Reference List Analysis and Summary
VerifiedAdded on 2020/05/16
|24
|4883
|49
AI Summary
This assignment tasks you with carefully examining a provided list of references related to healthcare topics such as prenatal testing, cost-effectiveness analysis in medicine, and the role of laboratory testing. The goal is to demonstrate your understanding of these concepts by analyzing the specific details within each reference.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
BUSINESS PLAN FOR STRATEGIES TO
CUT DOWN COST BY PHYSICIAN NOT
OFFERING UNNECESSARY TESTS
Student Name: Student ID:
Unit Name: Unit ID:
Date Due: Professor Name:
CUT DOWN COST BY PHYSICIAN NOT
OFFERING UNNECESSARY TESTS
Student Name: Student ID:
Unit Name: Unit ID:
Date Due: Professor Name:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

Executive Summary
Rising costs in the healthcare systems have been a huge worry for policy makers, insurance
companies, politicians and especially patient parties. Patients have often been prescribed a
number of tests that raise costs for overall treatment delivery. The scope of this project deals
with strategies that can impact substantial reduction in healthcare costs. An analysis of steps
according to algorithm and process map has been incorporated. New processes and procedure
along with changes in project objectives are defined that can bring about reduction in costs for
overall health care system. Objective definition includes changes to be impended to stakeholder
of the entire healthcare system. With such changes in strategies there is bound to be
transformations in financial implication for the entire health industry. Cost benefit analysis for
the transformed system needs to be analysed based upon the intensity of the care. Better costing
systems are assessed that can yield benefit for the entire health care industry. A timeline has been
provided for impending changes to be brought about in the healthcare industry which is depicted
by means of a GANTT chart. Further a continuous improvement and evaluation tool is included
such that quality healthcare can be provided at affordable costs. Recommendations while
conducting this critical study could easily be understood will be adopting new strategies and
implementing them into action for generation of greater impact.
Rising costs in the healthcare systems have been a huge worry for policy makers, insurance
companies, politicians and especially patient parties. Patients have often been prescribed a
number of tests that raise costs for overall treatment delivery. The scope of this project deals
with strategies that can impact substantial reduction in healthcare costs. An analysis of steps
according to algorithm and process map has been incorporated. New processes and procedure
along with changes in project objectives are defined that can bring about reduction in costs for
overall health care system. Objective definition includes changes to be impended to stakeholder
of the entire healthcare system. With such changes in strategies there is bound to be
transformations in financial implication for the entire health industry. Cost benefit analysis for
the transformed system needs to be analysed based upon the intensity of the care. Better costing
systems are assessed that can yield benefit for the entire health care industry. A timeline has been
provided for impending changes to be brought about in the healthcare industry which is depicted
by means of a GANTT chart. Further a continuous improvement and evaluation tool is included
such that quality healthcare can be provided at affordable costs. Recommendations while
conducting this critical study could easily be understood will be adopting new strategies and
implementing them into action for generation of greater impact.
Table of Contents
Executive Summary.........................................................................................................................2
Table of Figures...............................................................................................................................3
1.0 Introduction................................................................................................................................4
2.0 Algorithm...................................................................................................................................4
3.0 Process Map...............................................................................................................................6
4.0 New Procedure...........................................................................................................................8
5.0 Change Project Objectives.........................................................................................................9
6.0 Financial Implications.............................................................................................................11
7.0 Staff Implications.....................................................................................................................12
8.0 Cost/Benefit Ratio...................................................................................................................14
9.0 Timeline for Implementation...................................................................................................15
10.0 Tool to Evaluate Implementation of the Project....................................................................16
11.0 Chart/ Summary of National Standards, Accrediting body standards, regulatory body
standards........................................................................................................................................18
12.0 Comparison of best practices and standards compared to current facility practices.............19
13.0 Conclusion and Recommendation.........................................................................................20
Reference Lists..............................................................................................................................22
Table of Figures
Figure 1: Algorithm for Cost Cutting in Prescription of Medical Tests.......................................................5
Figure 2: Process Map.................................................................................................................................7
Figure 3: Cost Overheads Break Up..........................................................................................................14
Figure 4: CBA for the Project....................................................................................................................14
Figure 5: Gantt Chart for New Strategy Application.................................................................................16
Figure 6:PDCA Cycle................................................................................................................................17
Executive Summary.........................................................................................................................2
Table of Figures...............................................................................................................................3
1.0 Introduction................................................................................................................................4
2.0 Algorithm...................................................................................................................................4
3.0 Process Map...............................................................................................................................6
4.0 New Procedure...........................................................................................................................8
5.0 Change Project Objectives.........................................................................................................9
6.0 Financial Implications.............................................................................................................11
7.0 Staff Implications.....................................................................................................................12
8.0 Cost/Benefit Ratio...................................................................................................................14
9.0 Timeline for Implementation...................................................................................................15
10.0 Tool to Evaluate Implementation of the Project....................................................................16
11.0 Chart/ Summary of National Standards, Accrediting body standards, regulatory body
standards........................................................................................................................................18
12.0 Comparison of best practices and standards compared to current facility practices.............19
13.0 Conclusion and Recommendation.........................................................................................20
Reference Lists..............................................................................................................................22
Table of Figures
Figure 1: Algorithm for Cost Cutting in Prescription of Medical Tests.......................................................5
Figure 2: Process Map.................................................................................................................................7
Figure 3: Cost Overheads Break Up..........................................................................................................14
Figure 4: CBA for the Project....................................................................................................................14
Figure 5: Gantt Chart for New Strategy Application.................................................................................16
Figure 6:PDCA Cycle................................................................................................................................17
1.0 Introduction
Healthcare sector within the US is gradually expanding however it caters to a segment of the
society. The weaker section of the society cannot afford best possible healthcare as doctors often
recommend unnecessary clinical tests that raises costs of medical bill (Kotler, 2011). With rising
costs in healthcare facilities, there is an increase in financial stress amongst varied groups of
people. The scope of this project concerns development of strategies to cut down on high health
care costs in hospitals by way of reducing the burden of unnecessary clinical tests. Despite
presence of a large number of health and insurance plans in the market, cost related to medical
continues to grow. In most cases health insurance companies requires patient to bear 20% of total
medical bills. Often a sizable proportion of which is wasted, which if avoided could lead to
decrease in health care costs. Appropriate allocation of resources and proper management in
healthcare systems can help upkeep quality of patient care and reduce physicians from
prescribing unnecessary tests. Most physicians operates as business units where medical units
also demand substantially higher prices to be paid for medical treatments. The scope of this
business strategy is to identify key stakeholders that contribute significantly to such increase in
costs and then overcoming challenges in meeting external costs.
2.0 Algorithm
Healthcare costs in the US exceeds 17% of total GDP and depicts further rising trends. While
other countries also have increasing trends but spends comparably less compared to US. Experts
suggests various reasons behind such increasing trends as ageing population and development of
newer treatments (Garfield, 2012). Prescribing of unnecessary medical tests can be attributed a
Healthcare sector within the US is gradually expanding however it caters to a segment of the
society. The weaker section of the society cannot afford best possible healthcare as doctors often
recommend unnecessary clinical tests that raises costs of medical bill (Kotler, 2011). With rising
costs in healthcare facilities, there is an increase in financial stress amongst varied groups of
people. The scope of this project concerns development of strategies to cut down on high health
care costs in hospitals by way of reducing the burden of unnecessary clinical tests. Despite
presence of a large number of health and insurance plans in the market, cost related to medical
continues to grow. In most cases health insurance companies requires patient to bear 20% of total
medical bills. Often a sizable proportion of which is wasted, which if avoided could lead to
decrease in health care costs. Appropriate allocation of resources and proper management in
healthcare systems can help upkeep quality of patient care and reduce physicians from
prescribing unnecessary tests. Most physicians operates as business units where medical units
also demand substantially higher prices to be paid for medical treatments. The scope of this
business strategy is to identify key stakeholders that contribute significantly to such increase in
costs and then overcoming challenges in meeting external costs.
2.0 Algorithm
Healthcare costs in the US exceeds 17% of total GDP and depicts further rising trends. While
other countries also have increasing trends but spends comparably less compared to US. Experts
suggests various reasons behind such increasing trends as ageing population and development of
newer treatments (Garfield, 2012). Prescribing of unnecessary medical tests can be attributed a
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

fundamental reason for such escalation in costs structures. Absence in understanding ways costs
can compared outcomes of patients can help focus on causes of treating patients. Policy makers
and politicians further argue that burden of costs that they bear along with health insurance
companies for delivering patient treatment rather than focusing on costs that patients bear. While
payer reducing reimbursement does not reduce bill or lowers overall costs, rather it reduces bills
borne by insurers. In order to develop strategies for reduction in healthcare costs by reducing
number of tests prescribed by physicians, the following course or algorithm will be followed.
Figure 1: Algorithm for Cost Cutting in Prescription of Medical Tests
Source: Author
can compared outcomes of patients can help focus on causes of treating patients. Policy makers
and politicians further argue that burden of costs that they bear along with health insurance
companies for delivering patient treatment rather than focusing on costs that patients bear. While
payer reducing reimbursement does not reduce bill or lowers overall costs, rather it reduces bills
borne by insurers. In order to develop strategies for reduction in healthcare costs by reducing
number of tests prescribed by physicians, the following course or algorithm will be followed.
Figure 1: Algorithm for Cost Cutting in Prescription of Medical Tests
Source: Author
3.0 Process Map
A process map depicts flow of information and resources through decision making alternatives.
In this current situation a process map will depict flow of information through a particular
hospital or healthcare institute such that patient care can be delivered. A process map will
include all relevant stakeholders along with decisions processes involved in order to cater to
patient care (McCormick, 2012). The below depicted process map can be used to deliver patient
care reducing unnecessary costs that might raise costs associated with overall treatment.
Allocation of resources to departments and services is done on actual resources and not on basis
of reimbursement value.
A process map depicts flow of information and resources through decision making alternatives.
In this current situation a process map will depict flow of information through a particular
hospital or healthcare institute such that patient care can be delivered. A process map will
include all relevant stakeholders along with decisions processes involved in order to cater to
patient care (McCormick, 2012). The below depicted process map can be used to deliver patient
care reducing unnecessary costs that might raise costs associated with overall treatment.
Allocation of resources to departments and services is done on actual resources and not on basis
of reimbursement value.
