Human Respiratory and Cardiac Systems
VerifiedAdded on 2023/01/19
|26
|3751
|23
AI Summary
This document provides information on the human respiratory and cardiac systems. It covers topics such as inspiration, expiration, the structure of the trachea, and the functions of the alveoli. The document also includes a comparison between arteries and veins. Study material and solved assignments on this topic can be found on Desklib.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

HUMAN RESPIRATORY AND CARDIAC SYSTEMS
Student`s Name
Course Name
Professor`s Name
Institutional Affiliation
6th April, 2019
1
Student`s Name
Course Name
Professor`s Name
Institutional Affiliation
6th April, 2019
1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

Task 1
1. Nasal Cavity
2. Bronchus
3. Bronchiole
4. Alveolar duct
5. Pharynx
6. Trachea
7. Bronchus
8. Diaphragm
B ) Inspiration
2
1. Nasal Cavity
2. Bronchus
3. Bronchiole
4. Alveolar duct
5. Pharynx
6. Trachea
7. Bronchus
8. Diaphragm
B ) Inspiration
2
Rijnberk and Stokhof (2009, p 63-74) explain the process of inspiration. Respiration
occurs due to the movements of the respiratory muscles, the internal and external
intercostal muscles along with the diaphragm. During inspiration, the diaphragm
contracts, the internal intercostal muscles relax while the external intercostal muscles
contract thereby causing the rib cage to expand and move outward leading to an
increase in the volume of the thoracic cavity. This increase in the volume of the lungs
leads to a decrease in intra-alveolar pressure making it lower than atmospheric
pressure. The pressure accumulated then drives air into the lungs.
Expiration
During expiration, the diaphragm relaxes, the external intercostal muscles relax
whereas the internal intercostal muscles contract. This causes the ribcage to move
inwards and exerting pressure on the lungs. The effect is that the interpulmonary
pressure in the chest cavity rises above the atmospheric pressure, causing air to be
pushed out of the lungs.
3
occurs due to the movements of the respiratory muscles, the internal and external
intercostal muscles along with the diaphragm. During inspiration, the diaphragm
contracts, the internal intercostal muscles relax while the external intercostal muscles
contract thereby causing the rib cage to expand and move outward leading to an
increase in the volume of the thoracic cavity. This increase in the volume of the lungs
leads to a decrease in intra-alveolar pressure making it lower than atmospheric
pressure. The pressure accumulated then drives air into the lungs.
Expiration
During expiration, the diaphragm relaxes, the external intercostal muscles relax
whereas the internal intercostal muscles contract. This causes the ribcage to move
inwards and exerting pressure on the lungs. The effect is that the interpulmonary
pressure in the chest cavity rises above the atmospheric pressure, causing air to be
pushed out of the lungs.
3

Figure 1: Inspiration and Expiration, Rijnberk, Stokhof(2009)
C
The trachea is a wide hollow tube that connects the larynx and the bronchi of
the lungs. It also allows the passage of air in and out of the lungs during the breathing
process. To perform its functions effectively, the trachea’s structure has certain
adaptations.
The trachea has a thin membranous wall which is made up of C-shaped rings of
cartilage. The rings of cartilage may be between 16 and 20 in number along the whole
4
C
The trachea is a wide hollow tube that connects the larynx and the bronchi of
the lungs. It also allows the passage of air in and out of the lungs during the breathing
process. To perform its functions effectively, the trachea’s structure has certain
adaptations.
The trachea has a thin membranous wall which is made up of C-shaped rings of
cartilage. The rings of cartilage may be between 16 and 20 in number along the whole
4
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
length of the trachea. These rings of cartilage provide support to the trachea and keep
it open at all times for efficient airflow.
The walls of the trachea are made up of four walls of specialized tissues:
1. The Mucosa: it is the innermost layer and is made up of ciliated pseudostratified
columnar epithelium with numerous goblet cells. Goblet cells produce mucus, a sticky
substance that covers the inner lining of the trachea, used to trap any debris and
particles that may be in inhaled air before the particles reach the lungs. On the surface
of the columnar cells are cilia that work together in a rhythmic movement hence
pushing the mucous along with the trapped debris away from the lungs to the larynx
where it is either swallowed or expelled through coughing.
2. The Submucosa layer: this is a layer just below the mucosa. This layer of tissue
consists of areolar connective tissue containing blood vessels and the nervous tissue.
The collagen, elastic and reticular protein fibers provide support and elasticity to the
tracheal walls (Barclay, 2018). The blood vessels and nerves, on the other hand,
support the other layers of the tracheal wall. For the trachea to be able to adjust its
diameter appropriately, there are longitudinal smooth muscle fibers on the outside
trachea between the rings of cartilage.
3. Hyaline Cartilage: this is a layer surrounding the submucosa, and it forms the
supportive rings of the trachea. It also forms a strong and flexible structure that helps
in maintaining an open airway in the trachea while being resistant to external forces.
4. The Adventitia: this is the outermost layer of the tracheal wall made up of areolar
connective tissue. It anchors the trachea loosely to other surrounding soft tissues
structures.
D)
5
it open at all times for efficient airflow.
The walls of the trachea are made up of four walls of specialized tissues:
1. The Mucosa: it is the innermost layer and is made up of ciliated pseudostratified
columnar epithelium with numerous goblet cells. Goblet cells produce mucus, a sticky
substance that covers the inner lining of the trachea, used to trap any debris and
particles that may be in inhaled air before the particles reach the lungs. On the surface
of the columnar cells are cilia that work together in a rhythmic movement hence
pushing the mucous along with the trapped debris away from the lungs to the larynx
where it is either swallowed or expelled through coughing.
2. The Submucosa layer: this is a layer just below the mucosa. This layer of tissue
consists of areolar connective tissue containing blood vessels and the nervous tissue.
The collagen, elastic and reticular protein fibers provide support and elasticity to the
tracheal walls (Barclay, 2018). The blood vessels and nerves, on the other hand,
support the other layers of the tracheal wall. For the trachea to be able to adjust its
diameter appropriately, there are longitudinal smooth muscle fibers on the outside
trachea between the rings of cartilage.
3. Hyaline Cartilage: this is a layer surrounding the submucosa, and it forms the
supportive rings of the trachea. It also forms a strong and flexible structure that helps
in maintaining an open airway in the trachea while being resistant to external forces.
4. The Adventitia: this is the outermost layer of the tracheal wall made up of areolar
connective tissue. It anchors the trachea loosely to other surrounding soft tissues
structures.
D)
5

