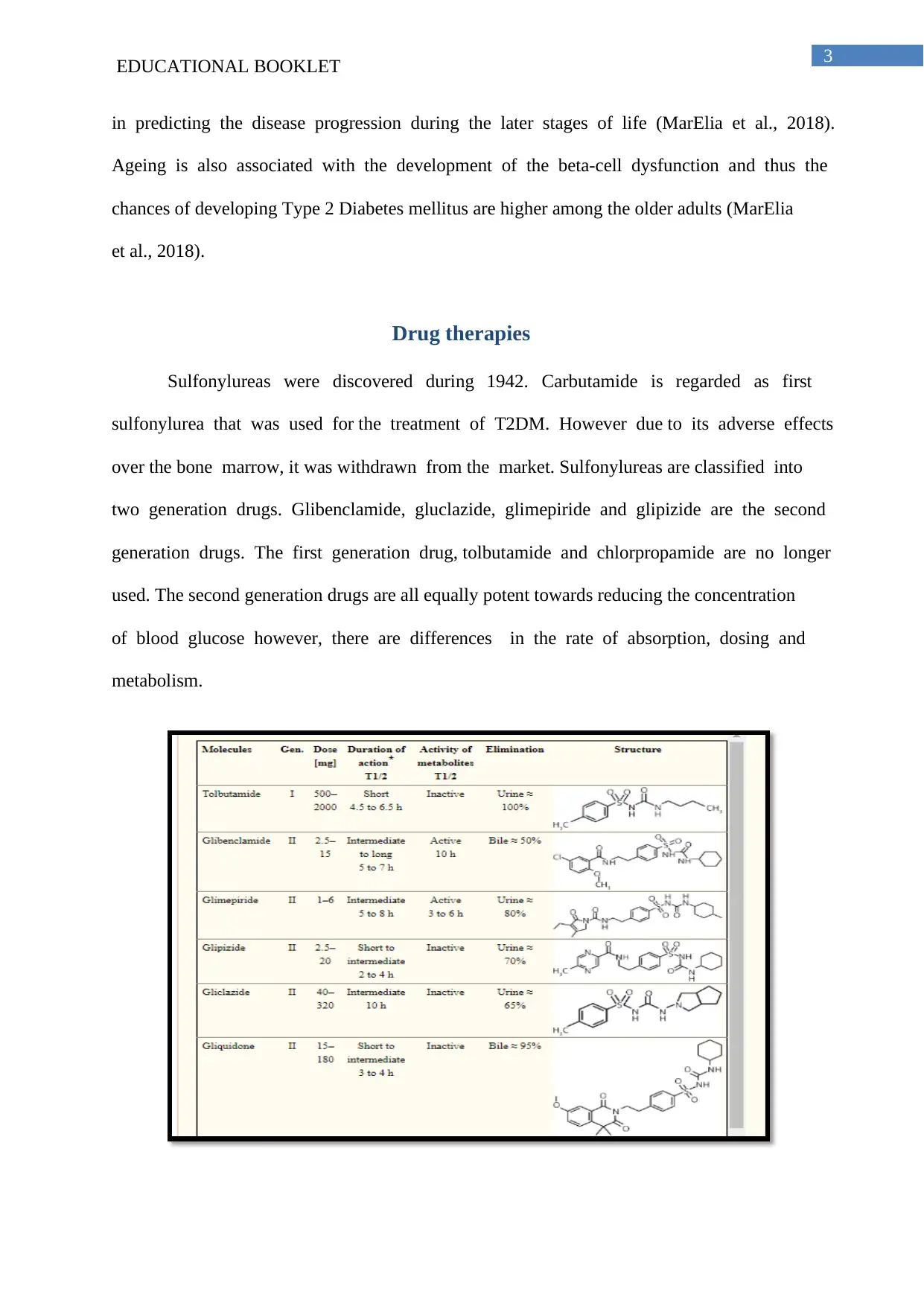
Drug therapies
Sulfonylureas were discovered during 1942. Carbutamide is regarded as first
sulfonylurea that was used for the treatment of T2DM. However due to its adverse effects
over the bone marrow, it was withdrawn from the market. Sulfonylureas are classified into
two generation drugs. Glibenclamide, gluclazide, glimepiride and glipizide are the second
generation drugs. The first generation drug, tolbutamide and chlorpropamide are no longer
used. The second generation drugs are all equally potent towards reducing the concentration
of blood glucose however, there are differences in the rate of absorption, dosing and
metabolism.
in predicting the disease progression during the later stages of life (MarElia et al., 2018).
