University Assignment: Human Skeleton and Muscle System Analysis
VerifiedAdded on 2020/03/01
|7
|1865
|202
Homework Assignment
AI Summary
This assignment provides a comprehensive overview of the human musculoskeletal system, encompassing the skeletal and muscular systems. It begins with an introduction to the skeletal system, detailing the functions of bones, bone tissue types, and bone anatomy, including the periosteum and compact bone. The assignment then explores different types of joints, such as hinge, pivot, saddle, fixed, and ellipsoidal joints, and their respective ranges of motion. The role of muscles and joints in complex movements like running and activities such as working on a computer are analyzed. The document further delves into the anatomy of skeletal muscles, including their structure, the roles of epimysium, fasciculi, and muscle fibers, and the sliding filament theory of muscle contraction. Finally, the assignment discusses various types of muscle contraction (isometric, isotonic, concentric, and eccentric) and the roles of agonists, antagonists, and synergists in muscle function. The document is well-referenced with multiple sources cited.

Anatomy and Physiology of Human Skeleton and Muscles
Name of the Student:
Name of the University:
Author’s Note:
Name of the Student:
Name of the University:
Author’s Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TAQ 1:
The Musculoskeletal System of the human body comprise of the bones (Skeletal
System), the muscles (Muscular system) and several other connective tissues such as tendons,
ligaments, cartilages and joints, which work in a coordinated manner to achieve the functions
of the whole system. The system is primarily concerned with support stability and movement
of the body. There are 206 bones in an adult body which provides support for the entire body,
stored minerals and lipids, produces blood cells, protects the internal organs and provides
leverage and movement (Neumann 2013). The three primary functions of the bones and the
skeletal system as a whole are protection of organs of the body, production of blood cells and
calcium homeostasis.
Two types of bone tissues are found in human body that consists of three different
kinds of cells namely osteoblasts, osteoclasts and osteocytes. Osteoblasts are the bone-
forming cells, osteoclasts are cells that break down and resorb bones and osteocytes are
mature bone cells. The anatomy of the cross section of bone comprises of a thin layer of
dense connective tissue layer called Periosteum. The Periosteum is further divided into a
fibrous outer layer consisting of the fibroblasts and an inner cambium consisting of
osteoblasts progenitor cells. This layer provides blood supply to the different bone cells and
is the site of muscular attachment. Under the Periosteum is the compact bone made of closely
packed harvesian systems. This solid section provides strength to the bones. The inside of the
bone is a spongy, lightweight and porous containing the bone marrow.
Further, bones are the calcium storage organ of the body. When calcium levels in the
blood decrease, bones release calcium and calcium is stored when excess calcium
accumulates in blood (Murshed and McKee 2010). The other major function of bones is
The Musculoskeletal System of the human body comprise of the bones (Skeletal
System), the muscles (Muscular system) and several other connective tissues such as tendons,
ligaments, cartilages and joints, which work in a coordinated manner to achieve the functions
of the whole system. The system is primarily concerned with support stability and movement
of the body. There are 206 bones in an adult body which provides support for the entire body,
stored minerals and lipids, produces blood cells, protects the internal organs and provides
leverage and movement (Neumann 2013). The three primary functions of the bones and the
skeletal system as a whole are protection of organs of the body, production of blood cells and
calcium homeostasis.
Two types of bone tissues are found in human body that consists of three different
kinds of cells namely osteoblasts, osteoclasts and osteocytes. Osteoblasts are the bone-
forming cells, osteoclasts are cells that break down and resorb bones and osteocytes are
mature bone cells. The anatomy of the cross section of bone comprises of a thin layer of
dense connective tissue layer called Periosteum. The Periosteum is further divided into a
fibrous outer layer consisting of the fibroblasts and an inner cambium consisting of
osteoblasts progenitor cells. This layer provides blood supply to the different bone cells and
is the site of muscular attachment. Under the Periosteum is the compact bone made of closely
packed harvesian systems. This solid section provides strength to the bones. The inside of the
bone is a spongy, lightweight and porous containing the bone marrow.
Further, bones are the calcium storage organ of the body. When calcium levels in the
blood decrease, bones release calcium and calcium is stored when excess calcium
accumulates in blood (Murshed and McKee 2010). The other major function of bones is
production of three kinds of blood cells, leucocytes, erythrocytes and platelets from
hematopoietic stem cells present within the bone marrow.