Structure and functions of the alveolus
The alveoli are only one cell thick in order to make the path of diffusion of oxygen
between alveoli and blood capillaries shorter.
An alveolar duct is a tube that is made up of connective tissue and smooth muscle and
opens up to a cluster of alveoli. A collection of many individual alveoli is known as
an alveolar sac (Biga et al. 2019).
Alveoli epithelium is composed of two types of cells, type 1 and type 2. Type 1 cells
make up about 95 percent of the surface and constitute mainly the air-blood barrier.
The type 1 cells form an epithelium that is attached to a thin elastic basement
membrane. The membrane is extremely thin and borders the capillary endothelial
membrane. These two epithelial membranes taken together form what is known as a
respiratory membrane, which is about 0.5mm, thick.it is across this membrane that
gaseous exchange occurs (Knudsen and Ochs, 2018).
6
The alveoli are only one cell thick in order to make the path of diffusion of oxygen
between alveoli and blood capillaries shorter.
An alveolar duct is a tube that is made up of connective tissue and smooth muscle and
opens up to a cluster of alveoli. A collection of many individual alveoli is known as
an alveolar sac (Biga et al. 2019).
Alveoli epithelium is composed of two types of cells, type 1 and type 2. Type 1 cells
make up about 95 percent of the surface and constitute mainly the air-blood barrier.
The type 1 cells form an epithelium that is attached to a thin elastic basement
membrane. The membrane is extremely thin and borders the capillary endothelial
membrane. These two epithelial membranes taken together form what is known as a
respiratory membrane, which is about 0.5mm, thick.it is across this membrane that
gaseous exchange occurs (Knudsen and Ochs, 2018).
6
Type 2 cells are smaller in size than type 1 and they produce the surfactant that forms
the coating in the inside surface of the alveolus helping to reduce surface tension. It is
the surfactant that is responsible for maintaining the shape of the alveoli every time
you inhale and exhale. Type 2 alveoli cells may also turn into stem cells if need be.
(Hecht, 2018)
There are over 700million alveoli in the lungs to increase and maximise the surface
area for gaseous exchange. Alveoli also have thin and elastic walls that expand during
inhalation thereby increasing the surface area for gaseous exchange. They are
connected to each other by alveolar pores to maintain a steady pressure throughout the
lung.
The alveolar macrophage is a phagocytic cell that moves around the alveolus to
remove debris and pathogens that managed to find their way into the alveolus.
The internal environment of the alveoli is kept warm and moist for optimum gaseous
exchange to take place. Gases can only cross the cell membranes while they are
dissolved in water and therefore the alveolar membranes are always moist. (Eldridge,
2018)
Task 2:
a)
7
the coating in the inside surface of the alveolus helping to reduce surface tension. It is
the surfactant that is responsible for maintaining the shape of the alveoli every time
you inhale and exhale. Type 2 alveoli cells may also turn into stem cells if need be.
(Hecht, 2018)
There are over 700million alveoli in the lungs to increase and maximise the surface
area for gaseous exchange. Alveoli also have thin and elastic walls that expand during
inhalation thereby increasing the surface area for gaseous exchange. They are
connected to each other by alveolar pores to maintain a steady pressure throughout the
lung.
The alveolar macrophage is a phagocytic cell that moves around the alveolus to
remove debris and pathogens that managed to find their way into the alveolus.
The internal environment of the alveoli is kept warm and moist for optimum gaseous
exchange to take place. Gases can only cross the cell membranes while they are
dissolved in water and therefore the alveolar membranes are always moist. (Eldridge,
2018)
Task 2:
a)
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
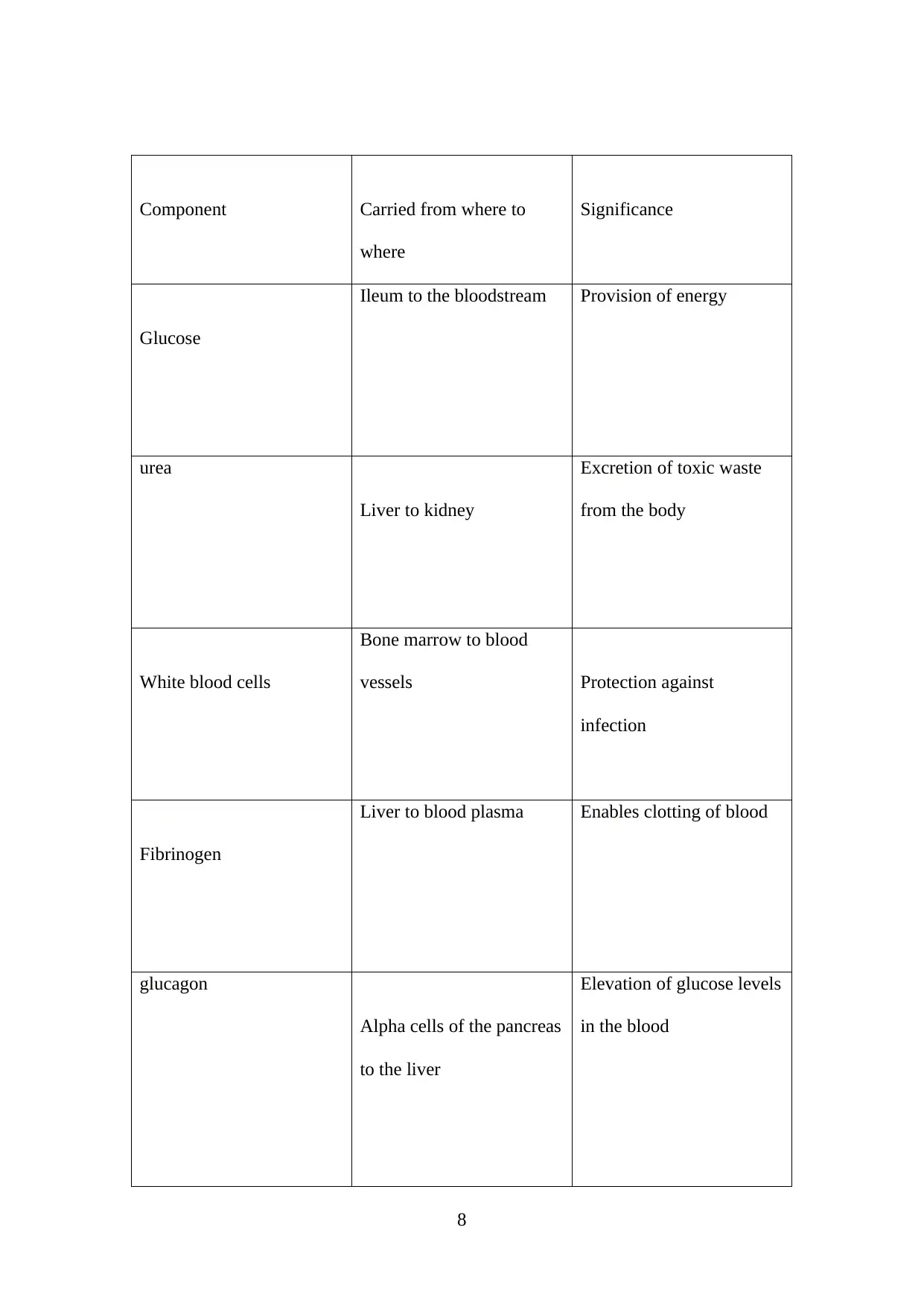
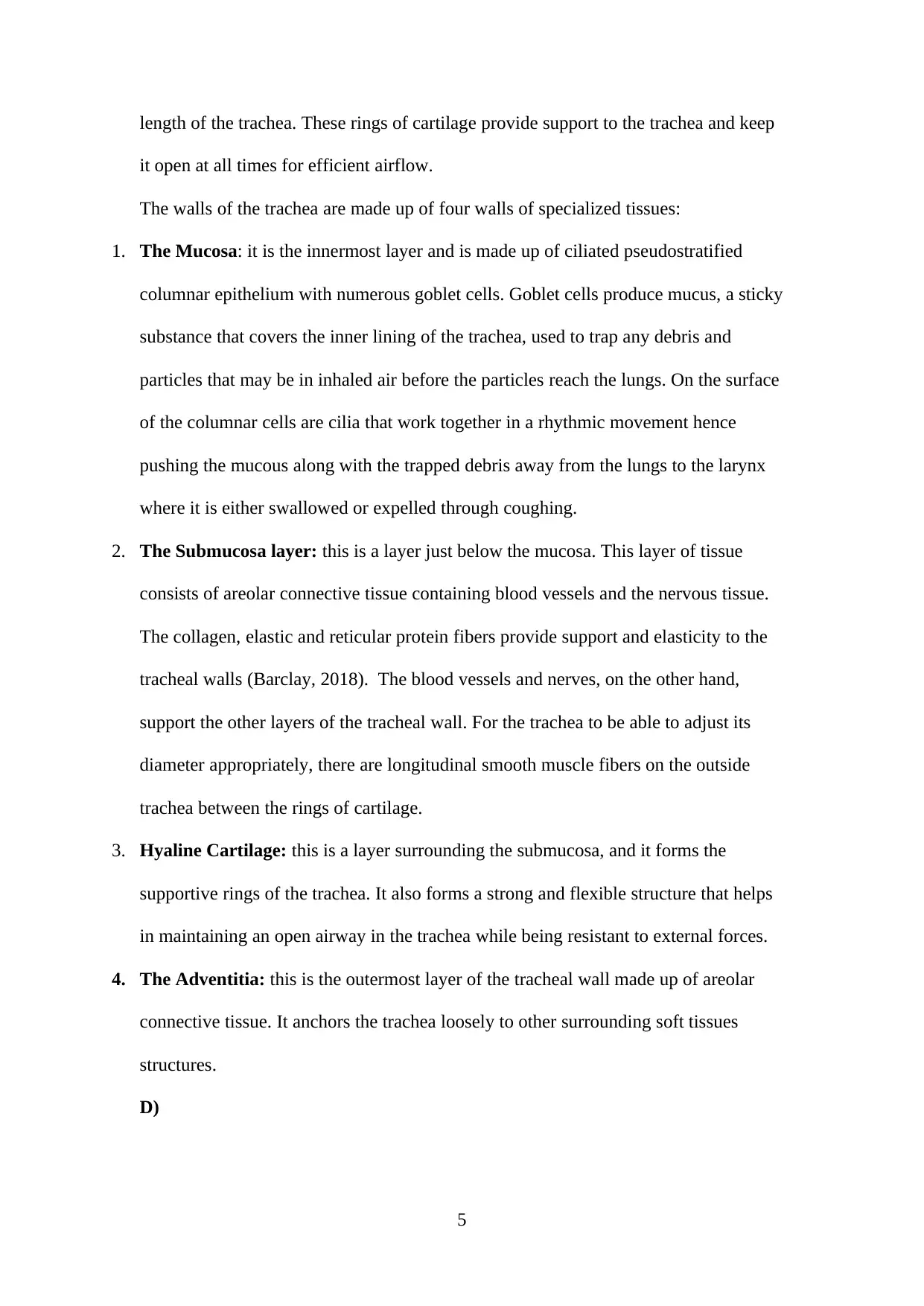
Component Carried from where to
where
Significance
Glucose
Ileum to the bloodstream Provision of energy
urea
Liver to kidney
Excretion of toxic waste
from the body
White blood cells
Bone marrow to blood
vessels Protection against
infection
Fibrinogen
Liver to blood plasma Enables clotting of blood
glucagon
Alpha cells of the pancreas
to the liver
Elevation of glucose levels
in the blood
8
where
Significance
Glucose
Ileum to the bloodstream Provision of energy
urea
Liver to kidney
Excretion of toxic waste
from the body
White blood cells
Bone marrow to blood
vessels Protection against
infection
Fibrinogen
Liver to blood plasma Enables clotting of blood
glucagon
Alpha cells of the pancreas
to the liver
Elevation of glucose levels
in the blood
8

