IoT in Telemedicine: Supporting Healthcare Delivery through Technology
VerifiedAdded on 2023/06/04
|14
|3428
|377
AI Summary
This article explores the impact of IoT on Telemedicine, its applications, challenges, and proposed solutions. It discusses how technology is supporting healthcare delivery through Telemedicine and the benefits it offers to patients and healthcare providers. The article also highlights the challenges faced in implementing Telemedicine and proposes solutions to overcome them.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

IoT in Telemedicine
Name
Institution
Professor
Course
Date
Name
Institution
Professor
Course
Date
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Executive Summary
Medical industry has been influenced by technological innovation through adoption of
Telemedicine. This is a medicine based technology which enables patients to access healthcare
services over the Internet of Things (IoT). Through use of Telemedicine, state governments are
able to increase healthcare delivery. Several application technologies such as mobile apps,
websites as well as messages and alerts are being used to support Telemedicine. Besides
technology, IoT support Telemedicine through use of tools such as wireless sensors, RFID and
Health Cards among others. Despite benefits realized from Telemedicine in conjunction with
IoT, there are some challenges that hinder its implementation. These issues are; security and
privacy of data, payment parity, widespread implementation of Telemedicine and misdiagnosis.
From the study, it has been observed that most states have Telemedicine services. However,
most of Telemedicine services from some states are poor while others are performing
excellently. Solutions to Telemedicine issues involves educating people on importance of online
medical services and enacting rules and regulations that govern Telemedicine operations.
Introduction
Technological innovations have made modern world more advanced than ever and almost
every industry has been affected. With almost every aspect of life is going online, it is now
possible to use Telemedicine to monitor patient conditions with help of advanced technologies
related to Internet of Things (IoT). Through use of IoT, it has been possible to construct a
patient-centric applications to facilitate remote medical consultation as well as monitoring
services meant to help patients with critical conditions (Mora et al., 2017). Some patients require
continuous monitoring with frequent visits to hospitals. To minimize number of visits to the
hospital, Telemedicine was introduced with aim of reducing congestions in hospitals when some
Medical industry has been influenced by technological innovation through adoption of
Telemedicine. This is a medicine based technology which enables patients to access healthcare
services over the Internet of Things (IoT). Through use of Telemedicine, state governments are
able to increase healthcare delivery. Several application technologies such as mobile apps,
websites as well as messages and alerts are being used to support Telemedicine. Besides
technology, IoT support Telemedicine through use of tools such as wireless sensors, RFID and
Health Cards among others. Despite benefits realized from Telemedicine in conjunction with
IoT, there are some challenges that hinder its implementation. These issues are; security and
privacy of data, payment parity, widespread implementation of Telemedicine and misdiagnosis.
From the study, it has been observed that most states have Telemedicine services. However,
most of Telemedicine services from some states are poor while others are performing
excellently. Solutions to Telemedicine issues involves educating people on importance of online
medical services and enacting rules and regulations that govern Telemedicine operations.
Introduction
Technological innovations have made modern world more advanced than ever and almost
every industry has been affected. With almost every aspect of life is going online, it is now
possible to use Telemedicine to monitor patient conditions with help of advanced technologies
related to Internet of Things (IoT). Through use of IoT, it has been possible to construct a
patient-centric applications to facilitate remote medical consultation as well as monitoring
services meant to help patients with critical conditions (Mora et al., 2017). Some patients require
continuous monitoring with frequent visits to hospitals. To minimize number of visits to the
hospital, Telemedicine was introduced with aim of reducing congestions in hospitals when some
of these patients does not require them. Telemedicine has been undergoing some advancements
and with help of sensors to monitor changes in patient’s body in real-time, it actually gives a
relief to both patients and doctors. Apart from monitoring patients to improve their lifestyle,
Telemedicine can provide lifesaving information as well as related educational programs on
medicine. To achieve Telemedicine goals, patient’s data is collected through implanted body
sensors and transmitted over the internet (Lazarev, 2016). Important to note is that, number of
patients have been quite high than available doctors required to treat acute diseases. To make
sure all patients receive services on timely manner, virtual doctor consultation through
Telemedicine has been of great help. Few experts from recognized health facilities are able to
serve a bigger number of patients across the globe. Therefore, technology in medical industry has
made it possible to extend quality medical services by providing continuous medical support and
educational programs (Kenganal & Rengaprabhu, 2016).
Application of technology
It is obvious that the backbone of Telemedicine is technology because all its aspects
should be run over the internet with help of some tools. Some of these technology tools that
support Telemedicine are; websites with medical information where patients can access
healthcare information, create accounts in order to contact available doctors, provide patients
feedback from analyzing provided symptoms and payment for services received. The next
technology involves mobile apps which help people to monitor their health by tracking
individual diet, heart rate and blood pressure (Sermakani, 2014). Additionally, patients are able
to receive their health status through alerts and notifications. System users are required to either
signup or subscribe to some alerts which would be generated automatically by system once a
certain condition has been detected by the system. Such alerts would be accompanied by
and with help of sensors to monitor changes in patient’s body in real-time, it actually gives a
relief to both patients and doctors. Apart from monitoring patients to improve their lifestyle,
Telemedicine can provide lifesaving information as well as related educational programs on
medicine. To achieve Telemedicine goals, patient’s data is collected through implanted body
sensors and transmitted over the internet (Lazarev, 2016). Important to note is that, number of
patients have been quite high than available doctors required to treat acute diseases. To make
sure all patients receive services on timely manner, virtual doctor consultation through
Telemedicine has been of great help. Few experts from recognized health facilities are able to
serve a bigger number of patients across the globe. Therefore, technology in medical industry has
made it possible to extend quality medical services by providing continuous medical support and
educational programs (Kenganal & Rengaprabhu, 2016).
Application of technology
It is obvious that the backbone of Telemedicine is technology because all its aspects
should be run over the internet with help of some tools. Some of these technology tools that
support Telemedicine are; websites with medical information where patients can access
healthcare information, create accounts in order to contact available doctors, provide patients
feedback from analyzing provided symptoms and payment for services received. The next
technology involves mobile apps which help people to monitor their health by tracking
individual diet, heart rate and blood pressure (Sermakani, 2014). Additionally, patients are able
to receive their health status through alerts and notifications. System users are required to either
signup or subscribe to some alerts which would be generated automatically by system once a
certain condition has been detected by the system. Such alerts would be accompanied by
recommendations on required preventive care, vaccines available and medications to take.