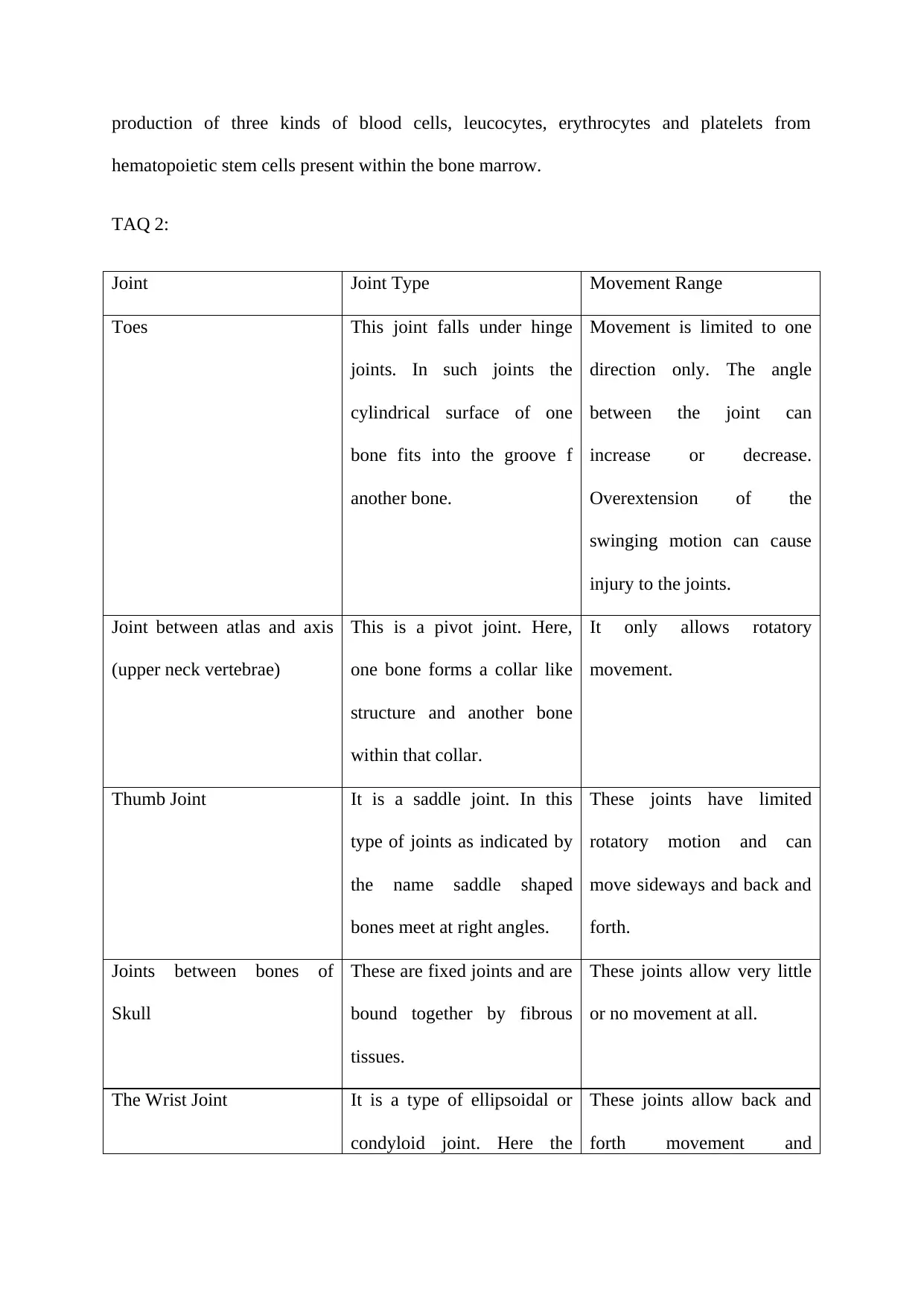
TAQ 2:
Joint Joint Type Movement Range
Toes This joint falls under hinge
joints. In such joints the
cylindrical surface of one
bone fits into the groove f
another bone.
Movement is limited to one
direction only. The angle
between the joint can
increase or decrease.
Overextension of the
swinging motion can cause
injury to the joints.
Joint between atlas and axis
(upper neck vertebrae)
This is a pivot joint. Here,
one bone forms a collar like
structure and another bone
within that collar.
It only allows rotatory
movement.
Thumb Joint It is a saddle joint. In this
type of joints as indicated by
the name saddle shaped
bones meet at right angles.
These joints have limited
rotatory motion and can
move sideways and back and
forth.
Joints between bones of
Skull
These are fixed joints and are
bound together by fibrous
tissues.
These joints allow very little
or no movement at all.
