Research Proposal: Novel Therapy Options for Multi-Drug Resistant TB
VerifiedAdded on 2023/06/15
|15
|3875
|484
Report
AI Summary
This research proposal investigates novel therapy options for multi-drug resistant tuberculosis (MDR-TB), addressing the urgent need for effective treatments due to increasing resistance to conventional drugs. The proposal focuses on genetically engineered antimicrobial peptides (AMPs), specifically human beta-defensins (HBD-3), derived from macrophages and neutrophils, aiming to target intracellular bacteria without harming host cells. The research will explore the efficacy of these modified AMPs, administered endogenously, in combating MDR-TB, with a detailed methodology involving fluorescence microscopy and animal trials, while adhering to ethical considerations. The literature review highlights existing treatments and the potential of defensins, setting the stage for a three-year research plan to develop and test this innovative therapeutic approach.

Running head: RESEARCH PROPOSAL
Research Proposal
Name of the Student
Name of the University
Author Note
Research Proposal
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
RESEARCH PROPOSAL
Table of Contents
Topic..........................................................................................................................................2
Introduction................................................................................................................................2
Aim of the Research...................................................................................................................3
Literature Review.......................................................................................................................4
Methodology..............................................................................................................................5
Ethical Consideration.................................................................................................................6
Time Plan...................................................................................................................................6
References..................................................................................................................................8
Bibliography.............................................................................................................................11
RESEARCH PROPOSAL
Table of Contents
Topic..........................................................................................................................................2
Introduction................................................................................................................................2
Aim of the Research...................................................................................................................3
Literature Review.......................................................................................................................4
Methodology..............................................................................................................................5
Ethical Consideration.................................................................................................................6
Time Plan...................................................................................................................................6
References..................................................................................................................................8
Bibliography.............................................................................................................................11
2
RESEARCH PROPOSAL
Topic
Finding a Therapy Option for MDR TB
Introduction
Despite the global efforts and the financial investment by the government and non-
governmental organisation, tuberculosis still remains a leading cause of death worldwide1.
According to the global report on tuberculosis as published by the world health organisation,
3.7% of the new cases and 20% of the previously treated cases of tuberculosis has now
transformed in multidrug resistant (MDR) variants2. This MDR is resistant to rifampicin and
isoniazid3. Not only MDR, the initial report as published from South Africa showed the
existence of the extensively drug resistant (XDR) tuberculosis4. The XDR strains are resistant
to rifampicin, isoniazid, fluoroquinolones and other second-line of injectable drugs like
capreomycin, amikacin and kanamycin5. The countries in the Easter Europe have highest
recorded cases of MDR tuberculosis around the world and the majority of the tuberculosis
cases arise in the china, India, Indonesia and Philippines6.The treatment of the MDR
tuberculosis is toxic, lengthy and expensive. It is also associated with poor outcomes. Certain
fluoroquilones, ethionamide or prothionamidehas been shown to provide effective response
against MDR-TB. However, randomized trials are required to optimize the treatment7.
1Murray, Christopher JL, et al. "Global, regional, and national incidence and mortality for HIV, tuberculosis,
and malaria during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013." The
Lancet 384.9947 (2014): 1005-1070.
2Abubakar, Ibrahim, et al. "Drug-resistant tuberculosis: time for visionary political leadership." The Lancet
infectious diseases13.6 (2013): 529-539.
3Udwadia, Zarir F., et al. "Totally drug-resistant tuberculosis in India." Clinical Infectious Diseases 54.4 (2012):
579-581.
4Streicher, Elizabeth M., et al. "Emergence and treatment of multidrug resistant (MDR) and extensively drug-
resistant (XDR) tuberculosis in South Africa." Infection, genetics and evolution 12.4 (2012): 686-694.
5Klopper, Marisa, et al. "Emergence and spread of extensively and totally drug-resistant tuberculosis, South
Africa." Emerging infectious diseases 19.3 (2013): 449.
6World Health Organization, ed. Global tuberculosis report 2013. World Health Organization, 2013.
7Ahuja, Shama D., et al. "Multidrug resistant pulmonary tuberculosis treatment regimens and patient outcomes:
an individual patient data meta-analysis of 9,153 patients." PLoS medicine 9.8 (2012): e1001300.
RESEARCH PROPOSAL
Topic
Finding a Therapy Option for MDR TB
Introduction
Despite the global efforts and the financial investment by the government and non-
governmental organisation, tuberculosis still remains a leading cause of death worldwide1.
According to the global report on tuberculosis as published by the world health organisation,
3.7% of the new cases and 20% of the previously treated cases of tuberculosis has now
transformed in multidrug resistant (MDR) variants2. This MDR is resistant to rifampicin and
isoniazid3. Not only MDR, the initial report as published from South Africa showed the
existence of the extensively drug resistant (XDR) tuberculosis4. The XDR strains are resistant
to rifampicin, isoniazid, fluoroquinolones and other second-line of injectable drugs like
capreomycin, amikacin and kanamycin5. The countries in the Easter Europe have highest
recorded cases of MDR tuberculosis around the world and the majority of the tuberculosis
cases arise in the china, India, Indonesia and Philippines6.The treatment of the MDR
tuberculosis is toxic, lengthy and expensive. It is also associated with poor outcomes. Certain
fluoroquilones, ethionamide or prothionamidehas been shown to provide effective response
against MDR-TB. However, randomized trials are required to optimize the treatment7.
1Murray, Christopher JL, et al. "Global, regional, and national incidence and mortality for HIV, tuberculosis,
and malaria during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013." The
Lancet 384.9947 (2014): 1005-1070.