Platelets
Bone marrow to the blood
vessels
Coagulation of blood
9
Bone marrow to the blood
vessels
Coagulation of blood
9

1. The biconcave shape of the red bool cells increases the surface area for oxygen
absorption
2. The red blood cells contain haemoglobin-a red protein that combines with oxygen to
form oxyhaemoglobin which is then transported to cells around the body
3. The red blood cells do not have a nucleus to pack more haemoglobin in the cells
b) The graph below shows the amount of oxygen carried by haemoglobin (% saturation)
at different concentrations of oxygen (partial pressure of oxygen ).
10
absorption
2. The red blood cells contain haemoglobin-a red protein that combines with oxygen to
form oxyhaemoglobin which is then transported to cells around the body
3. The red blood cells do not have a nucleus to pack more haemoglobin in the cells
b) The graph below shows the amount of oxygen carried by haemoglobin (% saturation)
at different concentrations of oxygen (partial pressure of oxygen ).
10
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

The partial pressure of any gas in a gaseous mixture is the equivalent to the amount of
pressure the same gas would exert if it occupied the space alone.
The partial pressure of oxygen is the measurement of oxygen in arterial blood and is
also known as PaO2. It is an indicator of how well oxygen can move from the lungs to
the bloodstream.
The alveolar gas equation is used to calculate alveolar oxygen pressure. The equation
is:
PAO2=(Patm-PH20) FiO2-PaCO2/RQ
This equation is used to calculate the driving force for diffusion of oxygen gases
across alveolar membranes, pulmonary capillary walls and into the arteriolar blood
flow for transportation by erythrocytes. (Leader, 2019)
The oxygen dissociation curve has the distinctive sigmoid shape due to the co-
operative binding of oxygen to the four polypeptide chains. This means that
haemoglobin has greater chances of binding with oxygen when a sub-unit has already
bound oxygen. Haemoglobin has its highest affinity for oxygen when 3 of the 4
polypeptide chains are bound to oxygen. There is a positive feedback effect whereby
loading oxygen accelerates the loading of more oxygen and this accounts for the
rapidly rising midpoint of the sigmoid curve. The graph plateaus when all four
11
pressure the same gas would exert if it occupied the space alone.
The partial pressure of oxygen is the measurement of oxygen in arterial blood and is
also known as PaO2. It is an indicator of how well oxygen can move from the lungs to
the bloodstream.
The alveolar gas equation is used to calculate alveolar oxygen pressure. The equation
is:
PAO2=(Patm-PH20) FiO2-PaCO2/RQ
This equation is used to calculate the driving force for diffusion of oxygen gases
across alveolar membranes, pulmonary capillary walls and into the arteriolar blood
flow for transportation by erythrocytes. (Leader, 2019)
The oxygen dissociation curve has the distinctive sigmoid shape due to the co-
operative binding of oxygen to the four polypeptide chains. This means that
haemoglobin has greater chances of binding with oxygen when a sub-unit has already
bound oxygen. Haemoglobin has its highest affinity for oxygen when 3 of the 4
polypeptide chains are bound to oxygen. There is a positive feedback effect whereby
loading oxygen accelerates the loading of more oxygen and this accounts for the
rapidly rising midpoint of the sigmoid curve. The graph plateaus when all four
11
polypeptide chains have loaded oxygen and the haemoglobin approaches 100%
saturation.
During exercise, a muscle produces more carbon dioxide while at the same
having a high oxygen affinity. In such a muscle, the partial pressure of carbon dioxide
increases while the partial pressure of oxygen decreases (Boulos and Schmidt, 2017,
p. 140).
Blood in the veins returning to the lungs will have a higher partial pressure of
carbon dioxide and a lower partial pressure of oxygen. The air in the alveoli, on the
other hand, has a higher partial pressure of oxygen and a lower partial pressure of
carbon dioxide. The effect of this will be an increase in the diffusion gradient for both
carbon dioxide and oxygen in the lungs and this will result in a more rapid and greater
amount of gaseous exchange. The high partial pressure of the oxygen in the alveoli
and relatively low partial pressure of oxygen in the blood ensures that haemoglobin is
almost fully saturated with oxygen and this leads to more oxygen being supplied to
the exercising muscles (Sharma and Rawat, 2019).
Arthurs and Sudhakar (2010, p 207-210) posit that transport of Carbon Dioxide in
the blood happens in three forms:
1. Dissolved in solution: Carbon dioxide obeys Henry’s Law that the number of
molecules in solution is proportional to the partial pressure at the liquid surface and it
is 20 times more soluble than oxygen. The partial pressure of Carbon Dioxide in
5.3pKa in arterial blood while it is 6.1pKa in mixed venous blood. Arterial blood will
12
saturation.
During exercise, a muscle produces more carbon dioxide while at the same
having a high oxygen affinity. In such a muscle, the partial pressure of carbon dioxide
increases while the partial pressure of oxygen decreases (Boulos and Schmidt, 2017,
p. 140).
Blood in the veins returning to the lungs will have a higher partial pressure of
carbon dioxide and a lower partial pressure of oxygen. The air in the alveoli, on the