The Wrist Joint It is a type of ellipsoidal or
condyloid joint. Here the
These joints allow back and
forth movement and
hematopoietic stem cells present within the bone marrow.
TAQ 2:
Joint Joint Type Movement Range
Toes This joint falls under hinge
joints. In such joints the
cylindrical surface of one
bone fits into the groove f
another bone.
Movement is limited to one
direction only. The angle
between the joint can
increase or decrease.
Overextension of the
swinging motion can cause
injury to the joints.
Joint between atlas and axis
(upper neck vertebrae)
This is a pivot joint. Here,
one bone forms a collar like
structure and another bone
within that collar.
It only allows rotatory
movement.
Thumb Joint It is a saddle joint. In this
type of joints as indicated by
the name saddle shaped
bones meet at right angles.
These joints have limited
rotatory motion and can
move sideways and back and
forth.
Joints between bones of
Skull
These are fixed joints and are
bound together by fibrous
tissues.
These joints allow very little
or no movement at all.
The Wrist Joint It is a type of ellipsoidal or
condyloid joint. Here the
These joints allow back and
forth movement and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
oval end of one bone fits into
a cup shaped structure of
another giving the joint an
ellipsoid shape.
sideways movement. The
rotational movement of such
joints are limited (Reese and
Bandy 2016).
TAQ 3:
Running is a complex process, which involves the combined action of different
muscles and joints of the body. Although the lower part of the body is mostly involved in
running movement, the torso, arm and core body muscles also play important role when a
person is running. The major muscles involved in the process of running are the Quadriceps
Femoris, hamstrings, Gluteus Maximus, hip flexors, calf muscles and the core abdominal
muscles. The joints involved are hip, knee and ankle joints (Higashihara, Ono, Kubota,
Okuwaki and Fukubayashi 2010). The quadriceps group of muscles which include rectus
femoris, vastus medialis, vastus lateralis and vastus intermedialis, located at the front of the
thighs are mainly responsible for flexion of the hip joint and extension of the knee joint. The
hamstring muscles, (biceps femoris, semimembranosus and semitendinosus) located at the
back of the thighs, help straighten the hips and bend and flex the knees. The gluteus
maximus, the largest and most superficial hip muscle help to maintain erect posture by
extending the hips (Bartlett, Sumner, Ellis and Kram 2014). The calf muscle, which include
the gastrocnemius and soleus help in plantar flexion of the ankle. Finally the abdominal
muscles support the torso and stabilize the pelvis while running by isometric contraction of
the upper body muscles.
Working on a computer in an office would involve maintaining a sitting posture on a
chair, typing on a keyboard and movement of the neck. To maintain a sitting posture activity
a cup shaped structure of
another giving the joint an
ellipsoid shape.
sideways movement. The
rotational movement of such
joints are limited (Reese and
Bandy 2016).
TAQ 3:
Running is a complex process, which involves the combined action of different
muscles and joints of the body. Although the lower part of the body is mostly involved in
running movement, the torso, arm and core body muscles also play important role when a
person is running. The major muscles involved in the process of running are the Quadriceps
Femoris, hamstrings, Gluteus Maximus, hip flexors, calf muscles and the core abdominal
muscles. The joints involved are hip, knee and ankle joints (Higashihara, Ono, Kubota,
Okuwaki and Fukubayashi 2010). The quadriceps group of muscles which include rectus
femoris, vastus medialis, vastus lateralis and vastus intermedialis, located at the front of the
thighs are mainly responsible for flexion of the hip joint and extension of the knee joint. The
hamstring muscles, (biceps femoris, semimembranosus and semitendinosus) located at the
back of the thighs, help straighten the hips and bend and flex the knees. The gluteus
maximus, the largest and most superficial hip muscle help to maintain erect posture by
extending the hips (Bartlett, Sumner, Ellis and Kram 2014). The calf muscle, which include
the gastrocnemius and soleus help in plantar flexion of the ankle. Finally the abdominal
muscles support the torso and stabilize the pelvis while running by isometric contraction of
the upper body muscles.
Working on a computer in an office would involve maintaining a sitting posture on a
chair, typing on a keyboard and movement of the neck. To maintain a sitting posture activity
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
of different skeletal muscles of the legs is required. As a person sits and stands while working
in an office the leg muscles quadriceps, hamstrings, calf muscles all the responsible for
flexing and straightening the body. The joints involved here are the knees joint, ankle joint
and the hip joint. The ball and socket joint of the hips is responsible for the angular rotation
and making a right angle required for sitting. For the movement of the neck in all directions
the major muscles responsible are sternocleidomastoid and the trapezius. These muscles
present both on the left and right side work in a coordinate manner to cause flexion and
extensions of the head and neck in frontward and backward direction and they work
individually to cause lateral movement of the neck and the head. For typing the wrist joint
and the elbow joint remain active. The flexor and extensor muscles of the arms and that of the
writs are active while performing typing on a keyboard.