2Abubakar, Ibrahim, et al. "Drug-resistant tuberculosis: time for visionary political leadership." The Lancet
infectious diseases13.6 (2013): 529-539.
3Udwadia, Zarir F., et al. "Totally drug-resistant tuberculosis in India." Clinical Infectious Diseases 54.4 (2012):
579-581.
4Streicher, Elizabeth M., et al. "Emergence and treatment of multidrug resistant (MDR) and extensively drug-
resistant (XDR) tuberculosis in South Africa." Infection, genetics and evolution 12.4 (2012): 686-694.
5Klopper, Marisa, et al. "Emergence and spread of extensively and totally drug-resistant tuberculosis, South
Africa." Emerging infectious diseases 19.3 (2013): 449.
6World Health Organization, ed. Global tuberculosis report 2013. World Health Organization, 2013.
7Ahuja, Shama D., et al. "Multidrug resistant pulmonary tuberculosis treatment regimens and patient outcomes:
an individual patient data meta-analysis of 9,153 patients." PLoS medicine 9.8 (2012): e1001300.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

3
RESEARCH PROPOSAL
Linezoliod is used off-label to treat MDR tuberculosis in the absence of strong systematic
evidence. Linezolid has strong efficacy against MDR tuberculosis but must be used with
proper caution8.
Aim of the Research
TB can be treated with a cocktail of antibiotics, chemotherapy and vaccines but the
efficacy is limited9. Therefore, there is a pressing need to the development of novel therapy
for the treatment of MDR-TB. Mycobacterium tuberculosis (Mtb) invades and then replicate
inside host macrophages, the novel therapy must target an approach to kill intracellular
bacteria without harming the host cell10. In this regards, anti-microbial peptides (AMPs) can
be treated to be effective. However, AMPs are cytotoxic to mammalian cells11.
The aim of this research is to genetically engineered AMPs from the marcophage and
neutrophil derive proteins, which are active at low concentration (not harming host cell). The
geneticalengineering will be performed via cloning the AMPs from the macrophage
derivedprotein followed by PCR verification. The study will target defensins, a class of
cationic peptides with microbicidal, immunomodulatory and cytotoxic activities12. It also
serves as an effective mediator between cellular and innate immunity. For this particular
study, the main target will be human beta-defensins (HBD-3) which are secreted by the
mucosal epithelial cells. They are the first line of defense against infection 13. The reason
behind choosing HBD is, it can retain its anti-microbial activity at physiological salt
8Sotgiu, Giovanni, et al. "Efficacy, safety and tolerability of linezolid containing regimens in treating MDR-TB
and XDR-TB: systematic review and meta-analysis." European Respiratory Journal 40.6 (2012): 1430-1442.
9Gandhi, Neel R., et al. "Multidrug-resistant and extensively drug-resistant tuberculosis: a threat to global
control of tuberculosis." The Lancet 375.9728 (2010): 1830-1843.
10Bhatt, Kamlesh, and PadminiSalgame. "Host innate immune response to Mycobacterium
tuberculosis." Journal of clinical immunology 27.4 (2007): 347-362.
11Garcia, Francia, et al. "Antimicrobial peptides from arachnid venoms and their microbicidal activity in the
presence of commercial antibiotics." The Journal of antibiotics 66.1 (2013): 3-10.
12Van Wetering, S. A. N. D. R. A., et al. "Effect of defensins on interleukin-8 synthesis in airway epithelial
cells." American Journal of Physiology-Lung Cellular and Molecular Physiology272.5 (1997): L888-L896.
13Shornick, Laurie P., et al. "Airway epithelial versus immune cell Stat1 function for innate defense against
respiratory viral infection." The Journal of Immunology 180.5 (2008): 3319-3328.
RESEARCH PROPOSAL
Linezoliod is used off-label to treat MDR tuberculosis in the absence of strong systematic
evidence. Linezolid has strong efficacy against MDR tuberculosis but must be used with
proper caution8.
Aim of the Research
TB can be treated with a cocktail of antibiotics, chemotherapy and vaccines but the
efficacy is limited9. Therefore, there is a pressing need to the development of novel therapy
for the treatment of MDR-TB. Mycobacterium tuberculosis (Mtb) invades and then replicate
inside host macrophages, the novel therapy must target an approach to kill intracellular
bacteria without harming the host cell10. In this regards, anti-microbial peptides (AMPs) can
be treated to be effective. However, AMPs are cytotoxic to mammalian cells11.
The aim of this research is to genetically engineered AMPs from the marcophage and
neutrophil derive proteins, which are active at low concentration (not harming host cell). The
geneticalengineering will be performed via cloning the AMPs from the macrophage
derivedprotein followed by PCR verification. The study will target defensins, a class of
cationic peptides with microbicidal, immunomodulatory and cytotoxic activities12. It also
serves as an effective mediator between cellular and innate immunity. For this particular
study, the main target will be human beta-defensins (HBD-3) which are secreted by the
mucosal epithelial cells. They are the first line of defense against infection 13. The reason
behind choosing HBD is, it can retain its anti-microbial activity at physiological salt
8Sotgiu, Giovanni, et al. "Efficacy, safety and tolerability of linezolid containing regimens in treating MDR-TB
and XDR-TB: systematic review and meta-analysis." European Respiratory Journal 40.6 (2012): 1430-1442.
9Gandhi, Neel R., et al. "Multidrug-resistant and extensively drug-resistant tuberculosis: a threat to global
control of tuberculosis." The Lancet 375.9728 (2010): 1830-1843.
