Non Alcoholic Fatty Liver Disease
VerifiedAdded on 2023/01/19
|21
|5586
|60
AI Summary
This essay provides an in-depth analysis of Non Alcoholic Fatty Liver Disease (NAFLD), including its pathophysiology, diagnosis, and treatment. It explores the causes, risk factors, and symptoms of NAFLD, as well as the various treatment options available. The essay also discusses the role of diet and exercise in managing NAFLD.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NON ALCOHOLIC FATTY LIVER DISEASE
NON ALCOHOLIC FATTY LIVER DISEASE
Name of the Student:
Name of the University:
Author note:
NON ALCOHOLIC FATTY LIVER DISEASE
Name of the Student:
Name of the University:
Author note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1NON ALCOHOLIC FATTY LIVER DISEASE
Abstract
Non-Alcoholic Fatty Liver Disease (NAFLD) describes a range of hepatic complications
associated with inflammation and increased deposition of adipose tissue in the hepatic surface.
Due to its association with metabolic complications, NAFLD has been found to prevail
extensively across developed countries as well as developing countries. A number of metabolic,
nutritional, lifestyle and hormonal factors are associated with the underlying pathophysiology of
NAFLD. Considering the same, primary treatments for NAFLD aim to target changes in diet,
lifestyle as well as anthropometric characteristics. However, additional treatments in terms of
bariatric surgery, antioxidant therapy, incretin interventions and insulin sensitizing agents have
been found to be beneficial in NAFLD treatment.
Abstract
Non-Alcoholic Fatty Liver Disease (NAFLD) describes a range of hepatic complications
associated with inflammation and increased deposition of adipose tissue in the hepatic surface.
Due to its association with metabolic complications, NAFLD has been found to prevail
extensively across developed countries as well as developing countries. A number of metabolic,
nutritional, lifestyle and hormonal factors are associated with the underlying pathophysiology of
NAFLD. Considering the same, primary treatments for NAFLD aim to target changes in diet,
lifestyle as well as anthropometric characteristics. However, additional treatments in terms of
bariatric surgery, antioxidant therapy, incretin interventions and insulin sensitizing agents have
been found to be beneficial in NAFLD treatment.
2NON ALCOHOLIC FATTY LIVER DISEASE
Introduction
Natural History
Non-Alcoholic Fatty Liver Disease (NAFLD) is a collective term implying the
occurrence of a range of hepatic disease conditions found to inflict individuals who avoid or
engage in negligible alcohol consumption(Pappachan et al. 2017). Taking insights from the self-
explanatory nature of the name itself, NAFLD is characterized by excessive deposition of
excessive lipid and adipose tissues in the liver (Younossi et al. 2016). While the specific
pathologies underlying NAFLD occurrence is unknown, obesity is implicated to be a key
causative factor. Indeed, NAFLD has been observed extensively in patient who are overweight
or obese (Bellentani 2017).
Epidemiology
NAFLD has been found to exist highest in developed countries as well as in some
developing nations like the United States (30%), Middle East (32%), South America (30%), Asia
(27%), Europe (24%) and Africa (13%) (Pappachan et al. 2017).
Overview
NAFLD is at present one of the most widely prevalent diseases worldwide considering
the association of its pathology with obesity and the alarming rates at which obesity is increasing
in the global population. Lack of timely treatment and management of NAFLD results in the
acquisition of increased metabolic complications such cardiovascular complications and type 2
diabetes mellitus which further results in hepatic mortality (Adams et al. 2017). While specific
pathologies associated with NAFLD is still left to be discerned, metabolic malfunctioning
Introduction
Natural History
Non-Alcoholic Fatty Liver Disease (NAFLD) is a collective term implying the
occurrence of a range of hepatic disease conditions found to inflict individuals who avoid or
engage in negligible alcohol consumption(Pappachan et al. 2017). Taking insights from the self-
explanatory nature of the name itself, NAFLD is characterized by excessive deposition of
excessive lipid and adipose tissues in the liver (Younossi et al. 2016). While the specific
pathologies underlying NAFLD occurrence is unknown, obesity is implicated to be a key
causative factor. Indeed, NAFLD has been observed extensively in patient who are overweight
or obese (Bellentani 2017).
Epidemiology
NAFLD has been found to exist highest in developed countries as well as in some
developing nations like the United States (30%), Middle East (32%), South America (30%), Asia
(27%), Europe (24%) and Africa (13%) (Pappachan et al. 2017).
Overview
NAFLD is at present one of the most widely prevalent diseases worldwide considering
the association of its pathology with obesity and the alarming rates at which obesity is increasing
in the global population. Lack of timely treatment and management of NAFLD results in the
acquisition of increased metabolic complications such cardiovascular complications and type 2
diabetes mellitus which further results in hepatic mortality (Adams et al. 2017). While specific
pathologies associated with NAFLD is still left to be discerned, metabolic malfunctioning
3NON ALCOHOLIC FATTY LIVER DISEASE
associated with decreased insulin sensitivity and increased insulin resistance is estimated to be
the major causative factor, coupled with additional factors in hormonal, lifestyle, humoral and
genetic platforms (Targher et al. 2016). Treatments aimed at management of metabolic
complications such as, reductions of weight, dietary modifications and lifestyle alterations have
been considered to be most beneficial in addition to antioxidant consumption, incretin based
drugs, insulin sensitizers and bariatric surgery (Angulo et al. 2015). The following essay will
hence aim to explore the various pathologies, diagnostic steps and treatment procedures
associated with the management of NAFLD.
Pathophysiology
Causes
Abnormalities associated with metabolic functioning such as impaired glucose
intolerance, diabetes mellitus, cardiovascular diseases such as atherosclerosis, due to excessive
levels of adiposity, hyperglycemia, dislipidemia and hypertension are considered to be the
primary causative factors underlying NAFLD incidence in the individuals. However, the
presence of metabolic complications may not always be associated with NAFLD incidence an
hence, alternative factors are being explored for the purpose of evaluating the true pathologies
underlying the disease (Hardy et al. 2016). A key causative factor which may be implicated for
NAFLD incidence is oxidative stress which is a resultant of the imbalance in the functioning pro-
inflammatory components in the human body hence leading to increased levels of inflammation,
especially across hepatocytes responsible for metabolic processes (Pirola et al. 2015).
Additionally, intrinsic defense mechanisms to combat the body’s acquisition with disease
conditions and lifestyle stress may be implicated to be a causative factor underlying NAFLD
associated with decreased insulin sensitivity and increased insulin resistance is estimated to be
the major causative factor, coupled with additional factors in hormonal, lifestyle, humoral and
genetic platforms (Targher et al. 2016). Treatments aimed at management of metabolic
complications such as, reductions of weight, dietary modifications and lifestyle alterations have
been considered to be most beneficial in addition to antioxidant consumption, incretin based
drugs, insulin sensitizers and bariatric surgery (Angulo et al. 2015). The following essay will
hence aim to explore the various pathologies, diagnostic steps and treatment procedures
associated with the management of NAFLD.
Pathophysiology
Causes
Abnormalities associated with metabolic functioning such as impaired glucose
intolerance, diabetes mellitus, cardiovascular diseases such as atherosclerosis, due to excessive
levels of adiposity, hyperglycemia, dislipidemia and hypertension are considered to be the
primary causative factors underlying NAFLD incidence in the individuals. However, the
presence of metabolic complications may not always be associated with NAFLD incidence an
hence, alternative factors are being explored for the purpose of evaluating the true pathologies
underlying the disease (Hardy et al. 2016). A key causative factor which may be implicated for
NAFLD incidence is oxidative stress which is a resultant of the imbalance in the functioning pro-
inflammatory components in the human body hence leading to increased levels of inflammation,
especially across hepatocytes responsible for metabolic processes (Pirola et al. 2015).
Additionally, intrinsic defense mechanisms to combat the body’s acquisition with disease
conditions and lifestyle stress may be implicated to be a causative factor underlying NAFLD
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4NON ALCOHOLIC FATTY LIVER DISEASE
acquisition. Increased engagement with detrimental dietary and lifestyle disorders such as fatty
food consumption and sedentary lifestyle experiences coupled with psychological stresses as
well as disease infliction results in the hepatic stimulation of intrinsic defense mechanism such as
hepatic production of pro-inflammatory cytokines which results in hepatocyte damage and lipid
accumulation (Francque, van der Graaff and Kwanten 2016). Additional factors which may be
implicated as the causes of NAFLD include white blood cell inflammatory defense processes,
consequences of the metabolic products released by intestinal gut micro flora functioning and
hepatocyte necrosis or apoptosis caused due to detrimental disease conditions (Haas, Francque.
and Staels 2016).
Pathology
The exact cause of NAFLD is relatively unknown. However, obesity and associated
increased adiposity in the abdomen has been implicated to be a key causative factor. Increased
adiposity has been associated with emergence of metabolic complications such as insulin
resistance and diabetes, which results in altered lipid metabolism, increased circulatory levels of
lipids, endothelial fatty streak deposition and the progressive deposition of adipose tissues in the
hepatocytes (Rahmani et al. 2016). The following pathological processes have been associated
with NAFLD emergence.
Nutrition
The consumption of a diet rich in saturated fat, carbohydrates and deficient in dietary
fiber are considerd to be the primary pathologies underlying NAFLD emergence, especially the
high intake of sucrose and fructose associated excessive sugary food and soda consumption.