other hand, has a higher partial pressure of oxygen and a lower partial pressure of
carbon dioxide. The effect of this will be an increase in the diffusion gradient for both
carbon dioxide and oxygen in the lungs and this will result in a more rapid and greater
amount of gaseous exchange. The high partial pressure of the oxygen in the alveoli
and relatively low partial pressure of oxygen in the blood ensures that haemoglobin is
almost fully saturated with oxygen and this leads to more oxygen being supplied to
the exercising muscles (Sharma and Rawat, 2019).
Arthurs and Sudhakar (2010, p 207-210) posit that transport of Carbon Dioxide in
the blood happens in three forms:
1. Dissolved in solution: Carbon dioxide obeys Henry’s Law that the number of
molecules in solution is proportional to the partial pressure at the liquid surface and it
is 20 times more soluble than oxygen. The partial pressure of Carbon Dioxide in
5.3pKa in arterial blood while it is 6.1pKa in mixed venous blood. Arterial blood will
12

contain approximately 2.5ml per 100ml of dissolved carbon dioxide while venous
blood will contain 3ml per 100ml. A cardiac output of 5litres per minute will transport
150ml of dissolved carbon dioxide to the lungs, of which only 25ml will be exhaled.
This high solubility and capacity to diffuse causes carbon dioxide partial pressure in
the alveolar cavity and pulmonary end-capillary blood to be virtually similar. (Arthurs
and Sudhakar, 2010)
2. Carbonic Acid: Carbon dioxide combines with water to form the weak carbonic acid,
in a reaction catalyzed by carbonic anhydrase. The carbonic acid freely dissociates
after being formed into hydrogen ions and bicarbonate ions. The bicarbonate ions
diffuse freely out of the red blood cell into the plasma and are exchanged with
Chloride ions in a process known as the Chloride Shift.
3. Bound to hemoglobin and other proteins: carbon dioxide combines rapidly with the
terminal uncharged amino groups(R-NH2) to form carbamino groups. Haemoglobin
on the other hand has a different effect when forming carbaminohaemoglobin.
Reduced haemoglobin is the only effective protein buffer of hydrogen ions at
physiological pH conditions. This is because it has a high concentration of the amino
acid histidine. Hydrogen ions get attached to the histidine’s imidazole group.
Approximately 30% of carbon dioxide exhaled in the lungs was combined with
haemoglobin protein. The amount of carbon dioxide in carbamino form is small but it
still caters for a third of the difference between venous and arterial carbon dioxide
content. It takes a lower partial pressure for carbon dioxide to combine with
haemoglobin than it does for oxygen but haemoglobin still carries and transports less
than a quarter the amount of carbon dioxide as compared to oxygen.
Task 3
13
blood will contain 3ml per 100ml. A cardiac output of 5litres per minute will transport
150ml of dissolved carbon dioxide to the lungs, of which only 25ml will be exhaled.
This high solubility and capacity to diffuse causes carbon dioxide partial pressure in
the alveolar cavity and pulmonary end-capillary blood to be virtually similar. (Arthurs
and Sudhakar, 2010)
2. Carbonic Acid: Carbon dioxide combines with water to form the weak carbonic acid,
in a reaction catalyzed by carbonic anhydrase. The carbonic acid freely dissociates
after being formed into hydrogen ions and bicarbonate ions. The bicarbonate ions
diffuse freely out of the red blood cell into the plasma and are exchanged with
Chloride ions in a process known as the Chloride Shift.
3. Bound to hemoglobin and other proteins: carbon dioxide combines rapidly with the
terminal uncharged amino groups(R-NH2) to form carbamino groups. Haemoglobin
on the other hand has a different effect when forming carbaminohaemoglobin.
Reduced haemoglobin is the only effective protein buffer of hydrogen ions at
physiological pH conditions. This is because it has a high concentration of the amino
acid histidine. Hydrogen ions get attached to the histidine’s imidazole group.
Approximately 30% of carbon dioxide exhaled in the lungs was combined with
haemoglobin protein. The amount of carbon dioxide in carbamino form is small but it
still caters for a third of the difference between venous and arterial carbon dioxide
content. It takes a lower partial pressure for carbon dioxide to combine with
haemoglobin than it does for oxygen but haemoglobin still carries and transports less
than a quarter the amount of carbon dioxide as compared to oxygen.
Task 3
13
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
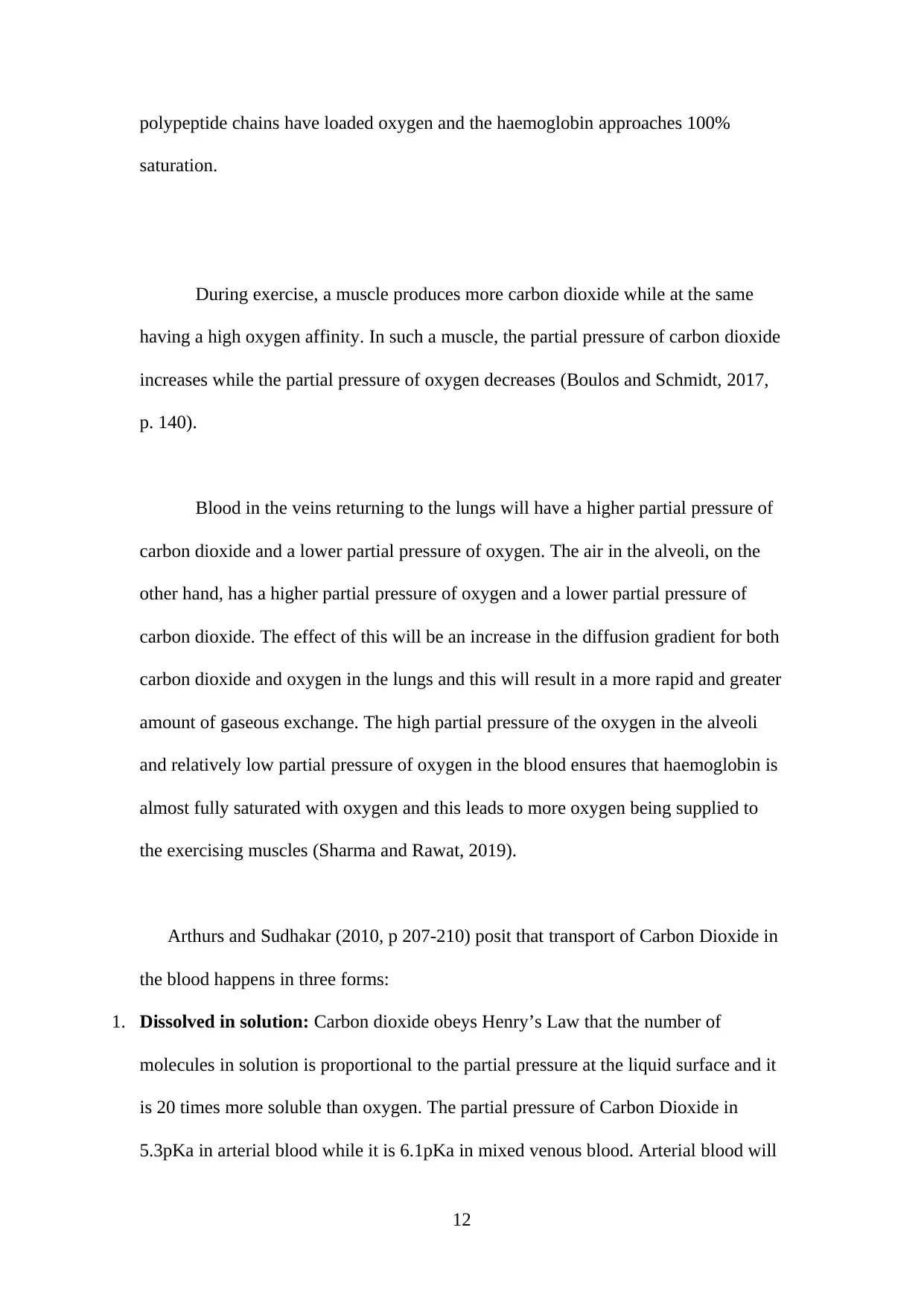
B A
This photo shows an artery and a vein. Which is which?
A is ____Vein__________________________
B is _____Artery_________________________
Provide one reason for your answer (Avoid the use of plain English in your
answers. Made use of appropriate scientific terminologies in your answers.)
B is an artery and therefore has a narrow lumen as compared to A which is a vein and
has a wide lumen
14
This photo shows an artery and a vein. Which is which?
A is ____Vein__________________________
B is _____Artery_________________________
Provide one reason for your answer (Avoid the use of plain English in your
answers. Made use of appropriate scientific terminologies in your answers.)
B is an artery and therefore has a narrow lumen as compared to A which is a vein and
has a wide lumen
14

