Evidence-Based Nursing Research: Sedation Breaks in Intensive Care
VerifiedAdded on 2021/04/21
|6
|1388
|56
Homework Assignment
AI Summary
This assignment delves into evidence-based nursing research, specifically investigating the impact of daily sedation breaks on ventilation time for intensive care unit (ICU) patients. The research question explores whether sedation breaks can reduce the duration of mechanical ventilation. The methodology involves a PICO framework, defining the population (ICU patients), intervention (sedation breaks), comparison (no sedation breaks), and outcome (reduced ventilation time). The assignment outlines the search strategy, including keywords, synonyms, and databases (CINAHL, PubMed, Google Scholar). Inclusion and exclusion criteria are defined, such as age range, publication year, and language. The assignment provides a literature review discussing the importance of sedation in ICU, the potential benefits of sedation breaks, and the negative impacts of deep sedation. Search results from the databases are summarized, and key studies are cited, highlighting the evidence supporting the use of sedation breaks to improve patient outcomes, including reduced ventilation time and hospital stay duration. The document also includes tables summarizing search terms and results.

Running head: EVIDENCE BASED NURSING RESEARCH
EVIDENCE BASED NURSING RESEARCH
Name of the Student
Name of the University
Author note
EVIDENCE BASED NURSING RESEARCH
Name of the Student
Name of the University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

1EVIDENCE BASED NURSING RESEARCH
Do Intensive Care Patients who receive daily Sedation Breaks Have Reduced
Ventilation Time?
P Describe your patient (age, sex, race, past medical history, etc.), the disease, or main topic of your
question.
Intensive Care Patients
I What intervention or action are you considering -
treatment, diagnostic test, etc. Is there a specific
issue you’d like to investigate?
For this purpose, the sedation break is used as an
intervention to determine the reduced time of
ventilation.
M
E
T
H
O
D
O
L
O
G
Y
What research method should be used to
compare the intervention group with the
comparison (or control) group?
□ randomized controlled trial
□ cohort study
□ case-controlled studies
□ case reports
□ systematic reviews
□ meta-analysis
□ editorials/expert opinions
C Are you trying to compare or decide between two
options - drugs, a drug and no medication or
placebo, or two diagnostic tests? Your clinical
question does not always need a specific
comparison.
In this analysis comparison between Sedation
Breaks and NO Sedation Breaks was performed.
O What is the outcome you’d like to achieve? What are you trying to do for the patient? Relieve or
eliminate the symptoms? Reduce the number of adverse events? Improve function or test scores?
The two outcomes, that is targeted to achieve for intensive care patients through this process are-
Reduced Ventilation Time
Shorter Intubation Time
Use the table below to identify the key words and Synonyms for each of the 4 sections
Table 1: PICO and Search Terms
Population Intervention Comparison Outcome
Main keyword
Intensive
Care Patients
OR Critical
Care,
Sedation Break
OR
Sedation
Vacation OR
Sedation
Protocol OR
Sedation
Interruption
No
Comparison
Shorter Ventilation
OR Less
Ventilation OR
Reduced
Ventilation OR
Duration of
Ventilation
Synonym CINAHL:
MeSH:
CINAHL:
MeSH:
sedation, deep
sedation,
conscious
sedation,
CINAHL:
MeSH:
Do Intensive Care Patients who receive daily Sedation Breaks Have Reduced
Ventilation Time?
P Describe your patient (age, sex, race, past medical history, etc.), the disease, or main topic of your
question.
Intensive Care Patients
I What intervention or action are you considering -
treatment, diagnostic test, etc. Is there a specific
issue you’d like to investigate?
For this purpose, the sedation break is used as an
intervention to determine the reduced time of
ventilation.
M
E
T
H
O
D
O
L
O
G
Y
What research method should be used to
compare the intervention group with the
comparison (or control) group?
□ randomized controlled trial
□ cohort study
□ case-controlled studies
□ case reports
□ systematic reviews
□ meta-analysis
□ editorials/expert opinions
C Are you trying to compare or decide between two
options - drugs, a drug and no medication or
placebo, or two diagnostic tests? Your clinical
question does not always need a specific
comparison.
In this analysis comparison between Sedation
Breaks and NO Sedation Breaks was performed.
O What is the outcome you’d like to achieve? What are you trying to do for the patient? Relieve or
eliminate the symptoms? Reduce the number of adverse events? Improve function or test scores?
