Nasogastric Tube Verification Article 2022
VerifiedAdded on 2022/09/23
|10
|2708
|24
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NASOGASTRIC TUBE VERIFICATION 1
The use of biochemical markers for determining the correct placement of nasogastric tube in
adult patients in hospital settings?
Student’s Name
University
The use of biochemical markers for determining the correct placement of nasogastric tube in
adult patients in hospital settings?
Student’s Name
University
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NASOGASTRIC TUBE VERIFICATION 2
The use of biochemical markers for determining the correct placement of nasogastric tube
in adult patients in hospital settings?
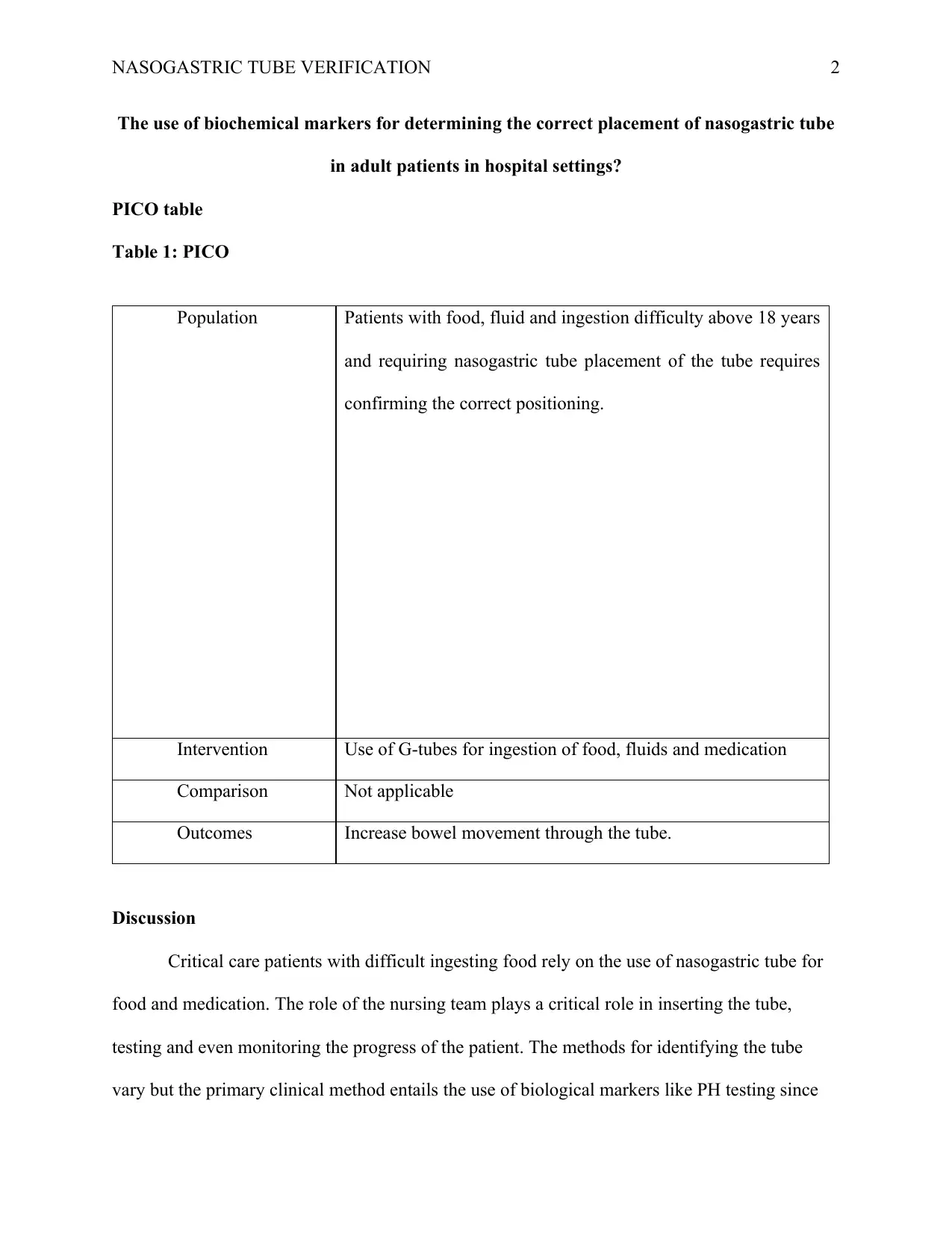
PICO table
Table 1: PICO
Population Patients with food, fluid and ingestion difficulty above 18 years
and requiring nasogastric tube placement of the tube requires
confirming the correct positioning.
Intervention Use of G-tubes for ingestion of food, fluids and medication
Comparison Not applicable
Outcomes Increase bowel movement through the tube.
Discussion
Critical care patients with difficult ingesting food rely on the use of nasogastric tube for
food and medication. The role of the nursing team plays a critical role in inserting the tube,
testing and even monitoring the progress of the patient. The methods for identifying the tube
vary but the primary clinical method entails the use of biological markers like PH testing since
The use of biochemical markers for determining the correct placement of nasogastric tube
in adult patients in hospital settings?
PICO table
Table 1: PICO
Population Patients with food, fluid and ingestion difficulty above 18 years
and requiring nasogastric tube placement of the tube requires
confirming the correct positioning.
Intervention Use of G-tubes for ingestion of food, fluids and medication
Comparison Not applicable
Outcomes Increase bowel movement through the tube.