Ageing is also associated with the development of the beta-cell dysfunction and thus the
chances of developing Type 2 Diabetes mellitus are higher among the older adults (MarElia
et al., 2018).
Drug therapies
Sulfonylureas were discovered during 1942. Carbutamide is regarded as first
sulfonylurea that was used for the treatment of T2DM. However due to its adverse effects
over the bone marrow, it was withdrawn from the market. Sulfonylureas are classified into
two generation drugs. Glibenclamide, gluclazide, glimepiride and glipizide are the second
generation drugs. The first generation drug, tolbutamide and chlorpropamide are no longer
used. The second generation drugs are all equally potent towards reducing the concentration
of blood glucose however, there are differences in the rate of absorption, dosing and
metabolism.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EDUCATIONAL BOOKLET 4
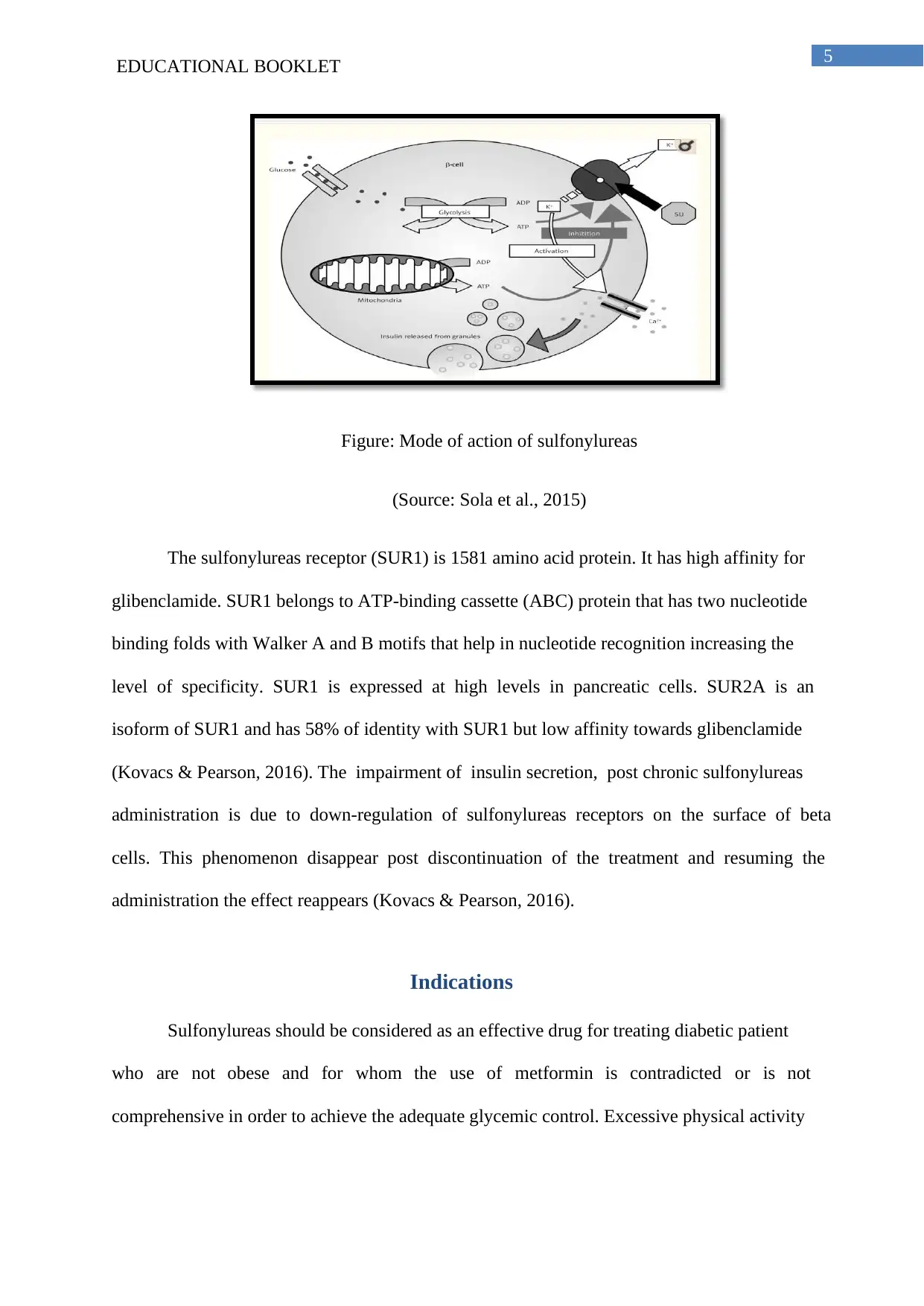
Figure: First and Second Generation Drug
(Source: Sola et al., 2015)
Mode of action
The effect of sulfonylureas deals with rise in the level of plasma insulin concentration
and they are only effective when the residual pancreatic beta cells are present. The increase in
the insulin levels in plasma mainly occurs for two different reasons. At first there occurs
stimulation of the insulin secretion by the pancreatic beta cells and secondly there is a
decrease in the hepatic clearance of insulin (Yu et al., 2018). The second effects mainly
appear after the increase in the secretion of insulin. During the initial month of the therapy,
the level of insulin and the overall response of insulin towards glucose increases rapidly
resulting in decreased blood glucose level (BGL). After this period, stimulated and baseline
insulin levels is lowered in comparison to those measured in the beginning of the treatment.