Besides, telemedicine is also supported by some other technologies to enforce required data
protection and confidentiality. Telemedicine is supported by both live video and audio
conferencing with patients to get required explanation and recommendations for treatment
(Zhang & Xu, 2012). Since communication would involve revealing personal information on
illness which should be kept confidential, privacy security has to be enforced.
Additionally, according to Sermakani (2014), there are special telemedicine equipment
that have been designed to facilitate secure patient monitoring. These remote tools and
equipment help service providers to collect important information about specific illness from
several patients for a long period of time without making single on-site patient visit. These tools
help doctors to monitor and control patient chronic illness such as; blood pressure, heart rate,
blood sugar and temperature among other signs. Majorly, these tools are being used to monitor
home based patients and elderly people who stay on their own. Due to nature of the age, they
require special health observation. Since it is challenging for them to take some advanced
precautionary measures, telemedicine technologies becomes an important part of their lives
(Castro et al., 2017). Once doctor receives an alert from the implanted equipment, immediate
actions such as visiting the patient at home or calling an on-site team to attend the patient should
be prioritized.
Besides, telemedicine is also supported by some other technologies to enforce required data
protection and confidentiality. Telemedicine is supported by both live video and audio
conferencing with patients to get required explanation and recommendations for treatment
(Zhang & Xu, 2012). Since communication would involve revealing personal information on
illness which should be kept confidential, privacy security has to be enforced.
Additionally, according to Sermakani (2014), there are special telemedicine equipment
that have been designed to facilitate secure patient monitoring. These remote tools and
equipment help service providers to collect important information about specific illness from
several patients for a long period of time without making single on-site patient visit. These tools
help doctors to monitor and control patient chronic illness such as; blood pressure, heart rate,
blood sugar and temperature among other signs. Majorly, these tools are being used to monitor
home based patients and elderly people who stay on their own. Due to nature of the age, they
require special health observation. Since it is challenging for them to take some advanced
precautionary measures, telemedicine technologies becomes an important part of their lives
(Castro et al., 2017). Once doctor receives an alert from the implanted equipment, immediate
actions such as visiting the patient at home or calling an on-site team to attend the patient should
be prioritized.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
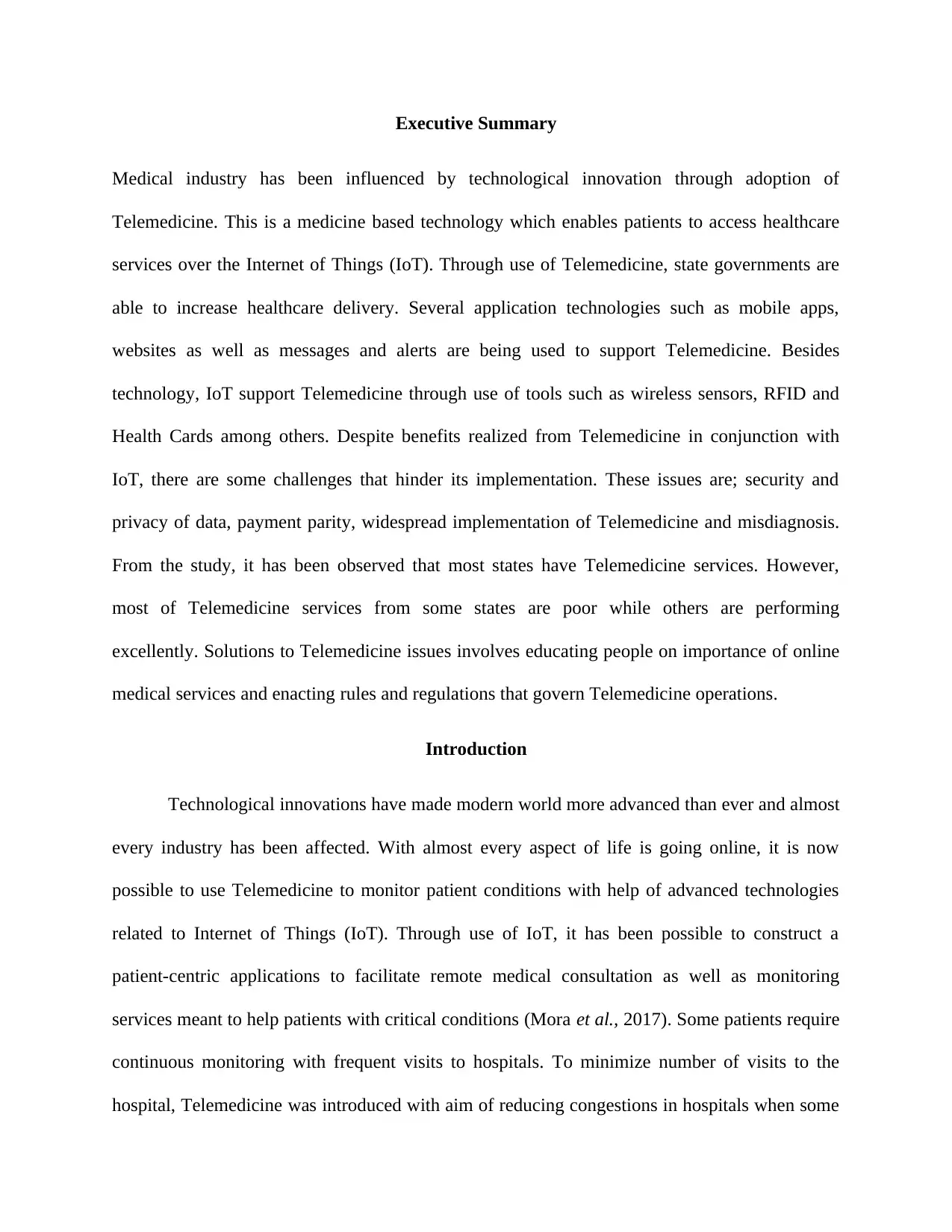
Figure 1: Telemedicine implementation
Internet of Things Technology and Telemedicine
Several technologies are in place to support Telemedicine through IoT. Applications from
medical industry has proved to be the key drivers of the entire process. These applications makes
it possible to monitor and send data from a specific patient to the doctor. These technologies are
meant to either make life simple to patients or provide them with valuable information regarding
their health status (Lazarev, 2016). Without these applications which support Telemedicine,
patients are not able to access required services remotely. In order for these applications to work
effectively, they need to connect online to facilitate required communication. These applications
should be able to integrate smoothly and support each other to deliver required services. These
applications are; smart wheelchair, RFID wristbands and GPS positioning and Health ID cards.