Discussion
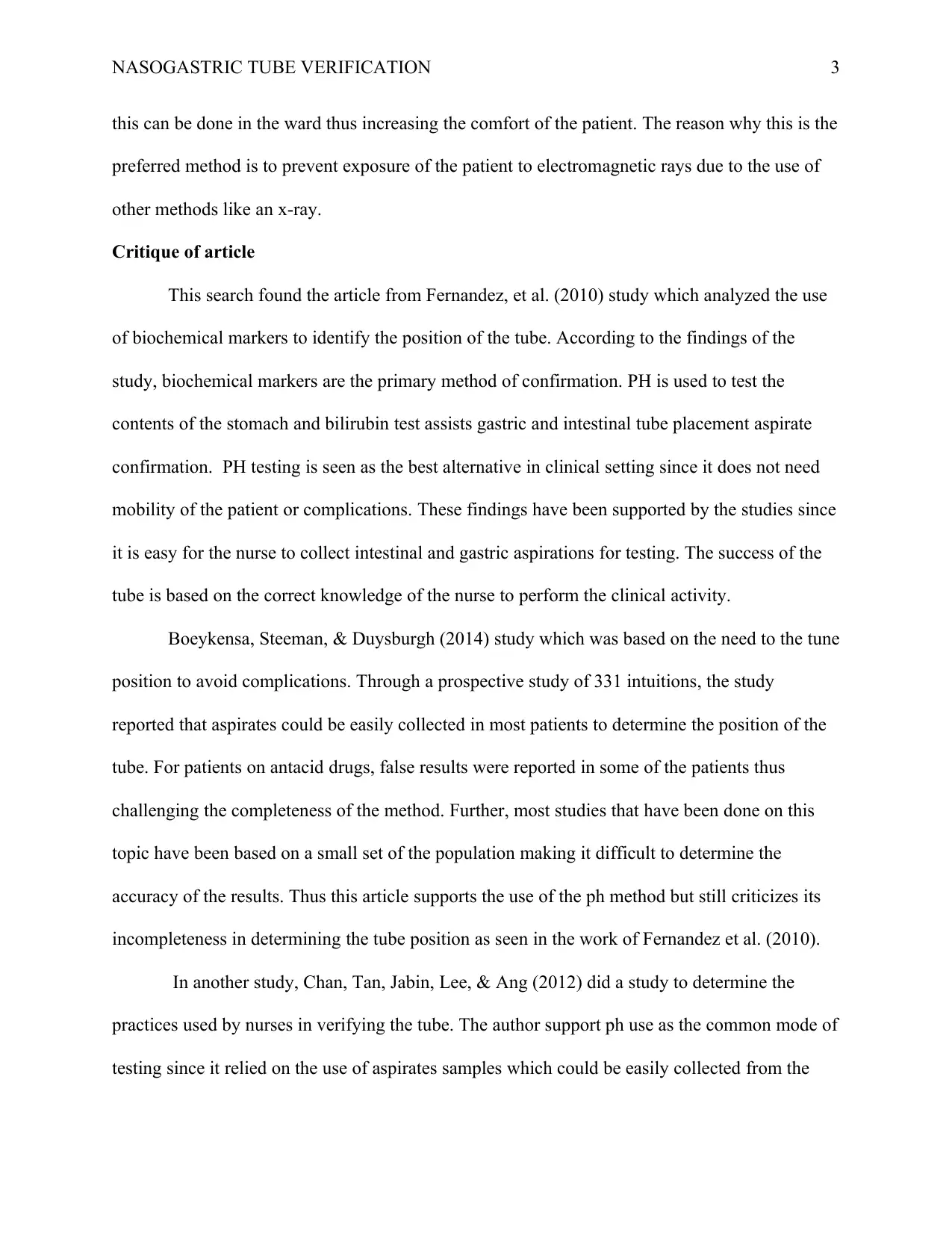
Critical care patients with difficult ingesting food rely on the use of nasogastric tube for
food and medication. The role of the nursing team plays a critical role in inserting the tube,
testing and even monitoring the progress of the patient. The methods for identifying the tube
vary but the primary clinical method entails the use of biological markers like PH testing since
NASOGASTRIC TUBE VERIFICATION 3
this can be done in the ward thus increasing the comfort of the patient. The reason why this is the
preferred method is to prevent exposure of the patient to electromagnetic rays due to the use of
other methods like an x-ray.
Critique of article
This search found the article from Fernandez, et al. (2010) study which analyzed the use
of biochemical markers to identify the position of the tube. According to the findings of the
study, biochemical markers are the primary method of confirmation. PH is used to test the
contents of the stomach and bilirubin test assists gastric and intestinal tube placement aspirate
confirmation. PH testing is seen as the best alternative in clinical setting since it does not need
mobility of the patient or complications. These findings have been supported by the studies since
it is easy for the nurse to collect intestinal and gastric aspirations for testing. The success of the
tube is based on the correct knowledge of the nurse to perform the clinical activity.
Boeykensa, Steeman, & Duysburgh (2014) study which was based on the need to the tune
position to avoid complications. Through a prospective study of 331 intuitions, the study
reported that aspirates could be easily collected in most patients to determine the position of the
tube. For patients on antacid drugs, false results were reported in some of the patients thus
challenging the completeness of the method. Further, most studies that have been done on this
topic have been based on a small set of the population making it difficult to determine the
accuracy of the results. Thus this article supports the use of the ph method but still criticizes its
incompleteness in determining the tube position as seen in the work of Fernandez et al. (2010).
In another study, Chan, Tan, Jabin, Lee, & Ang (2012) did a study to determine the
practices used by nurses in verifying the tube. The author support ph use as the common mode of
testing since it relied on the use of aspirates samples which could be easily collected from the
this can be done in the ward thus increasing the comfort of the patient. The reason why this is the
preferred method is to prevent exposure of the patient to electromagnetic rays due to the use of
other methods like an x-ray.
Critique of article
This search found the article from Fernandez, et al. (2010) study which analyzed the use
of biochemical markers to identify the position of the tube. According to the findings of the
study, biochemical markers are the primary method of confirmation. PH is used to test the
contents of the stomach and bilirubin test assists gastric and intestinal tube placement aspirate
confirmation. PH testing is seen as the best alternative in clinical setting since it does not need
mobility of the patient or complications. These findings have been supported by the studies since
it is easy for the nurse to collect intestinal and gastric aspirations for testing. The success of the
tube is based on the correct knowledge of the nurse to perform the clinical activity.
Boeykensa, Steeman, & Duysburgh (2014) study which was based on the need to the tune
position to avoid complications. Through a prospective study of 331 intuitions, the study
reported that aspirates could be easily collected in most patients to determine the position of the
tube. For patients on antacid drugs, false results were reported in some of the patients thus
challenging the completeness of the method. Further, most studies that have been done on this
topic have been based on a small set of the population making it difficult to determine the
accuracy of the results. Thus this article supports the use of the ph method but still criticizes its
incompleteness in determining the tube position as seen in the work of Fernandez et al. (2010).
In another study, Chan, Tan, Jabin, Lee, & Ang (2012) did a study to determine the
practices used by nurses in verifying the tube. The author support ph use as the common mode of
testing since it relied on the use of aspirates samples which could be easily collected from the
NASOGASTRIC TUBE VERIFICATION 4
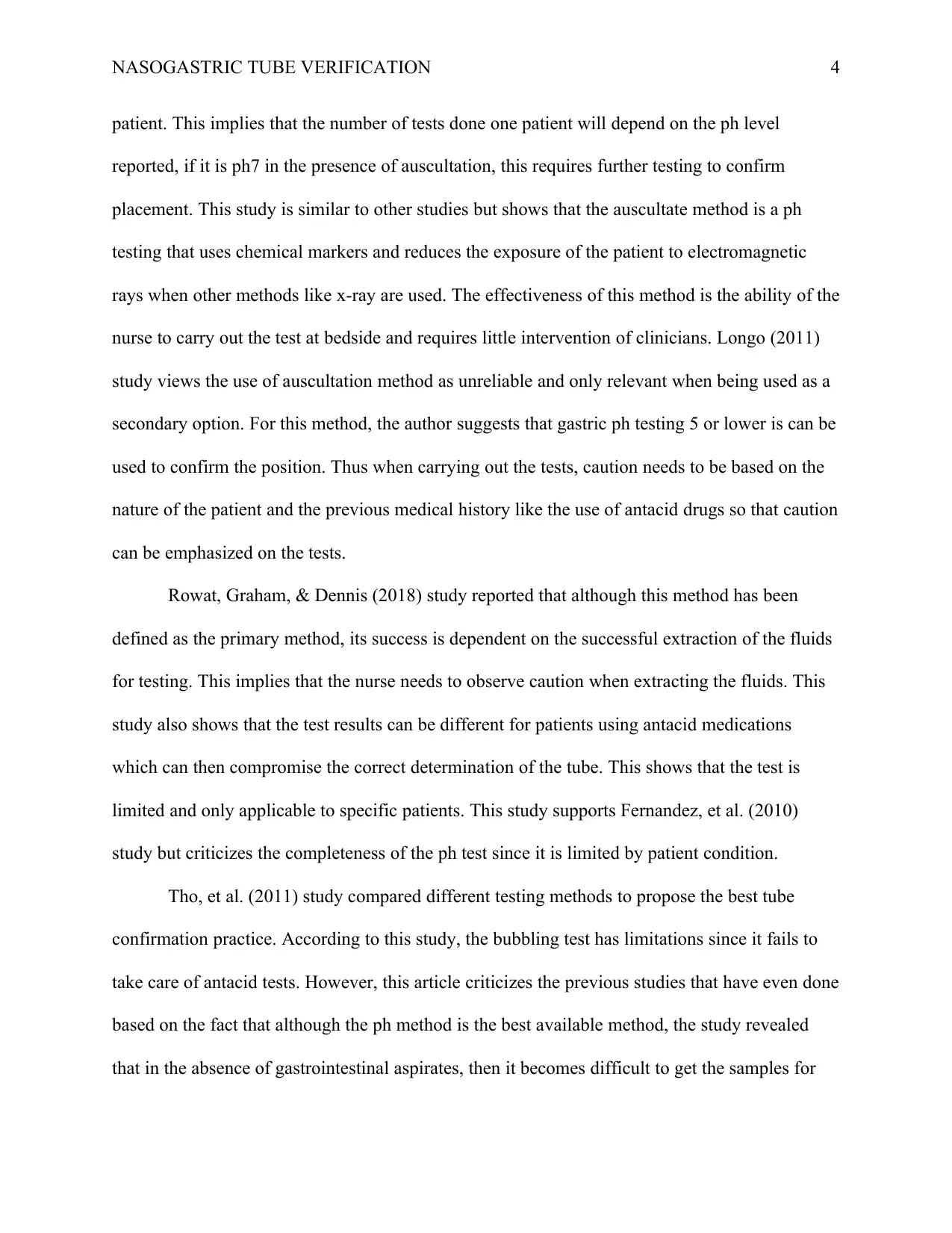
patient. This implies that the number of tests done one patient will depend on the ph level
reported, if it is ph7 in the presence of auscultation, this requires further testing to confirm
placement. This study is similar to other studies but shows that the auscultate method is a ph
testing that uses chemical markers and reduces the exposure of the patient to electromagnetic
rays when other methods like x-ray are used. The effectiveness of this method is the ability of the
nurse to carry out the test at bedside and requires little intervention of clinicians. Longo (2011)
study views the use of auscultation method as unreliable and only relevant when being used as a
secondary option. For this method, the author suggests that gastric ph testing 5 or lower is can be
used to confirm the position. Thus when carrying out the tests, caution needs to be based on the
nature of the patient and the previous medical history like the use of antacid drugs so that caution
can be emphasized on the tests.