However, the values of blood glucose level remain unchanged (Yu et al., 2018).
With regard to the secretary activity of sulfonylureas, the exact mechanism is still
unknown. They mainly act through binding of the specific receptors for sulfonylureas over
the pancreatic beta cells. This blocks the inflow of potassium ions through the ATP
dependent channel. Thus flow of potassium within the beta cells becomes zero. The cell
membrane is depolarized and leading to the influx of calcium into the beta cells. Increase in
the intracellular calcium concentration in the beta cells causes contraction of the actomysin
filaments that is responsible for the exocytosis of insulin and uptake of glucose from blood
(Kovacs & Pearson, 2016).
Figure: First and Second Generation Drug
(Source: Sola et al., 2015)
Mode of action
The effect of sulfonylureas deals with rise in the level of plasma insulin concentration
and they are only effective when the residual pancreatic beta cells are present. The increase in
the insulin levels in plasma mainly occurs for two different reasons. At first there occurs
stimulation of the insulin secretion by the pancreatic beta cells and secondly there is a
decrease in the hepatic clearance of insulin (Yu et al., 2018). The second effects mainly
appear after the increase in the secretion of insulin. During the initial month of the therapy,
the level of insulin and the overall response of insulin towards glucose increases rapidly
resulting in decreased blood glucose level (BGL). After this period, stimulated and baseline
insulin levels is lowered in comparison to those measured in the beginning of the treatment.
However, the values of blood glucose level remain unchanged (Yu et al., 2018).
With regard to the secretary activity of sulfonylureas, the exact mechanism is still
unknown. They mainly act through binding of the specific receptors for sulfonylureas over
the pancreatic beta cells. This blocks the inflow of potassium ions through the ATP
dependent channel. Thus flow of potassium within the beta cells becomes zero. The cell
membrane is depolarized and leading to the influx of calcium into the beta cells. Increase in
the intracellular calcium concentration in the beta cells causes contraction of the actomysin
filaments that is responsible for the exocytosis of insulin and uptake of glucose from blood
(Kovacs & Pearson, 2016).