Such dietary patterns have been associated to exert a pre-biotic effect and hence often results in
intestinal dysbiosis - a major consequence of SIBO or small intestinal bacterial overgrowth
acquisition. Increased engagement with detrimental dietary and lifestyle disorders such as fatty
food consumption and sedentary lifestyle experiences coupled with psychological stresses as
well as disease infliction results in the hepatic stimulation of intrinsic defense mechanism such as
hepatic production of pro-inflammatory cytokines which results in hepatocyte damage and lipid
accumulation (Francque, van der Graaff and Kwanten 2016). Additional factors which may be
implicated as the causes of NAFLD include white blood cell inflammatory defense processes,
consequences of the metabolic products released by intestinal gut micro flora functioning and
hepatocyte necrosis or apoptosis caused due to detrimental disease conditions (Haas, Francque.
and Staels 2016).
Pathology
The exact cause of NAFLD is relatively unknown. However, obesity and associated
increased adiposity in the abdomen has been implicated to be a key causative factor. Increased
adiposity has been associated with emergence of metabolic complications such as insulin
resistance and diabetes, which results in altered lipid metabolism, increased circulatory levels of
lipids, endothelial fatty streak deposition and the progressive deposition of adipose tissues in the
hepatocytes (Rahmani et al. 2016). The following pathological processes have been associated
with NAFLD emergence.
Nutrition
The consumption of a diet rich in saturated fat, carbohydrates and deficient in dietary
fiber are considerd to be the primary pathologies underlying NAFLD emergence, especially the
high intake of sucrose and fructose associated excessive sugary food and soda consumption.
Such dietary patterns have been associated to exert a pre-biotic effect and hence often results in
intestinal dysbiosis - a major consequence of SIBO or small intestinal bacterial overgrowth
5NON ALCOHOLIC FATTY LIVER DISEASE
(Asgharpour et al. 2016). It is worthwhile to remember that the intestinal microflora exerts key
functions in terms of carbohydrate, sugar and dietary fiber metabolism resulting in production of
short chain fatty acids (SCFA) such as propionic acid and butyric acid. While such SCFA are
associated with anti-inflammatory and anti-carcinogenic functioning, excessive production duo
increased microbial colonies characteristic in intestinal dysbiosis may result in alterations of lipid
metabolism and hence, increased adipose accumulation in the hepatic tissue and the emergence
of NAFLD (Jump et al. 2016). The resultant hepatic enlargement due to increased adiposity has
been associated with non-alcoholic steatohepatitis (NASH) – that is hepatic inflammation and
hepatocyte auto-immune damage. The links between intestinal gut microflora and NAFLD
associated damage are further established due to the characteristic presence of tight epithelial
junctions within such patients (Estes et al. 2018). The microbial overgrowth discussed earlier
enter such junction and hence gain accessibility to release pro-inflammatory cytokines through
the systemic circulatory processes (Kirpich, Marsano and McClain 2015).
Hormones
The associated hormonal pathologies underlying NAFLD are often a resultant of
detrimental lifestyle and dietary patterns such as high fat and high sugar consumption which
further disrupts hormonal equilibrium. The increased consumption of such foods have been
implicated to yield positive effects in the limbic areas of the brain - the cerebral sections for
reward perception and hypothalamic functioning (Chishima et al. 2017). Detrimental lifestyle
and dietary behaviors result in continuous hypothalamic functioning in terms of ghrelin and
leptin production – hormones associated with appetite and satiety. Increased reward center
activation may exert overproduction of appetite stimulating ghrelin resulting in a conundrum of
over eating and the increased adipose accumulation in hepatic tissues (Norheim et al. 2017).
(Asgharpour et al. 2016). It is worthwhile to remember that the intestinal microflora exerts key
functions in terms of carbohydrate, sugar and dietary fiber metabolism resulting in production of
short chain fatty acids (SCFA) such as propionic acid and butyric acid. While such SCFA are
associated with anti-inflammatory and anti-carcinogenic functioning, excessive production duo
increased microbial colonies characteristic in intestinal dysbiosis may result in alterations of lipid
metabolism and hence, increased adipose accumulation in the hepatic tissue and the emergence
of NAFLD (Jump et al. 2016). The resultant hepatic enlargement due to increased adiposity has
been associated with non-alcoholic steatohepatitis (NASH) – that is hepatic inflammation and
hepatocyte auto-immune damage. The links between intestinal gut microflora and NAFLD
associated damage are further established due to the characteristic presence of tight epithelial
junctions within such patients (Estes et al. 2018). The microbial overgrowth discussed earlier
enter such junction and hence gain accessibility to release pro-inflammatory cytokines through
the systemic circulatory processes (Kirpich, Marsano and McClain 2015).
Hormones
The associated hormonal pathologies underlying NAFLD are often a resultant of
detrimental lifestyle and dietary patterns such as high fat and high sugar consumption which
further disrupts hormonal equilibrium. The increased consumption of such foods have been
implicated to yield positive effects in the limbic areas of the brain - the cerebral sections for
reward perception and hypothalamic functioning (Chishima et al. 2017). Detrimental lifestyle
and dietary behaviors result in continuous hypothalamic functioning in terms of ghrelin and
leptin production – hormones associated with appetite and satiety. Increased reward center
activation may exert overproduction of appetite stimulating ghrelin resulting in a conundrum of
over eating and the increased adipose accumulation in hepatic tissues (Norheim et al. 2017).
6NON ALCOHOLIC FATTY LIVER DISEASE
Likewise, increased adiposity may result in overstimulation of satiety inducing hormone leptin
which may further result in leptin sensitivity and the resultant overconsumption associated with
NAFLD acquisition. Further, excessive consumption of sugary foods result in the continuous
activation of anabolic hormones such as glucagon-like peptide, insulin-like growth factor and
insulin, resulting in increased lipid accumulation and altered metabolic processes (Dichtel et al.
2017).
Metabolic Complications
Metabolic complications associated with obesity are additional contributing pathologies
underlying NAFLD occurrence. Obesity results in metabolic complications such as hypertension,
hyperglycemia, hyperlipidemia – all of which contribute to the acquisition of hyperinsulinemia
(Katsiki, Mikhailidis and Mantzoros 2016). Considering the anabolic nature of insulin,
hyperinsulinemia and the resultant insulin resistance results in the increased lipolysis of
adipocytes and circulating levels of free fatty acids. Such resultant products undergo uptake by
hepatocytes hence leading to increased hepatic adiposity and inflammation underlying NAFLD
(Pappachan et al. 2017). Further, increased insulin resistance results in the reduction of plasma
adiponectin – a key cytokine with functions of body mass and fat reduction. Further, insulin
resistance has been associated with leptin resistance and the resultant contributory NAFLD
pathologies as explained earlier (Lonardo et al. 2015).
Genetics
The patatin-like phospholipase domain containing 3 (PNPLA3) gene has been implicated
to be the causative factor underlying the acquisition of the NAFLD and is a protein with
activities of both acylglycerol transcyclase and triacylglycerol lipase. A single nucleotide
polyphormism of PNPLA3 has been implicated to be a key causative factor underlying NAFLD
Likewise, increased adiposity may result in overstimulation of satiety inducing hormone leptin
which may further result in leptin sensitivity and the resultant overconsumption associated with
NAFLD acquisition. Further, excessive consumption of sugary foods result in the continuous
activation of anabolic hormones such as glucagon-like peptide, insulin-like growth factor and
insulin, resulting in increased lipid accumulation and altered metabolic processes (Dichtel et al.
2017).
Metabolic Complications
Metabolic complications associated with obesity are additional contributing pathologies
underlying NAFLD occurrence. Obesity results in metabolic complications such as hypertension,
hyperglycemia, hyperlipidemia – all of which contribute to the acquisition of hyperinsulinemia
(Katsiki, Mikhailidis and Mantzoros 2016). Considering the anabolic nature of insulin,
hyperinsulinemia and the resultant insulin resistance results in the increased lipolysis of
adipocytes and circulating levels of free fatty acids. Such resultant products undergo uptake by
hepatocytes hence leading to increased hepatic adiposity and inflammation underlying NAFLD
(Pappachan et al. 2017). Further, increased insulin resistance results in the reduction of plasma
adiponectin – a key cytokine with functions of body mass and fat reduction. Further, insulin
resistance has been associated with leptin resistance and the resultant contributory NAFLD
pathologies as explained earlier (Lonardo et al. 2015).
Genetics
The patatin-like phospholipase domain containing 3 (PNPLA3) gene has been implicated
to be the causative factor underlying the acquisition of the NAFLD and is a protein with
activities of both acylglycerol transcyclase and triacylglycerol lipase. A single nucleotide
polyphormism of PNPLA3 has been implicated to be a key causative factor underlying NAFLD
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NON ALCOHOLIC FATTY LIVER DISEASE
acquisition (Dongiovanni and Valenti 2016). Such genetic alterations have been found
extensively Hispanic populations – the community with highest incidence of NAFLD – and least
in African Americans - the community with lowest incidence of NAFLD. Mexicans in the
Hispanic community have been recorded with the highest rates of such gene abnormalities.
Likewise, a change to isoleucine from serine in codon have been found to yield protective effects
on hepatic inflammation and steatosis. Indeed, such protective gene alterations have been found
extensively in African American communities (Anstee, Seth and Day 2016).
Risk Factors
Individuals who are obese with greater levels of abdominal adiposity, the elderly and
those with additional metabolic conditions such as diabetes, hypertension and renal disorders are
considered to be in possession of a high risk of disease acquisition. Likewise, additional
physiological and metabolic complications which may increase susceptibility of NAFLD, such
as: hypothyroidism, hypopituitarism, sleep apnea, hypercholesterolemia, hypertriglyceridemia
and polycystic ovary syndrome (Van Wagner et al. 2016).
