Therapeutic Relationships in Nursing
VerifiedAdded on 2020/05/04
|19
|4160
|30
AI Summary
This assignment focuses on the RNAO Best Practice Guideline 'Establishing Therapeutic Relationships' for nurses. The guideline emphasizes the significance of building strong therapeutic relationships with patients to enhance quality of care. It delves into strategies for effective communication, understanding patient needs, and fostering trust. Students are expected to critically analyze the guideline's content and its implications for nursing practice.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
How can we configure the therapeutic relationship with the demented people for
implementing person-centred care and reducing their frequency of falls?
Introduction
The assessment focuses on the evaluation of the person-centred interventions
requiring administration with the objective of decreasing the frequency of falls in the
demented people. Evidence-based research literature advocates the elevated risk of falls in
demented patients. The disorders related to Parkinson’s dementia and Lewy Body Dementia
predominantly increase the likelihood of the affected patients in terms of experiencing falls
while undertaking day-to-day activities (Aizen 2015). Limited evidence is available regarding
the development of definitive strategies for reducing the frequency of falls and associated
traumatic conditions in the demented people. Primary exercise approaches prove to be
effective modalities that increase stamina and confidence of demented patients and reduce
their risk of falls across the community environment. However, the method of their
implementation for the target population remains debatable in the medical community.
Evidence-based research literature advocates the pattern of dose-response relationship
between the frequency of falls in demented people and the administration of psychotropic
drugs (Jong, Elst & Hartholt 2013). The increased administration of psychotropic medication
results in the reciprocal elevation of the falling frequency in the demented people. Therefore,
medical professionals require administering person-centred approaches to streamline the
pattern of medication management for the associated reduction in falling frequency in the
demented population. Gait deterioration and cognitive decline include some of the significant
factors that evidently contribute to the falls in elderly demented people (Segev-Jacubovski et
al. 2011). The administration of multimodal cognitive interventions with the systematic
utilization of therapeutic communication is therefore highly warranted for controlling the
frequency of falling episodes in the patients affected with dementia and associated mental
implementing person-centred care and reducing their frequency of falls?
Introduction
The assessment focuses on the evaluation of the person-centred interventions
requiring administration with the objective of decreasing the frequency of falls in the
demented people. Evidence-based research literature advocates the elevated risk of falls in
demented patients. The disorders related to Parkinson’s dementia and Lewy Body Dementia
predominantly increase the likelihood of the affected patients in terms of experiencing falls
while undertaking day-to-day activities (Aizen 2015). Limited evidence is available regarding
the development of definitive strategies for reducing the frequency of falls and associated
traumatic conditions in the demented people. Primary exercise approaches prove to be
effective modalities that increase stamina and confidence of demented patients and reduce
their risk of falls across the community environment. However, the method of their
implementation for the target population remains debatable in the medical community.
Evidence-based research literature advocates the pattern of dose-response relationship
between the frequency of falls in demented people and the administration of psychotropic
drugs (Jong, Elst & Hartholt 2013). The increased administration of psychotropic medication
results in the reciprocal elevation of the falling frequency in the demented people. Therefore,
medical professionals require administering person-centred approaches to streamline the
pattern of medication management for the associated reduction in falling frequency in the
demented population. Gait deterioration and cognitive decline include some of the significant
factors that evidently contribute to the falls in elderly demented people (Segev-Jacubovski et
al. 2011). The administration of multimodal cognitive interventions with the systematic
utilization of therapeutic communication is therefore highly warranted for controlling the
frequency of falling episodes in the patients affected with dementia and associated mental
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
manifestations (Jootun & McGhee 2011). The presented research paper effectively explores
the implication of the therapeutic relationship on the pattern of person-centred care of
demented patients with the objective of substantially reducing their falling risk in the clinical
as well as residential settings. The improvement in patient outcomes through the utilization of
therapeutic communication will provide a new paradigm to dementia care in the medical
facilities.
Literature Review
The literature review was undertaken with the objective of exploring the influence of
therapeutic communication on improving the patient care outcomes in the dementia setting.
Evidence-based analysis attempted to affirm the potential of an effective therapeutic
relationship in terms of facilitating person-centred healthcare interventions requiring
administration by medical professionals for reducing the falling frequency in the demented
patients. The scientific databases including PubMed, CINAHL, Research Gate, Cochrane and
ProQuest Central were researched with the objective of exploring the articles of interest while
sequentially utilizing the search terms including therapeutic communication/Dementia/falls,
therapeutic communication/cognitive/dementia/falls, dementia/trauma/therapeutic
relationship, person-centred/dementia/therapeutic relationship and communication, nursing,
dementia care and patient-centred dementia care.
The factors including medications, footwear, assistive devices, home features, caregiver
support, age related deterioration, cognitive defect, gait abnormality, sensory deficit and
behavioural manifestations elevate the likelihood of falls and associated complications in the
demented patients. Each demented patient experience at least one fall per year under the
influence of mental manifestation and potential risk factors. The caregiver requires
effectively modifying the immediate environment of the demented individual in a manner to
facilitate the performance of daily activities including housekeeping, toileting and dressing
the implication of the therapeutic relationship on the pattern of person-centred care of
demented patients with the objective of substantially reducing their falling risk in the clinical
as well as residential settings. The improvement in patient outcomes through the utilization of
therapeutic communication will provide a new paradigm to dementia care in the medical
facilities.
Literature Review
The literature review was undertaken with the objective of exploring the influence of
therapeutic communication on improving the patient care outcomes in the dementia setting.
Evidence-based analysis attempted to affirm the potential of an effective therapeutic
relationship in terms of facilitating person-centred healthcare interventions requiring
administration by medical professionals for reducing the falling frequency in the demented
patients. The scientific databases including PubMed, CINAHL, Research Gate, Cochrane and
ProQuest Central were researched with the objective of exploring the articles of interest while
sequentially utilizing the search terms including therapeutic communication/Dementia/falls,
therapeutic communication/cognitive/dementia/falls, dementia/trauma/therapeutic
relationship, person-centred/dementia/therapeutic relationship and communication, nursing,
dementia care and patient-centred dementia care.