EDUCATIONAL BOOKLET 5
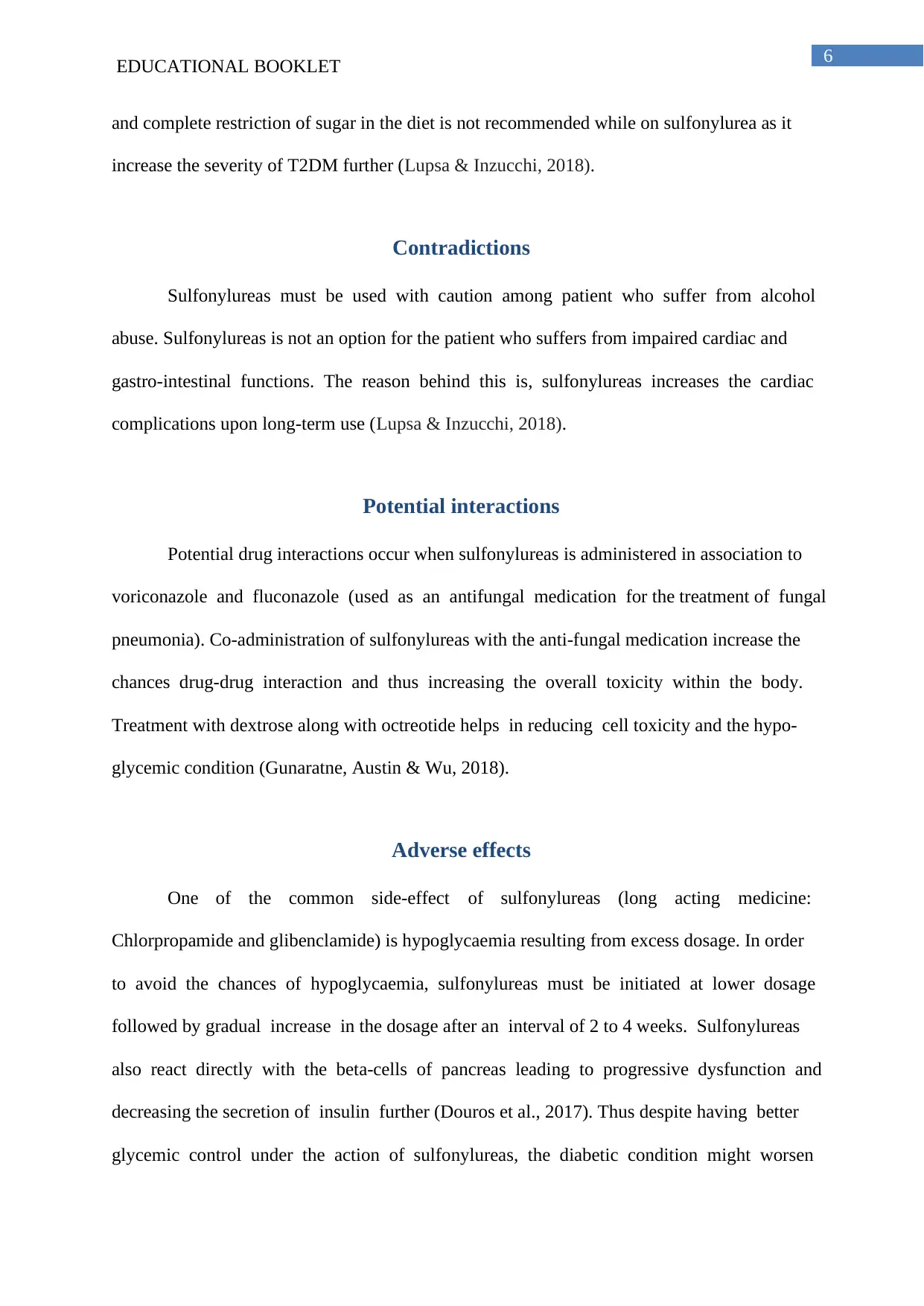
Figure: Mode of action of sulfonylureas
(Source: Sola et al., 2015)
The sulfonylureas receptor (SUR1) is 1581 amino acid protein. It has high affinity for
glibenclamide. SUR1 belongs to ATP-binding cassette (ABC) protein that has two nucleotide
binding folds with Walker A and B motifs that help in nucleotide recognition increasing the
level of specificity. SUR1 is expressed at high levels in pancreatic cells. SUR2A is an
isoform of SUR1 and has 58% of identity with SUR1 but low affinity towards glibenclamide
(Kovacs & Pearson, 2016). The impairment of insulin secretion, post chronic sulfonylureas
administration is due to down-regulation of sulfonylureas receptors on the surface of beta
cells. This phenomenon disappear post discontinuation of the treatment and resuming the
administration the effect reappears (Kovacs & Pearson, 2016).
Indications
Sulfonylureas should be considered as an effective drug for treating diabetic patient
who are not obese and for whom the use of metformin is contradicted or is not
comprehensive in order to achieve the adequate glycemic control. Excessive physical activity
Figure: Mode of action of sulfonylureas
(Source: Sola et al., 2015)
The sulfonylureas receptor (SUR1) is 1581 amino acid protein. It has high affinity for
glibenclamide. SUR1 belongs to ATP-binding cassette (ABC) protein that has two nucleotide
binding folds with Walker A and B motifs that help in nucleotide recognition increasing the
level of specificity. SUR1 is expressed at high levels in pancreatic cells. SUR2A is an
isoform of SUR1 and has 58% of identity with SUR1 but low affinity towards glibenclamide
(Kovacs & Pearson, 2016). The impairment of insulin secretion, post chronic sulfonylureas
administration is due to down-regulation of sulfonylureas receptors on the surface of beta
cells. This phenomenon disappear post discontinuation of the treatment and resuming the
administration the effect reappears (Kovacs & Pearson, 2016).
