Analysis of Three Interprofessional Collaboration Models in Healthcare
VerifiedAdded on 2023/06/10
|11
|8413
|106
Report
AI Summary
This document analyzes three interprofessional collaboration models in healthcare education, focusing on programs at Rosalind Franklin University of Medicine and Science, the University of Florida, and the University of Washington. The models include a didactic program emphasizing team-building and patient-centered care, a community-based experience highlighting service and resource impact, and an interprofessional-simulation experience developing communication and leadership skills. The report highlights common themes such as understanding professional identity, commitment from departments, diverse calendar agreements, curricular mapping, mentor and faculty training, a sense of community, adequate physical space, technology, and community relationships as critical resources for success. The paper underscores the importance of administrative support, infrastructure, faculty commitment, and student participation for developing IPE-centered programs, ultimately aiming to improve healthcare outcomes through collaborative practice. The document also provides a detailed overview of interprofessional collaboration and education, including definitions, characteristics, and the benefits of team-based approaches.
Interprofessionalcollaboration: three
best practice models of
interprofessionaleducation
Diane R. Bridges, MSN, RN, CCM 1*, Richard A. Davidson,
MD, MPH 2, Peggy Soule Odegard,PharmD, BCPS, CDE,
FASCP 3, Ian V. Maki, MPH 3 and John Tomkowiak, MD, MOL4
1Department of InterprofessionalHealthcare Studies, Rosalind Franklin University of Medicine and
Science, North Chicago, IL, USA;2Office of InterprofessionalEducation, University of Florida,
Gainesville, FL, USA;3Office of the Dean-Regional Affairs, UW School of Medicine, Seattle, WA, USA;
4Chicago Medical School, Rosalind Franklin University of Medicine and Science, North Chicago, IL, USA
Interprofessionaleducationis a collaborativeapproachto develophealthcarestudentsas future
interprofessionalteam members and a recommendation suggested by the Institute of Medicine.Complex
medical issues can be best addressed by interprofessional teams. Training future healthcare providers to work
in such teams willhelp facilitate this modelresulting in improved healthcare outcomes for patients.In
this paper,three universities,the Rosalind Franklin University of Medicine and Science,the University of
Florida and the University ofWashington describe their training curricula models ofcollaborative and
interprofessional education.
The models represent a didactic program, a community-based experience and an interprofessional-simulation
experience. The didactic program emphasizes interprofessional team building skills, knowledge of professions,
patient centered care, service learning, the impact of culture on healthcare delivery and an interprofessional
clinicalcomponent.The community-based experience demonstrates how interprofessionalcollaborations
provide service to patients and how the environment and availability of resources impact one’s health status.
The interprofessional-simulation experience describes clinicalteam skills training in both formative and
summative simulations used to develop skills in communication and leadership.
One common theme leading to a successful experience among these three interprofessional models included
helping students to understand their own professionalidentity while gaining an understanding ofother
professional’s roles on the health care team.Commitment from departments and colleges, diverse calendar
agreements, curricular mapping, mentor and faculty training, a sense of community, adequate physical space,
technology,and community relationships were allidentified as criticalresources for a successfulprogram.
Summary recommendations for best practices included the need for administrative support, interprofessional
programmaticinfrastructure,committed faculty,and the recognition ofstudentparticipation askey
components to success for anyone developing an IPE centered program.
Keywords:interprofessional; healthcare teams; collaboration; interprofessional education; interprofessional curricula models
Received: 25 January 2011;Revised: 25 March 2011;Accepted: 3 March 2011; Published: 8 April2011
Today’spatientshave complex health needsand
typicallyrequire more than one disciplineto
addressissuesregarding theirhealth status(1).
In 2001 a recommendation by the Institute of Medicine
Committeeon Quality of Health Care in America
suggestedthat healthcareprofessionalsworking in
interprofessionalteams can bestcommunicate and ad-
dress these complex and challenging needs (1,2). This
interprofessionalapproach may allow sharing of exper-
tise and perspectives to form a common goal of restoring
or maintaining an individual’shealth and improving
outcomes while combining resources (1, 3).
Interprofessionaleducation (IPE)is an approach to
develop healthcare students for future interprofessional
teams. Students trained using an IPE approach are more
likely to become collaborativeinterprofessionalteam
(page number not for citation purpose)
æ TREND ARTICLE
Medical Education Online 2011. # 2011 Diane R. Bridges et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution
Noncommercial3.0 Unported License (http://creativecommons.org/licenses/by-nc/3.0/), permitting allnon-commercialuse, distribution, and reproduction in
any medium, provided the originalwork is properly cited.
1
Citation: MedicalEducation Online 2011, 16: 6035 - DOI: 10.3402/meo.v16i0.6035
best practice models of
interprofessionaleducation
Diane R. Bridges, MSN, RN, CCM 1*, Richard A. Davidson,
MD, MPH 2, Peggy Soule Odegard,PharmD, BCPS, CDE,
FASCP 3, Ian V. Maki, MPH 3 and John Tomkowiak, MD, MOL4
1Department of InterprofessionalHealthcare Studies, Rosalind Franklin University of Medicine and
Science, North Chicago, IL, USA;2Office of InterprofessionalEducation, University of Florida,
Gainesville, FL, USA;3Office of the Dean-Regional Affairs, UW School of Medicine, Seattle, WA, USA;
4Chicago Medical School, Rosalind Franklin University of Medicine and Science, North Chicago, IL, USA
Interprofessionaleducationis a collaborativeapproachto develophealthcarestudentsas future
interprofessionalteam members and a recommendation suggested by the Institute of Medicine.Complex
medical issues can be best addressed by interprofessional teams. Training future healthcare providers to work
in such teams willhelp facilitate this modelresulting in improved healthcare outcomes for patients.In
this paper,three universities,the Rosalind Franklin University of Medicine and Science,the University of
Florida and the University ofWashington describe their training curricula models ofcollaborative and
interprofessional education.
The models represent a didactic program, a community-based experience and an interprofessional-simulation
experience. The didactic program emphasizes interprofessional team building skills, knowledge of professions,
patient centered care, service learning, the impact of culture on healthcare delivery and an interprofessional
clinicalcomponent.The community-based experience demonstrates how interprofessionalcollaborations
provide service to patients and how the environment and availability of resources impact one’s health status.
The interprofessional-simulation experience describes clinicalteam skills training in both formative and
summative simulations used to develop skills in communication and leadership.
One common theme leading to a successful experience among these three interprofessional models included
helping students to understand their own professionalidentity while gaining an understanding ofother
professional’s roles on the health care team.Commitment from departments and colleges, diverse calendar
agreements, curricular mapping, mentor and faculty training, a sense of community, adequate physical space,
technology,and community relationships were allidentified as criticalresources for a successfulprogram.
Summary recommendations for best practices included the need for administrative support, interprofessional
programmaticinfrastructure,committed faculty,and the recognition ofstudentparticipation askey
components to success for anyone developing an IPE centered program.
Keywords:interprofessional; healthcare teams; collaboration; interprofessional education; interprofessional curricula models
Received: 25 January 2011;Revised: 25 March 2011;Accepted: 3 March 2011; Published: 8 April2011
Today’spatientshave complex health needsand
typicallyrequire more than one disciplineto
addressissuesregarding theirhealth status(1).
In 2001 a recommendation by the Institute of Medicine
Committeeon Quality of Health Care in America
suggestedthat healthcareprofessionalsworking in
interprofessionalteams can bestcommunicate and ad-
dress these complex and challenging needs (1,2). This
interprofessionalapproach may allow sharing of exper-
tise and perspectives to form a common goal of restoring
or maintaining an individual’shealth and improving
outcomes while combining resources (1, 3).
Interprofessionaleducation (IPE)is an approach to
develop healthcare students for future interprofessional
teams. Students trained using an IPE approach are more
likely to become collaborativeinterprofessionalteam
(page number not for citation purpose)
æ TREND ARTICLE
Medical Education Online 2011. # 2011 Diane R. Bridges et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution
Noncommercial3.0 Unported License (http://creativecommons.org/licenses/by-nc/3.0/), permitting allnon-commercialuse, distribution, and reproduction in
any medium, provided the originalwork is properly cited.
1
Citation: MedicalEducation Online 2011, 16: 6035 - DOI: 10.3402/meo.v16i0.6035
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
members who show respect and positive attitudes towards
each other and work towards improving patient outcomes
(35).
What is interprofessionalcollaboration and
practice?
According to the Canadian InterprofessionalHealth
Collaborative,interprofessionalcollaboration is a ‘part-
nership between a team of health providers and a client in
a participatory collaborative and coordinated approach
to shared decision making around health and social
issues’(6). Interprofessionalcollaborative practice has
been defined as a process which includes communication
and decision-making,enabling a synergistic influence of
grouped knowledge and skills (7). Elements of collabora-
tive practice include responsibility,accountability,coor-
dination, communication,cooperation,assertiveness,
autonomy,and mutualtrust and respect(7). It is this
partnership thatcreatesan interprofessionalteam de-
signed to work on common goalsto improve patient
outcomes.Collaborative interactions exhibita blending
of professional cultures and are achieved though sharing
skills and knowledge to improve the quality ofpatient
care (8, 9).
There are importantcharacteristicsthat determine
team effectiveness,including members seeing their roles
as importantto the team,open communication,the
existence of autonomy, and equality of resources (9). It is
important to note that poor interprofessionalcollabora-
tion can have a negative impact on the quality of patient
care (10).Thus skills in working as an interprofessional
team,gained through interprofessionaleducation,are
important for high-quality care.
What is interprofessionaleducation?
IPE has been defined as ‘members or students of two or
more professions associated with health or socialcare,
engaged in learning with,from and abouteach other’
(4, 11). IPE provides an ability to share skills and
knowledge between professions and allows for a better
understanding, shared values, and respect for the roles of
other healthcare professionals (5,11, 12). Casto etal.
describedthe importanceof developingearly IPE
curricula and offering them beforestudentsbegin to
practice in order to build a basic value of working within
interprofessional teams (13, 14). The desired end result is
to develop an interprofessional,team-based,collabora-
tive approach thatimproves patientoutcomes and the
quality of care (5, 15).
In this paper we showcase three exemplary models of
collaborativeand interprofessionaleducationalexperi-
ences so thatother institutions may benefitfrom these
when creating interprofessional curricula.
Models of interprofessionalcollaborative
student experiences
Rosalind Franklin University of Medicine and
Science: HMTD 500 InterprofessionalHealthcare
Teams course
Rosalind Franklin University of Medicine and
Science (RFUMS) has responded to the challenge of
interprofessional training by designing a one-credit-hour,
pass/failcoursecalled HMTD 500: Interprofessional
HealthcareTeams(2, 16). The courseis a required
experiential learning opportunity where students interact
in interprofessionalhealthcare teams.Students focus on
a collaborative approach to patient-centered care,with
emphasison team interaction,communication,service
learning,evidence-based practice,and quality improve-
ment.
The course,which was instituted in 2004,spans the
months ofAugustMarch every year,and has evolved
into three separate components each with its own course
director:a required didacticcomponent(Table 1), a
required servicelearningcomponent,and a clinical
component with limited enrollment.
During the course,all first-yearstudents(approxi-
mately 480) are grouped into 16-member interprofessional
teams.Each team has student representation from allo-
pathic and podiatric medicine, clinical laboratory, medical
radiation physic,nurse anesthetists,pathologists’assis-
tants, psychology, and physician assistants. Each team has
a faculty or staff member, with a minimum of a master’s
degree, serving as a mentor. Mentors are trained prior to
each class,and the lunch hour of every class day is set
aside for mentors to review material and ask questions if
necessary.