Smart Wheelchair
Smart Wheelchair Applications was introduced to support patient movement from one
location to the other. The use of smart Wheelchair should be able to get and accept desirable user
instructions, navigation routes and obstacle avoidance. Smart Wheelchair involves collaboration
Internet of Things Technology and Telemedicine
Several technologies are in place to support Telemedicine through IoT. Applications from
medical industry has proved to be the key drivers of the entire process. These applications makes
it possible to monitor and send data from a specific patient to the doctor. These technologies are
meant to either make life simple to patients or provide them with valuable information regarding
their health status (Lazarev, 2016). Without these applications which support Telemedicine,
patients are not able to access required services remotely. In order for these applications to work
effectively, they need to connect online to facilitate required communication. These applications
should be able to integrate smoothly and support each other to deliver required services. These
applications are; smart wheelchair, RFID wristbands and GPS positioning and Health ID cards.
Smart Wheelchair
Smart Wheelchair Applications was introduced to support patient movement from one
location to the other. The use of smart Wheelchair should be able to get and accept desirable user
instructions, navigation routes and obstacle avoidance. Smart Wheelchair involves collaboration
from all its actors in order to function accordingly. The design of the Smart Wheelchair should
factor out several aspects such as comfort of the user, ease of operating the chair, safety while on
movement and applicable design modules (Federation of State Medical Boards, 2014). Smart
Wheelchair user should have different modules to help users choose various user module
depending on user disability. It is important that, user modules be removable as well as
replaceable with a goal of changing the design as disability advances either positively or
negatively. General functioning of the smart wheelchair is divided into various modules such as
controls functions, human-computer interaction and driving functions among others. The
functional analysis and modularization can be compressed to come up with only three modules;
the sensor, drive control and human interface. The sensor is made up of two other sub-
components; the internal state perception which coordinates all required operations of the
system. The other sensor module is environmental perception meant to perceive changes in some
factors such as weather conditions that are harmful and alert the user (Mahmood et al., 2012).
Combination of multiple modules that makes up the wheel chair should coordinate effectively to
facilitate smooth functioning.
RFID Wristbands
It is an obvious understanding that, each patient would most likely want to be treated by
an expert but not just a mere doctor. With this believe and ever increasing number of patient,
doctors would not be enough. To solve the menace of long queues of patients waiting to be
attended by a single doctor, doctor’s experience can be turned into database accessible by
millions of people at an instance (Jacob & Ramani, 2012). Once this experience is accumulated
in form database, other junior doctors are able to use it as a reference when attending to patients.
factor out several aspects such as comfort of the user, ease of operating the chair, safety while on
movement and applicable design modules (Federation of State Medical Boards, 2014). Smart
Wheelchair user should have different modules to help users choose various user module
depending on user disability. It is important that, user modules be removable as well as
replaceable with a goal of changing the design as disability advances either positively or
negatively. General functioning of the smart wheelchair is divided into various modules such as
controls functions, human-computer interaction and driving functions among others. The
functional analysis and modularization can be compressed to come up with only three modules;
the sensor, drive control and human interface. The sensor is made up of two other sub-
components; the internal state perception which coordinates all required operations of the
system. The other sensor module is environmental perception meant to perceive changes in some
factors such as weather conditions that are harmful and alert the user (Mahmood et al., 2012).
Combination of multiple modules that makes up the wheel chair should coordinate effectively to
facilitate smooth functioning.
RFID Wristbands
It is an obvious understanding that, each patient would most likely want to be treated by
an expert but not just a mere doctor. With this believe and ever increasing number of patient,
doctors would not be enough. To solve the menace of long queues of patients waiting to be
attended by a single doctor, doctor’s experience can be turned into database accessible by
millions of people at an instance (Jacob & Ramani, 2012). Once this experience is accumulated
in form database, other junior doctors are able to use it as a reference when attending to patients.
Important to note is that database experience would help doctors to distribute their experience for
use by both patients as well as junior medical practitioner. With this type of the system coupled
with pool of data to reference from, it would be possible for patients to get automatic diagnosis
without experts need (Shen et al., 2016). In order to make these database work effectively,
adequate amount of expertise data is collected, this form of data is collected to form operational
data indictors which in turn generate database model. A good example can be deduced from
databases where data indicators has 500 cases of treating leukemia, the database would have the
same number of available solutions to treat the disease (Alur et al., 2016). Eventually, the nature
of database would be transformed into applications which can run on mobile phones, hence
increasing treatment mobility. In cases where application cannot evaluate exact match of the
treatment, a human doctor can be called to take up the matter for advanced and controlled
analysis. This is an indication that with time, all people would be having their private robotic
doctor accessible from anywhere and at any time from mobile phones.
Issues and challenges of IoT in Telemedicine
Technology seems to be a solution to traditional health problems but important to note is
that telemedicine presents its challenges as well. Healthcare cost has been ballooning rapidly
forcing patients to take some measures in order to contain their situations without need to visit
healthcare practitioner (Jacob & Ramani, 2012). There is existence of payment parity as there is
no guarantee of parity between on-site healthcare and telemedicine. Even though there are some
laws enacted by states to control healthcare costs, no working parameters has been set to enforce
the same. Next, telemedicine has been facing misdiagnosis issues due to close context of data
presented by patient. Patients fails to provide the exact symptoms which in turn results to wrong
treatment. Wrong prescription many also result to other diseases. Hence, complicating patients’
use by both patients as well as junior medical practitioner. With this type of the system coupled
with pool of data to reference from, it would be possible for patients to get automatic diagnosis
without experts need (Shen et al., 2016). In order to make these database work effectively,
adequate amount of expertise data is collected, this form of data is collected to form operational
data indictors which in turn generate database model. A good example can be deduced from
databases where data indicators has 500 cases of treating leukemia, the database would have the
same number of available solutions to treat the disease (Alur et al., 2016). Eventually, the nature
of database would be transformed into applications which can run on mobile phones, hence
increasing treatment mobility. In cases where application cannot evaluate exact match of the
treatment, a human doctor can be called to take up the matter for advanced and controlled
analysis. This is an indication that with time, all people would be having their private robotic
doctor accessible from anywhere and at any time from mobile phones.
