Mental Health: Act, Practice, and Stigma Report - MHN 030
VerifiedAdded on 2022/11/28
|44
|13061
|132
Report
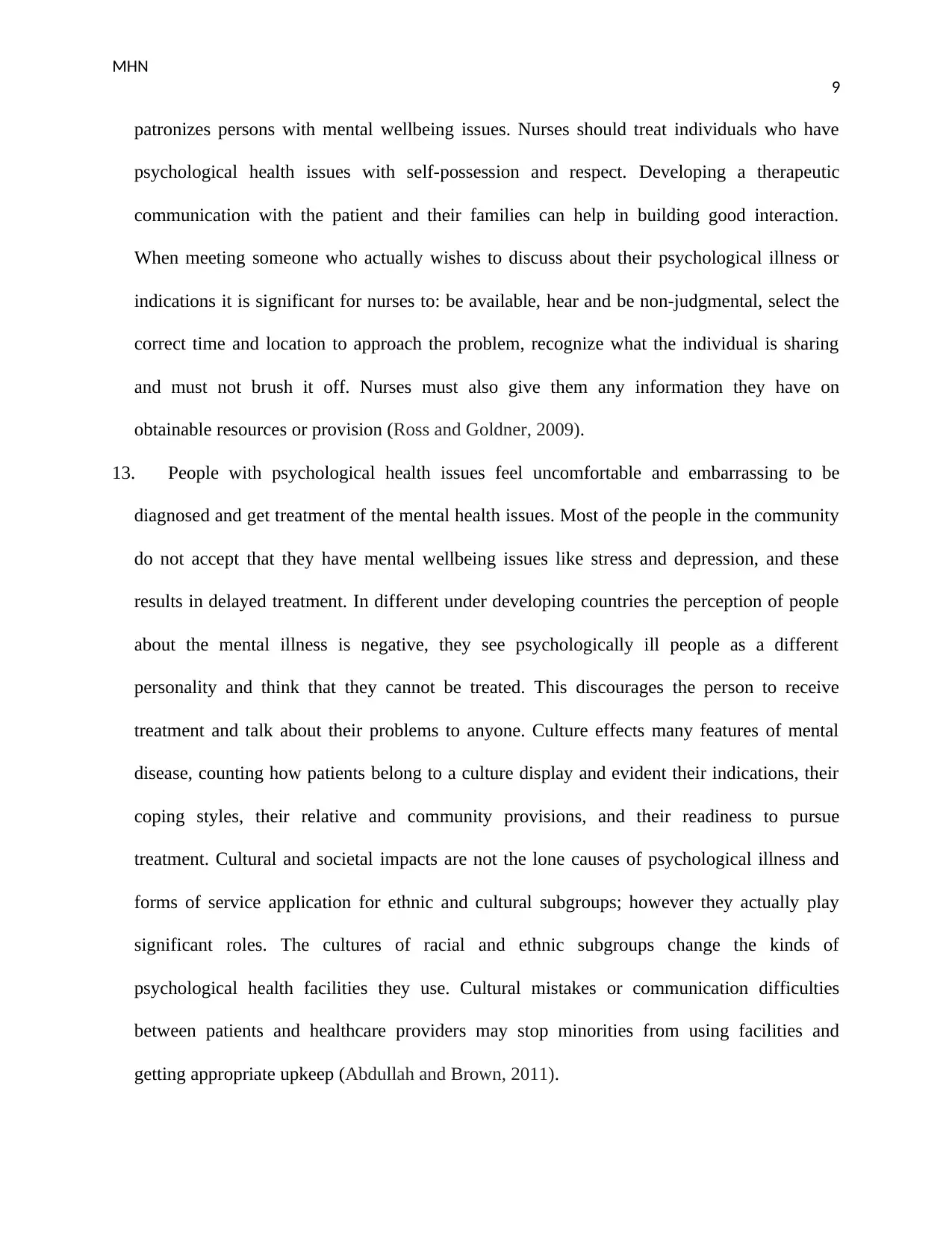
AI Summary
This report delves into the multifaceted realm of mental health, encompassing definitions of mental well-being and illness, and the factors influencing them. It examines the Mental Health Act 2013, outlining its key provisions concerning involuntary admission, consumer rights, review processes, and other critical aspects. The report analyzes how these legal frameworks and ethical guidelines, including the NMBA Enrolled Nurse Standards for Practice, the Code of Conduct for Nurses, and the Code of Ethics for Nurses, are applied in nursing practice. Furthermore, it explores the impact of stigma, discrimination, and cultural beliefs on individuals with mental illnesses, and discusses the role of the mental health practitioner, consent, and confidentiality. The report offers insights into the signs and symptoms of mental illness, and the social, psychological, cognitive, and physical factors that contribute to its development, providing a comprehensive overview of the subject matter.

Running Head: MHN
0
Mental Health Nursing
student
7/7/2019
0
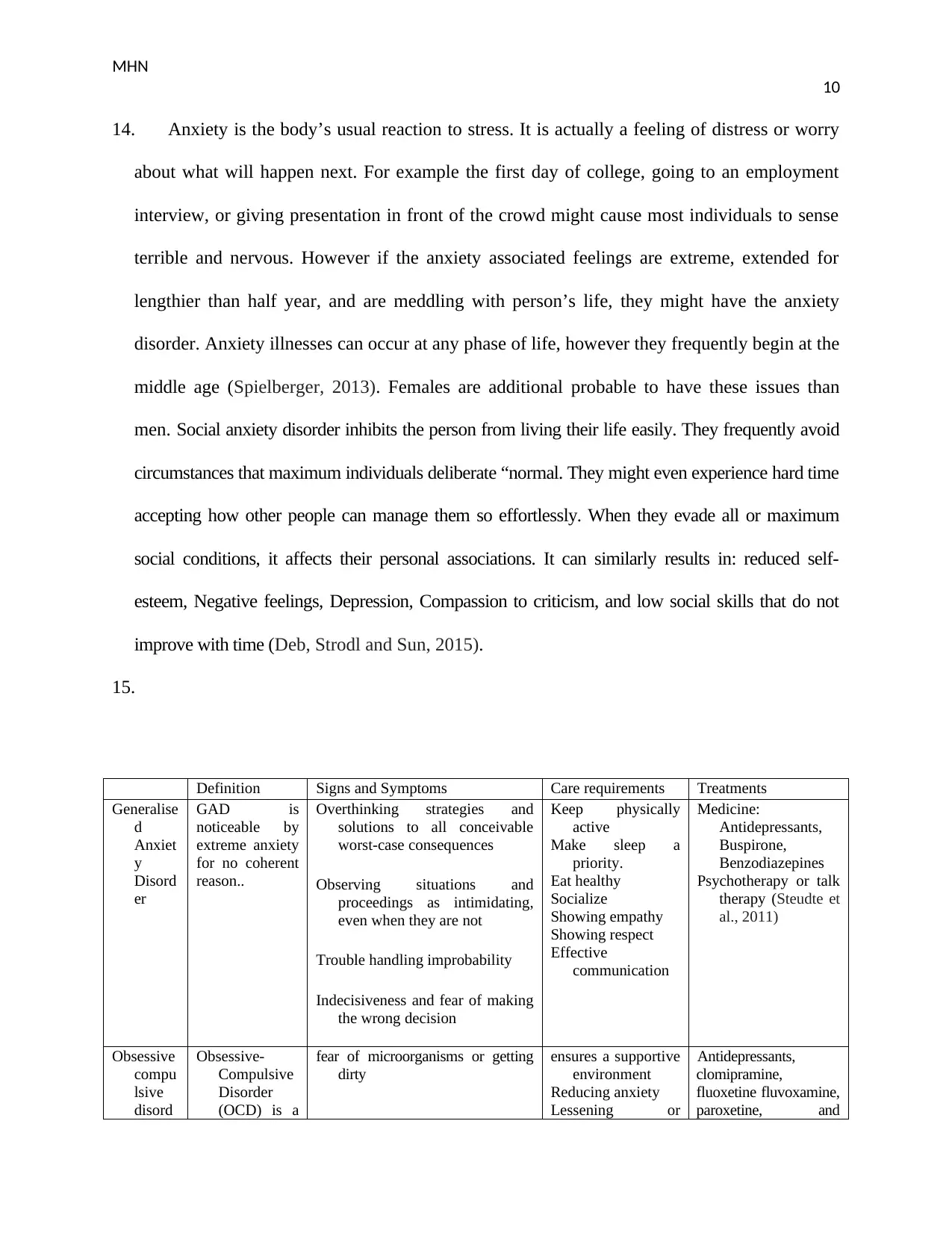
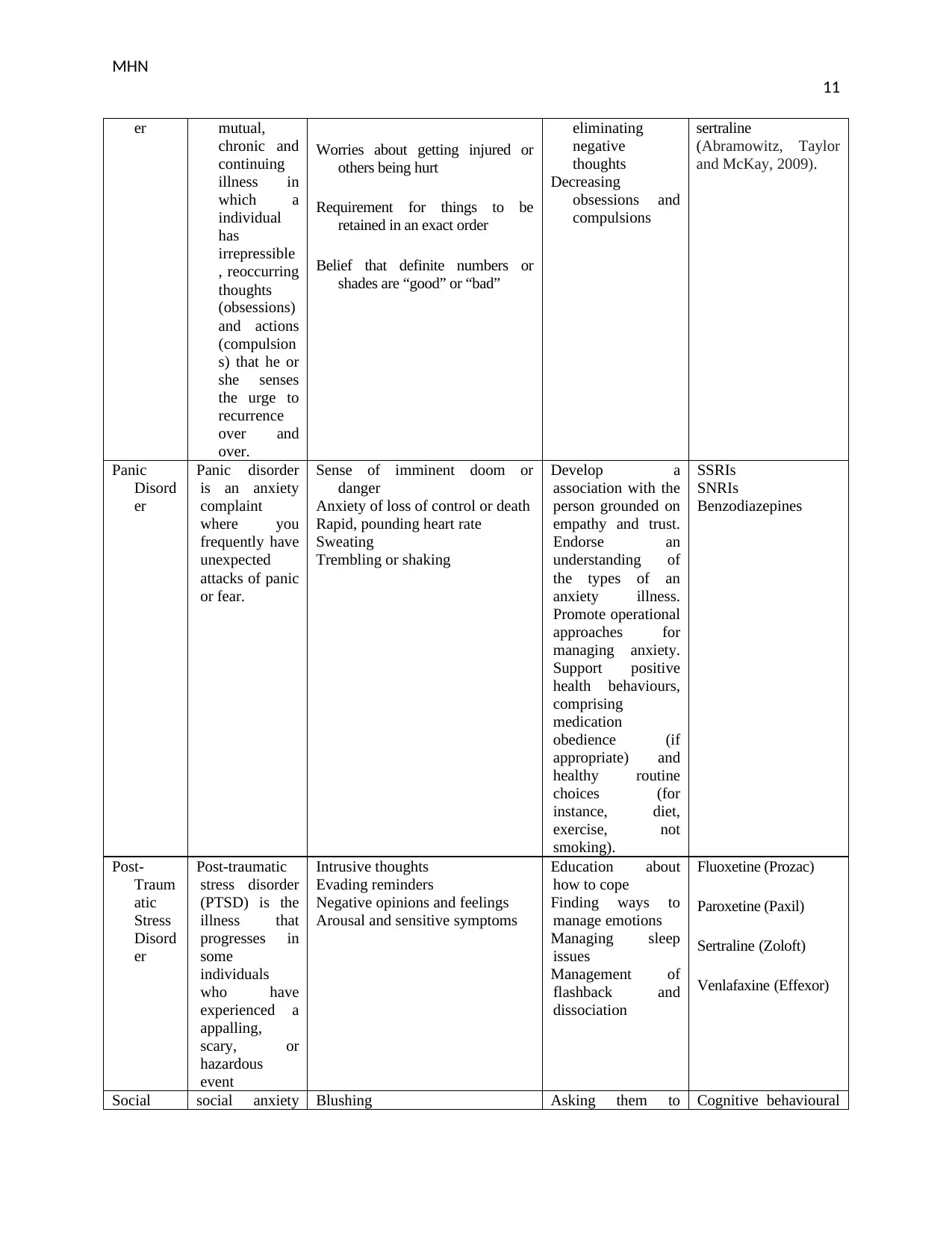
Mental Health Nursing
student
7/7/2019
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MHN
1
1. Mental health comprises a person’s emotional, mental and societal wellbeing. It impacts how
an individual thinks, sense, and act. It similarly assist in determining how people manage the
stress, relate to other people, and making decision. Mental wellbeing is essential at all stages
of life, ranging from babyhood to teenage through middle age. Positive mental health permits
individuals to realize their actual potential, cope with the stressful situation of life, work
productivity, and make significant support to their societies. One can manage the positive
mental health by getting help from professionals, connecting with other, staying positive etc.
(Corrigan, Druss and Perlick, 2014).
Mental illness, also termed psychological health disorders, can be referred as the wide range of
psychological health conditions or disorder that impacts the patient’s mood, thoughts, and
behaviour. Some of the mental health illnesses include addictive behaviour, depression,
anxiety related disorder, schizophrenia, and eating disorder. Some of the symptoms associated
with mental disease comprise feeling sad, extreme fear or worries, unusual mood changes,
social isolation, excessive anger, hostility, violence, and suicidal thoughts. It has been
identified by WHO that nearly 20 per cent of the children and teenage affected with mental
illness or issues globally (WHO, 2019)
2. I think these facts related to mental wellbeing and mental illness is mostly correct as the
researchers also evidenced these facts. Mental health is essential not only for psychological
health, but also for physical health. An individual with good physical health cannot assure that
the person is fit and vice versa. I think people with healthy mind can perform their activities
associated with the personal and professional life. I am well aware of above mentioned fact
and agree with them, as research shows that the increased levels of mental health is linked
with the increased learning ability, creativity, and productivity. I think people with positive
1
1. Mental health comprises a person’s emotional, mental and societal wellbeing. It impacts how
an individual thinks, sense, and act. It similarly assist in determining how people manage the
stress, relate to other people, and making decision. Mental wellbeing is essential at all stages
of life, ranging from babyhood to teenage through middle age. Positive mental health permits
individuals to realize their actual potential, cope with the stressful situation of life, work
productivity, and make significant support to their societies. One can manage the positive
mental health by getting help from professionals, connecting with other, staying positive etc.
(Corrigan, Druss and Perlick, 2014).
Mental illness, also termed psychological health disorders, can be referred as the wide range of
psychological health conditions or disorder that impacts the patient’s mood, thoughts, and
behaviour. Some of the mental health illnesses include addictive behaviour, depression,
anxiety related disorder, schizophrenia, and eating disorder. Some of the symptoms associated