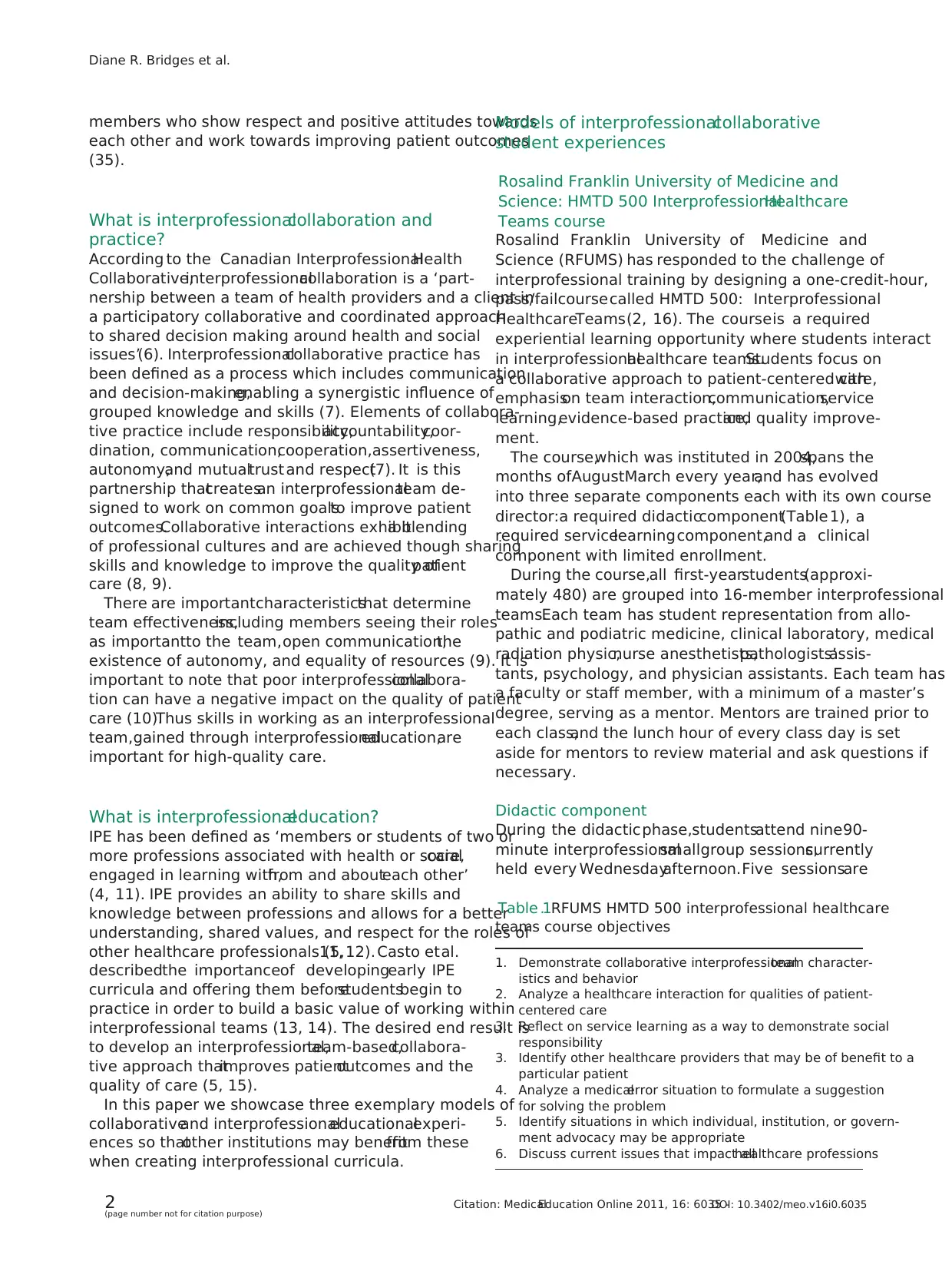
Didactic component
During the didacticphase,studentsattend nine90-
minute interprofessionalsmallgroup sessions,currently
held every Wednesdayafternoon.Five sessionsare
Table 1. RFUMS HMTD 500 interprofessional healthcare
teams course objectives
1. Demonstrate collaborative interprofessionalteam character-
istics and behavior
2. Analyze a healthcare interaction for qualities of patient-
centered care
3. Reflect on service learning as a way to demonstrate social
responsibility
3. Identify other healthcare providers that may be of benefit to a
particular patient
4. Analyze a medicalerror situation to formulate a suggestion
for solving the problem
5. Identify situations in which individual, institution, or govern-
ment advocacy may be appropriate
6. Discuss current issues that impact allhealthcare professions
Diane R. Bridges et al.
2(page number not for citation purpose)
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035
each other and work towards improving patient outcomes
(35).
What is interprofessionalcollaboration and
practice?
According to the Canadian InterprofessionalHealth
Collaborative,interprofessionalcollaboration is a ‘part-
nership between a team of health providers and a client in
a participatory collaborative and coordinated approach
to shared decision making around health and social
issues’(6). Interprofessionalcollaborative practice has
been defined as a process which includes communication
and decision-making,enabling a synergistic influence of
grouped knowledge and skills (7). Elements of collabora-
tive practice include responsibility,accountability,coor-
dination, communication,cooperation,assertiveness,
autonomy,and mutualtrust and respect(7). It is this
partnership thatcreatesan interprofessionalteam de-
signed to work on common goalsto improve patient
outcomes.Collaborative interactions exhibita blending
of professional cultures and are achieved though sharing
skills and knowledge to improve the quality ofpatient
care (8, 9).
There are importantcharacteristicsthat determine
team effectiveness,including members seeing their roles
as importantto the team,open communication,the
existence of autonomy, and equality of resources (9). It is
important to note that poor interprofessionalcollabora-
tion can have a negative impact on the quality of patient
care (10).Thus skills in working as an interprofessional
team,gained through interprofessionaleducation,are
important for high-quality care.
What is interprofessionaleducation?
IPE has been defined as ‘members or students of two or
more professions associated with health or socialcare,
engaged in learning with,from and abouteach other’
(4, 11). IPE provides an ability to share skills and
knowledge between professions and allows for a better
understanding, shared values, and respect for the roles of
other healthcare professionals (5,11, 12). Casto etal.
describedthe importanceof developingearly IPE
curricula and offering them beforestudentsbegin to
practice in order to build a basic value of working within
interprofessional teams (13, 14). The desired end result is
to develop an interprofessional,team-based,collabora-
tive approach thatimproves patientoutcomes and the
quality of care (5, 15).
In this paper we showcase three exemplary models of
collaborativeand interprofessionaleducationalexperi-
ences so thatother institutions may benefitfrom these
when creating interprofessional curricula.
Models of interprofessionalcollaborative
student experiences
Rosalind Franklin University of Medicine and
Science: HMTD 500 InterprofessionalHealthcare
Teams course
Rosalind Franklin University of Medicine and
Science (RFUMS) has responded to the challenge of
interprofessional training by designing a one-credit-hour,
pass/failcoursecalled HMTD 500: Interprofessional
HealthcareTeams(2, 16). The courseis a required
experiential learning opportunity where students interact
in interprofessionalhealthcare teams.Students focus on
a collaborative approach to patient-centered care,with
emphasison team interaction,communication,service
learning,evidence-based practice,and quality improve-
ment.
The course,which was instituted in 2004,spans the
months ofAugustMarch every year,and has evolved
into three separate components each with its own course
director:a required didacticcomponent(Table 1), a
required servicelearningcomponent,and a clinical
component with limited enrollment.
During the course,all first-yearstudents(approxi-
mately 480) are grouped into 16-member interprofessional
teams.Each team has student representation from allo-
pathic and podiatric medicine, clinical laboratory, medical
radiation physic,nurse anesthetists,pathologists’assis-
tants, psychology, and physician assistants. Each team has
a faculty or staff member, with a minimum of a master’s
degree, serving as a mentor. Mentors are trained prior to
each class,and the lunch hour of every class day is set
aside for mentors to review material and ask questions if
necessary.
Didactic component
During the didacticphase,studentsattend nine90-
minute interprofessionalsmallgroup sessions,currently
held every Wednesdayafternoon.Five sessionsare
Table 1. RFUMS HMTD 500 interprofessional healthcare
teams course objectives
1. Demonstrate collaborative interprofessionalteam character-
istics and behavior
2. Analyze a healthcare interaction for qualities of patient-
centered care
3. Reflect on service learning as a way to demonstrate social
responsibility
3. Identify other healthcare providers that may be of benefit to a
particular patient
4. Analyze a medicalerror situation to formulate a suggestion
for solving the problem
5. Identify situations in which individual, institution, or govern-
ment advocacy may be appropriate
6. Discuss current issues that impact allhealthcare professions
Diane R. Bridges et al.
2(page number not for citation purpose)
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035
devoted to thelearning conceptsof interprofessional
healthcareteams,collaborativepatient-centeredcare
(functioning asa collaborative team),service learning
and county health assessment,healthcare professions (a
time to learn abouttheir own health profession),and
error cases and advocacy.
The remaining sessionsare setaside fordiscussion,
preparation,presentations,and celebrations of achieve-
ments. Student objectives, case studies, and role-play are
used to developdiscussion.Two different students
volunteer each session to moderate the class to develop
their own leadershipand communicationskills. All
course materials are loaded into our information man-
agement learning system.
Service learning component
Students are tasked with working as an interprofessional
team to identify a community partner and engage in a
community serviceproject.Each team is expected to
perform a service learning project.One of the original
five sessions is designed to allow students time together to
discussideasfor their projects.Studentsassesslocal
community needs in their didactic phase and are given a
list of community projects performed in the past to help
them decide on a projectand partner.Two additional
sessionsallow them to plan theirprojectsand subse-
quently design a posterwhich showcasestheir service
learning experience and reflection.The focus of student
projects is prevention education in the form of physical
fitness training, nutrition education, health screening, or
instruction in making healthy choices.
Service learning allots time for students to process what
they learned abouttheir community:how their knowl-
edge was used to help meet the needs of the community
and how they better understand them as a result of this
activity (17). All HMTD 500 studentscompletea
reflection form.
The last session of the course culminates each year with
a group reflection and a celebration poster day where our
community partners are invited to visit the university to
review the work our students have accomplished.Com-
munity partners see posters created by each team and are
invited to join their student groups to reflectupon the
service learning project and share with the students how
the project impacted their organization.
The collaborative interprofessionalprevention educa-
tion service learning projects have been very rewarding
and well accepted byour communitypartnersand
students,as noted by student surveys and focus groups
and awardsreceived from somecommunity partners.
Student attitudes were positive regarding this aspect of
the course.Post-course survey indicated a majority of
respondents agreed or strongly agreed with statements
regarding collaboration,teamwork,socialresponsibility,
and diversity (18).
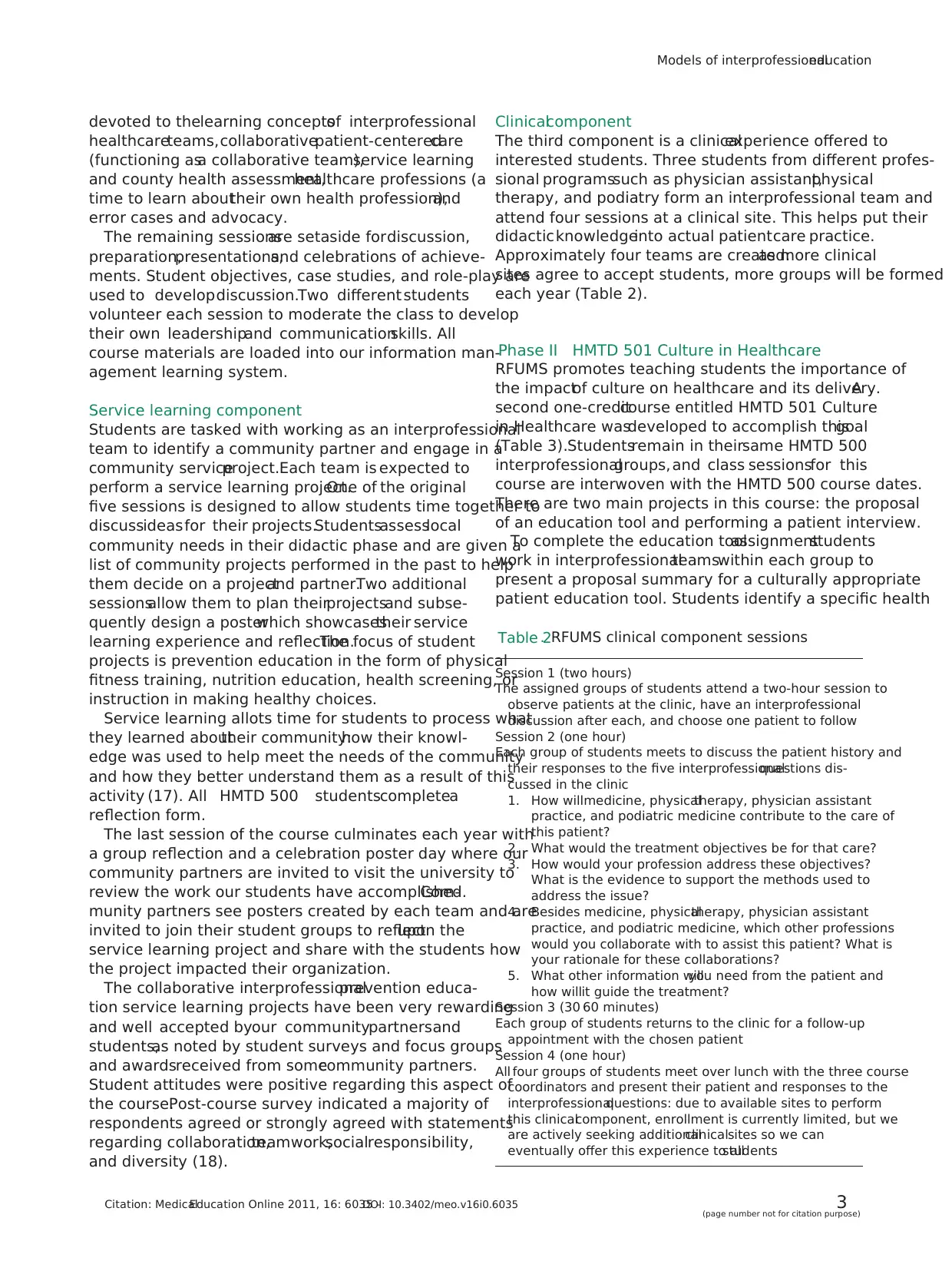
Clinicalcomponent
The third component is a clinicalexperience offered to
interested students. Three students from different profes-
sional programssuch as physician assistant,physical
therapy, and podiatry form an interprofessional team and
attend four sessions at a clinical site. This helps put their
didacticknowledgeinto actual patientcare practice.