Rowat, Graham, & Dennis (2018) study reported that although this method has been
defined as the primary method, its success is dependent on the successful extraction of the fluids
for testing. This implies that the nurse needs to observe caution when extracting the fluids. This
study also shows that the test results can be different for patients using antacid medications
which can then compromise the correct determination of the tube. This shows that the test is
limited and only applicable to specific patients. This study supports Fernandez, et al. (2010)
study but criticizes the completeness of the ph test since it is limited by patient condition.
Tho, et al. (2011) study compared different testing methods to propose the best tube
confirmation practice. According to this study, the bubbling test has limitations since it fails to
take care of antacid tests. However, this article criticizes the previous studies that have even done
based on the fact that although the ph method is the best available method, the study revealed
that in the absence of gastrointestinal aspirates, then it becomes difficult to get the samples for
patient. This implies that the number of tests done one patient will depend on the ph level
reported, if it is ph7 in the presence of auscultation, this requires further testing to confirm
placement. This study is similar to other studies but shows that the auscultate method is a ph
testing that uses chemical markers and reduces the exposure of the patient to electromagnetic
rays when other methods like x-ray are used. The effectiveness of this method is the ability of the
nurse to carry out the test at bedside and requires little intervention of clinicians. Longo (2011)
study views the use of auscultation method as unreliable and only relevant when being used as a
secondary option. For this method, the author suggests that gastric ph testing 5 or lower is can be
used to confirm the position. Thus when carrying out the tests, caution needs to be based on the
nature of the patient and the previous medical history like the use of antacid drugs so that caution
can be emphasized on the tests.
Rowat, Graham, & Dennis (2018) study reported that although this method has been
defined as the primary method, its success is dependent on the successful extraction of the fluids
for testing. This implies that the nurse needs to observe caution when extracting the fluids. This
study also shows that the test results can be different for patients using antacid medications
which can then compromise the correct determination of the tube. This shows that the test is
limited and only applicable to specific patients. This study supports Fernandez, et al. (2010)
study but criticizes the completeness of the ph test since it is limited by patient condition.
Tho, et al. (2011) study compared different testing methods to propose the best tube
confirmation practice. According to this study, the bubbling test has limitations since it fails to
take care of antacid tests. However, this article criticizes the previous studies that have even done
based on the fact that although the ph method is the best available method, the study revealed
that in the absence of gastrointestinal aspirates, then it becomes difficult to get the samples for
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NASOGASTRIC TUBE VERIFICATION 5
the test. These findings have been supported by Petitpas, Kerforne, Lacroix, & Mimoz (2012)
who argued that patient situations can present challenges on the nature of the method that is used
to test for tube placement. This implies that although the ph method is the simplest, it is subject
to limitations which make it only applicable to specific patients.
Borsci, Buckel, Huddy, Alaestant & Hanna (2017) study reported challenges in
differentiating the ph level that is required in clinical settings.. This is seen in the close ph
differences which are from a range of 5-7 which is supposed to be the baseline of the decision to
use the tube or not. This study further shows that there are 30% misinterpretation and 12% ph
reading errors due to the lack of unreliability in the visual ph inspection method. Further, in
situations where samples are collected and stored before being tested, this study showed that
there could be variations which were also supported by Rowat, Graham, & Dennis (2018) who
felt that the ph testing effectiveness can be affected by freezing and defrosting of the samples.
Thus for increased reliability, this study proposes that samples should be tasted when they are
fresh.
From the studies, it is evident that biochemical markers are the best to confirming the
tube location. However, there is a need for the use of other verification methods in case the ph
method fails to yield positive results. This is because the ph method has a few limitations like the
case of patients on antiacid drugs, failure to collect the gastrointestinal aspirates and the case of
critical care patients who may pose certain difficulties in using the method. Therefore, there is
the need for organizations to develop proper guidelines for the use of the ph methods and at the
same time to highlight the limitations of the method and what needs to be done in such cases.
the test. These findings have been supported by Petitpas, Kerforne, Lacroix, & Mimoz (2012)
who argued that patient situations can present challenges on the nature of the method that is used
to test for tube placement. This implies that although the ph method is the simplest, it is subject
to limitations which make it only applicable to specific patients.
Borsci, Buckel, Huddy, Alaestant & Hanna (2017) study reported challenges in
differentiating the ph level that is required in clinical settings.. This is seen in the close ph
differences which are from a range of 5-7 which is supposed to be the baseline of the decision to
use the tube or not. This study further shows that there are 30% misinterpretation and 12% ph
reading errors due to the lack of unreliability in the visual ph inspection method. Further, in
situations where samples are collected and stored before being tested, this study showed that
there could be variations which were also supported by Rowat, Graham, & Dennis (2018) who
felt that the ph testing effectiveness can be affected by freezing and defrosting of the samples.
Thus for increased reliability, this study proposes that samples should be tasted when they are
fresh.
From the studies, it is evident that biochemical markers are the best to confirming the
tube location. However, there is a need for the use of other verification methods in case the ph
method fails to yield positive results. This is because the ph method has a few limitations like the
case of patients on antiacid drugs, failure to collect the gastrointestinal aspirates and the case of
critical care patients who may pose certain difficulties in using the method. Therefore, there is
the need for organizations to develop proper guidelines for the use of the ph methods and at the
same time to highlight the limitations of the method and what needs to be done in such cases.
