Capstone Project: Surgical Site Infection Identification in Healthcare
VerifiedAdded on 2023/04/06
|20
|2269
|165
Project
AI Summary
This capstone project addresses the critical issue of Surgical Site Infections (SSIs) in healthcare settings. The project begins with a background on SSIs, emphasizing their impact on patient outcomes and healthcare costs, and presents a problem statement focused on reducing SSI rates before and after clinical operations. The purpose of the change proposal is to investigate the effectiveness of preoperative bathing with antiseptic soaps. A PICOT question is formulated to guide the research, comparing chlorhexidine baths to regular soap and water. The project employs an annotated bibliography to evaluate eight relevant articles, analyzing research questions, methods, and findings. It also discusses applicable change theories and proposes an implementation plan, including outcome measures and potential barriers. Recommendations for overcoming these barriers and evidence of revision are provided, with a focus on promoting evidence-based approaches to SSI prevention, such as the use of chlorhexidine soaps.
Running Head: Identification of Surgical Site Infection in Healthcare Settings
IDENTIFICATION OF SURGICAL SITE INFECTION IN
HEALTHCARE SETTINGS
IDENTIFICATION OF SURGICAL SITE INFECTION IN
HEALTHCARE SETTINGS
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2Identification of Surgical Site Infection in Healthcare Settings
Background
In the modern healthcare setting, the phrase ‘Surgical Site Infection’ covers a vast area of
consideration. According to the statement of clinical experts, Surgical Site Infection or SSI is one
of the most common issues in the clinical surgery process. It is considered as it retains a direct
connection with the financial burden, service quality reduction, and patient mortality. As per the
report of Webster & Osborne (2015), SSI generally occurs in the areas where the surgeries have
taken place. Unfortunately, the occurrence of SSI in modern healthcare settings is still prevalent.
Therefore, it can be assumed that the interventional requirement for SSI prevention is higher in
modern healthcare settings. Based on such a situation, the assignment is done for addressing the
effects of SSI on patients’ and service providers’ health, for developing some strategic plans to
prevent or reduce the surgical site infection.
Problem statement
The main problem statement, based on which the research study conducted, is to lower
the number of surgical site infection before and after the clinical operations. It is evident that
patients or care providers often use plain soaps for showering, bathing, or washing body parts,
after the surgical process. Now, the main question is to investigate the differences in antiseptic
soaps and plain soaps and their roles in preventing surgical site infection as well.
Purpose of the change proposal
The study aims to investigate the effectiveness of preoperative bathing along with
antiseptic soaps, which is one of the most common pathways of SSI prevention. Apart from this,
the differentiated impacts of antiseptic soaps and plain soaps on the areas of surgical site
infection are also a central part of the change proposal. In order to highlight the consequences
and to identify the possible changes, the researcher(s) has structured the following PICOT
question for specification of the issue.
Background
In the modern healthcare setting, the phrase ‘Surgical Site Infection’ covers a vast area of
consideration. According to the statement of clinical experts, Surgical Site Infection or SSI is one
of the most common issues in the clinical surgery process. It is considered as it retains a direct
connection with the financial burden, service quality reduction, and patient mortality. As per the
report of Webster & Osborne (2015), SSI generally occurs in the areas where the surgeries have
taken place. Unfortunately, the occurrence of SSI in modern healthcare settings is still prevalent.
Therefore, it can be assumed that the interventional requirement for SSI prevention is higher in
modern healthcare settings. Based on such a situation, the assignment is done for addressing the
effects of SSI on patients’ and service providers’ health, for developing some strategic plans to
prevent or reduce the surgical site infection.
Problem statement
The main problem statement, based on which the research study conducted, is to lower
the number of surgical site infection before and after the clinical operations. It is evident that
patients or care providers often use plain soaps for showering, bathing, or washing body parts,
after the surgical process. Now, the main question is to investigate the differences in antiseptic
soaps and plain soaps and their roles in preventing surgical site infection as well.
Purpose of the change proposal
The study aims to investigate the effectiveness of preoperative bathing along with
antiseptic soaps, which is one of the most common pathways of SSI prevention. Apart from this,
the differentiated impacts of antiseptic soaps and plain soaps on the areas of surgical site
infection are also a central part of the change proposal. In order to highlight the consequences
and to identify the possible changes, the researcher(s) has structured the following PICOT
question for specification of the issue.
3Identification of Surgical Site Infection in Healthcare Settings
PICOT
In preoperative patients (P), how effective are chlorhexidine baths (I) compared to
regular soap and water baths (C), in controlling the number of surgical site infections (O)
during the preoperative and recovery period after surgery (T)?