Describe two other differences between arteries and veins using a table. (Avoid
the use of plain English in your answers. Made use of appropriate scientific
terminologies in your answers.)
Arteries Veins
A thick layer of muscles and elastic
fibers
A thin layer of muscles and elastic fibers
Lack semi lunar valves Have semi lunar valves
Capillaries are microscopic channels that supply blood to the tissues in a
process known as perfusion. It is through capillaries that exchange of gases and other
substances occurs between the blood and the surrounding cells and tissue fluid. The
average diameter of a capillary’s lumen is between 5-10 micrometers. (Nicholls,
2017).
For capillaries to function properly, their walls have to be permeable to allow
substances to pass through. There are three types of capillaries, depending on their
leakiness:
Figure 2:capillaries, www.library.open.oregonstate.edu
15
the use of plain English in your answers. Made use of appropriate scientific
terminologies in your answers.)
Arteries Veins
A thick layer of muscles and elastic
fibers
A thin layer of muscles and elastic fibers
Lack semi lunar valves Have semi lunar valves
Capillaries are microscopic channels that supply blood to the tissues in a
process known as perfusion. It is through capillaries that exchange of gases and other
substances occurs between the blood and the surrounding cells and tissue fluid. The
average diameter of a capillary’s lumen is between 5-10 micrometers. (Nicholls,
2017).
For capillaries to function properly, their walls have to be permeable to allow
substances to pass through. There are three types of capillaries, depending on their
leakiness:
Figure 2:capillaries, www.library.open.oregonstate.edu
15

1. Continuous: they are characterized by complete endothelial linings with tight
junctions between the cells. The junctions are incomplete to allow water, tiny
molecules between the plasma and fluid to pass through clefts.
2. Fenestrated: these capillaries have pores in along with the tight junctions in the
endothelial lining. They are permeable to larger molecules. The number of pores and
the extent of permeability vary according to a location in the body. They are common
in the ileum as well as the kidney. They are also present in the brain’s choroid plexus
and many endocrine structures like the hypothalamus and pituitary glands.
3. Sinusoid: they are flattened with extensive intercellular gaps and incomplete
basement membranes along with clefts and fenestrations. Their large openings are
efficient for the passage of the relatively larger molecules, plasma proteins, and cells.
Blood flow in these capillaries is slow to maximize the time for exchange of
substances. They are mostly found in the liver, spleen, bone marrow and lymph
nodes.
Task 4
16
junctions between the cells. The junctions are incomplete to allow water, tiny
molecules between the plasma and fluid to pass through clefts.
2. Fenestrated: these capillaries have pores in along with the tight junctions in the
endothelial lining. They are permeable to larger molecules. The number of pores and
the extent of permeability vary according to a location in the body. They are common
in the ileum as well as the kidney. They are also present in the brain’s choroid plexus
and many endocrine structures like the hypothalamus and pituitary glands.
3. Sinusoid: they are flattened with extensive intercellular gaps and incomplete
basement membranes along with clefts and fenestrations. Their large openings are
efficient for the passage of the relatively larger molecules, plasma proteins, and cells.
Blood flow in these capillaries is slow to maximize the time for exchange of
substances. They are mostly found in the liver, spleen, bone marrow and lymph
nodes.
Task 4
16
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