Signs and Symptoms
Common symptoms indicating NAFLD include: a persistent pain in the top right area of
the abdomen, uncontrolled weight levels and excessive feelings of fatigue, weakness and
tiredness. Additional complications which may arise due to prolonged lack of management
include: fluid retention in the abdomen (ascites), hepatic cancer, esophageal varices resulting in
rupturing, bleeding and hemorrhage, end stage liver failure and slurring of speech coupled with
altered mental condition (Panahi et al. 2017).
acquisition (Dongiovanni and Valenti 2016). Such genetic alterations have been found
extensively Hispanic populations – the community with highest incidence of NAFLD – and least
in African Americans - the community with lowest incidence of NAFLD. Mexicans in the
Hispanic community have been recorded with the highest rates of such gene abnormalities.
Likewise, a change to isoleucine from serine in codon have been found to yield protective effects
on hepatic inflammation and steatosis. Indeed, such protective gene alterations have been found
extensively in African American communities (Anstee, Seth and Day 2016).
Risk Factors
Individuals who are obese with greater levels of abdominal adiposity, the elderly and
those with additional metabolic conditions such as diabetes, hypertension and renal disorders are
considered to be in possession of a high risk of disease acquisition. Likewise, additional
physiological and metabolic complications which may increase susceptibility of NAFLD, such
as: hypothyroidism, hypopituitarism, sleep apnea, hypercholesterolemia, hypertriglyceridemia
and polycystic ovary syndrome (Van Wagner et al. 2016).
Signs and Symptoms
Common symptoms indicating NAFLD include: a persistent pain in the top right area of
the abdomen, uncontrolled weight levels and excessive feelings of fatigue, weakness and
tiredness. Additional complications which may arise due to prolonged lack of management
include: fluid retention in the abdomen (ascites), hepatic cancer, esophageal varices resulting in
rupturing, bleeding and hemorrhage, end stage liver failure and slurring of speech coupled with
altered mental condition (Panahi et al. 2017).
8NON ALCOHOLIC FATTY LIVER DISEASE
Diagnosis
Routine physical, abdominal and vital signs assessment may be performed. Specifically,
liver functioning enzyme tests, imaging and obtaining hepatic samples for liver biopsy may be
performed to explore the progression of NAFLD and possibilities of scar tissue proliferation
indicating cirrhosis (Hallsworth et al. 2015).
Non Invasive Testing
A variety of non-invasive tests such as serological testing coupled with thorough
evaluation of personal details of the patient, such as acquisition of current as well as past
medications, history of disease acquisition in the family, details of alcohol intake and detailed
patient screening including documentation of weight alterations and habits associated with
lifestyle and diet, are recommended for NAFLD diagnosis (El-Kader and El-Den Ashmawy
2015).
Biochemical Markers
Serology includes collection of lipid profile, glycosylated hemoglobin, creatinine,
Hepatitis C virus antibody and enzymatic or additional blood evaluation such as antitrypsin,
lysosomal activity, ceruloplasmin (Imajo et al. 2016).
Biopsy and Histology
Liver biopsy evaluation may further include examination of hepatic tissue for scar tissue
formation, cirrhosis, fibrosis, steatohepatitis and steatosis (Cassinotto et al. 2016).
Radiological Diagnosis
Procedures like ultrasonography, magnetic resonance imaging and computer tomography
are recommended radiological procedures for NAFLD diagnosis (Pappachan et al. 2017).
Diagnosis
Routine physical, abdominal and vital signs assessment may be performed. Specifically,
liver functioning enzyme tests, imaging and obtaining hepatic samples for liver biopsy may be
performed to explore the progression of NAFLD and possibilities of scar tissue proliferation
indicating cirrhosis (Hallsworth et al. 2015).
Non Invasive Testing
A variety of non-invasive tests such as serological testing coupled with thorough
evaluation of personal details of the patient, such as acquisition of current as well as past
medications, history of disease acquisition in the family, details of alcohol intake and detailed
patient screening including documentation of weight alterations and habits associated with
lifestyle and diet, are recommended for NAFLD diagnosis (El-Kader and El-Den Ashmawy
2015).
Biochemical Markers
Serology includes collection of lipid profile, glycosylated hemoglobin, creatinine,
Hepatitis C virus antibody and enzymatic or additional blood evaluation such as antitrypsin,
lysosomal activity, ceruloplasmin (Imajo et al. 2016).
Biopsy and Histology
Liver biopsy evaluation may further include examination of hepatic tissue for scar tissue
formation, cirrhosis, fibrosis, steatohepatitis and steatosis (Cassinotto et al. 2016).
Radiological Diagnosis
Procedures like ultrasonography, magnetic resonance imaging and computer tomography
are recommended radiological procedures for NAFLD diagnosis (Pappachan et al. 2017).
9NON ALCOHOLIC FATTY LIVER DISEASE
Treatment
A healthy diet low in fat may prove to be beneficial coupled with exercise in the
management of obesity associated NAFLD. Complex carbohydrates may be replace with greater
degree of simple carbohydrates to provide enough calories for hepatic function sustainability.
Lean and vegetarian proteins may be required to instigate tissue repair without further fat
deposition. Consumption of medium chain triglycerides may be considered since these undergo
rapid excretion without the need for hepatic absorption processes and hence, conserve hepatic
functioning (Chen et al. 2015).
Weight Loss, Dietary and Lifestyle Interventions
Considering that diet and lifestyle are primary factors associated with metabolic
complications and the resultant causative hormonal and intestinal pathologies underlying
NAFLD emergence, alterations in body weight, diet and lifestyle have been implicated to be the
key treatment recommendations (Pappachan et al. 2017). Consumption of a diet low in
carbohydrates, primarily sugars along with adherence to a balanced diet containing adequate
amounts of all nutrients have been expected to yield beneficial effects on biochemical and
metabolic complications associated with NAFLD (Zelber‐Sagi, Salomone and Mlynarsky 2017).
Adherence to adequate nutrient consumption, especially proteins have been implicated to aid in
reversal of hepatic damage and immunological abnormalities associated with NAFLD. As
researched by Cheng et al. (2017), the administration of exercise interventions, either with or
without dietary alterations have been found to exert beneficial enhancement of insulin sensitivity
and improved nutrient intake by hepatocytes resulting in increased hepatic tissue repair and
prevention of possible cirrhotic scar tissue growth.
Treatment
A healthy diet low in fat may prove to be beneficial coupled with exercise in the
management of obesity associated NAFLD. Complex carbohydrates may be replace with greater
degree of simple carbohydrates to provide enough calories for hepatic function sustainability.
Lean and vegetarian proteins may be required to instigate tissue repair without further fat
deposition. Consumption of medium chain triglycerides may be considered since these undergo
rapid excretion without the need for hepatic absorption processes and hence, conserve hepatic
functioning (Chen et al. 2015).
Weight Loss, Dietary and Lifestyle Interventions
Considering that diet and lifestyle are primary factors associated with metabolic
complications and the resultant causative hormonal and intestinal pathologies underlying
NAFLD emergence, alterations in body weight, diet and lifestyle have been implicated to be the
key treatment recommendations (Pappachan et al. 2017). Consumption of a diet low in
carbohydrates, primarily sugars along with adherence to a balanced diet containing adequate
amounts of all nutrients have been expected to yield beneficial effects on biochemical and
metabolic complications associated with NAFLD (Zelber‐Sagi, Salomone and Mlynarsky 2017).
Adherence to adequate nutrient consumption, especially proteins have been implicated to aid in
reversal of hepatic damage and immunological abnormalities associated with NAFLD. As
researched by Cheng et al. (2017), the administration of exercise interventions, either with or
without dietary alterations have been found to exert beneficial enhancement of insulin sensitivity
and improved nutrient intake by hepatocytes resulting in increased hepatic tissue repair and
prevention of possible cirrhotic scar tissue growth.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10NON ALCOHOLIC FATTY LIVER DISEASE
Antioxidant Administration
Considering increased inflammation and oxidative stress are major causative factors as
well as the resultant disruptive consequences underlying NAFLD disease condition, targeted
reversal or regulation of these key inflammatory processes have been implicated as an additional
beneficial treatment intervention (Del Ben et al. 2017). As researched by Aller (2015), external
administration of the tocopherol antioxidant such as Vitamin E have been associated to yield the
most beneficial effects in terms of hepatic improvements such as alleviation of hepatic steatosis,
lobular inflammation, ballooning and fibrous tissue proliferation.
Insulin Sensitizing Agents
Considering that the presence of insulin resistance has been implicated as the most
prevalent cause and consequence associated with NAFLD, administration of insulin sensitizing
agents can be considered as an additional beneficial treatment intervention (Bruckbauer et al.
2016).Of these, metformin administration and its resultant effects on NAFLD management has
been explored widely. As researched by Chalasani et al. (2018), increments in insulin sensitivity
and improve hepatic uptake of glucose are essential metformin mechanisms of actions which
have been found to alleviate detrimental NAFLD consequences such as fibrosis, ballooning and
inflammation. However, such insulin based interventions may prove to be beneficial in NAFLD
patients suffering from diabetes.