with mental disease comprise feeling sad, extreme fear or worries, unusual mood changes,
social isolation, excessive anger, hostility, violence, and suicidal thoughts. It has been
identified by WHO that nearly 20 per cent of the children and teenage affected with mental
illness or issues globally (WHO, 2019)
2. I think these facts related to mental wellbeing and mental illness is mostly correct as the
researchers also evidenced these facts. Mental health is essential not only for psychological
health, but also for physical health. An individual with good physical health cannot assure that
the person is fit and vice versa. I think people with healthy mind can perform their activities
associated with the personal and professional life. I am well aware of above mentioned fact
and agree with them, as research shows that the increased levels of mental health is linked
with the increased learning ability, creativity, and productivity. I think people with positive
MHN
2
mental health can build a strong relationship with their loved ones and other people around
them. In my opinion mental health illnesses are not restricted to a particular country or state,
it has been affecting people from all around the world. I think people must take care of their
mental health and manage mental illnesses with the help health diet, exercise, social
interaction, and taking help from health professionals.
3. Some of the facts were just as I have expected, this is because mental health has become an
essential part of life in today’s scenarios. But there are some facts that really surprised me
including the number of young people affected with mental health issues. I knew that the
mental illnesses are mostly affect older people, It was surprising for me know that nearly 20
per cent of the young population including children are affected with this health condition.
One of the other facts that surprise me was the advantages of mental health in contribution
towards community services. I knew that positive mental health can help at individual level
and help people in developing healthy relationships, being able to cope with stressful
situation, but I was not aware about its role in community. But it can help the individual to
participate in activities and work in favour of the community; this can be only done of the
person is psychologically healthy (Knapp, McDaid and Parsonage, 2011).
4. Mental health is the state of healthiness in which the person realizes his or her personal
capabilities, how can manage the normal tensions of life, can work effectively and profitably
and is capable to make a support to his or her communal. Mental illness is the identified,
medically diagnosable disease that leads to the significant diminishing of a person’s cognitive,
affecting or relational capabilities. Mental ailments result from biological, developing and/or
psychosocial aspects and can be coped using methods comparable to those used to physical
illness (i.e., avoidance, diagnosis, management and rehabilitation). Though the terms are
2
mental health can build a strong relationship with their loved ones and other people around
them. In my opinion mental health illnesses are not restricted to a particular country or state,
it has been affecting people from all around the world. I think people must take care of their
mental health and manage mental illnesses with the help health diet, exercise, social
interaction, and taking help from health professionals.
3. Some of the facts were just as I have expected, this is because mental health has become an
essential part of life in today’s scenarios. But there are some facts that really surprised me
including the number of young people affected with mental health issues. I knew that the
mental illnesses are mostly affect older people, It was surprising for me know that nearly 20
per cent of the young population including children are affected with this health condition.
One of the other facts that surprise me was the advantages of mental health in contribution
towards community services. I knew that positive mental health can help at individual level
and help people in developing healthy relationships, being able to cope with stressful
situation, but I was not aware about its role in community. But it can help the individual to
participate in activities and work in favour of the community; this can be only done of the
person is psychologically healthy (Knapp, McDaid and Parsonage, 2011).