Indications
Sulfonylureas should be considered as an effective drug for treating diabetic patient
who are not obese and for whom the use of metformin is contradicted or is not
comprehensive in order to achieve the adequate glycemic control. Excessive physical activity
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EDUCATIONAL BOOKLET 6
and complete restriction of sugar in the diet is not recommended while on sulfonylurea as it
increase the severity of T2DM further (Lupsa & Inzucchi, 2018).
Contradictions
Sulfonylureas must be used with caution among patient who suffer from alcohol
abuse. Sulfonylureas is not an option for the patient who suffers from impaired cardiac and
gastro-intestinal functions. The reason behind this is, sulfonylureas increases the cardiac
complications upon long-term use (Lupsa & Inzucchi, 2018).
Potential interactions
Potential drug interactions occur when sulfonylureas is administered in association to
voriconazole and fluconazole (used as an antifungal medication for the treatment of fungal
pneumonia). Co-administration of sulfonylureas with the anti-fungal medication increase the
chances drug-drug interaction and thus increasing the overall toxicity within the body.
Treatment with dextrose along with octreotide helps in reducing cell toxicity and the hypo-
glycemic condition (Gunaratne, Austin & Wu, 2018).
Adverse effects
One of the common side-effect of sulfonylureas (long acting medicine:
Chlorpropamide and glibenclamide) is hypoglycaemia resulting from excess dosage. In order
to avoid the chances of hypoglycaemia, sulfonylureas must be initiated at lower dosage
followed by gradual increase in the dosage after an interval of 2 to 4 weeks. Sulfonylureas
also react directly with the beta-cells of pancreas leading to progressive dysfunction and
decreasing the secretion of insulin further (Douros et al., 2017). Thus despite having better
glycemic control under the action of sulfonylureas, the diabetic condition might worsen
and complete restriction of sugar in the diet is not recommended while on sulfonylurea as it
increase the severity of T2DM further (Lupsa & Inzucchi, 2018).
Contradictions
Sulfonylureas must be used with caution among patient who suffer from alcohol
abuse. Sulfonylureas is not an option for the patient who suffers from impaired cardiac and
gastro-intestinal functions. The reason behind this is, sulfonylureas increases the cardiac
complications upon long-term use (Lupsa & Inzucchi, 2018).
Potential interactions
Potential drug interactions occur when sulfonylureas is administered in association to
voriconazole and fluconazole (used as an antifungal medication for the treatment of fungal
pneumonia). Co-administration of sulfonylureas with the anti-fungal medication increase the
chances drug-drug interaction and thus increasing the overall toxicity within the body.
Treatment with dextrose along with octreotide helps in reducing cell toxicity and the hypo-
glycemic condition (Gunaratne, Austin & Wu, 2018).
Adverse effects
One of the common side-effect of sulfonylureas (long acting medicine:
Chlorpropamide and glibenclamide) is hypoglycaemia resulting from excess dosage. In order
to avoid the chances of hypoglycaemia, sulfonylureas must be initiated at lower dosage
followed by gradual increase in the dosage after an interval of 2 to 4 weeks. Sulfonylureas
also react directly with the beta-cells of pancreas leading to progressive dysfunction and
decreasing the secretion of insulin further (Douros et al., 2017). Thus despite having better
glycemic control under the action of sulfonylureas, the diabetic condition might worsen
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EDUCATIONAL BOOKLET 7
during the long run under the treatment of this medication This condition is known as
“secondary failure”. Other associated side-effects of sulfonylureas include weight gain,
nausea and skin reactions (exfoliative dermatitis and erythema multiforme). Sulfonylureas
might also affect the function of liver and cardiac cells (Douros et al., 2017).
Route of administration
The medication comes in the form of tablets or extended-release (long-acting) tablets
that are administered orally. The regular tables are consumed once or twice a day, at least half
an hour before meals, mainly breakfast. The extended-release tablets are taken once a day
before breakfast. The medication is mainly recommended for the older adults with T2DM
(Lupsa & Inzucchi, 2018).
