Effectiveness of CBT and Task-Oriented Balance Training in Reducing Fear of Falling in Chronic Stroke Patients
VerifiedAdded on 2023/01/20
|10
|8960
|76
AI Summary
This study protocol aims to evaluate the effectiveness of a combination of cognitive behavioral therapy (CBT) and task-oriented balance training (TOBT) in reducing the fear of falling in patients with chronic stroke. The study will be a randomized controlled trial with a placebo-controlled single-blind parallel-group design. The primary outcome measure is subjective balance confidence, and the secondary outcome measures include fear-avoidance behavior, balance ability, fall risk, level of activities of daily living, community reintegration, and health-related quality of life. The trial is registered on ClinicalTrials.gov with the registration number NCT02937532.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
STUDY PROTOCOL Open Access
Effectiveness of a combination of cognitive
behavioraltherapy and task-oriented
balance training in reducing the fear of
falling in patients with chronic stroke:study
protocolfor a randomized controlled trial
Tai-Wa Liu1,2
, GabrielY.F.Ng1 and Shamay S.M.Ng1*
Abstract
Background:The consequences offalls are devastating forpatients with stroke.Balance problems and fearof
falling are two majorchallenges,and recentsystematic reviews have revealed thathabitualphysicalexercise
training alone cannot reduce the occurrence of falls in stroke survivors.However,recent trials with community-dwelling
healthy older adults yielded the promising result that interventions with a cognitive behavioral therapy (CB
can simultaneously promote balance and reduce the fear of falling.Therefore,the aim of the proposed clinical trial is to
evaluate the effectiveness of a combination of CBT and task-oriented balance training (TOBT) in promoting
balance confidence,and thereby reducing fear-avoidance behavior,improving balance ability,reducing fall risk,and
promoting independent living,community reintegration,and health-related quality of life of patients with stroke.
Methods: The study will constitute a placebo-controlled single-blind parallel-group randomized controlled t
patients are assessed immediately,at 3 months,and at 12 months.The selected participants will be randomly allocated
into one of two parallel groups (the experimental group and the control group) with a 1:1 ratio.Both groups will receive
45 min of TOBT twice per week for 8 weeks.In addition,the experimental group will receive a 45-min CBT-based group
intervention,and the control group will receive 45 min of general health education (GHE) twice per week for 8
The primary outcome measure is subjective balance confidence.The secondary outcome measures are fear-avoidance
behavior,balance ability,fall risk,level of activities of daily living,community reintegration,and health-related quality of
life.
Discussion: The proposed clinical trial will compare the effectiveness of CBT combined with TOBT and GHE
with TOBT in promoting subjective balance confidence among chronic stroke patients.
We hope our results will provide evidence of a safe,cost-effective,and readily transferrable therapeutic approach to
clinical practice that reduces fear-avoidance behavior,improves balance ability,reduces fall risk,promotes independence
and community reintegration,and enhances health-related quality of life.
Trial registration: ClinicalTrials.gov,NCT02937532.Registered on 17 October 2016.
Keywords: Stroke rehabilitation,Cognitive behavioral therapy,Fear of falling,Subjective balance confidence,Balance self-
efficacy,Fall risk
* Correspondence:Shamay.Ng@polyu.edu.hk
1Department of Rehabilitation Sciences,The Hong Kong Polytechnic
University,Hung Hom,Hong Kong,SpecialAdministrative Region of China
Fulllist of author information is available at the end of the article
© The Author(s).2018 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0
InternationalLicense (http://creativecommons.org/licenses/by/4.0/),which permits unrestricted use,distribution,and
reproduction in any medium,provided you give appropriate credit to the originalauthor(s) and the source,provide a link to
the Creative Commons license,and indicate if changes were made.The Creative Commons Public Domain Dedication waiver
(http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,unless otherwise stated.
Liu et al.Trials (2018) 19:168
https://doi.org/10.1186/s13063-018-2549-z
Effectiveness of a combination of cognitive
behavioraltherapy and task-oriented
balance training in reducing the fear of
falling in patients with chronic stroke:study
protocolfor a randomized controlled trial
Tai-Wa Liu1,2
, GabrielY.F.Ng1 and Shamay S.M.Ng1*
Abstract
Background:The consequences offalls are devastating forpatients with stroke.Balance problems and fearof
falling are two majorchallenges,and recentsystematic reviews have revealed thathabitualphysicalexercise
training alone cannot reduce the occurrence of falls in stroke survivors.However,recent trials with community-dwelling
healthy older adults yielded the promising result that interventions with a cognitive behavioral therapy (CB
can simultaneously promote balance and reduce the fear of falling.Therefore,the aim of the proposed clinical trial is to
evaluate the effectiveness of a combination of CBT and task-oriented balance training (TOBT) in promoting
balance confidence,and thereby reducing fear-avoidance behavior,improving balance ability,reducing fall risk,and
promoting independent living,community reintegration,and health-related quality of life of patients with stroke.
Methods: The study will constitute a placebo-controlled single-blind parallel-group randomized controlled t
patients are assessed immediately,at 3 months,and at 12 months.The selected participants will be randomly allocated
into one of two parallel groups (the experimental group and the control group) with a 1:1 ratio.Both groups will receive
45 min of TOBT twice per week for 8 weeks.In addition,the experimental group will receive a 45-min CBT-based group
intervention,and the control group will receive 45 min of general health education (GHE) twice per week for 8
The primary outcome measure is subjective balance confidence.The secondary outcome measures are fear-avoidance
behavior,balance ability,fall risk,level of activities of daily living,community reintegration,and health-related quality of
life.
Discussion: The proposed clinical trial will compare the effectiveness of CBT combined with TOBT and GHE
with TOBT in promoting subjective balance confidence among chronic stroke patients.
We hope our results will provide evidence of a safe,cost-effective,and readily transferrable therapeutic approach to
clinical practice that reduces fear-avoidance behavior,improves balance ability,reduces fall risk,promotes independence
and community reintegration,and enhances health-related quality of life.
Trial registration: ClinicalTrials.gov,NCT02937532.Registered on 17 October 2016.
Keywords: Stroke rehabilitation,Cognitive behavioral therapy,Fear of falling,Subjective balance confidence,Balance self-
efficacy,Fall risk
* Correspondence:Shamay.Ng@polyu.edu.hk
1Department of Rehabilitation Sciences,The Hong Kong Polytechnic
University,Hung Hom,Hong Kong,SpecialAdministrative Region of China
Fulllist of author information is available at the end of the article
© The Author(s).2018 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0
InternationalLicense (http://creativecommons.org/licenses/by/4.0/),which permits unrestricted use,distribution,and
reproduction in any medium,provided you give appropriate credit to the originalauthor(s) and the source,provide a link to
the Creative Commons license,and indicate if changes were made.The Creative Commons Public Domain Dedication waiver
(http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,unless otherwise stated.
Liu et al.Trials (2018) 19:168
https://doi.org/10.1186/s13063-018-2549-z
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Background
Fear offalling (FoF)is one ofthe mostcommon post-
stroke complications,and is widely acknowledged as part
of a vicious circle [1] leading to actual falls [2].It is a de-
bilitating post-fallsyndrome stemming from low balance
self-efficacy and the fearfulanticipation offalling [3,4].
The reported prevalenceof FoF variesbetween post-
stroke stages,ranging from 54% before discharge [5] from
an acute unit to 44% at 6 months after stroke [6] and 58%
among community-dwelling patients with stroke [7].If no
action is taken, FoF spirals into a loss of physical function,
dependency on others for assistance with activities of daily
living (ADL),restrictionson daily activities[4], and a
higher fallrate,[8] eventually compromising community
integration [9].
Two recent systematic reviews synthesized the findings
of interventions targeting FoF.Bula et al.’s [10] review of
46 randomizedcontrolledtrials (RCTs) with 6794
community-dwelling elderly persons revealed that the ma-
jority of the reviewed studies (n = 38) focused on fall pre-
vention and balance improvement,with FoF regarded as a
secondary outcome.In the eight studies directly address-
ing the fear offearing,the use of physiologicalinterven-
tions such astai chi [11];strengthening,balance and
walking exercises [12]; psychological interventions such as
cognitive behavioraltherapy (CBT)[13,14];and guided
relaxation and exercise imagery [15] was reported to help
reduce FoF among community-dwelling older people.
In another systematic review, Tang et al.[16] examined
19 clinical trials addressingFoF among peoplewith
stroke.Despiteits significantinfluenceon strokere-
habilitation,FoF was regarded only as a secondary target
in the studies reviewed.Tang’s [16] meta-analysis of15
clinicaltrials with 627 participants revealed thatinten-
sive exercise-based physiologicalinterventions,such as
gait training [17–20],exergaming [21],yoga [22],and a
combination of fitness,mobility and functionalexercises
[23,24],can reduce FoF with a medium effect size (stan-
dardized mean difference 0.44;95% confidence interval
(0.11–0.77);p = 0.009).No improvements were noted in
the four reviewed studies using psychologicalinterven-
tions (motor imagery)[25–28],and no retention effect
was noted in the studies with a follow-up assessment.
However,the effectivenessof CBT as a psychological
intervention in reducing the FoF ofstroke patients has
not been examined.
CBT is a psychotherapeuticapproach thatredirects
negative cognitive,emotional,or behavioralresponses to
help people developcoping mechanismsand self-
confidence [29].For example,people with FoF originating
from impaired balanceself-efficacycan use CBT to
change their self-defeating beliefs,improve their balance
self-efficacy and replace theirunrealistic anticipation of
falls and magnified FoF consequenceswith a realistic,
positive perspective on falls,in turn reducing their fear
avoidance.
As summarized by Bula etal. [10] and Tang etal.
[16],studies have shown that physicalexercise can re-
duce FoF in older people and people with stroke as
either a primary or a secondary outcome.As psycho-
logicalinterventionsoffer anotherpossible meansof
reducing FoF,we aim to examine the effectiveness of
a combinationof CBT and task-orientedbalance
training (TOBT)in reducing the FoF ofpeople with
stroke.TOBT will be used in the proposed study be-
causeit targetsstroke-specificimpairmentsand has
been clinicallyproven to improvethe balanceper-
formance ofpeople with stroke [30,31]. The inclu-
sion of CBT in our treatmentarm is based on our
hypothesis thatCBT is an adjuncttherapy capable of
optimizing the treatmenteffectsof exercise in redu-
cing FoF.It is expected to tackle FoF directly through
the promotion ofbalance self-efficacy,and its indirect
effectswill be mediated by repeated exercise and re-
duced fear-avoidance behavior,further enhancing bal-
ance performanceand ADL, and therebyimproving
community integration.The combined effects ofCBT
and TOBT in reducing FoF are expected to improve
patients’balance,reduce their risk offalling,increase
their independence,and thereby promote theircom-
munity integration.Indeed,in Huang et al.’s[32] re-
centRCT with elderly persons,CBT with an exercise
intervention (n = 27)performed betterthan either
CBT alone (n = 27)or treatmentas usual(n = 26)in
reducing FoF and depression and enhancing mobility
and muscle strength,with retention effectsobserved
up to 5 monthslater.Therefore,the proposed study
aims to determinewhether combiningCBT with
TOBT augments the latter’s positive treatmenteffects
on FoF, and thus fear-avoidancebehavior,balance
ability,fall risk, independentliving, enhancing com-
munityintegration,and health-related qualityof life
among community-dwelling seniors with stroke.
To develop an intervention for clinical use, a protocol is
necessary to ensure the consistency ofimplementation
and ease ofreplication.Therefore,the objective ofthis
paper is to report the details of a protocolfor combining
CBT and TOBT to reduce FoF among people with stroke.
Methods
Trial design
The proposedstudy will be a placebo-controlled
single-blindparallel-groupRCT with a 12-month
follow-up, conducted with community-dwelling
chronic stroke survivorswith FoF at a university-
based rehabilitation center.The findingsof the trial
will be reported in accordance with the Consolidated
Standards ofReporting Statement [33].
Liu et al.Trials (2018) 19:168 Page 2 of 10
Fear offalling (FoF)is one ofthe mostcommon post-
stroke complications,and is widely acknowledged as part
of a vicious circle [1] leading to actual falls [2].It is a de-
bilitating post-fallsyndrome stemming from low balance
self-efficacy and the fearfulanticipation offalling [3,4].
The reported prevalenceof FoF variesbetween post-
stroke stages,ranging from 54% before discharge [5] from
an acute unit to 44% at 6 months after stroke [6] and 58%
among community-dwelling patients with stroke [7].If no
action is taken, FoF spirals into a loss of physical function,
dependency on others for assistance with activities of daily
living (ADL),restrictionson daily activities[4], and a
higher fallrate,[8] eventually compromising community
integration [9].
Two recent systematic reviews synthesized the findings
of interventions targeting FoF.Bula et al.’s [10] review of
46 randomizedcontrolledtrials (RCTs) with 6794
community-dwelling elderly persons revealed that the ma-
jority of the reviewed studies (n = 38) focused on fall pre-
vention and balance improvement,with FoF regarded as a
secondary outcome.In the eight studies directly address-
ing the fear offearing,the use of physiologicalinterven-
tions such astai chi [11];strengthening,balance and
walking exercises [12]; psychological interventions such as
cognitive behavioraltherapy (CBT)[13,14];and guided
relaxation and exercise imagery [15] was reported to help
reduce FoF among community-dwelling older people.
In another systematic review, Tang et al.[16] examined
19 clinical trials addressingFoF among peoplewith
stroke.Despiteits significantinfluenceon strokere-
habilitation,FoF was regarded only as a secondary target
in the studies reviewed.Tang’s [16] meta-analysis of15
clinicaltrials with 627 participants revealed thatinten-
sive exercise-based physiologicalinterventions,such as
gait training [17–20],exergaming [21],yoga [22],and a
combination of fitness,mobility and functionalexercises
[23,24],can reduce FoF with a medium effect size (stan-
dardized mean difference 0.44;95% confidence interval
(0.11–0.77);p = 0.009).No improvements were noted in
the four reviewed studies using psychologicalinterven-
tions (motor imagery)[25–28],and no retention effect
was noted in the studies with a follow-up assessment.
However,the effectivenessof CBT as a psychological
intervention in reducing the FoF ofstroke patients has
not been examined.
CBT is a psychotherapeuticapproach thatredirects
negative cognitive,emotional,or behavioralresponses to
help people developcoping mechanismsand self-
confidence [29].For example,people with FoF originating
from impaired balanceself-efficacycan use CBT to
change their self-defeating beliefs,improve their balance
self-efficacy and replace theirunrealistic anticipation of
falls and magnified FoF consequenceswith a realistic,
positive perspective on falls,in turn reducing their fear
avoidance.
As summarized by Bula etal. [10] and Tang etal.