10Bhatt, Kamlesh, and PadminiSalgame. "Host innate immune response to Mycobacterium
tuberculosis." Journal of clinical immunology 27.4 (2007): 347-362.
11Garcia, Francia, et al. "Antimicrobial peptides from arachnid venoms and their microbicidal activity in the
presence of commercial antibiotics." The Journal of antibiotics 66.1 (2013): 3-10.
12Van Wetering, S. A. N. D. R. A., et al. "Effect of defensins on interleukin-8 synthesis in airway epithelial
cells." American Journal of Physiology-Lung Cellular and Molecular Physiology272.5 (1997): L888-L896.
13Shornick, Laurie P., et al. "Airway epithelial versus immune cell Stat1 function for innate defense against
respiratory viral infection." The Journal of Immunology 180.5 (2008): 3319-3328.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
RESEARCH PROPOSAL
concentration14.Since Mtbdown regulates cationic peptides, the study will aim to introduce
exogenous peptide administration or via hormonal induction of peptides.
Literature Review
XDR and MDR-TB are associated with worse treatment outcomes with the patients of
TB. Recently delamandid (OPC-67683) has been discovered as a novel drug for the treatment
of MDR-Tb infection. The analysis performed over the patients of TB showed positive
outcome when they are treated with delamandid for 6 months at a stretch in combination with
an optimized background regime. This combinational treatment has been found to reduce the
mortality rate of the both XDR and MDR-TB patients15.
In 2012, 450,00 cases reported to be MDR-TB globally. According to WHO,
significant efforts are required to improve the present average rate of the successful treatment
of patients who are suffering from MDR-TB. The current therapy that is used for the
treatment of TB is arduous and long and is mainly concerned with the antiquated drugs that
are bacteriostatic in nature and are associated with several side effects. Bedaquiline, a
diarylquinolinehas been found to inhibit mycobacterial ATP synthase. It is considered as a
first ever anti-tuberculosis drug that is combating against TB under completely new
mechanism. The importance of Badaquilineis: it is bactericidal in nature. The inclusion of the
bedaquiline in the TB treatment regime is associated with reduced risk of pre-extensive drug
resistance along with reduced risk of other background drug resistance16.
14Garca, C., Jaumann, F., Schulz, S., Krause, A., Rodrguez-Jimnez, J., Forssmann, U., Adermann, K., Klver, E.,
Vogelmeier, C., Becker, D. and Hedrich, R., 2001. Identification of a novel, multifunctional-defensin (human-
defensin 3) with specific antimicrobial activityIts interaction with plasma membranes of Xenopus oocytes and
the induction of macrophage chemoattraction. Cell and Tissue Research, 2(306), pp.257-264.
15Skripconoka, Vija, et al. "Delamanid improves outcomes and reduces mortality in multidrug-resistant
tuberculosis." European Respiratory Journal 41.6 (2013): 1393-1400.
16Diacon, Andreas H., et al. "Multidrug-resistant tuberculosis and culture conversion with bedaquiline." New
England Journal of Medicine 371.8 (2014): 723-732.
RESEARCH PROPOSAL
concentration14.Since Mtbdown regulates cationic peptides, the study will aim to introduce
exogenous peptide administration or via hormonal induction of peptides.
Literature Review
XDR and MDR-TB are associated with worse treatment outcomes with the patients of
TB. Recently delamandid (OPC-67683) has been discovered as a novel drug for the treatment
of MDR-Tb infection. The analysis performed over the patients of TB showed positive
outcome when they are treated with delamandid for 6 months at a stretch in combination with
an optimized background regime. This combinational treatment has been found to reduce the
mortality rate of the both XDR and MDR-TB patients15.
In 2012, 450,00 cases reported to be MDR-TB globally. According to WHO,
significant efforts are required to improve the present average rate of the successful treatment
of patients who are suffering from MDR-TB. The current therapy that is used for the
treatment of TB is arduous and long and is mainly concerned with the antiquated drugs that
are bacteriostatic in nature and are associated with several side effects. Bedaquiline, a
diarylquinolinehas been found to inhibit mycobacterial ATP synthase. It is considered as a
first ever anti-tuberculosis drug that is combating against TB under completely new
mechanism. The importance of Badaquilineis: it is bactericidal in nature. The inclusion of the
bedaquiline in the TB treatment regime is associated with reduced risk of pre-extensive drug
resistance along with reduced risk of other background drug resistance16.
14Garca, C., Jaumann, F., Schulz, S., Krause, A., Rodrguez-Jimnez, J., Forssmann, U., Adermann, K., Klver, E.,
Vogelmeier, C., Becker, D. and Hedrich, R., 2001. Identification of a novel, multifunctional-defensin (human-
defensin 3) with specific antimicrobial activityIts interaction with plasma membranes of Xenopus oocytes and
the induction of macrophage chemoattraction. Cell and Tissue Research, 2(306), pp.257-264.
15Skripconoka, Vija, et al. "Delamanid improves outcomes and reduces mortality in multidrug-resistant
tuberculosis." European Respiratory Journal 41.6 (2013): 1393-1400.
16Diacon, Andreas H., et al. "Multidrug-resistant tuberculosis and culture conversion with bedaquiline." New
England Journal of Medicine 371.8 (2014): 723-732.
5
RESEARCH PROPOSAL
Pediatric MDR-TB is also a public health challenge. The clinical management of the
pediatric TB is challenging and the recommendations are strictly based on the restricted
evidence17. Moreover, the treatment of the MDR is not cost effective any only a small
fraction of the reported cases are treated according to the basis of the international
guidelines18. In India, Linezolid is used a safe and cost-effective alternative for the treatment
of the MDR tuberculosis especially for the patients who are failing to afford high cost
treatment19.
