Mechanical versus manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled trial
Select 7 articles published within the last 5 years that focus on a single intervention. Use primary and secondary research, quantitative and qualitative studies. Run Turnitin on your own work, not the selected articles. Use the provided tools and examples to set up your paper and reference page. Articulate the healthcare problem, its significance, current practice, and impact on background. Create a PICO table and question. Fill in an evidence matrix with the selected articles.
Added on 2023-06-15
About This Document
Mechanical versus manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled trial
Select 7 articles published within the last 5 years that focus on a single intervention. Use primary and secondary research, quantitative and qualitative studies. Run Turnitin on your own work, not the selected articles. Use the provided tools and examples to set up your paper and reference page. Articulate the healthcare problem, its significance, current practice, and impact on background. Create a PICO table and question. Fill in an evidence matrix with the selected articles.
Added on 2023-06-15
www.thelancet.com Vol 385 March 14, 2015 947
Mechanical versus manual chest compression for
out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic,
cluster randomised controlled trial
Gavin D Perkins, Ranjit Lall, Tom Quinn, Charles D Deakin, Matthew W Cooke, Jessica Horton, Sarah E Lamb, Anne-Marie Slowther,
Malcolm Woollard, Andy Carson, Mike Smyth, Richard Whitfield, Amanda Williams, Helen Pocock, John J M Black, John Wright, Kyee Han,
Simon Gates, PARAMEDIC trial collaborators*
Summary
Background Mechanical chest compression devices have the potential to help maintain high-quality cardiopulmonary
resuscitation (CPR), but despite their increasing use, little evidence exists for their effectiveness. We aimed to study
whether the introduction of LUCAS-2 mechanical CPR into front-line emergency response vehicles would improve
survival from out-of-hospital cardiac arrest.
Methods The pre-hospital randomised assessment of a mechanical compression device in cardiac arrest (PARAMEDIC)
trial was a pragmatic, cluster-randomised open-label trial including adults with non-traumatic, out-of-hospital cardiac
arrest from four UK Ambulance Services (West Midlands, North East England, Wales, South Central). 91 urban and
semi-urban ambulance stations were selected for participation. Clusters were ambulance service vehicles, which were
randomly assigned (1:2) to LUCAS-2 or manual CPR. Patients received LUCAS-2 mechanical chest compression or
manual chest compressions according to the first trial vehicle to arrive on scene. The primary outcome was survival at
30 days following cardiac arrest and was analysed by intention to treat. Ambulance dispatch staff and those collecting
the primary outcome were masked to treatment allocation. Masking of the ambulance staff who delivered the
interventions and reported initial response to treatment was not possible. The study is registered with Current
Controlled Trials, number ISRCTN08233942.
Findings We enrolled 4471 eligible patients (1652 assigned to the LUCAS-2 group, 2819 assigned to the control group)
between April 15, 2010 and June 10, 2013. 985 (60%) patients in the LUCAS-2 group received mechanical chest compression,
and 11 (<1%) patients in the control group received LUCAS-2. In the intention-to-treat analysis, 30 day survival was similar
in the LUCAS-2 group (104 [6%] of 1652 patients) and in the manual CPR group (193 [7%] of 2819 patients; adjusted odds
ratio [OR] 0·86, 95% CI 0·64–1·15). No serious adverse events were noted. Seven clinical adverse events were reported in
the LUCAS-2 group (three patients with chest bruising, two with chest lacerations, and two with blood in mouth). 15 device
incidents occurred during operational use. No adverse or serious adverse events were reported in the manual group.
Interpretation We noted no evidence of improvement in 30 day survival with LUCAS-2 compared with manual
compressions. On the basis of ours and other recent randomised trials, widespread adoption of mechanical CPR
devices for routine use does not improve survival.
Funding National Institute for Health Research HTA – 07/37/69.
Copyright © Perkins et al. Open Access article distributed under the terms of CC BY.