Therapeutic outcomes
The therapeutic health outcomes of the sulfonylureas include decrease in the level of
blood glucose however; however, the use of the sulfonylureas for a long-term might lead to
hypo-glycemic condition. Newer yet prolonged-release preparations of the sulfonylureas are
undoubtedly safer as it has lower chances of developing hypoglycemic function (Kovacs &
Pearson, 2016).
Conclusion
Use of sulfonylurea is suitable for the treatment of T2DM however, glucose level
must be monitored in order to reduce the chances of severe hypoglycemia. Sulfonylurea acts
through the regulation of the ion channels in the beta cells of the Islet langerhans of pancreas
and thus regulating the secretion of insulin and promoting glucose uptake. The medication is
during the long run under the treatment of this medication This condition is known as
“secondary failure”. Other associated side-effects of sulfonylureas include weight gain,
nausea and skin reactions (exfoliative dermatitis and erythema multiforme). Sulfonylureas
might also affect the function of liver and cardiac cells (Douros et al., 2017).
Route of administration
The medication comes in the form of tablets or extended-release (long-acting) tablets
that are administered orally. The regular tables are consumed once or twice a day, at least half
an hour before meals, mainly breakfast. The extended-release tablets are taken once a day
before breakfast. The medication is mainly recommended for the older adults with T2DM
(Lupsa & Inzucchi, 2018).
Therapeutic outcomes
The therapeutic health outcomes of the sulfonylureas include decrease in the level of
blood glucose however; however, the use of the sulfonylureas for a long-term might lead to
hypo-glycemic condition. Newer yet prolonged-release preparations of the sulfonylureas are
undoubtedly safer as it has lower chances of developing hypoglycemic function (Kovacs &
Pearson, 2016).
Conclusion
Use of sulfonylurea is suitable for the treatment of T2DM however, glucose level
must be monitored in order to reduce the chances of severe hypoglycemia. Sulfonylurea acts
through the regulation of the ion channels in the beta cells of the Islet langerhans of pancreas
and thus regulating the secretion of insulin and promoting glucose uptake. The medication is

EDUCATIONAL BOOKLET 8
given orally before diet and should never be used in association to anti-fungal medication and
in patients with cardio-vascular complications.
given orally before diet and should never be used in association to anti-fungal medication and
in patients with cardio-vascular complications.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EDUCATIONAL BOOKLET 9
References
Douros, A., Yin, H., Yu, O. H. Y., Filion, K. B., Azoulay, L., & Suissa, S. (2017).
Pharmacologic differences of sulfonylureas and the risk of adverse cardiovascular and
hypoglycemic events. Diabetes Care, 40(11), 1506-1513.
https://doi.org/10.2337/dc17-0595
Gunaratne, K., Austin, E., & Wu, P. E. (2018). Unintentional sulfonylurea toxicity due to a
drug–drug interaction: a case report. BMC research notes, 11(1), 331.
doi: 10.1186/s13104-018-3404-8
Kalra, S., Bahendeka, S., Sahay, R., Ghosh, S., Md, F., Orabi, A., ... & Abhayaratna, S.
(2018). Consensus recommendations on sulfonylurea and sulfonylurea combinations
in the management of Type 2 diabetes mellitus–International Task Force. Indian
journal of endocrinology and metabolism, 22(1), 132.
Kovacs, P., & Pearson, E. (2016). Pharmacogenetics of sulfonylureas. In The Genetics of
Type 2 Diabetes and Related Traits (pp. 483-497). Springer, Cham.
https://doi.org/10.1007/978-3-319-01574-3_23
Lupsa, B. C., & Inzucchi, S. E. (2018). Diabetes medications and cardiovascular disease: at
long last progress. Current Opinion in Endocrinology & Diabetes and Obesity, 25(2),
87-93. DOI: https://doi.org/10.1097/MED.0000000000000400
MarElia, C. B., Kuehl, M. N., Shemwell, T. A., Alman, A. C., & Burkhardt, B. R. (2018).
Circulating PANDER concentration is associated with increased HbA1c and fasting
blood glucose in Type 2 diabetic subjects. Journal of clinical & translational
endocrinology, 11, 26-30. https://doi.org/10.1016/j.jcte.2018.02.003
References
Douros, A., Yin, H., Yu, O. H. Y., Filion, K. B., Azoulay, L., & Suissa, S. (2017).