NASOGASTRIC TUBE VERIFICATION 6
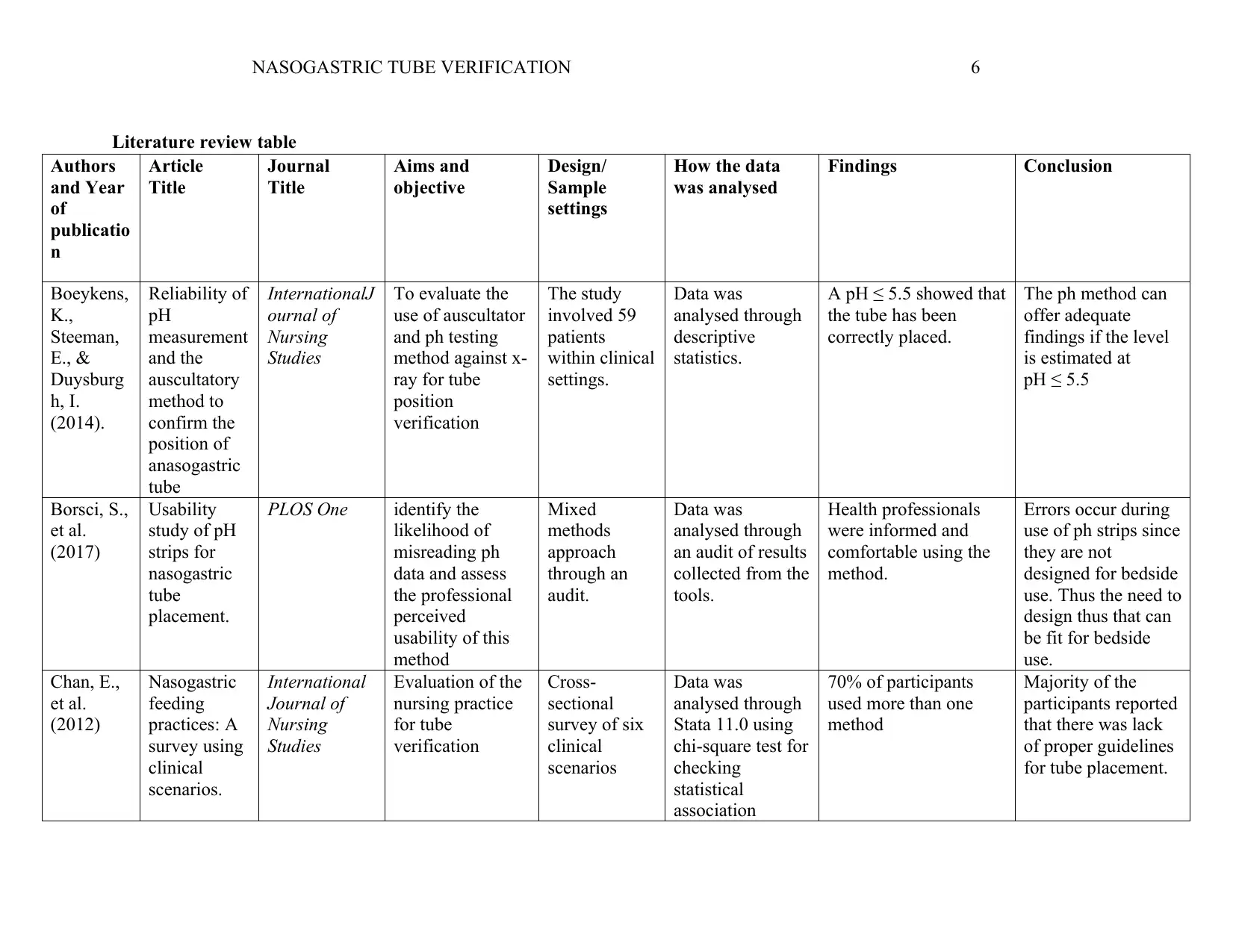
Literature review table
Authors
and Year
of
publicatio
n
Article
Title
Journal
Title
Aims and
objective
Design/
Sample
settings
How the data
was analysed
Findings Conclusion
Boeykens,
K.,
Steeman,
E., &
Duysburg
h, I.
(2014).
Reliability of
pH
measurement
and the
auscultatory
method to
confirm the
position of
anasogastric
tube
InternationalJ
ournal of
Nursing
Studies
To evaluate the
use of auscultator
and ph testing
method against x-
ray for tube
position
verification
The study
involved 59
patients
within clinical
settings.
Data was
analysed through
descriptive
statistics.
A pH ≤ 5.5 showed that
the tube has been
correctly placed.
The ph method can
offer adequate
findings if the level
is estimated at
pH ≤ 5.5
Borsci, S.,
et al.
(2017)
Usability
study of pH
strips for
nasogastric
tube
placement.
PLOS One identify the
likelihood of
misreading ph
data and assess
the professional
perceived
usability of this
method
Mixed
methods
approach
through an
audit.
Data was
analysed through
an audit of results
collected from the
tools.
Health professionals
were informed and
comfortable using the
method.
Errors occur during
use of ph strips since
they are not
designed for bedside
use. Thus the need to
design thus that can
be fit for bedside
use.
Chan, E.,
et al.
(2012)
Nasogastric
feeding
practices: A
survey using
clinical
scenarios.
International
Journal of
Nursing
Studies
Evaluation of the
nursing practice
for tube
verification
Cross-
sectional
survey of six
clinical
scenarios
Data was
analysed through
Stata 11.0 using
chi-square test for
checking
statistical
association
70% of participants
used more than one
method
Majority of the
participants reported
that there was lack
of proper guidelines
for tube placement.
Literature review table
Authors
and Year
of
publicatio
n
Article
Title
Journal
Title
Aims and
objective
Design/
Sample
settings
How the data
was analysed
Findings Conclusion
Boeykens,
K.,
Steeman,
E., &
Duysburg
h, I.
(2014).
Reliability of
pH
measurement
and the
auscultatory
method to
confirm the
position of
anasogastric
tube
InternationalJ
ournal of
Nursing
Studies
To evaluate the
use of auscultator
and ph testing
method against x-
ray for tube
position
verification
The study
involved 59
patients
within clinical
settings.
Data was
analysed through
descriptive
statistics.
A pH ≤ 5.5 showed that
the tube has been
correctly placed.
The ph method can
offer adequate
findings if the level
is estimated at
pH ≤ 5.5
Borsci, S.,
et al.
(2017)
Usability
study of pH
strips for
nasogastric
tube
placement.
PLOS One identify the
likelihood of
misreading ph
data and assess
the professional
perceived
usability of this
method
Mixed
methods
approach
through an
audit.
Data was
analysed through
an audit of results
collected from the
tools.
Health professionals
were informed and
comfortable using the
method.
Errors occur during
use of ph strips since
they are not
designed for bedside
use. Thus the need to
design thus that can
be fit for bedside
use.
Chan, E.,
et al.
(2012)
Nasogastric
feeding
practices: A
survey using
clinical
scenarios.
International
Journal of
Nursing
Studies
Evaluation of the
nursing practice
for tube
verification
Cross-
sectional
survey of six
clinical
scenarios
Data was
analysed through
Stata 11.0 using
chi-square test for
checking
statistical
association
70% of participants
used more than one
method
Majority of the
participants reported
that there was lack
of proper guidelines
for tube placement.