Issues and challenges of IoT in Telemedicine
Technology seems to be a solution to traditional health problems but important to note is
that telemedicine presents its challenges as well. Healthcare cost has been ballooning rapidly
forcing patients to take some measures in order to contain their situations without need to visit
healthcare practitioner (Jacob & Ramani, 2012). There is existence of payment parity as there is
no guarantee of parity between on-site healthcare and telemedicine. Even though there are some
laws enacted by states to control healthcare costs, no working parameters has been set to enforce
the same. Next, telemedicine has been facing misdiagnosis issues due to close context of data
presented by patient. Patients fails to provide the exact symptoms which in turn results to wrong
treatment. Wrong prescription many also result to other diseases. Hence, complicating patients’
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
health which in turn may result to higher treatment costs Majumder et al., 2017). The third issue
associated with telemedicine is its widespread implementation. Since telemedicine is being
offered in many forms, state governments have been unable to control the quality of services.
Other challenges are financial constraints when state governments want to implement specific
type of Telemedicine in order to diversify health services to its citizens.
The fourth issues is on Telemedicine vendors as it is quite difficult to quantify the
number of authorized vendors. On the same note, vendors may incur substantial costs but state
governments do not bother to compensate them when such a program becomes fruitful.
Moreover, security and privacy concerns of data shared over the internet has been of great
concern because health matters should not be taken lightly. Kim (2014) argues that health
records are considered matters of patient and doctor only. Personal health status should not be
shared without consent from patient. Finally, it is quite difficult to provide Telemedicine as one
package incases they are required by patient. Some patients require dentists, insurance services,
cardiologist and other specialists at an instance. With Telemedicine, it is quite difficult to have
this package from one provider.
Related work
For over 30 years, Telemedicine has been on existence but advancements have been
made to make it more established. Health sector has been lagging behind in technology adoption
but remarkable trends have been noticed within few years. To make Telemedicine more efficient,
it has to be a two way structure that facilitates communication between patient and healthcare
providers (Davey & Davey, 2014). Adoption of technology in healthcare has made it possible for
patients to get health services from distant health practitioners. Important to note is that
telemedicine practitioners are subject to state laws which is government’s effort to control the
associated with telemedicine is its widespread implementation. Since telemedicine is being
offered in many forms, state governments have been unable to control the quality of services.
Other challenges are financial constraints when state governments want to implement specific
type of Telemedicine in order to diversify health services to its citizens.
The fourth issues is on Telemedicine vendors as it is quite difficult to quantify the
number of authorized vendors. On the same note, vendors may incur substantial costs but state
governments do not bother to compensate them when such a program becomes fruitful.
Moreover, security and privacy concerns of data shared over the internet has been of great
concern because health matters should not be taken lightly. Kim (2014) argues that health
records are considered matters of patient and doctor only. Personal health status should not be
shared without consent from patient. Finally, it is quite difficult to provide Telemedicine as one
package incases they are required by patient. Some patients require dentists, insurance services,
cardiologist and other specialists at an instance. With Telemedicine, it is quite difficult to have
this package from one provider.
Related work
For over 30 years, Telemedicine has been on existence but advancements have been
made to make it more established. Health sector has been lagging behind in technology adoption
but remarkable trends have been noticed within few years. To make Telemedicine more efficient,
it has to be a two way structure that facilitates communication between patient and healthcare
providers (Davey & Davey, 2014). Adoption of technology in healthcare has made it possible for
patients to get health services from distant health practitioners. Important to note is that
telemedicine practitioners are subject to state laws which is government’s effort to control the
quality of health services provided to citizens. Despite technology requirement set up to provide
Telemedicine, state laws advocates for equal rates as if health service had been provided at on-
site. This has been introduced by state governments to control the cost of treatment. Most of the
states have Telemedicine but the quality of services offered differ substantially (Lin &
Bergmann, 2016). A research was done on all states and it was found that, though there is
disparity on cost and quality of services offered, the score was an average of B+. Since
Telemedicine are payable by individuals, some reimbursements are made by Medicare. It has
been observed that, Telemedicine has some share in the market and many people have adopted it
for treatment (Davey & Davey, 2014). Some of the key player in Telemedicine are; Philips
Healthcare, IBm and Siemens Healthcare among others.
Proposed solutions
Some of the solutions to issues faced in Telemedicine implementations are; educating
people on benefits and challenges of Telemedicine. Once all parameters are clear, it would be
very easy for an individual to decide if the illness require on-site doctor or Telemedicine doctor
(Babu, & Jayashree, 2016). Payment parity can be resolved through strict state government
regulation in order to prevent citizens from manipulation. Additionally, Misdiagnosis can be
resolved by developing artificial intelligence and defining clear statements during machine
learning process. Widespread implementation can be solved through government legislation to
approve vendors willing to invest in Telemedicine.