[16],studies have shown that physicalexercise can re-
duce FoF in older people and people with stroke as
either a primary or a secondary outcome.As psycho-
logicalinterventionsoffer anotherpossible meansof
reducing FoF,we aim to examine the effectiveness of
a combinationof CBT and task-orientedbalance
training (TOBT)in reducing the FoF ofpeople with
stroke.TOBT will be used in the proposed study be-
causeit targetsstroke-specificimpairmentsand has
been clinicallyproven to improvethe balanceper-
formance ofpeople with stroke [30,31]. The inclu-
sion of CBT in our treatmentarm is based on our
hypothesis thatCBT is an adjuncttherapy capable of
optimizing the treatmenteffectsof exercise in redu-
cing FoF.It is expected to tackle FoF directly through
the promotion ofbalance self-efficacy,and its indirect
effectswill be mediated by repeated exercise and re-
duced fear-avoidance behavior,further enhancing bal-
ance performanceand ADL, and therebyimproving
community integration.The combined effects ofCBT
and TOBT in reducing FoF are expected to improve
patients’balance,reduce their risk offalling,increase
their independence,and thereby promote theircom-
munity integration.Indeed,in Huang et al.’s[32] re-
centRCT with elderly persons,CBT with an exercise
intervention (n = 27)performed betterthan either
CBT alone (n = 27)or treatmentas usual(n = 26)in
reducing FoF and depression and enhancing mobility
and muscle strength,with retention effectsobserved
up to 5 monthslater.Therefore,the proposed study
aims to determinewhether combiningCBT with
TOBT augments the latter’s positive treatmenteffects
on FoF, and thus fear-avoidancebehavior,balance
ability,fall risk, independentliving, enhancing com-
munityintegration,and health-related qualityof life
among community-dwelling seniors with stroke.
To develop an intervention for clinical use, a protocol is
necessary to ensure the consistency ofimplementation
and ease ofreplication.Therefore,the objective ofthis
paper is to report the details of a protocolfor combining
CBT and TOBT to reduce FoF among people with stroke.
Methods
Trial design
The proposedstudy will be a placebo-controlled
single-blindparallel-groupRCT with a 12-month
follow-up, conducted with community-dwelling
chronic stroke survivorswith FoF at a university-
based rehabilitation center.The findingsof the trial
will be reported in accordance with the Consolidated
Standards ofReporting Statement [33].
Liu et al.Trials (2018) 19:168 Page 2 of 10
Choice of comparator
A placebo control intervention,general health education
(GHE), will be provided for the controlgroup to help
measure the effects ofCBT alone.To rule out potential
placebo effectssuch asattention from therapistsand
knowledge oftreatmentconditions,the GHE program
will provide no information related to subjective balance
confidence,activity avoidance,falls,or physicalactivity,
but only information related to generalhealth issues
such as healthy food choices and foot care.
Null hypothesis
The null hypothesiswill be that the efficacy ofCBT
combined with TOBT does not differ significantly from
that of GHE combined with TOBT in promoting balance
self-efficacy,thus reducing fear-avoidance behavior,en-
hancing balance ability,reducing fall risk,and improving
community reintegration and health-related quality of
life for people with stroke.
Participants
Prospective participants willbe required to meet the fol-
lowing inclusion criteria:(i) aged between 55 and 85,(ii)
diagnosed with a first unilateral ischemic brain injury or in-
tracerebral hemorrhage by magnetic resonance imaging or
computed tomography within 1–6 years post-stroke,(iii)
discharged from all rehabilitation services at least 6 months
before the program,(iv) able to walk independently for at
least 10 m with or without an assistive device,(v) showing
low balance self-efficacy [scoring less than 80 on the Chin-
ese version ofthe Activities-specific Balance Confidence
(ABC-C) Scale] [34],(vi) scoring higher than 7 out of 10
on the Chinese version ofthe Abbreviated MentalTest
[35],and (vii) able to follow instructions and provide writ-
ten informed consent.
Individuals willbe excluded if they have any additional
medical,cardiovascular,orthopedic,psychiatric,or psy-
chological conditions that will hinder proper treatment or
assessment,if they presentwith receptive dysphasia or
significant lower limb peripheral neuropathy, or if they are
involved in drug studies or other clinical trials.
Therapists and research personnel
Two research assistants with at least 2 years ofresearch
experience in physicalexercise training willbe the asses-
sors of this study.They will be given a 1-day training ses-
sion on obtainingoutcome measurementsby an
experienced physiotherapist before the study. Training will
be provided in both the theory and practice of using the
outcome measures.All of the assessors willrehearse the
outcome measures with the research team personnelto
standardize the assessment.To establish the interrater re-
liability,the two assessors willrate five participants and
then review for discrepancies, if any.
The two TOBT therapists willhave been trained by an
experienced physiotherapistand have at least2 years of
post-qualification experience as therapists in physicalex-
ercise training.They willbe provided with written pro-
gression guidelines (Table 1).A regular review of training
records and spotobservations willbe conducted by the
experienced physiotherapist to enhance adherence to the
written progression guidelines. The CBT therapists will be
three psychiatric nurses who have qualified as cognitive
therapists.They will all have atleast5 yearsof post-
qualification experience with applying CBT clinically.A
treatment manualand materials have already been devel-
oped with reference to Tennstedt et al.’s [13] and Zijlstra
et al.’s [14] researchon FoF as experiencedby
community-dwelling olderadultsand reviewed by the
three certified cognitive therapists involved in the study.
To ensure treatment integrity,the CBT intervention has
already been piloted and audiotaped.Each CBT therapist
evaluated the pilotsessionsto assesstheir compliance
with the treatmentmanual,the achievementof session
goals,and the use of CBT techniques.The GHE interven-
tion willbe delivered by two research assistants notin-
volvedin the assessmentor any other part of the
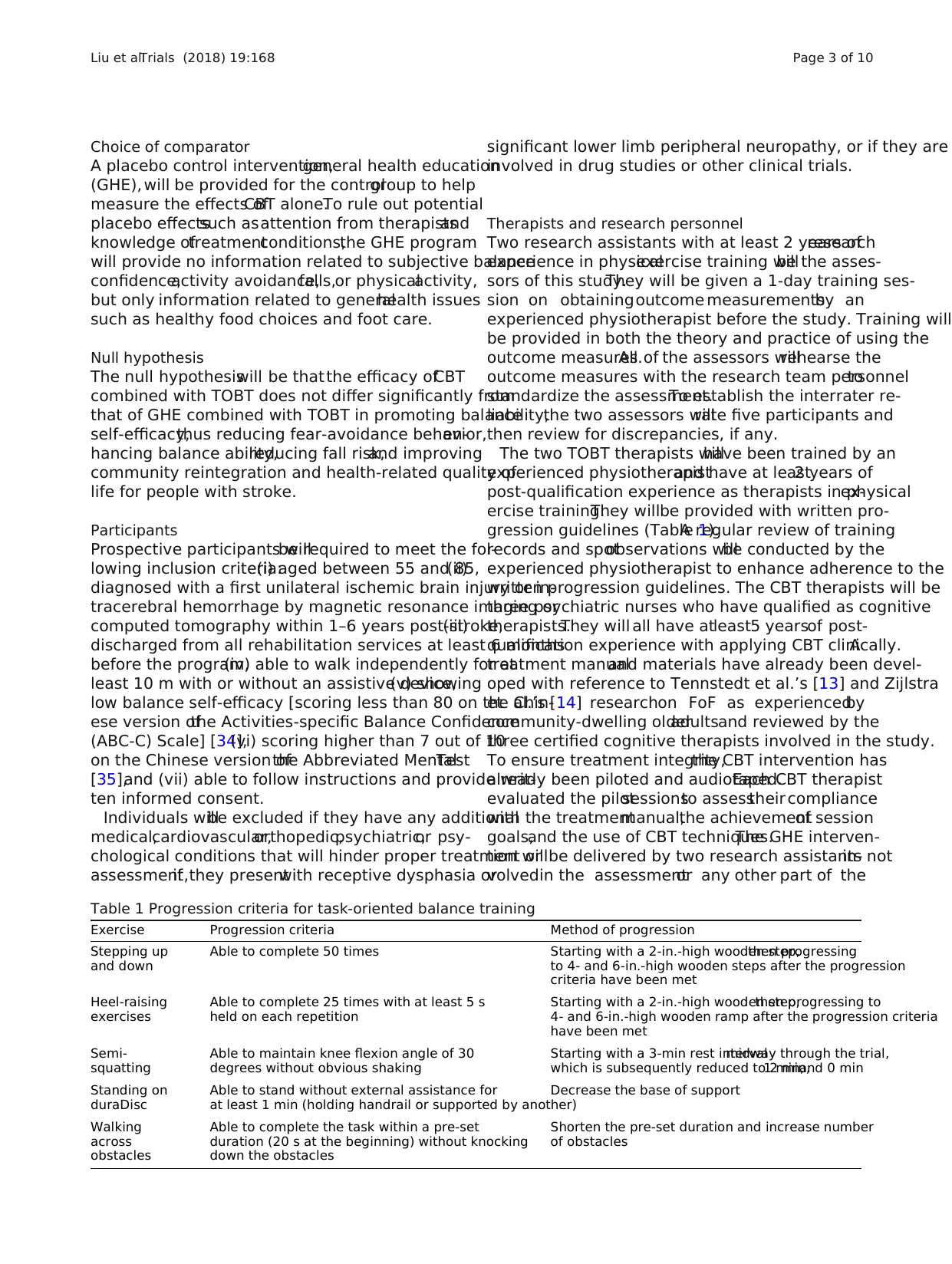
Table 1 Progression criteria for task-oriented balance training
Exercise Progression criteria Method of progression
Stepping up
and down
Able to complete 50 times Starting with a 2-in.-high wooden step,then progressing
to 4- and 6-in.-high wooden steps after the progression
criteria have been met
Heel-raising
exercises
Able to complete 25 times with at least 5 s
held on each repetition
Starting with a 2-in.-high wooden step,then progressing to
4- and 6-in.-high wooden ramp after the progression criteria
have been met
Semi-
squatting
Able to maintain knee flexion angle of 30
degrees without obvious shaking
Starting with a 3-min rest intervalmidway through the trial,
which is subsequently reduced to 2 min,1 min,and 0 min
Standing on
duraDisc
Able to stand without external assistance for
at least 1 min (holding handrail or supported by another)
Decrease the base of support
Walking
across
obstacles
Able to complete the task within a pre-set
duration (20 s at the beginning) without knocking
down the obstacles
Shorten the pre-set duration and increase number
of obstacles
Liu et al.Trials (2018) 19:168 Page 3 of 10
A placebo control intervention,general health education
(GHE), will be provided for the controlgroup to help
measure the effects ofCBT alone.To rule out potential
placebo effectssuch asattention from therapistsand
knowledge oftreatmentconditions,the GHE program
will provide no information related to subjective balance
confidence,activity avoidance,falls,or physicalactivity,
but only information related to generalhealth issues
such as healthy food choices and foot care.
Null hypothesis
The null hypothesiswill be that the efficacy ofCBT
combined with TOBT does not differ significantly from
that of GHE combined with TOBT in promoting balance
self-efficacy,thus reducing fear-avoidance behavior,en-
hancing balance ability,reducing fall risk,and improving
community reintegration and health-related quality of
life for people with stroke.
Participants
Prospective participants willbe required to meet the fol-
lowing inclusion criteria:(i) aged between 55 and 85,(ii)
diagnosed with a first unilateral ischemic brain injury or in-
tracerebral hemorrhage by magnetic resonance imaging or
computed tomography within 1–6 years post-stroke,(iii)
discharged from all rehabilitation services at least 6 months
before the program,(iv) able to walk independently for at
least 10 m with or without an assistive device,(v) showing
low balance self-efficacy [scoring less than 80 on the Chin-
ese version ofthe Activities-specific Balance Confidence
(ABC-C) Scale] [34],(vi) scoring higher than 7 out of 10
on the Chinese version ofthe Abbreviated MentalTest
[35],and (vii) able to follow instructions and provide writ-
ten informed consent.
Individuals willbe excluded if they have any additional
medical,cardiovascular,orthopedic,psychiatric,or psy-
chological conditions that will hinder proper treatment or
assessment,if they presentwith receptive dysphasia or
significant lower limb peripheral neuropathy, or if they are
involved in drug studies or other clinical trials.
Therapists and research personnel
Two research assistants with at least 2 years ofresearch
experience in physicalexercise training willbe the asses-
sors of this study.They will be given a 1-day training ses-
sion on obtainingoutcome measurementsby an
experienced physiotherapist before the study. Training will
be provided in both the theory and practice of using the
outcome measures.All of the assessors willrehearse the
outcome measures with the research team personnelto
standardize the assessment.To establish the interrater re-
liability,the two assessors willrate five participants and
then review for discrepancies, if any.
The two TOBT therapists willhave been trained by an
experienced physiotherapistand have at least2 years of
post-qualification experience as therapists in physicalex-
ercise training.They willbe provided with written pro-
gression guidelines (Table 1).A regular review of training
records and spotobservations willbe conducted by the
experienced physiotherapist to enhance adherence to the
written progression guidelines. The CBT therapists will be
three psychiatric nurses who have qualified as cognitive
therapists.They will all have atleast5 yearsof post-
qualification experience with applying CBT clinically.A
treatment manualand materials have already been devel-
oped with reference to Tennstedt et al.’s [13] and Zijlstra
et al.’s [14] researchon FoF as experiencedby
community-dwelling olderadultsand reviewed by the
three certified cognitive therapists involved in the study.
To ensure treatment integrity,the CBT intervention has
already been piloted and audiotaped.Each CBT therapist
evaluated the pilotsessionsto assesstheir compliance
with the treatmentmanual,the achievementof session
goals,and the use of CBT techniques.The GHE interven-
tion willbe delivered by two research assistants notin-
volvedin the assessmentor any other part of the
Table 1 Progression criteria for task-oriented balance training
Exercise Progression criteria Method of progression
Stepping up
and down
Able to complete 50 times Starting with a 2-in.-high wooden step,then progressing
to 4- and 6-in.-high wooden steps after the progression
criteria have been met
Heel-raising
exercises
Able to complete 25 times with at least 5 s
held on each repetition
Starting with a 2-in.-high wooden step,then progressing to
4- and 6-in.-high wooden ramp after the progression criteria
have been met
Semi-
squatting
Able to maintain knee flexion angle of 30
degrees without obvious shaking
Starting with a 3-min rest intervalmidway through the trial,
which is subsequently reduced to 2 min,1 min,and 0 min
Standing on
duraDisc
Able to stand without external assistance for
at least 1 min (holding handrail or supported by another)
Decrease the base of support
Walking
across
obstacles
Able to complete the task within a pre-set
duration (20 s at the beginning) without knocking
down the obstacles
Shorten the pre-set duration and increase number
of obstacles
Liu et al.Trials (2018) 19:168 Page 3 of 10
intervention,using audio-visualaidsand materialsthat
have already been developed.
Procedure
Participantswill be recruited from a local self-help
group for people with stroke through poster advertise-
ments.On receiving telephone calls from interested par-
ties,our recruitment research assistantwill perform an
initial eligibilityscreening and offerappointmentsto
gain written informed consentand complete a baseline
assessment.
All of the potentialparticipants willmeet individually
in the study venue to enable the researchers to explain
the details of the study,such as its aims,benefits,risks,
and confidentiality,and then check the applicants’eligi-
bility against the inclusion and exclusion criteria.If indi-
viduals are both interested in joining and eligible to join
the clinicaltrial,written informed consentwill be ob-
tainedbeforethe baselineassessmentis conducted.
Questionnaires relating to sociodemographic character-
istics,variables ofinterest,and physicaland functional
performance will be completed on the same day.