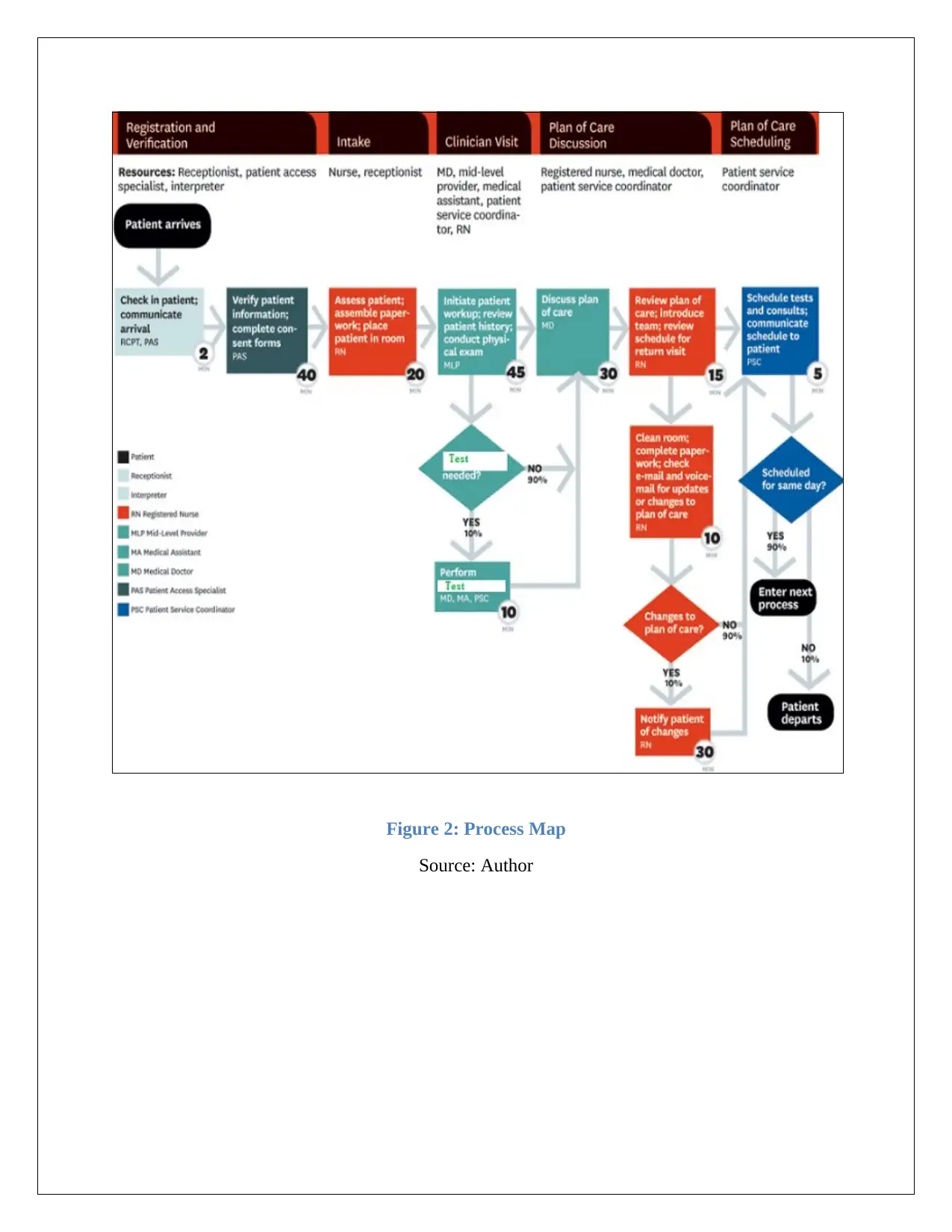
Figure 2: Process Map
Source: Author
Source: Author
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
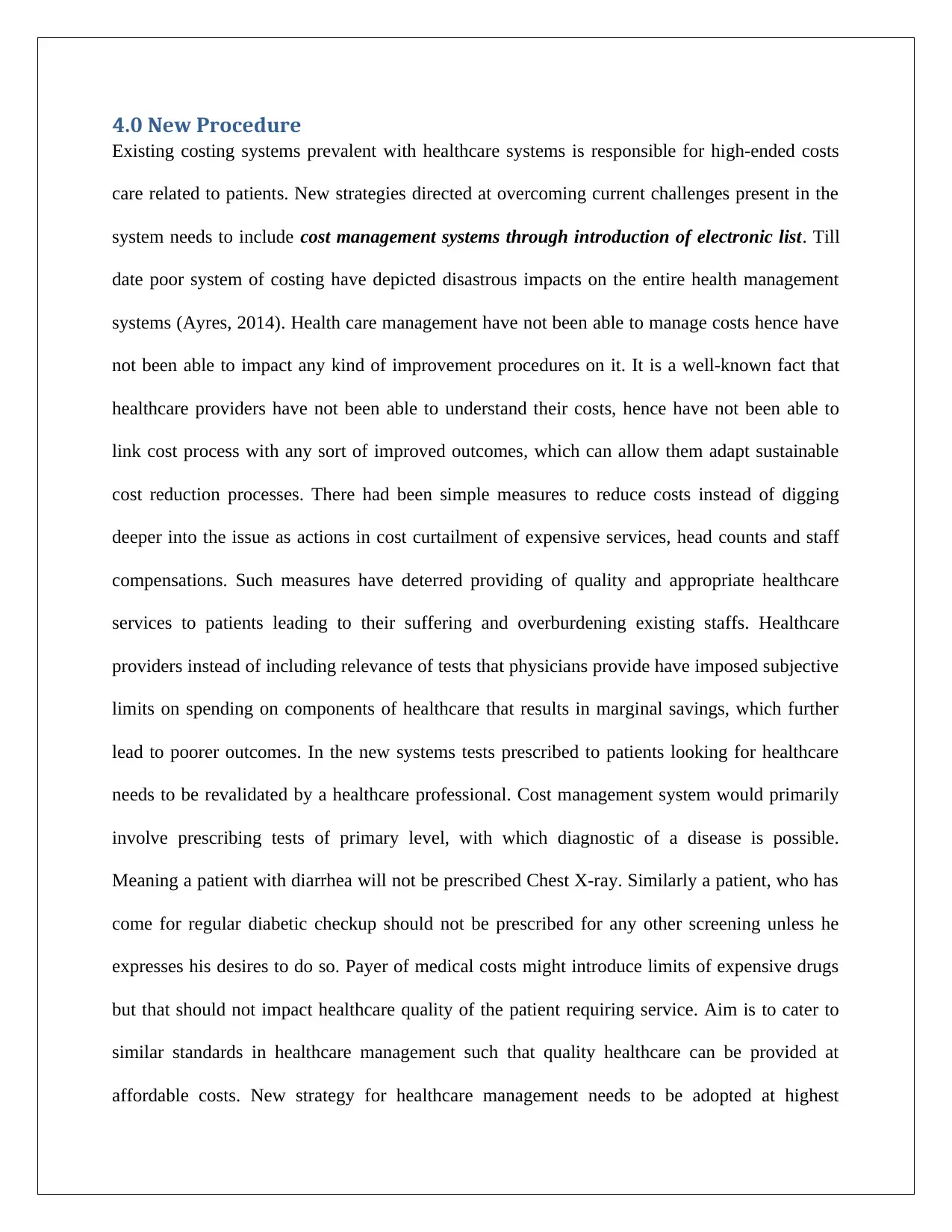
4.0 New Procedure
Existing costing systems prevalent with healthcare systems is responsible for high-ended costs
care related to patients. New strategies directed at overcoming current challenges present in the
system needs to include cost management systems through introduction of electronic list. Till
date poor system of costing have depicted disastrous impacts on the entire health management
systems (Ayres, 2014). Health care management have not been able to manage costs hence have
not been able to impact any kind of improvement procedures on it. It is a well-known fact that
healthcare providers have not been able to understand their costs, hence have not been able to
link cost process with any sort of improved outcomes, which can allow them adapt sustainable
cost reduction processes. There had been simple measures to reduce costs instead of digging
deeper into the issue as actions in cost curtailment of expensive services, head counts and staff
compensations. Such measures have deterred providing of quality and appropriate healthcare
services to patients leading to their suffering and overburdening existing staffs. Healthcare
providers instead of including relevance of tests that physicians provide have imposed subjective
limits on spending on components of healthcare that results in marginal savings, which further
lead to poorer outcomes. In the new systems tests prescribed to patients looking for healthcare
needs to be revalidated by a healthcare professional. Cost management system would primarily
involve prescribing tests of primary level, with which diagnostic of a disease is possible.
Meaning a patient with diarrhea will not be prescribed Chest X-ray. Similarly a patient, who has
come for regular diabetic checkup should not be prescribed for any other screening unless he
expresses his desires to do so. Payer of medical costs might introduce limits of expensive drugs
but that should not impact healthcare quality of the patient requiring service. Aim is to cater to
similar standards in healthcare management such that quality healthcare can be provided at
affordable costs. New strategy for healthcare management needs to be adopted at highest
Existing costing systems prevalent with healthcare systems is responsible for high-ended costs
care related to patients. New strategies directed at overcoming current challenges present in the
system needs to include cost management systems through introduction of electronic list. Till
date poor system of costing have depicted disastrous impacts on the entire health management
systems (Ayres, 2014). Health care management have not been able to manage costs hence have
not been able to impact any kind of improvement procedures on it. It is a well-known fact that
healthcare providers have not been able to understand their costs, hence have not been able to
link cost process with any sort of improved outcomes, which can allow them adapt sustainable
cost reduction processes. There had been simple measures to reduce costs instead of digging
deeper into the issue as actions in cost curtailment of expensive services, head counts and staff
compensations. Such measures have deterred providing of quality and appropriate healthcare
services to patients leading to their suffering and overburdening existing staffs. Healthcare
providers instead of including relevance of tests that physicians provide have imposed subjective
limits on spending on components of healthcare that results in marginal savings, which further
lead to poorer outcomes. In the new systems tests prescribed to patients looking for healthcare
needs to be revalidated by a healthcare professional. Cost management system would primarily
involve prescribing tests of primary level, with which diagnostic of a disease is possible.