Approximately four teams are created:as more clinical
sites agree to accept students, more groups will be formed
each year (Table 2).
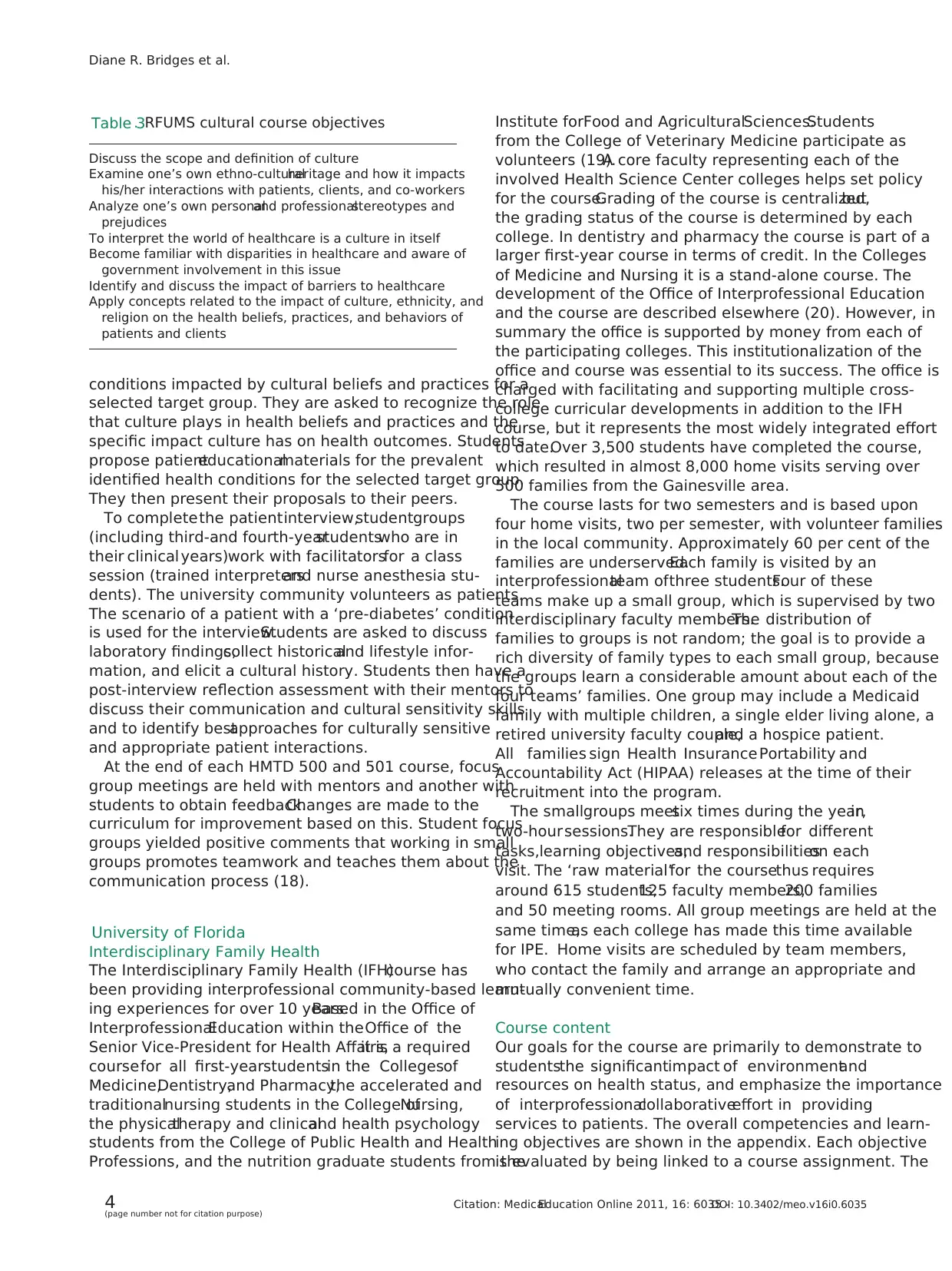
Phase II HMTD 501 Culture in Healthcare
RFUMS promotes teaching students the importance of
the impactof culture on healthcare and its delivery.A
second one-creditcourse entitled HMTD 501 Culture
in Healthcare wasdeveloped to accomplish thisgoal
(Table 3).Studentsremain in theirsame HMTD 500
interprofessionalgroups,and class sessionsfor this
course are interwoven with the HMTD 500 course dates.
There are two main projects in this course: the proposal
of an education tool and performing a patient interview.
To complete the education toolassignmentstudents
work in interprofessionalteamswithin each group to
present a proposal summary for a culturally appropriate
patient education tool. Students identify a specific health
Table 2. RFUMS clinical component sessions
Session 1 (two hours)
The assigned groups of students attend a two-hour session to
observe patients at the clinic, have an interprofessional
discussion after each, and choose one patient to follow
Session 2 (one hour)
Each group of students meets to discuss the patient history and
their responses to the five interprofessionalquestions dis-
cussed in the clinic
1. How willmedicine, physicaltherapy, physician assistant
practice, and podiatric medicine contribute to the care of
this patient?
2. What would the treatment objectives be for that care?
3. How would your profession address these objectives?
What is the evidence to support the methods used to
address the issue?
4. Besides medicine, physicaltherapy, physician assistant
practice, and podiatric medicine, which other professions
would you collaborate with to assist this patient? What is
your rationale for these collaborations?
5. What other information willyou need from the patient and
how willit guide the treatment?
Session 3 (30 60 minutes)
Each group of students returns to the clinic for a follow-up
appointment with the chosen patient
Session 4 (one hour)
All four groups of students meet over lunch with the three course
coordinators and present their patient and responses to the
interprofessionalquestions: due to available sites to perform
this clinicalcomponent, enrollment is currently limited, but we
are actively seeking additionalclinicalsites so we can
eventually offer this experience to allstudents
Models of interprofessionaleducation
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035 3(page number not for citation purpose)
healthcareteams,collaborativepatient-centeredcare
(functioning asa collaborative team),service learning
and county health assessment,healthcare professions (a
time to learn abouttheir own health profession),and
error cases and advocacy.
The remaining sessionsare setaside fordiscussion,
preparation,presentations,and celebrations of achieve-
ments. Student objectives, case studies, and role-play are
used to developdiscussion.Two different students
volunteer each session to moderate the class to develop
their own leadershipand communicationskills. All
course materials are loaded into our information man-
agement learning system.
Service learning component
Students are tasked with working as an interprofessional
team to identify a community partner and engage in a
community serviceproject.Each team is expected to
perform a service learning project.One of the original
five sessions is designed to allow students time together to
discussideasfor their projects.Studentsassesslocal
community needs in their didactic phase and are given a
list of community projects performed in the past to help
them decide on a projectand partner.Two additional
sessionsallow them to plan theirprojectsand subse-
quently design a posterwhich showcasestheir service
learning experience and reflection.The focus of student
projects is prevention education in the form of physical
fitness training, nutrition education, health screening, or
instruction in making healthy choices.
Service learning allots time for students to process what
they learned abouttheir community:how their knowl-
edge was used to help meet the needs of the community
and how they better understand them as a result of this
activity (17). All HMTD 500 studentscompletea
reflection form.
The last session of the course culminates each year with
a group reflection and a celebration poster day where our
community partners are invited to visit the university to
review the work our students have accomplished.Com-
munity partners see posters created by each team and are
invited to join their student groups to reflectupon the
service learning project and share with the students how
the project impacted their organization.
The collaborative interprofessionalprevention educa-
tion service learning projects have been very rewarding
and well accepted byour communitypartnersand
students,as noted by student surveys and focus groups
and awardsreceived from somecommunity partners.
Student attitudes were positive regarding this aspect of
the course.Post-course survey indicated a majority of
respondents agreed or strongly agreed with statements
regarding collaboration,teamwork,socialresponsibility,
and diversity (18).
Clinicalcomponent
The third component is a clinicalexperience offered to
interested students. Three students from different profes-
sional programssuch as physician assistant,physical
therapy, and podiatry form an interprofessional team and
attend four sessions at a clinical site. This helps put their
didacticknowledgeinto actual patientcare practice.
Approximately four teams are created:as more clinical
sites agree to accept students, more groups will be formed
each year (Table 2).
Phase II HMTD 501 Culture in Healthcare
RFUMS promotes teaching students the importance of
the impactof culture on healthcare and its delivery.A
second one-creditcourse entitled HMTD 501 Culture
in Healthcare wasdeveloped to accomplish thisgoal
(Table 3).Studentsremain in theirsame HMTD 500
interprofessionalgroups,and class sessionsfor this
course are interwoven with the HMTD 500 course dates.
There are two main projects in this course: the proposal
of an education tool and performing a patient interview.
To complete the education toolassignmentstudents
work in interprofessionalteamswithin each group to
present a proposal summary for a culturally appropriate
patient education tool. Students identify a specific health
Table 2. RFUMS clinical component sessions
Session 1 (two hours)
The assigned groups of students attend a two-hour session to
observe patients at the clinic, have an interprofessional
discussion after each, and choose one patient to follow
Session 2 (one hour)
Each group of students meets to discuss the patient history and
their responses to the five interprofessionalquestions dis-
cussed in the clinic
1. How willmedicine, physicaltherapy, physician assistant
practice, and podiatric medicine contribute to the care of
this patient?
2. What would the treatment objectives be for that care?
3. How would your profession address these objectives?
What is the evidence to support the methods used to
address the issue?
4. Besides medicine, physicaltherapy, physician assistant
practice, and podiatric medicine, which other professions
would you collaborate with to assist this patient? What is
your rationale for these collaborations?
5. What other information willyou need from the patient and
how willit guide the treatment?
Session 3 (30 60 minutes)
Each group of students returns to the clinic for a follow-up
appointment with the chosen patient
Session 4 (one hour)
All four groups of students meet over lunch with the three course
coordinators and present their patient and responses to the
interprofessionalquestions: due to available sites to perform
this clinicalcomponent, enrollment is currently limited, but we
are actively seeking additionalclinicalsites so we can
eventually offer this experience to allstudents
Models of interprofessionaleducation
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035 3(page number not for citation purpose)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
conditions impacted by cultural beliefs and practices for a
selected target group. They are asked to recognize the role
that culture plays in health beliefs and practices and the
specific impact culture has on health outcomes. Students
propose patienteducationalmaterials for the prevalent
identified health conditions for the selected target group.
They then present their proposals to their peers.
To completethe patientinterview,studentgroups
(including third-and fourth-yearstudentswho are in
their clinical years)work with facilitatorsfor a class
session (trained interpretersand nurse anesthesia stu-
dents). The university community volunteers as patients.
The scenario of a patient with a ‘pre-diabetes’ condition
is used for the interview.Students are asked to discuss
laboratory findings,collect historicaland lifestyle infor-
mation, and elicit a cultural history. Students then have a
post-interview reflection assessment with their mentors to
discuss their communication and cultural sensitivity skills
and to identify bestapproaches for culturally sensitive
and appropriate patient interactions.
At the end of each HMTD 500 and 501 course, focus
group meetings are held with mentors and another with
students to obtain feedback.Changes are made to the
curriculum for improvement based on this. Student focus
groups yielded positive comments that working in small
groups promotes teamwork and teaches them about the
communication process (18).
University of Florida
Interdisciplinary Family Health
The Interdisciplinary Family Health (IFH)course has
been providing interprofessional community-based learn-
ing experiences for over 10 years.Based in the Office of
InterprofessionalEducation within theOffice of the
Senior Vice-President for Health Affairs,it is a required
coursefor all first-yearstudentsin the Collegesof
Medicine,Dentistry,and Pharmacy,the accelerated and
traditionalnursing students in the College ofNursing,
the physicaltherapy and clinicaland health psychology
students from the College of Public Health and Health
Professions, and the nutrition graduate students from the
Institute forFood and AgriculturalSciences.Students
from the College of Veterinary Medicine participate as
volunteers (19).A core faculty representing each of the
involved Health Science Center colleges helps set policy
for the course.Grading of the course is centralized,but
the grading status of the course is determined by each
college. In dentistry and pharmacy the course is part of a
larger first-year course in terms of credit. In the Colleges
of Medicine and Nursing it is a stand-alone course. The
development of the Office of Interprofessional Education
and the course are described elsewhere (20). However, in
summary the office is supported by money from each of
the participating colleges. This institutionalization of the
office and course was essential to its success. The office is
charged with facilitating and supporting multiple cross-
college curricular developments in addition to the IFH
course, but it represents the most widely integrated effort
to date.Over 3,500 students have completed the course,
which resulted in almost 8,000 home visits serving over
500 families from the Gainesville area.