4. Mental health is the state of healthiness in which the person realizes his or her personal
capabilities, how can manage the normal tensions of life, can work effectively and profitably
and is capable to make a support to his or her communal. Mental illness is the identified,
medically diagnosable disease that leads to the significant diminishing of a person’s cognitive,
affecting or relational capabilities. Mental ailments result from biological, developing and/or
psychosocial aspects and can be coped using methods comparable to those used to physical
illness (i.e., avoidance, diagnosis, management and rehabilitation). Though the terms are
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MHN
3
frequently applied interchangeably, psychological health and psychological illness is not the
similar thing; however they are likewise not equally exclusive. A important difference
between psychological health and psychological illness is that everybody has certain level of
psychological health every time, just like bodily health, while it is probable to be deprived of
mental disease (Rogers and Pilgrim, 2014).
5. Social risk factors associated with mental illness includes disorganized attachment with
parents or caregivers, low socio-economic status, exposure to violence, loss of significant
relationships. Negative thoughts about the past and present conditions might cause depression
and stress. Distorted ways of thinking or cognitive distortion may also cause mental illness.
Low self-efficacy is also associated with mental illness. Diseases, injuries and other type of
physical disorder commonly contribute to the poor mental wellbeing and occasionally mental
illness. When people are not happy, they often internalize their negative feeling or
unhappiness. This will later appears as the bad or difficult behaviors for example using
abusive words, becoming aggressive or violent and even damaging the property. Some of the
physical causes of mental illnesses include birth trauma, injuries to the brain, or drug abuse
are directly affect the chemistry of brain and cause mental illness. The poor bodily health can
impact the self-esteem and individual’s ability to encounter their life goals. These all factors
are associated with mental illnesses (Collins et al., 2011).
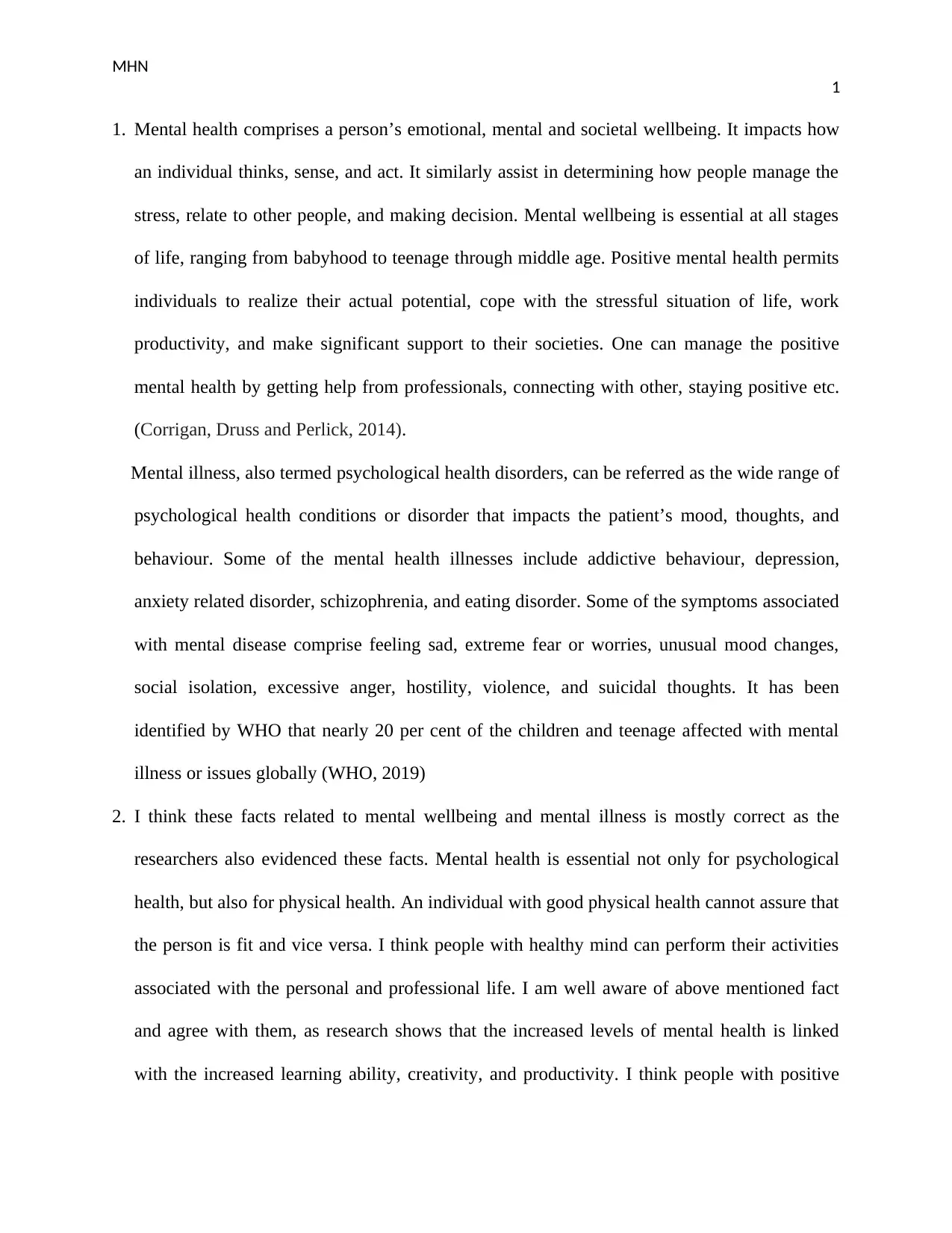
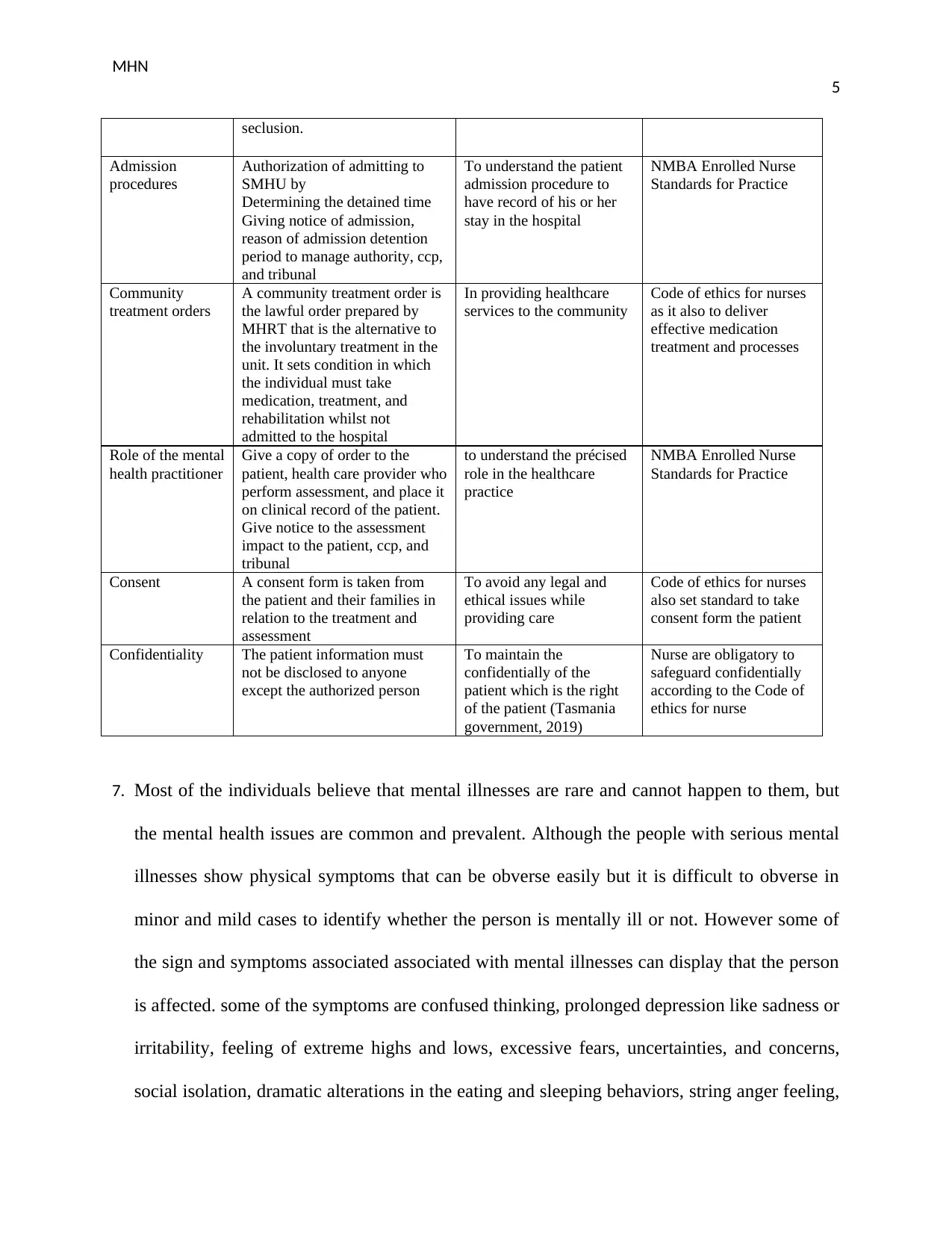
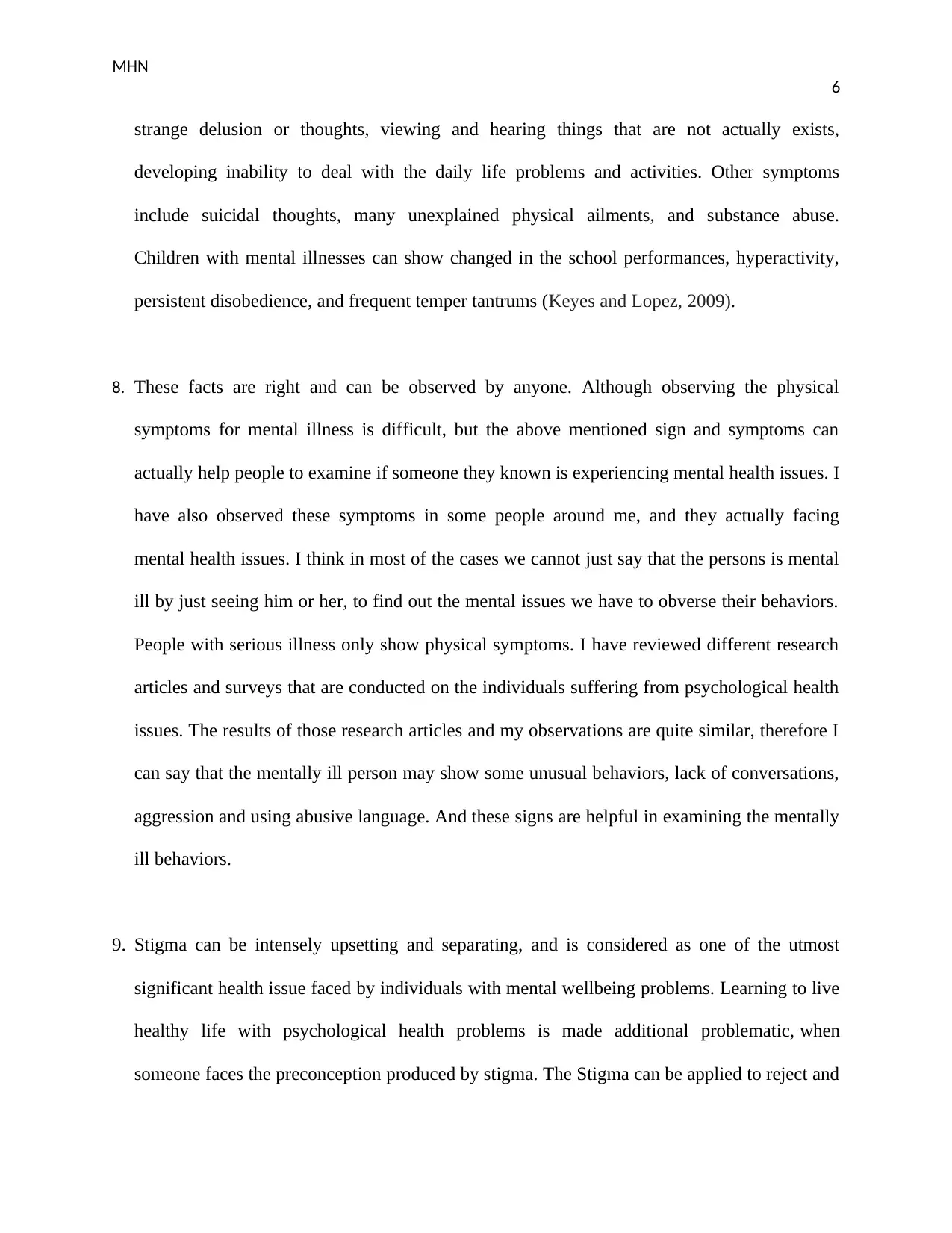
6.
Define and discuss How will you apply this to
your nursing practice?
Alignment to one of the
following: NMBA
Enrolled Nurse Standards
for Practice, Code of
Conduct for Nurses or
Code of ethics for nurses.
Objectives To deliver for the assessment
and treatment of mentally ill
patient
To provide proper oversight and
This can be applied to
provide the effective care
to the patient while
assessing for vital signs,
NMBA Enrolled Nurse
Standards for Practice as
they set similar objective
like mental health act
3
frequently applied interchangeably, psychological health and psychological illness is not the
similar thing; however they are likewise not equally exclusive. A important difference
between psychological health and psychological illness is that everybody has certain level of
psychological health every time, just like bodily health, while it is probable to be deprived of