The factors including medications, footwear, assistive devices, home features, caregiver
support, age related deterioration, cognitive defect, gait abnormality, sensory deficit and
behavioural manifestations elevate the likelihood of falls and associated complications in the
demented patients. Each demented patient experience at least one fall per year under the
influence of mental manifestation and potential risk factors. The caregiver requires
effectively modifying the immediate environment of the demented individual in a manner to
facilitate the performance of daily activities including housekeeping, toileting and dressing
(Phelan et al. 2015). Furthermore, administration of personal assistance for the safe
undertaking of the personal care of demented people is necessarily required for reducing the
risk of falling episodes. Medical professionals and rehabilitation experts require interacting
with the demented patients for regularly monitoring their daily activities in the context of
improving the pattern of their safety and associated outcomes. This interaction warrants the
administration of therapeutic communication with the objective of evaluating the treatment
challenges and individualized healthcare requirements of the demented people (Velea &
Purcărea 2014). Demented patients affected with various co-morbid conditions require
undertaking numerous treatment interventions under the recommendation of multiple
healthcare professionals. Eventually, they might experience polypharmacy and other risk
factors that could elevate the frequency of falling episodes and associated adverse
manifestations (Hammond & Wilson 2013).
Utilization of dialogue and closeness interventions is required for evaluating the
causative factors of the falling episodes among demented individuals (Struksnes et al. 2011).
Medical professionals need to administer a questionnaire to the demented people with the
objective of determining their environmental constraints as well as psycho-socio-somatic
deficits contributing to the pattern of falling episodes. The questionnaire administration and
collection of data require the systematic establishment of a therapeutic relationship with the
demented patients in the context of motivating them for sharing their concerns and
apprehensions regarding the falling episodes. The pattern of therapeutic relation also assists
in mitigating the problematic behaviour of the treated patients in the clinical setting
(Westermann et al. 2015). Furthermore, systematic documentation of patient concerns
provides an insight to the medical professionals in terms of configuring patient-centred
interventions for acquiring desirable healthcare outcomes (Struksnes et al. 2011).
undertaking of the personal care of demented people is necessarily required for reducing the
risk of falling episodes. Medical professionals and rehabilitation experts require interacting
with the demented patients for regularly monitoring their daily activities in the context of
improving the pattern of their safety and associated outcomes. This interaction warrants the
administration of therapeutic communication with the objective of evaluating the treatment
challenges and individualized healthcare requirements of the demented people (Velea &
Purcărea 2014). Demented patients affected with various co-morbid conditions require
undertaking numerous treatment interventions under the recommendation of multiple
healthcare professionals. Eventually, they might experience polypharmacy and other risk
factors that could elevate the frequency of falling episodes and associated adverse
manifestations (Hammond & Wilson 2013).
Utilization of dialogue and closeness interventions is required for evaluating the
causative factors of the falling episodes among demented individuals (Struksnes et al. 2011).
Medical professionals need to administer a questionnaire to the demented people with the
objective of determining their environmental constraints as well as psycho-socio-somatic
deficits contributing to the pattern of falling episodes. The questionnaire administration and
collection of data require the systematic establishment of a therapeutic relationship with the
demented patients in the context of motivating them for sharing their concerns and
apprehensions regarding the falling episodes. The pattern of therapeutic relation also assists
in mitigating the problematic behaviour of the treated patients in the clinical setting
(Westermann et al. 2015). Furthermore, systematic documentation of patient concerns
provides an insight to the medical professionals in terms of configuring patient-centred
interventions for acquiring desirable healthcare outcomes (Struksnes et al. 2011).
Rehabilitation professionals require undertaking horticulture interventions to facilitate the
pattern of a therapeutic relationship with the objective of enhancing person-centred outcomes
(Detweiler et al. 2012). Horticulture therapy advocates the utilization of gardening
interventions and plants for enhancing the focus and attention span of the demented patients
while concomitantly reducing the level of their agitation, stress and antipsychotic medication
requirement. This eventually reduces the risk of falls and associated traumatic conditions in
the demented patients. The effective configuration of socializing environments through
protective parks increases the plant contact of the demented people that relax their minds and
provide them psychosocial stability (Detweiler et al. 2012). These modifications substantially
decrease the falling episodes of the demented individuals. The therapeutic alliance of the
medical professionals with the demented patients across the natural surroundings elevates
their tactile and visual experience and motivates them for eating enhancement (Detweiler et
al. 2012). The significant effects considerably improve the overall senses of the demented
people that substantially decrease their risk of experiencing falls and associated adverse
somatic complications (Detweiler et al. 2012). The pattern of therapeutic relationship
improves the level of cortisol of the demented patients that resultantly improves their
confidence and memory and reduce their predisposition towards the development of affective
conditions and associated falling episodes.
BEET Tool
Practice change implementation for the demented people requires the systematic
configuration of a proactive plan for the acquisition of the desirable patient-centred outcomes
for the demented patients. The administration of the person-centred fall reduction
interventions requires active collaboration between the clinicians, nurses, rehabilitation
experts, physicians and other members of the healthcare team. Accordingly, the therapeutic
alliance with the demented patients would require configuration for effectively decreasing the
pattern of a therapeutic relationship with the objective of enhancing person-centred outcomes
(Detweiler et al. 2012). Horticulture therapy advocates the utilization of gardening
interventions and plants for enhancing the focus and attention span of the demented patients
while concomitantly reducing the level of their agitation, stress and antipsychotic medication
requirement. This eventually reduces the risk of falls and associated traumatic conditions in
the demented patients. The effective configuration of socializing environments through
protective parks increases the plant contact of the demented people that relax their minds and
provide them psychosocial stability (Detweiler et al. 2012). These modifications substantially
decrease the falling episodes of the demented individuals. The therapeutic alliance of the
medical professionals with the demented patients across the natural surroundings elevates
their tactile and visual experience and motivates them for eating enhancement (Detweiler et
al. 2012). The significant effects considerably improve the overall senses of the demented
people that substantially decrease their risk of experiencing falls and associated adverse
somatic complications (Detweiler et al. 2012). The pattern of therapeutic relationship
improves the level of cortisol of the demented patients that resultantly improves their
confidence and memory and reduce their predisposition towards the development of affective
conditions and associated falling episodes.