The course lasts for two semesters and is based upon
four home visits, two per semester, with volunteer families
in the local community. Approximately 60 per cent of the
families are underserved.Each family is visited by an
interprofessionalteam ofthree students.Four of these
teams make up a small group, which is supervised by two
interdisciplinary faculty members.The distribution of
families to groups is not random; the goal is to provide a
rich diversity of family types to each small group, because
the groups learn a considerable amount about each of the
four teams’ families. One group may include a Medicaid
family with multiple children, a single elder living alone, a
retired university faculty couple,and a hospice patient.
All families sign Health Insurance Portability and
Accountability Act (HIPAA) releases at the time of their
recruitment into the program.
The smallgroups meetsix times during the year,in
two-hour sessions.They are responsiblefor different
tasks,learning objectives,and responsibilitieson each
visit. The ‘raw material’for the coursethus requires
around 615 students,125 faculty members,200 families
and 50 meeting rooms. All group meetings are held at the
same time,as each college has made this time available
for IPE. Home visits are scheduled by team members,
who contact the family and arrange an appropriate and
mutually convenient time.
Course content
Our goals for the course are primarily to demonstrate to
studentsthe significantimpact of environmentand
resources on health status, and emphasize the importance
of interprofessionalcollaborativeeffort in providing
services to patients. The overall competencies and learn-
ing objectives are shown in the appendix. Each objective
is evaluated by being linked to a course assignment. The
Table 3. RFUMS cultural course objectives
Discuss the scope and definition of culture
Examine one’s own ethno-culturalheritage and how it impacts
his/her interactions with patients, clients, and co-workers
Analyze one’s own personaland professionalstereotypes and
prejudices
To interpret the world of healthcare is a culture in itself
Become familiar with disparities in healthcare and aware of
government involvement in this issue
Identify and discuss the impact of barriers to healthcare
Apply concepts related to the impact of culture, ethnicity, and
religion on the health beliefs, practices, and behaviors of
patients and clients
Diane R. Bridges et al.
4(page number not for citation purpose)
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035
selected target group. They are asked to recognize the role
that culture plays in health beliefs and practices and the
specific impact culture has on health outcomes. Students
propose patienteducationalmaterials for the prevalent
identified health conditions for the selected target group.
They then present their proposals to their peers.
To completethe patientinterview,studentgroups
(including third-and fourth-yearstudentswho are in
their clinical years)work with facilitatorsfor a class
session (trained interpretersand nurse anesthesia stu-
dents). The university community volunteers as patients.
The scenario of a patient with a ‘pre-diabetes’ condition
is used for the interview.Students are asked to discuss
laboratory findings,collect historicaland lifestyle infor-
mation, and elicit a cultural history. Students then have a
post-interview reflection assessment with their mentors to
discuss their communication and cultural sensitivity skills
and to identify bestapproaches for culturally sensitive
and appropriate patient interactions.
At the end of each HMTD 500 and 501 course, focus
group meetings are held with mentors and another with
students to obtain feedback.Changes are made to the
curriculum for improvement based on this. Student focus
groups yielded positive comments that working in small
groups promotes teamwork and teaches them about the
communication process (18).
University of Florida
Interdisciplinary Family Health
The Interdisciplinary Family Health (IFH)course has
been providing interprofessional community-based learn-
ing experiences for over 10 years.Based in the Office of
InterprofessionalEducation within theOffice of the
Senior Vice-President for Health Affairs,it is a required
coursefor all first-yearstudentsin the Collegesof
Medicine,Dentistry,and Pharmacy,the accelerated and
traditionalnursing students in the College ofNursing,
the physicaltherapy and clinicaland health psychology
students from the College of Public Health and Health
Professions, and the nutrition graduate students from the
Institute forFood and AgriculturalSciences.Students
from the College of Veterinary Medicine participate as
volunteers (19).A core faculty representing each of the
involved Health Science Center colleges helps set policy
for the course.Grading of the course is centralized,but
the grading status of the course is determined by each
college. In dentistry and pharmacy the course is part of a
larger first-year course in terms of credit. In the Colleges
of Medicine and Nursing it is a stand-alone course. The
development of the Office of Interprofessional Education
and the course are described elsewhere (20). However, in
summary the office is supported by money from each of
the participating colleges. This institutionalization of the
office and course was essential to its success. The office is
charged with facilitating and supporting multiple cross-
college curricular developments in addition to the IFH
course, but it represents the most widely integrated effort
to date.Over 3,500 students have completed the course,
which resulted in almost 8,000 home visits serving over
500 families from the Gainesville area.
The course lasts for two semesters and is based upon
four home visits, two per semester, with volunteer families
in the local community. Approximately 60 per cent of the
families are underserved.Each family is visited by an
interprofessionalteam ofthree students.Four of these
teams make up a small group, which is supervised by two
interdisciplinary faculty members.The distribution of
families to groups is not random; the goal is to provide a
rich diversity of family types to each small group, because
the groups learn a considerable amount about each of the
four teams’ families. One group may include a Medicaid
family with multiple children, a single elder living alone, a
retired university faculty couple,and a hospice patient.
All families sign Health Insurance Portability and
Accountability Act (HIPAA) releases at the time of their
recruitment into the program.
The smallgroups meetsix times during the year,in
two-hour sessions.They are responsiblefor different
tasks,learning objectives,and responsibilitieson each
visit. The ‘raw material’for the coursethus requires
around 615 students,125 faculty members,200 families
and 50 meeting rooms. All group meetings are held at the
same time,as each college has made this time available
for IPE. Home visits are scheduled by team members,
who contact the family and arrange an appropriate and
mutually convenient time.
Course content
Our goals for the course are primarily to demonstrate to
studentsthe significantimpact of environmentand
resources on health status, and emphasize the importance
of interprofessionalcollaborativeeffort in providing
services to patients. The overall competencies and learn-
ing objectives are shown in the appendix. Each objective
is evaluated by being linked to a course assignment. The
Table 3. RFUMS cultural course objectives
Discuss the scope and definition of culture
Examine one’s own ethno-culturalheritage and how it impacts
his/her interactions with patients, clients, and co-workers
Analyze one’s own personaland professionalstereotypes and
prejudices
To interpret the world of healthcare is a culture in itself
Become familiar with disparities in healthcare and aware of
government involvement in this issue
Identify and discuss the impact of barriers to healthcare
Apply concepts related to the impact of culture, ethnicity, and
religion on the health beliefs, practices, and behaviors of
patients and clients
Diane R. Bridges et al.
4(page number not for citation purpose)
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
competencies are in three major categories:patient care,
interpersonaland communication skills,and profession-
alism.The assigned tasks for the course are designed to
allow the students to implement learning activities they
have been taughtin their didactic coursework.For
instance, all colleges teach students about taking a family
history or genogram,and during the firsthome visit
students are required to develop a genogram for their
family.Students who are taughtto do vital signsare
expected to take vital signs of the family members.
Assignments vary by visit. After every home visit, each
student submits a report that describes the visit from the
student’s perspective. For the first home visit, students are
asked to submita family genogram and a ‘windshield
survey’which describes the neighborhood in which the
family resides,including accessto drug and grocery
stores,an assessment of the safety of the location,and
other information thatis to be filled out when the
students are driving to their visit.At the second visit,
students fillout an extensive health survey that assesses
the family’s health status, resources, and health behaviors.
After that visit, student teams develop a project that will
hopefully positively address the family’s health status in
some way.This could be preventive (such as an exercise
program for weightloss);social(arranging experiences
and aid for single elders);economic (helping families
enrollin Medicaid or other assistance);or educational
(teachingfamiliesabout their medicaland/or socio-
behavioralconcerns).At the third group meeting,a
socialworker attends each meeting and provides assis-
tance to the teams with regard to access to resources.
A variety of required reading and discussion questions
are also assigned and discussed during themeetings.
These address such appropriate topics as definitions of
family,techniques specific to family interviewing,caring
for the poor,issues ofadherence and compliance,and
healthcare teams and communication.
During the spring semesterthe teamspresenttheir
projectsto the family,and the last home visit is to
determine the effectiveness or acceptability of the project
from the family’s perspective.This coming year,for the
first time,we are adding contentconcerning the colla-
borative aspects of patient safety education.
At the conclusion ofthe course,teams submittheir
family projectto their group.This can be done asa
PowerPoint presentation,video,poster,or a written/oral
presentation.The projectis done as a team, but all
studentsmust submit a reflectionpaper discussing
various aspects of their participation in the course and
its impact on their development as a health professional.
Extensive online evaluations of the students and faculty
have taken place over the years,as an entire course and
by discipline.
It is importantthat we clarify a crucialpart of our
program: because the supervising faculty include a range
of disciplines,and the faculty rarely ifevermeetthe
family directly,we are notproviding medical,nursing,
dental, or pharmaceutical care to these families, although
the students may help arrange such services.
Future
Based on evaluationsand faculty feedback,we make
changes in the course each year. Because our overarching
goalis to have interprofessionallearning experiences in
all years of training, we have been working towards ways
to keep the groups together beyond their first year. This
meets with challengesbecause the traditionalnursing,
physical therapy, and clinical psychology students have a
two-yearcurriculum,while pharmacy,medicine,and
dentistry have four-yearprograms.A committee com-
posed ofthe education deans from allsix colleges has
developed a common set of interprofessionalcompeten-
cies for allstudents.Newly developed interprofessional
coursework based on these competencies will be required
for all students.
University of Washington
The University of Washington ishome to six health
professions schools medicine, pharmacy, nursing, social
work, public health, and dentistry and includes the sole
allopathic medicalschoolfor the states of Washington,
Wyoming,Alaska, Montana, and Idaho (known as
WWAMI). In 1997 the university established the Center
for Health Sciences InterprofessionalEducation
(CHSIE), in an effort to integrate better the teaching,
research,and professionalactivitiesof these health
science schools,the information school,and the health
scienceslibraries.The CHSIE was developed through
grant support from the University Initiatives Fund (21
24). To date,over2,300 health sciencesstudentshave
participated in formal IPE programs offered through the
CHSIE.
The course catalog for the University of Washington
includesmore than 50 collaborativeinterprofessional
offeringsfor studentsin the health sciences,ranging
from issues in treatmentof alcoholism to care for
medicallyunderserved populations.The existenceof
these courses, and support for them, provides a platform
from which studentsfrom diversehealth profession
programs can learn ‘with,from,and about’each other,
outsideof their program ‘silos.’In addition to the
integratedcoursework,co-curricularservicelearning
and experientialtraining activities are available. Because
healthcare is typically provided by teams, the opportunity
to establish strategic teamsof learnershas been well
received by collaborating students,faculty,clinicalprac-
tice sites, and communityorganizations,promoting
sustainability of these efforts.
Models of interprofessionaleducation
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035 5(page number not for citation purpose)
interpersonaland communication skills,and profession-
alism.The assigned tasks for the course are designed to
allow the students to implement learning activities they
have been taughtin their didactic coursework.For
instance, all colleges teach students about taking a family
history or genogram,and during the firsthome visit
students are required to develop a genogram for their
family.Students who are taughtto do vital signsare
expected to take vital signs of the family members.
Assignments vary by visit. After every home visit, each
student submits a report that describes the visit from the
student’s perspective. For the first home visit, students are
asked to submita family genogram and a ‘windshield
survey’which describes the neighborhood in which the
family resides,including accessto drug and grocery
stores,an assessment of the safety of the location,and
other information thatis to be filled out when the
students are driving to their visit.At the second visit,
students fillout an extensive health survey that assesses
the family’s health status, resources, and health behaviors.
After that visit, student teams develop a project that will
hopefully positively address the family’s health status in
some way.This could be preventive (such as an exercise
program for weightloss);social(arranging experiences
and aid for single elders);economic (helping families
enrollin Medicaid or other assistance);or educational
(teachingfamiliesabout their medicaland/or socio-
behavioralconcerns).At the third group meeting,a
socialworker attends each meeting and provides assis-
tance to the teams with regard to access to resources.
A variety of required reading and discussion questions
are also assigned and discussed during themeetings.
These address such appropriate topics as definitions of
family,techniques specific to family interviewing,caring
for the poor,issues ofadherence and compliance,and
healthcare teams and communication.
During the spring semesterthe teamspresenttheir
projectsto the family,and the last home visit is to
determine the effectiveness or acceptability of the project
from the family’s perspective.This coming year,for the
first time,we are adding contentconcerning the colla-
borative aspects of patient safety education.
At the conclusion ofthe course,teams submittheir
family projectto their group.This can be done asa
PowerPoint presentation,video,poster,or a written/oral
presentation.The projectis done as a team, but all
studentsmust submit a reflectionpaper discussing
various aspects of their participation in the course and
its impact on their development as a health professional.
Extensive online evaluations of the students and faculty
have taken place over the years,as an entire course and
by discipline.
It is importantthat we clarify a crucialpart of our
program: because the supervising faculty include a range
of disciplines,and the faculty rarely ifevermeetthe
family directly,we are notproviding medical,nursing,
dental, or pharmaceutical care to these families, although
the students may help arrange such services.
Future
Based on evaluationsand faculty feedback,we make
changes in the course each year. Because our overarching
goalis to have interprofessionallearning experiences in
all years of training, we have been working towards ways
to keep the groups together beyond their first year. This
meets with challengesbecause the traditionalnursing,
physical therapy, and clinical psychology students have a
two-yearcurriculum,while pharmacy,medicine,and
dentistry have four-yearprograms.A committee com-
posed ofthe education deans from allsix colleges has
developed a common set of interprofessionalcompeten-
cies for allstudents.Newly developed interprofessional
coursework based on these competencies will be required
for all students.