mental disease (Rogers and Pilgrim, 2014).
5. Social risk factors associated with mental illness includes disorganized attachment with
parents or caregivers, low socio-economic status, exposure to violence, loss of significant
relationships. Negative thoughts about the past and present conditions might cause depression
and stress. Distorted ways of thinking or cognitive distortion may also cause mental illness.
Low self-efficacy is also associated with mental illness. Diseases, injuries and other type of
physical disorder commonly contribute to the poor mental wellbeing and occasionally mental
illness. When people are not happy, they often internalize their negative feeling or
unhappiness. This will later appears as the bad or difficult behaviors for example using
abusive words, becoming aggressive or violent and even damaging the property. Some of the
physical causes of mental illnesses include birth trauma, injuries to the brain, or drug abuse
are directly affect the chemistry of brain and cause mental illness. The poor bodily health can
impact the self-esteem and individual’s ability to encounter their life goals. These all factors
are associated with mental illnesses (Collins et al., 2011).
6.
Define and discuss How will you apply this to
your nursing practice?
Alignment to one of the
following: NMBA
Enrolled Nurse Standards
for Practice, Code of
Conduct for Nurses or
Code of ethics for nurses.
Objectives To deliver for the assessment
and treatment of mentally ill
patient
To provide proper oversight and
This can be applied to
provide the effective care
to the patient while
assessing for vital signs,
NMBA Enrolled Nurse
Standards for Practice as
they set similar objective
like mental health act
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MHN
4
safeguard about such assessment
and treatment
To deliver everyone clear
direction about their rights and
duties
To deliver least restrictive
setting by comparing all needs,
legal and juridical constraints,
safety of people
To promote voluntary
assessment and treatment over
involuntary
and treatment process
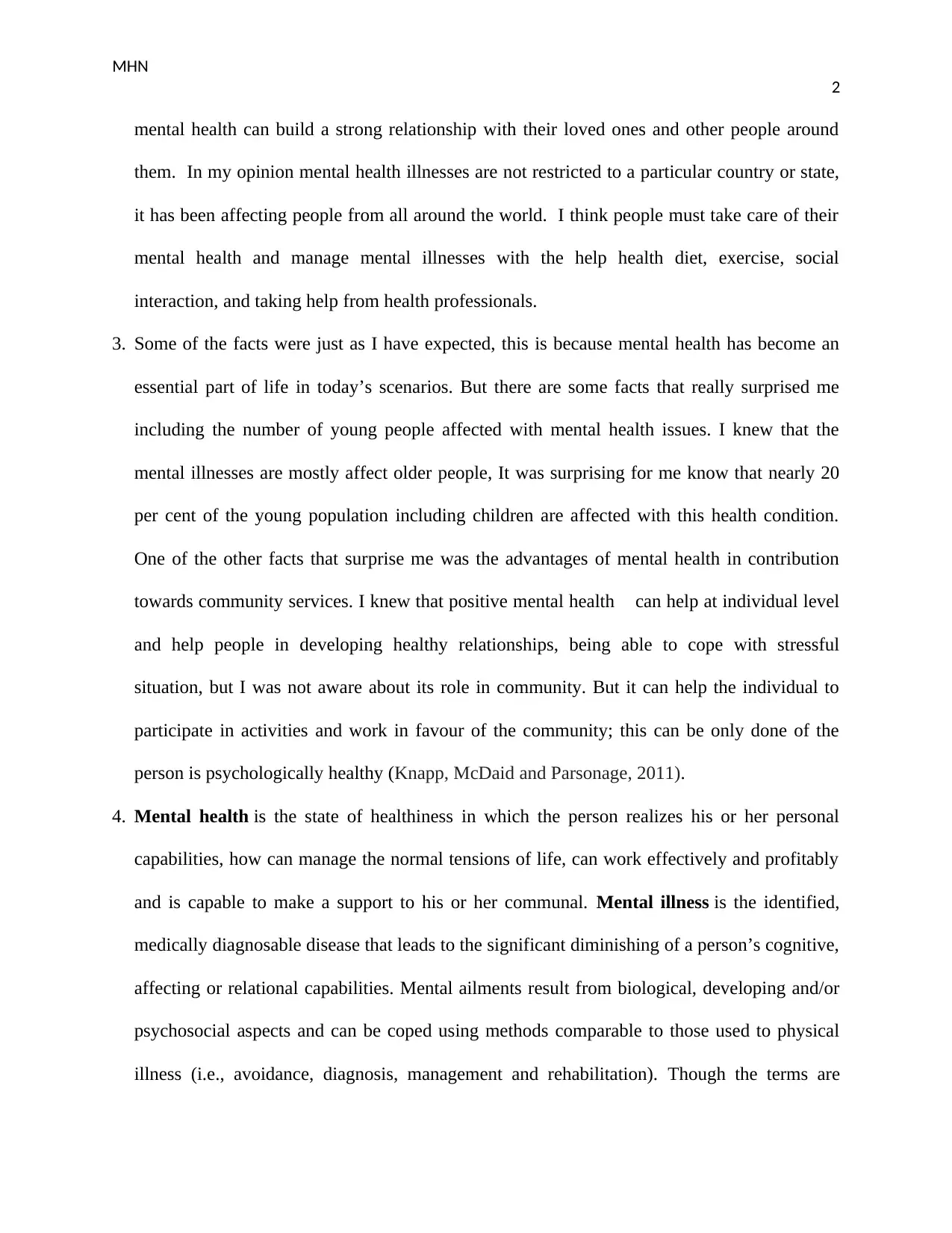
Involuntary
admission
An individual can be admitted to
the mental hospital
involuntarily, or without their
will. Mental health act sets the
criteria such as he or she must
be mentally ill, and should be no
other type of care like voluntary
admission
To involve the patient and
the decision making
process, ask the patient’s
permission
NMBA Enrolled Nurse
Standards for Practice as
it also have similar
requirements like
including patient in
decision making process
Consumer rights To have limitation on
interference with the dignity,
rights and freedom
Being involved indecision
making ability if capable
Receiving current information
To receive general health care
To wear their clothes
Propers assessment, treatment,
and care
To practice religion of their
choice
To avoid any legal and
ethical issues this can be
helpful
Code of Conduct for
Nurses as it also help the
nurse to follow patient’s
rights
Involuntary
review processes
The tribunal should review the
admission within three days
Must review the admission at
any other time period
Tribunal might affirm the
admission, but direct that it must
be shortened the patient be
relocated to the approved
hospital.