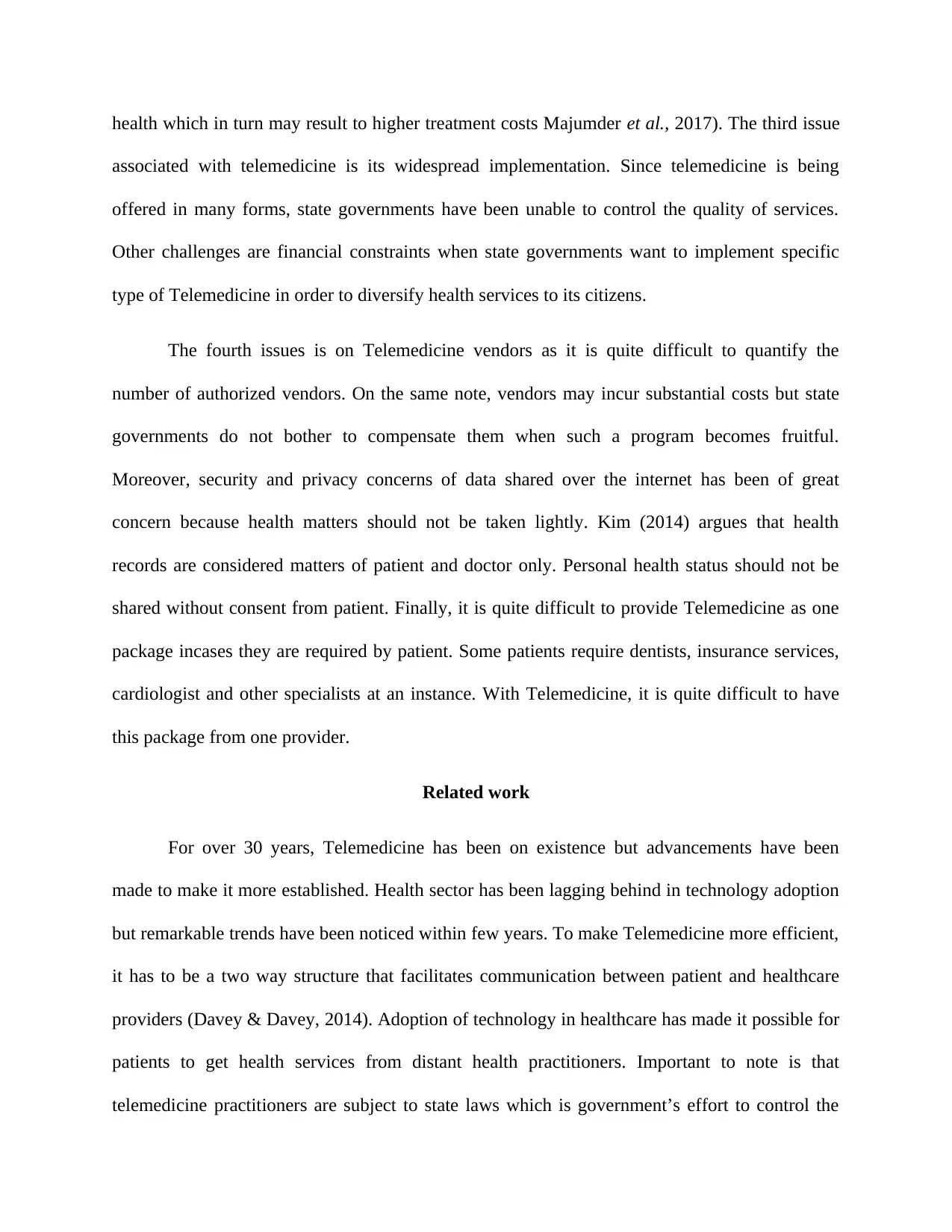
Experimental analysis
There is no doubt that number of users getting health services through Telemedicine has
been increasing over time. From year 2012-2018, the number has been increasing as well as
Telemedicine, state laws advocates for equal rates as if health service had been provided at on-
site. This has been introduced by state governments to control the cost of treatment. Most of the
states have Telemedicine but the quality of services offered differ substantially (Lin &
Bergmann, 2016). A research was done on all states and it was found that, though there is
disparity on cost and quality of services offered, the score was an average of B+. Since
Telemedicine are payable by individuals, some reimbursements are made by Medicare. It has
been observed that, Telemedicine has some share in the market and many people have adopted it
for treatment (Davey & Davey, 2014). Some of the key player in Telemedicine are; Philips
Healthcare, IBm and Siemens Healthcare among others.
Proposed solutions
Some of the solutions to issues faced in Telemedicine implementations are; educating
people on benefits and challenges of Telemedicine. Once all parameters are clear, it would be
very easy for an individual to decide if the illness require on-site doctor or Telemedicine doctor
(Babu, & Jayashree, 2016). Payment parity can be resolved through strict state government
regulation in order to prevent citizens from manipulation. Additionally, Misdiagnosis can be
resolved by developing artificial intelligence and defining clear statements during machine
learning process. Widespread implementation can be solved through government legislation to
approve vendors willing to invest in Telemedicine.