University of Washington
The University of Washington ishome to six health
professions schools medicine, pharmacy, nursing, social
work, public health, and dentistry and includes the sole
allopathic medicalschoolfor the states of Washington,
Wyoming,Alaska, Montana, and Idaho (known as
WWAMI). In 1997 the university established the Center
for Health Sciences InterprofessionalEducation
(CHSIE), in an effort to integrate better the teaching,
research,and professionalactivitiesof these health
science schools,the information school,and the health
scienceslibraries.The CHSIE was developed through
grant support from the University Initiatives Fund (21
24). To date,over2,300 health sciencesstudentshave
participated in formal IPE programs offered through the
CHSIE.
The course catalog for the University of Washington
includesmore than 50 collaborativeinterprofessional
offeringsfor studentsin the health sciences,ranging
from issues in treatmentof alcoholism to care for
medicallyunderserved populations.The existenceof
these courses, and support for them, provides a platform
from which studentsfrom diversehealth profession
programs can learn ‘with,from,and about’each other,
outsideof their program ‘silos.’In addition to the
integratedcoursework,co-curricularservicelearning
and experientialtraining activities are available. Because
healthcare is typically provided by teams, the opportunity
to establish strategic teamsof learnershas been well
received by collaborating students,faculty,clinicalprac-
tice sites, and communityorganizations,promoting
sustainability of these efforts.
Models of interprofessionaleducation
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035 5(page number not for citation purpose)
Experientialtraining programs
Interprofessionalteam simulation
A clinical team training and skills assessment simulation
is currently in developmentat the University ofWa-
shington for integration into the core curricula ofthe
Medex, medicine,nursing, and pharmacyprograms
through a grant from the Josiah Macy Foundation, using
simulation to promote interprofessionalteamwork.In
this project,interprofessionalstudent teams collaborate
to provide urgent care to simulatedpatients.The
simulated cases involve an acute asthma exacerbation in
an emergency room setting, a serious cardiac arrhythmia
in an intensive care setting,a patientpresenting to an
urgent care setting with acute shortness of breath,and
two cases involving disclosure of medical errors. Content
primers using web-based reviews and recorded presenta-
tions are available in preparation forthe simulations,
along with appropriate orientation to the simulation tools
(e.g., mannequin, crash cart, monitoring devices). Curri-
cular mapping hasbeen conducted to identify ideal
timing of the simulationsin each program to ensure
sustainable curricular integration and comparability in
student clinical preparation for participation. The objec-
tives of the simulations are both formative and summa-
tive,allowing participants to practice and demonstrate
team-based skills including communication, mutual sup-
port, leadership,and situationalmonitoring (25).To
receive a pass score,students participate in the training
simulations and demonstrate acceptable performance in
the summative assessmentsimulation.In summer 2010
beta testingof casestook place, with 24 students
participatingin the human patientemergencycases
simulator and 20 students in the error disclosure standar-
dized patient simulation.A common set of IPE compe-
tencies(Table 4), based on learning objectivesand
competencies published by the Halifax Nursing Associa-
tion, the CHSIE, and the TeamSTEPPS model, were used
to guide development of the simulation (21, 25, 26).
SPARX (studentproviders aspiring to ruraland under-
served experience)
The SPARX program was developed in 1994 asan
interprofessionalco-curricular(outsidethe classroom)
opportunity (27). The goal of SPARX is to provide health
science students with a variety of co-curricular activities,
including exposure to successfulpractitioners who serve
rural and medically underserved populations. A SPARX
steering committee composed of staff and faculty from
the health science schools created the infrastructure to
link the schools around the program and,in 1996,the
WWAMI Area Health Education Center Program Office
assumed responsibility for administering and funding the
SPARX program.
Staff and students collaboratively develop topics and
projects.Studentparticipantsare continually engaged
and asked to suggest new topics and direction for SPARX
to ensure thatprogram offerings resonate with student
interests, which shift over time in response to social and
political eventslike health reform efforts,emerging
research,and pop culture. SPARX reaches out to
studentsthrough a variety ofmeans,including flyers,
advertisements,and social media such as Facebook.
Experiencehas demonstrated,however,that nothing
substitutesfor the effective outreach realized through
student meetings and class orientations.
The SPARX program consists of three elements:
forums and seminars on topics ofinterest or value for
rural and urban underserved providersto stimulate
studentinterest,training to develop skillsand foster
interprofessionalrelationships among students,and ser-
vice projects to provide experientiallearning and foster
collaborative teamwork acrossinvolved health profes-
sions students.Early SPARX projects focused on health
and wellnessin rural children,kids’ health screening,
clothing drives, and outreach to migrant farm workers in
the fields.In the late 1990s SPARX supported a mobile
outreach and primary care projectfor urban homeless
and street-involved youth.More recently,SPARX has
partnered with Seattle Head Startto provide sensory
assessments for children in its programs and larger urban
health fairs targeting medically underserved Latinos.
In 1997 SPARX created the SPARX Participation
Award to allow studentsto earn a certificate through
attendance at seminars and support for projects. Students
who gain the certificate are named in a letter to their
respective deans and faculty advisors.In 2007 SPARX
and a sister program in the Departmentof Family
Medicine, the Community Health Advancement Program
(CHAP), linked through a shared rolein delivering
program seminars,combinedthe award. This link
allowed students participating in either program to earn
points towards the shared SPARX/CHAP Award, recog-
nizing thatstudentshad increasingly limited time for
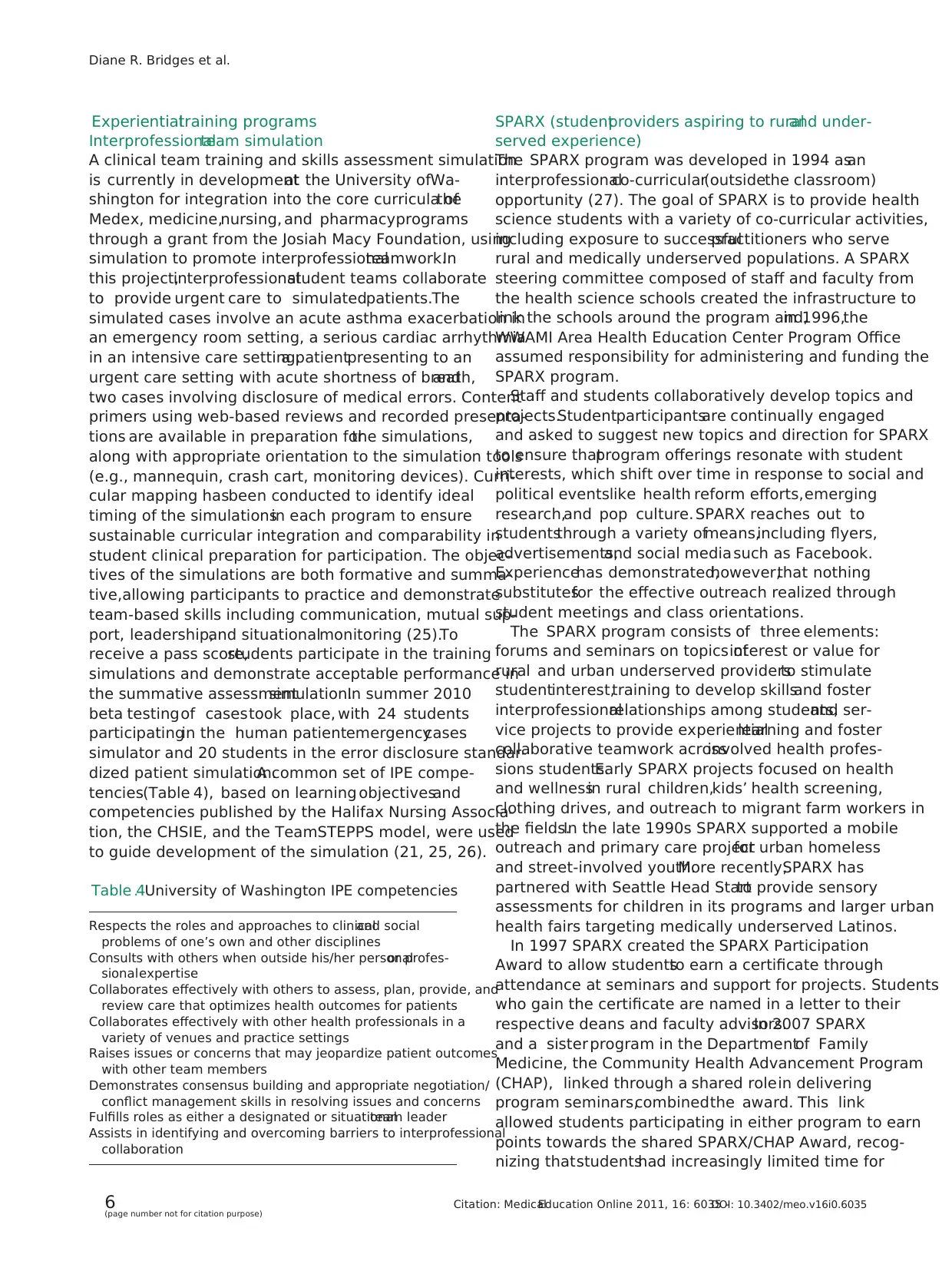
Table 4. University of Washington IPE competencies
Respects the roles and approaches to clinicaland social
problems of one’s own and other disciplines
Consults with others when outside his/her personalor profes-
sionalexpertise
Collaborates effectively with others to assess, plan, provide, and
review care that optimizes health outcomes for patients
Collaborates effectively with other health professionals in a
variety of venues and practice settings
Raises issues or concerns that may jeopardize patient outcomes
with other team members
Demonstrates consensus building and appropriate negotiation/
conflict management skills in resolving issues and concerns
Fulfills roles as either a designated or situationalteam leader
Assists in identifying and overcoming barriers to interprofessional
collaboration
Diane R. Bridges et al.
6(page number not for citation purpose)
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035
Interprofessionalteam simulation
A clinical team training and skills assessment simulation
is currently in developmentat the University ofWa-
shington for integration into the core curricula ofthe
Medex, medicine,nursing, and pharmacyprograms
through a grant from the Josiah Macy Foundation, using
simulation to promote interprofessionalteamwork.In
this project,interprofessionalstudent teams collaborate
to provide urgent care to simulatedpatients.The
simulated cases involve an acute asthma exacerbation in
an emergency room setting, a serious cardiac arrhythmia
in an intensive care setting,a patientpresenting to an
urgent care setting with acute shortness of breath,and
two cases involving disclosure of medical errors. Content
primers using web-based reviews and recorded presenta-
tions are available in preparation forthe simulations,
along with appropriate orientation to the simulation tools
(e.g., mannequin, crash cart, monitoring devices). Curri-
cular mapping hasbeen conducted to identify ideal
timing of the simulationsin each program to ensure
sustainable curricular integration and comparability in
student clinical preparation for participation. The objec-
tives of the simulations are both formative and summa-
tive,allowing participants to practice and demonstrate
team-based skills including communication, mutual sup-
port, leadership,and situationalmonitoring (25).To
receive a pass score,students participate in the training
simulations and demonstrate acceptable performance in
the summative assessmentsimulation.In summer 2010
beta testingof casestook place, with 24 students
participatingin the human patientemergencycases
simulator and 20 students in the error disclosure standar-
dized patient simulation.A common set of IPE compe-
tencies(Table 4), based on learning objectivesand
competencies published by the Halifax Nursing Associa-
tion, the CHSIE, and the TeamSTEPPS model, were used
to guide development of the simulation (21, 25, 26).
SPARX (studentproviders aspiring to ruraland under-
served experience)
The SPARX program was developed in 1994 asan
interprofessionalco-curricular(outsidethe classroom)
opportunity (27). The goal of SPARX is to provide health
science students with a variety of co-curricular activities,
including exposure to successfulpractitioners who serve
rural and medically underserved populations. A SPARX
steering committee composed of staff and faculty from
the health science schools created the infrastructure to
link the schools around the program and,in 1996,the
WWAMI Area Health Education Center Program Office
assumed responsibility for administering and funding the
SPARX program.
Staff and students collaboratively develop topics and
projects.Studentparticipantsare continually engaged
and asked to suggest new topics and direction for SPARX
to ensure thatprogram offerings resonate with student
interests, which shift over time in response to social and
political eventslike health reform efforts,emerging
research,and pop culture. SPARX reaches out to
studentsthrough a variety ofmeans,including flyers,
advertisements,and social media such as Facebook.
Experiencehas demonstrated,however,that nothing
substitutesfor the effective outreach realized through
student meetings and class orientations.