To help review every
checks so that the patient
must not be admitted to
the setting forcefully
NMBA Enrolled Nurse
Standards for Practice as
it set standard for
examine patient before
medication administration
Seclusion and
restraint
The tribunal might: review on its
personal motions at any time
Review on the application of
any individual with essential
standing
Review even if the time period
of seclusion and restraint has
completed
May affirm the use of restraint
and seclusion, and direct them to
be terminated, and declare the
patient must not possess
subjective to the constraint and
It will help in providing
patient cantered care to the
person with disease or
adverse condition
NMBA Enrolled Nurse
Standards for Practice
also set criteria for
providing patient cantered
approach
4
safeguard about such assessment
and treatment
To deliver everyone clear
direction about their rights and
duties
To deliver least restrictive
setting by comparing all needs,
legal and juridical constraints,
safety of people
To promote voluntary
assessment and treatment over
involuntary
and treatment process
Involuntary
admission
An individual can be admitted to
the mental hospital
involuntarily, or without their
will. Mental health act sets the
criteria such as he or she must
be mentally ill, and should be no
other type of care like voluntary
admission
To involve the patient and
the decision making
process, ask the patient’s
permission
NMBA Enrolled Nurse
Standards for Practice as
it also have similar
requirements like
including patient in
decision making process
Consumer rights To have limitation on
interference with the dignity,
rights and freedom
Being involved indecision
making ability if capable
Receiving current information
To receive general health care
To wear their clothes
Propers assessment, treatment,
and care
To practice religion of their
choice
To avoid any legal and
ethical issues this can be
helpful
Code of Conduct for
Nurses as it also help the
nurse to follow patient’s
rights
Involuntary
review processes
The tribunal should review the
admission within three days
Must review the admission at
any other time period
Tribunal might affirm the
admission, but direct that it must
be shortened the patient be
relocated to the approved
hospital.
To help review every
checks so that the patient
must not be admitted to
the setting forcefully
NMBA Enrolled Nurse
Standards for Practice as
it set standard for
examine patient before
medication administration
Seclusion and
restraint
The tribunal might: review on its
personal motions at any time
Review on the application of
any individual with essential
standing
Review even if the time period
of seclusion and restraint has
completed
May affirm the use of restraint
and seclusion, and direct them to
be terminated, and declare the
patient must not possess
subjective to the constraint and
It will help in providing
patient cantered care to the
person with disease or
adverse condition
NMBA Enrolled Nurse
Standards for Practice
also set criteria for
providing patient cantered
approach
MHN
5
seclusion.
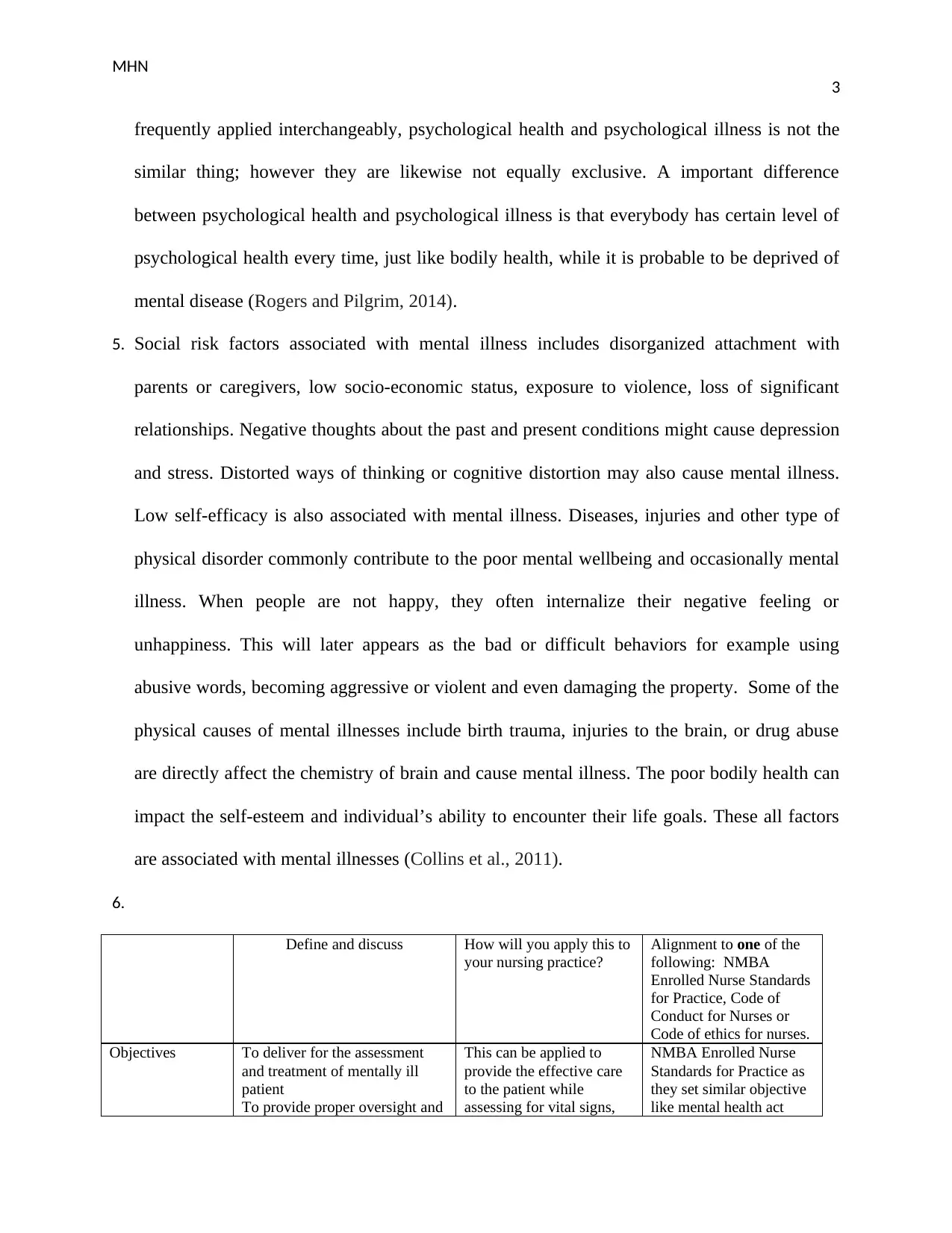
Admission
procedures
Authorization of admitting to
SMHU by
Determining the detained time
Giving notice of admission,
reason of admission detention
period to manage authority, ccp,
and tribunal
To understand the patient
admission procedure to
have record of his or her
stay in the hospital
NMBA Enrolled Nurse
Standards for Practice
Community
treatment orders
A community treatment order is
the lawful order prepared by
MHRT that is the alternative to
the involuntary treatment in the
unit. It sets condition in which
the individual must take
medication, treatment, and
rehabilitation whilst not
admitted to the hospital
In providing healthcare
services to the community
Code of ethics for nurses
as it also to deliver
effective medication
treatment and processes
Role of the mental
health practitioner
Give a copy of order to the
patient, health care provider who
perform assessment, and place it
on clinical record of the patient.