X
a) Place arrows on the diagram to indicate the direction of flow of blood.
b) On the diagram, label:
Bicuspid valve
Right atrium
Aortic valve
Pulmonary artery
Superior Vena cava
The cardiac muscles of the heart can co tract very quickly in a wave-like pattern due
to the passage of signals from cell to cell. The cardiac muscle tissue can set its
contraction rhythm due to the presence of the pacemaker cells that stimulate other
cardiac cells.
17
a) Place arrows on the diagram to indicate the direction of flow of blood.
b) On the diagram, label:
Bicuspid valve
Right atrium
Aortic valve
Pulmonary artery
Superior Vena cava
The cardiac muscles of the heart can co tract very quickly in a wave-like pattern due
to the passage of signals from cell to cell. The cardiac muscle tissue can set its
contraction rhythm due to the presence of the pacemaker cells that stimulate other
cardiac cells.
17

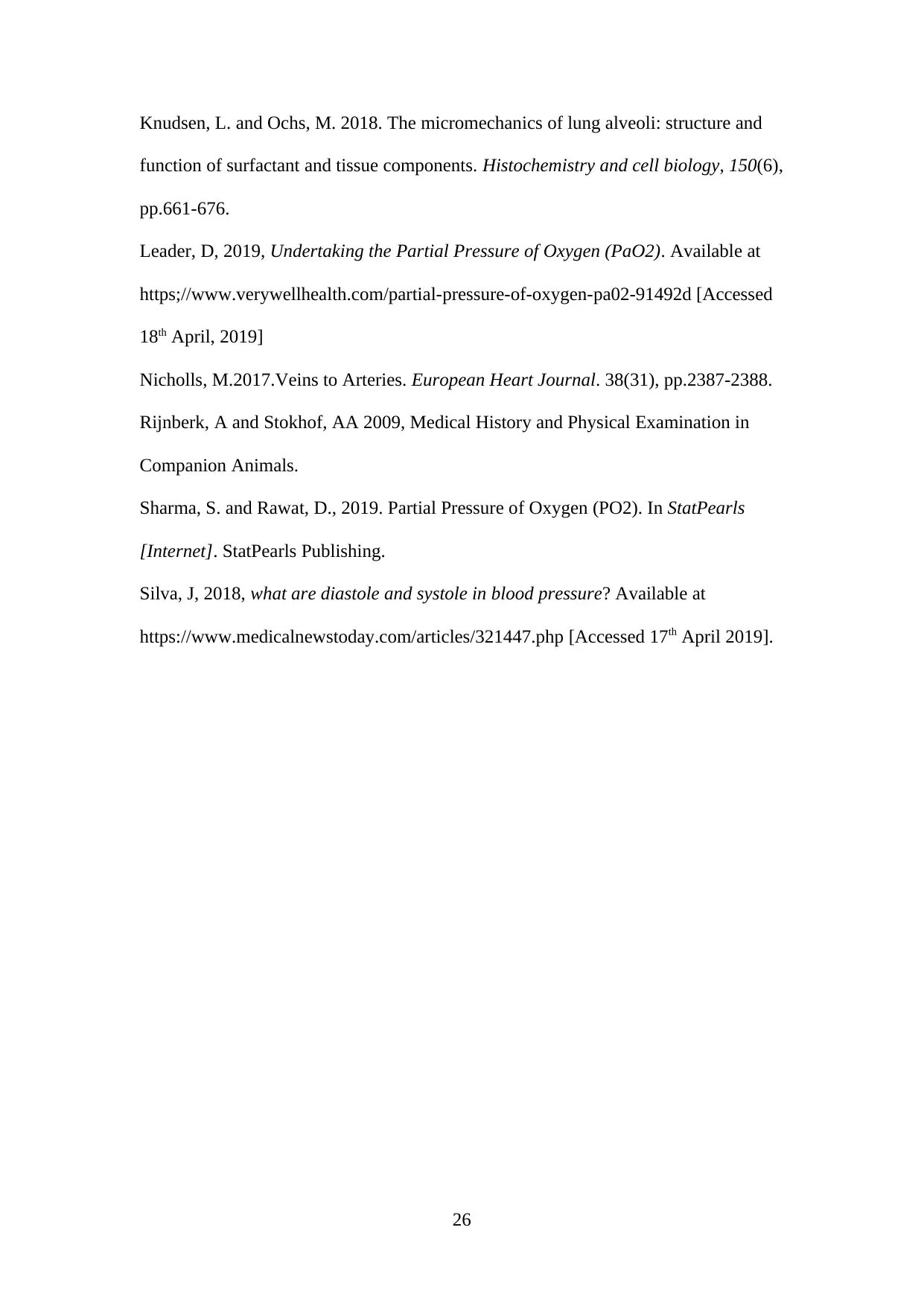
C)
Figure 3: Systole and Diastole Movements, Klabunde, RE, Cardiovascular Physiology
Concepts
A single cardiac activity comprises of two phases, systole, and diastole
During Diastole the ventricles are relaxed, and there is substantial blood flow from the
left and right atria into the left and right ventricles respectively. The blood flows
through the atrioventricular valves (tricuspid valve and mitral valve) which separate
the atria from the ventricles. The right atrium receives deoxygenated blood from the
Vena Cava whereas the left atrium receives oxygenated blood from the lungs through
the four Pulmonary Veins. At the end of the diastole, action potential triggers both the
left atrium and right atrium contract, pushing additional amounts of blood into the
respective ventricles (Klabunde, 2011).
18
Figure 3: Systole and Diastole Movements, Klabunde, RE, Cardiovascular Physiology
Concepts
A single cardiac activity comprises of two phases, systole, and diastole
During Diastole the ventricles are relaxed, and there is substantial blood flow from the
left and right atria into the left and right ventricles respectively. The blood flows
through the atrioventricular valves (tricuspid valve and mitral valve) which separate
the atria from the ventricles. The right atrium receives deoxygenated blood from the
Vena Cava whereas the left atrium receives oxygenated blood from the lungs through
the four Pulmonary Veins. At the end of the diastole, action potential triggers both the
left atrium and right atrium contract, pushing additional amounts of blood into the
respective ventricles (Klabunde, 2011).
18

Systole is when the left ventricle and right ventricle both contract and eject blood into
the Aorta and Pulmonary Artery respectively. During this time, the aortic and
pulmonic valves open to let blood from the two ventricles through the Aorta and
Pulmonary Artery. During systole, the atrioventricular valves are closed, preventing
any blood from entering the ventricles; however, blood continues to flow into the atria
through the Vena Cava and Pulmonary Veins. (Silva, 2018).
Task 5
19
the Aorta and Pulmonary Artery respectively. During this time, the aortic and
pulmonic valves open to let blood from the two ventricles through the Aorta and
Pulmonary Artery. During systole, the atrioventricular valves are closed, preventing
any blood from entering the ventricles; however, blood continues to flow into the atria
through the Vena Cava and Pulmonary Veins. (Silva, 2018).
Task 5
19
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