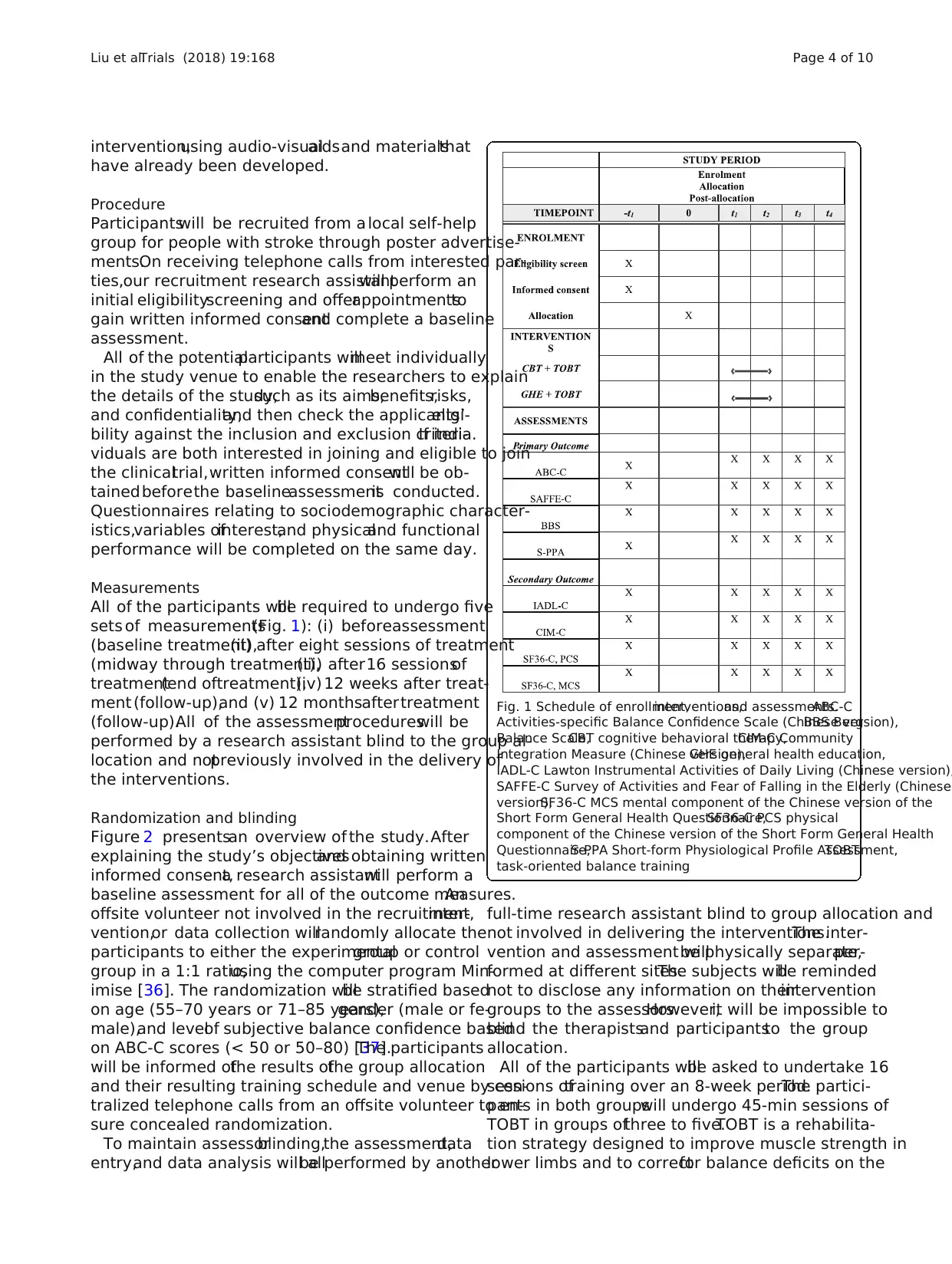
Measurements
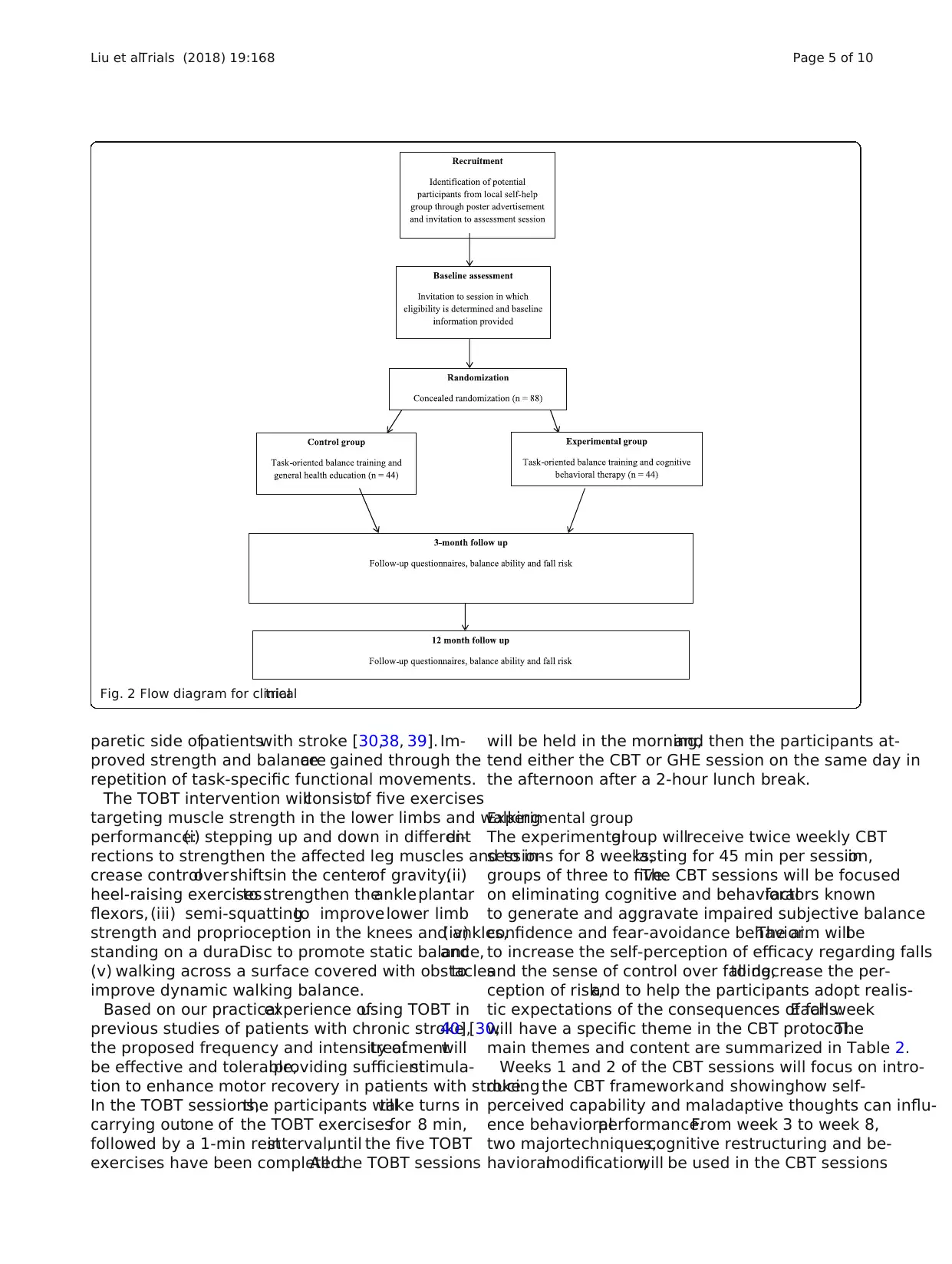
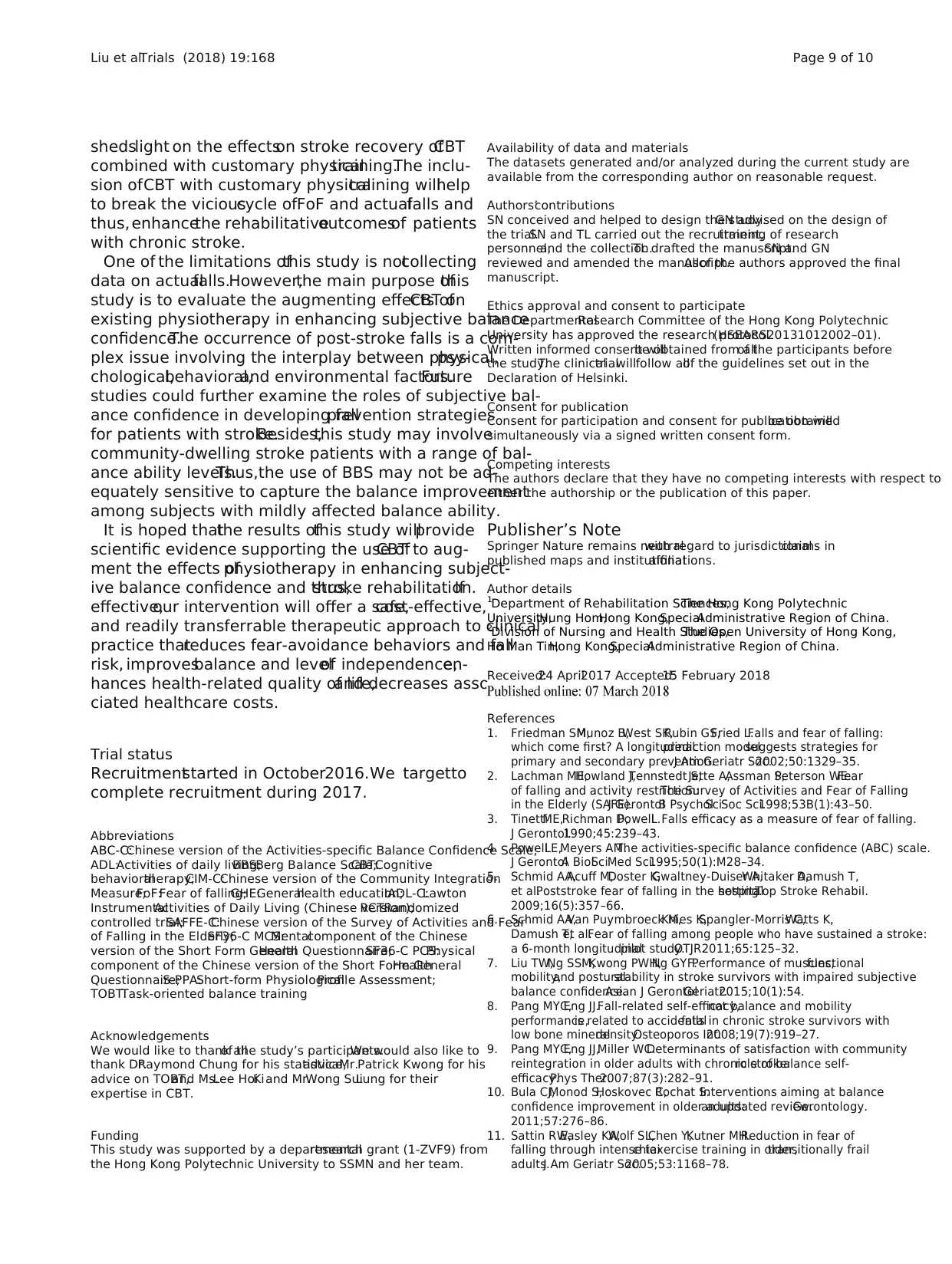
All of the participants willbe required to undergo five
sets of measurements(Fig. 1): (i) beforeassessment
(baseline treatment),(ii) after eight sessions of treatment
(midway through treatment),(iii) after16 sessionsof
treatment(end oftreatment),(iv) 12 weeks after treat-
ment (follow-up),and (v) 12 monthsaftertreatment
(follow-up).All of the assessmentprocedureswill be
performed by a research assistant blind to the group al-
location and notpreviously involved in the delivery of
the interventions.
Randomization and blinding
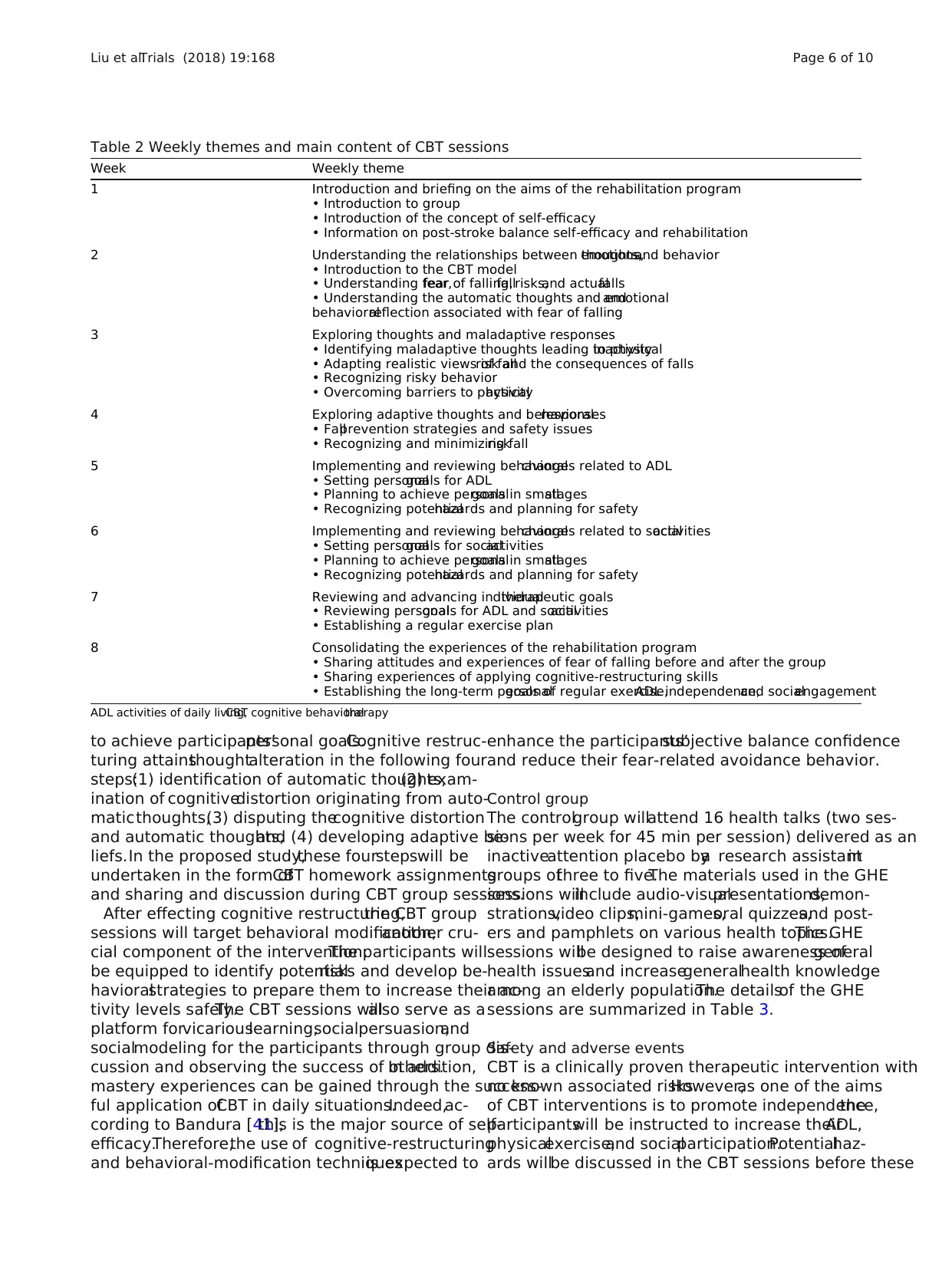
Figure 2 presentsan overview of the study.After
explaining the study’s objectivesand obtaining written
informed consent,a research assistantwill perform a
baseline assessment for all of the outcome measures.An
offsite volunteer not involved in the recruitment,inter-
vention,or data collection willrandomly allocate the
participants to either the experimentalgroup or control
group in a 1:1 ratio,using the computer program Min-
imise [36]. The randomization willbe stratified based
on age (55–70 years or 71–85 years),gender (male or fe-
male),and levelof subjective balance confidence based
on ABC-C scores (< 50 or 50–80) [37].The participants
will be informed ofthe results ofthe group allocation
and their resulting training schedule and venue by cen-
tralized telephone calls from an offsite volunteer to en-
sure concealed randomization.