Meaning a patient with diarrhea will not be prescribed Chest X-ray. Similarly a patient, who has
come for regular diabetic checkup should not be prescribed for any other screening unless he
expresses his desires to do so. Payer of medical costs might introduce limits of expensive drugs
but that should not impact healthcare quality of the patient requiring service. Aim is to cater to
similar standards in healthcare management such that quality healthcare can be provided at
affordable costs. New strategy for healthcare management needs to be adopted at highest
possible level of healthcare and all stakeholders needs to abide by it. In case hospital authority
decides to reduce tests that is prescribed to patient care but physicians needs to abide by the same
(Carreyrou, 2008). Staff needs to follow instructions specific to such strategies to bring down
costs hence impact to overall healthcare facilities. This will allow people from all section of the
society avail quality healthcare facilities.
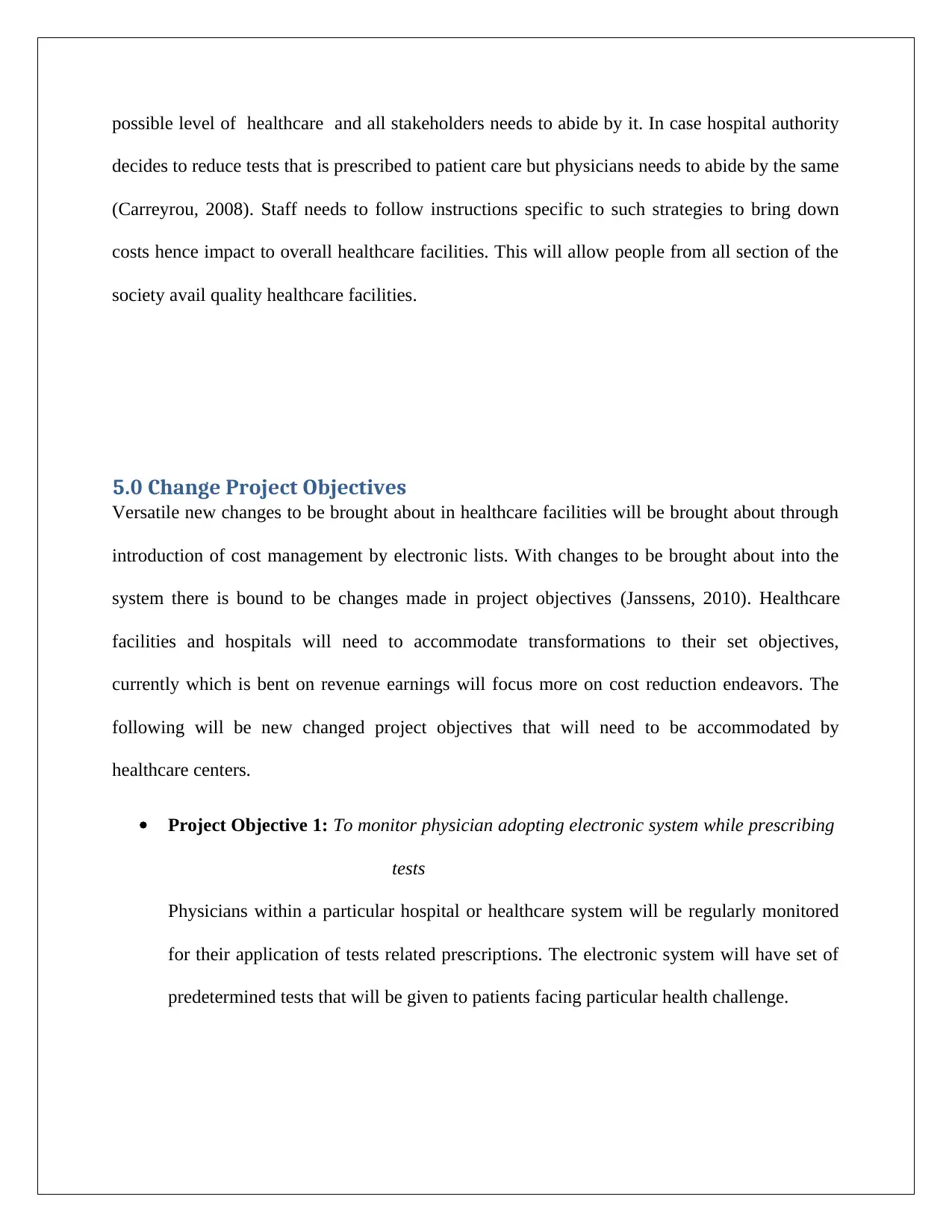
5.0 Change Project Objectives
Versatile new changes to be brought about in healthcare facilities will be brought about through
introduction of cost management by electronic lists. With changes to be brought about into the
system there is bound to be changes made in project objectives (Janssens, 2010). Healthcare
facilities and hospitals will need to accommodate transformations to their set objectives,
currently which is bent on revenue earnings will focus more on cost reduction endeavors. The
following will be new changed project objectives that will need to be accommodated by
healthcare centers.
Project Objective 1: To monitor physician adopting electronic system while prescribing
tests
Physicians within a particular hospital or healthcare system will be regularly monitored
for their application of tests related prescriptions. The electronic system will have set of
predetermined tests that will be given to patients facing particular health challenge.
decides to reduce tests that is prescribed to patient care but physicians needs to abide by the same
(Carreyrou, 2008). Staff needs to follow instructions specific to such strategies to bring down
costs hence impact to overall healthcare facilities. This will allow people from all section of the
society avail quality healthcare facilities.
5.0 Change Project Objectives
Versatile new changes to be brought about in healthcare facilities will be brought about through
introduction of cost management by electronic lists. With changes to be brought about into the
system there is bound to be changes made in project objectives (Janssens, 2010). Healthcare
facilities and hospitals will need to accommodate transformations to their set objectives,
currently which is bent on revenue earnings will focus more on cost reduction endeavors. The
following will be new changed project objectives that will need to be accommodated by
healthcare centers.
Project Objective 1: To monitor physician adopting electronic system while prescribing
tests
Physicians within a particular hospital or healthcare system will be regularly monitored
for their application of tests related prescriptions. The electronic system will have set of
predetermined tests that will be given to patients facing particular health challenge.
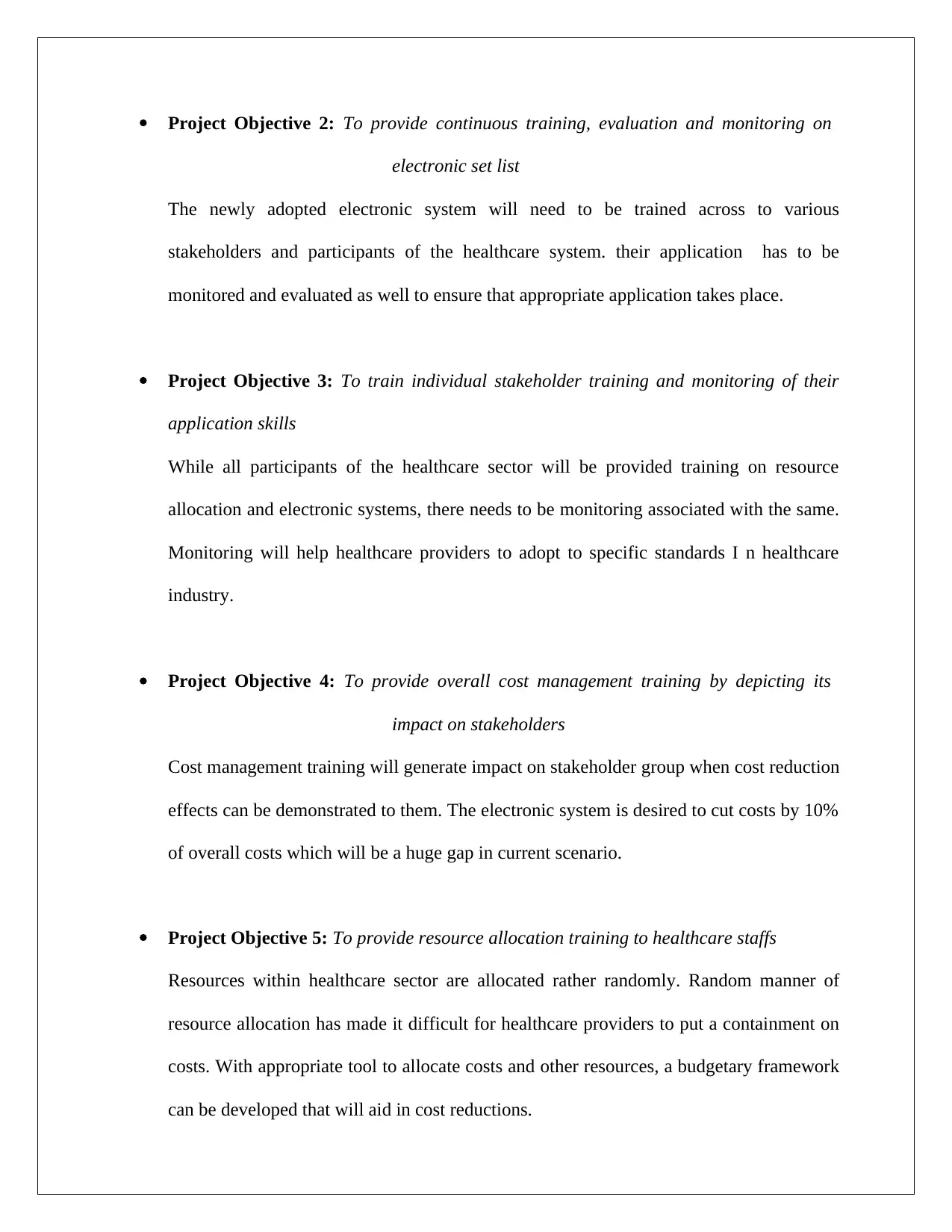
Project Objective 2: To provide continuous training, evaluation and monitoring on
electronic set list
The newly adopted electronic system will need to be trained across to various
stakeholders and participants of the healthcare system. their application has to be
monitored and evaluated as well to ensure that appropriate application takes place.
Project Objective 3: To train individual stakeholder training and monitoring of their
application skills
While all participants of the healthcare sector will be provided training on resource
allocation and electronic systems, there needs to be monitoring associated with the same.
Monitoring will help healthcare providers to adopt to specific standards I n healthcare
industry.
Project Objective 4: To provide overall cost management training by depicting its
impact on stakeholders
Cost management training will generate impact on stakeholder group when cost reduction
effects can be demonstrated to them. The electronic system is desired to cut costs by 10%
of overall costs which will be a huge gap in current scenario.