At present, next-generation antibiotics, AMPs and proteins, popularly known as
"natural antibiotics" administered alone or in conjunction with other conventional drugs are
showing promising results20. Out of defensins, beta-defensins can be excepted to have
promising results against Mtb. Mtb infection lead to the over-expression of beta-defensins in
the endothelial cells 21. Further results suggested that L-isoleucine lead to the over-expression
of beta-defensins that promotes reducing of the viral over-load (MDR-Mtb). Beta-defensins
exerts bactericidal activity on the latent phase of Mtbinfection 22.
Methodology
Endogeneous administration of the purified defensins (AMP) followed by the study of
the intracellular killing of the bacteria via study under the fluorescence microscopy. The
efficacy of AMP protein upon bactericidal activity will be studied alone and in combination
17Ettehad, Dena, et al. "Treatment outcomes for children with multidrug-resistant tuberculosis: a systematic
review and meta-analysis." The Lancet infectious diseases 12.6 (2012): 449-456.
18Fitzpatrick, Christopher, and Katherine Floyd."A systematic review of the cost and cost effectiveness of
treatment for multidrug-resistant tuberculosis." Pharmacoeconomics 30.1 (2012): 63-80.
19Singla, Rupak, et al. "Linezolid: an effective, safe and cheap drug for patients failing multidrug-resistant
tuberculosis treatment in India." European Respiratory Journal 39.4 (2012): 956-962.
20Wang, Guangshun, Xia Li, and Zhe Wang. "APD2: the updated antimicrobial peptide database and its
application in peptide design." Nucleic acids research 37.suppl_1 (2008): D933-D937.
21García-Pérez, Blanca Estela, et al. "Innate response of human endothelial cells infected with
mycobacteria." Immunobiology216.8 (2011): 925-935.
22Rivas‐Santiago, B., et al. "The Potential Role of Lung Epithelial Cells and β‐defensins in Experimental Latent
Tuberculosis." Scandinavian journal of immunology 67.5 (2008): 448-452.
RESEARCH PROPOSAL
Pediatric MDR-TB is also a public health challenge. The clinical management of the
pediatric TB is challenging and the recommendations are strictly based on the restricted
evidence17. Moreover, the treatment of the MDR is not cost effective any only a small
fraction of the reported cases are treated according to the basis of the international
guidelines18. In India, Linezolid is used a safe and cost-effective alternative for the treatment
of the MDR tuberculosis especially for the patients who are failing to afford high cost
treatment19.
At present, next-generation antibiotics, AMPs and proteins, popularly known as
"natural antibiotics" administered alone or in conjunction with other conventional drugs are
showing promising results20. Out of defensins, beta-defensins can be excepted to have
promising results against Mtb. Mtb infection lead to the over-expression of beta-defensins in
the endothelial cells 21. Further results suggested that L-isoleucine lead to the over-expression
of beta-defensins that promotes reducing of the viral over-load (MDR-Mtb). Beta-defensins
exerts bactericidal activity on the latent phase of Mtbinfection 22.
Methodology
Endogeneous administration of the purified defensins (AMP) followed by the study of
the intracellular killing of the bacteria via study under the fluorescence microscopy. The
efficacy of AMP protein upon bactericidal activity will be studied alone and in combination
17Ettehad, Dena, et al. "Treatment outcomes for children with multidrug-resistant tuberculosis: a systematic
review and meta-analysis." The Lancet infectious diseases 12.6 (2012): 449-456.
18Fitzpatrick, Christopher, and Katherine Floyd."A systematic review of the cost and cost effectiveness of
treatment for multidrug-resistant tuberculosis." Pharmacoeconomics 30.1 (2012): 63-80.
19Singla, Rupak, et al. "Linezolid: an effective, safe and cheap drug for patients failing multidrug-resistant
tuberculosis treatment in India." European Respiratory Journal 39.4 (2012): 956-962.
20Wang, Guangshun, Xia Li, and Zhe Wang. "APD2: the updated antimicrobial peptide database and its
application in peptide design." Nucleic acids research 37.suppl_1 (2008): D933-D937.
21García-Pérez, Blanca Estela, et al. "Innate response of human endothelial cells infected with
mycobacteria." Immunobiology216.8 (2011): 925-935.
22Rivas‐Santiago, B., et al. "The Potential Role of Lung Epithelial Cells and β‐defensins in Experimental Latent
Tuberculosis." Scandinavian journal of immunology 67.5 (2008): 448-452.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
RESEARCH PROPOSAL
of anti-Mtb drugs.The main challenge of the research is to frame effective peptide delivery
system for the endogenous expression of AMP.
Ethical Consideration
The overall affect of defensinswill be studied over swiss albino mice and hence prior
approval from the animal ethical committee will be taken before the initial of the animal trial
in the research.