Introduction
The burden of cardiac arrest out of hospital is
substantial, with an estimated 424 000 cardiac arrests
occurring each year of about in the USA 1 and 275 000 in
Europe. 2 As few as one in 12 victims of cardiac arrest out
of hospital survive to return home. 3,4 High-quality chest
compressions of sufficient depth 5 and rate, 6 with full
recoil of the chest between compressions 7 and avoidance
of interruptions 8 are crucial to survival. Maintenance
of high-quality compressions during out-of-hospital
resuscitation is difficult because of the small number of
crew present, fatigue, patient access, competing tasks
(eg, defibrillation, vascular access) and difficulty of
performing resuscitation in a moving vehicle. 9
Mechanical compression devices suitable for use in the
pre-hospital environment have been developed to automate
and potentially improve this process. At the time of
initiating this study, one large randomised trial of a load
distributing band mechanical device had been done and
was terminated early because of the worsened long-term
outcomes in patients allocated to mechanical compression.10
The subsequent Cochrane review reported insufficient
evidence to conclude that mechanical chest compressions
are associated with benefit or harm and their widespread
use is not supported.11 Since then, two further large
randomised efficacy trials have been reported. The CIRC
trial12 assessed the load distributing band and reported
it was equivalent to manual cardiopulmonary resuscitation
Lancet 2015; 385: 947–55
Published Online
November 16, 2014
http://dx.doi.org/10.1016/
S0140-6736(14)61886-9
See Comment page 920
*Collaborators listed at end
of paper
Warwick Clinical Trials Unit,
University of Warwick,
Coventry, UK
(Prof G D Perkins MD, R Lall PhD,
Prof M W Cooke PhD,
J Horton MSc,
Prof S E Lamb DPhil,
A-M Slowther DPhil,
M Smyth MSc, Prof S Gates PhD);
Heart of England NHS
Foundation Trust,
Birmingham, UK,
(Prof G D Perkins); Surrey
Peri-operative Anaesthesia
Critical care collaborative
Research Group, Faculty of
Health and Medical Sciences,
University of Surrey, Guildford,
UK (Prof T Quinn M Phil,
Prof M Woollard MPH,
Prof C D Deakin MD); South
Central Ambulance Service
NHS Foundation Trust,
Otterbourne, UK
(Prof C D Deakin, H Pocock MSc,
J J M Black FCEM); NIHR
Southampton Respiratory
Biomedical Research Unit,
University Hospital
Southampton NHS Foundation
Trust, Southampton
Hampshire (Prof C D Deakin);
University of Oxford, Oxford,
UK (Prof S E Lamb); West
Midlands Ambulance Service
NHS Foundation Trust, Brierley
Hill, UK (A Carson FRCGP,
M Smyth); Welsh Ambulance
Services NHS Trust,
Denbighshire, Wales, UK
(R Whitfield BSc, A Williams MA);
North East Ambulance Service
NHS Foundation Trust,
Newcastle upon Tyne, UK
(J Wright FCEM, K Han FCEM);
and Royal Victoria Infirmary,
Newcastle upon Tyne, UK
(J Wright)
948 www.thelancet.com Vol 385 March 14, 2015
Correspondence to:
Prof Gavin Perkins, Warwick
Clinical Trials Unit, University of
Warwick, Coventry CV4 7AL, UK
g.d.perkins@warwick.ac.uk
(CPR). The LINC trial13 assessed the LUCAS device and
concluded that mechanical CPR did not result in improved
outcomes compared with manual CPR.13
Previous trials were designed as efficacy (explanatory)
trials, which aim to answer the question “Can this
intervention work under ideal conditions?”. We sought to
study mechanical CPR use under real life conditions, and
therefore adopted a pragmatic design for the pre-hospital
randomised assessment of a mechanical compression
device in cardiac arrest (PARAMEDIC) trial. The trial
sought to assess whether LUCAS-2 was better than
manual CPR for the improvement of 30 day survival
in adults receiving resuscitation for non-traumatic,
out-of-hospital cardiac arrest.