Give notice to the assessment
impact to the patient, ccp, and
tribunal
to understand the précised
role in the healthcare
practice
NMBA Enrolled Nurse
Standards for Practice
Consent A consent form is taken from
the patient and their families in
relation to the treatment and
assessment
To avoid any legal and
ethical issues while
providing care
Code of ethics for nurses
also set standard to take
consent form the patient
Confidentiality The patient information must
not be disclosed to anyone
except the authorized person
To maintain the
confidentially of the
patient which is the right
of the patient (Tasmania
government, 2019)
Nurse are obligatory to
safeguard confidentially
according to the Code of
ethics for nurse
7. Most of the individuals believe that mental illnesses are rare and cannot happen to them, but
the mental health issues are common and prevalent. Although the people with serious mental
illnesses show physical symptoms that can be obverse easily but it is difficult to obverse in
minor and mild cases to identify whether the person is mentally ill or not. However some of
the sign and symptoms associated associated with mental illnesses can display that the person
is affected. some of the symptoms are confused thinking, prolonged depression like sadness or
irritability, feeling of extreme highs and lows, excessive fears, uncertainties, and concerns,
social isolation, dramatic alterations in the eating and sleeping behaviors, string anger feeling,
5
seclusion.
Admission
procedures
Authorization of admitting to
SMHU by
Determining the detained time
Giving notice of admission,
reason of admission detention
period to manage authority, ccp,
and tribunal
To understand the patient
admission procedure to
have record of his or her
stay in the hospital
NMBA Enrolled Nurse
Standards for Practice
Community
treatment orders
A community treatment order is
the lawful order prepared by
MHRT that is the alternative to
the involuntary treatment in the
unit. It sets condition in which
the individual must take
medication, treatment, and
rehabilitation whilst not
admitted to the hospital
In providing healthcare
services to the community
Code of ethics for nurses
as it also to deliver
effective medication
treatment and processes
Role of the mental
health practitioner
Give a copy of order to the
patient, health care provider who
perform assessment, and place it
on clinical record of the patient.
Give notice to the assessment
impact to the patient, ccp, and
tribunal
to understand the précised
role in the healthcare
practice
NMBA Enrolled Nurse
Standards for Practice
Consent A consent form is taken from
the patient and their families in
relation to the treatment and
assessment
To avoid any legal and
ethical issues while
providing care
Code of ethics for nurses
also set standard to take
consent form the patient
Confidentiality The patient information must
not be disclosed to anyone
except the authorized person
To maintain the
confidentially of the
patient which is the right
of the patient (Tasmania
government, 2019)
Nurse are obligatory to
safeguard confidentially
according to the Code of
ethics for nurse
7. Most of the individuals believe that mental illnesses are rare and cannot happen to them, but
the mental health issues are common and prevalent. Although the people with serious mental
illnesses show physical symptoms that can be obverse easily but it is difficult to obverse in
minor and mild cases to identify whether the person is mentally ill or not. However some of
the sign and symptoms associated associated with mental illnesses can display that the person
is affected. some of the symptoms are confused thinking, prolonged depression like sadness or
irritability, feeling of extreme highs and lows, excessive fears, uncertainties, and concerns,
social isolation, dramatic alterations in the eating and sleeping behaviors, string anger feeling,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MHN
6
strange delusion or thoughts, viewing and hearing things that are not actually exists,
developing inability to deal with the daily life problems and activities. Other symptoms
include suicidal thoughts, many unexplained physical ailments, and substance abuse.
Children with mental illnesses can show changed in the school performances, hyperactivity,
persistent disobedience, and frequent temper tantrums (Keyes and Lopez, 2009).
8. These facts are right and can be observed by anyone. Although observing the physical
symptoms for mental illness is difficult, but the above mentioned sign and symptoms can
actually help people to examine if someone they known is experiencing mental health issues. I
have also observed these symptoms in some people around me, and they actually facing
mental health issues. I think in most of the cases we cannot just say that the persons is mental
ill by just seeing him or her, to find out the mental issues we have to obverse their behaviors.
People with serious illness only show physical symptoms. I have reviewed different research
articles and surveys that are conducted on the individuals suffering from psychological health
issues. The results of those research articles and my observations are quite similar, therefore I
can say that the mentally ill person may show some unusual behaviors, lack of conversations,
aggression and using abusive language. And these signs are helpful in examining the mentally
ill behaviors.
9. Stigma can be intensely upsetting and separating, and is considered as one of the utmost
significant health issue faced by individuals with mental wellbeing problems. Learning to live
healthy life with psychological health problems is made additional problematic, when
someone faces the preconception produced by stigma. The Stigma can be applied to reject and
6
strange delusion or thoughts, viewing and hearing things that are not actually exists,
developing inability to deal with the daily life problems and activities. Other symptoms
include suicidal thoughts, many unexplained physical ailments, and substance abuse.
Children with mental illnesses can show changed in the school performances, hyperactivity,
persistent disobedience, and frequent temper tantrums (Keyes and Lopez, 2009).
8. These facts are right and can be observed by anyone. Although observing the physical
symptoms for mental illness is difficult, but the above mentioned sign and symptoms can
actually help people to examine if someone they known is experiencing mental health issues. I
have also observed these symptoms in some people around me, and they actually facing
mental health issues. I think in most of the cases we cannot just say that the persons is mental
ill by just seeing him or her, to find out the mental issues we have to obverse their behaviors.
People with serious illness only show physical symptoms. I have reviewed different research
articles and surveys that are conducted on the individuals suffering from psychological health
issues. The results of those research articles and my observations are quite similar, therefore I
can say that the mentally ill person may show some unusual behaviors, lack of conversations,
aggression and using abusive language. And these signs are helpful in examining the mentally
ill behaviors.
9. Stigma can be intensely upsetting and separating, and is considered as one of the utmost
significant health issue faced by individuals with mental wellbeing problems. Learning to live
healthy life with psychological health problems is made additional problematic, when
someone faces the preconception produced by stigma. The Stigma can be applied to reject and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MHN
7
marginalize persons. The preconception and anxiety produced by stigma might even inhibit
people from coming frontward and looking for the help they require. Stigma can similarly
stop individuals proposing help or being helpful. Stigma frequently constrains individuals
from receiving the jobs they are capable to do and it can stop individuals with psychological
health issues from playing a lively role in their society. It reduces self-esteem and deprives
persons of societal opportunities”. This can comprise being deprived of opportunities for
example employment or housing due to their disorder. Stigma can also be a barricade to
pursuing early management, cause deterioration and delay recovery. Stigma similarly costs
the state economically. If individuals are too embarrassed or concerned to talk, they might not
come frontward to pursue help. That postponement can source even more suffering
(Henderson, Evans-Lacko and Thornicroft, 2013).
10. Stigma is when people sees someone in a negative manner due to a specific characteristic
or quality for example skin color, cultural contextual, an incapacity or a psychological
illness). When people treat someone in a negative manner on account of the psychological
illness, this is called discrimination. The Stigma related problems happens when an individual
describes someone according to their disease instead of who they actually are as the
individual. For instance, they may be labeling someone as psychotic instead of ‘a person
suffering psychoses (Abbey et al., 2011). For persons with mental wellbeing issues, the
societal stigma and negative perception they face can make their issues poorer, making it
more difficult to recover. It might cause the individual to evade receiving the assistance they
require due to the distress of being stigmatized. The person with stigma starts being
discriminated when other people compare themselves with them and how they are different
7
marginalize persons. The preconception and anxiety produced by stigma might even inhibit
people from coming frontward and looking for the help they require. Stigma can similarly
stop individuals proposing help or being helpful. Stigma frequently constrains individuals
from receiving the jobs they are capable to do and it can stop individuals with psychological
health issues from playing a lively role in their society. It reduces self-esteem and deprives
persons of societal opportunities”. This can comprise being deprived of opportunities for
example employment or housing due to their disorder. Stigma can also be a barricade to
pursuing early management, cause deterioration and delay recovery. Stigma similarly costs
the state economically. If individuals are too embarrassed or concerned to talk, they might not
come frontward to pursue help. That postponement can source even more suffering
(Henderson, Evans-Lacko and Thornicroft, 2013).