Literature search strategy employed
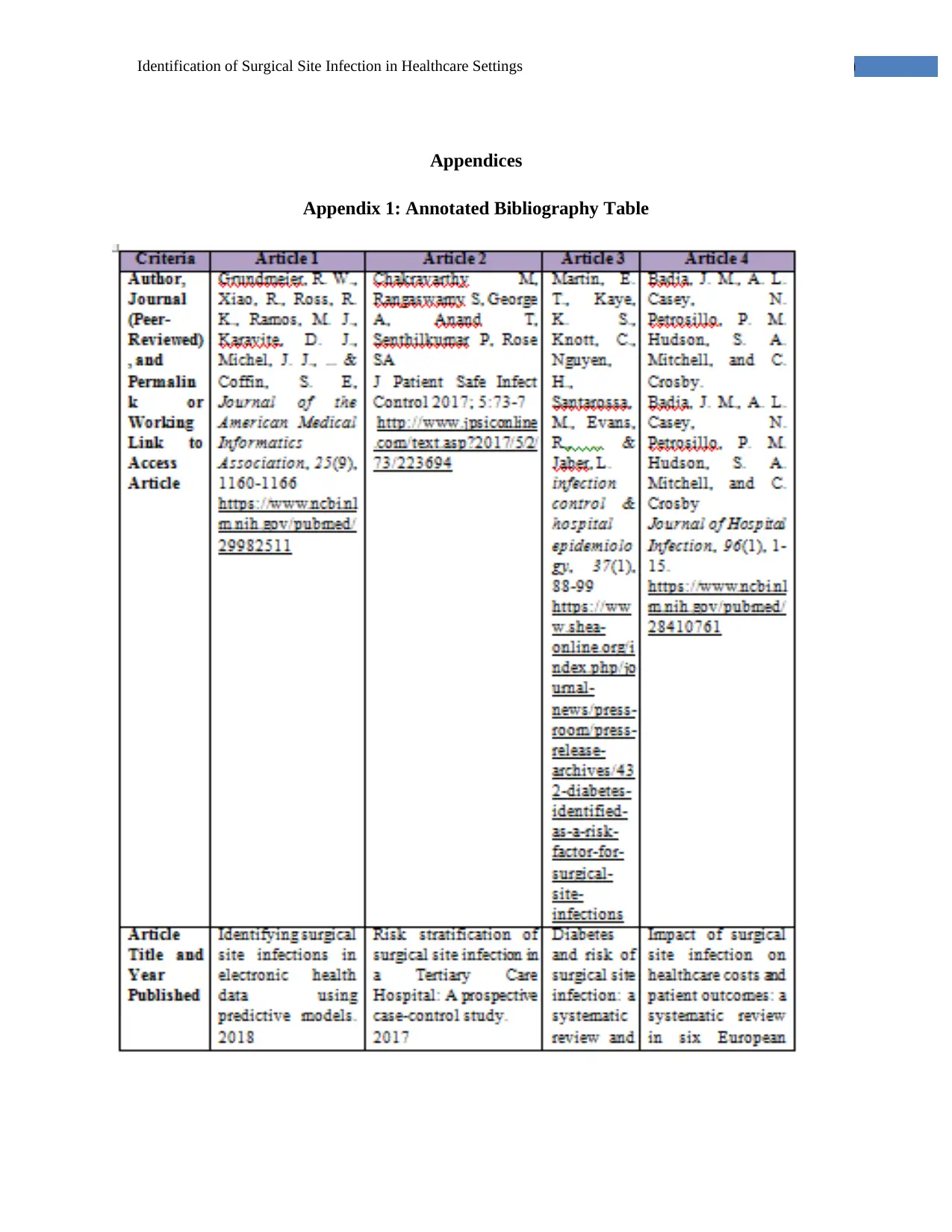
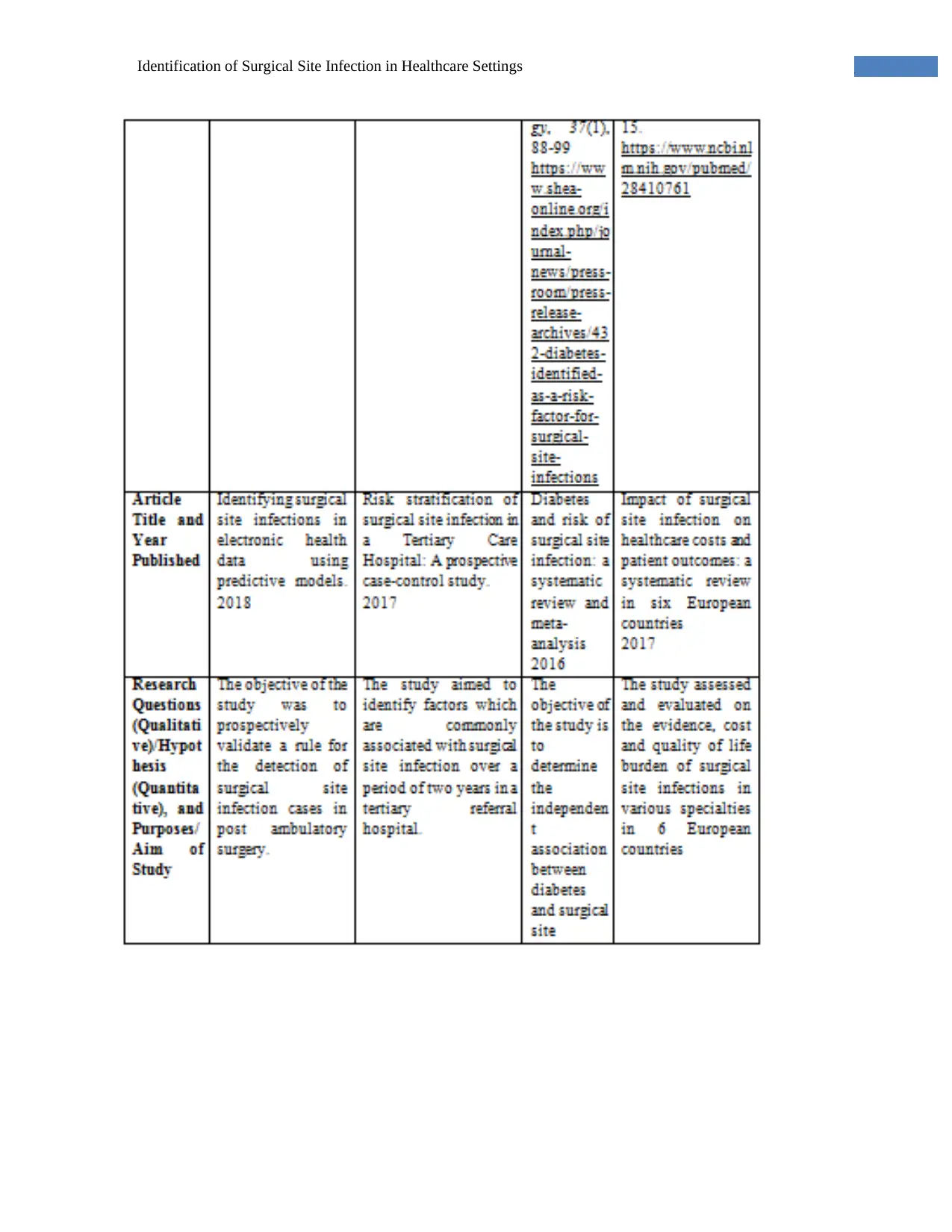
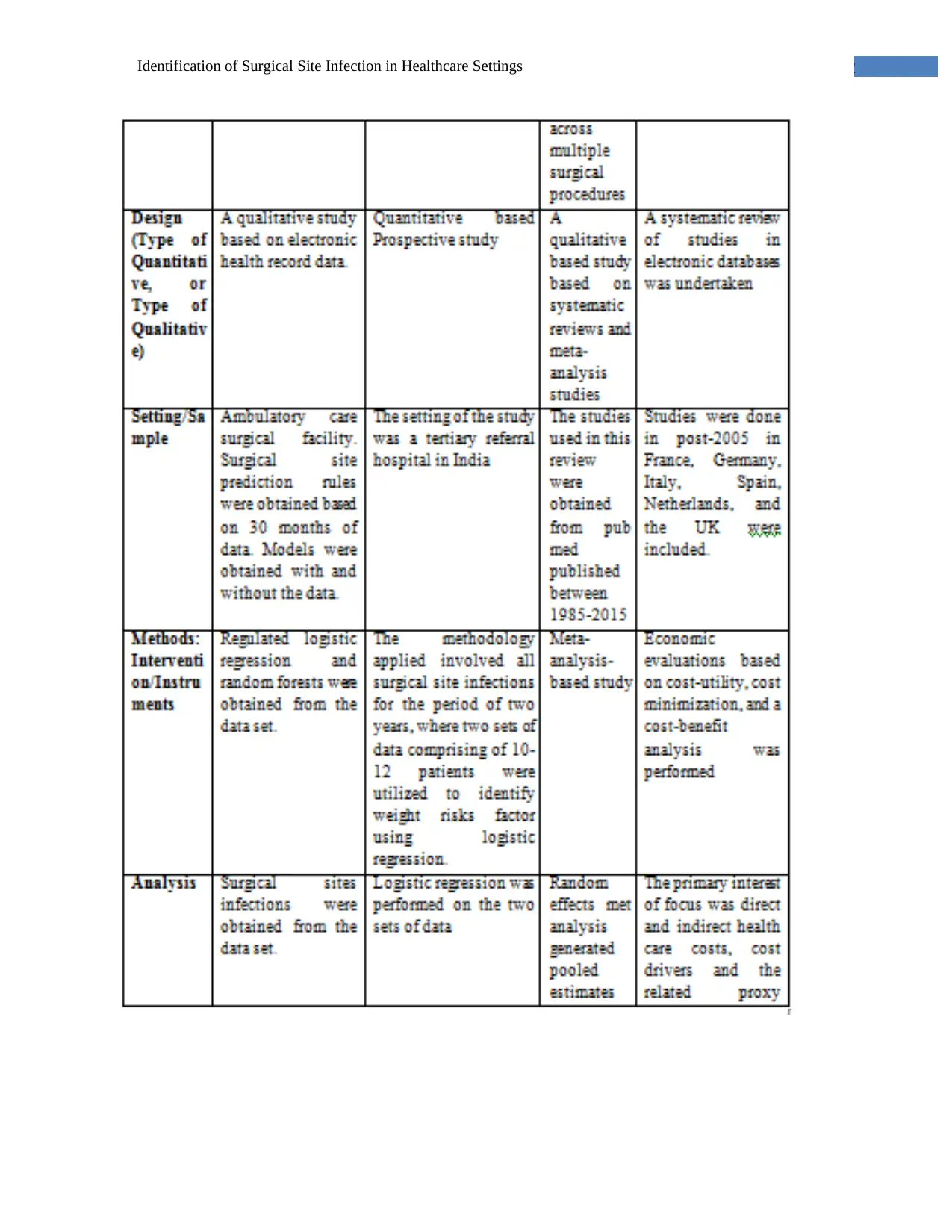
In order to evaluate the literature investigated on the topic of SSI in current healthcare
settings, the researcher(s) has applied an annotated bibliography structure. The literature
searched by the researcher(s) has been obtained from different online databases. Based on some
inclusion and exclusion criteria, the researcher(s) has chosen total eight articles, which are
relevant with the selected topic, and include specific research paper structure, e.g. research
questions, research methods, design, samples, interventions, analysis, key findings, and
recommendation parts. The brief table of the annotated bibliography is attached in the Appendix
section.