To maintain assessorblinding,the assessment,data
entry,and data analysis will allbe performed by another
full-time research assistant blind to group allocation and
not involved in delivering the interventions.The inter-
vention and assessment willbe physically separate,per-
formed at different sites.The subjects willbe reminded
not to disclose any information on theirintervention
groups to the assessors.However,it will be impossible to
blind the therapistsand participantsto the group
allocation.
All of the participants willbe asked to undertake 16
sessions oftraining over an 8-week period.The partici-
pants in both groupswill undergo 45-min sessions of
TOBT in groups ofthree to five.TOBT is a rehabilita-
tion strategy designed to improve muscle strength in
lower limbs and to correctfor balance deficits on the
Fig. 1 Schedule of enrollment,interventions,and assessments.ABC-C
Activities-specific Balance Confidence Scale (Chinese version),BBS Berg
Balance Scale,CBT cognitive behavioral therapy,CIM-C Community
Integration Measure (Chinese version),GHE general health education,
IADL-C Lawton Instrumental Activities of Daily Living (Chinese version),
SAFFE-C Survey of Activities and Fear of Falling in the Elderly (Chinese
version),SF36-C MCS mental component of the Chinese version of the
Short Form General Health Questionnaire,SF36-C PCS physical
component of the Chinese version of the Short Form General Health
Questionnaire,S-PPA Short-form Physiological Profile Assessment,TOBT
task-oriented balance training
Liu et al.Trials (2018) 19:168 Page 4 of 10
have already been developed.
Procedure
Participantswill be recruited from a local self-help
group for people with stroke through poster advertise-
ments.On receiving telephone calls from interested par-
ties,our recruitment research assistantwill perform an
initial eligibilityscreening and offerappointmentsto
gain written informed consentand complete a baseline
assessment.
All of the potentialparticipants willmeet individually
in the study venue to enable the researchers to explain
the details of the study,such as its aims,benefits,risks,
and confidentiality,and then check the applicants’eligi-
bility against the inclusion and exclusion criteria.If indi-
viduals are both interested in joining and eligible to join
the clinicaltrial,written informed consentwill be ob-
tainedbeforethe baselineassessmentis conducted.
Questionnaires relating to sociodemographic character-
istics,variables ofinterest,and physicaland functional
performance will be completed on the same day.
Measurements
All of the participants willbe required to undergo five
sets of measurements(Fig. 1): (i) beforeassessment
(baseline treatment),(ii) after eight sessions of treatment
(midway through treatment),(iii) after16 sessionsof
treatment(end oftreatment),(iv) 12 weeks after treat-
ment (follow-up),and (v) 12 monthsaftertreatment
(follow-up).All of the assessmentprocedureswill be
performed by a research assistant blind to the group al-
location and notpreviously involved in the delivery of
the interventions.
Randomization and blinding
Figure 2 presentsan overview of the study.After
explaining the study’s objectivesand obtaining written
informed consent,a research assistantwill perform a
baseline assessment for all of the outcome measures.An
offsite volunteer not involved in the recruitment,inter-
vention,or data collection willrandomly allocate the
participants to either the experimentalgroup or control
group in a 1:1 ratio,using the computer program Min-
imise [36]. The randomization willbe stratified based
on age (55–70 years or 71–85 years),gender (male or fe-
male),and levelof subjective balance confidence based
on ABC-C scores (< 50 or 50–80) [37].The participants
will be informed ofthe results ofthe group allocation
and their resulting training schedule and venue by cen-
tralized telephone calls from an offsite volunteer to en-
sure concealed randomization.
To maintain assessorblinding,the assessment,data
entry,and data analysis will allbe performed by another
full-time research assistant blind to group allocation and
not involved in delivering the interventions.The inter-
vention and assessment willbe physically separate,per-
formed at different sites.The subjects willbe reminded
not to disclose any information on theirintervention
groups to the assessors.However,it will be impossible to
blind the therapistsand participantsto the group
allocation.
All of the participants willbe asked to undertake 16
sessions oftraining over an 8-week period.The partici-
pants in both groupswill undergo 45-min sessions of
TOBT in groups ofthree to five.TOBT is a rehabilita-
tion strategy designed to improve muscle strength in
lower limbs and to correctfor balance deficits on the
Fig. 1 Schedule of enrollment,interventions,and assessments.ABC-C
Activities-specific Balance Confidence Scale (Chinese version),BBS Berg
Balance Scale,CBT cognitive behavioral therapy,CIM-C Community
Integration Measure (Chinese version),GHE general health education,
IADL-C Lawton Instrumental Activities of Daily Living (Chinese version),
SAFFE-C Survey of Activities and Fear of Falling in the Elderly (Chinese
version),SF36-C MCS mental component of the Chinese version of the
Short Form General Health Questionnaire,SF36-C PCS physical
component of the Chinese version of the Short Form General Health
Questionnaire,S-PPA Short-form Physiological Profile Assessment,TOBT
task-oriented balance training
Liu et al.Trials (2018) 19:168 Page 4 of 10
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
paretic side ofpatientswith stroke [30,38, 39]. Im-
proved strength and balanceare gained through the
repetition of task-specific functional movements.
The TOBT intervention willconsistof five exercises
targeting muscle strength in the lower limbs and walking
performance:(i) stepping up and down in differentdi-
rections to strengthen the affected leg muscles and to in-
crease controlovershiftsin the centerof gravity,(ii)
heel-raising exercisesto strengthen theankleplantar
flexors, (iii) semi-squattingto improvelower limb
strength and proprioception in the knees and ankles,(iv)
standing on a duraDisc to promote static balance,and
(v) walking across a surface covered with obstaclesto
improve dynamic walking balance.
Based on our practicalexperience ofusing TOBT in
previous studies of patients with chronic stroke [30,40],
the proposed frequency and intensity oftreatmentwill
be effective and tolerable,providing sufficientstimula-
tion to enhance motor recovery in patients with stroke.
In the TOBT sessions,the participants willtake turns in
carrying outone of the TOBT exercisesfor 8 min,
followed by a 1-min restinterval,until the five TOBT
exercises have been completed.All the TOBT sessions
will be held in the morning,and then the participants at-
tend either the CBT or GHE session on the same day in
the afternoon after a 2-hour lunch break.
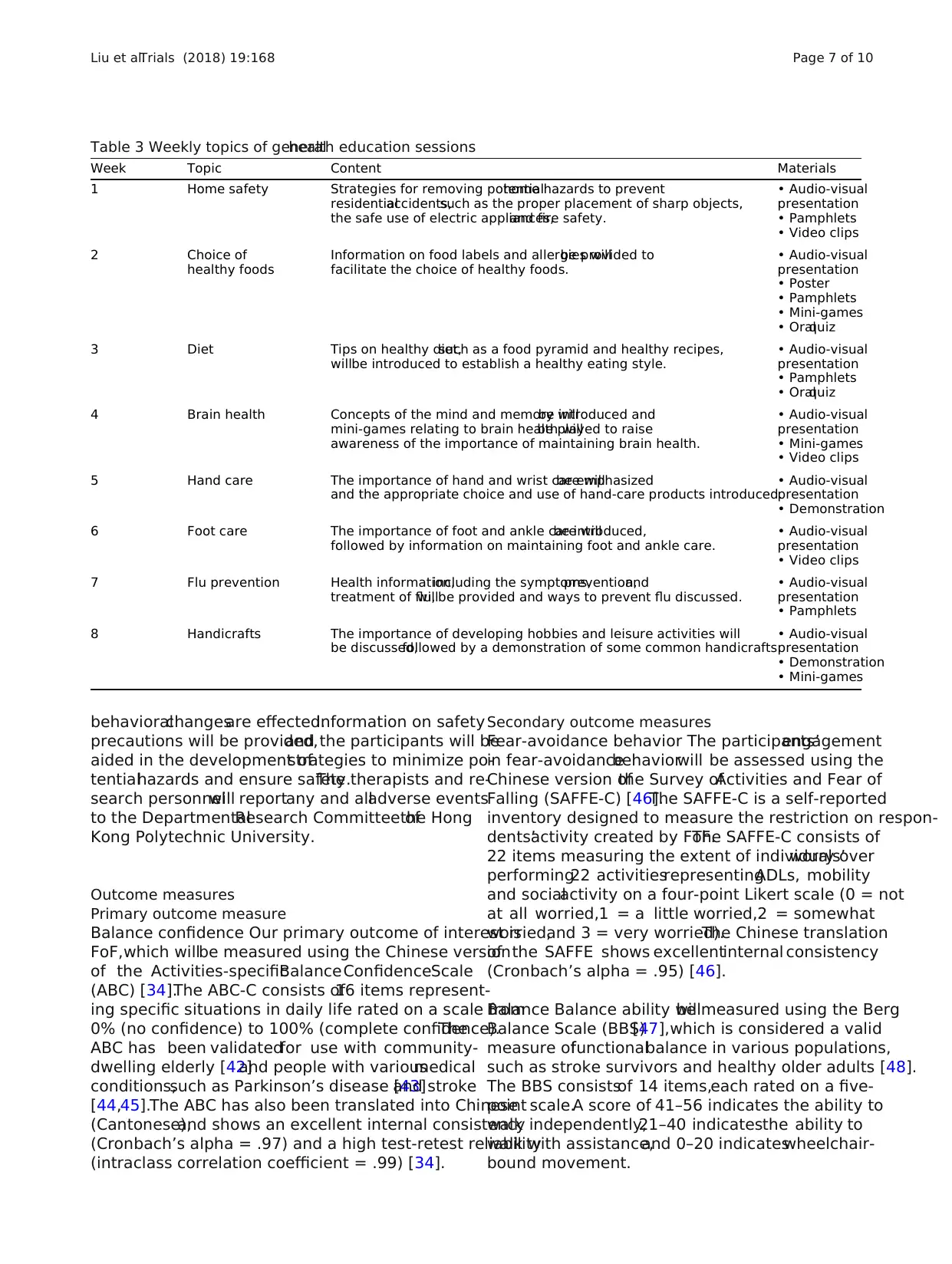
Experimental group
The experimentalgroup willreceive twice weekly CBT
sessions for 8 weeks,lasting for 45 min per session,in
groups of three to five.The CBT sessions will be focused
on eliminating cognitive and behavioralfactors known
to generate and aggravate impaired subjective balance
confidence and fear-avoidance behavior.The aim willbe
to increase the self-perception of efficacy regarding falls
and the sense of control over falling,to decrease the per-
ception of risk,and to help the participants adopt realis-
tic expectations of the consequences of falls.Each week
will have a specific theme in the CBT protocol.The
main themes and content are summarized in Table 2.
Weeks 1 and 2 of the CBT sessions will focus on intro-
ducing the CBT frameworkand showinghow self-
perceived capability and maladaptive thoughts can influ-
ence behavioralperformance.From week 3 to week 8,
two majortechniques,cognitive restructuring and be-
havioralmodification,will be used in the CBT sessions
Fig. 2 Flow diagram for clinicaltrial
Liu et al.Trials (2018) 19:168 Page 5 of 10
proved strength and balanceare gained through the
repetition of task-specific functional movements.
The TOBT intervention willconsistof five exercises
targeting muscle strength in the lower limbs and walking
performance:(i) stepping up and down in differentdi-
rections to strengthen the affected leg muscles and to in-
crease controlovershiftsin the centerof gravity,(ii)
heel-raising exercisesto strengthen theankleplantar
flexors, (iii) semi-squattingto improvelower limb
strength and proprioception in the knees and ankles,(iv)
standing on a duraDisc to promote static balance,and
(v) walking across a surface covered with obstaclesto
improve dynamic walking balance.
Based on our practicalexperience ofusing TOBT in
previous studies of patients with chronic stroke [30,40],
the proposed frequency and intensity oftreatmentwill
be effective and tolerable,providing sufficientstimula-
tion to enhance motor recovery in patients with stroke.
In the TOBT sessions,the participants willtake turns in
carrying outone of the TOBT exercisesfor 8 min,
followed by a 1-min restinterval,until the five TOBT
exercises have been completed.All the TOBT sessions
will be held in the morning,and then the participants at-
tend either the CBT or GHE session on the same day in
the afternoon after a 2-hour lunch break.
Experimental group
The experimentalgroup willreceive twice weekly CBT
sessions for 8 weeks,lasting for 45 min per session,in
groups of three to five.The CBT sessions will be focused
on eliminating cognitive and behavioralfactors known
to generate and aggravate impaired subjective balance
confidence and fear-avoidance behavior.The aim willbe
to increase the self-perception of efficacy regarding falls
and the sense of control over falling,to decrease the per-
ception of risk,and to help the participants adopt realis-
tic expectations of the consequences of falls.Each week
will have a specific theme in the CBT protocol.The
main themes and content are summarized in Table 2.
Weeks 1 and 2 of the CBT sessions will focus on intro-
ducing the CBT frameworkand showinghow self-
perceived capability and maladaptive thoughts can influ-
ence behavioralperformance.From week 3 to week 8,
two majortechniques,cognitive restructuring and be-
havioralmodification,will be used in the CBT sessions
Fig. 2 Flow diagram for clinicaltrial
Liu et al.Trials (2018) 19:168 Page 5 of 10
to achieve participants’personal goals.Cognitive restruc-
turing attainsthoughtalteration in the following four
steps:(1) identification of automatic thoughts,(2) exam-
ination of cognitivedistortion originating from auto-
maticthoughts,(3) disputing thecognitive distortion
and automatic thoughts,and (4) developing adaptive be-
liefs.In the proposed study,these fourstepswill be
undertaken in the form ofCBT homework assignments
and sharing and discussion during CBT group sessions.
After effecting cognitive restructuring,the CBT group
sessions will target behavioral modification,another cru-
cial component of the intervention.The participants will
be equipped to identify potentialrisks and develop be-
havioralstrategies to prepare them to increase their ac-
tivity levels safely.The CBT sessions willalso serve as a
platform forvicariouslearning,socialpersuasion,and
socialmodeling for the participants through group dis-
cussion and observing the success of others.In addition,
mastery experiences can be gained through the success-
ful application ofCBT in daily situations.Indeed,ac-
cording to Bandura [41],this is the major source of self-
efficacy.Therefore,the use of cognitive-restructuring
and behavioral-modification techniquesis expected to
enhance the participants’subjective balance confidence
and reduce their fear-related avoidance behavior.