The SPARX program consists of three elements:
forums and seminars on topics ofinterest or value for
rural and urban underserved providersto stimulate
studentinterest,training to develop skillsand foster
interprofessionalrelationships among students,and ser-
vice projects to provide experientiallearning and foster
collaborative teamwork acrossinvolved health profes-
sions students.Early SPARX projects focused on health
and wellnessin rural children,kids’ health screening,
clothing drives, and outreach to migrant farm workers in
the fields.In the late 1990s SPARX supported a mobile
outreach and primary care projectfor urban homeless
and street-involved youth.More recently,SPARX has
partnered with Seattle Head Startto provide sensory
assessments for children in its programs and larger urban
health fairs targeting medically underserved Latinos.
In 1997 SPARX created the SPARX Participation
Award to allow studentsto earn a certificate through
attendance at seminars and support for projects. Students
who gain the certificate are named in a letter to their
respective deans and faculty advisors.In 2007 SPARX
and a sister program in the Departmentof Family
Medicine, the Community Health Advancement Program
(CHAP), linked through a shared rolein delivering
program seminars,combinedthe award. This link
allowed students participating in either program to earn
points towards the shared SPARX/CHAP Award, recog-
nizing thatstudentshad increasingly limited time for
Table 4. University of Washington IPE competencies
Respects the roles and approaches to clinicaland social
problems of one’s own and other disciplines
Consults with others when outside his/her personalor profes-
sionalexpertise
Collaborates effectively with others to assess, plan, provide, and
review care that optimizes health outcomes for patients
Collaborates effectively with other health professionals in a
variety of venues and practice settings
Raises issues or concerns that may jeopardize patient outcomes
with other team members
Demonstrates consensus building and appropriate negotiation/
conflict management skills in resolving issues and concerns
Fulfills roles as either a designated or situationalteam leader
Assists in identifying and overcoming barriers to interprofessional
collaboration
Diane R. Bridges et al.
6(page number not for citation purpose)
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
service activities and shouldn’thave to choose between
program offerings on account of the certificate.
Demand for and participation in the SPARX program
has increased over time.In 19951996 fewer than 100
students participated, and of those more than 70 per cent
were medicalstudents.In 20092010 more than 500
students from allthe health sciences participated in at
least one SPARX activity and 87 students will receive the
SPARX/CHAP Award. The Latina Health Fair activity
drew over 140 studentvolunteers,a record for any
University ofWashington-sponsored service projectex-
cept the institutional support for the Martin Luther King
Jr Day of Service.In 20092010 SPARX offered 13
seminars,panels,and forums and seven service projects,
including sensory screening atHead Start, breakfast
programs at a youth homeless shelter nine days a month,
Martin Luther King Jr Day of Service projects, the One
Night Count of Homeless,the Latina Health Fair,and
mentoring at a school for homeless children. The Latina
Health Fair alone reached over 500 families with health
screenings,education,counseling,and referralto the
community health clinic for follow-up, demonstrating the
ability of these programs to reach far into communities.
Common elements among interprofessional
curriculum models
There are many elements ofcollaborative practice that
find their way into successfulIPE experiences like those
described in this paper. These elements include responsi-
bility,accountability,coordination,communication,co-
operation, assertiveness, autonomy, and mutual trust and
respect (6). A successful interprofessional curriculum will
ensure that students can experience,share,and practice
these traits with each other.
Understanding others’professions and your own role
in the healthcareteam is critical in IPE (28). This
represents a longitudinal developmental goal; as students
become more immersed in their own education they are
likely to gain a better and more comprehensive under-
standing of their role in the healthcare team. Though at
first students may not understand the complexities of the
relationships between their profession and others,it is
importantto develop a common framework early in
their education thatdescribes a bestpractice modelof
interprofessional interaction. This will provide a goal that
they can work towards as they move from studentto
professionalhealthcare team member.As a part of this
enhanced understanding,exploring boundaries ofeach
profession will help students understand better the duties
for his/her profession.
Another key element is for students to ‘see’ the impact
of interprofessionalefforts and reflect on the experience
to help reinforce interprofessional learning outcomes.
For students, their attitudes and perceptions regarding
successfulmodels ofcollaboration,whether clinicalor
educational,can be essentialto the value of the instruc-
tion. Grading studentparticipation willalso add value
for them.
Lastly, the training of mentors/faculty is an important
elementin the successfulinterprofessionalcurriculum.
Mentors and faculty need to feelconfidentin their
interactionswith students.The significanceof any
interprofessionalcourse needs to be shared with faculty
so they can see its importance.
Resources
An interprofessionalcurriculum requiresa significant
commitmentfrom university administration,as wellas
deans and faculty from multiple professions who must
be willing to champion the effort. Each curriculum
effort should be critically evaluated,both quantitatively
and qualitatively.In addition, we have found the
following resources to be crucialto the success ofthe
interprofessionalleaning experience.
For didactic learning experiences,consider the
following.
1. Commitment from departments and colleges to set
aside time for students to participate in the course.
2. Curricular mapping between schools can facilitate
activities.
3. Adequate rooms and facilities able to accommodate
large numbers of students,faculty,staff,and com-
munity members.
4. Creation of a space for a sense of community and
shared purpose through ice-breaking activities and
introductions.
5. Technology for web-based conferences to reach all
participants, as well as a learning system to admin-
ister course content materials and grade students.
For community-based learning experiencesfor stu-
dents, consider the following.
1. Do you have an enthusiasticcommitmentfrom
community partners?
2. Create projects which utilize a diversity ofprofes-
sions.
3. If you are using families or individuals, do you have
clear expectations as to whether this is simply an
educational experience for your students or delivery
of healthcare?
4. Are there contingencies for community participants
who become lost to follow-up?
5. Confidentiality of personal health information must
be a high priority.
6. The university must develop a community presence
so that year after year these relationships can be
strengthened and new partnerships formed.
Models of interprofessionaleducation
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035 7(page number not for citation purpose)
program offerings on account of the certificate.
Demand for and participation in the SPARX program
has increased over time.In 19951996 fewer than 100
students participated, and of those more than 70 per cent
were medicalstudents.In 20092010 more than 500
students from allthe health sciences participated in at
least one SPARX activity and 87 students will receive the
SPARX/CHAP Award. The Latina Health Fair activity
drew over 140 studentvolunteers,a record for any
University ofWashington-sponsored service projectex-
cept the institutional support for the Martin Luther King
Jr Day of Service.In 20092010 SPARX offered 13
seminars,panels,and forums and seven service projects,
including sensory screening atHead Start, breakfast
programs at a youth homeless shelter nine days a month,
Martin Luther King Jr Day of Service projects, the One
Night Count of Homeless,the Latina Health Fair,and
mentoring at a school for homeless children. The Latina
Health Fair alone reached over 500 families with health
screenings,education,counseling,and referralto the
community health clinic for follow-up, demonstrating the
ability of these programs to reach far into communities.
Common elements among interprofessional
curriculum models
There are many elements ofcollaborative practice that
find their way into successfulIPE experiences like those
described in this paper. These elements include responsi-
bility,accountability,coordination,communication,co-
operation, assertiveness, autonomy, and mutual trust and
respect (6). A successful interprofessional curriculum will
ensure that students can experience,share,and practice
these traits with each other.
Understanding others’professions and your own role
in the healthcareteam is critical in IPE (28). This
represents a longitudinal developmental goal; as students
become more immersed in their own education they are
likely to gain a better and more comprehensive under-
standing of their role in the healthcare team. Though at
first students may not understand the complexities of the
relationships between their profession and others,it is
importantto develop a common framework early in
their education thatdescribes a bestpractice modelof
interprofessional interaction. This will provide a goal that
they can work towards as they move from studentto
professionalhealthcare team member.As a part of this
enhanced understanding,exploring boundaries ofeach
profession will help students understand better the duties
for his/her profession.
Another key element is for students to ‘see’ the impact
of interprofessionalefforts and reflect on the experience
to help reinforce interprofessional learning outcomes.
For students, their attitudes and perceptions regarding
successfulmodels ofcollaboration,whether clinicalor
educational,can be essentialto the value of the instruc-
tion. Grading studentparticipation willalso add value
for them.
Lastly, the training of mentors/faculty is an important
elementin the successfulinterprofessionalcurriculum.
Mentors and faculty need to feelconfidentin their
interactionswith students.The significanceof any
interprofessionalcourse needs to be shared with faculty
so they can see its importance.
Resources
An interprofessionalcurriculum requiresa significant
commitmentfrom university administration,as wellas
deans and faculty from multiple professions who must
be willing to champion the effort. Each curriculum
effort should be critically evaluated,both quantitatively
and qualitatively.In addition, we have found the
following resources to be crucialto the success ofthe
interprofessionalleaning experience.
For didactic learning experiences,consider the
following.
1. Commitment from departments and colleges to set
aside time for students to participate in the course.
2. Curricular mapping between schools can facilitate
activities.
3. Adequate rooms and facilities able to accommodate
large numbers of students,faculty,staff,and com-
munity members.
4. Creation of a space for a sense of community and
shared purpose through ice-breaking activities and
introductions.
5. Technology for web-based conferences to reach all
participants, as well as a learning system to admin-
ister course content materials and grade students.
For community-based learning experiencesfor stu-
dents, consider the following.
1. Do you have an enthusiasticcommitmentfrom
community partners?
2. Create projects which utilize a diversity ofprofes-
sions.
3. If you are using families or individuals, do you have
clear expectations as to whether this is simply an
educational experience for your students or delivery
of healthcare?
4. Are there contingencies for community participants
who become lost to follow-up?
5. Confidentiality of personal health information must
be a high priority.
6. The university must develop a community presence
so that year after year these relationships can be
strengthened and new partnerships formed.
Models of interprofessionaleducation
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035 7(page number not for citation purpose)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7. Remember thatreflection is an importantpart of
service learning programs.
If you are planning an interprofessionalsimulation
experience for students, consider the following.
1. Calendar and schedule agreement among the parti-
cipating colleges and programs.
2. Evening and weekend activity opportunities.
3. Expertiseto develop simulation experienceswith
interprofessional objectives in mind.
4. Personnel to debrief experiences.
Summary recommendations
There are several factors that are essential to the success
of interprofessional programs and activities.
1. Administrative support. Coordination of interprofessional
experiences may require significantchanges in the
curriculum structure of one or more colleges. Deans,
curriculum committees, and educational administra-
tors must be supportive of these activities.
2. Interprofessionalprogrammatic infrastructure.Fa-
culty resources are essential. Faculty members from
each college are needed to provide leadership and
recruit teaching faculty from their college, as well as
coordinating activities between colleges.Addition-
ally, administrative supportis needed to schedule
rooms,confirm mentoravailability,submitatten-
dancesand grades,and find substituteswhen
necessary.
3. Committed,experienced faculty.It takes dedicated
and educated faculty and staff to provide leadership
to student groups, whether in a didactic or a clinical
setting.
4. Acknowledge student efforts through awards,certi-
ficates, or grades.
While there are many barriers to developing successful
interprofessionallearning experiences,they can be over-
come with persistence and commitment, as demonstrated
in these examplesof successfulprograms.Given the
importance of quality care outcomes and the recognition
that collaborativepracticeimprovestheseoutcomes,
interprofessionaleducation should bea high priority
for every training instution. We hope our experiences will
guide you to develop rewarding IPE curricula for your
students.
Acknowledgements
The authorswould like to acknowledgethe Rosalind Franklin
University of Medicine and Science Curriculum Task Force; Rhond-
da Waddell PhD from the University of Florida; and the University
of Washington Center for Health Sciences Interprofessional Educa-
tion and Research and the Josiah Macy Foundation for funding
support for the University of Washington interprofessional simula-
tion research.We also acknowledgethe studentsat our three
institutions, whose buy-in and support allow IPE programs to thrive.
Conflict of interest and funding
The authors have notreceived any funding or benefits
from industry or elsewhere to conduct this study.
References
1. Lumague M, Morgan A, Mak D, Hanna M, Kwong J, Cameron
C, et al.Interprofessionaleducation:the student perspective.J
Interprof Care 2008; 20: 24653.
2. Institute of Medicine Committee on Quality of Health Care in
America. Crossing the Quality Chasm: a new health system for
the 21stcentury.Washington,DC: National Academy Press;
2001.
3. Barker K, Oandasan I. Interprofessionalcare review with
medical residents: lessons learned, tensions aired a pilot study.
J Interprof Care 2005; 19: 20714.
4. Barr H, KoppelI, Reeves S,Hammick M,Freeth D.Effective
interprofessionaleducation: argument, assumption and
evidence. Oxford: Blackwell Publishing; 2005.
5. Karim R, Ross C. Interprofessional education and chiropractic.
J Can Chiropr Assoc 2008; 52: 76678.
6. Canadian InterprofessionalHealth Collaborative.A national
interprofessional competency framework; February 2010. Avail-
able from: http://www.cihc.ca/files/CIHC_IPCompetencies_
Feb1210.pdf (cited 20 March 2010).
7. Kasperski M. Implementation strategies:‘Collaboration in
primary care family doctors and nurse practitioners delivering
shared care.’Toronto,ON: Ontario College ofFamily Physi-
cians,2000.Available from:http://www.cfpc.ca/English/CFPC/
CLFM/bibnursing/default.asp?s1 (cited 22 March 2010).
8. Roa R. Dignity and impudence:how should medicalstudents
acquire and practice clinicalskills for use with older people?