Evaluation of the literature
The chosen eight articles provide critical or argumentative supports to the developed
PICOT question from different viewpoints. Such as the study conducted by Grundmeier, Xiao,
Ross, Ramos, Karavite, Michel, and Coffin (2018), to identify the presence of SSI, clinicians
could apply EHR technology, as it is efficient in detecting ambulatory surgical infection. A study
conducted by Chakravarthy, Rangaswamy, George, Anand, Senthilkumar & Rose (2017)
includes research questions represents the process of SSI factor determination, which supports
the developed PICOT statement, as based on the identified factors, researcher(s) could create SSI
prevention strategies.
The researcher(s) has also performed comparison and evaluation of the sample
population, research limitation, conclusion, and recommendation parts along with research
questions. For example, Martin, Kaye, Knott, Nguyen, Santarossa, Evans, Elizabeth, and Jaber
(2015) included total 94 peer-reviewed journals whereas Kunutsor, Whitehouse, Blom, and
Beswick (2017) included total nine peer-reviewed journals as the sample population for this
research paper. However, the articles also retain certain types of limitations, such as Badia,
Casey, Petrosillo, Hudson, Mitchell & Crosby (2017) used samples from six countries, which is
PICOT
In preoperative patients (P), how effective are chlorhexidine baths (I) compared to
regular soap and water baths (C), in controlling the number of surgical site infections (O)
during the preoperative and recovery period after surgery (T)?
Literature search strategy employed
In order to evaluate the literature investigated on the topic of SSI in current healthcare
settings, the researcher(s) has applied an annotated bibliography structure. The literature
searched by the researcher(s) has been obtained from different online databases. Based on some
inclusion and exclusion criteria, the researcher(s) has chosen total eight articles, which are
relevant with the selected topic, and include specific research paper structure, e.g. research
questions, research methods, design, samples, interventions, analysis, key findings, and
recommendation parts. The brief table of the annotated bibliography is attached in the Appendix
section.
Evaluation of the literature
The chosen eight articles provide critical or argumentative supports to the developed
PICOT question from different viewpoints. Such as the study conducted by Grundmeier, Xiao,
Ross, Ramos, Karavite, Michel, and Coffin (2018), to identify the presence of SSI, clinicians
could apply EHR technology, as it is efficient in detecting ambulatory surgical infection. A study
conducted by Chakravarthy, Rangaswamy, George, Anand, Senthilkumar & Rose (2017)
includes research questions represents the process of SSI factor determination, which supports
the developed PICOT statement, as based on the identified factors, researcher(s) could create SSI
prevention strategies.
The researcher(s) has also performed comparison and evaluation of the sample
population, research limitation, conclusion, and recommendation parts along with research
questions. For example, Martin, Kaye, Knott, Nguyen, Santarossa, Evans, Elizabeth, and Jaber
(2015) included total 94 peer-reviewed journals whereas Kunutsor, Whitehouse, Blom, and
Beswick (2017) included total nine peer-reviewed journals as the sample population for this
research paper. However, the articles also retain certain types of limitations, such as Badia,
Casey, Petrosillo, Hudson, Mitchell & Crosby (2017) used samples from six countries, which is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4Identification of Surgical Site Infection in Healthcare Settings
comparatively larger for the capstone research project. At the last part, all the studies reflect a
number of solutions regarding the reduction of SSI in modern healthcare organisations.
Applicable change or nursing theory utilise
The chosen journals or articles provide evidence for understanding the process by which
clinical experts could change the occurrence of SSI in healthcare settings. As mentioned in the
earlier part, Grundmeier, Xiao, Ross, Ramos, Karavite, Michel, and Coffin (2018) mentioned
about the EHR technology implementation, which is efficient in case of evaluating the number of
SSI in a specific surgical unit. Mueck & Kao (2017) reflects that nurses could integrate the SSI
assessment protocol for identifying the post-discharge risks associated with post-surgical
patients. Chakravarthy, Rangaswamy, George, Anand, Senthilkumar & Rose (2017) mentioned
that nurses and other caregivers could develop SSI prevention plans based on some internal and
external factors, such as Body Mass Index, Antiseptic shower, and so on.