BEET Tool
Practice change implementation for the demented people requires the systematic
configuration of a proactive plan for the acquisition of the desirable patient-centred outcomes
for the demented patients. The administration of the person-centred fall reduction
interventions requires active collaboration between the clinicians, nurses, rehabilitation
experts, physicians and other members of the healthcare team. Accordingly, the therapeutic
alliance with the demented patients would require configuration for effectively decreasing the
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
frequency of the falling episodes (Bunn et al. 2014). The establishment of the change process
would require the systematic deployment of BEET (Building Effective Engagement
Techniques) tool for controlling the elevated frequency of falling episodes among the
demented patients. Undoubtedly, the deployment of effective patient-physician engagement
interventions increases the quality and efficiency of patient-centred medical services in a
matrix environment (IOM 2013). BEET tool is categorized into the following subsections.
1. Puzzle and purpose include the research question (indicating the practice change
requirement) and associated rationale.
2. Evidence includes evidence-based findings that advocate benefits of the
recommended practice change requirement.
3. Context indicates the target population requiring the change intervention for the
systematic acquisition of the patient-centred outcomes. It also includes the medical
professionals who need to be part of the change process.
4. Facilitation includes the recommended strategies warranting implementation for
bringing the desirable change in the healthcare management of the demented patients.
Puzzle and Purpose
Healthcare professionals require using positive language with the demented patients
and must not criticise them for their psychosocial deficits while extending therapeutic
communication. The clinicians and nurses should not set any pre-condition while configuring
the pattern of a therapeutic relationship with the treated patients. The following question is
configured with the objective of acquiring the person-centred outcomes.
“How can we configure the therapeutic relationship with the demented people for
implementing person-centred care and reducing their frequency of falls?”
The puzzle remains entirely positive in the context of improving the wellness pattern of the
demented population. The puzzle does not hinder the administration of patient-centred care to
would require the systematic deployment of BEET (Building Effective Engagement
Techniques) tool for controlling the elevated frequency of falling episodes among the
demented patients. Undoubtedly, the deployment of effective patient-physician engagement
interventions increases the quality and efficiency of patient-centred medical services in a
matrix environment (IOM 2013). BEET tool is categorized into the following subsections.
1. Puzzle and purpose include the research question (indicating the practice change
requirement) and associated rationale.
2. Evidence includes evidence-based findings that advocate benefits of the
recommended practice change requirement.
3. Context indicates the target population requiring the change intervention for the
systematic acquisition of the patient-centred outcomes. It also includes the medical
professionals who need to be part of the change process.
4. Facilitation includes the recommended strategies warranting implementation for
bringing the desirable change in the healthcare management of the demented patients.
Puzzle and Purpose
Healthcare professionals require using positive language with the demented patients
and must not criticise them for their psychosocial deficits while extending therapeutic
communication. The clinicians and nurses should not set any pre-condition while configuring
the pattern of a therapeutic relationship with the treated patients. The following question is
configured with the objective of acquiring the person-centred outcomes.
“How can we configure the therapeutic relationship with the demented people for
implementing person-centred care and reducing their frequency of falls?”
The puzzle remains entirely positive in the context of improving the wellness pattern of the
demented population. The puzzle does not hinder the administration of patient-centred care to
the target population while imposing any constraint and does not define any pre-condition or
assumes any predefined solution to the problem. The problem states the requirement of
effectively engaging the nurse practitioners, physicians and rehabilitations experts and
facilitating the process of mutual collaboration for improving patient communication and the
resultant patient-care outcomes (i.e. risk reduction in relation to the falling episodes). The
configured puzzle is framed in a positive format and does not invite criticism of any type
because of the absence of pre-condition. The puzzle remains open in terms of acquiring a
range of interventions warranted to improve the therapeutic relationship pattern for reducing
the risk of falls in the demented patients. The straightforward answering (i.e. yes or no)
cannot (objectively or subjectively) accomplish the requirements of the posted
question/puzzle. These facts rationally indicate that the puzzle is configured in a manner to
acquire innovative and comprehensive solutions with the objective of improving the person-
centred care of the demented patients through improved communication pattern for reducing
the length and severity of their adverse complications. Outcomes of the puzzle resolution
would indicate the considerable reduction in the falling episodes and associated traumatic
conditions of the demented people through the establishment of their improved cognition.
The healthcare teams would find a range of evidence-based methods in the healthcare setting
for improving the person-centred outcomes. The puzzle finally proposes the engagement of
the healthcare professionals, demented patients and their family members in the process of
their medical-decision making in the context of reducing their predisposition towards
experiencing falling episodes.
assumes any predefined solution to the problem. The problem states the requirement of
effectively engaging the nurse practitioners, physicians and rehabilitations experts and
facilitating the process of mutual collaboration for improving patient communication and the
resultant patient-care outcomes (i.e. risk reduction in relation to the falling episodes). The
configured puzzle is framed in a positive format and does not invite criticism of any type
because of the absence of pre-condition. The puzzle remains open in terms of acquiring a
range of interventions warranted to improve the therapeutic relationship pattern for reducing
the risk of falls in the demented patients. The straightforward answering (i.e. yes or no)
cannot (objectively or subjectively) accomplish the requirements of the posted
question/puzzle. These facts rationally indicate that the puzzle is configured in a manner to
acquire innovative and comprehensive solutions with the objective of improving the person-
centred care of the demented patients through improved communication pattern for reducing
the length and severity of their adverse complications. Outcomes of the puzzle resolution
would indicate the considerable reduction in the falling episodes and associated traumatic
conditions of the demented people through the establishment of their improved cognition.
The healthcare teams would find a range of evidence-based methods in the healthcare setting
for improving the person-centred outcomes. The puzzle finally proposes the engagement of
the healthcare professionals, demented patients and their family members in the process of
their medical-decision making in the context of reducing their predisposition towards
experiencing falling episodes.
Checkpoint – 1
We are proposing to engage with our key partners around the question of configuring
therapeutic relationship with the purpose of enhancing person-centred care for reducing the
risk of falls and trauma in the demented people.
This puzzle relates to the heart of our practice/work in the following way:
The configuration of interpersonal therapeutic relationship between nurses, physicians and
patients will reduce the length of patient stay in the clinical setting and reduce the
caregiving burden of the medical professionals.
Evidence
Indeed, substantial evidence is available in the clinical literature that advocates the
requirement of undertaking the recommended practice change with the objective of
improving the patient-centred outcomes in the demented people.