Methods
Trial design and participants
The PARAMEDIC trial was a pragmatic, cluster
randomised trial, with ambulance service vehicles as the
unit of randomisation. The trial protocol has been
published previously.14
The trial was done in partnership with four UK National
Health Service (NHS) Ambulance Services (West Midlands,
North East England, Wales, South Central). These sites
serve a total population of 13 million people spread over
62 160 km². We selected 91 ambulance stations for
participation based on their location (urban and semi-urban
settings, representing 25% of stations). A dispatch centre
in each region coordinated the emergency response. The
nearest available rapid response vehicle (RRV) or
ambulance was dispatched to cases of suspected cardiac
arrest. Back-up was provided by a second vehicle as soon as
possible. If there was clear evidence that life was extinct (eg,
rigor mortis, post-mortem staining; see appendix for full
details) or the patient had a do-not-attempt-resuscitation
order, ambulance staff were authorised to recognise death
and withhold CPR. Where resuscitation was indicated,
ambulance staff had been trained in advanced airway
management, drug administration, and external defib-
rillation, and follow standardised national guidelines based
on the European Resuscitation Council Guidelines.15,16 If
the patient did not respond despite full ALS intervention
and remained asystolic for more than 20 min then the
resuscitation attempt could be discontinued. Unless these
criteria were met, resuscitation was continued and the
patient was transported to the nearest emergency
department with continuous CPR. CPR quality and
feedback technology was not available in any of the
participating ambulance services.
We chose broad eligibility criteria, indicating the
pragmatic nature of the trial. Individual patients were
included in the study if a trial vehicle was the first
ambulance service vehicle on scene, the patient was in
cardiac arrest outside of a hospital, resuscitation was
attempted, and the patient was known or believed to be
aged 18 years or older. Exclusion criteria were cardiac
arrest caused by trauma, and known or clinically
apparent pregnancy.
Ambulance services recorded cardiac arrest data
according to variables contained in the Utstein template.17
Every ambulance service submitted these data to a central
trial database.
Enrolment proceeded with a waiver of informed
consent, in line with the Mental Capacity Act 2005. The
trial team contacted patients who were discharged from
hospital to let them know of their enrolment and to invite
them to take part in the follow-up 3 months and
12 months after cardiac arrest. Those willing to take part
provided written informed consent. For those who did
not have capacity, a personal consultee completed the
questionnaires on behalf of the patient.
The Coventry Research Ethics Committee (reference
09/H1210/69) approved the study, and University of
Warwick, UK sponsored it. The study was done in
accordance with the principles of Good Clinical Practice
and the Mental Capacity Act (2005).
Randomisation and masking
Because the number of LUCAS devices available to the
trial was limited to 143, we used a ratio of about 1 LUCAS
to 2 control to optimise efficiency. Individual ambulance
See Online for appendix
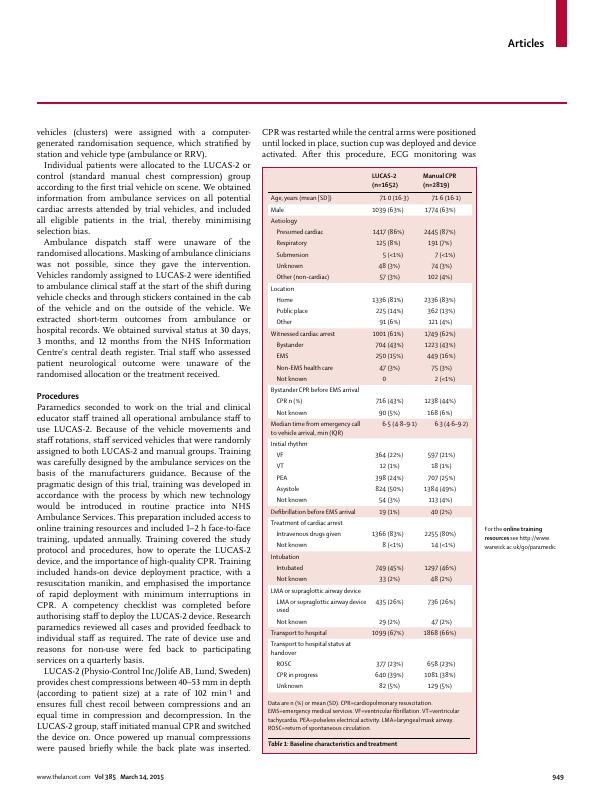
Figure 1: Trial profile
*Seven met more than one exclusion criteria. †Reasons LUCAS-2 not used: 78 because of crew not trained;
168 because of crew error; 26 no device in vehicle; 102 unsuitable patients (58 patient too large, 22 patient too
small, 22 other reason–eg, chest deformity), 14 device issues, 140 not possible to use device; 110 reason unknown.
Reasons for LUCAS-2 use in control group were crew error.