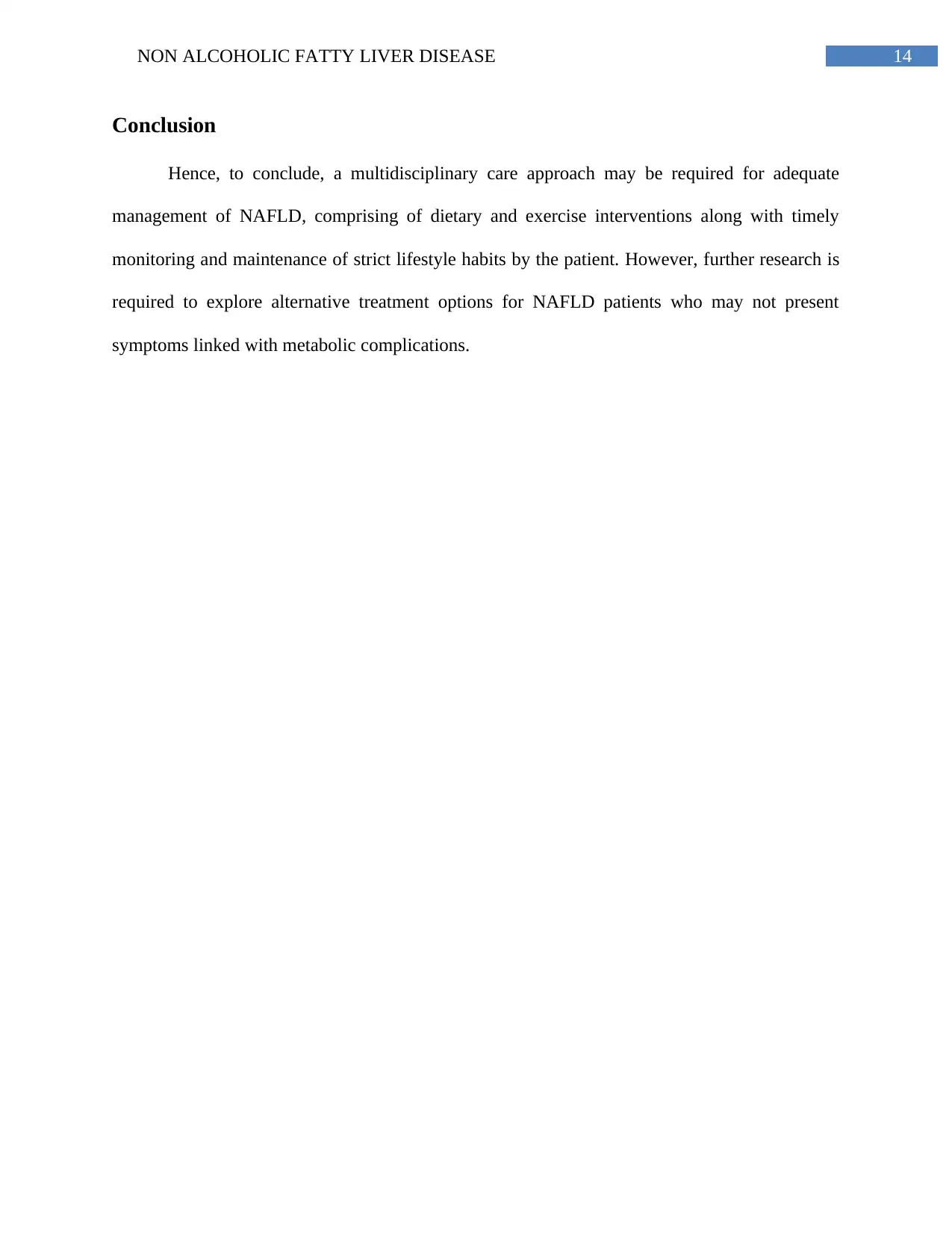
Bariatric Surgery
As researched by Kalinowski et al. (2017), In patients with severe and almost irreversible
complications of NAFLD have been implicated to encounter beneficial effects upon
administration of bariatric surgery, especially during simultaneous presence of NAFLD and
morbid obesity. Performance of bariatric surgery has been found to improve levels of hepatic
Antioxidant Administration
Considering increased inflammation and oxidative stress are major causative factors as
well as the resultant disruptive consequences underlying NAFLD disease condition, targeted
reversal or regulation of these key inflammatory processes have been implicated as an additional
beneficial treatment intervention (Del Ben et al. 2017). As researched by Aller (2015), external
administration of the tocopherol antioxidant such as Vitamin E have been associated to yield the
most beneficial effects in terms of hepatic improvements such as alleviation of hepatic steatosis,
lobular inflammation, ballooning and fibrous tissue proliferation.
Insulin Sensitizing Agents
Considering that the presence of insulin resistance has been implicated as the most
prevalent cause and consequence associated with NAFLD, administration of insulin sensitizing
agents can be considered as an additional beneficial treatment intervention (Bruckbauer et al.
2016).Of these, metformin administration and its resultant effects on NAFLD management has
been explored widely. As researched by Chalasani et al. (2018), increments in insulin sensitivity
and improve hepatic uptake of glucose are essential metformin mechanisms of actions which
have been found to alleviate detrimental NAFLD consequences such as fibrosis, ballooning and
inflammation. However, such insulin based interventions may prove to be beneficial in NAFLD
patients suffering from diabetes.
Bariatric Surgery
As researched by Kalinowski et al. (2017), In patients with severe and almost irreversible
complications of NAFLD have been implicated to encounter beneficial effects upon
administration of bariatric surgery, especially during simultaneous presence of NAFLD and
morbid obesity. Performance of bariatric surgery has been found to improve levels of hepatic
11NON ALCOHOLIC FATTY LIVER DISEASE
functioning enzymes such as alkaline phosphatase, ALT, AST and glutamyl transferase along
with improvements in NAFLD symptoms of inflammation, ballooning and fibrous tissue
development.
Incretin-based Therapeutic Interventions
As researched by Armstrong et al. (2016), in patients suffering from NAFLD as well as
type 2 diabetes mellitus, the administration of incretin based drugs have been found to be
particularly useful in disease management. Considering previously discussed role of glucagon-
like peptide 1 (GLP 1) in NAFLD pathogenesis, external administration of GLP inhibitors as
well as GLP-1 analogues have been found to mitigate the pathogenic effects of GLP-1 and
insulin resistance in type 2 diabetes mellitus and NAFLD by regulating the production of insulin
during mealtimes. Likewise, GLP-1 analogues have also been implicated to the yield additional
beneficial effects such as weight loss and hence, proves to be useful in the management of
NAFLD in morbidly obese patients (Rotman and Sanyal 2017).
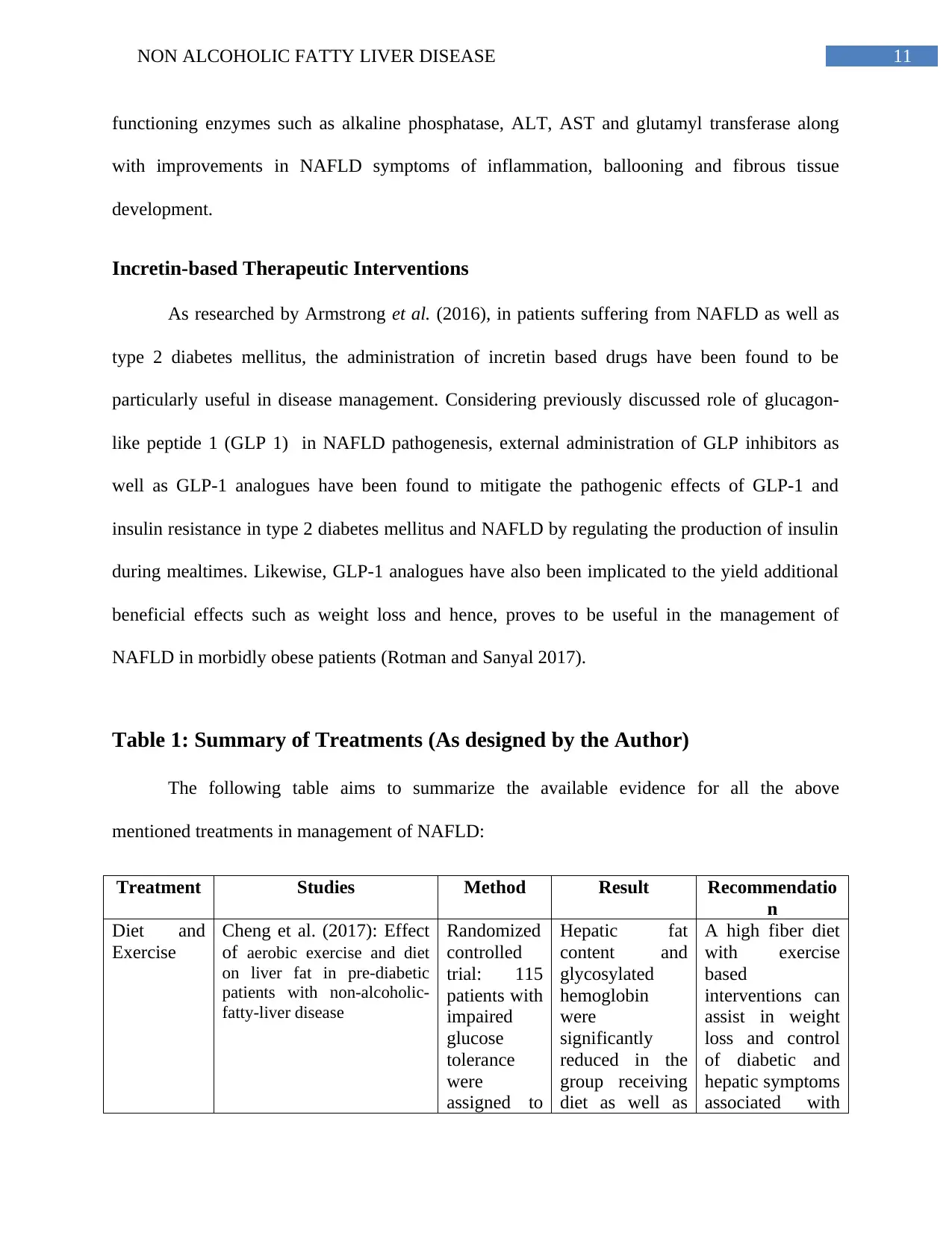
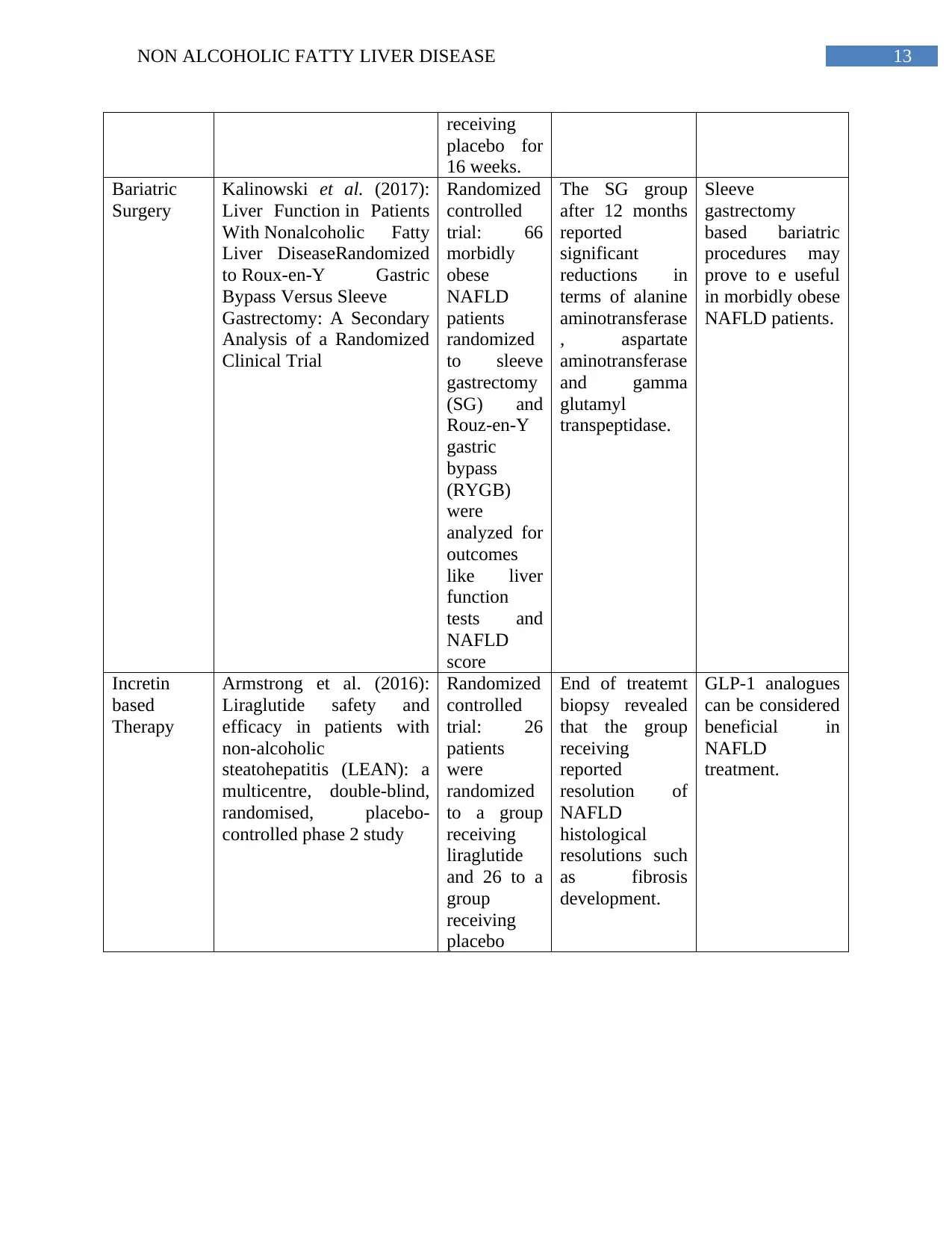
Table 1: Summary of Treatments (As designed by the Author)
The following table aims to summarize the available evidence for all the above
mentioned treatments in management of NAFLD:
Treatment Studies Method Result Recommendatio
n
Diet and
Exercise
Cheng et al. (2017): Effect
of aerobic exercise and diet
on liver fat in pre-diabetic
patients with non-alcoholic-
fatty-liver disease
Randomized
controlled
trial: 115
patients with
impaired
glucose
tolerance
were
assigned to
Hepatic fat
content and
glycosylated
hemoglobin
were
significantly
reduced in the
group receiving
diet as well as
A high fiber diet
with exercise
based
interventions can
assist in weight
loss and control
of diabetic and
hepatic symptoms
associated with
functioning enzymes such as alkaline phosphatase, ALT, AST and glutamyl transferase along
with improvements in NAFLD symptoms of inflammation, ballooning and fibrous tissue
development.
Incretin-based Therapeutic Interventions