Checkpoint – 2 : Supporting evidence/information
The evidence on which we are basing our proposal is mentioned below:
The clinical investigation by (Swaminathan & Jicha 2014) reveals the requirement of
administering nutritional supplementation to the patients affected with Alzheimer’s
dementia with the objective of decreasing their adverse psychosomatic manifestations and
resultant falling episodes. The effective dietary modifications and nutritional management
is facilitated by the configuration of a potential therapeutic interpersonal relationship with
the demented patients (Abdolrahimi et al. 2017). The conventional dementia care
modalities do not objectively consider the requirement of utilizing therapeutic
communication for the enhancement of the treatment outcomes. Therefore, the
implementation of the recommended patient care methodology (i.e. practice change) is
We are proposing to engage with our key partners around the question of configuring
therapeutic relationship with the purpose of enhancing person-centred care for reducing the
risk of falls and trauma in the demented people.
This puzzle relates to the heart of our practice/work in the following way:
The configuration of interpersonal therapeutic relationship between nurses, physicians and
patients will reduce the length of patient stay in the clinical setting and reduce the
caregiving burden of the medical professionals.
Evidence
Indeed, substantial evidence is available in the clinical literature that advocates the
requirement of undertaking the recommended practice change with the objective of
improving the patient-centred outcomes in the demented people.
Checkpoint – 2 : Supporting evidence/information
The evidence on which we are basing our proposal is mentioned below:
The clinical investigation by (Swaminathan & Jicha 2014) reveals the requirement of
administering nutritional supplementation to the patients affected with Alzheimer’s
dementia with the objective of decreasing their adverse psychosomatic manifestations and
resultant falling episodes. The effective dietary modifications and nutritional management
is facilitated by the configuration of a potential therapeutic interpersonal relationship with
the demented patients (Abdolrahimi et al. 2017). The conventional dementia care
modalities do not objectively consider the requirement of utilizing therapeutic
communication for the enhancement of the treatment outcomes. Therefore, the
implementation of the recommended patient care methodology (i.e. practice change) is
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
necessarily warranted in the context of acquiring the patient-centred and goal oriented
outcomes in the population of interest. The healthcare proposal is based on the clinical
evidence that reveals the pattern of elevated mortality and morbidity experienced by the
demented patients under the influence of increased falling episodes (Kim et al. 2011). The
elevated falling rate in demented people leads to the substantial increase in their healthcare
cost as well as adverse psychological and physical outcomes.
Context
The configuration of an effective therapeutic relationship would require the active
engagement of nursing professionals, physicians, patients and their caretakers in the clinical
setting. Nurse professionals must undertake informed decision-making and systematically
involve the demented patients as well as their family members in the process of their medical
care and treatment (Smebye, Kirkevold & Engedal 2012). The multidisciplinary (i.e. team
based) collaboration between the healthcare professionals and direct engagement of nurses in
the process of patient communication will substantially decrease the scope of patient care
errors and increase the pattern of compliance, satisfaction and trust of the demented patients
on the recommended person-centred approaches (Wen & Schulman 2014). Resultantly, the
improvement in the healthcare outcomes will enhance the cognitive and somatic capacities of
the treated patients. This will eventually reduce their falling episodes and associated
traumatic manifestations.
Checkpoint – 3
Our key partners are likely to be: patients and their family members, nurses and physicians
Our key supporters are likely to be: Hospital management and administrative teams
We have a good relationship with: Patients and their care takers
outcomes in the population of interest. The healthcare proposal is based on the clinical
evidence that reveals the pattern of elevated mortality and morbidity experienced by the
demented patients under the influence of increased falling episodes (Kim et al. 2011). The
elevated falling rate in demented people leads to the substantial increase in their healthcare
cost as well as adverse psychological and physical outcomes.
Context
The configuration of an effective therapeutic relationship would require the active
engagement of nursing professionals, physicians, patients and their caretakers in the clinical
setting. Nurse professionals must undertake informed decision-making and systematically
involve the demented patients as well as their family members in the process of their medical
care and treatment (Smebye, Kirkevold & Engedal 2012). The multidisciplinary (i.e. team
based) collaboration between the healthcare professionals and direct engagement of nurses in
the process of patient communication will substantially decrease the scope of patient care
errors and increase the pattern of compliance, satisfaction and trust of the demented patients
on the recommended person-centred approaches (Wen & Schulman 2014). Resultantly, the
improvement in the healthcare outcomes will enhance the cognitive and somatic capacities of
the treated patients. This will eventually reduce their falling episodes and associated
traumatic manifestations.
Checkpoint – 3
Our key partners are likely to be: patients and their family members, nurses and physicians
Our key supporters are likely to be: Hospital management and administrative teams
We have a good relationship with: Patients and their care takers
We have some work to do on our relationship with: Multidisciplinary physicians
The overall response to our proposal is likely to be: Positive in terms of the sustained
enhancement of wellness outcomes in demented people
Checkpoint – 4
My analysis of the readiness of the workplace affirms the requirement of configuring a
protective environment to facilitate the reduction in work stress of nurses and eventual
increase in their interpersonal engagement with the demented people for reducing the
frequency of their falling episodes and associated traumatic conditions.
Facilitation
The dynamic therapeutic alliance and elevated clinician’s competence leads to
improved patient care outcomes (Campbell et al. 2015). The shortage of nursing staff and
their excessive workload might constrain them in terms of investing additional time in
improving the pattern of interpersonal relationship with the treated patient while utilizing
therapeutic communication (Alghamdi 2016). Eventually, this could impact the acquisition of
the treatment outcomes and the demented patient might continue to experience falls and
trauma at the same pace. The nurse professionals therefore, require developing
transformational leadership skills in the context of effectively delegating their daily work
requirements for reducing the level of their stress and additional time consumed in
undertaking the daily job roles (Negussie & Demissie 2013). The hospital administration
must also consider the provision of financial incentives in the context of accomplishing
additional patient requirements by the nurse professionals. In this manner, nurse professionals
will acquire motivation and enthusiasm with the objective of potentially configuring a
therapeutic relationship with the demented patients for reducing the frequency of their falling
episodes. An additional intervention for improving the desirable patient-centred outcomes
The overall response to our proposal is likely to be: Positive in terms of the sustained
enhancement of wellness outcomes in demented people
Checkpoint – 4
My analysis of the readiness of the workplace affirms the requirement of configuring a
protective environment to facilitate the reduction in work stress of nurses and eventual
increase in their interpersonal engagement with the demented people for reducing the
frequency of their falling episodes and associated traumatic conditions.