NASOGASTRIC TUBE VERIFICATION 7
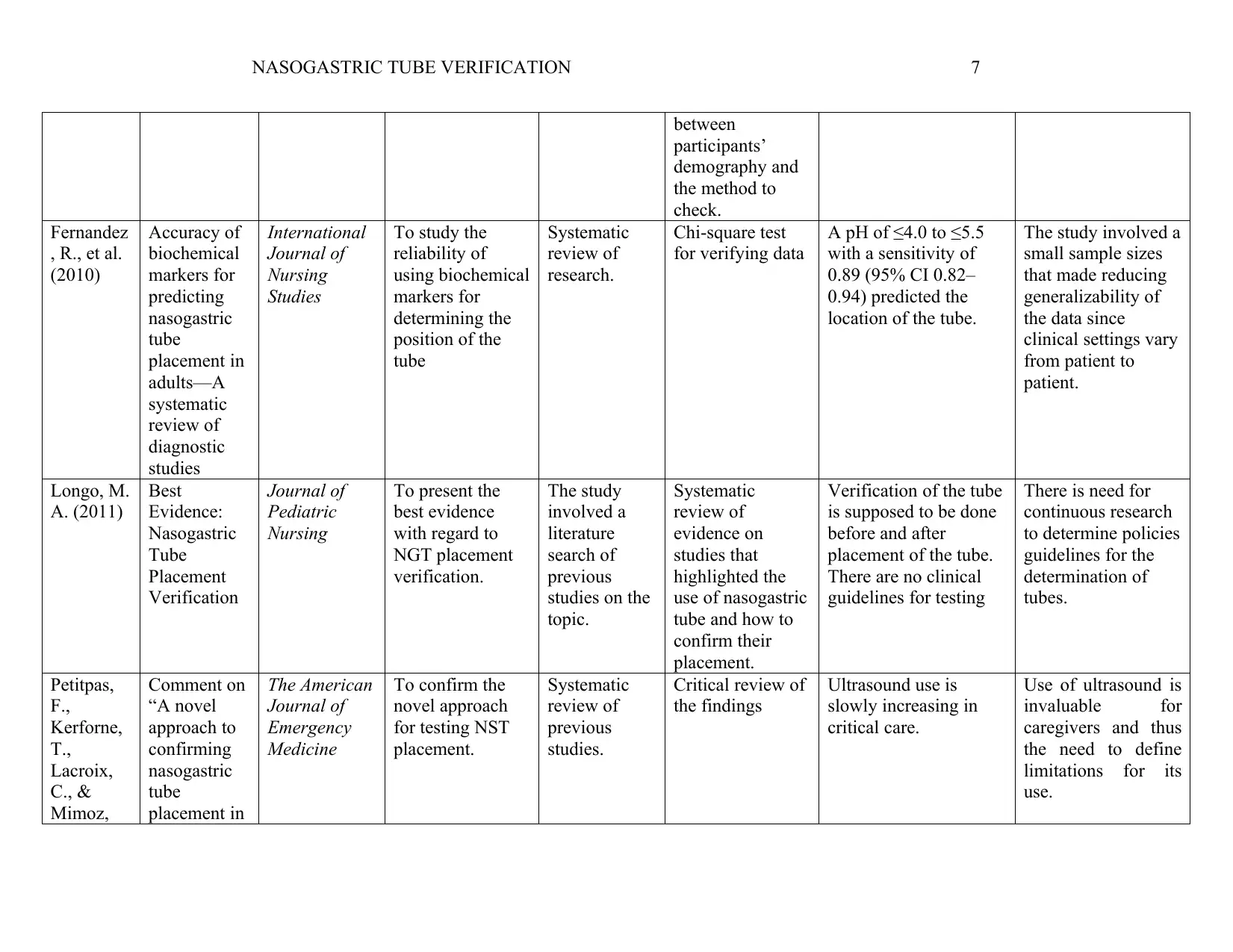
between
participants’
demography and
the method to
check.
Fernandez
, R., et al.
(2010)
Accuracy of
biochemical
markers for
predicting
nasogastric
tube
placement in
adults—A
systematic
review of
diagnostic
studies
International
Journal of
Nursing
Studies
To study the
reliability of
using biochemical
markers for
determining the
position of the
tube
Systematic
review of
research.
Chi-square test
for verifying data
A pH of ≤4.0 to ≤5.5
with a sensitivity of
0.89 (95% CI 0.82–
0.94) predicted the
location of the tube.
The study involved a
small sample sizes
that made reducing
generalizability of
the data since
clinical settings vary
from patient to
patient.
Longo, M.
A. (2011)
Best
Evidence:
Nasogastric
Tube
Placement
Verification
Journal of
Pediatric
Nursing
To present the
best evidence
with regard to
NGT placement
verification.
The study
involved a
literature
search of
previous
studies on the
topic.
Systematic
review of
evidence on
studies that
highlighted the
use of nasogastric
tube and how to
confirm their
placement.
Verification of the tube
is supposed to be done
before and after
placement of the tube.
There are no clinical
guidelines for testing
There is need for
continuous research
to determine policies
guidelines for the
determination of
tubes.
Petitpas,
F.,
Kerforne,
T.,
Lacroix,
C., &
Mimoz,
Comment on
“A novel
approach to
confirming
nasogastric
tube
placement in
The American
Journal of
Emergency
Medicine
To confirm the
novel approach
for testing NST
placement.
Systematic
review of
previous
studies.
Critical review of
the findings
Ultrasound use is
slowly increasing in
critical care.
Use of ultrasound is
invaluable for
caregivers and thus
the need to define
limitations for its
use.
between
participants’
demography and
the method to
check.
Fernandez
, R., et al.
(2010)
Accuracy of
biochemical
markers for
predicting
nasogastric
tube
placement in
adults—A
systematic
review of
diagnostic
studies
International
Journal of
Nursing
Studies
To study the
reliability of
using biochemical
markers for
determining the
position of the
tube
Systematic
review of
research.
Chi-square test
for verifying data
A pH of ≤4.0 to ≤5.5
with a sensitivity of
0.89 (95% CI 0.82–
0.94) predicted the
location of the tube.
The study involved a
small sample sizes
that made reducing
generalizability of
the data since
clinical settings vary
from patient to
patient.
Longo, M.
A. (2011)
Best
Evidence:
Nasogastric
Tube
Placement
Verification
Journal of
Pediatric
Nursing
To present the
best evidence
with regard to
NGT placement
verification.
The study
involved a
literature
search of
previous
studies on the
topic.
Systematic
review of
evidence on
studies that
highlighted the
use of nasogastric
tube and how to
confirm their
placement.
Verification of the tube
is supposed to be done
before and after
placement of the tube.
There are no clinical
guidelines for testing
There is need for
continuous research
to determine policies
guidelines for the
determination of
tubes.
Petitpas,
F.,
Kerforne,
T.,
Lacroix,
C., &
Mimoz,
Comment on
“A novel
approach to
confirming
nasogastric
tube
placement in
The American
Journal of
Emergency
Medicine
To confirm the
novel approach
for testing NST
placement.
Systematic
review of
previous
studies.
Critical review of
the findings
Ultrasound use is
slowly increasing in
critical care.