According to the statement of Allegranzi, Bischoff & de Jonge (2016), the most basic
evidence-based solution of this SSI is the application of CHG or Chlorhexidine Gluconate, which
is one of the traditional and significant antiseptic components. The safe agent acts against a range
of microorganisms, including gram-positive, non-spore-forming, and gram-negative yeast,
bacteria, and viruses. However, based on the sensitivity of human skin, clinicians suggest
application of CHG by 2-3 times separated applications. The first one would be done a night
before surgery, the second would be in the morning, and the final one would be just before going
to the operation room.
Therefore, through summarising the evidence gathered from the chosen articles and other
resources, the changes required for preventing SSI are as follows-
Application of Prophylactic Antibiotics through an appropriate manner
Avoiding functioning on the operative sites or the sensitive post-operative sites
Implementation of fundamental prevention strategies developed by CDC, such as
preventing consumption of tobacco, applying sterile antiseptic materials, showering by
CHG or other antiseptic soaps, using Personal Protective Equipment, and so on (Changes
to Prevent Surgical Site Infection, 2018)
comparatively larger for the capstone research project. At the last part, all the studies reflect a
number of solutions regarding the reduction of SSI in modern healthcare organisations.
Applicable change or nursing theory utilise
The chosen journals or articles provide evidence for understanding the process by which
clinical experts could change the occurrence of SSI in healthcare settings. As mentioned in the
earlier part, Grundmeier, Xiao, Ross, Ramos, Karavite, Michel, and Coffin (2018) mentioned
about the EHR technology implementation, which is efficient in case of evaluating the number of
SSI in a specific surgical unit. Mueck & Kao (2017) reflects that nurses could integrate the SSI
assessment protocol for identifying the post-discharge risks associated with post-surgical
patients. Chakravarthy, Rangaswamy, George, Anand, Senthilkumar & Rose (2017) mentioned
that nurses and other caregivers could develop SSI prevention plans based on some internal and
external factors, such as Body Mass Index, Antiseptic shower, and so on.
According to the statement of Allegranzi, Bischoff & de Jonge (2016), the most basic
evidence-based solution of this SSI is the application of CHG or Chlorhexidine Gluconate, which
is one of the traditional and significant antiseptic components. The safe agent acts against a range
of microorganisms, including gram-positive, non-spore-forming, and gram-negative yeast,
bacteria, and viruses. However, based on the sensitivity of human skin, clinicians suggest
application of CHG by 2-3 times separated applications. The first one would be done a night
before surgery, the second would be in the morning, and the final one would be just before going
to the operation room.
Therefore, through summarising the evidence gathered from the chosen articles and other
resources, the changes required for preventing SSI are as follows-
Application of Prophylactic Antibiotics through an appropriate manner
Avoiding functioning on the operative sites or the sensitive post-operative sites
Implementation of fundamental prevention strategies developed by CDC, such as
preventing consumption of tobacco, applying sterile antiseptic materials, showering by
CHG or other antiseptic soaps, using Personal Protective Equipment, and so on (Changes
to Prevent Surgical Site Infection, 2018)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5Identification of Surgical Site Infection in Healthcare Settings
Proposed implementation plan with outcome measures
Nurses would use their intervention plans for supporting patients during the application
of CHG antiseptic soaps. The first step of applying this soap is to assess the sensitivity of
patients’ skin to CHG. During the assessment, nurses would also provide suggestions about the
process of soap application in the pre-operative areas and the number of application required
before surgery. On the other hand, Kang, Holekamp, Wagner & Lehman (2015) stated that it is
also necessary to evaluate the skin hypersensitivity standards, for avoiding any other skin
complications. Nurses would also provide attention on the time of baths taken by the patients, the
time of bathing completion, and the presence of any irritation or sensitivity standards.
The implication of SSI prevention techniques is required to prioritise during the post-
operative wound-care management system. Nurses and other caregivers need to provide attention
to the PACU or Post Anaesthesia Care Unit, for checking the dressing materials. Apart from this,
maintenance of hand hygiene standards would be a prominent part of SSI prevention, along with
stronger asepsis protocols. As stated by Leaper & Ousey (2015), nurses would focus on
delivering all the relevant and required information to the patients about the post-operative
system and SSI consequences, along with specifying the practical process of eliminating the
possibilities of surgical hazards. Application of 2-4% of the CHG soaps is determined as safe and
effective for the prevention of surgical site infection.