Pharmacologic differences of sulfonylureas and the risk of adverse cardiovascular and
hypoglycemic events. Diabetes Care, 40(11), 1506-1513.
https://doi.org/10.2337/dc17-0595
Gunaratne, K., Austin, E., & Wu, P. E. (2018). Unintentional sulfonylurea toxicity due to a
drug–drug interaction: a case report. BMC research notes, 11(1), 331.
doi: 10.1186/s13104-018-3404-8
Kalra, S., Bahendeka, S., Sahay, R., Ghosh, S., Md, F., Orabi, A., ... & Abhayaratna, S.
(2018). Consensus recommendations on sulfonylurea and sulfonylurea combinations
in the management of Type 2 diabetes mellitus–International Task Force. Indian
journal of endocrinology and metabolism, 22(1), 132.
Kovacs, P., & Pearson, E. (2016). Pharmacogenetics of sulfonylureas. In The Genetics of
Type 2 Diabetes and Related Traits (pp. 483-497). Springer, Cham.
https://doi.org/10.1007/978-3-319-01574-3_23
Lupsa, B. C., & Inzucchi, S. E. (2018). Diabetes medications and cardiovascular disease: at
long last progress. Current Opinion in Endocrinology & Diabetes and Obesity, 25(2),
87-93. DOI: https://doi.org/10.1097/MED.0000000000000400
MarElia, C. B., Kuehl, M. N., Shemwell, T. A., Alman, A. C., & Burkhardt, B. R. (2018).
Circulating PANDER concentration is associated with increased HbA1c and fasting
blood glucose in Type 2 diabetic subjects. Journal of clinical & translational
endocrinology, 11, 26-30. https://doi.org/10.1016/j.jcte.2018.02.003
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EDUCATIONAL BOOKLET 10
Shehata, M. M., Kamal, M. M., El-Hefnawy, M. H., & EL-Mesallamy, H. O. (2017).
Association of serum pancreatic derived factor (PANDER) with beta-cell dysfunction
in type 2 diabetes mellitus. Journal of Diabetes and its Complications, 31(4), 748-
752. https://doi.org/10.1016/j.jdiacomp.2017.01.001
Sola, D., Rossi, L., Schianca, G. P. C., Maffioli, P., Bigliocca, M., Mella, R., ... & Derosa, G.
(2015). Sulfonylureas and their use in clinical practice. Archives of medical science:
AMS, 11(4), 840. doi: 10.5114/aoms.2015.53304
Yu, O., Azoulay, L., Yin, H., Filion, K. B., & Suissa, S. (2018). Sulfonylureas as initial
treatment for type 2 diabetes and the risk of severe hypoglycemia. The American
journal of medicine, 131(3), 317-e11. https://doi.org/10.1016/j.amjmed.2017.09.044
Zaccardi, F., Webb, D. R., Yates, T., & Davies, M. J. (2016). Pathophysiology of type 1 and
type 2 diabetes mellitus: a 90-year perspective. Postgraduate medical
journal, 92(1084), 63-69. http://dx.doi.org/10.1136/postgradmedj-2015-133281
Shehata, M. M., Kamal, M. M., El-Hefnawy, M. H., & EL-Mesallamy, H. O. (2017).
Association of serum pancreatic derived factor (PANDER) with beta-cell dysfunction
in type 2 diabetes mellitus. Journal of Diabetes and its Complications, 31(4), 748-
752. https://doi.org/10.1016/j.jdiacomp.2017.01.001
Sola, D., Rossi, L., Schianca, G. P. C., Maffioli, P., Bigliocca, M., Mella, R., ... & Derosa, G.
(2015). Sulfonylureas and their use in clinical practice. Archives of medical science:
AMS, 11(4), 840. doi: 10.5114/aoms.2015.53304
Yu, O., Azoulay, L., Yin, H., Filion, K. B., & Suissa, S. (2018). Sulfonylureas as initial
treatment for type 2 diabetes and the risk of severe hypoglycemia. The American
journal of medicine, 131(3), 317-e11. https://doi.org/10.1016/j.amjmed.2017.09.044
Zaccardi, F., Webb, D. R., Yates, T., & Davies, M. J. (2016). Pathophysiology of type 1 and
type 2 diabetes mellitus: a 90-year perspective. Postgraduate medical
journal, 92(1084), 63-69. http://dx.doi.org/10.1136/postgradmedj-2015-133281
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