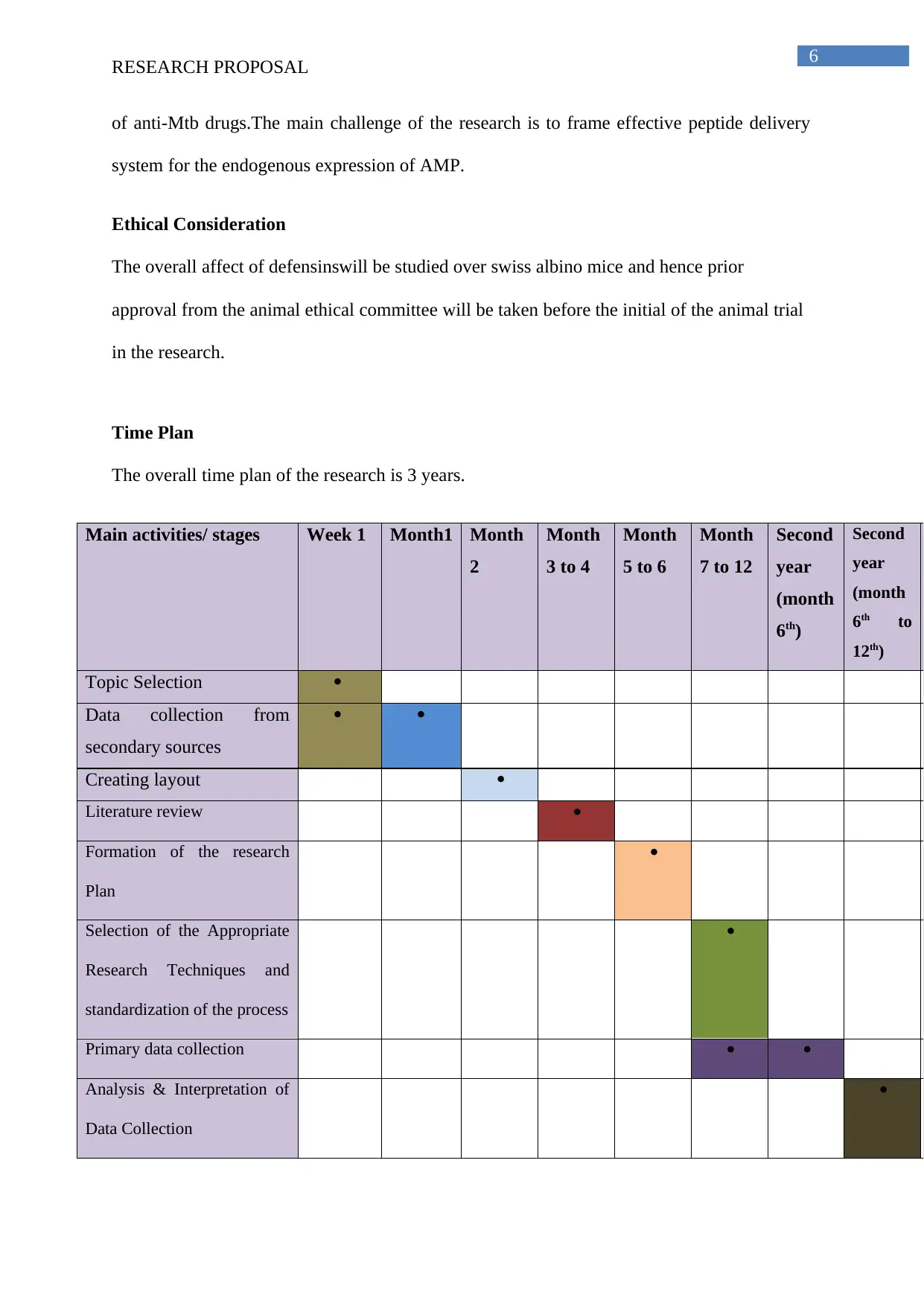
Time Plan
The overall time plan of the research is 3 years.
Main activities/ stages Week 1 Month1 Month
2
Month
3 to 4
Month
5 to 6
Month
7 to 12
Second
year
(month
6th)
Second
year
(month
6th to
12th)
Topic Selection
Data collection from
secondary sources
Creating layout
Literature review
Formation of the research
Plan
Selection of the Appropriate
Research Techniques and
standardization of the process
Primary data collection
Analysis & Interpretation of
Data Collection
RESEARCH PROPOSAL
of anti-Mtb drugs.The main challenge of the research is to frame effective peptide delivery
system for the endogenous expression of AMP.
Ethical Consideration
The overall affect of defensinswill be studied over swiss albino mice and hence prior
approval from the animal ethical committee will be taken before the initial of the animal trial
in the research.
Time Plan
The overall time plan of the research is 3 years.