Med Educ 2003; 37: 1901.
9. Morrison S. Working together: why bother with collaboration?
Work Bas Learn Prim Care 2007; 5: 6570.
10. ZwarensteinM, Reeves S, Perrier L. Effectivenessof
pre-licensureinterprofessionaleducationand post-licensure
collaborative interventions. J Interprof Care 2005; 19: 14865.
11. Craddock D, O’Halloran C, Borthwick A, McPherson K.
Interprofessionaleducation in health and socialcare:fashion
or informed practice? Learn Health Soc Care 2006; 5: 22042.
12. Jones R. Working togetherlearning together. Occasional
Paper, J Roy Coll Gen Pract 1986; 33: 126.
13. Casto R, Nystrom E, Burgess-EllisonJ. Interprofessional
collaboration:attitudechangesamong studentsengaged in
interprofessionaleducation.In: Interdisciplinary Health Team
Care, ed. Proceedings of Seventh Annual Conference. Chicago,
IL: Center for Educational Development,University of
Chicago; 1986, pp. 20116.
14. Casto R. Pre-servicecoursesfor interprofessionalpractice.
Theory into Pract 1987; 26: 1039.
15. Young L, Baker P,Waller S,Hodgson L,Moor M. Knowing
your allies:medicaleducation and interprofessionalexposure.
J Interprof Care 2007; 21: 15563.
16. Courtnage L,Smith-Davis J.Interdisciplinary team training:a
national survey of special education teacher training programs.
Except Child 1987; 53: 4519.
17. SidelingerD, Meyer D, Blaschke G,Hametz P, Batista M,
Salguero R, et al. Communities as teachers: learning to deliver
Diane R. Bridges et al.
8(page number not for citation purpose)
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035
service learning programs.
If you are planning an interprofessionalsimulation
experience for students, consider the following.
1. Calendar and schedule agreement among the parti-
cipating colleges and programs.
2. Evening and weekend activity opportunities.
3. Expertiseto develop simulation experienceswith
interprofessional objectives in mind.
4. Personnel to debrief experiences.
Summary recommendations
There are several factors that are essential to the success
of interprofessional programs and activities.
1. Administrative support. Coordination of interprofessional
experiences may require significantchanges in the
curriculum structure of one or more colleges. Deans,
curriculum committees, and educational administra-
tors must be supportive of these activities.
2. Interprofessionalprogrammatic infrastructure.Fa-
culty resources are essential. Faculty members from
each college are needed to provide leadership and
recruit teaching faculty from their college, as well as
coordinating activities between colleges.Addition-
ally, administrative supportis needed to schedule
rooms,confirm mentoravailability,submitatten-
dancesand grades,and find substituteswhen
necessary.
3. Committed,experienced faculty.It takes dedicated
and educated faculty and staff to provide leadership
to student groups, whether in a didactic or a clinical
setting.
4. Acknowledge student efforts through awards,certi-
ficates, or grades.
While there are many barriers to developing successful
interprofessionallearning experiences,they can be over-
come with persistence and commitment, as demonstrated
in these examplesof successfulprograms.Given the
importance of quality care outcomes and the recognition
that collaborativepracticeimprovestheseoutcomes,
interprofessionaleducation should bea high priority
for every training instution. We hope our experiences will
guide you to develop rewarding IPE curricula for your
students.
Acknowledgements
The authorswould like to acknowledgethe Rosalind Franklin
University of Medicine and Science Curriculum Task Force; Rhond-
da Waddell PhD from the University of Florida; and the University
of Washington Center for Health Sciences Interprofessional Educa-
tion and Research and the Josiah Macy Foundation for funding
support for the University of Washington interprofessional simula-
tion research.We also acknowledgethe studentsat our three
institutions, whose buy-in and support allow IPE programs to thrive.
Conflict of interest and funding
The authors have notreceived any funding or benefits
from industry or elsewhere to conduct this study.
References
1. Lumague M, Morgan A, Mak D, Hanna M, Kwong J, Cameron
C, et al.Interprofessionaleducation:the student perspective.J
Interprof Care 2008; 20: 24653.
2. Institute of Medicine Committee on Quality of Health Care in
America. Crossing the Quality Chasm: a new health system for
the 21stcentury.Washington,DC: National Academy Press;
2001.
3. Barker K, Oandasan I. Interprofessionalcare review with
medical residents: lessons learned, tensions aired a pilot study.
J Interprof Care 2005; 19: 20714.
4. Barr H, KoppelI, Reeves S,Hammick M,Freeth D.Effective
interprofessionaleducation: argument, assumption and
evidence. Oxford: Blackwell Publishing; 2005.
5. Karim R, Ross C. Interprofessional education and chiropractic.
J Can Chiropr Assoc 2008; 52: 76678.
6. Canadian InterprofessionalHealth Collaborative.A national
interprofessional competency framework; February 2010. Avail-
able from: http://www.cihc.ca/files/CIHC_IPCompetencies_
Feb1210.pdf (cited 20 March 2010).
7. Kasperski M. Implementation strategies:‘Collaboration in
primary care family doctors and nurse practitioners delivering
shared care.’Toronto,ON: Ontario College ofFamily Physi-
cians,2000.Available from:http://www.cfpc.ca/English/CFPC/
CLFM/bibnursing/default.asp?s1 (cited 22 March 2010).
8. Roa R. Dignity and impudence:how should medicalstudents
acquire and practice clinicalskills for use with older people?
Med Educ 2003; 37: 1901.
9. Morrison S. Working together: why bother with collaboration?
Work Bas Learn Prim Care 2007; 5: 6570.
10. ZwarensteinM, Reeves S, Perrier L. Effectivenessof
pre-licensureinterprofessionaleducationand post-licensure
collaborative interventions. J Interprof Care 2005; 19: 14865.
11. Craddock D, O’Halloran C, Borthwick A, McPherson K.
Interprofessionaleducation in health and socialcare:fashion
or informed practice? Learn Health Soc Care 2006; 5: 22042.
12. Jones R. Working togetherlearning together. Occasional
Paper, J Roy Coll Gen Pract 1986; 33: 126.
13. Casto R, Nystrom E, Burgess-EllisonJ. Interprofessional
collaboration:attitudechangesamong studentsengaged in
interprofessionaleducation.In: Interdisciplinary Health Team
Care, ed. Proceedings of Seventh Annual Conference. Chicago,
IL: Center for Educational Development,University of
Chicago; 1986, pp. 20116.
14. Casto R. Pre-servicecoursesfor interprofessionalpractice.
Theory into Pract 1987; 26: 1039.
15. Young L, Baker P,Waller S,Hodgson L,Moor M. Knowing
your allies:medicaleducation and interprofessionalexposure.
J Interprof Care 2007; 21: 15563.
16. Courtnage L,Smith-Davis J.Interdisciplinary team training:a
national survey of special education teacher training programs.
Except Child 1987; 53: 4519.
17. SidelingerD, Meyer D, Blaschke G,Hametz P, Batista M,
Salguero R, et al. Communities as teachers: learning to deliver
Diane R. Bridges et al.
8(page number not for citation purpose)
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035
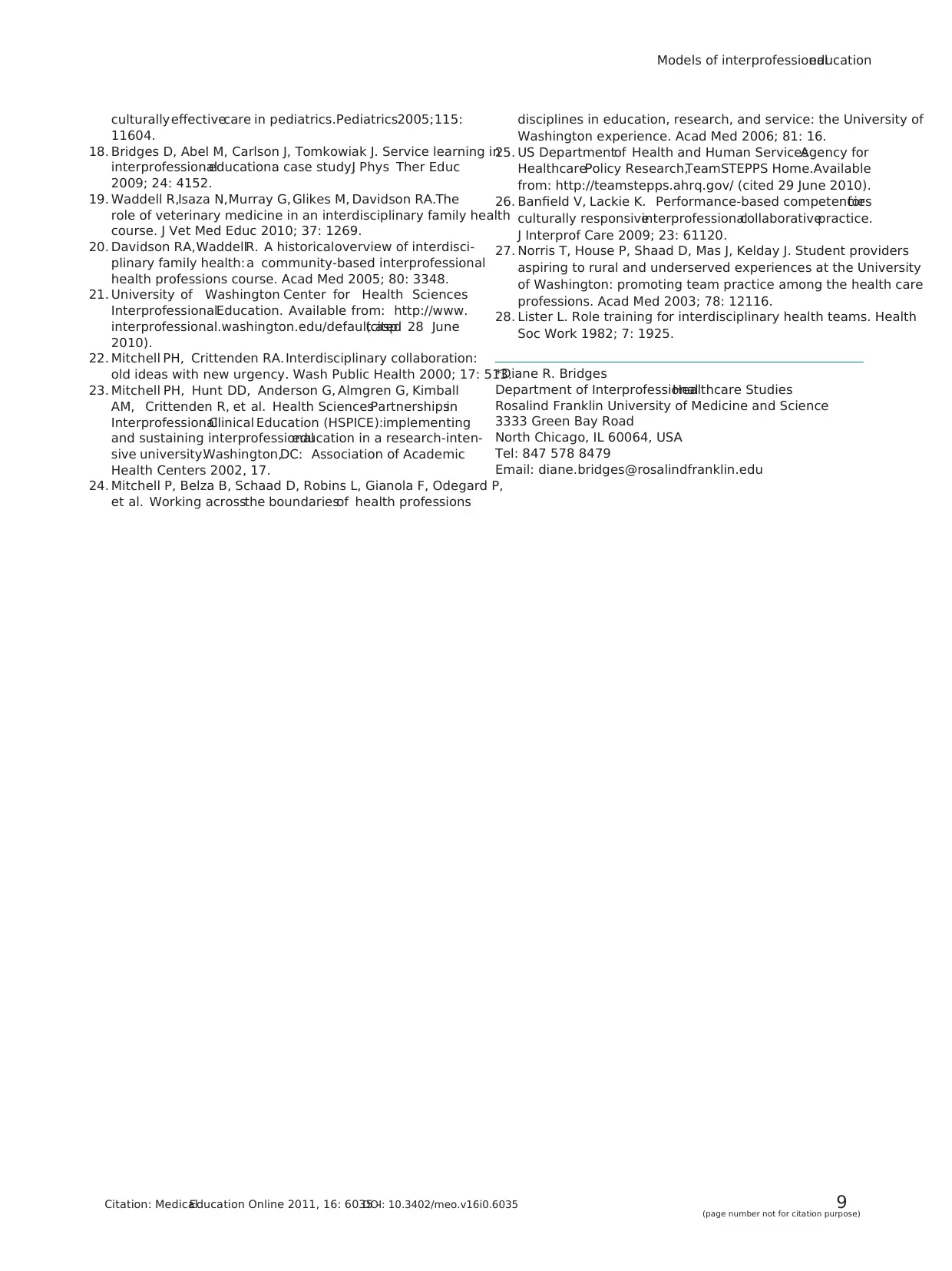
culturallyeffectivecare in pediatrics.Pediatrics2005;115:
11604.
18. Bridges D, Abel M, Carlson J, Tomkowiak J. Service learning in
interprofessionaleducation:a case study.J Phys Ther Educ
2009; 24: 4152.
19. Waddell R,Isaza N,Murray G, Glikes M, Davidson RA.The
role of veterinary medicine in an interdisciplinary family health
course. J Vet Med Educ 2010; 37: 1269.
20. Davidson RA,WaddellR. A historicaloverview of interdisci-
plinary family health: a community-based interprofessional
health professions course. Acad Med 2005; 80: 3348.
21. University of Washington Center for Health Sciences
InterprofessionalEducation. Available from: http://www.
interprofessional.washington.edu/default.asp(cited 28 June
2010).
22. Mitchell PH, Crittenden RA. Interdisciplinary collaboration:
old ideas with new urgency. Wash Public Health 2000; 17: 513.
23. Mitchell PH, Hunt DD, Anderson G, Almgren G, Kimball
AM, Crittenden R, et al. Health SciencesPartnershipsin
InterprofessionalClinical Education (HSPICE):implementing
and sustaining interprofessionaleducation in a research-inten-
sive university.Washington,DC: Association of Academic
Health Centers 2002, 17.
24. Mitchell P, Belza B, Schaad D, Robins L, Gianola F, Odegard P,
et al. Working acrossthe boundariesof health professions
disciplines in education, research, and service: the University of
Washington experience. Acad Med 2006; 81: 16.
25. US Departmentof Health and Human ServicesAgency for
HealthcarePolicy Research,TeamSTEPPS Home.Available
from: http://teamstepps.ahrq.gov/ (cited 29 June 2010).
26. Banfield V, Lackie K. Performance-based competenciesfor
culturally responsiveinterprofessionalcollaborativepractice.
J Interprof Care 2009; 23: 61120.
27. Norris T, House P, Shaad D, Mas J, Kelday J. Student providers
aspiring to rural and underserved experiences at the University
of Washington: promoting team practice among the health care
professions. Acad Med 2003; 78: 12116.
28. Lister L. Role training for interdisciplinary health teams. Health
Soc Work 1982; 7: 1925.