Project Objective 5: To provide resource allocation training to healthcare staffs
Resources within healthcare sector are allocated rather randomly. Random manner of
resource allocation has made it difficult for healthcare providers to put a containment on
costs. With appropriate tool to allocate costs and other resources, a budgetary framework
can be developed that will aid in cost reductions.
electronic set list
The newly adopted electronic system will need to be trained across to various
stakeholders and participants of the healthcare system. their application has to be
monitored and evaluated as well to ensure that appropriate application takes place.
Project Objective 3: To train individual stakeholder training and monitoring of their
application skills
While all participants of the healthcare sector will be provided training on resource
allocation and electronic systems, there needs to be monitoring associated with the same.
Monitoring will help healthcare providers to adopt to specific standards I n healthcare
industry.
Project Objective 4: To provide overall cost management training by depicting its
impact on stakeholders
Cost management training will generate impact on stakeholder group when cost reduction
effects can be demonstrated to them. The electronic system is desired to cut costs by 10%
of overall costs which will be a huge gap in current scenario.
Project Objective 5: To provide resource allocation training to healthcare staffs
Resources within healthcare sector are allocated rather randomly. Random manner of
resource allocation has made it difficult for healthcare providers to put a containment on
costs. With appropriate tool to allocate costs and other resources, a budgetary framework
can be developed that will aid in cost reductions.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
The above objectives set will help adapt to new procedures easily and meet goals adequately.
Once these objectives has been environed, there will appropriate implementation such that goals
and objectives can be met appropriately.
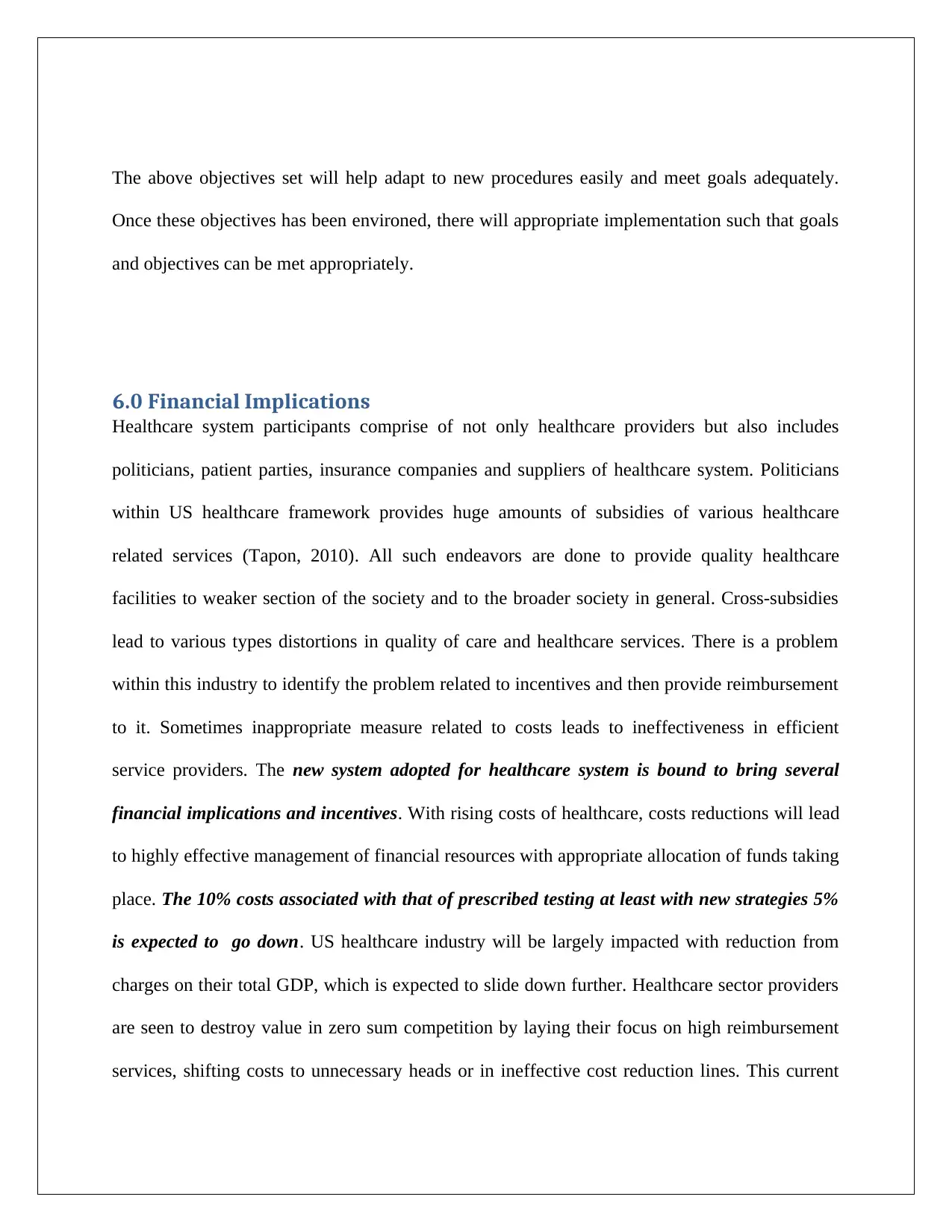
6.0 Financial Implications
Healthcare system participants comprise of not only healthcare providers but also includes
politicians, patient parties, insurance companies and suppliers of healthcare system. Politicians
within US healthcare framework provides huge amounts of subsidies of various healthcare
related services (Tapon, 2010). All such endeavors are done to provide quality healthcare
facilities to weaker section of the society and to the broader society in general. Cross-subsidies
lead to various types distortions in quality of care and healthcare services. There is a problem
within this industry to identify the problem related to incentives and then provide reimbursement
to it. Sometimes inappropriate measure related to costs leads to ineffectiveness in efficient
service providers. The new system adopted for healthcare system is bound to bring several
financial implications and incentives. With rising costs of healthcare, costs reductions will lead
to highly effective management of financial resources with appropriate allocation of funds taking
place. The 10% costs associated with that of prescribed testing at least with new strategies 5%
is expected to go down. US healthcare industry will be largely impacted with reduction from
charges on their total GDP, which is expected to slide down further. Healthcare sector providers
are seen to destroy value in zero sum competition by laying their focus on high reimbursement
services, shifting costs to unnecessary heads or in ineffective cost reduction lines. This current
Once these objectives has been environed, there will appropriate implementation such that goals
and objectives can be met appropriately.
6.0 Financial Implications
Healthcare system participants comprise of not only healthcare providers but also includes
politicians, patient parties, insurance companies and suppliers of healthcare system. Politicians
within US healthcare framework provides huge amounts of subsidies of various healthcare
related services (Tapon, 2010). All such endeavors are done to provide quality healthcare
facilities to weaker section of the society and to the broader society in general. Cross-subsidies
lead to various types distortions in quality of care and healthcare services. There is a problem
within this industry to identify the problem related to incentives and then provide reimbursement
to it. Sometimes inappropriate measure related to costs leads to ineffectiveness in efficient
service providers. The new system adopted for healthcare system is bound to bring several
financial implications and incentives. With rising costs of healthcare, costs reductions will lead
to highly effective management of financial resources with appropriate allocation of funds taking
place. The 10% costs associated with that of prescribed testing at least with new strategies 5%
is expected to go down. US healthcare industry will be largely impacted with reduction from
charges on their total GDP, which is expected to slide down further. Healthcare sector providers
are seen to destroy value in zero sum competition by laying their focus on high reimbursement
services, shifting costs to unnecessary heads or in ineffective cost reduction lines. This current
system will enhance access to inefficient systems attending to fundamental value issue, which is
to provide quality healthcare at affordable costs.
The new measure does not require any medical science breakthroughs as it entails ascertaining
cost and comparing them to outcomes related to patients. Value in healthcare systems is
measured by patient outcomes that are generated per dollar spent (Wolfson, 2014). It can be
derived from this, more the number of services delivered more expensive the care and not
necessarily amounting to better care. There are a hosts of healthcare centers that are currently
incorporating such measures as the Cleft Lip and Palate Program at Children’s Hospital in
Boston , the Head and Neck Center at MD Anderson Cancer Center in Houston, and Brigham &
Women’s Hospital in Boston and units performing knee replacements at Schön Klinik in
Germany. Financial implications for these healthcare centers along with those that implement
measures for cost reductions is bound to take place. Overall it can be estimated with gradual
declining of patient’s bill at these centers, there is bound to be more patients at some healthcare
centers compared to other. This in turn will lead to greater revenue influx for these centers hence
healthcare stakeholders needs to envision the greater implications associated with such reducing
costs in prescribed tests.
7.0 Staff Implications
Healthcare stakeholders needs to understand proper goals for healthcare systems which is to
enhance overall value that is provided to patients. Patient outcomes and cost measured at patient
level can provide useful insights for patient care (Mello, 2010). Patient care is delivered by a
team of multiple specialists, who perform interventions and supporting staffs that help in
to provide quality healthcare at affordable costs.
The new measure does not require any medical science breakthroughs as it entails ascertaining
cost and comparing them to outcomes related to patients. Value in healthcare systems is
measured by patient outcomes that are generated per dollar spent (Wolfson, 2014). It can be
derived from this, more the number of services delivered more expensive the care and not
necessarily amounting to better care. There are a hosts of healthcare centers that are currently
incorporating such measures as the Cleft Lip and Palate Program at Children’s Hospital in
Boston , the Head and Neck Center at MD Anderson Cancer Center in Houston, and Brigham &
Women’s Hospital in Boston and units performing knee replacements at Schön Klinik in
Germany. Financial implications for these healthcare centers along with those that implement
measures for cost reductions is bound to take place. Overall it can be estimated with gradual
declining of patient’s bill at these centers, there is bound to be more patients at some healthcare
centers compared to other. This in turn will lead to greater revenue influx for these centers hence
healthcare stakeholders needs to envision the greater implications associated with such reducing
costs in prescribed tests.
7.0 Staff Implications
Healthcare stakeholders needs to understand proper goals for healthcare systems which is to
enhance overall value that is provided to patients. Patient outcomes and cost measured at patient
level can provide useful insights for patient care (Mello, 2010). Patient care is delivered by a
team of multiple specialists, who perform interventions and supporting staffs that help in
delivering, such outcomes. Medical conditions in patients and healthcare service delivery is best
attended to when patient circumstances, complications and comorbidities are considered
together. A major challenge in healthcare service delivery is associated with staff coordination.