As researched by Armstrong et al. (2016), in patients suffering from NAFLD as well as
type 2 diabetes mellitus, the administration of incretin based drugs have been found to be
particularly useful in disease management. Considering previously discussed role of glucagon-
like peptide 1 (GLP 1) in NAFLD pathogenesis, external administration of GLP inhibitors as
well as GLP-1 analogues have been found to mitigate the pathogenic effects of GLP-1 and
insulin resistance in type 2 diabetes mellitus and NAFLD by regulating the production of insulin
during mealtimes. Likewise, GLP-1 analogues have also been implicated to the yield additional
beneficial effects such as weight loss and hence, proves to be useful in the management of
NAFLD in morbidly obese patients (Rotman and Sanyal 2017).
Table 1: Summary of Treatments (As designed by the Author)
The following table aims to summarize the available evidence for all the above
mentioned treatments in management of NAFLD:
Treatment Studies Method Result Recommendatio
n
Diet and
Exercise
Cheng et al. (2017): Effect
of aerobic exercise and diet
on liver fat in pre-diabetic
patients with non-alcoholic-
fatty-liver disease
Randomized
controlled
trial: 115
patients with
impaired
glucose
tolerance
were
assigned to
Hepatic fat
content and
glycosylated
hemoglobin
were
significantly
reduced in the
group receiving
diet as well as
A high fiber diet
with exercise
based
interventions can
assist in weight
loss and control
of diabetic and
hepatic symptoms
associated with
12NON ALCOHOLIC FATTY LIVER DISEASE
groups
receiving
aerobic
exercise,
high fiber
diet,
exercise and
diet and no
intervention.
exercise as
compared to
group receiving
no intervention.
NAFLD.
Antioxidant
s
Aller et al. (2015): Effect of
silymarin plus vitamin E in
patients with non-alcoholic
fatty liver disease
Randomized
controlled
trial: 36
NAFLD
patients
were
randomized
to two
groups: One
group
receiving
silymarin
plus
Vitamin E
and a hypo-
calorific diet
and another
group
receiving
only the
hypocalorifi
c diet
Both groups
demonstrated
decrease in body
mass index,
gamma glutamyl
transferase, fatty
liver index and
NAFLD index.
Decrease in
ALT and AST
was observed in
the group
receiving only
diet.
A combined
treatment of low
calorie diet and
oral antioxidant
Vitamin E can be
beneficial in
combating
NAFLD
complications.
Insulin
Sensitizing
Agents:
Metformin
Chalasani et al. (2018):
Randomised clinical trial: a
leucine‐metformin‐
sildenafil combination
(NS‐0200) vs placebo in
patients with non‐alcoholic
fatty liver disease
Randomized
controlled
trial:
NAFLD
patients
were
randomized
to a group
receiving
medication
(1.1g
leucine and
0.5 g
metformin)
and a group
Hepatic fat was
found to be
reduced by
15.7% in
NAFLD
medications
receiving insulin
and leucine
medications.
Administration of
insulin sensitizing
agents may prove
to beneficial in
NAFLD
management.
groups
receiving
aerobic
exercise,
high fiber
diet,
exercise and
diet and no
intervention.
exercise as
compared to
group receiving
no intervention.
NAFLD.
Antioxidant
s
Aller et al. (2015): Effect of
silymarin plus vitamin E in
patients with non-alcoholic
fatty liver disease
Randomized
controlled
trial: 36
NAFLD
patients
were
randomized
to two
groups: One
group
receiving
silymarin
plus
Vitamin E
and a hypo-
calorific diet
and another
group
receiving
only the
hypocalorifi
c diet
Both groups
demonstrated
decrease in body
mass index,
gamma glutamyl
transferase, fatty
liver index and
NAFLD index.
Decrease in
ALT and AST
was observed in
the group
receiving only
diet.
A combined
treatment of low
calorie diet and
oral antioxidant
Vitamin E can be
beneficial in
combating
NAFLD
complications.
Insulin
Sensitizing
Agents:
Metformin
Chalasani et al. (2018):
Randomised clinical trial: a
leucine‐metformin‐
sildenafil combination
(NS‐0200) vs placebo in
patients with non‐alcoholic
fatty liver disease
Randomized
controlled
trial:
NAFLD
patients
were
randomized
to a group
receiving
medication
(1.1g
leucine and
0.5 g
metformin)
and a group
Hepatic fat was
found to be
reduced by
15.7% in
NAFLD
medications
receiving insulin
and leucine
medications.
Administration of
insulin sensitizing
agents may prove
to beneficial in
NAFLD
management.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13NON ALCOHOLIC FATTY LIVER DISEASE
receiving
placebo for
16 weeks.