10. Stigma is when people sees someone in a negative manner due to a specific characteristic
or quality for example skin color, cultural contextual, an incapacity or a psychological
illness). When people treat someone in a negative manner on account of the psychological
illness, this is called discrimination. The Stigma related problems happens when an individual
describes someone according to their disease instead of who they actually are as the
individual. For instance, they may be labeling someone as psychotic instead of ‘a person
suffering psychoses (Abbey et al., 2011). For persons with mental wellbeing issues, the
societal stigma and negative perception they face can make their issues poorer, making it
more difficult to recover. It might cause the individual to evade receiving the assistance they
require due to the distress of being stigmatized. The person with stigma starts being
discriminated when other people compare themselves with them and how they are different
MHN
8
from the affected person, rather seeing it as the health issues. Stigma and discrimination might
trap individuals in a series of mental illness (Parker, 2012).
11. The lives of individuals with psychological health illnesses are frequently overwhelmed
by stigma in addition to discrimination. Stigma is actually the negative stereotype. Certain of
the sign of stigma that can result in discrimination comprise social isolation, poor housing, job
loss, and poverty. Persons with a psychological illness are challenged with manifold,
interconnecting coatings of discrimination due to their mental disease and their individuality.
For instance, a female with a psychological illness might face discrimination because of
sexism in addition to her disease, and the racialized individual might practice discrimination
because of racism as well as their mental disease. Furthermore, experiencing discrimination
can negatively influence the mental health. It disturbs individual’s self-esteem, contributes in
disrupting their family relations and bounds their capability to meet people and acquire
accommodation and occupations. It hinders the deterrence of mental wellbeing disorders, the
elevation of psychological health and the delivery of operational management and care. It
furthermore subsidises to the abuse of hominoid rights (Abbey et al., 2011).
12. As the health care professional it is my duty to provide my services to all patients’
equality in the health care setting and community. For the successful delivery of health care
services, stigma should be removed. Nurses are in a distinctive situation to create a positive
influence on the community and can apply their situation of trust to assist the community
identify the role and chance for backing to end stigma. All the Nurses can apply the stop
criteria to identify the attitudes and actions that favour the stigma of psychological health
situation to identify stigma and discrimination includes stereotyping in the healthcare setting,
trivializes people with psychological issues, someone offending mentally ill people, and
8
from the affected person, rather seeing it as the health issues. Stigma and discrimination might
trap individuals in a series of mental illness (Parker, 2012).
11. The lives of individuals with psychological health illnesses are frequently overwhelmed
by stigma in addition to discrimination. Stigma is actually the negative stereotype. Certain of
the sign of stigma that can result in discrimination comprise social isolation, poor housing, job
loss, and poverty. Persons with a psychological illness are challenged with manifold,
interconnecting coatings of discrimination due to their mental disease and their individuality.
For instance, a female with a psychological illness might face discrimination because of
sexism in addition to her disease, and the racialized individual might practice discrimination
because of racism as well as their mental disease. Furthermore, experiencing discrimination
can negatively influence the mental health. It disturbs individual’s self-esteem, contributes in
disrupting their family relations and bounds their capability to meet people and acquire
accommodation and occupations. It hinders the deterrence of mental wellbeing disorders, the
elevation of psychological health and the delivery of operational management and care. It
furthermore subsidises to the abuse of hominoid rights (Abbey et al., 2011).
12. As the health care professional it is my duty to provide my services to all patients’
equality in the health care setting and community. For the successful delivery of health care
services, stigma should be removed. Nurses are in a distinctive situation to create a positive
influence on the community and can apply their situation of trust to assist the community
identify the role and chance for backing to end stigma. All the Nurses can apply the stop
criteria to identify the attitudes and actions that favour the stigma of psychological health
situation to identify stigma and discrimination includes stereotyping in the healthcare setting,
trivializes people with psychological issues, someone offending mentally ill people, and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MHN
9
patronizes persons with mental wellbeing issues. Nurses should treat individuals who have
psychological health issues with self-possession and respect. Developing a therapeutic
communication with the patient and their families can help in building good interaction.
When meeting someone who actually wishes to discuss about their psychological illness or
indications it is significant for nurses to: be available, hear and be non-judgmental, select the
correct time and location to approach the problem, recognize what the individual is sharing
and must not brush it off. Nurses must also give them any information they have on
obtainable resources or provision (Ross and Goldner, 2009).
13. People with psychological health issues feel uncomfortable and embarrassing to be
diagnosed and get treatment of the mental health issues. Most of the people in the community
do not accept that they have mental wellbeing issues like stress and depression, and these
results in delayed treatment. In different under developing countries the perception of people
about the mental illness is negative, they see psychologically ill people as a different
personality and think that they cannot be treated. This discourages the person to receive
treatment and talk about their problems to anyone. Culture effects many features of mental
disease, counting how patients belong to a culture display and evident their indications, their
coping styles, their relative and community provisions, and their readiness to pursue
treatment. Cultural and societal impacts are not the lone causes of psychological illness and
forms of service application for ethnic and cultural subgroups; however they actually play
significant roles. The cultures of racial and ethnic subgroups change the kinds of
psychological health facilities they use. Cultural mistakes or communication difficulties
between patients and healthcare providers may stop minorities from using facilities and
getting appropriate upkeep (Abdullah and Brown, 2011).
9
patronizes persons with mental wellbeing issues. Nurses should treat individuals who have
psychological health issues with self-possession and respect. Developing a therapeutic
communication with the patient and their families can help in building good interaction.
When meeting someone who actually wishes to discuss about their psychological illness or
indications it is significant for nurses to: be available, hear and be non-judgmental, select the
correct time and location to approach the problem, recognize what the individual is sharing
and must not brush it off. Nurses must also give them any information they have on
obtainable resources or provision (Ross and Goldner, 2009).
13. People with psychological health issues feel uncomfortable and embarrassing to be
diagnosed and get treatment of the mental health issues. Most of the people in the community
do not accept that they have mental wellbeing issues like stress and depression, and these
results in delayed treatment. In different under developing countries the perception of people
about the mental illness is negative, they see psychologically ill people as a different
personality and think that they cannot be treated. This discourages the person to receive
treatment and talk about their problems to anyone. Culture effects many features of mental
disease, counting how patients belong to a culture display and evident their indications, their
coping styles, their relative and community provisions, and their readiness to pursue
treatment. Cultural and societal impacts are not the lone causes of psychological illness and
forms of service application for ethnic and cultural subgroups; however they actually play
significant roles. The cultures of racial and ethnic subgroups change the kinds of
psychological health facilities they use. Cultural mistakes or communication difficulties
between patients and healthcare providers may stop minorities from using facilities and
getting appropriate upkeep (Abdullah and Brown, 2011).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MHN
10
14. Anxiety is the body’s usual reaction to stress. It is actually a feeling of distress or worry
about what will happen next. For example the first day of college, going to an employment
interview, or giving presentation in front of the crowd might cause most individuals to sense
terrible and nervous. However if the anxiety associated feelings are extreme, extended for
lengthier than half year, and are meddling with person’s life, they might have the anxiety
disorder. Anxiety illnesses can occur at any phase of life, however they frequently begin at the
middle age (Spielberger, 2013). Females are additional probable to have these issues than
men. Social anxiety disorder inhibits the person from living their life easily. They frequently avoid
circumstances that maximum individuals deliberate “normal. They might even experience hard time
accepting how other people can manage them so effortlessly. When they evade all or maximum
social conditions, it affects their personal associations. It can similarly results in: reduced self-
esteem, Negative feelings, Depression, Compassion to criticism, and low social skills that do not
improve with time (Deb, Strodl and Sun, 2015).