418 clusters recruited
11 171 patients from emergency
incidents attended
4689 assessed for eligibility
6482 recognition of life extinct or
no resuscitation attempted
218 excluded*
2 pregnant
107 trauma
107 aged younger than 18 years
9 not out of hospital4471 enrolled
147 clusters allocated to LUCAS-2 group
1652 patients allocated to LUCAS-2 group
985 received LUCAS-2 chest compression
638 received manual chest compression†
29 intervention received unknown
271 clusters allocated to control group
2819 patients allocated to control group
2808 received manual chest compression
11 received LUCAS-2 chest compression
1 unknown survival status
1652 followed up to 3 months and 12 months
1652 analysed
2818 followed up to 3 months and 12 months
2818 analysed
www.thelancet.com Vol 385 March 14, 2015 949
vehicles (clusters) were assigned with a computer-
generated randomisation sequence, which stratified by
station and vehicle type (ambulance or RRV).
Individual patients were allocated to the LUCAS-2 or
control (standard manual chest compression) group
according to the first trial vehicle on scene. We obtained
information from ambulance services on all potential
cardiac arrests attended by trial vehicles, and included
all eligible patients in the trial, thereby minimising
selection bias.
Ambulance dispatch staff were unaware of the
randomised allocations. Masking of ambulance clinicians
was not possible, since they gave the intervention.
Vehicles randomly assigned to LUCAS-2 were identified
to ambulance clinical staff at the start of the shift during
vehicle checks and through stickers contained in the cab
of the vehicle and on the outside of the vehicle. We
extracted short-term outcomes from ambulance or
hospital records. We obtained survival status at 30 days,
3 months, and 12 months from the NHS Information
Centre’s central death register. Trial staff who assessed
patient neurological outcome were unaware of the
randomised allocation or the treatment received.
Procedures
Paramedics seconded to work on the trial and clinical
educator staff trained all operational ambulance staff to
use LUCAS-2. Because of the vehicle movements and
staff rotations, staff serviced vehicles that were randomly
assigned to both LUCAS-2 and manual groups. Training
was carefully designed by the ambulance services on the
basis of the manufacturers guidance. Because of the
pragmatic design of this trial, training was developed in
accordance with the process by which new technology
would be introduced in routine practice into NHS
Ambulance Services. This preparation included access to
online training resources and included 1–2 h face-to-face
training, updated annually. Training covered the study
protocol and procedures, how to operate the LUCAS-2
device, and the importance of high-quality CPR. Training
included hands-on device deployment practice, with a
resuscitation manikin, and emphasised the importance
of rapid deployment with minimum interruptions in
CPR. A competency checklist was completed before
authorising staff to deploy the LUCAS-2 device. Research
paramedics reviewed all cases and provided feedback to
individual staff as required. The rate of device use and
reasons for non-use were fed back to participating
services on a quarterly basis.
LUCAS-2 (Physio-Control Inc/Jolife AB, Lund, Sweden)
provides chest compressions between 40–53 mm in depth
(according to patient size) at a rate of 102 min–
¹ and
ensures full chest recoil between compressions and an
equal time in compression and decompression. In the
LUCAS-2 group, staff initiated manual CPR and switched
the device on. Once powered up manual compressions
were paused briefly while the back plate was inserted.
CPR was restarted while the central arms were positioned
until locked in place, suction cup was deployed and device
activated. After this procedure, ECG monitoring was
For the online training
resources see http://www.