The two outcomes, that is targeted to achieve for intensive care patients through this process are-
Reduced Ventilation Time
Shorter Intubation Time
Use the table below to identify the key words and Synonyms for each of the 4 sections
Table 1: PICO and Search Terms
Population Intervention Comparison Outcome
Main keyword
Intensive
Care Patients
OR Critical
Care,
Sedation Break
OR
Sedation
Vacation OR
Sedation
Protocol OR
Sedation
Interruption
No
Comparison
Shorter Ventilation
OR Less
Ventilation OR
Reduced
Ventilation OR
Duration of
Ventilation
Synonym CINAHL:
MeSH:
CINAHL:
MeSH:
sedation, deep
sedation,
conscious
sedation,
CINAHL:
MeSH:

2EVIDENCE BASED NURSING RESEARCH
conscious
sedation
Sedation hold
List databases you plan to search: CINAHL, PubMed or PubMed Clinical Trials, PsyArticles.
-CINAHL
-PubMed
-Google Scholar
Three databases were searched i.e. CINAHL, PubMed and Google Scholar using the exact search terms
outlined in Table 1.
List other criteria –gender, age, year of publication, language to be used to limit your
search.
The age of the patient can vary from 40 to 85 years
irrespective of the gender the intervention can be applied
the year of publication was restricted to last ten years
language was restricted to English
Sedation is an important aspect of healthcare for the patients receiving intensive care,
as it helps them to reduce their stress and depression related to the healthcare practice and
minimizes their response to the external environmental factors (Shebabi et al., 2012).
Therefore sedation holds an important place in the care process for critically ill patients as
duration of sedation determines the rate of attaining wellbeing in the patients. There are
different systems through which, the sedation limit for particular patients can be assessed
such as electroencephalograms, bispectral index and different non-pharmacological process
ensuing patient comfort and wellbeing (Barr et al., 2013).
The goal of this activity is to identify the effect of breaks in sedation to reduce the
ventilation time. Patients in Intensive Care routinely receive sedation to facilitate ventilation,
intubation and tolerance of tubes and lines that is responsible for the cause of anxiety and
distress. Historically it was thought that a patient in Intensive Care should be kept deeply
sedated. However, medical staffs nowadays are trying to change their practice in accordance
with the most recent data but still both doctors and nurses need to be reminded of the
importance of daily sedation breaks. Devlin and Roberts (2011), suggest that patients who
receive daily sedation breaks have a shorter duration in ventilation. Different studies have
determined that deep sedations are responsible for the poor long-term outcomes such as
conscious
sedation
Sedation hold
List databases you plan to search: CINAHL, PubMed or PubMed Clinical Trials, PsyArticles.
-CINAHL
-PubMed
-Google Scholar
Three databases were searched i.e. CINAHL, PubMed and Google Scholar using the exact search terms
outlined in Table 1.
List other criteria –gender, age, year of publication, language to be used to limit your
search.
The age of the patient can vary from 40 to 85 years
irrespective of the gender the intervention can be applied
the year of publication was restricted to last ten years
language was restricted to English
Sedation is an important aspect of healthcare for the patients receiving intensive care,
as it helps them to reduce their stress and depression related to the healthcare practice and
minimizes their response to the external environmental factors (Shebabi et al., 2012).
Therefore sedation holds an important place in the care process for critically ill patients as
duration of sedation determines the rate of attaining wellbeing in the patients. There are
different systems through which, the sedation limit for particular patients can be assessed
such as electroencephalograms, bispectral index and different non-pharmacological process
ensuing patient comfort and wellbeing (Barr et al., 2013).
The goal of this activity is to identify the effect of breaks in sedation to reduce the
ventilation time. Patients in Intensive Care routinely receive sedation to facilitate ventilation,
intubation and tolerance of tubes and lines that is responsible for the cause of anxiety and
distress. Historically it was thought that a patient in Intensive Care should be kept deeply
sedated. However, medical staffs nowadays are trying to change their practice in accordance
with the most recent data but still both doctors and nurses need to be reminded of the
importance of daily sedation breaks. Devlin and Roberts (2011), suggest that patients who
receive daily sedation breaks have a shorter duration in ventilation. Different studies have
determined that deep sedations are responsible for the poor long-term outcomes such as
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3EVIDENCE BASED NURSING RESEARCH
cognitive skill deficiencies, psychological issues and issues related to mortality. Other issues
related to sedation arises in the patients of intensive care as unpredictable pharmacokinetics
and dynamics within the ICU alters the drug interaction, impaired functioning of different
organs therefore, it needs proper treatment strategy. Furthermore, other drawbacks to deep
sedation include an increase in the length of stay not only in the ICU but also a patient’s
overall length of hospital stay. Several interventions are recommended to help with this issue
of poor long-term outcomes such as application of pain assessment, goal-directed therapeutic
care and many more. One of these interventions is the implementation of daily sedation
breaks (Hughes, McGrane & Pandharipande, 2012).