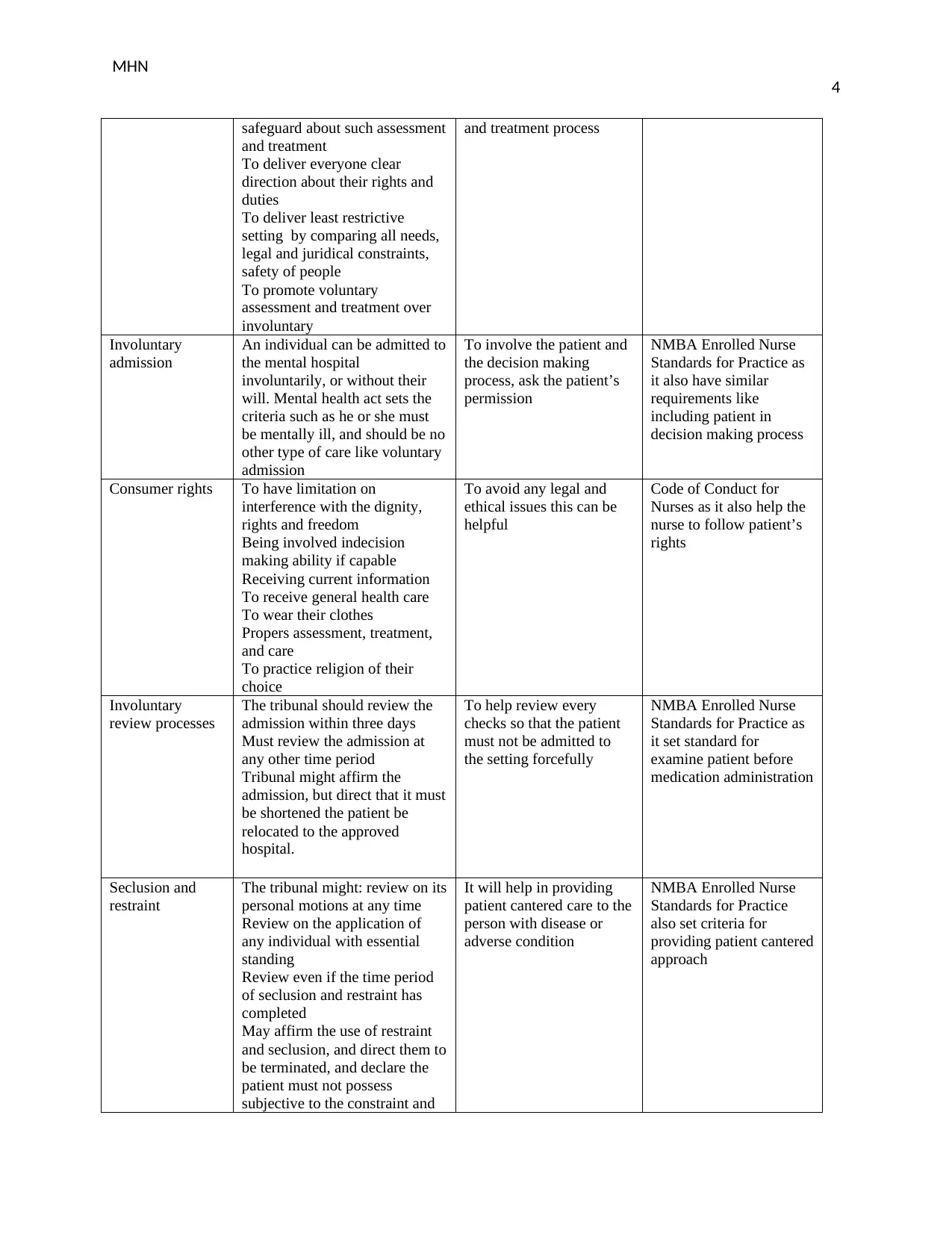
15.
Definition Signs and Symptoms Care requirements Treatments
Generalise
d
Anxiet
y
Disord
er
GAD is
noticeable by
extreme anxiety
for no coherent
reason..
Overthinking strategies and
solutions to all conceivable
worst-case consequences
Observing situations and
proceedings as intimidating,
even when they are not
Trouble handling improbability
Indecisiveness and fear of making
the wrong decision
Keep physically
active
Make sleep a
priority.
Eat healthy
Socialize
Showing empathy
Showing respect
Effective
communication
Medicine:
Antidepressants,
Buspirone,
Benzodiazepines
Psychotherapy or talk
therapy (Steudte et
al., 2011)
Obsessive
compu
lsive
disord
Obsessive-
Compulsive
Disorder
(OCD) is a
fear of microorganisms or getting
dirty
ensures a supportive
environment
Reducing anxiety
Lessening or
Antidepressants,
clomipramine,
fluoxetine fluvoxamine,
paroxetine, and
10
14. Anxiety is the body’s usual reaction to stress. It is actually a feeling of distress or worry
about what will happen next. For example the first day of college, going to an employment
interview, or giving presentation in front of the crowd might cause most individuals to sense
terrible and nervous. However if the anxiety associated feelings are extreme, extended for
lengthier than half year, and are meddling with person’s life, they might have the anxiety
disorder. Anxiety illnesses can occur at any phase of life, however they frequently begin at the
middle age (Spielberger, 2013). Females are additional probable to have these issues than
men. Social anxiety disorder inhibits the person from living their life easily. They frequently avoid
circumstances that maximum individuals deliberate “normal. They might even experience hard time
accepting how other people can manage them so effortlessly. When they evade all or maximum
social conditions, it affects their personal associations. It can similarly results in: reduced self-
esteem, Negative feelings, Depression, Compassion to criticism, and low social skills that do not
improve with time (Deb, Strodl and Sun, 2015).
15.
Definition Signs and Symptoms Care requirements Treatments
Generalise
d
Anxiet
y
Disord
er
GAD is
noticeable by
extreme anxiety
for no coherent
reason..
Overthinking strategies and
solutions to all conceivable
worst-case consequences
Observing situations and
proceedings as intimidating,
even when they are not
Trouble handling improbability
Indecisiveness and fear of making
the wrong decision
Keep physically
active
Make sleep a
priority.
Eat healthy
Socialize
Showing empathy
Showing respect
Effective
communication
Medicine:
Antidepressants,
Buspirone,
Benzodiazepines
Psychotherapy or talk
therapy (Steudte et
al., 2011)
Obsessive
compu
lsive
disord
Obsessive-
Compulsive
Disorder
(OCD) is a
fear of microorganisms or getting
dirty
ensures a supportive
environment
Reducing anxiety
Lessening or
Antidepressants,
clomipramine,
fluoxetine fluvoxamine,
paroxetine, and
MHN
11
er mutual,
chronic and
continuing
illness in
which a
individual
has
irrepressible
, reoccurring
thoughts
(obsessions)
and actions
(compulsion
s) that he or
she senses
the urge to
recurrence
over and
over.
Worries about getting injured or
others being hurt
Requirement for things to be
retained in an exact order
Belief that definite numbers or
shades are “good” or “bad”
eliminating
negative
thoughts
Decreasing
obsessions and
compulsions
sertraline
(Abramowitz, Taylor
and McKay, 2009).
Panic
Disord
er
Panic disorder
is an anxiety
complaint
where you
frequently have
unexpected
attacks of panic
or fear.
Sense of imminent doom or
danger
Anxiety of loss of control or death
Rapid, pounding heart rate
Sweating
Trembling or shaking
Develop a
association with the
person grounded on
empathy and trust.
Endorse an
understanding of
the types of an
anxiety illness.
Promote operational
approaches for
managing anxiety.
Support positive
health behaviours,
comprising
medication
obedience (if
appropriate) and
healthy routine
choices (for
instance, diet,
exercise, not
smoking).
SSRIs
SNRIs
Benzodiazepines
Post-
Traum
atic
Stress
Disord
er
Post-traumatic
stress disorder
(PTSD) is the
illness that
progresses in
some
individuals
who have
experienced a
appalling,
scary, or
hazardous
event
Intrusive thoughts
Evading reminders
Negative opinions and feelings
Arousal and sensitive symptoms
Education about
how to cope
Finding ways to
manage emotions
Managing sleep
issues
Management of
flashback and
dissociation
Fluoxetine (Prozac)
Paroxetine (Paxil)
Sertraline (Zoloft)
Venlafaxine (Effexor)
Social social anxiety Blushing Asking them to Cognitive behavioural
11
er mutual,
chronic and
continuing
illness in
which a
individual
has
irrepressible
, reoccurring
thoughts
(obsessions)
and actions
(compulsion
s) that he or
she senses
the urge to
recurrence
over and
over.
Worries about getting injured or
others being hurt
Requirement for things to be
retained in an exact order
Belief that definite numbers or
shades are “good” or “bad”
eliminating
negative
thoughts
Decreasing
obsessions and
compulsions
sertraline
(Abramowitz, Taylor
and McKay, 2009).
Panic
Disord
er
Panic disorder
is an anxiety
complaint
where you
frequently have
unexpected
attacks of panic
or fear.
Sense of imminent doom or
danger
Anxiety of loss of control or death
Rapid, pounding heart rate
Sweating
Trembling or shaking
Develop a
association with the
person grounded on
empathy and trust.
Endorse an
understanding of
the types of an
anxiety illness.
Promote operational
approaches for
managing anxiety.
Support positive
health behaviours,
comprising
medication
obedience (if
appropriate) and
healthy routine
choices (for
instance, diet,
exercise, not
smoking).
SSRIs
SNRIs
Benzodiazepines
Post-
Traum
atic
Stress
Disord
er
Post-traumatic
stress disorder
(PTSD) is the
illness that
progresses in
some
individuals
who have
experienced a
appalling,
scary, or
hazardous
event
Intrusive thoughts
Evading reminders
Negative opinions and feelings
Arousal and sensitive symptoms
Education about
how to cope
Finding ways to
manage emotions
Managing sleep
issues
Management of
flashback and
dissociation
Fluoxetine (Prozac)
Paroxetine (Paxil)
Sertraline (Zoloft)
Venlafaxine (Effexor)
Social social anxiety Blushing Asking them to Cognitive behavioural
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 44
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