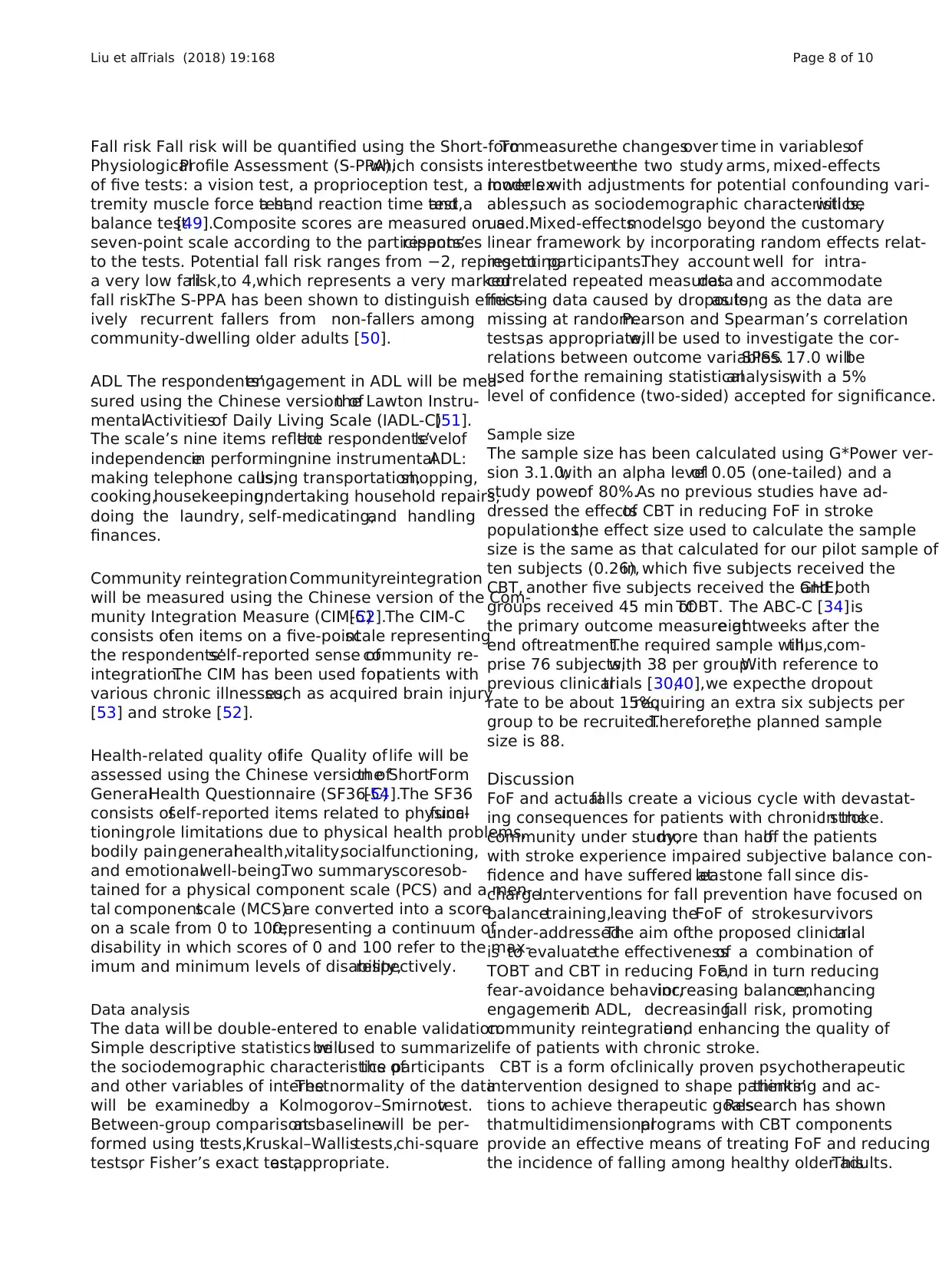
Control group
The controlgroup willattend 16 health talks (two ses-
sions per week for 45 min per session) delivered as an
inactiveattention placebo bya research assistantin
groups ofthree to five.The materials used in the GHE
sessions willinclude audio-visualpresentations,demon-
strations,video clips,mini-games,oral quizzes,and post-
ers and pamphlets on various health topics.The GHE
sessions willbe designed to raise awareness ofgeneral
health issuesand increasegeneralhealth knowledge
among an elderly population.The detailsof the GHE
sessions are summarized in Table 3.
Safety and adverse events
CBT is a clinically proven therapeutic intervention with
no known associated risks.However,as one of the aims
of CBT interventions is to promote independence,the
participantswill be instructed to increase theirADL,
physicalexercise,and socialparticipation.Potentialhaz-
ards willbe discussed in the CBT sessions before these
Table 2 Weekly themes and main content of CBT sessions
Week Weekly theme
1 Introduction and briefing on the aims of the rehabilitation program
• Introduction to group
• Introduction of the concept of self-efficacy
• Information on post-stroke balance self-efficacy and rehabilitation
2 Understanding the relationships between thoughts,emotions,and behavior
• Introduction to the CBT model
• Understanding fear,fear of falling,fallrisks,and actualfalls
• Understanding the automatic thoughts and emotionaland
behavioralreflection associated with fear of falling
3 Exploring thoughts and maladaptive responses
• Identifying maladaptive thoughts leading to physicalinactivity
• Adapting realistic views of fallrisk and the consequences of falls
• Recognizing risky behavior
• Overcoming barriers to physicalactivity
4 Exploring adaptive thoughts and behavioralresponses
• Fallprevention strategies and safety issues
• Recognizing and minimizing fallrisk
5 Implementing and reviewing behavioralchanges related to ADL
• Setting personalgoals for ADL
• Planning to achieve personalgoals in smallstages
• Recognizing potentialhazards and planning for safety
6 Implementing and reviewing behavioralchanges related to socialactivities
• Setting personalgoals for socialactivities
• Planning to achieve personalgoals in smallstages
• Recognizing potentialhazards and planning for safety
7 Reviewing and advancing individualtherapeutic goals
• Reviewing personalgoals for ADL and socialactivities
• Establishing a regular exercise plan
8 Consolidating the experiences of the rehabilitation program
• Sharing attitudes and experiences of fear of falling before and after the group
• Sharing experiences of applying cognitive-restructuring skills
• Establishing the long-term personalgoals of regular exercise,ADL independence,and socialengagement
ADL activities of daily living,CBT cognitive behavioraltherapy
Liu et al.Trials (2018) 19:168 Page 6 of 10
turing attainsthoughtalteration in the following four
steps:(1) identification of automatic thoughts,(2) exam-
ination of cognitivedistortion originating from auto-
maticthoughts,(3) disputing thecognitive distortion
and automatic thoughts,and (4) developing adaptive be-
liefs.In the proposed study,these fourstepswill be
undertaken in the form ofCBT homework assignments
and sharing and discussion during CBT group sessions.
After effecting cognitive restructuring,the CBT group
sessions will target behavioral modification,another cru-
cial component of the intervention.The participants will
be equipped to identify potentialrisks and develop be-
havioralstrategies to prepare them to increase their ac-
tivity levels safely.The CBT sessions willalso serve as a
platform forvicariouslearning,socialpersuasion,and
socialmodeling for the participants through group dis-
cussion and observing the success of others.In addition,
mastery experiences can be gained through the success-
ful application ofCBT in daily situations.Indeed,ac-
cording to Bandura [41],this is the major source of self-
efficacy.Therefore,the use of cognitive-restructuring
and behavioral-modification techniquesis expected to
enhance the participants’subjective balance confidence
and reduce their fear-related avoidance behavior.
Control group
The controlgroup willattend 16 health talks (two ses-
sions per week for 45 min per session) delivered as an
inactiveattention placebo bya research assistantin
groups ofthree to five.The materials used in the GHE
sessions willinclude audio-visualpresentations,demon-
strations,video clips,mini-games,oral quizzes,and post-
ers and pamphlets on various health topics.The GHE
sessions willbe designed to raise awareness ofgeneral
health issuesand increasegeneralhealth knowledge
among an elderly population.The detailsof the GHE
sessions are summarized in Table 3.
Safety and adverse events
CBT is a clinically proven therapeutic intervention with
no known associated risks.However,as one of the aims
of CBT interventions is to promote independence,the
participantswill be instructed to increase theirADL,
physicalexercise,and socialparticipation.Potentialhaz-
ards willbe discussed in the CBT sessions before these
Table 2 Weekly themes and main content of CBT sessions
Week Weekly theme
1 Introduction and briefing on the aims of the rehabilitation program
• Introduction to group
• Introduction of the concept of self-efficacy
• Information on post-stroke balance self-efficacy and rehabilitation
2 Understanding the relationships between thoughts,emotions,and behavior
• Introduction to the CBT model
• Understanding fear,fear of falling,fallrisks,and actualfalls
• Understanding the automatic thoughts and emotionaland
behavioralreflection associated with fear of falling
3 Exploring thoughts and maladaptive responses
• Identifying maladaptive thoughts leading to physicalinactivity
• Adapting realistic views of fallrisk and the consequences of falls
• Recognizing risky behavior
• Overcoming barriers to physicalactivity
4 Exploring adaptive thoughts and behavioralresponses
• Fallprevention strategies and safety issues
• Recognizing and minimizing fallrisk
5 Implementing and reviewing behavioralchanges related to ADL
• Setting personalgoals for ADL
• Planning to achieve personalgoals in smallstages
• Recognizing potentialhazards and planning for safety
6 Implementing and reviewing behavioralchanges related to socialactivities
• Setting personalgoals for socialactivities
• Planning to achieve personalgoals in smallstages
• Recognizing potentialhazards and planning for safety
7 Reviewing and advancing individualtherapeutic goals
• Reviewing personalgoals for ADL and socialactivities
• Establishing a regular exercise plan
8 Consolidating the experiences of the rehabilitation program
• Sharing attitudes and experiences of fear of falling before and after the group
• Sharing experiences of applying cognitive-restructuring skills
• Establishing the long-term personalgoals of regular exercise,ADL independence,and socialengagement
ADL activities of daily living,CBT cognitive behavioraltherapy
Liu et al.Trials (2018) 19:168 Page 6 of 10
behavioralchangesare effected.Information on safety
precautions will be provided,and the participants will be
aided in the development ofstrategies to minimize po-
tentialhazards and ensure safety.The therapists and re-
search personnelwill reportany and alladverse events
to the DepartmentalResearch Committee ofthe Hong
Kong Polytechnic University.
Outcome measures
Primary outcome measure
Balance confidence Our primary outcome of interest is
FoF,which willbe measured using the Chinese version
of the Activities-specificBalanceConfidenceScale
(ABC) [34].The ABC-C consists of16 items represent-
ing specific situations in daily life rated on a scale from
0% (no confidence) to 100% (complete confidence).The
ABC has been validatedfor use with community-
dwelling elderly [42]and people with variousmedical
conditions,such as Parkinson’s disease [43]and stroke
[44,45].The ABC has also been translated into Chinese
(Cantonese),and shows an excellent internal consistency
(Cronbach’s alpha = .97) and a high test-retest reliability
(intraclass correlation coefficient = .99) [34].
Secondary outcome measures
Fear-avoidance behavior The participants’engagement
in fear-avoidancebehaviorwill be assessed using the
Chinese version ofthe Survey ofActivities and Fear of
Falling (SAFFE-C) [46].The SAFFE-C is a self-reported
inventory designed to measure the restriction on respon-
dents’activity created by FoF.The SAFFE-C consists of
22 items measuring the extent of individuals’worry over
performing22 activitiesrepresentingADLs, mobility
and socialactivity on a four-point Likert scale (0 = not
at all worried,1 = a little worried,2 = somewhat
worried,and 3 = very worried).The Chinese translation
of the SAFFE shows excellentinternal consistency
(Cronbach’s alpha = .95) [46].
Balance Balance ability willbe measured using the Berg
Balance Scale (BBS)[47],which is considered a valid
measure offunctionalbalance in various populations,
such as stroke survivors and healthy older adults [48].
The BBS consistsof 14 items,each rated on a five-
point scale.A score of 41–56 indicates the ability to
walk independently,21–40 indicatesthe ability to
walk with assistance,and 0–20 indicateswheelchair-
bound movement.
Table 3 Weekly topics of generalhealth education sessions
Week Topic Content Materials
1 Home safety Strategies for removing potentialhome hazards to prevent
residentialaccidents,such as the proper placement of sharp objects,
the safe use of electric appliances,and fire safety.
• Audio-visual
presentation
• Pamphlets
• Video clips
2 Choice of
healthy foods
Information on food labels and allergies willbe provided to
facilitate the choice of healthy foods.
• Audio-visual
presentation
• Poster
• Pamphlets
• Mini-games
• Oralquiz
3 Diet Tips on healthy diet,such as a food pyramid and healthy recipes,
willbe introduced to establish a healthy eating style.
• Audio-visual
presentation
• Pamphlets
• Oralquiz
4 Brain health Concepts of the mind and memory willbe introduced and
mini-games relating to brain health willbe played to raise
awareness of the importance of maintaining brain health.
• Audio-visual
presentation
• Mini-games
• Video clips
5 Hand care The importance of hand and wrist care willbe emphasized
and the appropriate choice and use of hand-care products introduced.
• Audio-visual
presentation
• Demonstration
6 Foot care The importance of foot and ankle care willbe introduced,
followed by information on maintaining foot and ankle care.
• Audio-visual
presentation
• Video clips
7 Flu prevention Health information,including the symptoms,prevention,and
treatment of flu,willbe provided and ways to prevent flu discussed.
• Audio-visual
presentation
• Pamphlets
8 Handicrafts The importance of developing hobbies and leisure activities will
be discussed,followed by a demonstration of some common handicrafts.
• Audio-visual
presentation
• Demonstration
• Mini-games
Liu et al.Trials (2018) 19:168 Page 7 of 10
precautions will be provided,and the participants will be
aided in the development ofstrategies to minimize po-
tentialhazards and ensure safety.The therapists and re-
search personnelwill reportany and alladverse events
to the DepartmentalResearch Committee ofthe Hong
Kong Polytechnic University.
Outcome measures
Primary outcome measure
Balance confidence Our primary outcome of interest is
FoF,which willbe measured using the Chinese version
of the Activities-specificBalanceConfidenceScale
(ABC) [34].The ABC-C consists of16 items represent-
ing specific situations in daily life rated on a scale from
0% (no confidence) to 100% (complete confidence).The
ABC has been validatedfor use with community-
dwelling elderly [42]and people with variousmedical
conditions,such as Parkinson’s disease [43]and stroke
[44,45].The ABC has also been translated into Chinese
(Cantonese),and shows an excellent internal consistency
(Cronbach’s alpha = .97) and a high test-retest reliability
(intraclass correlation coefficient = .99) [34].
Secondary outcome measures
Fear-avoidance behavior The participants’engagement
in fear-avoidancebehaviorwill be assessed using the
Chinese version ofthe Survey ofActivities and Fear of
Falling (SAFFE-C) [46].The SAFFE-C is a self-reported
inventory designed to measure the restriction on respon-
dents’activity created by FoF.The SAFFE-C consists of
22 items measuring the extent of individuals’worry over
performing22 activitiesrepresentingADLs, mobility
and socialactivity on a four-point Likert scale (0 = not
at all worried,1 = a little worried,2 = somewhat
worried,and 3 = very worried).The Chinese translation
of the SAFFE shows excellentinternal consistency
(Cronbach’s alpha = .95) [46].
Balance Balance ability willbe measured using the Berg
Balance Scale (BBS)[47],which is considered a valid
measure offunctionalbalance in various populations,
such as stroke survivors and healthy older adults [48].
The BBS consistsof 14 items,each rated on a five-
point scale.A score of 41–56 indicates the ability to
walk independently,21–40 indicatesthe ability to
walk with assistance,and 0–20 indicateswheelchair-
bound movement.
Table 3 Weekly topics of generalhealth education sessions
Week Topic Content Materials
1 Home safety Strategies for removing potentialhome hazards to prevent
residentialaccidents,such as the proper placement of sharp objects,
the safe use of electric appliances,and fire safety.