The heartbeat is triggered by special electrical impulses that travel through a specific
pathway in your heart. The pathway is made up of:
1. SA Node (Sinoatrial node): it is also called the heart’s pacemaker. The impulse for a
heartbeat originates in a small cluster of specialized cells called the SA Node, located
in the right atrium. The impulse spreads throughout the atrial walls bringing about
contraction and thereby forcing blood into the ventricles.it is the SA Node that sets
the rate and rhythm for the heartbeat.
2. AV Node (atrioventricular node): this is a group of cells located in the heart’s
center, between the atria and ventricles. It functions like a blockade that slows down
an electrical impulse before it reaches the ventricles. This delay provides time for the
atria to perform its function before the ventricles.
3. His-Purkinje Network: this is the pathway made up of specialized fibers that
transmit the impulses to the muscular ventricular walls causing them to contract. This
contraction forces the blood in the ventricles out of the heart into the lungs and the
rest of the body. (Cleveland Clinic, 2019)
20
pathway in your heart. The pathway is made up of:
1. SA Node (Sinoatrial node): it is also called the heart’s pacemaker. The impulse for a
heartbeat originates in a small cluster of specialized cells called the SA Node, located
in the right atrium. The impulse spreads throughout the atrial walls bringing about
contraction and thereby forcing blood into the ventricles.it is the SA Node that sets
the rate and rhythm for the heartbeat.
2. AV Node (atrioventricular node): this is a group of cells located in the heart’s
center, between the atria and ventricles. It functions like a blockade that slows down
an electrical impulse before it reaches the ventricles. This delay provides time for the
atria to perform its function before the ventricles.
3. His-Purkinje Network: this is the pathway made up of specialized fibers that
transmit the impulses to the muscular ventricular walls causing them to contract. This
contraction forces the blood in the ventricles out of the heart into the lungs and the
rest of the body. (Cleveland Clinic, 2019)
20

Task 6
a) CO=HR × SV
CO= 70×0.08
CO=5.6l/min
= 5.6l/min
During exercise, the cardiac output of the person is expected to increase.
Furthermore, the heart rate will increase to supply sufficient blood to the working
muscles, the blood which contains enough oxygen and nutrients. This increased heart
rate also increases the rate at which waste products are removed. The heart rate will
increase proportionally with the workload until heart rates close to maximal are
reached (Evans, DL, 1985)
Cardiac output increases during exercise more than the total resistance decreases and
as a result, the average arterial pressure increases by a small amount. In contrast,
pulse pressure increases significantly because of an increase in both stroke volume
and the speed of ejection of the stroke volume. The effect of a great increase in heart
rate and a small increase in stroke volume is a drastic rise in the cardiac output.
21
a) CO=HR × SV
CO= 70×0.08
CO=5.6l/min
= 5.6l/min
During exercise, the cardiac output of the person is expected to increase.
Furthermore, the heart rate will increase to supply sufficient blood to the working
muscles, the blood which contains enough oxygen and nutrients. This increased heart
rate also increases the rate at which waste products are removed. The heart rate will
increase proportionally with the workload until heart rates close to maximal are
reached (Evans, DL, 1985)
Cardiac output increases during exercise more than the total resistance decreases and
as a result, the average arterial pressure increases by a small amount. In contrast,
pulse pressure increases significantly because of an increase in both stroke volume
and the speed of ejection of the stroke volume. The effect of a great increase in heart
rate and a small increase in stroke volume is a drastic rise in the cardiac output.
21
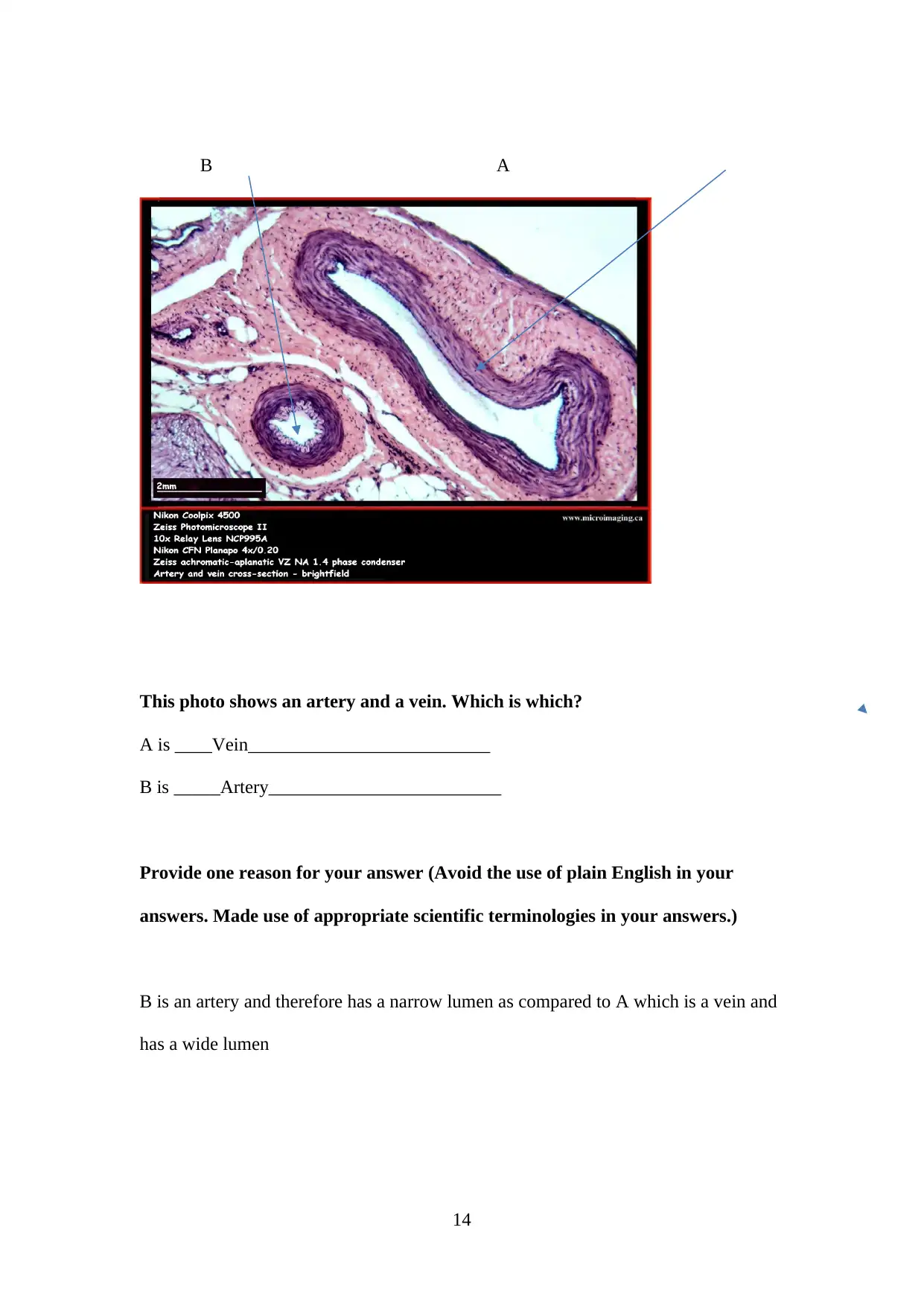
Figure 4: Graph of heart rate and stroke volume during exercise, The McGill
Physiology Virtual Lab
The heart rate increases because of a drop in parasympathetic activity of the
SA Node alongside a marked increase in sympathetic activity.
The stroke volume, on the other hand, increases due to increases in ventricular
contractility which is noticeable through an increased ejection fraction and mediated
by sympathetic nerves of the ventricular myocardium.
Maintaining cardiac output is important because it enables the body to maintain the
blood pressure at sustainable levels to supply oxygenated blood and nutrients to the
brain and other vital organs. (Klabunde, 2011)
22
Physiology Virtual Lab
The heart rate increases because of a drop in parasympathetic activity of the
SA Node alongside a marked increase in sympathetic activity.
The stroke volume, on the other hand, increases due to increases in ventricular
contractility which is noticeable through an increased ejection fraction and mediated
by sympathetic nerves of the ventricular myocardium.
Maintaining cardiac output is important because it enables the body to maintain the
blood pressure at sustainable levels to supply oxygenated blood and nutrients to the
brain and other vital organs. (Klabunde, 2011)
22
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