TAQ 4:
The Skeletal Muscles are the voluntary muscles of the body responsible for
locomotion and movement and mostly occur in pairs one performing agonistic and the other
antagonistic actions at the same time. Skeletal Muscles come in various shapes and sizes,
however the basic structure of all the skeletal muscles are the same. The cross section of
skeletal muscles show a connective tissue outer covering called Epimysium, which eventually
extends as the muscle tendon. It acts as a protective sheath. Inside there are bundles of fibres,
Fasciculi surrounded by another layer of connective tissue called Perimysium. Each fasciculi
may contain anywhere between 10-100 individual muscle fibres. These are multinucleated
elongated cells called Myocytes (Schiaffino and Reggiani 2011). They can length anywhere
between 1mm-30cm depending on the location of the muscle.
Each Myocytes appear striated under the microscope due to the presence of highly
organised actin and myosin filaments, which are the main component responsible for
in an office the leg muscles quadriceps, hamstrings, calf muscles all the responsible for
flexing and straightening the body. The joints involved here are the knees joint, ankle joint
and the hip joint. The ball and socket joint of the hips is responsible for the angular rotation
and making a right angle required for sitting. For the movement of the neck in all directions
the major muscles responsible are sternocleidomastoid and the trapezius. These muscles
present both on the left and right side work in a coordinate manner to cause flexion and
extensions of the head and neck in frontward and backward direction and they work
individually to cause lateral movement of the neck and the head. For typing the wrist joint
and the elbow joint remain active. The flexor and extensor muscles of the arms and that of the
writs are active while performing typing on a keyboard.
TAQ 4:
The Skeletal Muscles are the voluntary muscles of the body responsible for
locomotion and movement and mostly occur in pairs one performing agonistic and the other
antagonistic actions at the same time. Skeletal Muscles come in various shapes and sizes,
however the basic structure of all the skeletal muscles are the same. The cross section of
skeletal muscles show a connective tissue outer covering called Epimysium, which eventually
extends as the muscle tendon. It acts as a protective sheath. Inside there are bundles of fibres,
Fasciculi surrounded by another layer of connective tissue called Perimysium. Each fasciculi
may contain anywhere between 10-100 individual muscle fibres. These are multinucleated
elongated cells called Myocytes (Schiaffino and Reggiani 2011). They can length anywhere
between 1mm-30cm depending on the location of the muscle.
Each Myocytes appear striated under the microscope due to the presence of highly
organised actin and myosin filaments, which are the main component responsible for
contraction of the muscle cells. The skeletal muscle cell membrane is call sarcolemma the
cytoplasm within is called sarcoplasm. The sarcolemma contains various pit like
invaginations called Transverse tubules which play a role in supplying calcium ions to the
cells essential for muscular contraction. The myofibrils run parallel to the cells and are
surrounded by sarcoplasmic reticulum which are closely associated with the Transverse
tubules and act as a calcium ion sink of the cells. The actin and myosin filaments are
organised into sarcomeres along with other associated proteins. Within the sarcomere the
actin and myosin slide over each other to act as a contractile unit of the cell. Hence the
contractile role of each Myocytes solely depends on the sliding over of thin and thick
filaments over each other, which is the underlying principle that causes contraction of the
muscles as a whole. Contraction of skeletal muscles eventually causes movement of the
bones via tendons.
TAQ 5:
Muscle contraction occurs during work to create movement of the relevant part of the
body. As discussed earlier, the voluntary skeletal muscles attached to the bones by strong
connective tissues called tendons, cause movement of the bones by contraction over the edges
of the bones. Several types of muscle contraction are prevalent namely isometric, isotonic,
concentric and eccentric contraction. Muscles are classified as Agonists, Antagonists and
Synergists according to their mode of action while contraction. Muscles act in pair where
simple lack of contraction does not return the limb back to its original position. This is known
as antagonistic pairing and involves and an extensor muscle. The agonists are the prime
mover. During flexing of the forearm the biceps act as the agonist and pulls the forearm
towards the shoulder. The triceps on the other hand act as the antagonist resisting the
movement of the forearm up towards the shoulder. Hence, in antagonistic pairing one muscle
move the bone on one direction and the other moves the bone in another direction. One
cytoplasm within is called sarcoplasm. The sarcolemma contains various pit like
invaginations called Transverse tubules which play a role in supplying calcium ions to the
cells essential for muscular contraction. The myofibrils run parallel to the cells and are
surrounded by sarcoplasmic reticulum which are closely associated with the Transverse
tubules and act as a calcium ion sink of the cells. The actin and myosin filaments are
organised into sarcomeres along with other associated proteins. Within the sarcomere the
actin and myosin slide over each other to act as a contractile unit of the cell. Hence the
contractile role of each Myocytes solely depends on the sliding over of thin and thick
filaments over each other, which is the underlying principle that causes contraction of the
muscles as a whole. Contraction of skeletal muscles eventually causes movement of the
bones via tendons.