Identification of potential barriers to planning implementation and recommendation for
overcoming
Although, prevention of SSI is essential in the current clinical settings, however,
clinicians often explore different internal or external barriers while implementing the prevention
plans in the existing operational environments. For example, nurses often face obstacles in
applying SSI prevention tools and techniques as they have insufficient knowledge about the
topic. On the other hand, patients often could not receive proper information from the clinical
experts; therefore, they feel afraid of using such antiseptic soaps and other elements. For
overcoming these barriers, Chen, Song, Chen, Lin & Zhang (2016) suggested that
implementation of SSI prevention techniques in the training and education programs would be
helpful for the healthcare providers. They would understand the significance of SSI prevention
techniques, tools, and processes, and deliver proficient information to the patients. This would
Proposed implementation plan with outcome measures
Nurses would use their intervention plans for supporting patients during the application
of CHG antiseptic soaps. The first step of applying this soap is to assess the sensitivity of
patients’ skin to CHG. During the assessment, nurses would also provide suggestions about the
process of soap application in the pre-operative areas and the number of application required
before surgery. On the other hand, Kang, Holekamp, Wagner & Lehman (2015) stated that it is
also necessary to evaluate the skin hypersensitivity standards, for avoiding any other skin
complications. Nurses would also provide attention on the time of baths taken by the patients, the
time of bathing completion, and the presence of any irritation or sensitivity standards.
The implication of SSI prevention techniques is required to prioritise during the post-
operative wound-care management system. Nurses and other caregivers need to provide attention
to the PACU or Post Anaesthesia Care Unit, for checking the dressing materials. Apart from this,
maintenance of hand hygiene standards would be a prominent part of SSI prevention, along with
stronger asepsis protocols. As stated by Leaper & Ousey (2015), nurses would focus on
delivering all the relevant and required information to the patients about the post-operative
system and SSI consequences, along with specifying the practical process of eliminating the
possibilities of surgical hazards. Application of 2-4% of the CHG soaps is determined as safe and
effective for the prevention of surgical site infection.
Identification of potential barriers to planning implementation and recommendation for
overcoming
Although, prevention of SSI is essential in the current clinical settings, however,
clinicians often explore different internal or external barriers while implementing the prevention
plans in the existing operational environments. For example, nurses often face obstacles in
applying SSI prevention tools and techniques as they have insufficient knowledge about the
topic. On the other hand, patients often could not receive proper information from the clinical
experts; therefore, they feel afraid of using such antiseptic soaps and other elements. For
overcoming these barriers, Chen, Song, Chen, Lin & Zhang (2016) suggested that
implementation of SSI prevention techniques in the training and education programs would be
helpful for the healthcare providers. They would understand the significance of SSI prevention
techniques, tools, and processes, and deliver proficient information to the patients. This would
6Identification of Surgical Site Infection in Healthcare Settings
help in improving the entire public health outcomes by lowering the mortality or morbidity rate
associated with the surgical site infection.
Evidence of Revision
Since the prevalence of SSI is highly expanded in the current healthcare settings,
therefore, evidence for revision can be obtained from different government and institutional
websites. As per the evidence of WHO, for omitting the possibility of SSI from the clinical
settings, all the clinical experts, surgical team members, support staffs, and patients need to play
their distinctive roles and responsibilities during the pre-operative period. In addition, the
cautious steps would also be taken during the intra-operative and postoperative periods for
lowering the possibility of infection recurrence (Preventing Surgical Site Infection, 2018) [Refer
to Appendix].
As mentioned in the earlier portion, clinicians can provide a recommendation about the
using of pre-operative showering along with 4% CHG, which is supported evidence by
(Allegranzi, Bischoff & de Jonge, 2016). On the other hand, Mueck & Kao (2017) commented
that it is necessary to minimise the number of bacteria or other harmful microorganisms over the
skin regions, due to which it is evident that CHG soaps are more useful for the prevention of SSI
from wounded or pre-operative places. According to my job role, I need to focus on promoting
some evidence-based approaches for the patients in order to help them in overcoming the threats
of Surgical Site Infection. Through revising the evidence, nurses or other care providers might
provide advice to the patients for reporting skin integrity, skin breaks, or rashes. Patients would
get instruction about leaving the CHG soap on the per-operative areas before rinsing, as it would
help in the effective prevention of SSI.
help in improving the entire public health outcomes by lowering the mortality or morbidity rate
associated with the surgical site infection.
Evidence of Revision
Since the prevalence of SSI is highly expanded in the current healthcare settings,
therefore, evidence for revision can be obtained from different government and institutional
websites. As per the evidence of WHO, for omitting the possibility of SSI from the clinical
settings, all the clinical experts, surgical team members, support staffs, and patients need to play
their distinctive roles and responsibilities during the pre-operative period. In addition, the
cautious steps would also be taken during the intra-operative and postoperative periods for
lowering the possibility of infection recurrence (Preventing Surgical Site Infection, 2018) [Refer
to Appendix].