• Audio-visual
presentation
• Pamphlets
• Video clips
2 Choice of
healthy foods
Information on food labels and allergies willbe provided to
facilitate the choice of healthy foods.
• Audio-visual
presentation
• Poster
• Pamphlets
• Mini-games
• Oralquiz
3 Diet Tips on healthy diet,such as a food pyramid and healthy recipes,
willbe introduced to establish a healthy eating style.
• Audio-visual
presentation
• Pamphlets
• Oralquiz
4 Brain health Concepts of the mind and memory willbe introduced and
mini-games relating to brain health willbe played to raise
awareness of the importance of maintaining brain health.
• Audio-visual
presentation
• Mini-games
• Video clips
5 Hand care The importance of hand and wrist care willbe emphasized
and the appropriate choice and use of hand-care products introduced.
• Audio-visual
presentation
• Demonstration
6 Foot care The importance of foot and ankle care willbe introduced,
followed by information on maintaining foot and ankle care.
• Audio-visual
presentation
• Video clips
7 Flu prevention Health information,including the symptoms,prevention,and
treatment of flu,willbe provided and ways to prevent flu discussed.
• Audio-visual
presentation
• Pamphlets
8 Handicrafts The importance of developing hobbies and leisure activities will
be discussed,followed by a demonstration of some common handicrafts.
• Audio-visual
presentation
• Demonstration
• Mini-games
Liu et al.Trials (2018) 19:168 Page 7 of 10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Fall risk Fall risk will be quantified using the Short-form
PhysiologicalProfile Assessment (S-PPA),which consists
of five tests: a vision test, a proprioception test, a lower ex-
tremity muscle force test,a hand reaction time test,and a
balance test[49].Composite scores are measured on a
seven-point scale according to the participants’responses
to the tests. Potential fall risk ranges from −2, representing
a very low fallrisk,to 4,which represents a very marked
fall risk.The S-PPA has been shown to distinguish effect-
ively recurrent fallers from non-fallers among
community-dwelling older adults [50].
ADL The respondents’engagement in ADL will be mea-
sured using the Chinese version ofthe Lawton Instru-
mentalActivitiesof Daily Living Scale (IADL-C)[51].
The scale’s nine items reflectthe respondents’levelof
independencein performingnine instrumentalADL:
making telephone calls,using transportation,shopping,
cooking,housekeeping,undertaking household repairs,
doing the laundry, self-medicating,and handling
finances.
Community reintegration Communityreintegration
will be measured using the Chinese version of the Com-
munity Integration Measure (CIM-C)[52].The CIM-C
consists often items on a five-pointscale representing
the respondents’self-reported sense ofcommunity re-
integration.The CIM has been used forpatients with
various chronic illnesses,such as acquired brain injury
[53] and stroke [52].
Health-related quality oflife Quality oflife will be
assessed using the Chinese version ofthe ShortForm
GeneralHealth Questionnaire (SF36-C)[54].The SF36
consists ofself-reported items related to physicalfunc-
tioning,role limitations due to physical health problems,
bodily pain,generalhealth,vitality,socialfunctioning,
and emotionalwell-being.Two summaryscoresob-
tained for a physical component scale (PCS) and a men-
tal componentscale (MCS)are converted into a score
on a scale from 0 to 100,representing a continuum of
disability in which scores of 0 and 100 refer to the max-
imum and minimum levels of disability,respectively.
Data analysis
The data will be double-entered to enable validation.
Simple descriptive statistics willbe used to summarize
the sociodemographic characteristics ofthe participants
and other variables of interest.The normality of the data
will be examinedby a Kolmogorov–Smirnovtest.
Between-group comparisonsat baselinewill be per-
formed using ttests,Kruskal–Wallistests,chi-square
tests,or Fisher’s exact test,as appropriate.
To measurethe changesover time in variablesof
interestbetweenthe two study arms, mixed-effects
models with adjustments for potential confounding vari-
ables,such as sociodemographic characteristics,will be
used.Mixed-effectsmodelsgo beyond the customary
linear framework by incorporating random effects relat-
ing to participants.They account well for intra-
correlated repeated measuresdata and accommodate
missing data caused by dropouts,as long as the data are
missing at random.Pearson and Spearman’s correlation
tests,as appropriate,will be used to investigate the cor-
relations between outcome variables.SPSS 17.0 willbe
used for the remaining statisticalanalysis,with a 5%
level of confidence (two-sided) accepted for significance.
Sample size
The sample size has been calculated using G*Power ver-
sion 3.1.0,with an alpha levelof 0.05 (one-tailed) and a
study powerof 80%.As no previous studies have ad-
dressed the effectsof CBT in reducing FoF in stroke
populations,the effect size used to calculate the sample
size is the same as that calculated for our pilot sample of
ten subjects (0.26),in which five subjects received the
CBT, another five subjects received the GHE,and both
groups received 45 min ofTOBT. The ABC-C [34]is
the primary outcome measure ateightweeks after the
end oftreatment.The required sample will,thus,com-
prise 76 subjects,with 38 per group.With reference to
previous clinicaltrials [30,40],we expectthe dropout
rate to be about 15%,requiring an extra six subjects per
group to be recruited.Therefore,the planned sample
size is 88.
Discussion
FoF and actualfalls create a vicious cycle with devastat-
ing consequences for patients with chronic stroke.In the
community under study,more than halfof the patients
with stroke experience impaired subjective balance con-
fidence and have suffered atleastone fall since dis-
charge.Interventions for fall prevention have focused on
balancetraining,leaving theFoF of strokesurvivors
under-addressed.The aim ofthe proposed clinicaltrial
is to evaluatethe effectivenessof a combination of
TOBT and CBT in reducing FoF,and in turn reducing
fear-avoidance behavior,increasing balance,enhancing
engagementin ADL, decreasingfall risk, promoting
community reintegration,and enhancing the quality of
life of patients with chronic stroke.
CBT is a form ofclinically proven psychotherapeutic
intervention designed to shape patients’thinking and ac-
tions to achieve therapeutic goals.Research has shown
thatmultidimensionalprograms with CBT components
provide an effective means of treating FoF and reducing
the incidence of falling among healthy older adults.This
Liu et al.Trials (2018) 19:168 Page 8 of 10
PhysiologicalProfile Assessment (S-PPA),which consists
of five tests: a vision test, a proprioception test, a lower ex-
tremity muscle force test,a hand reaction time test,and a
balance test[49].Composite scores are measured on a
seven-point scale according to the participants’responses
to the tests. Potential fall risk ranges from −2, representing
a very low fallrisk,to 4,which represents a very marked
fall risk.The S-PPA has been shown to distinguish effect-
ively recurrent fallers from non-fallers among
community-dwelling older adults [50].
ADL The respondents’engagement in ADL will be mea-
sured using the Chinese version ofthe Lawton Instru-
mentalActivitiesof Daily Living Scale (IADL-C)[51].
The scale’s nine items reflectthe respondents’levelof
independencein performingnine instrumentalADL:
making telephone calls,using transportation,shopping,
cooking,housekeeping,undertaking household repairs,
doing the laundry, self-medicating,and handling
finances.
Community reintegration Communityreintegration
will be measured using the Chinese version of the Com-
munity Integration Measure (CIM-C)[52].The CIM-C
consists often items on a five-pointscale representing
the respondents’self-reported sense ofcommunity re-
integration.The CIM has been used forpatients with
various chronic illnesses,such as acquired brain injury
[53] and stroke [52].
Health-related quality oflife Quality oflife will be
assessed using the Chinese version ofthe ShortForm
GeneralHealth Questionnaire (SF36-C)[54].The SF36
consists ofself-reported items related to physicalfunc-
tioning,role limitations due to physical health problems,
bodily pain,generalhealth,vitality,socialfunctioning,
and emotionalwell-being.Two summaryscoresob-
tained for a physical component scale (PCS) and a men-
tal componentscale (MCS)are converted into a score
on a scale from 0 to 100,representing a continuum of
disability in which scores of 0 and 100 refer to the max-
imum and minimum levels of disability,respectively.
Data analysis
The data will be double-entered to enable validation.
Simple descriptive statistics willbe used to summarize
the sociodemographic characteristics ofthe participants
and other variables of interest.The normality of the data
will be examinedby a Kolmogorov–Smirnovtest.
Between-group comparisonsat baselinewill be per-
formed using ttests,Kruskal–Wallistests,chi-square
tests,or Fisher’s exact test,as appropriate.
To measurethe changesover time in variablesof
interestbetweenthe two study arms, mixed-effects
models with adjustments for potential confounding vari-
ables,such as sociodemographic characteristics,will be
used.Mixed-effectsmodelsgo beyond the customary
linear framework by incorporating random effects relat-
ing to participants.They account well for intra-
correlated repeated measuresdata and accommodate
missing data caused by dropouts,as long as the data are
missing at random.Pearson and Spearman’s correlation
tests,as appropriate,will be used to investigate the cor-
relations between outcome variables.SPSS 17.0 willbe
used for the remaining statisticalanalysis,with a 5%
level of confidence (two-sided) accepted for significance.
Sample size
The sample size has been calculated using G*Power ver-
sion 3.1.0,with an alpha levelof 0.05 (one-tailed) and a
study powerof 80%.As no previous studies have ad-
dressed the effectsof CBT in reducing FoF in stroke
populations,the effect size used to calculate the sample
size is the same as that calculated for our pilot sample of
ten subjects (0.26),in which five subjects received the
CBT, another five subjects received the GHE,and both
groups received 45 min ofTOBT. The ABC-C [34]is
the primary outcome measure ateightweeks after the
end oftreatment.The required sample will,thus,com-
prise 76 subjects,with 38 per group.With reference to
previous clinicaltrials [30,40],we expectthe dropout
rate to be about 15%,requiring an extra six subjects per
group to be recruited.Therefore,the planned sample
size is 88.
Discussion
FoF and actualfalls create a vicious cycle with devastat-
ing consequences for patients with chronic stroke.In the
community under study,more than halfof the patients
with stroke experience impaired subjective balance con-
fidence and have suffered atleastone fall since dis-
charge.Interventions for fall prevention have focused on
balancetraining,leaving theFoF of strokesurvivors
under-addressed.The aim ofthe proposed clinicaltrial
is to evaluatethe effectivenessof a combination of
TOBT and CBT in reducing FoF,and in turn reducing
fear-avoidance behavior,increasing balance,enhancing
engagementin ADL, decreasingfall risk, promoting
community reintegration,and enhancing the quality of
life of patients with chronic stroke.
CBT is a form ofclinically proven psychotherapeutic
intervention designed to shape patients’thinking and ac-
tions to achieve therapeutic goals.Research has shown
thatmultidimensionalprograms with CBT components
provide an effective means of treating FoF and reducing
the incidence of falling among healthy older adults.This
Liu et al.Trials (2018) 19:168 Page 8 of 10
shedslight on the effectson stroke recovery ofCBT
combined with customary physicaltraining.The inclu-
sion ofCBT with customary physicaltraining willhelp
to break the viciouscycle ofFoF and actualfalls and
thus, enhancethe rehabilitativeoutcomesof patients
with chronic stroke.
One of the limitations ofthis study is notcollecting
data on actualfalls.However,the main purpose ofthis
study is to evaluate the augmenting effects ofCBT on
existing physiotherapy in enhancing subjective balance
confidence.The occurrence of post-stroke falls is a com-
plex issue involving the interplay between physical,psy-
chological,behavioral,and environmental factors.Future
studies could further examine the roles of subjective bal-
ance confidence in developing fallprevention strategies
for patients with stroke.Besides,this study may involve
community-dwelling stroke patients with a range of bal-
ance ability levels.Thus,the use of BBS may not be ad-
equately sensitive to capture the balance improvement
among subjects with mildly affected balance ability.
It is hoped thatthe results ofthis study willprovide
scientific evidence supporting the use ofCBT to aug-
ment the effects ofphysiotherapy in enhancing subject-
ive balance confidence and thus,stroke rehabilitation.If
effective,our intervention will offer a safe,cost-effective,
and readily transferrable therapeutic approach to clinical
practice thatreduces fear-avoidance behaviors and fall
risk, improvesbalance and levelof independence,en-
hances health-related quality of life,and decreases asso-
ciated healthcare costs.
Trial status
Recruitmentstarted in October2016.We targetto
complete recruitment during 2017.
Abbreviations
ABC-C:Chinese version of the Activities-specific Balance Confidence Scale;
ADL:Activities of daily living;BBS:Berg Balance Scale;CBT:Cognitive
behavioraltherapy;CIM-C:Chinese version of the Community Integration
Measure;FoF:Fear of falling;GHE:Generalhealth education;IADL-C:Lawton
InstrumentalActivities of Daily Living (Chinese version);RCT:Randomized
controlled trial;SAFFE-C:Chinese version of the Survey of Activities and Fear
of Falling in the Elderly;SF36-C MCS:Mentalcomponent of the Chinese
version of the Short Form GeneralHealth Questionnaire;SF36-C PCS:Physical
component of the Chinese version of the Short Form GeneralHealth
Questionnaire;S-PPA:Short-form PhysiologicalProfile Assessment;
TOBT:Task-oriented balance training
Acknowledgements
We would like to thank allof the study’s participants.We would also like to
thank Dr.Raymond Chung for his statisticaladvice,Mr.Patrick Kwong for his
advice on TOBT,and Ms.Lee HoiKiand Mr.Wong SuiLung for their
expertise in CBT.
Funding
This study was supported by a departmentalresearch grant (1-ZVF9) from
the Hong Kong Polytechnic University to SSMN and her team.
Availability of data and materials
The datasets generated and/or analyzed during the current study are
available from the corresponding author on reasonable request.
Authors’contributions
SN conceived and helped to design the study.GN advised on the design of
the trial.SN and TL carried out the recruitment,training of research
personnel,and the collection.TL drafted the manuscript.SN and GN
reviewed and amended the manuscript.Allof the authors approved the final
manuscript.
Ethics approval and consent to participate
The DepartmentalResearch Committee of the Hong Kong Polytechnic
University has approved the research protocol(HSEARS20131012002–01).
Written informed consent willbe obtained from allof the participants before
the study.The clinicaltrialwillfollow allof the guidelines set out in the
Declaration of Helsinki.
Consent for publication
Consent for participation and consent for publication willbe obtained
simultaneously via a signed written consent form.
Competing interests
The authors declare that they have no competing interests with respect to
either the authorship or the publication of this paper.
Publisher’s Note
Springer Nature remains neutralwith regard to jurisdictionalclaims in
published maps and institutionalaffiliations.
Author details
1Department of Rehabilitation Sciences,The Hong Kong Polytechnic
University,Hung Hom,Hong Kong,SpecialAdministrative Region of China.
2Division of Nursing and Health Studies,The Open University of Hong Kong,
Ho Man Tin,Hong Kong,SpecialAdministrative Region of China.
Received:24 April2017 Accepted:15 February 2018
References
1. Friedman SM,Munoz B,West SK,Rubin GS,Fried L.Falls and fear of falling:
which come first? A longitudinalprediction modelsuggests strategies for
primary and secondary prevention.J Am Geriatr Soc.2002;50:1329–35.
2. Lachman ME,Howland J,Tennstedt S,Jette A,Assman S,Peterson WE.Fear
of falling and activity restriction:The Survey of Activities and Fear of Falling
in the Elderly (SAFE).J GerontolB PsycholSciSoc Sci.1998;53B(1):43–50.
3. TinettiME,Richman D,PowellL.Falls efficacy as a measure of fear of falling.
J Gerontol.1990;45:239–43.