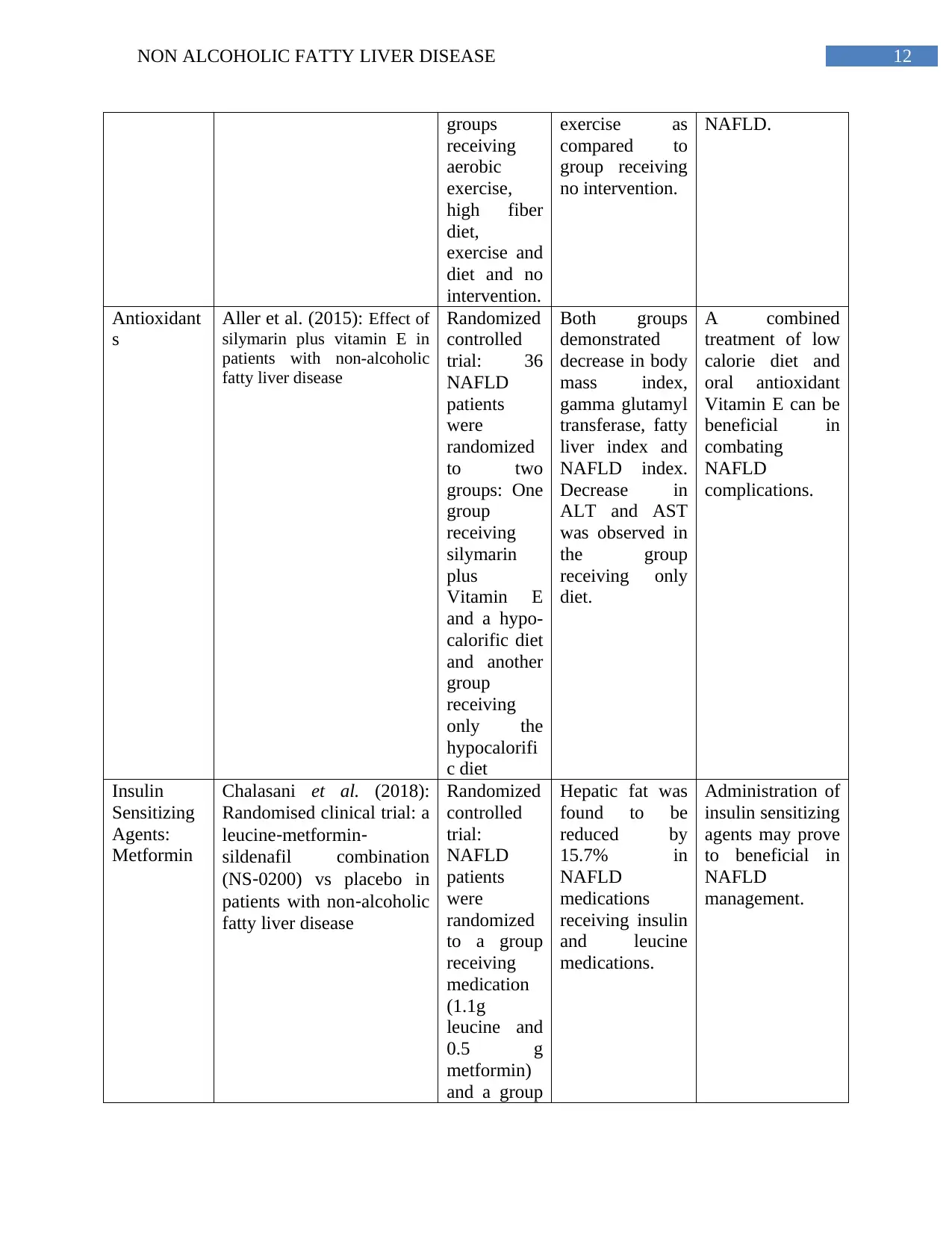
Bariatric
Surgery
Kalinowski et al. (2017):
Liver Function in Patients
With Nonalcoholic Fatty
Liver DiseaseRandomized
to Roux-en-Y Gastric
Bypass Versus Sleeve
Gastrectomy: A Secondary
Analysis of a Randomized
Clinical Trial
Randomized
controlled
trial: 66
morbidly
obese
NAFLD
patients
randomized
to sleeve
gastrectomy
(SG) and
Rouz-en-Y
gastric
bypass
(RYGB)
were
analyzed for
outcomes
like liver
function
tests and
NAFLD
score
The SG group
after 12 months
reported
significant
reductions in
terms of alanine
aminotransferase
, aspartate
aminotransferase
and gamma
glutamyl
transpeptidase.
Sleeve
gastrectomy
based bariatric
procedures may
prove to e useful
in morbidly obese
NAFLD patients.
Incretin
based
Therapy
Armstrong et al. (2016):
Liraglutide safety and
efficacy in patients with
non-alcoholic
steatohepatitis (LEAN): a
multicentre, double-blind,
randomised, placebo-
controlled phase 2 study
Randomized
controlled
trial: 26
patients
were
randomized
to a group
receiving
liraglutide
and 26 to a
group
receiving
placebo
End of treatemt
biopsy revealed
that the group
receiving
reported
resolution of
NAFLD
histological
resolutions such
as fibrosis
development.
GLP-1 analogues
can be considered
beneficial in
NAFLD
treatment.
receiving
placebo for
16 weeks.
Bariatric
Surgery
Kalinowski et al. (2017):
Liver Function in Patients
With Nonalcoholic Fatty
Liver DiseaseRandomized
to Roux-en-Y Gastric
Bypass Versus Sleeve
Gastrectomy: A Secondary
Analysis of a Randomized
Clinical Trial
Randomized
controlled
trial: 66
morbidly
obese
NAFLD
patients
randomized
to sleeve
gastrectomy
(SG) and
Rouz-en-Y
gastric
bypass
(RYGB)
were
analyzed for
outcomes
like liver
function
tests and
NAFLD
score
The SG group
after 12 months
reported
significant
reductions in
terms of alanine
aminotransferase
, aspartate
aminotransferase
and gamma
glutamyl
transpeptidase.
Sleeve
gastrectomy
based bariatric
procedures may
prove to e useful
in morbidly obese
NAFLD patients.
Incretin
based
Therapy
Armstrong et al. (2016):
Liraglutide safety and
efficacy in patients with
non-alcoholic
steatohepatitis (LEAN): a
multicentre, double-blind,
randomised, placebo-
controlled phase 2 study
Randomized
controlled
trial: 26
patients
were
randomized
to a group
receiving
liraglutide
and 26 to a
group
receiving
placebo
End of treatemt
biopsy revealed
that the group
receiving
reported
resolution of
NAFLD
histological
resolutions such
as fibrosis
development.
GLP-1 analogues
can be considered
beneficial in
NAFLD
treatment.
14NON ALCOHOLIC FATTY LIVER DISEASE
Conclusion
Hence, to conclude, a multidisciplinary care approach may be required for adequate
management of NAFLD, comprising of dietary and exercise interventions along with timely
monitoring and maintenance of strict lifestyle habits by the patient. However, further research is
required to explore alternative treatment options for NAFLD patients who may not present
symptoms linked with metabolic complications.
Conclusion
Hence, to conclude, a multidisciplinary care approach may be required for adequate
management of NAFLD, comprising of dietary and exercise interventions along with timely
monitoring and maintenance of strict lifestyle habits by the patient. However, further research is
required to explore alternative treatment options for NAFLD patients who may not present
symptoms linked with metabolic complications.
15NON ALCOHOLIC FATTY LIVER DISEASE
References
Adams, L.A., Anstee, Q.M., Tilg, H. and Targher, G., 2017. Non-alcoholic fatty liver disease and
its relationship with cardiovascular disease and other extrahepatic diseases. Gut, 66(6), pp.1138-
1153.
Aller, R., Izaola, O., Gómez, S., Tafur, C., Gonzalez, G., Berroa, E., Mora, N., González, J.M.
and De Luis, D.A., 2015. Effect of silymarin plus vitamin E in patients with non-alcoholic fatty
liver disease. A randomized clinical pilot study. Eur Rev Med Pharmacol Sci, 19(16), pp.3118-
24.
Angulo, P., Kleiner, D.E., Dam-Larsen, S., Adams, L.A., Bjornsson, E.S.,
Charatcharoenwitthaya, P., Mills, P.R., Keach, J.C., Lafferty, H.D., Stahler, A. and Haflidadottir,
S., 2015. Liver fibrosis, but no other histologic features, is associated with long-term outcomes
of patients with nonalcoholic fatty liver disease. Gastroenterology, 149(2), pp.389-397.
Anstee, Q.M., Seth, D. and Day, C.P., 2016. Genetic factors that affect risk of alcoholic and
nonalcoholic fatty liver disease. Gastroenterology, 150(8), pp.1728-1744.
Armstrong, M.J., Gaunt, P., Aithal, G.P., Barton, D., Hull, D., Parker, R., Hazlehurst, J.M., Guo,
K., Abouda, G., Aldersley, M.A. and Stocken, D., 2016. Liraglutide safety and efficacy in
patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised,
placebo-controlled phase 2 study. The Lancet, 387(10019), pp.679-690.
Asgharpour, A., Cazanave, S.C., Pacana, T., Seneshaw, M., Vincent, R., Banini, B.A., Kumar,
D.P., Daita, K., Min, H.K., Mirshahi, F. and Bedossa, P., 2016. A diet-induced animal model of
References
Adams, L.A., Anstee, Q.M., Tilg, H. and Targher, G., 2017. Non-alcoholic fatty liver disease and
its relationship with cardiovascular disease and other extrahepatic diseases. Gut, 66(6), pp.1138-
1153.