Staffs within healthcare management systems holds the key top appropriate service delivery such
that patient care can be catered adequately. While implementing new strategy for healthcare
outcomes, staff is the major stakeholder who will play a major role. Hence, staff will need to be
briefed regarding the new procedure which will help them adapt the same. There will need to be
formal training and induction procedure adopted for purpose of staff training and induction by
which staff can be briefed regarding the testing procedures. Staff will play a major role in taking
feedback from patients such that they can provide the same back to the management and
physicians (Horvath, 2013). Feedback mechanism will allow greatly adapt cost control
mechanism, which in turn will allow reduction in cost. Staffs as Pathologists and Laboratory
Practioner will need to get briefed regarding electronic procedure for cost reduction and test
prescriptions. Appropriate guidelines set for laboratory tests will provide scope for reducing
number of tests that are given in general to patients. Staffs will play a major role in reducing
burden of huge expenditure that are done by healthcare centers in testing procedures. Healthcare
facilities will be focused mainly on components of testing when required. Staff role will remain
primary in impacting roles related to healthcare facilities as they are the primary stakeholders
meeting customers.
attended to when patient circumstances, complications and comorbidities are considered
together. A major challenge in healthcare service delivery is associated with staff coordination.
Staffs within healthcare management systems holds the key top appropriate service delivery such
that patient care can be catered adequately. While implementing new strategy for healthcare
outcomes, staff is the major stakeholder who will play a major role. Hence, staff will need to be
briefed regarding the new procedure which will help them adapt the same. There will need to be
formal training and induction procedure adopted for purpose of staff training and induction by
which staff can be briefed regarding the testing procedures. Staff will play a major role in taking
feedback from patients such that they can provide the same back to the management and
physicians (Horvath, 2013). Feedback mechanism will allow greatly adapt cost control
mechanism, which in turn will allow reduction in cost. Staffs as Pathologists and Laboratory
Practioner will need to get briefed regarding electronic procedure for cost reduction and test
prescriptions. Appropriate guidelines set for laboratory tests will provide scope for reducing
number of tests that are given in general to patients. Staffs will play a major role in reducing
burden of huge expenditure that are done by healthcare centers in testing procedures. Healthcare
facilities will be focused mainly on components of testing when required. Staff role will remain
primary in impacting roles related to healthcare facilities as they are the primary stakeholders
meeting customers.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
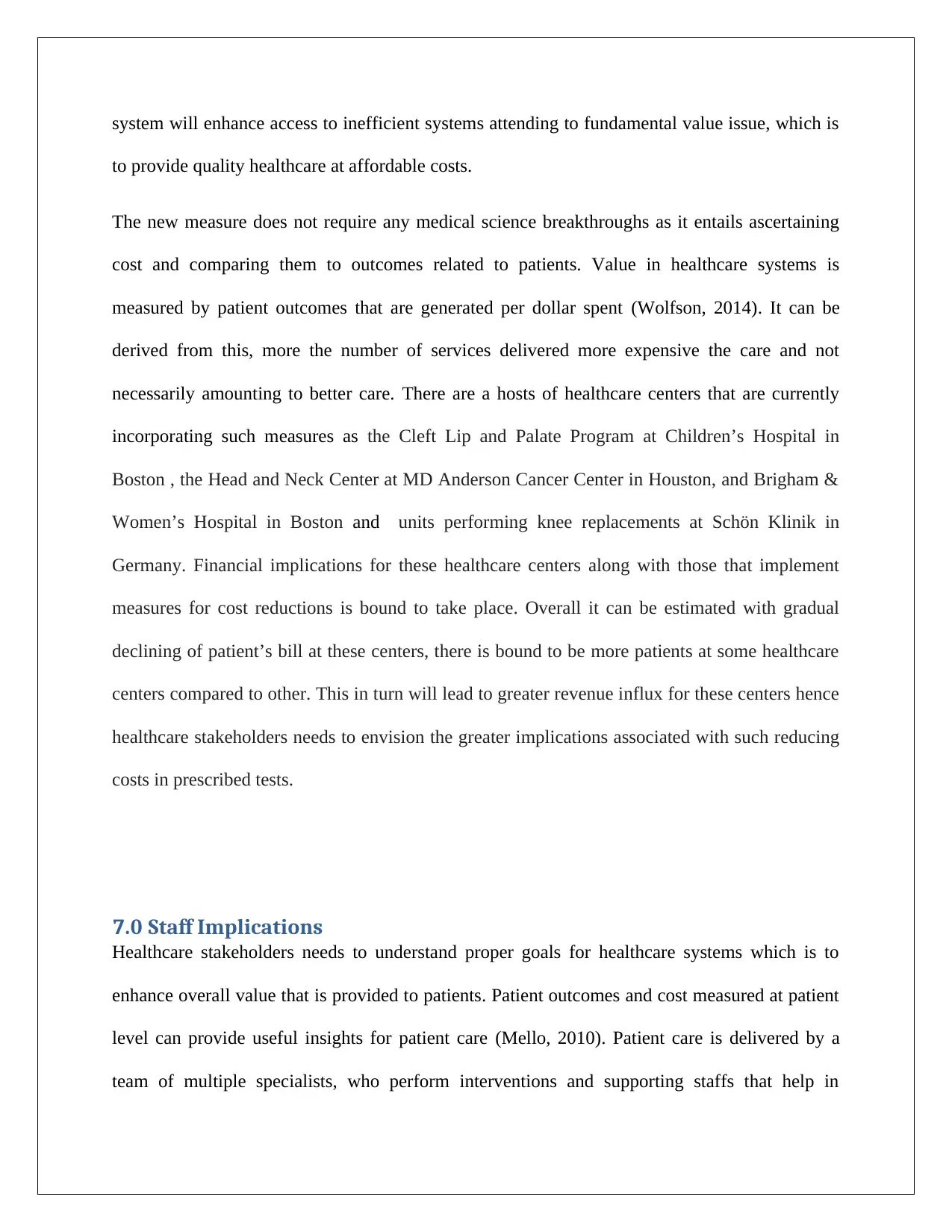
8.0 Cost/Benefit Ratio
Cost-benefit analysis (CBA) also referred sometimes to as benefit cost analysis (BCA) is a
procedure to evaluate strengths and weakness associated with a given process. This approach
helps preserving savings while achieving benefits from certain procedures. It involves a decision
policy related to any particular project (Kreindler, 2010). In this case, CBA concerns adaptation
of electronic cost management systems for test prescriptions. As discussed above, there are
several benefits for accommodating in cost reduction approaches and such benefits will continue
to reap in the future. However, costs associated with the procedure will include significant costs
related to designing systems, training staffs and so on. A break of costs is given below;