Facilitation
The dynamic therapeutic alliance and elevated clinician’s competence leads to
improved patient care outcomes (Campbell et al. 2015). The shortage of nursing staff and
their excessive workload might constrain them in terms of investing additional time in
improving the pattern of interpersonal relationship with the treated patient while utilizing
therapeutic communication (Alghamdi 2016). Eventually, this could impact the acquisition of
the treatment outcomes and the demented patient might continue to experience falls and
trauma at the same pace. The nurse professionals therefore, require developing
transformational leadership skills in the context of effectively delegating their daily work
requirements for reducing the level of their stress and additional time consumed in
undertaking the daily job roles (Negussie & Demissie 2013). The hospital administration
must also consider the provision of financial incentives in the context of accomplishing
additional patient requirements by the nurse professionals. In this manner, nurse professionals
will acquire motivation and enthusiasm with the objective of potentially configuring a
therapeutic relationship with the demented patients for reducing the frequency of their falling
episodes. An additional intervention for improving the desirable patient-centred outcomes
includes the administration of counselling and training sessions to the registered nurses in
relation to improving their work management skills in the clinical settings. This will
substantially improve their capacity of utilizing therapeutic communication while handling
dementia patients for the systematic accomplishment of the patient care goals.
Checkpoint – 5: List of specific pre-engagement actions
To prepare myself I will enhance my leadership skills and clinical expertise for effectively
mitigating the workplace challenges that arise under the influence of complex clinical
situations.
To prepare the workplace I will attempt to transform the work culture and facilitate the
organization of training sessions in the context of improving the patient handling skills of
nurse practitioners.
To prepare the people who will hopefully be involved, I will monitor their progress and
consistently motivate them towards the systematic acquisition of the patient-centred and
goal oriented healthcare targets.
Learning Resource
Indeed, BEET tool is an effectively modality for systematically engaging the medical
professionals and the treated patients in terms of bringing the desirable patient care outcomes.
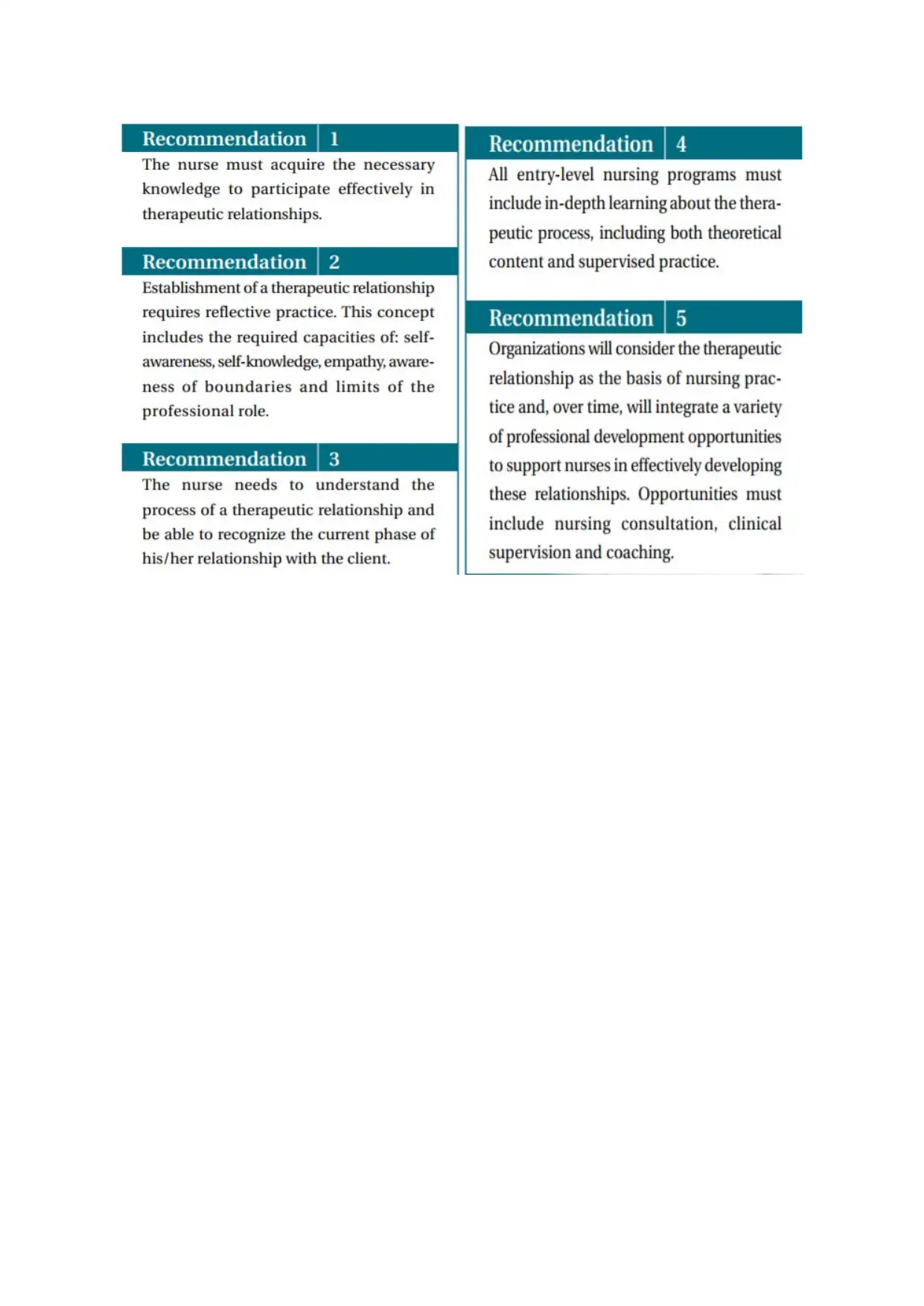
The presented context requires the effective implementation of the Top-14 best practice
recommendations with the objective of improving the therapeutic relationship of the
demented patients with the treating clinicians for acquiring the goal-oriented patient-centred
relation to improving their work management skills in the clinical settings. This will
substantially improve their capacity of utilizing therapeutic communication while handling
dementia patients for the systematic accomplishment of the patient care goals.