warwick.ac.uk/go/paramedic
LUCAS-2
(n=1652)
Manual CPR
(n=2819)
Age, years (mean [SD]) 71·0 (16·3) 71·6 (16·1)
Male 1039 (63%) 1774 (63%)
Aetiology
Presumed cardiac 1417 (86%) 2445 (87%)
Respiratory 125 (8%) 191 (7%)
Submersion 5 (<1%) 7 (<1%)
Unknown 48 (3%) 74 (3%)
Other (non-cardiac) 57 (3%) 102 (4%)
Location
Home 1336 (81%) 2336 (83%)
Public place 225 (14%) 362 (13%)
Other 91 (6%) 121 (4%)
Witnessed cardiac arrest 1001 (61%) 1749 (62%)
Bystander 704 (43%) 1223 (43%)
EMS 250 (15%) 449 (16%)
Non-EMS health care 47 (3%) 75 (3%)
Not known 0 2 (<1%)
Bystander CPR before EMS arrival
CPR n (%) 716 (43%) 1238 (44%)
Not known 90 (5%) 168 (6%)
Median time from emergency call
to vehicle arrival, min (IQR)
6·5 (4·8–9·1) 6·3 (4·6–9·2)
Initial rhythm
VF 364 (22%) 597 (21%)
VT 12 (1%) 18 (1%)
PEA 398 (24%) 707 (25%)
Asystole 824 (50%) 1384 (49%)
Not known 54 (3%) 113 (4%)
Defi brillation before EMS arrival 19 (1%) 40 (2%)
Treatment of cardiac arrest
Intravenous drugs given 1366 (83%) 2255 (80%)
Not known 8 (<1%) 14 (<1%)
Intubation
Intubated 749 (45%) 1297 (46%)
Not known 33 (2%) 48 (2%)
LMA or supraglottic airway device
LMA or supraglottic airway device
used
435 (26%) 736 (26%)
Not known 29 (2%) 47 (2%)
Transport to hospital 1099 (67%) 1868 (66%)
Transport to hospital status at
handover
ROSC 377 (23%) 658 (23%)
CPR in progress 640 (39%) 1081 (38%)
Unknown 82 (5%) 129 (5%)
Data are n (%) or mean (SD). CPR=cardiopulmonary resuscitation.
EMS=emergency medical services. VF=ventricular fibrillation. VT=ventricular
tachycardia. PEA=pulseless electrical activity. LMA=laryngeal mask airway.
ROSC=return of spontaneous circulation.
Table 1: Baseline characteristics and treatment
950 www.thelancet.com Vol 385 March 14, 2015
established and LUCAS-2 was briefly paused to check the
ECG rhythm. If the patient was in a shockable rhythm
LUCAS-2 was restarted and defibrillation was attempted
with continuous mechanical CPR.
Patients in the control group received manual CPR
aiming for a target compression depth of 50–60 mm,
rate 100–120 min – ¹, full recoil between compressions
and an equal time in compression and decompression
in line with guidelines. CPR was started on arrival and
ECG monitoring established. Chest compressions were
paused briefly to allow rhythm analysis and if
appropriate, attempted defibrillation. Both groups
received compression to ventilation ratio of 30:2 before
intubation and continuous compressions with asyn-
chronous ventilation after intubation.
Outcomes
The primary outcome of the study was survival to 30 days
after the cardiac arrest event. The main secondary clinical
outcomes were survived event (return of spontaneous
circulation [ROSC] sustained until admission and
transfer of care to medical staff at the receiving hospital),
survival to 3 months, survival to 12 months, and survival
with favourable neurological outcome at 3 months. The
initial trial protocol originally specified survival to
hospital discharge as an additional outcome; this
outcome is not reported here because survival to 30 days
is more clinically meaningful, and these data could not
be obtained from all hospitals included in the trial
because of logistical and governance difficulties. We have
reported ROSC as an additional (non-prespecified)
outcome since it is part of the Utstein template. 17
We defined favourable neurological outcome as a
Cerebral Performance Category (CPC) score17 of 1 or 2 at
3 months. CPC was extracted from medical records or
assessed at a face-to-face visit done by research staff.
Statistical analysis
At the time of the design of this study, there were no
randomised trials using the LUCAS device on which to
base the likely treatment effect. We determined the
minimally important diff erence to our decision makers
(the NHS) through discussion with partner ambulance
services and subsequent agreement with the funder. The
study had 80% power to find a significant result (with
threshold two-sided p value of 0·05) if the incidence of
survival to 30 days was 5% in the manual CPR group and
7·5% in the LUCAS-2 group. Using an intracluster
correlation coefficient of 0·01 to allow for clustering, and
a cluster size of 15, we aimed to recruit 245 clusters
(3675 patients) into the trial.
The target sample size was revised in September, 2012,
after recruitment of 2469 patients, to take account of the
frequency of use of LUCAS-2 and updated information
on the cluster size. With the agreement of the Data
Monitoring Committee and the Trial Steering Committee,
we increased the target sample size to 4344 patients. We
estimated this sample size to have a sufficient number of
cases of LUCAS-2 use to maintain the originally specified
power. The sample size re-estimation did not use any
information from comparisons between the trial groups.