As mentioned in the earlier portion, clinicians can provide a recommendation about the
using of pre-operative showering along with 4% CHG, which is supported evidence by
(Allegranzi, Bischoff & de Jonge, 2016). On the other hand, Mueck & Kao (2017) commented
that it is necessary to minimise the number of bacteria or other harmful microorganisms over the
skin regions, due to which it is evident that CHG soaps are more useful for the prevention of SSI
from wounded or pre-operative places. According to my job role, I need to focus on promoting
some evidence-based approaches for the patients in order to help them in overcoming the threats
of Surgical Site Infection. Through revising the evidence, nurses or other care providers might
provide advice to the patients for reporting skin integrity, skin breaks, or rashes. Patients would
get instruction about leaving the CHG soap on the per-operative areas before rinsing, as it would
help in the effective prevention of SSI.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7Identification of Surgical Site Infection in Healthcare Settings
Reference List
Allegranzi, B., Bischoff, P., & de Jonge, S. (2016). Surgical Site Infections 1. New WHO
Recommendations on Preoperative Measures for Surgical Site Infection Prevention: an
Evidence-Based Global Perspective. Lancet Infect Dis, 16(12), e276-87. Retrieved
fromhttps://www.researchgate.net/profile/Bassim_Zayed/publication/
309656390_New_WHO_recommendations_on_preoperative_measures_for_surgical_site
_infection_prevention_an_evidence-based_global_perspective/links/
5b39cddbaca272078501033a/New-WHO-recommendations-on-preoperative-measures-
for-surgical-site-infection-prevention-an-evidence-based-global-perspective.pdf
Badia, J. M., Casey, A. L., Petrosillo, N., Hudson, P. M., Mitchell, S. A., & Crosby, C. (2017).
Impact of surgical site infection on healthcare costs and patient outcomes: a systematic
review in six European countries. Journal of Hospital Infection, 96(1), 1-15. Retrieved
from https://www.sciencedirect.com/science/article/pii/S0195670117301354
Chakravarthy, M., Rangaswamy, S., George, A., Anand, T., Senthilkumar, P., & Rose, S. A.
(2017). Risk stratification of surgical site infection in a Tertiary Care Hospital: A
prospective case-control study. Journal of Patient Safety and Infection Control, 5(2),
73.
Changes to Prevent Surgical Site Infection. (2018). [online]. Retrieved from
http://www.ihi.org/resources/Pages/Changes/ChangestoPreventSurgicalSiteInfection.as
px
Chen, M., Song, X., Chen, L. Z., Lin, Z. D., & Zhang, X. L. (2016). Comparing mechanical
bowel preparation with both oral and systemic antibiotics versus mechanical bowel
preparation and systemic antibiotics alone for the prevention of surgical site infection
after elective colorectal surgery. Diseases of the Colon & Rectum, 59(1), 70-78.
Retrieved
fromhttps://www.ingentaconnect.com/content/wk/dcr/2016/00000059/00000001/
art00016
Reference List
Allegranzi, B., Bischoff, P., & de Jonge, S. (2016). Surgical Site Infections 1. New WHO
Recommendations on Preoperative Measures for Surgical Site Infection Prevention: an
Evidence-Based Global Perspective. Lancet Infect Dis, 16(12), e276-87. Retrieved
fromhttps://www.researchgate.net/profile/Bassim_Zayed/publication/
309656390_New_WHO_recommendations_on_preoperative_measures_for_surgical_site
_infection_prevention_an_evidence-based_global_perspective/links/
5b39cddbaca272078501033a/New-WHO-recommendations-on-preoperative-measures-
for-surgical-site-infection-prevention-an-evidence-based-global-perspective.pdf
Badia, J. M., Casey, A. L., Petrosillo, N., Hudson, P. M., Mitchell, S. A., & Crosby, C. (2017).
Impact of surgical site infection on healthcare costs and patient outcomes: a systematic
review in six European countries. Journal of Hospital Infection, 96(1), 1-15. Retrieved
from https://www.sciencedirect.com/science/article/pii/S0195670117301354
Chakravarthy, M., Rangaswamy, S., George, A., Anand, T., Senthilkumar, P., & Rose, S. A.
(2017). Risk stratification of surgical site infection in a Tertiary Care Hospital: A
prospective case-control study. Journal of Patient Safety and Infection Control, 5(2),
73.
Changes to Prevent Surgical Site Infection. (2018). [online]. Retrieved from
http://www.ihi.org/resources/Pages/Changes/ChangestoPreventSurgicalSiteInfection.as
px
Chen, M., Song, X., Chen, L. Z., Lin, Z. D., & Zhang, X. L. (2016). Comparing mechanical
bowel preparation with both oral and systemic antibiotics versus mechanical bowel
preparation and systemic antibiotics alone for the prevention of surgical site infection
after elective colorectal surgery. Diseases of the Colon & Rectum, 59(1), 70-78.