Checkpoint – 5: List of specific pre-engagement actions
To prepare myself I will enhance my leadership skills and clinical expertise for effectively
mitigating the workplace challenges that arise under the influence of complex clinical
situations.
To prepare the workplace I will attempt to transform the work culture and facilitate the
organization of training sessions in the context of improving the patient handling skills of
nurse practitioners.
To prepare the people who will hopefully be involved, I will monitor their progress and
consistently motivate them towards the systematic acquisition of the patient-centred and
goal oriented healthcare targets.
Learning Resource
Indeed, BEET tool is an effectively modality for systematically engaging the medical
professionals and the treated patients in terms of bringing the desirable patient care outcomes.
The presented context requires the effective implementation of the Top-14 best practice
recommendations with the objective of improving the therapeutic relationship of the
demented patients with the treating clinicians for acquiring the goal-oriented patient-centred
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
outcome (i.e. falls reduction) (Virani et al. 2002). These recommendations are sequentially
provided in the attached appendix. These recommendations require encapsulated in the walls
of the clinical setting in the context of motivating the nurse professionals, physicians,
demented patients and their family members for practicing therapeutic communication and
shared medical decision-making for systematic improvement in the psycho-socio-somatic
outcomes. The configuration of interpersonal relationship with the demented patients through
extended professional communication (while utilizing the practice recommendations will
substantially reduce the risk of their prospective falls in the clinical as well as residential
settings.
Practice Implications
The practice implications of the recommended Top-14 recommendations include the
substantial reduction in the length of stay of the demented patients in the clinical settings and
reduction in the additional cost incurred in treating traumatic complications that emanate
under the influence of frequent falling episodes. The empathic and person-centred healthcare
approaches will improve the pattern of self-sufficiency of the demented patients and increase
their partnership in the process of medical decision-making. The systematic deployment of
goal oriented dementia care approaches in the clinical settings will eventually reduce the
development of co-morbid states and physical challenges that could potentially elevate the
scope of falls and associated trauma.
Conclusion
The BEET tool was categorically explored for evaluating the scope of establishing a
systematic transformation in the conventional practice methodology for the demented patients
in the context of reducing their frequency of falls and traumatic conditions. The subject of
study was researched in evidence-based literature and the findings advocated the requirement
of actively engaging the nurse professionals and patients in the process of medical decision-
provided in the attached appendix. These recommendations require encapsulated in the walls
of the clinical setting in the context of motivating the nurse professionals, physicians,
demented patients and their family members for practicing therapeutic communication and
shared medical decision-making for systematic improvement in the psycho-socio-somatic
outcomes. The configuration of interpersonal relationship with the demented patients through
extended professional communication (while utilizing the practice recommendations will
substantially reduce the risk of their prospective falls in the clinical as well as residential
settings.
Practice Implications
The practice implications of the recommended Top-14 recommendations include the
substantial reduction in the length of stay of the demented patients in the clinical settings and
reduction in the additional cost incurred in treating traumatic complications that emanate
under the influence of frequent falling episodes. The empathic and person-centred healthcare
approaches will improve the pattern of self-sufficiency of the demented patients and increase
their partnership in the process of medical decision-making. The systematic deployment of
goal oriented dementia care approaches in the clinical settings will eventually reduce the
development of co-morbid states and physical challenges that could potentially elevate the
scope of falls and associated trauma.
Conclusion
The BEET tool was categorically explored for evaluating the scope of establishing a
systematic transformation in the conventional practice methodology for the demented patients
in the context of reducing their frequency of falls and traumatic conditions. The subject of
study was researched in evidence-based literature and the findings advocated the requirement
of actively engaging the nurse professionals and patients in the process of medical decision-

making with the utilization of therapeutic communication. The Top – 14 best practice
recommendations require implementation in the dementia care settings for enhancing the
pattern of person-centred approaches requiring administration with the objective of reducing
the frequency of falling episodes and associated adverse clinical complications in the
demented people.
References
Abdolrahimi, M, Ghiyasvandian, S, Zakerimoghadam, M & Ebadi, A 2017, 'Therapeutic
communication in nursing students: A Walker & Avant concept analysis', Electronic
recommendations require implementation in the dementia care settings for enhancing the
pattern of person-centred approaches requiring administration with the objective of reducing
the frequency of falling episodes and associated adverse clinical complications in the
demented people.
References
Abdolrahimi, M, Ghiyasvandian, S, Zakerimoghadam, M & Ebadi, A 2017, 'Therapeutic
communication in nursing students: A Walker & Avant concept analysis', Electronic
Physician, vol 9, no. 8, pp. 4968-4977,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5614280/>.
Aizen , E 2015, 'FALLS IN PATIENTS WITH DEMENTIA', Harefuah, vol 154, no. 5, pp.
323-6, 338, <https://www.ncbi.nlm.nih.gov/pubmed/26168645>.
Alghamdi , MG 2016, 'Nursing workload: a concept analysis', Journal of Nursing
Management, vol 24, no. 4, pp. 449-457,
<https://www.ncbi.nlm.nih.gov/pubmed/26749124>.
Bunn, F, Dickinson, A, Simpson, C, Narayanan, V, Humphrey, D, Griffiths, C, Martin, W &
Victor, C 2014, 'Preventing falls among older people with mental health problems: a
systematic review', BMC Nursing,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3942767/>.
Campbell, BK, Guydish, J, Le, T, Wells, EA & MacCarty, D 2015, 'The Relationship of
Therapeutic Alliance and Treatment Delivery Fidelity with Treatment Retention in a
Multisite Trial of Twelve-Step Facilitation', Psychology of Addictive Behaviors, vol 29, no. 1,
pp. 106-113, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4739723/>.
Detweiler, MB, Sharma, T, Detweiler, JG, Murphy, PF, Lane, S, Carman, J, Chudhary, AS,
Halling, MH & Kim, KY 2012, 'What Is the Evidence to Support the Use of Therapeutic
Gardens for the Elderly?', Psychiatry Investigation, vol 9, no. 2, pp. 100-110,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3372556/>.
Hammond, T & Wilson, A 2013, 'Polypharmacy and Falls in the Elderly: A Literature
Review', Nursing and Midwifery Studies, vol 2, no. 2, pp. 171-175,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4228551/>.
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5614280/>.