Experimental analysis
There is no doubt that number of users getting health services through Telemedicine has
been increasing over time. From year 2012-2018, the number has been increasing as well as
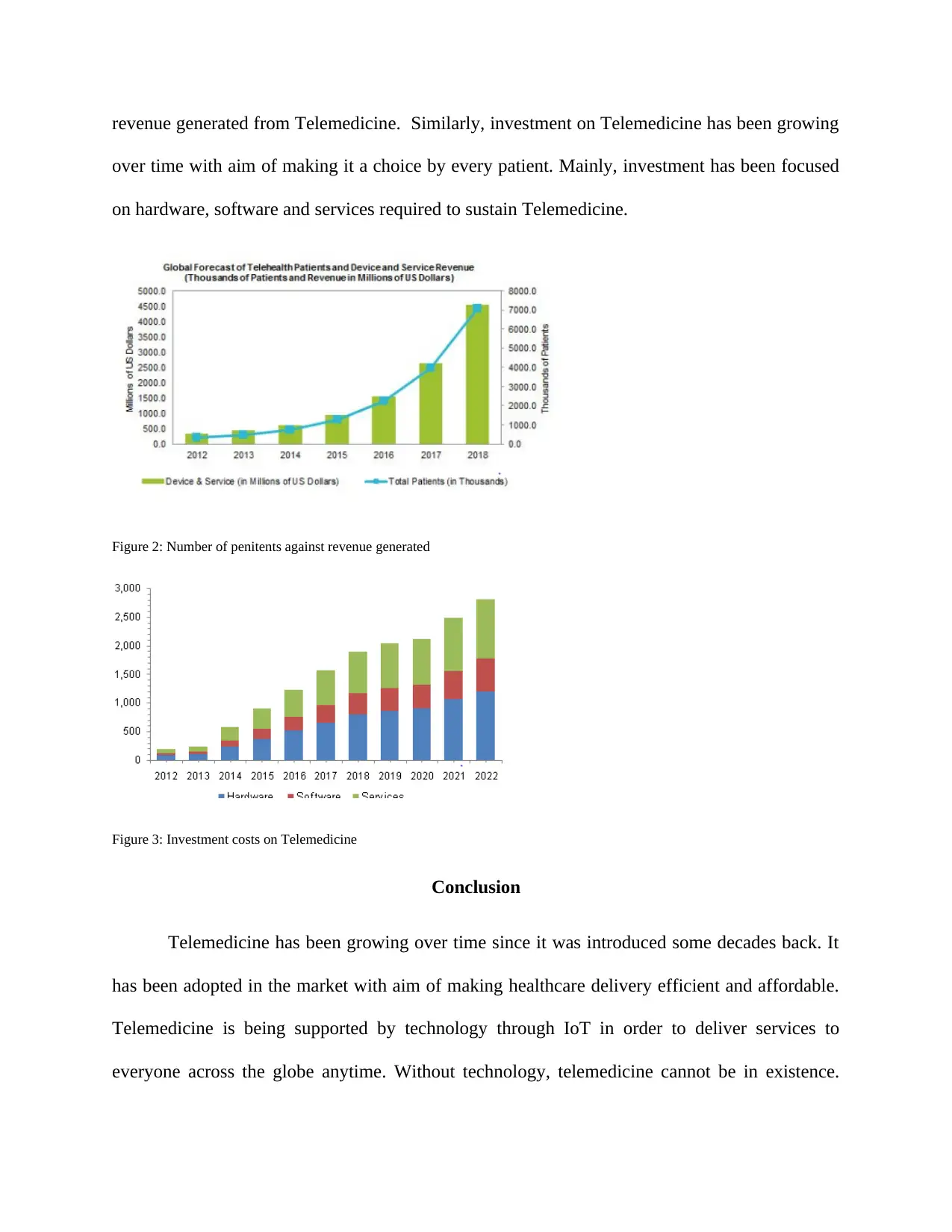
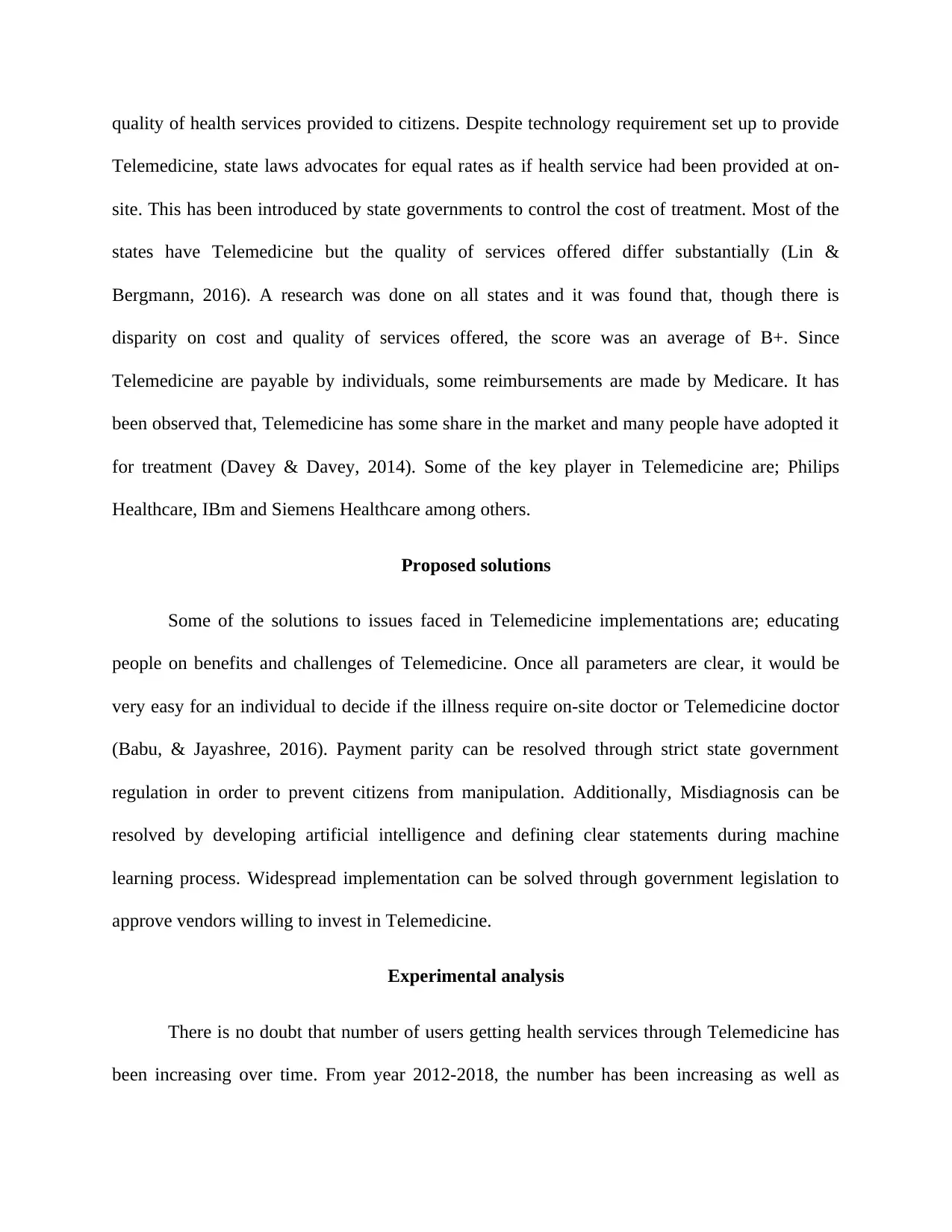
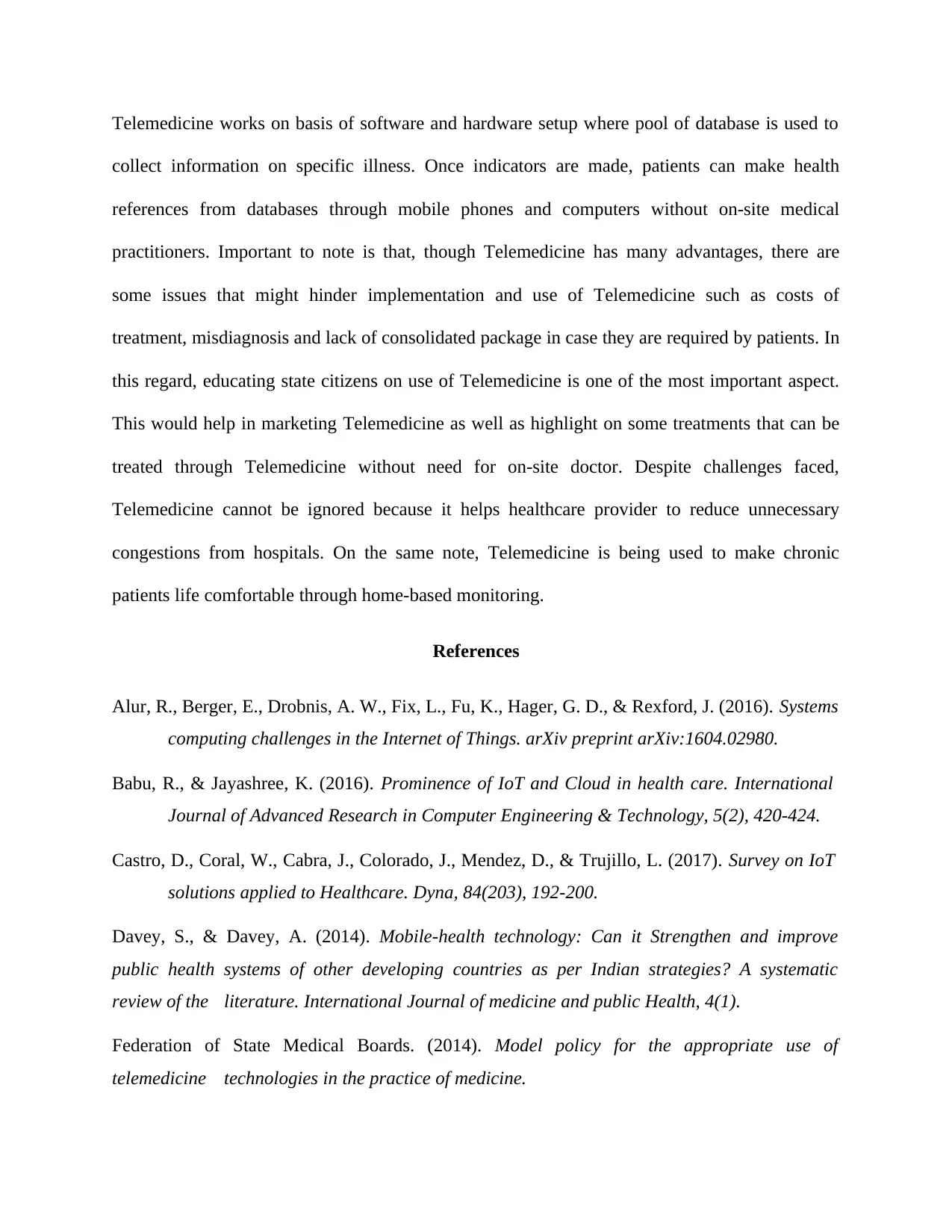
revenue generated from Telemedicine. Similarly, investment on Telemedicine has been growing
over time with aim of making it a choice by every patient. Mainly, investment has been focused
on hardware, software and services required to sustain Telemedicine.
Figure 2: Number of penitents against revenue generated
Figure 3: Investment costs on Telemedicine
Conclusion
Telemedicine has been growing over time since it was introduced some decades back. It
has been adopted in the market with aim of making healthcare delivery efficient and affordable.
Telemedicine is being supported by technology through IoT in order to deliver services to
everyone across the globe anytime. Without technology, telemedicine cannot be in existence.
over time with aim of making it a choice by every patient. Mainly, investment has been focused
on hardware, software and services required to sustain Telemedicine.
Figure 2: Number of penitents against revenue generated
Figure 3: Investment costs on Telemedicine
Conclusion
Telemedicine has been growing over time since it was introduced some decades back. It
has been adopted in the market with aim of making healthcare delivery efficient and affordable.
Telemedicine is being supported by technology through IoT in order to deliver services to
everyone across the globe anytime. Without technology, telemedicine cannot be in existence.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Telemedicine works on basis of software and hardware setup where pool of database is used to