4. PowellLE,Meyers AM.The activities-specific balance confidence (ABC) scale.
J GerontolA BiolSciMed Sci.1995;50(1):M28–34.
5. Schmid AA,Acuff M,Doster K,Gwaltney-Duiser A,Whitaker A,Damush T,
et al.Poststroke fear of falling in the hospitalsetting.Top Stroke Rehabil.
2009;16(5):357–66.
6. Schmid AA,Van Puymbroeck M,Knies K,Spangler-Morris C,Watts K,
Damush T,et al.Fear of falling among people who have sustained a stroke:
a 6-month longitudinalpilot study.OTJR.2011;65:125–32.
7. Liu TW,Ng SSM,Kwong PWH,Ng GYF.Performance of muscles,functional
mobility,and posturalstability in stroke survivors with impaired subjective
balance confidence.Asian J GerontolGeriatr.2015;10(1):54.
8. Pang MYC,Eng JJ.Fall-related self-efficacy,not balance and mobility
performance,is related to accidentalfalls in chronic stroke survivors with
low bone mineraldensity.Osteoporos Int.2008;19(7):919–27.
9. Pang MYC,Eng JJ,Miller WC.Determinants of satisfaction with community
reintegration in older adults with chronic stroke:role of balance self-
efficacy.Phys Ther.2007;87(3):282–91.
10. Bula CJ,Monod S,Hoskovec C,Rochat S.Interventions aiming at balance
confidence improvement in older adults:an updated review.Gerontology.
2011;57:276–86.
11. Sattin RW,Easley KA,Wolf SL,Chen Y,Kutner MH.Reduction in fear of
falling through intense taichiexercise training in older,transitionally frail
adults.J Am Geriatr Soc.2005;53:1168–78.
Liu et al.Trials (2018) 19:168 Page 9 of 10
combined with customary physicaltraining.The inclu-
sion ofCBT with customary physicaltraining willhelp
to break the viciouscycle ofFoF and actualfalls and
thus, enhancethe rehabilitativeoutcomesof patients
with chronic stroke.
One of the limitations ofthis study is notcollecting
data on actualfalls.However,the main purpose ofthis
study is to evaluate the augmenting effects ofCBT on
existing physiotherapy in enhancing subjective balance
confidence.The occurrence of post-stroke falls is a com-
plex issue involving the interplay between physical,psy-
chological,behavioral,and environmental factors.Future
studies could further examine the roles of subjective bal-
ance confidence in developing fallprevention strategies
for patients with stroke.Besides,this study may involve
community-dwelling stroke patients with a range of bal-
ance ability levels.Thus,the use of BBS may not be ad-
equately sensitive to capture the balance improvement
among subjects with mildly affected balance ability.
It is hoped thatthe results ofthis study willprovide
scientific evidence supporting the use ofCBT to aug-
ment the effects ofphysiotherapy in enhancing subject-
ive balance confidence and thus,stroke rehabilitation.If
effective,our intervention will offer a safe,cost-effective,
and readily transferrable therapeutic approach to clinical
practice thatreduces fear-avoidance behaviors and fall
risk, improvesbalance and levelof independence,en-
hances health-related quality of life,and decreases asso-
ciated healthcare costs.
Trial status
Recruitmentstarted in October2016.We targetto
complete recruitment during 2017.
Abbreviations
ABC-C:Chinese version of the Activities-specific Balance Confidence Scale;
ADL:Activities of daily living;BBS:Berg Balance Scale;CBT:Cognitive
behavioraltherapy;CIM-C:Chinese version of the Community Integration
Measure;FoF:Fear of falling;GHE:Generalhealth education;IADL-C:Lawton
InstrumentalActivities of Daily Living (Chinese version);RCT:Randomized
controlled trial;SAFFE-C:Chinese version of the Survey of Activities and Fear
of Falling in the Elderly;SF36-C MCS:Mentalcomponent of the Chinese
version of the Short Form GeneralHealth Questionnaire;SF36-C PCS:Physical
component of the Chinese version of the Short Form GeneralHealth
Questionnaire;S-PPA:Short-form PhysiologicalProfile Assessment;
TOBT:Task-oriented balance training
Acknowledgements
We would like to thank allof the study’s participants.We would also like to
thank Dr.Raymond Chung for his statisticaladvice,Mr.Patrick Kwong for his
advice on TOBT,and Ms.Lee HoiKiand Mr.Wong SuiLung for their
expertise in CBT.
Funding
This study was supported by a departmentalresearch grant (1-ZVF9) from
the Hong Kong Polytechnic University to SSMN and her team.
Availability of data and materials
The datasets generated and/or analyzed during the current study are
available from the corresponding author on reasonable request.
Authors’contributions
SN conceived and helped to design the study.GN advised on the design of
the trial.SN and TL carried out the recruitment,training of research
personnel,and the collection.TL drafted the manuscript.SN and GN
reviewed and amended the manuscript.Allof the authors approved the final
manuscript.
Ethics approval and consent to participate
The DepartmentalResearch Committee of the Hong Kong Polytechnic
University has approved the research protocol(HSEARS20131012002–01).
Written informed consent willbe obtained from allof the participants before
the study.The clinicaltrialwillfollow allof the guidelines set out in the
Declaration of Helsinki.
Consent for publication
Consent for participation and consent for publication willbe obtained
simultaneously via a signed written consent form.
Competing interests
The authors declare that they have no competing interests with respect to
either the authorship or the publication of this paper.
Publisher’s Note
Springer Nature remains neutralwith regard to jurisdictionalclaims in
published maps and institutionalaffiliations.
Author details
1Department of Rehabilitation Sciences,The Hong Kong Polytechnic
University,Hung Hom,Hong Kong,SpecialAdministrative Region of China.
2Division of Nursing and Health Studies,The Open University of Hong Kong,
Ho Man Tin,Hong Kong,SpecialAdministrative Region of China.
Received:24 April2017 Accepted:15 February 2018
References
1. Friedman SM,Munoz B,West SK,Rubin GS,Fried L.Falls and fear of falling:
which come first? A longitudinalprediction modelsuggests strategies for
primary and secondary prevention.J Am Geriatr Soc.2002;50:1329–35.
2. Lachman ME,Howland J,Tennstedt S,Jette A,Assman S,Peterson WE.Fear
of falling and activity restriction:The Survey of Activities and Fear of Falling
in the Elderly (SAFE).J GerontolB PsycholSciSoc Sci.1998;53B(1):43–50.
3. TinettiME,Richman D,PowellL.Falls efficacy as a measure of fear of falling.
J Gerontol.1990;45:239–43.
4. PowellLE,Meyers AM.The activities-specific balance confidence (ABC) scale.
J GerontolA BiolSciMed Sci.1995;50(1):M28–34.
5. Schmid AA,Acuff M,Doster K,Gwaltney-Duiser A,Whitaker A,Damush T,
et al.Poststroke fear of falling in the hospitalsetting.Top Stroke Rehabil.
2009;16(5):357–66.
6. Schmid AA,Van Puymbroeck M,Knies K,Spangler-Morris C,Watts K,
Damush T,et al.Fear of falling among people who have sustained a stroke:
a 6-month longitudinalpilot study.OTJR.2011;65:125–32.
7. Liu TW,Ng SSM,Kwong PWH,Ng GYF.Performance of muscles,functional
mobility,and posturalstability in stroke survivors with impaired subjective
balance confidence.Asian J GerontolGeriatr.2015;10(1):54.
8. Pang MYC,Eng JJ.Fall-related self-efficacy,not balance and mobility
performance,is related to accidentalfalls in chronic stroke survivors with
low bone mineraldensity.Osteoporos Int.2008;19(7):919–27.
9. Pang MYC,Eng JJ,Miller WC.Determinants of satisfaction with community
reintegration in older adults with chronic stroke:role of balance self-
efficacy.Phys Ther.2007;87(3):282–91.
10. Bula CJ,Monod S,Hoskovec C,Rochat S.Interventions aiming at balance
confidence improvement in older adults:an updated review.Gerontology.
2011;57:276–86.
11. Sattin RW,Easley KA,Wolf SL,Chen Y,Kutner MH.Reduction in fear of
falling through intense taichiexercise training in older,transitionally frail
adults.J Am Geriatr Soc.2005;53:1168–78.
Liu et al.Trials (2018) 19:168 Page 9 of 10
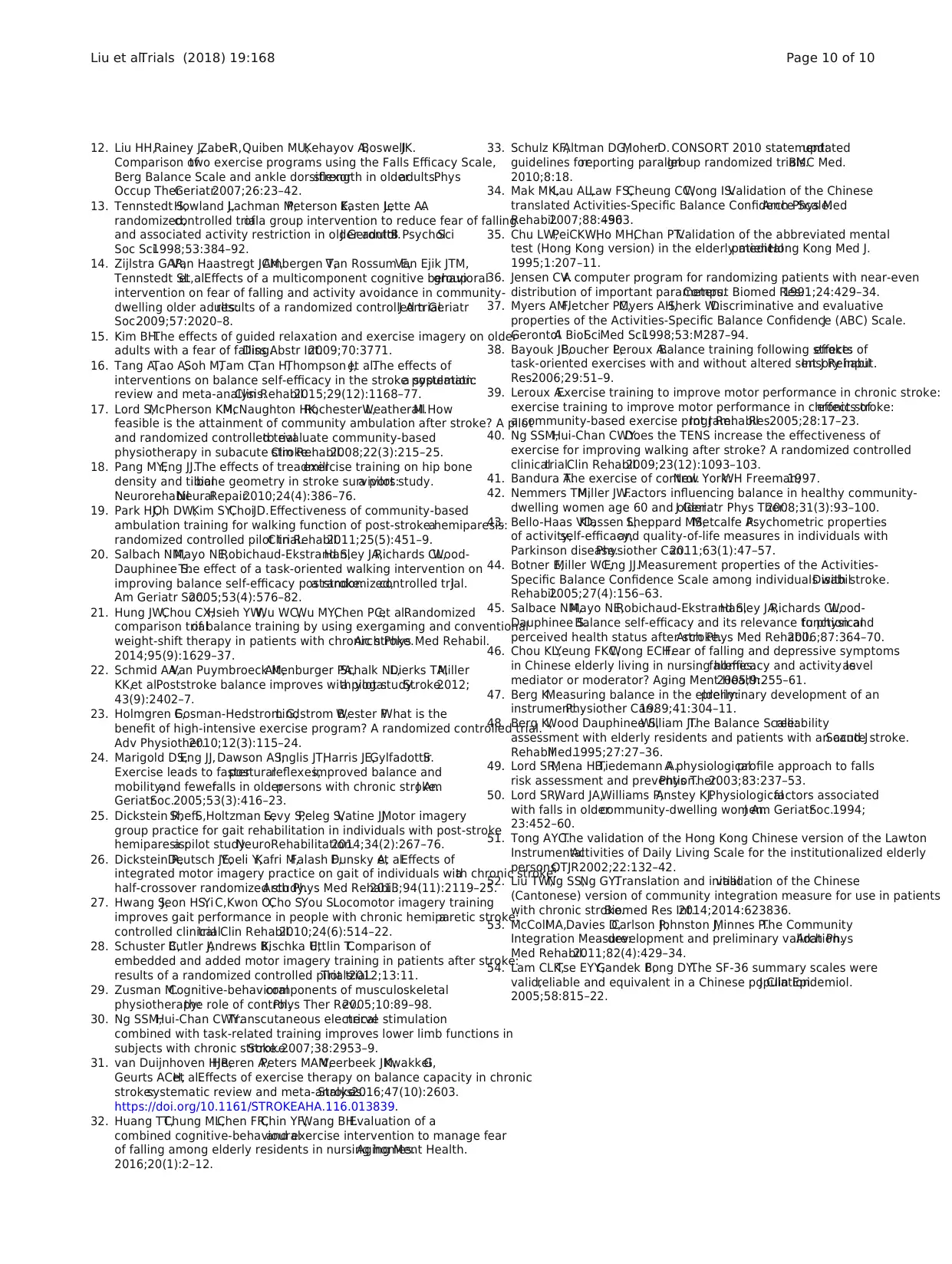
12. Liu HH,Rainey J,ZabelR,Quiben MU,Kehayov A,BoswellJK.
Comparison oftwo exercise programs using the Falls Efficacy Scale,
Berg Balance Scale and ankle dorsiflexorstrength in olderadults.Phys
Occup TherGeriatr.2007;26:23–42.
13. Tennstedt S,Howland J,Lachman M,Peterson E,Kasten L,Jette A.A
randomized,controlled trialof a group intervention to reduce fear of falling
and associated activity restriction in older adults.J GerontolB PsycholSci
Soc Sci.1998;53:384–92.
14. Zijlstra GAR,Van Haastregt JCM,Ambergen T,Van Rossum E,Van Ejik JTM,
Tennstedt SL,et al.Effects of a multicomponent cognitive behavioralgroup
intervention on fear of falling and activity avoidance in community-
dwelling older adults:results of a randomized controlled trial.J Am Geriatr
Soc.2009;57:2020–8.
15. Kim BH.The effects of guided relaxation and exercise imagery on older
adults with a fear of falling.Diss Abstr Int.2009;70:3771.
16. Tang A,Tao A,Soh M,Tam C,Tan H,Thompson J,et al.The effects of
interventions on balance self-efficacy in the stroke population:a systematic
review and meta-analysis.Clin Rehabil.2015;29(12):1168–77.
17. Lord S,McPherson KM,McNaughton HK,Rochester L,WeatherallM.How
feasible is the attainment of community ambulation after stroke? A pilot
and randomized controlled trialto evaluate community-based
physiotherapy in subacute stroke.Clin Rehabil.2008;22(3):215–25.
18. Pang MY,Eng JJ.The effects of treadmillexercise training on hip bone
density and tibialbone geometry in stroke survivors:a pilot study.
NeurorehabilNeuralRepair.2010;24(4):386–76.
19. Park HJ,Oh DW,Kim SY,ChoiJD.Effectiveness of community-based
ambulation training for walking function of post-stroke hemiparesis:a
randomized controlled pilot trial.Clin Rehabil.2011;25(5):451–9.
20. Salbach NM,Mayo NE,Robichaud-Ekstrand S,Hanley JA,Richards CL,Wood-
Dauphinee S.The effect of a task-oriented walking intervention on
improving balance self-efficacy poststroke:a randomized,controlled trial.J
Am Geriatr Soc.2005;53(4):576–82.
21. Hung JW,Chou CX,Hsieh YW,Wu WC,Wu MY,Chen PC,et al.Randomized
comparison trialof balance training by using exergaming and conventional
weight-shift therapy in patients with chronic stroke.Arch Phys Med Rehabil.
2014;95(9):1629–37.
22. Schmid AA,Van Puymbroeck M,Altenburger PA,Schalk NL,Dierks TA,Miller
KK,et al.Poststroke balance improves with yoga:a pilot study.Stroke.2012;
43(9):2402–7.
23. Holmgren E,Gosman-Hedstrom G,Lindstrom B,Wester P.What is the
benefit of high-intensive exercise program? A randomized controlled trial.
Adv Physiother.2010;12(3):115–24.
24. Marigold DS,Eng JJ, Dawson AS,Inglis JT,Harris JE,GylfadottirS.
Exercise leads to fasterposturalreflexes,improved balance and
mobility,and fewerfalls in olderpersons with chronic stroke.J Am
GeriatrSoc.2005;53(3):416–23.