Aizen , E 2015, 'FALLS IN PATIENTS WITH DEMENTIA', Harefuah, vol 154, no. 5, pp.
323-6, 338, <https://www.ncbi.nlm.nih.gov/pubmed/26168645>.
Alghamdi , MG 2016, 'Nursing workload: a concept analysis', Journal of Nursing
Management, vol 24, no. 4, pp. 449-457,
<https://www.ncbi.nlm.nih.gov/pubmed/26749124>.
Bunn, F, Dickinson, A, Simpson, C, Narayanan, V, Humphrey, D, Griffiths, C, Martin, W &
Victor, C 2014, 'Preventing falls among older people with mental health problems: a
systematic review', BMC Nursing,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3942767/>.
Campbell, BK, Guydish, J, Le, T, Wells, EA & MacCarty, D 2015, 'The Relationship of
Therapeutic Alliance and Treatment Delivery Fidelity with Treatment Retention in a
Multisite Trial of Twelve-Step Facilitation', Psychology of Addictive Behaviors, vol 29, no. 1,
pp. 106-113, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4739723/>.
Detweiler, MB, Sharma, T, Detweiler, JG, Murphy, PF, Lane, S, Carman, J, Chudhary, AS,
Halling, MH & Kim, KY 2012, 'What Is the Evidence to Support the Use of Therapeutic
Gardens for the Elderly?', Psychiatry Investigation, vol 9, no. 2, pp. 100-110,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3372556/>.
Hammond, T & Wilson, A 2013, 'Polypharmacy and Falls in the Elderly: A Literature
Review', Nursing and Midwifery Studies, vol 2, no. 2, pp. 171-175,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4228551/>.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
IOM 2013, 'Engaging Patients, Families, and Communities', in Best Care at Lower Cost: The
Path to Continuously Learning Health Care in America, National Academies Press, USA,
<https://www.ncbi.nlm.nih.gov/books/NBK207234/>.
Jong, MRD, Elst, MVD & Hartholt, KA 2013, 'Drug-related falls in older patients: implicated
drugs, consequences, and possible prevention strategies', Therapeutic Advances in Drug
Safety, vol 4, no. 4, pp. 147-154,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4125318/>.
Jootun , D & McGhee , G 2011, 'Effective communication with people who have dementia',
Nursing Standard, vol 25, no. 25, pp. 40-46,
<https://www.ncbi.nlm.nih.gov/pubmed/21469475>.
Kim, DH, Brown , RT, Ding, EL, Kiel, DP & Berry, SD 2011, 'Dementia Medications and
Risk of Falls, Syncope, and Related Adverse Events Meta-Analysis of Randomized
Controlled Trials', Journal of the American Geriatrics Society, vol 59, no. 6, pp. 1019-1031,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3260523/>.
Negussie, N & Demissie, A 2013, 'Relationship Between Leadership Styles of Nurese
Managers and Nurses' Job Satisfaction in Jimma University Specialized Hospital', Ethiopian
Journal of Health Science, vol 23, no. 1, pp. 49-58,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3613815/>.
Phelan, EA, Mahoney, JE, Voit, JC & Stevens, JA 2015, 'Assessment and Management of
Fall Risk in Primary Care Settings', Medical Clinics of North America, vol 99, no. 2, pp. 281-
293, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4707663/>.
Segev-Jacubovski, O, Herman, T, Yogev-Seligmann, G, Mirelman, A, Giladi, N &
Hausdorff, JM 2011, 'The interplay between gait, falls and cognition: can cognitive therapy
Path to Continuously Learning Health Care in America, National Academies Press, USA,
<https://www.ncbi.nlm.nih.gov/books/NBK207234/>.
Jong, MRD, Elst, MVD & Hartholt, KA 2013, 'Drug-related falls in older patients: implicated
drugs, consequences, and possible prevention strategies', Therapeutic Advances in Drug
Safety, vol 4, no. 4, pp. 147-154,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4125318/>.
Jootun , D & McGhee , G 2011, 'Effective communication with people who have dementia',
Nursing Standard, vol 25, no. 25, pp. 40-46,
<https://www.ncbi.nlm.nih.gov/pubmed/21469475>.
Kim, DH, Brown , RT, Ding, EL, Kiel, DP & Berry, SD 2011, 'Dementia Medications and
Risk of Falls, Syncope, and Related Adverse Events Meta-Analysis of Randomized
Controlled Trials', Journal of the American Geriatrics Society, vol 59, no. 6, pp. 1019-1031,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3260523/>.
Negussie, N & Demissie, A 2013, 'Relationship Between Leadership Styles of Nurese
Managers and Nurses' Job Satisfaction in Jimma University Specialized Hospital', Ethiopian
Journal of Health Science, vol 23, no. 1, pp. 49-58,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3613815/>.
Phelan, EA, Mahoney, JE, Voit, JC & Stevens, JA 2015, 'Assessment and Management of
Fall Risk in Primary Care Settings', Medical Clinics of North America, vol 99, no. 2, pp. 281-
293, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4707663/>.
Segev-Jacubovski, O, Herman, T, Yogev-Seligmann, G, Mirelman, A, Giladi, N &
Hausdorff, JM 2011, 'The interplay between gait, falls and cognition: can cognitive therapy
reduce fall risk?', Expert Review of Neurotherapeutics, vol 11, no. 7, pp. 1057–1075,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3163836/>.
Smebye, KL, Kirkevold, M & Engedal, K 2012, 'How do persons with dementia participate
in decision making related to health and daily care? A multi-case study', BMC Health
Services Research, p. 241, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3475075/>.
Struksnes, S, Bachrach-Lindström, M, Hall-Lord, ML, Slaasletten, R & Johansson, I 2011,
'The nursing staff's opinion of falls among older persons with dementia. a cross-sectional
study', BMC Nursing, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3142214/>.
Swaminathan, A & Jicha, GA 2014, 'Nutrition and prevention of Alzheimer’s dementia',
Frontiers in Aging Neuroscience, p. 282,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4202787/>.
Velea, P & Purcărea, VL 2014, 'Issues of therapeutic communication relevant for improving
quality of care', Journal of Medicine and Life, vol 7, no. 4, pp. 39-45,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4813615/>.