TAQ 5:
Muscle contraction occurs during work to create movement of the relevant part of the
body. As discussed earlier, the voluntary skeletal muscles attached to the bones by strong
connective tissues called tendons, cause movement of the bones by contraction over the edges
of the bones. Several types of muscle contraction are prevalent namely isometric, isotonic,
concentric and eccentric contraction. Muscles are classified as Agonists, Antagonists and
Synergists according to their mode of action while contraction. Muscles act in pair where
simple lack of contraction does not return the limb back to its original position. This is known
as antagonistic pairing and involves and an extensor muscle. The agonists are the prime
mover. During flexing of the forearm the biceps act as the agonist and pulls the forearm
towards the shoulder. The triceps on the other hand act as the antagonist resisting the
movement of the forearm up towards the shoulder. Hence, in antagonistic pairing one muscle
move the bone on one direction and the other moves the bone in another direction. One
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
muscle relaxes while the other contracts and it is not possible stimulate contraction of both
the muscles at the same time.
References
Bartlett, J.L., Sumner, B., Ellis, R.G. and Kram, R., 2014. Activity and functions of the
human gluteal muscles in walking, running, sprinting, and climbing. American journal of
physical anthropology, 153(1), pp.124-131.
Higashihara, A., Ono, T., Kubota, J., Okuwaki, T. and Fukubayashi, T., 2010. Functional
differences in the activity of the hamstring muscles with increasing running speed. Journal of
sports sciences, 28(10), pp.1085-1092.
Murshed, M. and McKee, M.D., 2010. Molecular determinants of extracellular matrix
mineralization in bone and blood vessels. Current opinion in nephrology and
hypertension, 19(4), pp.359-365.
Neumann, D.A., 2013. Kinesiology of the Musculoskeletal System-E-Book: Foundations for
Rehabilitation. Elsevier Health Sciences.
Reese, N.B. and Bandy, W.D., 2016. Joint Range of Motion and Muscle Length Testing-E-
Book. Elsevier Health Sciences.
Schiaffino, S. and Reggiani, C., 2011. Fiber types in mammalian skeletal
muscles. Physiological reviews, 91(4), pp.1447-1531.
Weinstein, R., Guendelman, E. and Fedkiw, R., 2008. Impulse-based control of joints and
muscles. IEEE Transactions on Visualization and Computer Graphics, 14(1), pp.37-46.
the muscles at the same time.
References
Bartlett, J.L., Sumner, B., Ellis, R.G. and Kram, R., 2014. Activity and functions of the
human gluteal muscles in walking, running, sprinting, and climbing. American journal of
physical anthropology, 153(1), pp.124-131.
Higashihara, A., Ono, T., Kubota, J., Okuwaki, T. and Fukubayashi, T., 2010. Functional
differences in the activity of the hamstring muscles with increasing running speed. Journal of
sports sciences, 28(10), pp.1085-1092.
Murshed, M. and McKee, M.D., 2010. Molecular determinants of extracellular matrix
mineralization in bone and blood vessels. Current opinion in nephrology and
hypertension, 19(4), pp.359-365.
Neumann, D.A., 2013. Kinesiology of the Musculoskeletal System-E-Book: Foundations for
Rehabilitation. Elsevier Health Sciences.
Reese, N.B. and Bandy, W.D., 2016. Joint Range of Motion and Muscle Length Testing-E-
Book. Elsevier Health Sciences.
Schiaffino, S. and Reggiani, C., 2011. Fiber types in mammalian skeletal
muscles. Physiological reviews, 91(4), pp.1447-1531.
Weinstein, R., Guendelman, E. and Fedkiw, R., 2008. Impulse-based control of joints and
muscles. IEEE Transactions on Visualization and Computer Graphics, 14(1), pp.37-46.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