*Diane R. Bridges
Department of InterprofessionalHealthcare Studies
Rosalind Franklin University of Medicine and Science
3333 Green Bay Road
North Chicago, IL 60064, USA
Tel: 847 578 8479
Email: diane.bridges@rosalindfranklin.edu
Models of interprofessionaleducation
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035 9(page number not for citation purpose)
11604.
18. Bridges D, Abel M, Carlson J, Tomkowiak J. Service learning in
interprofessionaleducation:a case study.J Phys Ther Educ
2009; 24: 4152.
19. Waddell R,Isaza N,Murray G, Glikes M, Davidson RA.The
role of veterinary medicine in an interdisciplinary family health
course. J Vet Med Educ 2010; 37: 1269.
20. Davidson RA,WaddellR. A historicaloverview of interdisci-
plinary family health: a community-based interprofessional
health professions course. Acad Med 2005; 80: 3348.
21. University of Washington Center for Health Sciences
InterprofessionalEducation. Available from: http://www.
interprofessional.washington.edu/default.asp(cited 28 June
2010).
22. Mitchell PH, Crittenden RA. Interdisciplinary collaboration:
old ideas with new urgency. Wash Public Health 2000; 17: 513.
23. Mitchell PH, Hunt DD, Anderson G, Almgren G, Kimball
AM, Crittenden R, et al. Health SciencesPartnershipsin
InterprofessionalClinical Education (HSPICE):implementing
and sustaining interprofessionaleducation in a research-inten-
sive university.Washington,DC: Association of Academic
Health Centers 2002, 17.
24. Mitchell P, Belza B, Schaad D, Robins L, Gianola F, Odegard P,
et al. Working acrossthe boundariesof health professions
disciplines in education, research, and service: the University of
Washington experience. Acad Med 2006; 81: 16.
25. US Departmentof Health and Human ServicesAgency for
HealthcarePolicy Research,TeamSTEPPS Home.Available
from: http://teamstepps.ahrq.gov/ (cited 29 June 2010).
26. Banfield V, Lackie K. Performance-based competenciesfor
culturally responsiveinterprofessionalcollaborativepractice.
J Interprof Care 2009; 23: 61120.
27. Norris T, House P, Shaad D, Mas J, Kelday J. Student providers
aspiring to rural and underserved experiences at the University
of Washington: promoting team practice among the health care
professions. Acad Med 2003; 78: 12116.
28. Lister L. Role training for interdisciplinary health teams. Health
Soc Work 1982; 7: 1925.
*Diane R. Bridges
Department of InterprofessionalHealthcare Studies
Rosalind Franklin University of Medicine and Science
3333 Green Bay Road
North Chicago, IL 60064, USA
Tel: 847 578 8479
Email: diane.bridges@rosalindfranklin.edu
Models of interprofessionaleducation
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035 9(page number not for citation purpose)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
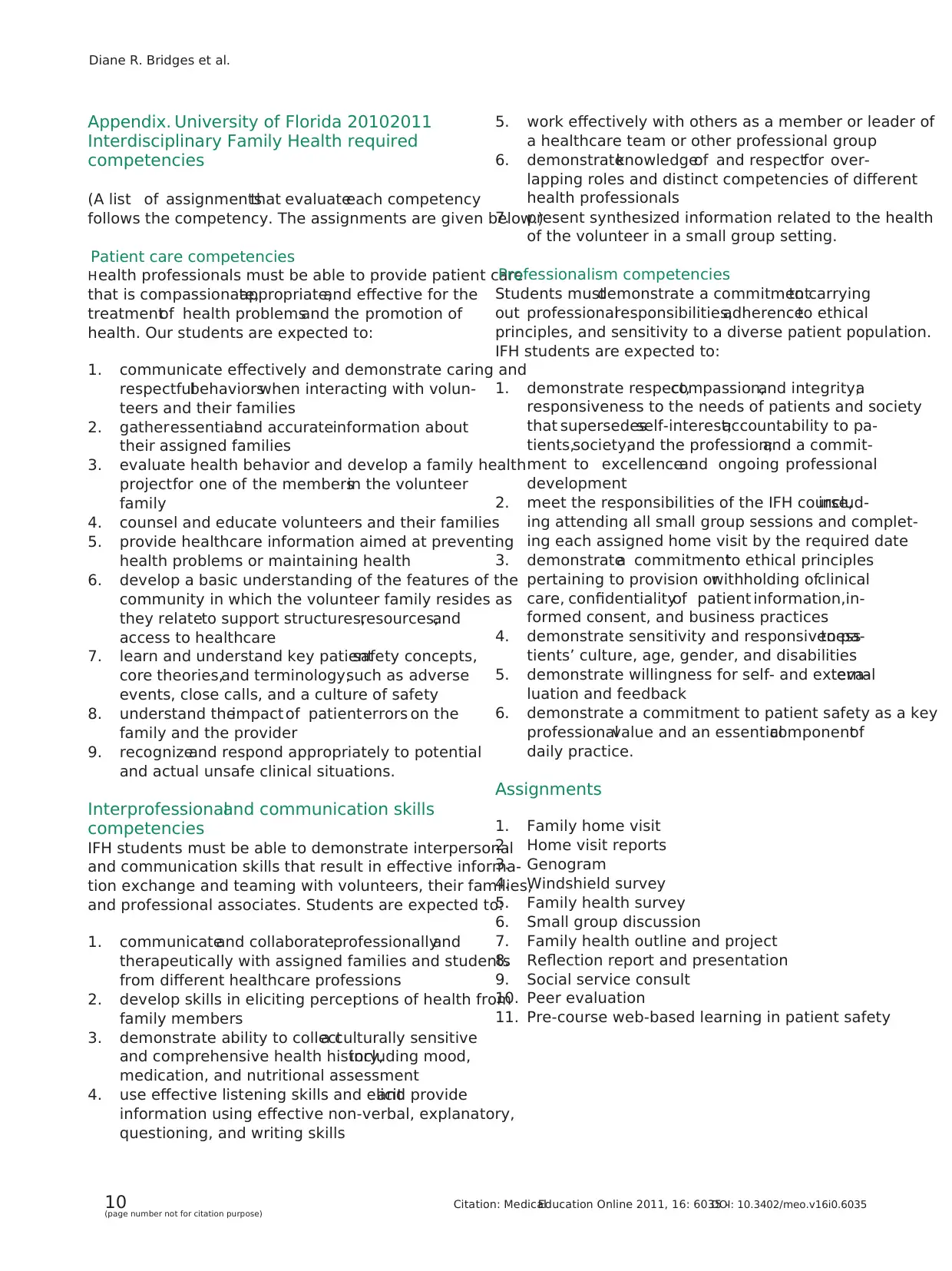
Appendix. University of Florida 20102011
Interdisciplinary Family Health required
competencies
(A list of assignmentsthat evaluateeach competency
follows the competency. The assignments are given below.)
Patient care competencies
Health professionals must be able to provide patient care
that is compassionate,appropriate,and effective for the
treatmentof health problemsand the promotion of
health. Our students are expected to:
1. communicate effectively and demonstrate caring and
respectfulbehaviorswhen interacting with volun-
teers and their families
2. gatheressentialand accurateinformation about
their assigned families
3. evaluate health behavior and develop a family health
projectfor one of the membersin the volunteer
family
4. counsel and educate volunteers and their families
5. provide healthcare information aimed at preventing
health problems or maintaining health
6. develop a basic understanding of the features of the
community in which the volunteer family resides as
they relateto support structures,resources,and
access to healthcare
7. learn and understand key patientsafety concepts,
core theories,and terminology,such as adverse
events, close calls, and a culture of safety
8. understand theimpact of patienterrors on the
family and the provider
9. recognizeand respond appropriately to potential
and actual unsafe clinical situations.
Interprofessionaland communication skills
competencies
IFH students must be able to demonstrate interpersonal
and communication skills that result in effective informa-
tion exchange and teaming with volunteers, their families,
and professional associates. Students are expected to:
1. communicateand collaborateprofessionallyand
therapeutically with assigned families and students
from different healthcare professions
2. develop skills in eliciting perceptions of health from
family members
3. demonstrate ability to collecta culturally sensitive
and comprehensive health history,including mood,
medication, and nutritional assessment
4. use effective listening skills and elicitand provide
information using effective non-verbal, explanatory,
questioning, and writing skills
5. work effectively with others as a member or leader of
a healthcare team or other professional group
6. demonstrateknowledgeof and respectfor over-
lapping roles and distinct competencies of different
health professionals
7. present synthesized information related to the health
of the volunteer in a small group setting.
Professionalism competencies
Students mustdemonstrate a commitmentto carrying
out professionalresponsibilities,adherenceto ethical
principles, and sensitivity to a diverse patient population.
IFH students are expected to:
1. demonstrate respect,compassion,and integrity;a
responsiveness to the needs of patients and society
that supersedesself-interest;accountability to pa-
tients,society,and the profession;and a commit-
ment to excellenceand ongoing professional
development
2. meet the responsibilities of the IFH course,includ-
ing attending all small group sessions and complet-
ing each assigned home visit by the required date
3. demonstratea commitmentto ethical principles
pertaining to provision orwithholding ofclinical
care, confidentialityof patient information,in-
formed consent, and business practices
4. demonstrate sensitivity and responsivenessto pa-
tients’ culture, age, gender, and disabilities
5. demonstrate willingness for self- and externaleva-
luation and feedback
6. demonstrate a commitment to patient safety as a key
professionalvalue and an essentialcomponentof
daily practice.
Assignments
1. Family home visit
2. Home visit reports
3. Genogram
4. Windshield survey
5. Family health survey
6. Small group discussion
7. Family health outline and project
8. Reflection report and presentation
9. Social service consult
10. Peer evaluation
11. Pre-course web-based learning in patient safety
Diane R. Bridges et al.
10(page number not for citation purpose)
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035
Interdisciplinary Family Health required
competencies
(A list of assignmentsthat evaluateeach competency
follows the competency. The assignments are given below.)
Patient care competencies
Health professionals must be able to provide patient care
that is compassionate,appropriate,and effective for the
treatmentof health problemsand the promotion of
health. Our students are expected to:
1. communicate effectively and demonstrate caring and
respectfulbehaviorswhen interacting with volun-
teers and their families
2. gatheressentialand accurateinformation about
their assigned families
3. evaluate health behavior and develop a family health
projectfor one of the membersin the volunteer
family
4. counsel and educate volunteers and their families
5. provide healthcare information aimed at preventing
health problems or maintaining health
6. develop a basic understanding of the features of the
community in which the volunteer family resides as
they relateto support structures,resources,and
access to healthcare
7. learn and understand key patientsafety concepts,
core theories,and terminology,such as adverse
events, close calls, and a culture of safety
8. understand theimpact of patienterrors on the
family and the provider
9. recognizeand respond appropriately to potential
and actual unsafe clinical situations.
Interprofessionaland communication skills
competencies
IFH students must be able to demonstrate interpersonal
and communication skills that result in effective informa-
tion exchange and teaming with volunteers, their families,
and professional associates. Students are expected to:
1. communicateand collaborateprofessionallyand
therapeutically with assigned families and students
from different healthcare professions
2. develop skills in eliciting perceptions of health from
family members
3. demonstrate ability to collecta culturally sensitive
and comprehensive health history,including mood,
medication, and nutritional assessment
4. use effective listening skills and elicitand provide
information using effective non-verbal, explanatory,
questioning, and writing skills
5. work effectively with others as a member or leader of
a healthcare team or other professional group
6. demonstrateknowledgeof and respectfor over-
lapping roles and distinct competencies of different
health professionals
7. present synthesized information related to the health
of the volunteer in a small group setting.
Professionalism competencies
Students mustdemonstrate a commitmentto carrying
out professionalresponsibilities,adherenceto ethical
principles, and sensitivity to a diverse patient population.
IFH students are expected to:
1. demonstrate respect,compassion,and integrity;a
responsiveness to the needs of patients and society
that supersedesself-interest;accountability to pa-
tients,society,and the profession;and a commit-
ment to excellenceand ongoing professional
development
2. meet the responsibilities of the IFH course,includ-
ing attending all small group sessions and complet-
ing each assigned home visit by the required date
3. demonstratea commitmentto ethical principles
pertaining to provision orwithholding ofclinical
care, confidentialityof patient information,in-
formed consent, and business practices
4. demonstrate sensitivity and responsivenessto pa-
tients’ culture, age, gender, and disabilities
5. demonstrate willingness for self- and externaleva-
luation and feedback
6. demonstrate a commitment to patient safety as a key
professionalvalue and an essentialcomponentof
daily practice.
Assignments
1. Family home visit
2. Home visit reports
3. Genogram
4. Windshield survey
5. Family health survey
6. Small group discussion
7. Family health outline and project
8. Reflection report and presentation
9. Social service consult
10. Peer evaluation
11. Pre-course web-based learning in patient safety
Diane R. Bridges et al.
10(page number not for citation purpose)
Citation: MedicalEducation Online 2011, 16: 6035 -DOI: 10.3402/meo.v16i0.6035
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Copyright of Medical Education Online is the property of Co-Action Publishing and its content may not be
copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written
permission. However, users may print, download, or email articles for individual use.
copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written
permission. However, users may print, download, or email articles for individual use.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