Use of ultrasound is
invaluable for
caregivers and thus
the need to define
limitations for its
use.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NASOGASTRIC TUBE VERIFICATION 8
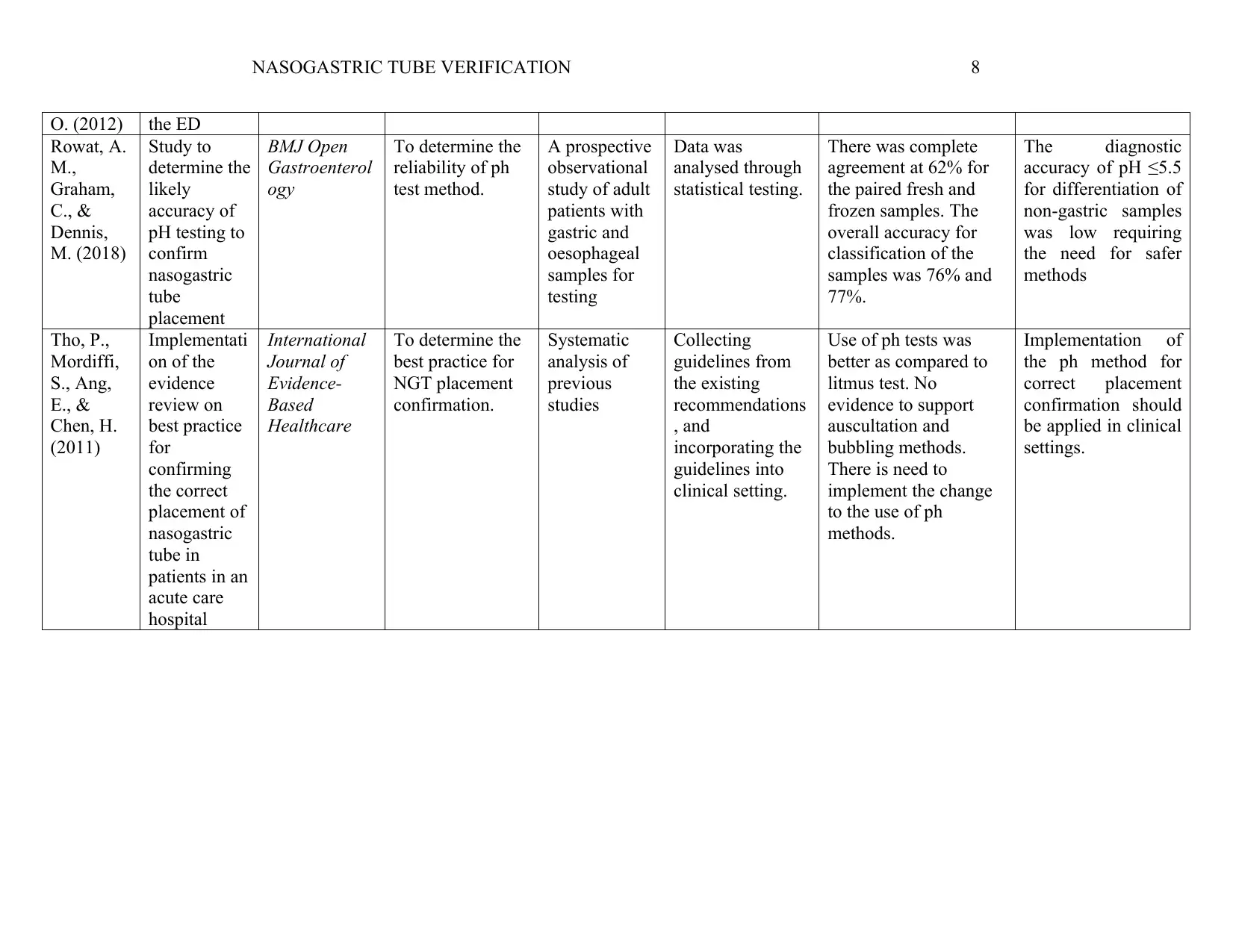
O. (2012) the ED
Rowat, A.
M.,
Graham,
C., &
Dennis,
M. (2018)
Study to
determine the
likely
accuracy of
pH testing to
confirm
nasogastric
tube
placement
BMJ Open
Gastroenterol
ogy
To determine the
reliability of ph
test method.
A prospective
observational
study of adult
patients with
gastric and
oesophageal
samples for
testing
Data was
analysed through
statistical testing.
There was complete
agreement at 62% for
the paired fresh and
frozen samples. The
overall accuracy for
classification of the
samples was 76% and
77%.
The diagnostic
accuracy of pH ≤5.5
for differentiation of
non-gastric samples
was low requiring
the need for safer
methods
Tho, P.,
Mordiffi,
S., Ang,
E., &
Chen, H.
(2011)
Implementati
on of the
evidence
review on
best practice
for
confirming
the correct
placement of
nasogastric
tube in
patients in an
acute care
hospital
International
Journal of
Evidence-
Based
Healthcare
To determine the
best practice for
NGT placement
confirmation.
Systematic
analysis of
previous
studies
Collecting
guidelines from
the existing
recommendations
, and
incorporating the
guidelines into
clinical setting.
Use of ph tests was
better as compared to
litmus test. No
evidence to support
auscultation and
bubbling methods.
There is need to
implement the change
to the use of ph
methods.
Implementation of
the ph method for
correct placement
confirmation should
be applied in clinical
settings.
O. (2012) the ED
Rowat, A.
M.,
Graham,
C., &
Dennis,
M. (2018)
Study to
determine the
likely
accuracy of
pH testing to
confirm
nasogastric
tube
placement
BMJ Open
Gastroenterol
ogy
To determine the
reliability of ph
test method.
A prospective
observational
study of adult
patients with
gastric and
oesophageal
samples for
testing
Data was
analysed through
statistical testing.
There was complete
agreement at 62% for
the paired fresh and
frozen samples. The
overall accuracy for
classification of the
samples was 76% and
77%.
The diagnostic
accuracy of pH ≤5.5
for differentiation of
non-gastric samples
was low requiring
the need for safer
methods
Tho, P.,
Mordiffi,
S., Ang,
E., &
Chen, H.
(2011)
Implementati
on of the
evidence
review on
best practice
for
confirming
the correct
placement of
nasogastric
tube in
patients in an
acute care
hospital
International
Journal of
Evidence-
Based
Healthcare
To determine the
best practice for
NGT placement
confirmation.
Systematic
analysis of
previous
studies
Collecting
guidelines from
the existing
recommendations
, and
incorporating the
guidelines into
clinical setting.
Use of ph tests was
better as compared to
litmus test. No
evidence to support
auscultation and
bubbling methods.
There is need to
implement the change
to the use of ph
methods.
Implementation of
the ph method for
correct placement
confirmation should
be applied in clinical
settings.
NASOGASTRIC TUBE VERIFICATION 9
References
Boeykensa, K., Steeman, E., & Duysburgh, I. (2014). Reliability of pH measurement and the
auscultatory method to confirm the position of anasogastric tube. InternationalJournal of
Nursing Studies, 51, 1427-1433.
Borsci, S., Buckle, P., Huddy, J., Alaestante, Z., Ni, Z., & Hanna, G. B. (2017). Usability study
of pH strips for nasogastric tube placement. PLOS One, 12(11).
Chan, E., Tan, S., Jabin, K., Lee, L., & Ang, C. (2012). Nasogastric feeding practices: A survey
using clinical scenarios. International Journal of Nursing Studies,, 49(3), 310-319.
Fernandez, R., Chau, J., Thompson, D., Griffiths, R., & Lo, H. (2010). Accuracy of biochemical
markers for predicting nasogastric tube placement in adults—A systematic review of
diagnostic studies. , 47(8),. International Journal of Nursing Studies, 47(8), 1037-104.
Longo, M. A. (2011). Best Evidence: Nasogastric Tube Placement Verification. Journal of
Pediatric Nursing, 26, 373–376.