COSTS USD
DESIGNING COSTS 120,000
TRAINING COST
3,20,00
0
IMPLEMENTATION COSTS 160,000
MONITORING & EVALUATION 80,000
YEARLY COSTS 180,000
Figure 3: Cost Overheads Break Up
Source: Author
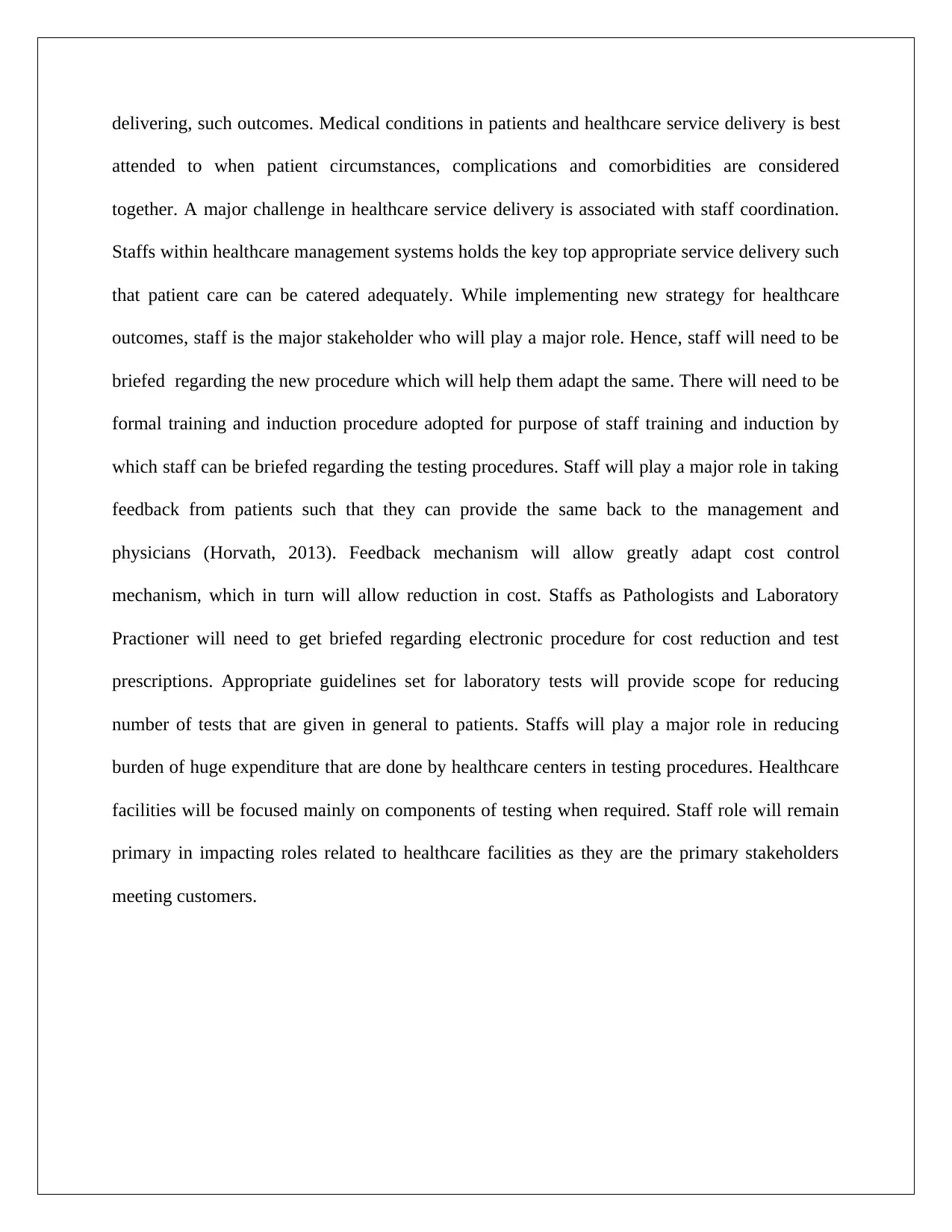
i* 10
YEAR 0 1 2 3 4 5
COST 540,000
380,00
0
380,00
0 380,000
380,00
0 380,000
NPV 578,000
BENEFITS
10,000,00
0
800,00
0
500,00
0
6,000,00
0
700,00
0
88,500,00
0
106,500,00
0
CBA 184.25613
Figure 4: CBA for the Project
Source: Author
Cost-benefit analysis (CBA) also referred sometimes to as benefit cost analysis (BCA) is a
procedure to evaluate strengths and weakness associated with a given process. This approach
helps preserving savings while achieving benefits from certain procedures. It involves a decision
policy related to any particular project (Kreindler, 2010). In this case, CBA concerns adaptation
of electronic cost management systems for test prescriptions. As discussed above, there are
several benefits for accommodating in cost reduction approaches and such benefits will continue
to reap in the future. However, costs associated with the procedure will include significant costs
related to designing systems, training staffs and so on. A break of costs is given below;
COSTS USD
DESIGNING COSTS 120,000
TRAINING COST
3,20,00
0
IMPLEMENTATION COSTS 160,000
MONITORING & EVALUATION 80,000
YEARLY COSTS 180,000
Figure 3: Cost Overheads Break Up
Source: Author
i* 10
YEAR 0 1 2 3 4 5
COST 540,000
380,00
0
380,00
0 380,000
380,00
0 380,000
NPV 578,000
BENEFITS
10,000,00
0
800,00
0
500,00
0
6,000,00
0
700,00
0
88,500,00
0
106,500,00
0
CBA 184.25613
Figure 4: CBA for the Project
Source: Author
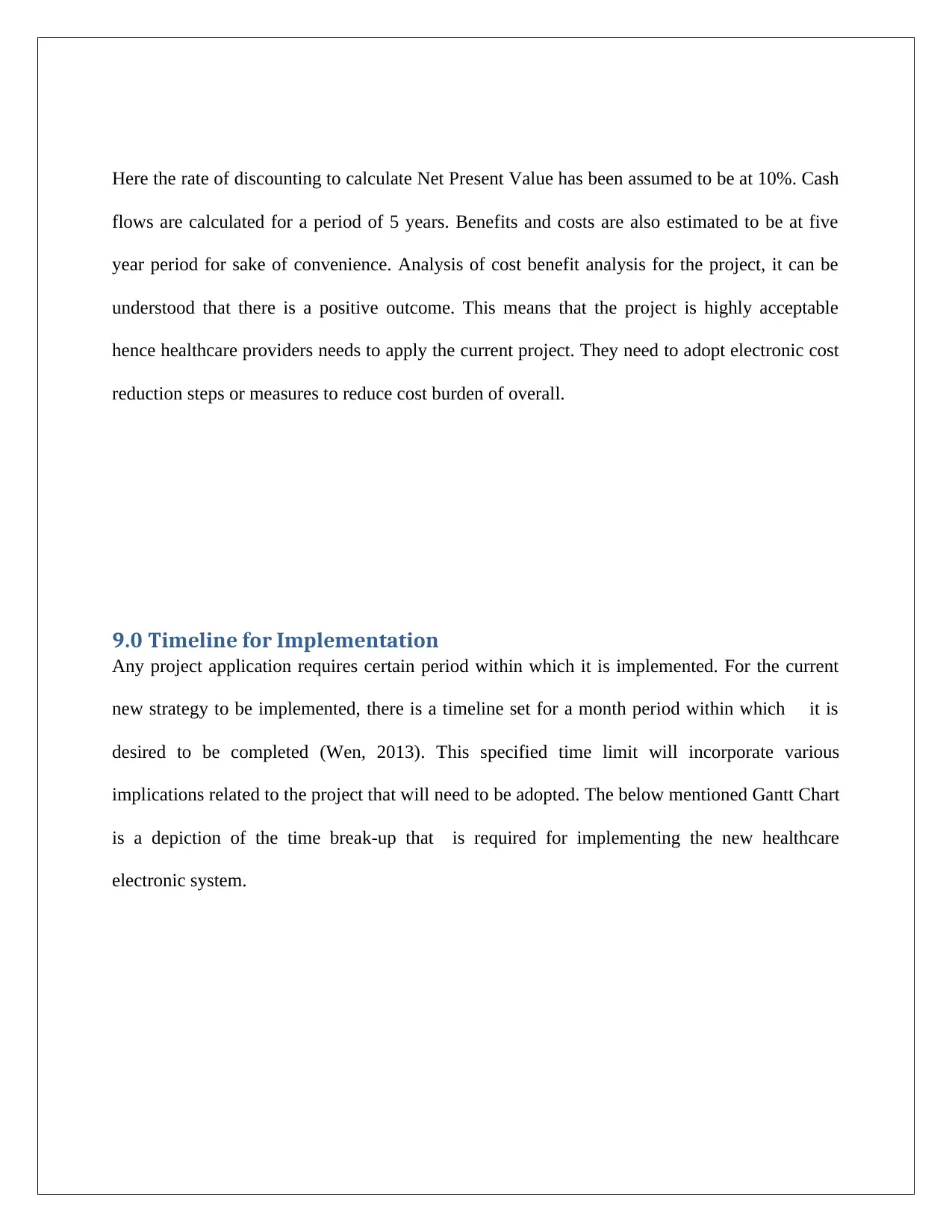
Here the rate of discounting to calculate Net Present Value has been assumed to be at 10%. Cash
flows are calculated for a period of 5 years. Benefits and costs are also estimated to be at five
year period for sake of convenience. Analysis of cost benefit analysis for the project, it can be
understood that there is a positive outcome. This means that the project is highly acceptable
hence healthcare providers needs to apply the current project. They need to adopt electronic cost
reduction steps or measures to reduce cost burden of overall.
9.0 Timeline for Implementation
Any project application requires certain period within which it is implemented. For the current
new strategy to be implemented, there is a timeline set for a month period within which it is
desired to be completed (Wen, 2013). This specified time limit will incorporate various
implications related to the project that will need to be adopted. The below mentioned Gantt Chart
is a depiction of the time break-up that is required for implementing the new healthcare
electronic system.
flows are calculated for a period of 5 years. Benefits and costs are also estimated to be at five
year period for sake of convenience. Analysis of cost benefit analysis for the project, it can be
understood that there is a positive outcome. This means that the project is highly acceptable
hence healthcare providers needs to apply the current project. They need to adopt electronic cost
reduction steps or measures to reduce cost burden of overall.
9.0 Timeline for Implementation
Any project application requires certain period within which it is implemented. For the current
new strategy to be implemented, there is a timeline set for a month period within which it is
desired to be completed (Wen, 2013). This specified time limit will incorporate various
implications related to the project that will need to be adopted. The below mentioned Gantt Chart
is a depiction of the time break-up that is required for implementing the new healthcare
electronic system.
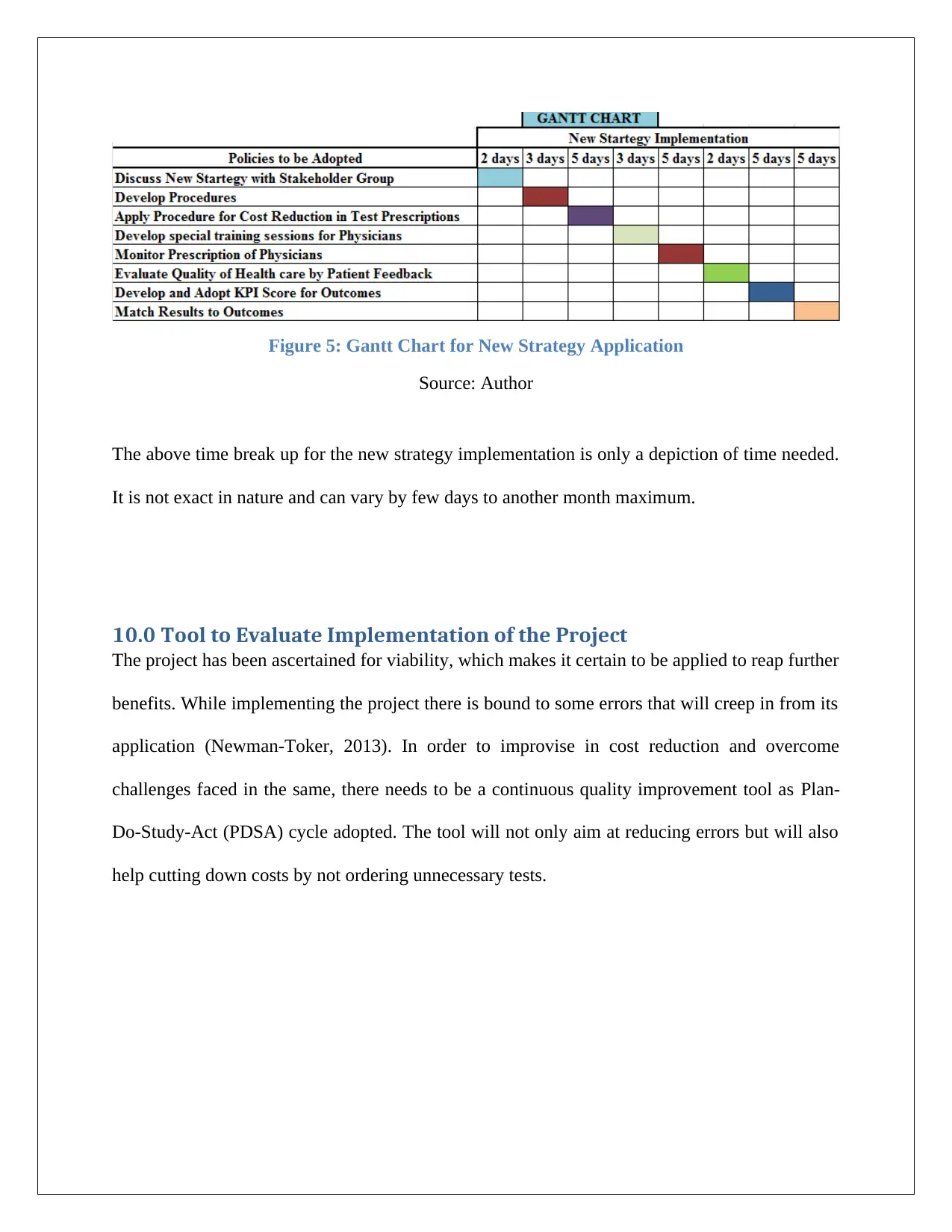
Figure 5: Gantt Chart for New Strategy Application
Source: Author
The above time break up for the new strategy implementation is only a depiction of time needed.