The primary analysis was by intention to treat. This
analysis explores if the treatment works under the usual
conditions, with all the noise inherent therein. We used
complier average causal effect (CACE) analyses, to
estimate the effect in cardiac arrest where the protocol was
followed.18,19 CACE estimates the treatment effect in people
randomly assigned to the intervention who actually
received it, by comparing compliers in the intervention
group with those participants in the control group who
would have been compliers if they had been allocated
to the intervention group. This analysis retains the
advantages of randomisation and avoids introducing bias,
hence CACE is preferred to per-protocol analysis. We did
two CACE analyses, defining compliers in different ways.
In CACE1, we treated as non-compliant those cases in
which LUCAS-2 was not used for unknown or trial-related
reasons that would not occur in real-life clinical practice
(eg, crew were not trained in trial procedures, crew
misunderstood the trial protocol, the device was missing
from the vehicle). This analysis omits trial-related non-use
and might be a better estimate of the treatment effect in
real-world clinical practice analysis by intention to treat. In
the CACE2 analysis, we only treated as compliant those
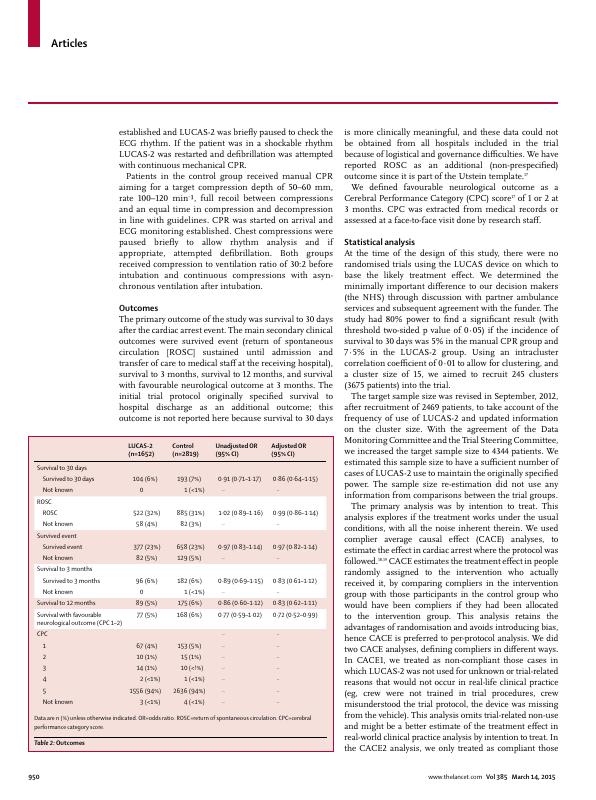
LUCAS-2
(n=1652)
Control
(n=2819)
Unadjusted OR
(95% CI)
Adjusted OR
(95% CI)
Survival to 30 days
Survived to 30 days 104 (6%) 193 (7%) 0·91 (0·71–1·17) 0·86 (0·64–1·15)
Not known 0 1 (<1%) ·· ··
ROSC
ROSC 522 (32%) 885 (31%) 1·02 (0·89–1·16) 0·99 (0·86–1·14)
Not known 58 (4%) 82 (3%) ·· ··
Survived event
Survived event 377 (23%) 658 (23%) 0·97 (0·83–1·14) 0·97 (0·82–1·14)
Not known 82 (5%) 129 (5%) ·· ··
Survival to 3 months
Survived to 3 months 96 (6%) 182 (6%) 0·89 (0·69–1·15) 0·83 (0·61–1·12)
Not known 0 1 (<1%) ·· ··
Survival to 12 months 89 (5%) 175 (6%) 0·86 (0·60–1·12) 0·83 (0·62–1·11)
Survival with favourable
neurological outcome (CPC 1–2)
77 (5%) 168 (6%) 0·77 (0·59–1·02) 0·72 (0·52–0·99)
CPC ·· ··
1 67 (4%) 153 (5%) ·· ··
2 10 (1%) 15 (1%) ·· ··
3 14 (1%) 10 (<!%) ·· ··
4 2 (<1%) 1 (<1%) ·· ··
5 1556 (94%) 2636 (94%) ·· ··
Not known 3 (<1%) 4 (<1%) ·· ··
Data are n (%) unless otherwise indicated. OR=odds ratio. ROSC=return of spontaneous circulation. CPC=cerebral
performance category score.
Table 2: Outcomes
End of preview
Want to access all the pages? Upload your documents or become a member.