Retrieved
fromhttps://www.ingentaconnect.com/content/wk/dcr/2016/00000059/00000001/
art00016
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8Identification of Surgical Site Infection in Healthcare Settings
Grundmeier, R. W., Xiao, R., Ross, R. K., Ramos, M. J., Karavite, D. J., Michel, J. J., ... &
Coffin, S. E. (2018). Identifying surgical site infections in electronic health data using
predictive models. Journal of the American Medical Informatics Association, 25(9),
1160-1166. Retrieved from
https://academic.oup.com/jamia/article-abstract/25/9/1160/5047136
Kang, D. G., Holekamp, T. F., Wagner, S. C., & Lehman Jr, R. A. (2015). Intrasite vancomycin
powder for the prevention of surgical site infection in spine surgery: a systematic
literature review. The Spine Journal, 15(4), 762-770. Retrieved
fromhttp://www.academia.edu/download/41701847/Intrasite_Vancomycin_Powder_for_t
he_Prev20160128-27160-1vaphke.pdf
Kunutsor, S. K., Whitehouse, M. R., Blom, A. W., & Beswick, A. D. (2017). Systematic review
of risk prediction scores for surgical site infection or periprosthetic joint infection
following joint arthroplasty. Epidemiology & Infection, 145(9), 1738-1749. Retrieved
from
https://pdfs.semanticscholar.org/c5d8/008b5f03151180128dd9d5f03489d9563c33.pdf
Leaper, D., & Ousey, K. (2015). Evidence update on prevention of surgical site
infection. Current opinion in infectious diseases, 28(2), 158-163. Retrieved
fromhttp://eprints.hud.ac.uk/id/eprint/23433/1/QCO280202_Leaper_MS_%282%29.pdf
Martin, E. T., Kaye, K. S., Knott, C., Nguyen, H., Santarossa, M., Evans, R., ... & Jaber, L.
(2016). Diabetes and risk of surgical site infection: a systematic review and meta-
analysis. infection control & hospital epidemiology, 37(1), 88-99. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4914132/
Mueck, K. M., & Kao, L. S. (2017). Patients at High-Risk for Surgical Site Infection. Surgical
infections, 18(4), 440-446. Retrieved from
https://www.liebertpub.com/doi/pdf/10.1089/sur.2017.058
Preventing Surgical Site Infection. (2018). World health Organization. [online]. Retrieved from
https://apps.who.int/iris/bitstream/handle/10665/273154/9789241514385-eng.pdf?ua=1
Grundmeier, R. W., Xiao, R., Ross, R. K., Ramos, M. J., Karavite, D. J., Michel, J. J., ... &
Coffin, S. E. (2018). Identifying surgical site infections in electronic health data using
predictive models. Journal of the American Medical Informatics Association, 25(9),
1160-1166. Retrieved from
https://academic.oup.com/jamia/article-abstract/25/9/1160/5047136
Kang, D. G., Holekamp, T. F., Wagner, S. C., & Lehman Jr, R. A. (2015). Intrasite vancomycin
powder for the prevention of surgical site infection in spine surgery: a systematic
literature review. The Spine Journal, 15(4), 762-770. Retrieved
fromhttp://www.academia.edu/download/41701847/Intrasite_Vancomycin_Powder_for_t
he_Prev20160128-27160-1vaphke.pdf
Kunutsor, S. K., Whitehouse, M. R., Blom, A. W., & Beswick, A. D. (2017). Systematic review
of risk prediction scores for surgical site infection or periprosthetic joint infection
following joint arthroplasty. Epidemiology & Infection, 145(9), 1738-1749. Retrieved
from
https://pdfs.semanticscholar.org/c5d8/008b5f03151180128dd9d5f03489d9563c33.pdf
Leaper, D., & Ousey, K. (2015). Evidence update on prevention of surgical site
infection. Current opinion in infectious diseases, 28(2), 158-163. Retrieved
fromhttp://eprints.hud.ac.uk/id/eprint/23433/1/QCO280202_Leaper_MS_%282%29.pdf
Martin, E. T., Kaye, K. S., Knott, C., Nguyen, H., Santarossa, M., Evans, R., ... & Jaber, L.
(2016). Diabetes and risk of surgical site infection: a systematic review and meta-
analysis. infection control & hospital epidemiology, 37(1), 88-99. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4914132/
Mueck, K. M., & Kao, L. S. (2017). Patients at High-Risk for Surgical Site Infection. Surgical
infections, 18(4), 440-446. Retrieved from
https://www.liebertpub.com/doi/pdf/10.1089/sur.2017.058
Preventing Surgical Site Infection. (2018). World health Organization. [online]. Retrieved from
https://apps.who.int/iris/bitstream/handle/10665/273154/9789241514385-eng.pdf?ua=1
9Identification of Surgical Site Infection in Healthcare Settings
Webster, J., & Osborne, S. (2015). Preoperative bathing or showering with skin antiseptics to
prevent surgical site infection. Cochrane database of systematic reviews, (2).Retrieved
from https://eprints.qut.edu.au/84491/1/__staffhome.qut.edu.au_staffgroupb
%24_bozzetto_Documents_2015002448.pdf
Webster, J., & Osborne, S. (2015). Preoperative bathing or showering with skin antiseptics to
prevent surgical site infection. Cochrane database of systematic reviews, (2).Retrieved
from https://eprints.qut.edu.au/84491/1/__staffhome.qut.edu.au_staffgroupb
%24_bozzetto_Documents_2015002448.pdf
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10Identification of Surgical Site Infection in Healthcare Settings
Appendices
Appendix 1: Annotated Bibliography Table
Appendices
Appendix 1: Annotated Bibliography Table
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11Identification of Surgical Site Infection in Healthcare Settings
12Identification of Surgical Site Infection in Healthcare Settings
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