Aller, R., Izaola, O., Gómez, S., Tafur, C., Gonzalez, G., Berroa, E., Mora, N., González, J.M.
and De Luis, D.A., 2015. Effect of silymarin plus vitamin E in patients with non-alcoholic fatty
liver disease. A randomized clinical pilot study. Eur Rev Med Pharmacol Sci, 19(16), pp.3118-
24.
Angulo, P., Kleiner, D.E., Dam-Larsen, S., Adams, L.A., Bjornsson, E.S.,
Charatcharoenwitthaya, P., Mills, P.R., Keach, J.C., Lafferty, H.D., Stahler, A. and Haflidadottir,
S., 2015. Liver fibrosis, but no other histologic features, is associated with long-term outcomes
of patients with nonalcoholic fatty liver disease. Gastroenterology, 149(2), pp.389-397.
Anstee, Q.M., Seth, D. and Day, C.P., 2016. Genetic factors that affect risk of alcoholic and
nonalcoholic fatty liver disease. Gastroenterology, 150(8), pp.1728-1744.
Armstrong, M.J., Gaunt, P., Aithal, G.P., Barton, D., Hull, D., Parker, R., Hazlehurst, J.M., Guo,
K., Abouda, G., Aldersley, M.A. and Stocken, D., 2016. Liraglutide safety and efficacy in
patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised,
placebo-controlled phase 2 study. The Lancet, 387(10019), pp.679-690.
Asgharpour, A., Cazanave, S.C., Pacana, T., Seneshaw, M., Vincent, R., Banini, B.A., Kumar,
D.P., Daita, K., Min, H.K., Mirshahi, F. and Bedossa, P., 2016. A diet-induced animal model of
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16NON ALCOHOLIC FATTY LIVER DISEASE
non-alcoholic fatty liver disease and hepatocellular cancer. Journal of hepatology, 65(3), pp.579-
588.
Bellentani, S., 2017. The epidemiology of non‐alcoholic fatty liver disease. Liver
international, 37, pp.81-84.
Bruckbauer, A., Banerjee, J., Fu, L., Li, F., Cao, Q., Cui, X., Wu, R., Shi, H., Xue, B. and Zemel,
M.B., 2016. A combination of leucine, metformin, and sildenafil treats nonalcoholic fatty liver
disease and steatohepatitis in mice. International journal of hepatology, 2016.
Cassinotto, C., Boursier, J., de Lédinghen, V., Lebigot, J., Lapuyade, B., Cales, P., Hiriart, J.B.,
Michalak, S., Bail, B.L., Cartier, V. and Mouries, A., 2016. Liver stiffness in nonalcoholic fatty
liver disease: A comparison of supersonic shear imaging, FibroScan, and ARFI with liver
biopsy. Hepatology, 63(6), pp.1817-1827.
Chalasani, N., Vuppalanchi, R., Rinella, M., Middleton, M.S., Siddiqui, M.S., Barritt IV, A.S.,
Kolterman, O., Flores, O., Alonso, C., Iruarrizaga‐Lejarreta, M. and Gil‐Redondo, R., 2018.
Randomised clinical trial: a leucine‐metformin‐sildenafil combination (NS‐0200) vs placebo in
patients with non‐alcoholic fatty liver disease. Alimentary pharmacology & therapeutics, 47(12),
pp.1639-1651.
Chen, S., Zhao, X., Ran, L., Wan, J., Wang, X., Qin, Y., Shu, F., Gao, Y., Yuan, L., Zhang, Q.
and Mi, M., 2015. Resveratrol improves insulin resistance, glucose and lipid metabolism in
patients with non-alcoholic fatty liver disease: a randomized controlled trial. Digestive and Liver
Disease, 47(3), pp.226-232.
non-alcoholic fatty liver disease and hepatocellular cancer. Journal of hepatology, 65(3), pp.579-
588.
Bellentani, S., 2017. The epidemiology of non‐alcoholic fatty liver disease. Liver
international, 37, pp.81-84.
Bruckbauer, A., Banerjee, J., Fu, L., Li, F., Cao, Q., Cui, X., Wu, R., Shi, H., Xue, B. and Zemel,
M.B., 2016. A combination of leucine, metformin, and sildenafil treats nonalcoholic fatty liver
disease and steatohepatitis in mice. International journal of hepatology, 2016.
Cassinotto, C., Boursier, J., de Lédinghen, V., Lebigot, J., Lapuyade, B., Cales, P., Hiriart, J.B.,
Michalak, S., Bail, B.L., Cartier, V. and Mouries, A., 2016. Liver stiffness in nonalcoholic fatty
liver disease: A comparison of supersonic shear imaging, FibroScan, and ARFI with liver
biopsy. Hepatology, 63(6), pp.1817-1827.
Chalasani, N., Vuppalanchi, R., Rinella, M., Middleton, M.S., Siddiqui, M.S., Barritt IV, A.S.,
Kolterman, O., Flores, O., Alonso, C., Iruarrizaga‐Lejarreta, M. and Gil‐Redondo, R., 2018.
Randomised clinical trial: a leucine‐metformin‐sildenafil combination (NS‐0200) vs placebo in
patients with non‐alcoholic fatty liver disease. Alimentary pharmacology & therapeutics, 47(12),
pp.1639-1651.
Chen, S., Zhao, X., Ran, L., Wan, J., Wang, X., Qin, Y., Shu, F., Gao, Y., Yuan, L., Zhang, Q.
and Mi, M., 2015. Resveratrol improves insulin resistance, glucose and lipid metabolism in
patients with non-alcoholic fatty liver disease: a randomized controlled trial. Digestive and Liver
Disease, 47(3), pp.226-232.
17NON ALCOHOLIC FATTY LIVER DISEASE
Cheng, S., Ge, J., Zhao, C., Le, S., Yang, Y., Ke, D., Wu, N., Tan, X., Zhang, X., Du, X. and
Sun, J., 2017. Effect of aerobic exercise and diet on liver fat in pre-diabetic patients with non-
alcoholic-fatty-liver-disease: A randomized controlled trial. Scientific reports, 7(1), p.15952.
Chishima, S., Kogiso, T., Matsushita, N., Hashimoto, E. and Tokushige, K., 2017. The
relationship between the growth hormone/insulin-like growth factor system and the histological
features of nonalcoholic fatty liver disease. Internal Medicine, 56(5), pp.473-480.
Del Ben, M., Polimeni, L., Baratta, F., Pastori, D. and Angelico, F., 2017. The role of
nutraceuticals for the treatment of non‐alcoholic fatty liver disease. British journal of clinical
pharmacology, 83(1), pp.88-95.
Dichtel, L.E., Corey, K.E., Misdraji, J., Bredella, M.A., Schorr, M., Osganian, S.A., Young, B.J.,
Sung, J.C. and Miller, K.K., 2017. The association between IGF-1 levels and the histologic
severity of nonalcoholic fatty liver disease. Clinical and translational gastroenterology, 8(1),
p.e217.
Dongiovanni, P. and Valenti, L., 2016. Genetics of nonalcoholic fatty liver
disease. Metabolism, 65(8), pp.1026-1037.
El-Kader, S.M.A. and El-Den Ashmawy, E.M.S., 2015. Non-alcoholic fatty liver disease: The
diagnosis and management. World journal of hepatology, 7(6), p.846.
Estes, C., Razavi, H., Loomba, R., Younossi, Z. and Sanyal, A.J., 2018. Modeling the epidemic
of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of
disease. Hepatology, 67(1), pp.123-133.
Cheng, S., Ge, J., Zhao, C., Le, S., Yang, Y., Ke, D., Wu, N., Tan, X., Zhang, X., Du, X. and
Sun, J., 2017. Effect of aerobic exercise and diet on liver fat in pre-diabetic patients with non-
alcoholic-fatty-liver-disease: A randomized controlled trial. Scientific reports, 7(1), p.15952.
Chishima, S., Kogiso, T., Matsushita, N., Hashimoto, E. and Tokushige, K., 2017. The
relationship between the growth hormone/insulin-like growth factor system and the histological
features of nonalcoholic fatty liver disease. Internal Medicine, 56(5), pp.473-480.
Del Ben, M., Polimeni, L., Baratta, F., Pastori, D. and Angelico, F., 2017. The role of
nutraceuticals for the treatment of non‐alcoholic fatty liver disease. British journal of clinical
pharmacology, 83(1), pp.88-95.
Dichtel, L.E., Corey, K.E., Misdraji, J., Bredella, M.A., Schorr, M., Osganian, S.A., Young, B.J.,
Sung, J.C. and Miller, K.K., 2017. The association between IGF-1 levels and the histologic
severity of nonalcoholic fatty liver disease. Clinical and translational gastroenterology, 8(1),
p.e217.
Dongiovanni, P. and Valenti, L., 2016. Genetics of nonalcoholic fatty liver
disease. Metabolism, 65(8), pp.1026-1037.
El-Kader, S.M.A. and El-Den Ashmawy, E.M.S., 2015. Non-alcoholic fatty liver disease: The
diagnosis and management. World journal of hepatology, 7(6), p.846.
Estes, C., Razavi, H., Loomba, R., Younossi, Z. and Sanyal, A.J., 2018. Modeling the epidemic
of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of
disease. Hepatology, 67(1), pp.123-133.
18NON ALCOHOLIC FATTY LIVER DISEASE
Francque, S.M., van der Graaff, D. and Kwanten, W.J., 2016. Non-alcoholic fatty liver disease
and cardiovascular risk: Pathophysiological mechanisms and implications. Journal of
hepatology, 65(2), pp.425-443.