It is not exact in nature and can vary by few days to another month maximum.
10.0 Tool to Evaluate Implementation of the Project
The project has been ascertained for viability, which makes it certain to be applied to reap further
benefits. While implementing the project there is bound to some errors that will creep in from its
application (Newman-Toker, 2013). In order to improvise in cost reduction and overcome
challenges faced in the same, there needs to be a continuous quality improvement tool as Plan-
Do-Study-Act (PDSA) cycle adopted. The tool will not only aim at reducing errors but will also
help cutting down costs by not ordering unnecessary tests.
Source: Author
The above time break up for the new strategy implementation is only a depiction of time needed.
It is not exact in nature and can vary by few days to another month maximum.
10.0 Tool to Evaluate Implementation of the Project
The project has been ascertained for viability, which makes it certain to be applied to reap further
benefits. While implementing the project there is bound to some errors that will creep in from its
application (Newman-Toker, 2013). In order to improvise in cost reduction and overcome
challenges faced in the same, there needs to be a continuous quality improvement tool as Plan-
Do-Study-Act (PDSA) cycle adopted. The tool will not only aim at reducing errors but will also
help cutting down costs by not ordering unnecessary tests.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

Figure 6:PDCA Cycle
Source: Author
The PDCA is a well-established procedure and tool for continuous for continuous improvements.
This tool helps in continuous monitoring and evaluation of procedures adopted and then
overcoming of the same. In this tool first a plan is made that ascertains steps that has to be taken
for reducing overall costs related to prescribed testing procedures. A chart will be integrated into
the electronic testing procedure that will be evaluated each time patients will be provided with a
test. Then next is Do step where action of relevant stakeholders will be evaluated. In this step an
action is taken such that goals or desired objectives can be met adequately. In the check
procedure there will be a monitoring and evaluation that will be included for incorporating
changes to be made for stakeholders. This step of evaluation is critical as it makes sure that all
desired outcomes are attended to by relevant stakeholder group (Paterniti, 2010). The final step is
to act, once desired actions has been ascertained by the monitoring team then such can easily be
Source: Author
The PDCA is a well-established procedure and tool for continuous for continuous improvements.
This tool helps in continuous monitoring and evaluation of procedures adopted and then
overcoming of the same. In this tool first a plan is made that ascertains steps that has to be taken
for reducing overall costs related to prescribed testing procedures. A chart will be integrated into
the electronic testing procedure that will be evaluated each time patients will be provided with a
test. Then next is Do step where action of relevant stakeholders will be evaluated. In this step an
action is taken such that goals or desired objectives can be met adequately. In the check
procedure there will be a monitoring and evaluation that will be included for incorporating
changes to be made for stakeholders. This step of evaluation is critical as it makes sure that all
desired outcomes are attended to by relevant stakeholder group (Paterniti, 2010). The final step is
to act, once desired actions has been ascertained by the monitoring team then such can easily be
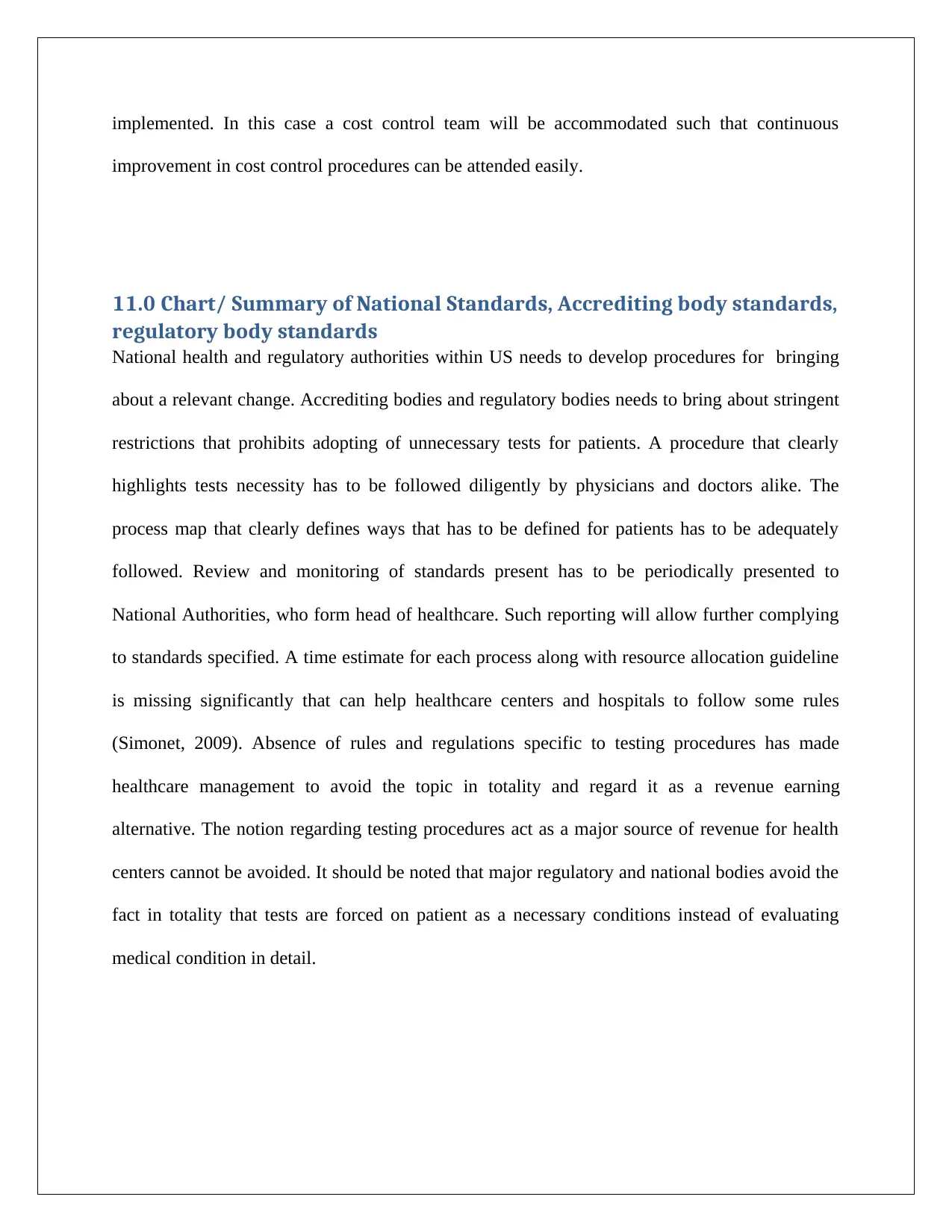
implemented. In this case a cost control team will be accommodated such that continuous
improvement in cost control procedures can be attended easily.
11.0 Chart/ Summary of National Standards, Accrediting body standards,
regulatory body standards
National health and regulatory authorities within US needs to develop procedures for bringing
about a relevant change. Accrediting bodies and regulatory bodies needs to bring about stringent
restrictions that prohibits adopting of unnecessary tests for patients. A procedure that clearly
highlights tests necessity has to be followed diligently by physicians and doctors alike. The
process map that clearly defines ways that has to be defined for patients has to be adequately
followed. Review and monitoring of standards present has to be periodically presented to
National Authorities, who form head of healthcare. Such reporting will allow further complying
to standards specified. A time estimate for each process along with resource allocation guideline
is missing significantly that can help healthcare centers and hospitals to follow some rules
(Simonet, 2009). Absence of rules and regulations specific to testing procedures has made
healthcare management to avoid the topic in totality and regard it as a revenue earning
alternative. The notion regarding testing procedures act as a major source of revenue for health
centers cannot be avoided. It should be noted that major regulatory and national bodies avoid the
fact in totality that tests are forced on patient as a necessary conditions instead of evaluating
medical condition in detail.
improvement in cost control procedures can be attended easily.
11.0 Chart/ Summary of National Standards, Accrediting body standards,
regulatory body standards
National health and regulatory authorities within US needs to develop procedures for bringing
about a relevant change. Accrediting bodies and regulatory bodies needs to bring about stringent
restrictions that prohibits adopting of unnecessary tests for patients. A procedure that clearly
highlights tests necessity has to be followed diligently by physicians and doctors alike. The
process map that clearly defines ways that has to be defined for patients has to be adequately
followed. Review and monitoring of standards present has to be periodically presented to
National Authorities, who form head of healthcare. Such reporting will allow further complying
to standards specified. A time estimate for each process along with resource allocation guideline
is missing significantly that can help healthcare centers and hospitals to follow some rules
(Simonet, 2009). Absence of rules and regulations specific to testing procedures has made
healthcare management to avoid the topic in totality and regard it as a revenue earning
alternative. The notion regarding testing procedures act as a major source of revenue for health
centers cannot be avoided. It should be noted that major regulatory and national bodies avoid the
fact in totality that tests are forced on patient as a necessary conditions instead of evaluating
medical condition in detail.

12.0 Comparison of best practices and standards compared to current
facility practices
Prevalence of high costs within the health industry has become acceptable. there is a host of
complex costing systems prevalent in current healthcare industry that has led to significant
challenges. Over the past few years politicians, health care industry leaders and insurance
companies are exploring ways and means to reduce such costs by keeping standards in quality of
healthcare constant (Pear, 2009). Best practices are yet to adapted by healthcare service
providers, who have not been able to explore dearth of information to arrive at findings related to
the study. Though healthcare standards and best practices are focused on delivering patient with
best possible quality in healthcare, it often comes at high cost. Cost control measures aimed at
reducing tests prescribed are yet to be accommodated, which again reflects greater challenge.
With possibility of adoption of electronic medium to predict tests in patient of adults or children,
better quality healthcare with affordable costs might become a feasible solution in near future.