25. Dickstein R,ShefiS,Holtzman S,Levy S,Peleg S,Vatine JJ.Motor imagery
group practice for gait rehabilitation in individuals with post-stroke
hemiparesis:a pilot study.NeuroRehabilitation.2014;34(2):267–76.
26. Dickstein R,Deutsch JE,Yoeli Y,Kafri M,Falash F,Dunsky A,et al.Effects of
integrated motor imagery practice on gait of individuals with chronic stroke:a
half-crossover randomized study.Arch Phys Med Rehabil.2013;94(11):2119–25.
27. Hwang S,Jeon HS,Yi C,Kwon O,Cho S,You S.Locomotor imagery training
improves gait performance in people with chronic hemiparetic stroke:a
controlled clinicaltrial.Clin Rehabil.2010;24(6):514–22.
28. Schuster C,Butler J,Andrews B,Kischka U,Ettlin T.Comparison of
embedded and added motor imagery training in patients after stroke:
results of a randomized controlled pilot trial.Trials.2012;13:11.
29. Zusman M.Cognitive-behavioralcomponents of musculoskeletal
physiotherapy:the role of control.Phys Ther Rev.2005;10:89–98.
30. Ng SSM,Hui-Chan CWY.Transcutaneous electricalnerve stimulation
combined with task-related training improves lower limb functions in
subjects with chronic stroke.Stroke.2007;38:2953–9.
31. van Duijnhoven HJR,Heeren A,Peters MAM,Veerbeek JM,KwakkelG,
Geurts ACH,et al.Effects of exercise therapy on balance capacity in chronic
stroke:systematic review and meta-analysis.Stroke.2016;47(10):2603.
https://doi.org/10.1161/STROKEAHA.116.013839.
32. Huang TT,Chung ML,Chen FR,Chin YF,Wang BH.Evaluation of a
combined cognitive-behaviouraland exercise intervention to manage fear
of falling among elderly residents in nursing homes.Aging Ment Health.
2016;20(1):2–12.
33. Schulz KF,Altman DG,MoherD. CONSORT 2010 statement:updated
guidelines forreporting parallelgroup randomized trials.BMC Med.
2010;8:18.
34. Mak MK,Lau AL,Law FS,Cheung CC,Wong IS.Validation of the Chinese
translated Activities-Specific Balance Confidence Scale.Arch Phys Med
Rehabil.2007;88:496–503.
35. Chu LW,PeiCKW,Ho MH,Chan PT.Validation of the abbreviated mental
test (Hong Kong version) in the elderly medicalpatient.Hong Kong Med J.
1995;1:207–11.
36. Jensen CV.A computer program for randomizing patients with near-even
distribution of important parameters.Comput Biomed Res.1991;24:429–34.
37. Myers AM,Fletcher PC,Myers AH,Sherk W.Discriminative and evaluative
properties of the Activities-Specific Balance Confidence (ABC) Scale.J
GerontolA BiolSciMed Sci.1998;53:M287–94.
38. Bayouk JF,Boucher P,Leroux A.Balance training following stroke:effects of
task-oriented exercises with and without altered sensory input.Int J Rehabil
Res.2006;29:51–9.
39. Leroux A.Exercise training to improve motor performance in chronic stroke:
exercise training to improve motor performance in chronic stroke:effects of
a community-based exercise program.Int J RehabilRes.2005;28:17–23.
40. Ng SSM,Hui-Chan CWY.Does the TENS increase the effectiveness of
exercise for improving walking after stroke? A randomized controlled
clinicaltrial.Clin Rehabil.2009;23(12):1093–103.
41. Bandura A.The exercise of control.New York:WH Freeman;1997.
42. Nemmers TM,Miller JW.Factors influencing balance in healthy community-
dwelling women age 60 and older.J Geriatr Phys Ther.2008;31(3):93–100.
43. Bello-Haas VD,Klassen L,Sheppard MS,Metcalfe A.Psychometric properties
of activity,self-efficacy,and quality-of-life measures in individuals with
Parkinson disease.Physiother Can.2011;63(1):47–57.
44. Botner E,Miller WC,Eng JJ.Measurement properties of the Activities-
Specific Balance Confidence Scale among individuals with stroke.Disabil
Rehabil.2005;27(4):156–63.
45. Salbace NM,Mayo NE,Robichaud-Ekstrand S,Hanley JA,Richards CL,Wood-
Dauphinee S.Balance self-efficacy and its relevance to physicalfunction and
perceived health status after stroke.Arch Phys Med Rehabil.2006;87:364–70.
46. Chou KL,Yeung FKC,Wong ECH.Fear of falling and depressive symptoms
in Chinese elderly living in nursing homes:fallefficacy and activity levelas
mediator or moderator? Aging Ment Health.2005;9:255–61.
47. Berg K.Measuring balance in the elderly:preliminary development of an
instrument.Physiother Can.1989;41:304–11.
48. Berg K,Wood Dauphinee S,William JI.The Balance Scale:reliability
assessment with elderly residents and patients with an acute stroke.Scand J
RehabilMed.1995;27:27–36.
49. Lord SR,Mena HB,Tiedemann A.A physiologicalprofile approach to falls
risk assessment and prevention.Phys Ther.2003;83:237–53.
50. Lord SR,Ward JA,Williams P,Anstey KJ.Physiologicalfactors associated
with falls in oldercommunity-dwelling women.J Am GeriatrSoc.1994;
23:452–60.
51. Tong AYC.The validation of the Hong Kong Chinese version of the Lawton
InstrumentalActivities of Daily Living Scale for the institutionalized elderly
persons.OTJR.2002;22:132–42.
52. Liu TW,Ng SS,Ng GY.Translation and initialvalidation of the Chinese
(Cantonese) version of community integration measure for use in patients
with chronic stroke.Biomed Res Int.2014;2014:623836.
53. McCollMA,Davies D,Carlson P,Johnston J,Minnes P.The Community
Integration Measure:development and preliminary validation.Arch Phys
Med Rehabil.2011;82(4):429–34.
54. Lam CLK,Tse EYY,Gandek B,Fong DY.The SF-36 summary scales were
valid,reliable and equivalent in a Chinese population.J Clin Epidemiol.
2005;58:815–22.
Liu et al.Trials (2018) 19:168 Page 10 of 10
Comparison oftwo exercise programs using the Falls Efficacy Scale,
Berg Balance Scale and ankle dorsiflexorstrength in olderadults.Phys
Occup TherGeriatr.2007;26:23–42.
13. Tennstedt S,Howland J,Lachman M,Peterson E,Kasten L,Jette A.A
randomized,controlled trialof a group intervention to reduce fear of falling
and associated activity restriction in older adults.J GerontolB PsycholSci
Soc Sci.1998;53:384–92.
14. Zijlstra GAR,Van Haastregt JCM,Ambergen T,Van Rossum E,Van Ejik JTM,
Tennstedt SL,et al.Effects of a multicomponent cognitive behavioralgroup
intervention on fear of falling and activity avoidance in community-
dwelling older adults:results of a randomized controlled trial.J Am Geriatr
Soc.2009;57:2020–8.
15. Kim BH.The effects of guided relaxation and exercise imagery on older
adults with a fear of falling.Diss Abstr Int.2009;70:3771.
16. Tang A,Tao A,Soh M,Tam C,Tan H,Thompson J,et al.The effects of
interventions on balance self-efficacy in the stroke population:a systematic
review and meta-analysis.Clin Rehabil.2015;29(12):1168–77.
17. Lord S,McPherson KM,McNaughton HK,Rochester L,WeatherallM.How
feasible is the attainment of community ambulation after stroke? A pilot
and randomized controlled trialto evaluate community-based
physiotherapy in subacute stroke.Clin Rehabil.2008;22(3):215–25.
18. Pang MY,Eng JJ.The effects of treadmillexercise training on hip bone
density and tibialbone geometry in stroke survivors:a pilot study.
NeurorehabilNeuralRepair.2010;24(4):386–76.
19. Park HJ,Oh DW,Kim SY,ChoiJD.Effectiveness of community-based
ambulation training for walking function of post-stroke hemiparesis:a
randomized controlled pilot trial.Clin Rehabil.2011;25(5):451–9.
20. Salbach NM,Mayo NE,Robichaud-Ekstrand S,Hanley JA,Richards CL,Wood-
Dauphinee S.The effect of a task-oriented walking intervention on
improving balance self-efficacy poststroke:a randomized,controlled trial.J
Am Geriatr Soc.2005;53(4):576–82.
21. Hung JW,Chou CX,Hsieh YW,Wu WC,Wu MY,Chen PC,et al.Randomized
comparison trialof balance training by using exergaming and conventional
weight-shift therapy in patients with chronic stroke.Arch Phys Med Rehabil.
2014;95(9):1629–37.
22. Schmid AA,Van Puymbroeck M,Altenburger PA,Schalk NL,Dierks TA,Miller
KK,et al.Poststroke balance improves with yoga:a pilot study.Stroke.2012;
43(9):2402–7.
23. Holmgren E,Gosman-Hedstrom G,Lindstrom B,Wester P.What is the
benefit of high-intensive exercise program? A randomized controlled trial.
Adv Physiother.2010;12(3):115–24.
24. Marigold DS,Eng JJ, Dawson AS,Inglis JT,Harris JE,GylfadottirS.
Exercise leads to fasterposturalreflexes,improved balance and
mobility,and fewerfalls in olderpersons with chronic stroke.J Am
GeriatrSoc.2005;53(3):416–23.
25. Dickstein R,ShefiS,Holtzman S,Levy S,Peleg S,Vatine JJ.Motor imagery
group practice for gait rehabilitation in individuals with post-stroke
hemiparesis:a pilot study.NeuroRehabilitation.2014;34(2):267–76.
26. Dickstein R,Deutsch JE,Yoeli Y,Kafri M,Falash F,Dunsky A,et al.Effects of
integrated motor imagery practice on gait of individuals with chronic stroke:a
half-crossover randomized study.Arch Phys Med Rehabil.2013;94(11):2119–25.
27. Hwang S,Jeon HS,Yi C,Kwon O,Cho S,You S.Locomotor imagery training
improves gait performance in people with chronic hemiparetic stroke:a
controlled clinicaltrial.Clin Rehabil.2010;24(6):514–22.
28. Schuster C,Butler J,Andrews B,Kischka U,Ettlin T.Comparison of
embedded and added motor imagery training in patients after stroke:
results of a randomized controlled pilot trial.Trials.2012;13:11.
29. Zusman M.Cognitive-behavioralcomponents of musculoskeletal
physiotherapy:the role of control.Phys Ther Rev.2005;10:89–98.
30. Ng SSM,Hui-Chan CWY.Transcutaneous electricalnerve stimulation
combined with task-related training improves lower limb functions in
subjects with chronic stroke.Stroke.2007;38:2953–9.
31. van Duijnhoven HJR,Heeren A,Peters MAM,Veerbeek JM,KwakkelG,
Geurts ACH,et al.Effects of exercise therapy on balance capacity in chronic
stroke:systematic review and meta-analysis.Stroke.2016;47(10):2603.
https://doi.org/10.1161/STROKEAHA.116.013839.
32. Huang TT,Chung ML,Chen FR,Chin YF,Wang BH.Evaluation of a
combined cognitive-behaviouraland exercise intervention to manage fear
of falling among elderly residents in nursing homes.Aging Ment Health.
2016;20(1):2–12.
33. Schulz KF,Altman DG,MoherD. CONSORT 2010 statement:updated
guidelines forreporting parallelgroup randomized trials.BMC Med.
2010;8:18.
34. Mak MK,Lau AL,Law FS,Cheung CC,Wong IS.Validation of the Chinese
translated Activities-Specific Balance Confidence Scale.Arch Phys Med
Rehabil.2007;88:496–503.
35. Chu LW,PeiCKW,Ho MH,Chan PT.Validation of the abbreviated mental
test (Hong Kong version) in the elderly medicalpatient.Hong Kong Med J.
1995;1:207–11.
36. Jensen CV.A computer program for randomizing patients with near-even
distribution of important parameters.Comput Biomed Res.1991;24:429–34.
37. Myers AM,Fletcher PC,Myers AH,Sherk W.Discriminative and evaluative
properties of the Activities-Specific Balance Confidence (ABC) Scale.J
GerontolA BiolSciMed Sci.1998;53:M287–94.
38. Bayouk JF,Boucher P,Leroux A.Balance training following stroke:effects of
task-oriented exercises with and without altered sensory input.Int J Rehabil
Res.2006;29:51–9.
39. Leroux A.Exercise training to improve motor performance in chronic stroke:
exercise training to improve motor performance in chronic stroke:effects of
a community-based exercise program.Int J RehabilRes.2005;28:17–23.
40. Ng SSM,Hui-Chan CWY.Does the TENS increase the effectiveness of
exercise for improving walking after stroke? A randomized controlled
clinicaltrial.Clin Rehabil.2009;23(12):1093–103.
41. Bandura A.The exercise of control.New York:WH Freeman;1997.
42. Nemmers TM,Miller JW.Factors influencing balance in healthy community-
dwelling women age 60 and older.J Geriatr Phys Ther.2008;31(3):93–100.
43. Bello-Haas VD,Klassen L,Sheppard MS,Metcalfe A.Psychometric properties
of activity,self-efficacy,and quality-of-life measures in individuals with
Parkinson disease.Physiother Can.2011;63(1):47–57.
44. Botner E,Miller WC,Eng JJ.Measurement properties of the Activities-
Specific Balance Confidence Scale among individuals with stroke.Disabil
Rehabil.2005;27(4):156–63.
45. Salbace NM,Mayo NE,Robichaud-Ekstrand S,Hanley JA,Richards CL,Wood-
Dauphinee S.Balance self-efficacy and its relevance to physicalfunction and
perceived health status after stroke.Arch Phys Med Rehabil.2006;87:364–70.
46. Chou KL,Yeung FKC,Wong ECH.Fear of falling and depressive symptoms
in Chinese elderly living in nursing homes:fallefficacy and activity levelas
mediator or moderator? Aging Ment Health.2005;9:255–61.
47. Berg K.Measuring balance in the elderly:preliminary development of an
instrument.Physiother Can.1989;41:304–11.
48. Berg K,Wood Dauphinee S,William JI.The Balance Scale:reliability
assessment with elderly residents and patients with an acute stroke.Scand J
RehabilMed.1995;27:27–36.
49. Lord SR,Mena HB,Tiedemann A.A physiologicalprofile approach to falls
risk assessment and prevention.Phys Ther.2003;83:237–53.
50. Lord SR,Ward JA,Williams P,Anstey KJ.Physiologicalfactors associated
with falls in oldercommunity-dwelling women.J Am GeriatrSoc.1994;
23:452–60.
51. Tong AYC.The validation of the Hong Kong Chinese version of the Lawton
InstrumentalActivities of Daily Living Scale for the institutionalized elderly
persons.OTJR.2002;22:132–42.
52. Liu TW,Ng SS,Ng GY.Translation and initialvalidation of the Chinese
(Cantonese) version of community integration measure for use in patients
with chronic stroke.Biomed Res Int.2014;2014:623836.
53. McCollMA,Davies D,Carlson P,Johnston J,Minnes P.The Community
Integration Measure:development and preliminary validation.Arch Phys
Med Rehabil.2011;82(4):429–34.
54. Lam CLK,Tse EYY,Gandek B,Fong DY.The SF-36 summary scales were
valid,reliable and equivalent in a Chinese population.J Clin Epidemiol.
2005;58:815–22.
Liu et al.Trials (2018) 19:168 Page 10 of 10
1 out of 10
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.