Main activities/ stages Week 1 Month1 Month
2
Month
3 to 4
Month
5 to 6
Month
7 to 12
Second
year
(month
6th)
Second
year
(month
6th to
12th)
Topic Selection
Data collection from
secondary sources
Creating layout
Literature review
Formation of the research
Plan
Selection of the Appropriate
Research Techniques and
standardization of the process
Primary data collection
Analysis & Interpretation of
Data Collection
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
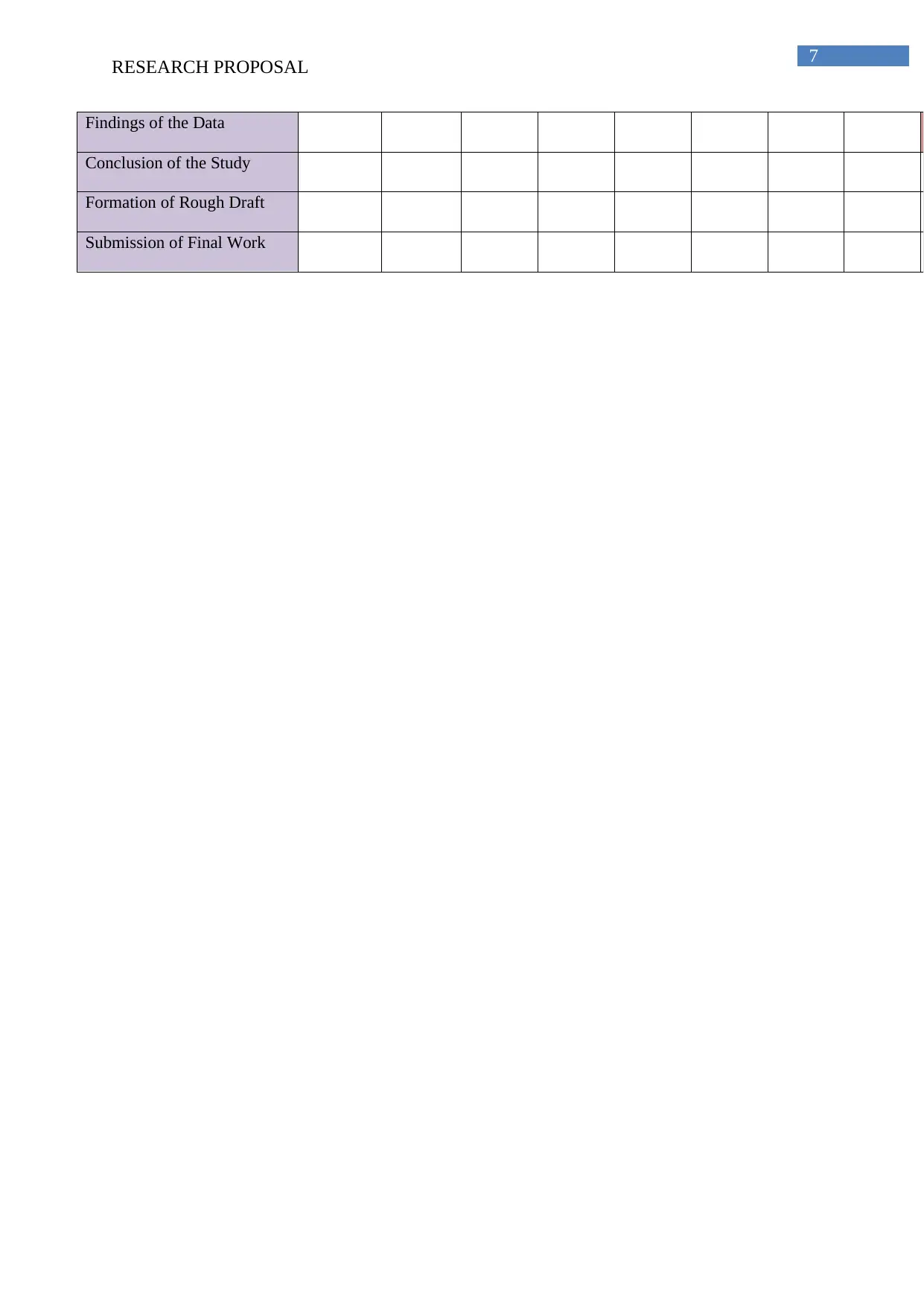
7
RESEARCH PROPOSAL
Findings of the Data
Conclusion of the Study
Formation of Rough Draft
Submission of Final Work
RESEARCH PROPOSAL
Findings of the Data
Conclusion of the Study
Formation of Rough Draft
Submission of Final Work
8
RESEARCH PROPOSAL
References
Abubakar, Ibrahim, et al. "Drug-resistant tuberculosis: time for visionary political
leadership." The Lancet infectious diseases13.6 (2013): 529-539.
Ahuja, Shama D., et al. "Multidrug resistant pulmonary tuberculosis treatment regimens and
patient outcomes: an individual patient data meta-analysis of 9,153 patients." PLoS
medicine 9.8 (2012): e1001300.
Bhatt, Kamlesh, and PadminiSalgame. "Host innate immune response to Mycobacterium
tuberculosis." Journal of clinical immunology 27.4 (2007): 347-362.
Diacon, Andreas H., et al. "Multidrug-resistant tuberculosis and culture conversion with
bedaquiline." New England Journal of Medicine 371.8 (2014): 723-732.
Ettehad, Dena, et al. "Treatment outcomes for children with multidrug-resistant tuberculosis:
a systematic review and meta-analysis." The Lancet infectious diseases 12.6 (2012): 449-456.
Fitzpatrick, Christopher, and Katherine Floyd."A systematic review of the cost and cost
effectiveness of treatment for multidrug-resistant tuberculosis." Pharmacoeconomics 30.1
(2012): 63-80.
Gandhi, Neel R., et al. "Multidrug-resistant and extensively drug-resistant tuberculosis: a
threat to global control of tuberculosis." The Lancet 375.9728 (2010): 1830-1843.
Garca, C., Jaumann, F., Schulz, S., Krause, A., Rodrguez-Jimnez, J., Forssmann, U.,
Adermann, K., Klver, E., Vogelmeier, C., Becker, D. and Hedrich, R.,.Identification of a
novel, multifunctional-defensin (human-defensin 3) with specific antimicrobial activityIts
interaction with plasma membranes of Xenopus oocytes and the induction of macrophage
chemoattraction. Cell and Tissue Research, 2(306) (2001), pp.257-264.
RESEARCH PROPOSAL
References
Abubakar, Ibrahim, et al. "Drug-resistant tuberculosis: time for visionary political
leadership." The Lancet infectious diseases13.6 (2013): 529-539.
Ahuja, Shama D., et al. "Multidrug resistant pulmonary tuberculosis treatment regimens and
patient outcomes: an individual patient data meta-analysis of 9,153 patients." PLoS
medicine 9.8 (2012): e1001300.