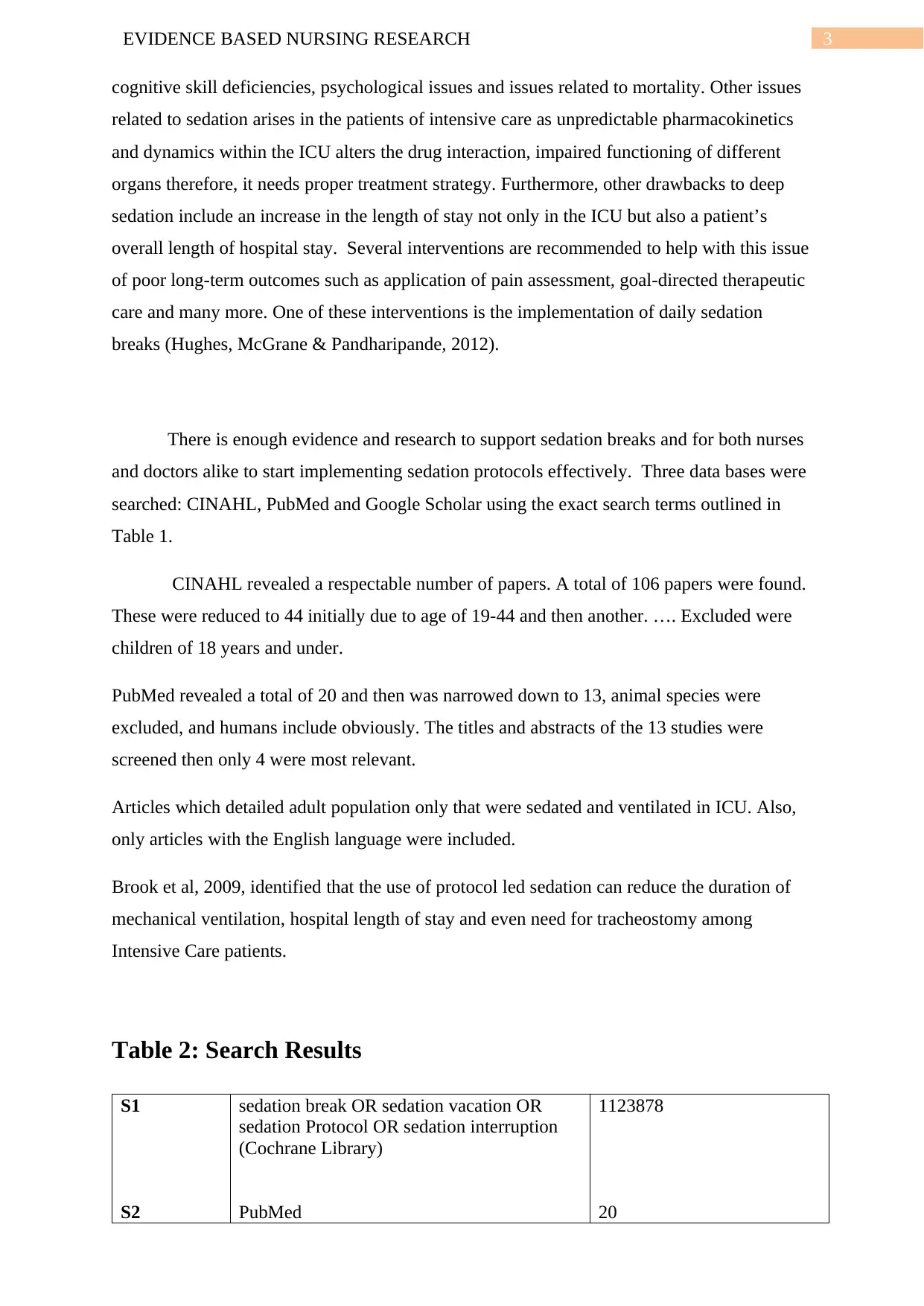
There is enough evidence and research to support sedation breaks and for both nurses
and doctors alike to start implementing sedation protocols effectively. Three data bases were
searched: CINAHL, PubMed and Google Scholar using the exact search terms outlined in
Table 1.
CINAHL revealed a respectable number of papers. A total of 106 papers were found.
These were reduced to 44 initially due to age of 19-44 and then another. …. Excluded were
children of 18 years and under.
PubMed revealed a total of 20 and then was narrowed down to 13, animal species were
excluded, and humans include obviously. The titles and abstracts of the 13 studies were
screened then only 4 were most relevant.