Petitpas, F., Kerforne, T., Lacroix, C., & Mimoz, O. (2012). Comment on “A novel approach to
confirming nasogastric tube placement in the ED”. The American Journal of Emergency
Medicine, 30(4), 631-632.
Rowat, A. M., Graham, C., & Dennis, M. (2018). Study to determine the likely accuracy of pH
testing to confirm nasogastric tube placement. BMJ Open Gastroenterology, 5(1).
Tho, P., Mordiffi, S., Ang, E., & Chen, H. (2011). Implementation of the evidence review on
best practice for confirming the correct placement of nasogastric tube in patients in an
acute care hospital. International Journal of Evidence-Based Healthcare, 1.
References
Boeykensa, K., Steeman, E., & Duysburgh, I. (2014). Reliability of pH measurement and the
auscultatory method to confirm the position of anasogastric tube. InternationalJournal of
Nursing Studies, 51, 1427-1433.
Borsci, S., Buckle, P., Huddy, J., Alaestante, Z., Ni, Z., & Hanna, G. B. (2017). Usability study
of pH strips for nasogastric tube placement. PLOS One, 12(11).
Chan, E., Tan, S., Jabin, K., Lee, L., & Ang, C. (2012). Nasogastric feeding practices: A survey
using clinical scenarios. International Journal of Nursing Studies,, 49(3), 310-319.
Fernandez, R., Chau, J., Thompson, D., Griffiths, R., & Lo, H. (2010). Accuracy of biochemical
markers for predicting nasogastric tube placement in adults—A systematic review of
diagnostic studies. , 47(8),. International Journal of Nursing Studies, 47(8), 1037-104.
Longo, M. A. (2011). Best Evidence: Nasogastric Tube Placement Verification. Journal of
Pediatric Nursing, 26, 373–376.
Petitpas, F., Kerforne, T., Lacroix, C., & Mimoz, O. (2012). Comment on “A novel approach to
confirming nasogastric tube placement in the ED”. The American Journal of Emergency
Medicine, 30(4), 631-632.