Virani, T, Tait, A, McConnell, H, Scott, C & Gergolas, E 2002, Nursing Best Practice
Guideline - Shaping the future of Nursing (Establishing Therapeutic Relationships), RNAO,
Ontario, <http://rnao.ca/sites/rnao-ca/files/Establishing_Therapeutic_Relationships.pdf>.
Wen, J & Schulman, KA 2014, 'Can Team-Based Care Improve Patient Satisfaction? A
Systematic Review of Randomized Controlled Trials', PLoS One, vol 9, no. 7,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4094385/>.
Westermann, S, Cavelti, M, Heibach, E & Caspar, F 2015, 'Motive-oriented therapeutic
relationship building for patients diagnosed with schizophrenia', Frontiers in Psychology, p.
1294, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4557062/>.
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3163836/>.
Smebye, KL, Kirkevold, M & Engedal, K 2012, 'How do persons with dementia participate
in decision making related to health and daily care? A multi-case study', BMC Health
Services Research, p. 241, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3475075/>.
Struksnes, S, Bachrach-Lindström, M, Hall-Lord, ML, Slaasletten, R & Johansson, I 2011,
'The nursing staff's opinion of falls among older persons with dementia. a cross-sectional
study', BMC Nursing, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3142214/>.
Swaminathan, A & Jicha, GA 2014, 'Nutrition and prevention of Alzheimer’s dementia',
Frontiers in Aging Neuroscience, p. 282,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4202787/>.
Velea, P & Purcărea, VL 2014, 'Issues of therapeutic communication relevant for improving
quality of care', Journal of Medicine and Life, vol 7, no. 4, pp. 39-45,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4813615/>.
Virani, T, Tait, A, McConnell, H, Scott, C & Gergolas, E 2002, Nursing Best Practice
Guideline - Shaping the future of Nursing (Establishing Therapeutic Relationships), RNAO,
Ontario, <http://rnao.ca/sites/rnao-ca/files/Establishing_Therapeutic_Relationships.pdf>.
Wen, J & Schulman, KA 2014, 'Can Team-Based Care Improve Patient Satisfaction? A
Systematic Review of Randomized Controlled Trials', PLoS One, vol 9, no. 7,
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4094385/>.
Westermann, S, Cavelti, M, Heibach, E & Caspar, F 2015, 'Motive-oriented therapeutic
relationship building for patients diagnosed with schizophrenia', Frontiers in Psychology, p.
1294, <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4557062/>.

Appendix
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
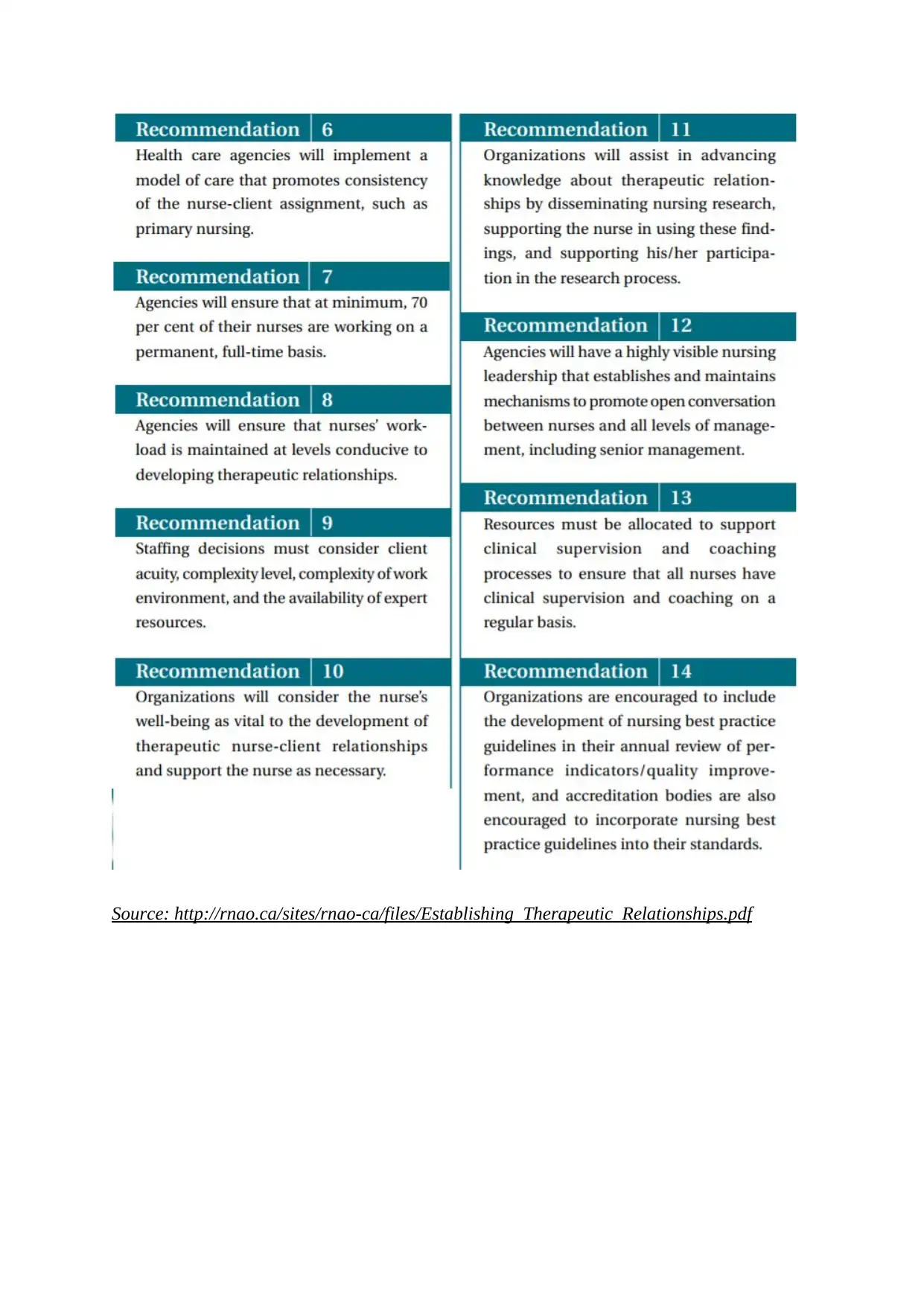
Source: http://rnao.ca/sites/rnao-ca/files/Establishing_Therapeutic_Relationships.pdf

1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