collect information on specific illness. Once indicators are made, patients can make health
references from databases through mobile phones and computers without on-site medical
practitioners. Important to note is that, though Telemedicine has many advantages, there are
some issues that might hinder implementation and use of Telemedicine such as costs of
treatment, misdiagnosis and lack of consolidated package in case they are required by patients. In
this regard, educating state citizens on use of Telemedicine is one of the most important aspect.
This would help in marketing Telemedicine as well as highlight on some treatments that can be
treated through Telemedicine without need for on-site doctor. Despite challenges faced,
Telemedicine cannot be ignored because it helps healthcare provider to reduce unnecessary
congestions from hospitals. On the same note, Telemedicine is being used to make chronic
patients life comfortable through home-based monitoring.
References
Alur, R., Berger, E., Drobnis, A. W., Fix, L., Fu, K., Hager, G. D., & Rexford, J. (2016). Systems
computing challenges in the Internet of Things. arXiv preprint arXiv:1604.02980.
Babu, R., & Jayashree, K. (2016). Prominence of IoT and Cloud in health care. International
Journal of Advanced Research in Computer Engineering & Technology, 5(2), 420-424.
Castro, D., Coral, W., Cabra, J., Colorado, J., Mendez, D., & Trujillo, L. (2017). Survey on IoT
solutions applied to Healthcare. Dyna, 84(203), 192-200.
Davey, S., & Davey, A. (2014). Mobile-health technology: Can it Strengthen and improve
public health systems of other developing countries as per Indian strategies? A systematic
review of the literature. International Journal of medicine and public Health, 4(1).