Bhatt, Kamlesh, and PadminiSalgame. "Host innate immune response to Mycobacterium
tuberculosis." Journal of clinical immunology 27.4 (2007): 347-362.
Diacon, Andreas H., et al. "Multidrug-resistant tuberculosis and culture conversion with
bedaquiline." New England Journal of Medicine 371.8 (2014): 723-732.
Ettehad, Dena, et al. "Treatment outcomes for children with multidrug-resistant tuberculosis:
a systematic review and meta-analysis." The Lancet infectious diseases 12.6 (2012): 449-456.
Fitzpatrick, Christopher, and Katherine Floyd."A systematic review of the cost and cost
effectiveness of treatment for multidrug-resistant tuberculosis." Pharmacoeconomics 30.1
(2012): 63-80.
Gandhi, Neel R., et al. "Multidrug-resistant and extensively drug-resistant tuberculosis: a
threat to global control of tuberculosis." The Lancet 375.9728 (2010): 1830-1843.
Garca, C., Jaumann, F., Schulz, S., Krause, A., Rodrguez-Jimnez, J., Forssmann, U.,
Adermann, K., Klver, E., Vogelmeier, C., Becker, D. and Hedrich, R.,.Identification of a
novel, multifunctional-defensin (human-defensin 3) with specific antimicrobial activityIts
interaction with plasma membranes of Xenopus oocytes and the induction of macrophage
chemoattraction. Cell and Tissue Research, 2(306) (2001), pp.257-264.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
RESEARCH PROPOSAL
Garcia, Francia, et al. "Antimicrobial peptides from arachnid venoms and their microbicidal
activity in the presence of commercial antibiotics." The Journal of antibiotics 66.1 (2013): 3-
10.
García-Pérez, Blanca Estela, et al. "Innate response of human endothelial cells infected with
mycobacteria." Immunobiology216.8 (2011): 925-935.
Klopper, Marisa, et al. "Emergence and spread of extensively and totally drug-resistant
tuberculosis, South Africa." Emerging infectious diseases 19.3 (2013): 449.
Murray, Christopher JL, et al. "Global, regional, and national incidence and mortality for
HIV, tuberculosis, and malaria during 1990–2013: a systematic analysis for the Global
Burden of Disease Study 2013." The Lancet 384.9947 (2014): 1005-1070.
Rivas‐Santiago, B., et al. "The Potential Role of Lung Epithelial Cells and β‐defensins in
Experimental Latent Tuberculosis." Scandinavian journal of immunology 67.5 (2008): 448-
452.
Shornick, Laurie P., et al. "Airway epithelial versus immune cell Stat1 function for innate
defense against respiratory viral infection." The Journal of Immunology 180.5 (2008): 3319-
3328.
Singla, Rupak, et al. "Linezolid: an effective, safe and cheap drug for patients failing
multidrug-resistant tuberculosis treatment in India." European Respiratory Journal 39.4
(2012): 956-962.
Skripconoka, Vija, et al. "Delamanid improves outcomes and reduces mortality in multidrug-
resistant tuberculosis." European Respiratory Journal 41.6 (2013): 1393-1400.
RESEARCH PROPOSAL
Garcia, Francia, et al. "Antimicrobial peptides from arachnid venoms and their microbicidal
activity in the presence of commercial antibiotics." The Journal of antibiotics 66.1 (2013): 3-
10.
García-Pérez, Blanca Estela, et al. "Innate response of human endothelial cells infected with
mycobacteria." Immunobiology216.8 (2011): 925-935.
Klopper, Marisa, et al. "Emergence and spread of extensively and totally drug-resistant
tuberculosis, South Africa." Emerging infectious diseases 19.3 (2013): 449.
Murray, Christopher JL, et al. "Global, regional, and national incidence and mortality for
HIV, tuberculosis, and malaria during 1990–2013: a systematic analysis for the Global
Burden of Disease Study 2013." The Lancet 384.9947 (2014): 1005-1070.
Rivas‐Santiago, B., et al. "The Potential Role of Lung Epithelial Cells and β‐defensins in
Experimental Latent Tuberculosis." Scandinavian journal of immunology 67.5 (2008): 448-
452.
Shornick, Laurie P., et al. "Airway epithelial versus immune cell Stat1 function for innate
defense against respiratory viral infection." The Journal of Immunology 180.5 (2008): 3319-
3328.
Singla, Rupak, et al. "Linezolid: an effective, safe and cheap drug for patients failing
multidrug-resistant tuberculosis treatment in India." European Respiratory Journal 39.4
(2012): 956-962.
Skripconoka, Vija, et al. "Delamanid improves outcomes and reduces mortality in multidrug-
resistant tuberculosis." European Respiratory Journal 41.6 (2013): 1393-1400.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
RESEARCH PROPOSAL
Sotgiu, Giovanni, et al. "Efficacy, safety and tolerability of linezolid containing regimens in
treating MDR-TB and XDR-TB: systematic review and meta-analysis." European
Respiratory Journal 40.6 (2012): 1430-1442.
Streicher, Elizabeth M., et al. "Emergence and treatment of multidrug resistant (MDR) and
extensively drug-resistant (XDR) tuberculosis in South Africa." Infection, genetics and
evolution 12.4 (2012): 686-694.
Udwadia, Zarir F., et al. "Totally drug-resistant tuberculosis in India." Clinical Infectious
Diseases 54.4 (2012): 579-581.
Van Wetering, S. A. N. D. R. A., et al. "Effect of defensins on interleukin-8 synthesis in
airway epithelial cells." American Journal of Physiology-Lung Cellular and Molecular
Physiology272.5 (1997): L888-L896.