Articles which detailed adult population only that were sedated and ventilated in ICU. Also,
only articles with the English language were included.
Brook et al, 2009, identified that the use of protocol led sedation can reduce the duration of
mechanical ventilation, hospital length of stay and even need for tracheostomy among
Intensive Care patients.
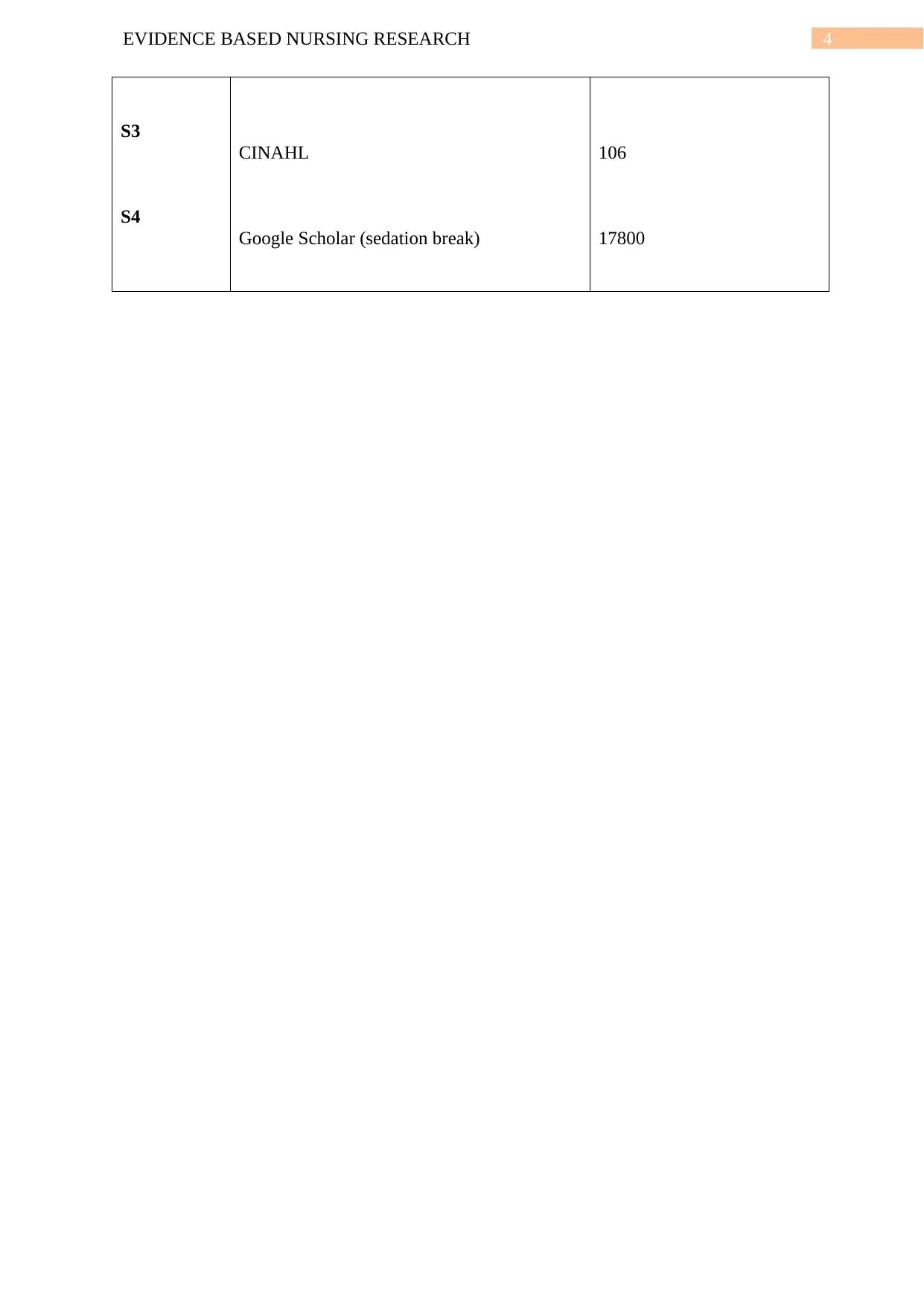
Table 2: Search Results
S1
S2
sedation break OR sedation vacation OR
sedation Protocol OR sedation interruption
(Cochrane Library)
PubMed
1123878
20
cognitive skill deficiencies, psychological issues and issues related to mortality. Other issues
related to sedation arises in the patients of intensive care as unpredictable pharmacokinetics
and dynamics within the ICU alters the drug interaction, impaired functioning of different
organs therefore, it needs proper treatment strategy. Furthermore, other drawbacks to deep
sedation include an increase in the length of stay not only in the ICU but also a patient’s
overall length of hospital stay. Several interventions are recommended to help with this issue
of poor long-term outcomes such as application of pain assessment, goal-directed therapeutic
care and many more. One of these interventions is the implementation of daily sedation
breaks (Hughes, McGrane & Pandharipande, 2012).