Federation of State Medical Boards. (2014). Model policy for the appropriate use of
telemedicine technologies in the practice of medicine.
collect information on specific illness. Once indicators are made, patients can make health
references from databases through mobile phones and computers without on-site medical
practitioners. Important to note is that, though Telemedicine has many advantages, there are
some issues that might hinder implementation and use of Telemedicine such as costs of
treatment, misdiagnosis and lack of consolidated package in case they are required by patients. In
this regard, educating state citizens on use of Telemedicine is one of the most important aspect.
This would help in marketing Telemedicine as well as highlight on some treatments that can be
treated through Telemedicine without need for on-site doctor. Despite challenges faced,
Telemedicine cannot be ignored because it helps healthcare provider to reduce unnecessary
congestions from hospitals. On the same note, Telemedicine is being used to make chronic
patients life comfortable through home-based monitoring.
References
Alur, R., Berger, E., Drobnis, A. W., Fix, L., Fu, K., Hager, G. D., & Rexford, J. (2016). Systems
computing challenges in the Internet of Things. arXiv preprint arXiv:1604.02980.
Babu, R., & Jayashree, K. (2016). Prominence of IoT and Cloud in health care. International
Journal of Advanced Research in Computer Engineering & Technology, 5(2), 420-424.
Castro, D., Coral, W., Cabra, J., Colorado, J., Mendez, D., & Trujillo, L. (2017). Survey on IoT
solutions applied to Healthcare. Dyna, 84(203), 192-200.
Davey, S., & Davey, A. (2014). Mobile-health technology: Can it Strengthen and improve
public health systems of other developing countries as per Indian strategies? A systematic
review of the literature. International Journal of medicine and public Health, 4(1).
Federation of State Medical Boards. (2014). Model policy for the appropriate use of
telemedicine technologies in the practice of medicine.
Jacob, S. G., & Ramani, R. G. (2012). Data mining in clinical data sets: a review. IJAIS-ISSN:
2249-0868 Foundation of Computer Science FCS, New York, USA, 4(6).
Kenganal, M. S. S., & Rengaprabhu, P. (2016). Real Time Wireless Patient Monitoring System
Based On IOT. Imperial Journal of Interdisciplinary Research, 2(13).
Kim, J. T. (2014). Privacy and security issues for healthcare system with embedded RFID
system on Internet of Things. Advanced Science and Technology Letters, 72, 109-112.
Lazarev, K. (2016). Internet of Things for personal healthcare: Study of eHealth sector. Smart
wearable design.
Lin, H., & Bergmann, N. W. (2016). IoT privacy and security challenges for smart home
environments. Information, 7(3), 44.
Mahmood, N., Burney, A., Abbas, Z., & Rizwan, K. (2012). Data and knowledge management
in designing healthcare information systems. International Journal of Computer
Applications, 50(2).
Majumder, S., Aghayi, E., Noferesti, M., Memarzadeh-Tehran, H., Mondal, T., Pang, Z., &
Deen, M. J. (2017). Smart Homes for Elderly Healthcare—Recent Advances and
Research Challenges. Sensors, 17(11), 2496.
Mora, H., Gil, D., Terol, R. M., Azorín, J., & Szymanski, J. (2017). An IoT-Based
Computational Framework for Healthcare Monitoring in Mobile Environments. Sensors,
17(10), 2302.
Sermakani, V. (2014). Transforming healthcare through Internet of Things. In of Project
Management Practitioners' Conference.
Shen, J., Xu, B., Pei, M., & Jia, Y. (2016). A low-cost tele-presence wheelchair system. In
Intelligent Robots and Systems (IROS), 2016 IEEE/RSJ International Conference on (pp.
2452- 2457). IEEE.
Spyropoulos, B. (2017). Incorporating the Internet of Things in the Modern Hospital:
Attempting a “Taxonomy” of Pertinent Equipment and Services. American Journal of
Management Science and Engineering, 2(6), 160.
2249-0868 Foundation of Computer Science FCS, New York, USA, 4(6).
Kenganal, M. S. S., & Rengaprabhu, P. (2016). Real Time Wireless Patient Monitoring System
Based On IOT. Imperial Journal of Interdisciplinary Research, 2(13).
Kim, J. T. (2014). Privacy and security issues for healthcare system with embedded RFID
system on Internet of Things. Advanced Science and Technology Letters, 72, 109-112.
Lazarev, K. (2016). Internet of Things for personal healthcare: Study of eHealth sector. Smart
wearable design.
Lin, H., & Bergmann, N. W. (2016). IoT privacy and security challenges for smart home
environments. Information, 7(3), 44.
Mahmood, N., Burney, A., Abbas, Z., & Rizwan, K. (2012). Data and knowledge management
in designing healthcare information systems. International Journal of Computer
Applications, 50(2).
Majumder, S., Aghayi, E., Noferesti, M., Memarzadeh-Tehran, H., Mondal, T., Pang, Z., &
Deen, M. J. (2017). Smart Homes for Elderly Healthcare—Recent Advances and
Research Challenges. Sensors, 17(11), 2496.
Mora, H., Gil, D., Terol, R. M., Azorín, J., & Szymanski, J. (2017). An IoT-Based
Computational Framework for Healthcare Monitoring in Mobile Environments. Sensors,
17(10), 2302.
Sermakani, V. (2014). Transforming healthcare through Internet of Things. In of Project
Management Practitioners' Conference.
Shen, J., Xu, B., Pei, M., & Jia, Y. (2016). A low-cost tele-presence wheelchair system. In
Intelligent Robots and Systems (IROS), 2016 IEEE/RSJ International Conference on (pp.
2452- 2457). IEEE.
Spyropoulos, B. (2017). Incorporating the Internet of Things in the Modern Hospital:
Attempting a “Taxonomy” of Pertinent Equipment and Services. American Journal of
Management Science and Engineering, 2(6), 160.

Zhang, X. M., & Xu, C. (2012). A multimedia telemedicine system in internet of things.
Proceedings of the Computer Science & Information Technology, 42, 180-187.
Proceedings of the Computer Science & Information Technology, 42, 180-187.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