Figure 5:
distribution of
the systemic
cardiac
output at rest
and during
strenuous exercise, The McGill Physiology Virtual Lab
Task 7
Acetylcholine, however, is not a hormone but a neurotransmitter. Acetylcholine is a
chemical messenger. It is released from the synaptic knob of a presynaptic neuron and
then travels across a synapse and binds to a receptor. Acetylcholine, when it fails to
bind with acetylcholinesterase or a receptor, may travel a significant distance through
the cerebrospinal fluid while searching for a receptor. In this case, it would be acting
as a neuromodulator, but it should not be considered a hormone (Bennett et al. 2019).
23
distribution of
the systemic
cardiac
output at rest
and during
strenuous exercise, The McGill Physiology Virtual Lab
Task 7
Acetylcholine, however, is not a hormone but a neurotransmitter. Acetylcholine is a
chemical messenger. It is released from the synaptic knob of a presynaptic neuron and
then travels across a synapse and binds to a receptor. Acetylcholine, when it fails to
bind with acetylcholinesterase or a receptor, may travel a significant distance through
the cerebrospinal fluid while searching for a receptor. In this case, it would be acting
as a neuromodulator, but it should not be considered a hormone (Bennett et al. 2019).
23

24

References
Arthurs, GJ and Sudhakar, M, 2005, ‘Carbon Dioxide Transport’. Continuing
Education in Anaesthesia Critical Care and Pain, 5(6), pp.207-210.
Barclay, T. 2017. Trachea (Windpipe). Available at
https;//www.innerbody.com/image_cardo6/card13.html [Accessed 18th April 2019]
Bennet et al, .2019.Acetylcholine inhibits platelet activation. Journal of
Pharmacology and Experimental Therapeutics, 369(2), pp.34-70.
Biga et al., 2019. Anatomy and Physiology. Open Oregon State: Oregon State
University.
Boulos, SN and Schmidt, GA, 2017. ‘Estimating Arterial Partial Pressure of Carbon
Dioxide in Ventilated Patients: How Valid Are Surrogate Measures?’, Annals of the
American Society,13(5),pp.134-150.
Cleveland Clinic, 2019. Heartbeat. Available at
https://my.clevelandclinic.org/health/articles/17064-heart-beat.[Accessed 16th April
2019].
Eldridge, L. 2018. Functions and Disorders of the Alveoli. Available at
https://www.verywellhealth.com/what -are-alveoli-2249043. [Accessed 18th April,
2019]
Hecht, M, 2018. The Alveoli in Your Lungs. Available at
https://www.healthline.com/health/alveoli-function [Accessed 17th April 2019]
Klabunde, R., 2011. Cardiovascular physiology concepts. Lippincott Williams &
Wilkins.
25
Arthurs, GJ and Sudhakar, M, 2005, ‘Carbon Dioxide Transport’. Continuing
Education in Anaesthesia Critical Care and Pain, 5(6), pp.207-210.
Barclay, T. 2017. Trachea (Windpipe). Available at
https;//www.innerbody.com/image_cardo6/card13.html [Accessed 18th April 2019]
Bennet et al, .2019.Acetylcholine inhibits platelet activation. Journal of
Pharmacology and Experimental Therapeutics, 369(2), pp.34-70.
Biga et al., 2019. Anatomy and Physiology. Open Oregon State: Oregon State
University.
Boulos, SN and Schmidt, GA, 2017. ‘Estimating Arterial Partial Pressure of Carbon
Dioxide in Ventilated Patients: How Valid Are Surrogate Measures?’, Annals of the
American Society,13(5),pp.134-150.
Cleveland Clinic, 2019. Heartbeat. Available at
https://my.clevelandclinic.org/health/articles/17064-heart-beat.[Accessed 16th April
2019].
Eldridge, L. 2018. Functions and Disorders of the Alveoli. Available at
https://www.verywellhealth.com/what -are-alveoli-2249043. [Accessed 18th April,
2019]
Hecht, M, 2018. The Alveoli in Your Lungs. Available at
https://www.healthline.com/health/alveoli-function [Accessed 17th April 2019]
Klabunde, R., 2011. Cardiovascular physiology concepts. Lippincott Williams &
Wilkins.
25
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Knudsen, L. and Ochs, M. 2018. The micromechanics of lung alveoli: structure and
function of surfactant and tissue components. Histochemistry and cell biology, 150(6),
pp.661-676.
Leader, D, 2019, Undertaking the Partial Pressure of Oxygen (PaO2). Available at
https;//www.verywellhealth.com/partial-pressure-of-oxygen-pa02-91492d [Accessed
18th April, 2019]
Nicholls, M.2017.Veins to Arteries. European Heart Journal. 38(31), pp.2387-2388.
Rijnberk, A and Stokhof, AA 2009, Medical History and Physical Examination in
Companion Animals.
Sharma, S. and Rawat, D., 2019. Partial Pressure of Oxygen (PO2). In StatPearls
[Internet]. StatPearls Publishing.
Silva, J, 2018, what are diastole and systole in blood pressure? Available at
https://www.medicalnewstoday.com/articles/321447.php [Accessed 17th April 2019].
26
function of surfactant and tissue components. Histochemistry and cell biology, 150(6),
pp.661-676.
Leader, D, 2019, Undertaking the Partial Pressure of Oxygen (PaO2). Available at
https;//www.verywellhealth.com/partial-pressure-of-oxygen-pa02-91492d [Accessed
18th April, 2019]
Nicholls, M.2017.Veins to Arteries. European Heart Journal. 38(31), pp.2387-2388.
Rijnberk, A and Stokhof, AA 2009, Medical History and Physical Examination in
Companion Animals.
Sharma, S. and Rawat, D., 2019. Partial Pressure of Oxygen (PO2). In StatPearls
[Internet]. StatPearls Publishing.
Silva, J, 2018, what are diastole and systole in blood pressure? Available at
https://www.medicalnewstoday.com/articles/321447.php [Accessed 17th April 2019].
26
1 out of 26
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