Rowat, A. M., Graham, C., & Dennis, M. (2018). Study to determine the likely accuracy of pH
testing to confirm nasogastric tube placement. BMJ Open Gastroenterology, 5(1).
Tho, P., Mordiffi, S., Ang, E., & Chen, H. (2011). Implementation of the evidence review on
best practice for confirming the correct placement of nasogastric tube in patients in an
acute care hospital. International Journal of Evidence-Based Healthcare, 1.
NASOGASTRIC TUBE VERIFICATION 10
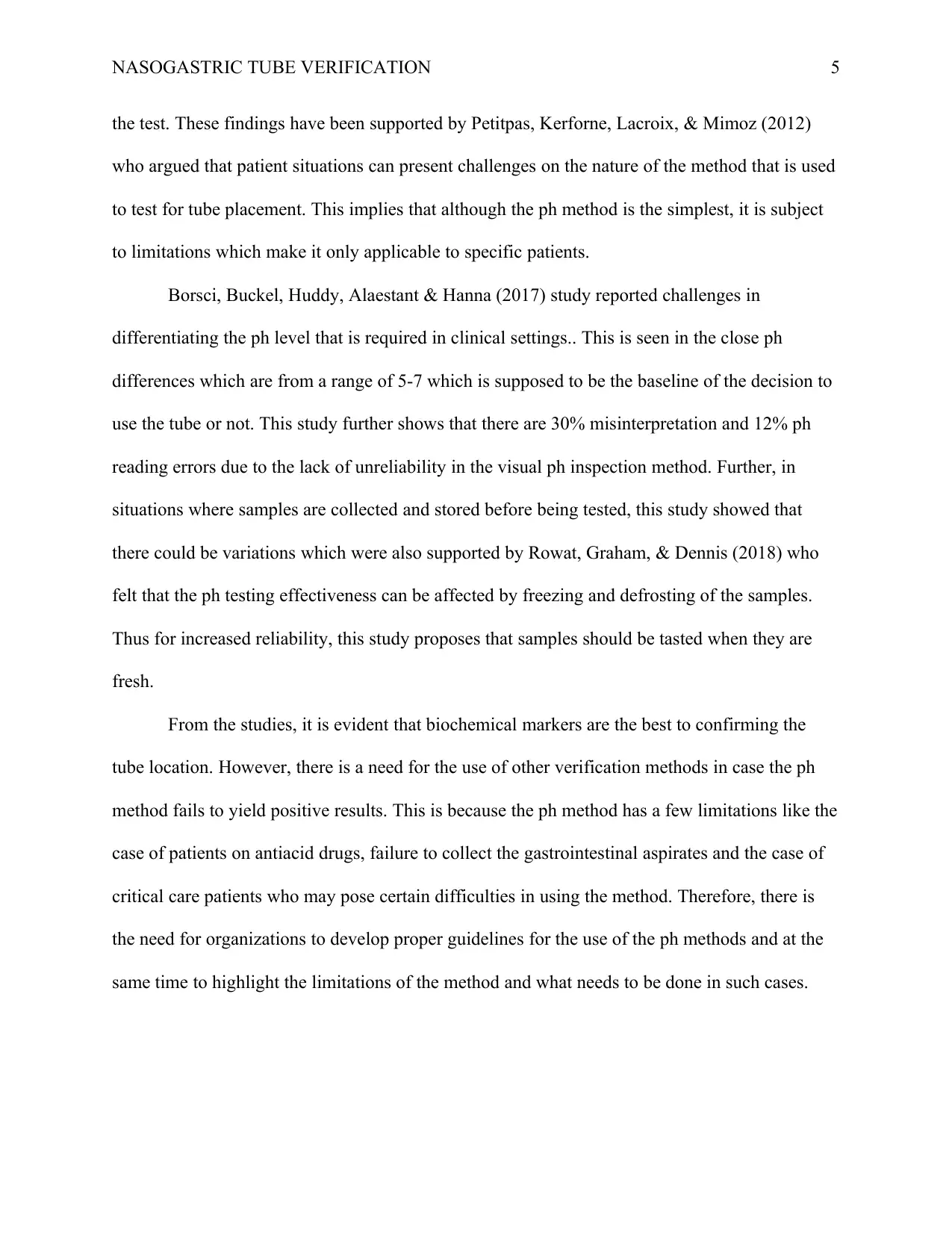
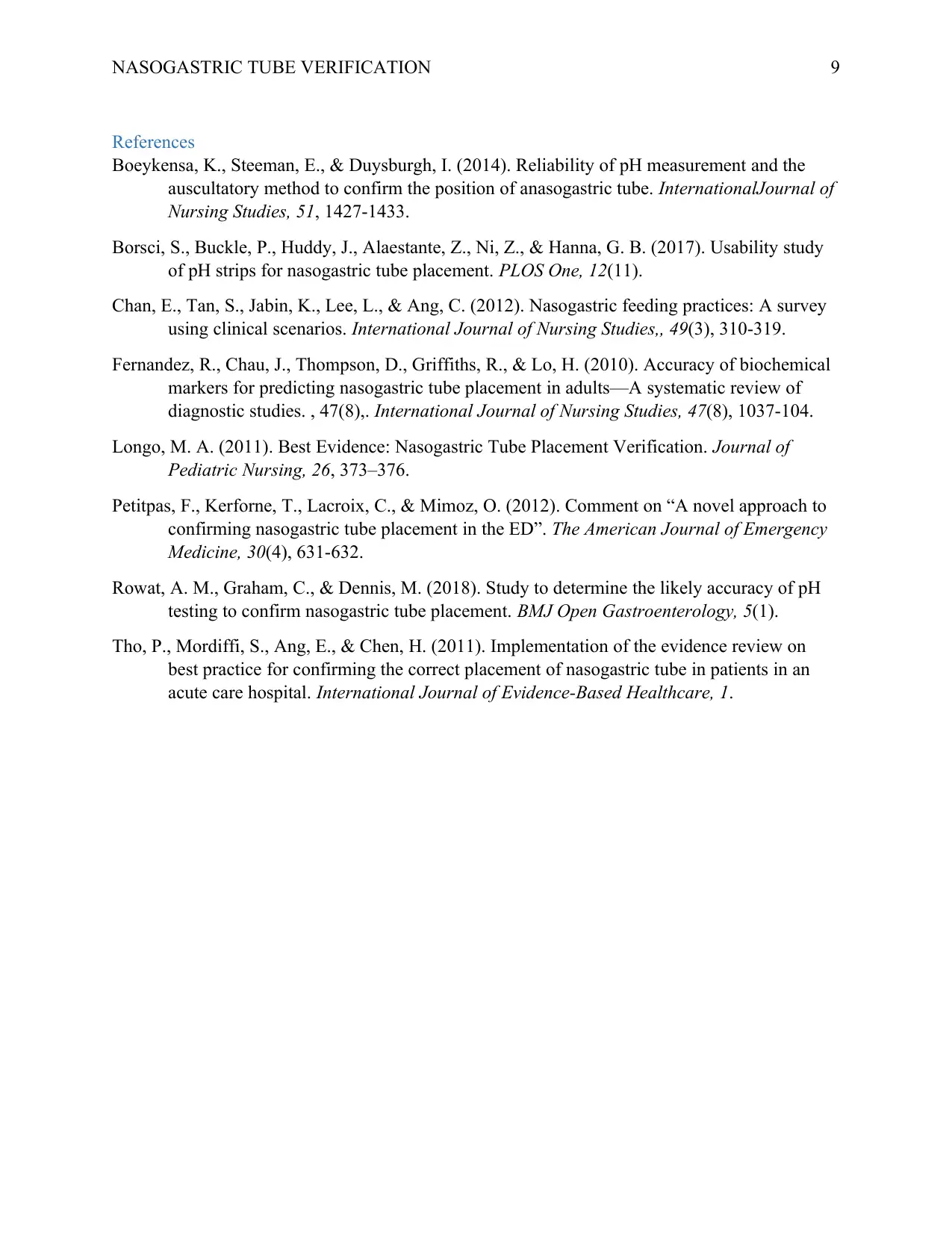
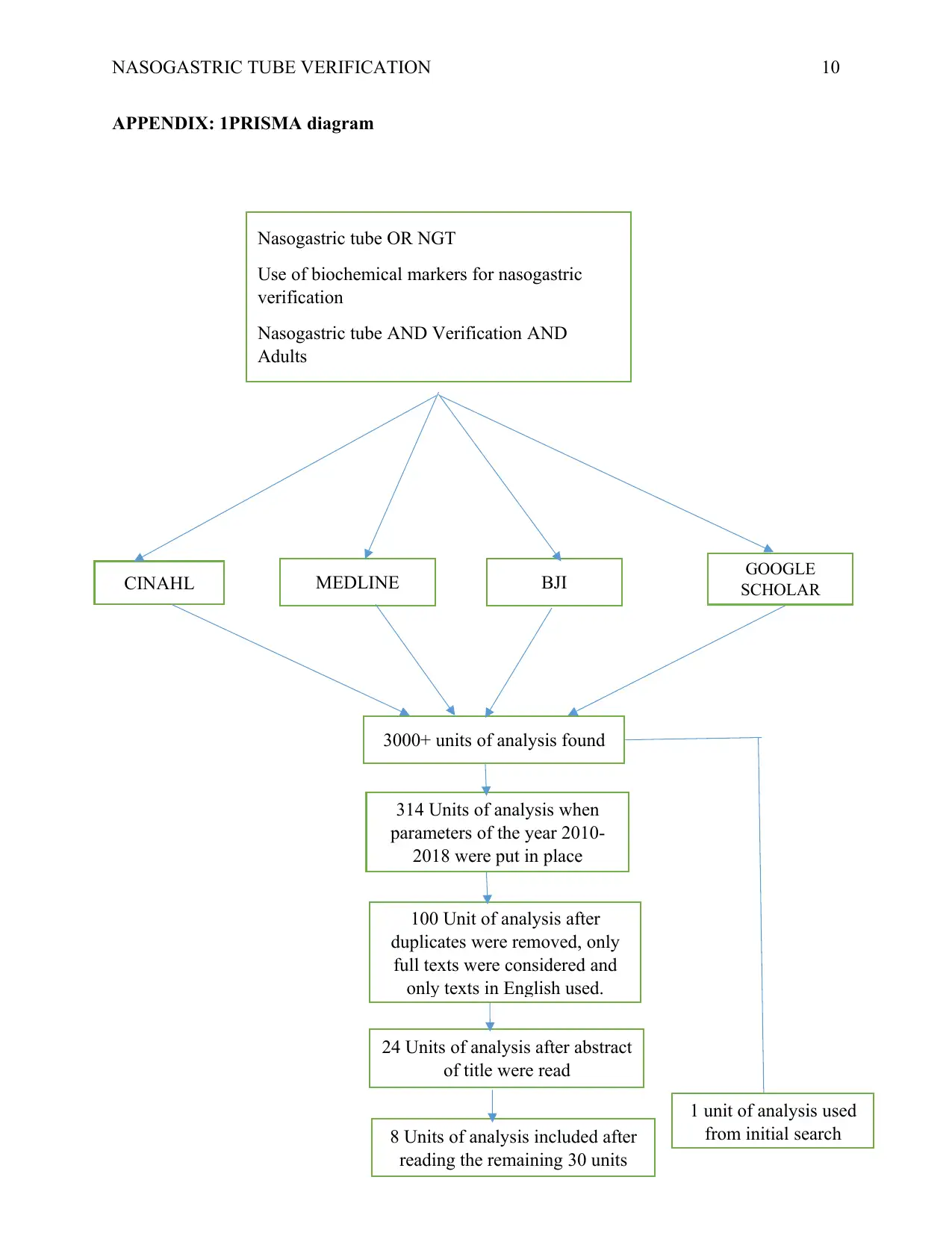
APPENDIX: 1PRISMA diagram
Nasogastric tube OR NGT
Use of biochemical markers for nasogastric
verification
Nasogastric tube AND Verification AND
Adults
CINAHL MEDLINE BJI GOOGLE
SCHOLAR
3000+ units of analysis found
314 Units of analysis when
parameters of the year 2010-
2018 were put in place
100 Unit of analysis after
duplicates were removed, only
full texts were considered and
only texts in English used.
24 Units of analysis after abstract
of title were read
8 Units of analysis included after
reading the remaining 30 units
1 unit of analysis used
from initial search
APPENDIX: 1PRISMA diagram
Nasogastric tube OR NGT
Use of biochemical markers for nasogastric
verification
Nasogastric tube AND Verification AND
Adults
CINAHL MEDLINE BJI GOOGLE
SCHOLAR
3000+ units of analysis found
314 Units of analysis when
parameters of the year 2010-
2018 were put in place
100 Unit of analysis after
duplicates were removed, only
full texts were considered and
only texts in English used.
24 Units of analysis after abstract
of title were read
8 Units of analysis included after
reading the remaining 30 units
1 unit of analysis used
from initial search
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