There is enough evidence and research to support sedation breaks and for both nurses
and doctors alike to start implementing sedation protocols effectively. Three data bases were
searched: CINAHL, PubMed and Google Scholar using the exact search terms outlined in
Table 1.
CINAHL revealed a respectable number of papers. A total of 106 papers were found.
These were reduced to 44 initially due to age of 19-44 and then another. …. Excluded were
children of 18 years and under.
PubMed revealed a total of 20 and then was narrowed down to 13, animal species were
excluded, and humans include obviously. The titles and abstracts of the 13 studies were
screened then only 4 were most relevant.
Articles which detailed adult population only that were sedated and ventilated in ICU. Also,
only articles with the English language were included.
Brook et al, 2009, identified that the use of protocol led sedation can reduce the duration of
mechanical ventilation, hospital length of stay and even need for tracheostomy among
Intensive Care patients.
Table 2: Search Results
S1
S2
sedation break OR sedation vacation OR
sedation Protocol OR sedation interruption
(Cochrane Library)
PubMed
1123878
20
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4EVIDENCE BASED NURSING RESEARCH
S3
S4
CINAHL
Google Scholar (sedation break)
106
17800
S3
S4
CINAHL
Google Scholar (sedation break)
106
17800

5EVIDENCE BASED NURSING RESEARCH
References
Barr, J., Fraser, G. L., Puntillo, K., Ely, E. W., Gélinas, C., Dasta, J. F., ... & Coursin, D. B.
(2013). Clinical practice guidelines for the management of pain, agitation, and
delirium in adult patients in the intensive care unit. Critical care medicine, 41(1), 263-
306.
Hughes, C. G., McGrane, S., & Pandharipande, P. P. (2012). Sedation in the intensive care
setting. Clinical pharmacology: advances and applications, 4, 53.
Kallet, R. H., et al. (2018). "Spontaneous Breathing Trials and Conservative Sedation
Practices Reduce Mechanical Ventilation Duration in Subjects With ARDS."
Respiratory Care 63(1): 1-10.
Kress, J. P., et al. (2000). "Daily interruption of sedative infusions in critically ill patients
undergoing mechanical ventilation." N Engl J Med 342(20): 1471-1477.
Pinder, S. and M. Christensen (2008). "Sedation breaks: are they good for the critically ill
patient? A review." Nursing in Critical Care 13(2): 64-70.
Shehabi, Y., Bellomo, R., Reade, M. C., Bailey, M., Bass, F., Howe, B., ... & Weisbrodt, L.
(2012). Sedation Practice in Intensive Care Evaluation (SPICE) Study Investigators;
ANZICS Clinical Trials Group. Early intensive care sedation predicts long-term
mortality in ventilated critically ill patients. Am J Respir Crit Care Med, 186(8), 724-
31.
References
Barr, J., Fraser, G. L., Puntillo, K., Ely, E. W., Gélinas, C., Dasta, J. F., ... & Coursin, D. B.
(2013). Clinical practice guidelines for the management of pain, agitation, and
delirium in adult patients in the intensive care unit. Critical care medicine, 41(1), 263-
306.
Hughes, C. G., McGrane, S., & Pandharipande, P. P. (2012). Sedation in the intensive care
setting. Clinical pharmacology: advances and applications, 4, 53.
Kallet, R. H., et al. (2018). "Spontaneous Breathing Trials and Conservative Sedation
Practices Reduce Mechanical Ventilation Duration in Subjects With ARDS."
Respiratory Care 63(1): 1-10.
Kress, J. P., et al. (2000). "Daily interruption of sedative infusions in critically ill patients
undergoing mechanical ventilation." N Engl J Med 342(20): 1471-1477.
Pinder, S. and M. Christensen (2008). "Sedation breaks: are they good for the critically ill
patient? A review." Nursing in Critical Care 13(2): 64-70.
Shehabi, Y., Bellomo, R., Reade, M. C., Bailey, M., Bass, F., Howe, B., ... & Weisbrodt, L.
(2012). Sedation Practice in Intensive Care Evaluation (SPICE) Study Investigators;
ANZICS Clinical Trials Group. Early intensive care sedation predicts long-term
mortality in ventilated critically ill patients. Am J Respir Crit Care Med, 186(8), 724-
31.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