Wang, Guangshun, Xia Li, and Zhe Wang. "APD2: the updated antimicrobial peptide
database and its application in peptide design." Nucleic acids research 37.suppl_1 (2008):
D933-D937.
World Health Organization, ed. Global tuberculosis report 2013.World Health Organization,
2013.
RESEARCH PROPOSAL
Sotgiu, Giovanni, et al. "Efficacy, safety and tolerability of linezolid containing regimens in
treating MDR-TB and XDR-TB: systematic review and meta-analysis." European
Respiratory Journal 40.6 (2012): 1430-1442.
Streicher, Elizabeth M., et al. "Emergence and treatment of multidrug resistant (MDR) and
extensively drug-resistant (XDR) tuberculosis in South Africa." Infection, genetics and
evolution 12.4 (2012): 686-694.
Udwadia, Zarir F., et al. "Totally drug-resistant tuberculosis in India." Clinical Infectious
Diseases 54.4 (2012): 579-581.
Van Wetering, S. A. N. D. R. A., et al. "Effect of defensins on interleukin-8 synthesis in
airway epithelial cells." American Journal of Physiology-Lung Cellular and Molecular
Physiology272.5 (1997): L888-L896.
Wang, Guangshun, Xia Li, and Zhe Wang. "APD2: the updated antimicrobial peptide
database and its application in peptide design." Nucleic acids research 37.suppl_1 (2008):
D933-D937.
World Health Organization, ed. Global tuberculosis report 2013.World Health Organization,
2013.
11
RESEARCH PROPOSAL
Bibliography
Ashitani J, Mukae H, Hiratsuka T, Nakazato M, Kumamoto K, Matsukura S. Elevated levels
of a-defensins in plasma and BAL fluid of patients with active pulmonary tuberculosis. Chest
2002;121:519e26.
Baltzer SA, Brown MH. Antimicrobial peptides: promising alternatives to conventional
antibiotics. J MolMicrobiolBiotechnol 2011;20(4):228e35.
Chan DI, Prenner EJ, Vogel HJ. Tryptophan- and arginine-rich antimicrobial peptides:
structures and mechanisms of action.BiochimBiophysActa 2006;1758(9):1184e202.
Driss V, Legrand F, Hermann E, Loiseau S, Guerardel Y, Kremer L, Adam E, Woerly G,
Dombrowicz D, Capron M. TLR2-dependent eosinophil interactions with mycobacteria: role
of alpha-defensins. Blood 2009;113(14): 3235e44.
Faurschou M, Kamp S, Cowland JB, Udby L, Johnsen AH, Calafat J, Winther H, Borregaard
N. Prodefensins are matrix proteins of specific granules in human neutrophils. J LeukocBiol
2005;78(3):785e93.
Garcia JRC, Jaumann F, Schulz S, Krause A, Rodriguez-Jimenez J, Forssmann U, Adermann
K, Klüver E, Vogelmeier C, Becker D, Hedrich R, Forssmann WG, Bals R. Identification of a
novel, multifunctional defensin (human defensin 3) with specific antimicrobial activity: its
interaction with plasma membranes of Xenopus oocytes and the induction of macrophage
chemoattraction. Cell Tissue Res 2001;306(2):257e64.
García-Pérez BE, Villagómez-Palatto DA, Castañeda-Sánchez JI, CoralVázquez RM,
Ramírez-Sánchez I, Ordoñez-Razo RM, Luna-Herrera J. Innate response of human
endothelial cells infected with mycobacteria. Immunobiology 2011;216(8):925e35.
RESEARCH PROPOSAL
Bibliography
Ashitani J, Mukae H, Hiratsuka T, Nakazato M, Kumamoto K, Matsukura S. Elevated levels
of a-defensins in plasma and BAL fluid of patients with active pulmonary tuberculosis. Chest
2002;121:519e26.
Baltzer SA, Brown MH. Antimicrobial peptides: promising alternatives to conventional
antibiotics. J MolMicrobiolBiotechnol 2011;20(4):228e35.
Chan DI, Prenner EJ, Vogel HJ. Tryptophan- and arginine-rich antimicrobial peptides:
structures and mechanisms of action.BiochimBiophysActa 2006;1758(9):1184e202.
Driss V, Legrand F, Hermann E, Loiseau S, Guerardel Y, Kremer L, Adam E, Woerly G,
Dombrowicz D, Capron M. TLR2-dependent eosinophil interactions with mycobacteria: role
of alpha-defensins. Blood 2009;113(14): 3235e44.
Faurschou M, Kamp S, Cowland JB, Udby L, Johnsen AH, Calafat J, Winther H, Borregaard
N. Prodefensins are matrix proteins of specific granules in human neutrophils. J LeukocBiol
2005;78(3):785e93.
Garcia JRC, Jaumann F, Schulz S, Krause A, Rodriguez-Jimenez J, Forssmann U, Adermann
K, Klüver E, Vogelmeier C, Becker D, Hedrich R, Forssmann WG, Bals R. Identification of a
novel, multifunctional defensin (human defensin 3) with specific antimicrobial activity: its
interaction with plasma membranes of Xenopus oocytes and the induction of macrophage
chemoattraction. Cell Tissue Res 2001;306(2):257e64.
García-Pérez BE, Villagómez-Palatto DA, Castañeda-Sánchez JI, CoralVázquez RM,
Ramírez-Sánchez I, Ordoñez-Razo RM, Luna-Herrera J. Innate response of human
endothelial cells infected with mycobacteria. Immunobiology 2011;216(8):925e35.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