Cost management procedures needs to begin by detecting of medical condition of the patient that
includes identifying comorbidities or complications. Processes that affect patient care as
resources used and patient care cycle needs to be taken into consideration. Then a specific
definition of delivery of care value chain is determined to access principal activities that are
involves in delivering patient care (Share, 2011). Setting time for specific processes will help
allocate resources and also reduce stress of costs that are put on patients. Medical practioner,
doctors and physicians needs to provide greater time allocation to evaluating patient’s health and
medical condition also take into consideration previous reports prior to accommodating any new
facility practices
Prevalence of high costs within the health industry has become acceptable. there is a host of
complex costing systems prevalent in current healthcare industry that has led to significant
challenges. Over the past few years politicians, health care industry leaders and insurance
companies are exploring ways and means to reduce such costs by keeping standards in quality of
healthcare constant (Pear, 2009). Best practices are yet to adapted by healthcare service
providers, who have not been able to explore dearth of information to arrive at findings related to
the study. Though healthcare standards and best practices are focused on delivering patient with
best possible quality in healthcare, it often comes at high cost. Cost control measures aimed at
reducing tests prescribed are yet to be accommodated, which again reflects greater challenge.
With possibility of adoption of electronic medium to predict tests in patient of adults or children,
better quality healthcare with affordable costs might become a feasible solution in near future.
Cost management procedures needs to begin by detecting of medical condition of the patient that
includes identifying comorbidities or complications. Processes that affect patient care as
resources used and patient care cycle needs to be taken into consideration. Then a specific
definition of delivery of care value chain is determined to access principal activities that are
involves in delivering patient care (Share, 2011). Setting time for specific processes will help
allocate resources and also reduce stress of costs that are put on patients. Medical practioner,
doctors and physicians needs to provide greater time allocation to evaluating patient’s health and
medical condition also take into consideration previous reports prior to accommodating any new
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
procedures or processes. A key performance indicator (KPI) score needs to be adopted by
healthcare facilities to ensure that better quality healthcare for patients can be provided.
13.0 Conclusion and Recommendation
Applying cost management and control measures can be highly complicated resulting in a
number of challenges for healthcare stakeholders. Management and physicians within healthcare
systems might not be convinced to implement complex challenges that might pose from cost
management. This might include disrupting entire processes followed so far such as to
incorporate new norms. It would also implement additional changes to be made to existing
systems that are already functional in nature. To do away with entire system of such nature might
include further cost burden into the entire healthcare industry, for which they might not be ready
at all. The new strategy of implementing electronic system might impose several difficulties,
which can be overcome by means of the following;
Legislative Policy Changes: The new electronic system within healthcare
infrastructure has to be implemented with some legislative policy changes. Politicians
needs to adopt genuine measures that can help lower costs associated with healthcare
prescribed tests. Legislative measures will make sure that all healthcare systems within
the US implements the newly developed system.
Cost Saving Adaptation: Electronic system for healthcare is bound to bring benefits
to thousands of patients of healthcare within the US, it might also be effective in
reducing overall burden on insurance companies. Therefore, a costs management
healthcare facilities to ensure that better quality healthcare for patients can be provided.
13.0 Conclusion and Recommendation
Applying cost management and control measures can be highly complicated resulting in a
number of challenges for healthcare stakeholders. Management and physicians within healthcare
systems might not be convinced to implement complex challenges that might pose from cost
management. This might include disrupting entire processes followed so far such as to
incorporate new norms. It would also implement additional changes to be made to existing
systems that are already functional in nature. To do away with entire system of such nature might
include further cost burden into the entire healthcare industry, for which they might not be ready
at all. The new strategy of implementing electronic system might impose several difficulties,
which can be overcome by means of the following;
Legislative Policy Changes: The new electronic system within healthcare
infrastructure has to be implemented with some legislative policy changes. Politicians
needs to adopt genuine measures that can help lower costs associated with healthcare
prescribed tests. Legislative measures will make sure that all healthcare systems within
the US implements the newly developed system.
Cost Saving Adaptation: Electronic system for healthcare is bound to bring benefits
to thousands of patients of healthcare within the US, it might also be effective in
reducing overall burden on insurance companies. Therefore, a costs management
system that makes adaptation of this system easy has to be provided to healthcare
providers such that they can implement the system easily.
Benchmarking KPI Score: Healthcare providers might initially face immense
challenges from monitoring of the electronic system. Therefore an industry based KPI
score has to be developed that makes participants in the healthcare sector easily adopt
new strategies and procedures.
Resource Allocation & Budget: Resource allocation is a critical factor that makes it
difficult to incorporate cost reduction in overall healthcare facility. All healthcare
facilities needs to be allocated certain amounts of resource allocation such that they are
able to create their own budget and adhere to the same.
providers such that they can implement the system easily.
Benchmarking KPI Score: Healthcare providers might initially face immense
challenges from monitoring of the electronic system. Therefore an industry based KPI
score has to be developed that makes participants in the healthcare sector easily adopt
new strategies and procedures.
Resource Allocation & Budget: Resource allocation is a critical factor that makes it
difficult to incorporate cost reduction in overall healthcare facility. All healthcare
facilities needs to be allocated certain amounts of resource allocation such that they are
able to create their own budget and adhere to the same.
Reference Lists
Ayres, A. C. (2014). A cost‐effectiveness analysis comparing different strategies to implement
noninvasive prenatal testing into a Down syndrome screening program. Australian and
New Zealand Journal of Obstetrics and Gynaecology, 54(5), 412-417.
Carreyrou, J. (2008). Nonprofit hospitals flex pricing power. Wall Street Journal, 1A.
Garfield, S. S. (2012). Clinical and Cost Consequences of Incorporating a Novel Non-Invasive
Prenatal Test into the Diagnostic Pathway for Fetal Trisomies. Journal of Managed Care
Medicine, 15(2).
Horvath, A. R. (2013). From evidence to best practice in laboratory medicine. The Clinical
Biochemist Reviews, 34(2), 47.
Janssens, P. M. (2010). Managing the demand for laboratory testing: options and opportunities.
Clinica chimica acta, 411(21-22), 1596-1602.
Kotler, P. S. (2011). Strategic marketing for health care organizations: building a customer-
driven health system. John Wiley & Sons.
Kreindler, S. A. (2010). Policy strategies to reduce waits for elective care: a synthesis of
international evidence. British Medical Bulletin, 95(1), 7-32.
McCormick, D. B. (2012). Giving office-based physicians electronic access to patients’ prior
imaging and lab results did not deter ordering of tests. Health Affairs, 31(3), 488-496.
Mello, M. M. (2010). National costs of the medical liability system. Health affairs, 29(9), 1569-
1577.
Newman-Toker, D. E. (2013). How much diagnostic safety can we afford, and how should we
decide? A health economics perspective. BMJ Qual Saf, 22(Suppl 2), ii11-ii20.
Paterniti, D. A. (2010). Getting to “no”: strategies primary care physicians use to deny patient
requests. Archives of internal medicine, 170(4), 381-388.
Pear, R. (2009). Health care spending disparities stir a fight. New York Times.
Share, D. A. (2011). How a regional collaborative of hospitals and physicians in Michigan cut
costs and improved the quality of care. Health Affairs, 30(4), 636-645.
Ayres, A. C. (2014). A cost‐effectiveness analysis comparing different strategies to implement
noninvasive prenatal testing into a Down syndrome screening program. Australian and
New Zealand Journal of Obstetrics and Gynaecology, 54(5), 412-417.
Carreyrou, J. (2008). Nonprofit hospitals flex pricing power. Wall Street Journal, 1A.
Garfield, S. S. (2012). Clinical and Cost Consequences of Incorporating a Novel Non-Invasive
Prenatal Test into the Diagnostic Pathway for Fetal Trisomies. Journal of Managed Care
Medicine, 15(2).
Horvath, A. R. (2013). From evidence to best practice in laboratory medicine. The Clinical
Biochemist Reviews, 34(2), 47.
Janssens, P. M. (2010). Managing the demand for laboratory testing: options and opportunities.
Clinica chimica acta, 411(21-22), 1596-1602.
Kotler, P. S. (2011). Strategic marketing for health care organizations: building a customer-
driven health system. John Wiley & Sons.
Kreindler, S. A. (2010). Policy strategies to reduce waits for elective care: a synthesis of
international evidence. British Medical Bulletin, 95(1), 7-32.
McCormick, D. B. (2012). Giving office-based physicians electronic access to patients’ prior
imaging and lab results did not deter ordering of tests. Health Affairs, 31(3), 488-496.
Mello, M. M. (2010). National costs of the medical liability system. Health affairs, 29(9), 1569-
1577.
Newman-Toker, D. E. (2013). How much diagnostic safety can we afford, and how should we
decide? A health economics perspective. BMJ Qual Saf, 22(Suppl 2), ii11-ii20.
Paterniti, D. A. (2010). Getting to “no”: strategies primary care physicians use to deny patient
requests. Archives of internal medicine, 170(4), 381-388.
Pear, R. (2009). Health care spending disparities stir a fight. New York Times.
Share, D. A. (2011). How a regional collaborative of hospitals and physicians in Michigan cut
costs and improved the quality of care. Health Affairs, 30(4), 636-645.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Simonet, D. (2009). Cost reduction strategies for emergency services: insurance role, practice
changes and patients accountability. Health Care Analysis, 17(1), 1-19.
Tapon, D. (2010). Prenatal testing for Down syndrome: comparison of screening practices in the
UK and USA. Journal of genetic counseling, 19(2), 112-130.
Wen, L. S. (2013). When doctors Don't listen: How to avoid misdiagnoses and unnecessary tests.
Macmillan.
Wolfson, D. S. (2014). Engaging physicians and consumers in conversations about treatment
overuse and waste: a short history of the choosing wisely campaign. Academic Medicine,
89(7), 990-995.
changes and patients accountability. Health Care Analysis, 17(1), 1-19.
Tapon, D. (2010). Prenatal testing for Down syndrome: comparison of screening practices in the
UK and USA. Journal of genetic counseling, 19(2), 112-130.
Wen, L. S. (2013). When doctors Don't listen: How to avoid misdiagnoses and unnecessary tests.
Macmillan.
Wolfson, D. S. (2014). Engaging physicians and consumers in conversations about treatment
overuse and waste: a short history of the choosing wisely campaign. Academic Medicine,
89(7), 990-995.
1 out of 24
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