Haas, J.T., Francque, S. and Staels, B., 2016. Pathophysiology and mechanisms of nonalcoholic
fatty liver disease. Annual review of physiology, 78, pp.181-205.
Hallsworth, K., Thoma, C., Hollingsworth, K.G., Cassidy, S., Anstee, Q.M., Day, C.P. and
Trenell, M.I., 2015. Modified high-intensity interval training reduces liver fat and improves
cardiac function in non-alcoholic fatty liver disease: a randomized controlled trial. Clinical
science, 129(12), pp.1097-1105.
Hardy, T., Oakley, F., Anstee, Q.M. and Day, C.P., 2016. Nonalcoholic fatty liver disease:
pathogenesis and disease spectrum. Annual Review of Pathology: Mechanisms of Disease, 11,
pp.451-496.
Imajo, K., Kessoku, T., Honda, Y., Tomeno, W., Ogawa, Y., Mawatari, H., Fujita, K., Yoneda,
M., Taguri, M., Hyogo, H. and Sumida, Y., 2016. Magnetic resonance imaging more accurately
classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient
elastography. Gastroenterology, 150(3), pp.626-637.
Jump, D.B., Depner, C.M., Tripathy, S. and Lytle, K.A., 2016. Impact of dietary fat on the
development of non-alcoholic fatty liver disease in Ldlr−/− mice. Proceedings of the Nutrition
Society, 75(1), pp.1-9.
Kalinowski, P., Paluszkiewicz, R., Ziarkiewicz-Wróblewska, B., Wróblewski, T., Remiszewski,
P., Grodzicki, M. and Krawczyk, M., 2017. Liver function in patients with nonalcoholic fatty
Francque, S.M., van der Graaff, D. and Kwanten, W.J., 2016. Non-alcoholic fatty liver disease
and cardiovascular risk: Pathophysiological mechanisms and implications. Journal of
hepatology, 65(2), pp.425-443.
Haas, J.T., Francque, S. and Staels, B., 2016. Pathophysiology and mechanisms of nonalcoholic
fatty liver disease. Annual review of physiology, 78, pp.181-205.
Hallsworth, K., Thoma, C., Hollingsworth, K.G., Cassidy, S., Anstee, Q.M., Day, C.P. and
Trenell, M.I., 2015. Modified high-intensity interval training reduces liver fat and improves
cardiac function in non-alcoholic fatty liver disease: a randomized controlled trial. Clinical
science, 129(12), pp.1097-1105.
Hardy, T., Oakley, F., Anstee, Q.M. and Day, C.P., 2016. Nonalcoholic fatty liver disease:
pathogenesis and disease spectrum. Annual Review of Pathology: Mechanisms of Disease, 11,
pp.451-496.
Imajo, K., Kessoku, T., Honda, Y., Tomeno, W., Ogawa, Y., Mawatari, H., Fujita, K., Yoneda,
M., Taguri, M., Hyogo, H. and Sumida, Y., 2016. Magnetic resonance imaging more accurately
classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient
elastography. Gastroenterology, 150(3), pp.626-637.
Jump, D.B., Depner, C.M., Tripathy, S. and Lytle, K.A., 2016. Impact of dietary fat on the
development of non-alcoholic fatty liver disease in Ldlr−/− mice. Proceedings of the Nutrition
Society, 75(1), pp.1-9.
Kalinowski, P., Paluszkiewicz, R., Ziarkiewicz-Wróblewska, B., Wróblewski, T., Remiszewski,
P., Grodzicki, M. and Krawczyk, M., 2017. Liver function in patients with nonalcoholic fatty
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
19NON ALCOHOLIC FATTY LIVER DISEASE
liver disease randomized to Roux-en-Y gastric bypass versus sleeve gastrectomy: a secondary
analysis of a randomized clinical trial. Annals of surgery, 266(5), pp.738-745.
Katsiki, N., Mikhailidis, D.P. and Mantzoros, C.S., 2016. Non-alcoholic fatty liver disease and
dyslipidemia: an update. Metabolism, 65(8), pp.1109-1123.
Kirpich, I.A., Marsano, L.S. and McClain, C.J., 2015. Gut–liver axis, nutrition, and non-
alcoholic fatty liver disease. Clinical biochemistry, 48(13-14), pp.923-930.
Lonardo, A., Ballestri, S., Marchesini, G., Angulo, P. and Loria, P., 2015. Nonalcoholic fatty
liver disease: a precursor of the metabolic syndrome. Digestive and Liver Disease, 47(3), pp.181-
190.
Norheim, F., Hui, S.T., Kulahcioglu, E., Mehrabian, M., Cantor, R.M., Pan, C., Parks, B.W. and
Lusis, A.J., 2017. Genetic and hormonal control of hepatic steatosis in female and male
mice. Journal of lipid research, 58(1), pp.178-187.
Panahi, Y., Kianpour, P., Mohtashami, R., Jafari, R., Simental-Mendía, L.E. and Sahebkar, A.,
2017. Efficacy and safety of phytosomal curcumin in non-alcoholic fatty liver disease: a
randomized controlled trial. Drug research, 67(04), pp.244-251.
Pappachan, J.M., Babu, S., Krishnan, B. and Ravindran, N.C., 2017. Non-alcoholic fatty liver
disease: a clinical update. Journal of clinical and translational hepatology, 5(4), p.384.
Pirola, C.J., Gianotti, T.F., Castaño, G.O., Mallardi, P., San Martino, J., Ledesma, M.M.G.L.,
Flichman, D., Mirshahi, F., Sanyal, A.J. and Sookoian, S., 2015. Circulating microRNA
signature in non-alcoholic fatty liver disease: from serum non-coding RNAs to liver histology
and disease pathogenesis. Gut, 64(5), pp.800-812.
liver disease randomized to Roux-en-Y gastric bypass versus sleeve gastrectomy: a secondary
analysis of a randomized clinical trial. Annals of surgery, 266(5), pp.738-745.
Katsiki, N., Mikhailidis, D.P. and Mantzoros, C.S., 2016. Non-alcoholic fatty liver disease and
dyslipidemia: an update. Metabolism, 65(8), pp.1109-1123.
Kirpich, I.A., Marsano, L.S. and McClain, C.J., 2015. Gut–liver axis, nutrition, and non-
alcoholic fatty liver disease. Clinical biochemistry, 48(13-14), pp.923-930.
Lonardo, A., Ballestri, S., Marchesini, G., Angulo, P. and Loria, P., 2015. Nonalcoholic fatty
liver disease: a precursor of the metabolic syndrome. Digestive and Liver Disease, 47(3), pp.181-
190.
Norheim, F., Hui, S.T., Kulahcioglu, E., Mehrabian, M., Cantor, R.M., Pan, C., Parks, B.W. and
Lusis, A.J., 2017. Genetic and hormonal control of hepatic steatosis in female and male
mice. Journal of lipid research, 58(1), pp.178-187.
Panahi, Y., Kianpour, P., Mohtashami, R., Jafari, R., Simental-Mendía, L.E. and Sahebkar, A.,
2017. Efficacy and safety of phytosomal curcumin in non-alcoholic fatty liver disease: a
randomized controlled trial. Drug research, 67(04), pp.244-251.
Pappachan, J.M., Babu, S., Krishnan, B. and Ravindran, N.C., 2017. Non-alcoholic fatty liver
disease: a clinical update. Journal of clinical and translational hepatology, 5(4), p.384.
Pirola, C.J., Gianotti, T.F., Castaño, G.O., Mallardi, P., San Martino, J., Ledesma, M.M.G.L.,
Flichman, D., Mirshahi, F., Sanyal, A.J. and Sookoian, S., 2015. Circulating microRNA
signature in non-alcoholic fatty liver disease: from serum non-coding RNAs to liver histology
and disease pathogenesis. Gut, 64(5), pp.800-812.
20NON ALCOHOLIC FATTY LIVER DISEASE
Rahmani, S., Asgary, S., Askari, G., Keshvari, M., Hatamipour, M., Feizi, A. and Sahebkar, A.,
2016. Treatment of non‐alcoholic fatty liver disease with curcumin: A randomized placebo‐
controlled trial. Phytotherapy Research, 30(9), pp.1540-1548.
Rotman, Y. and Sanyal, A.J., 2017. Current and upcoming pharmacotherapy for non-alcoholic
fatty liver disease. Gut, 66(1), pp.180-190.
Targher, G., Byrne, C.D., Lonardo, A., Zoppini, G. and Barbui, C., 2016. Non-alcoholic fatty
liver disease and risk of incident cardiovascular disease: a meta-analysis. Journal of
hepatology, 65(3), pp.589-600.
Van Wagner, L.B., Koppe, S.W., Brunt, E.M., Gottstein, J., Gardikiotes, K., Green, R.M. and
Rinella, M.E., 2016. Pentoxifylline for the treatment of non-alcoholic steatohepatitis: a
randomized controlled trial. Annals of hepatology, 10(3), pp.277-286.
Younossi, Z.M., Koenig, A.B., Abdelatif, D., Fazel, Y., Henry, L. and Wymer, M., 2016. Global
epidemiology of nonalcoholic fatty liver disease—meta‐analytic assessment of prevalence,
incidence, and outcomes. Hepatology, 64(1), pp.73-84.
Zelber‐Sagi, S., Salomone, F. and Mlynarsky, L., 2017. The Mediterranean dietary pattern as the
diet of choice for non‐alcoholic fatty liver disease: Evidence and plausible mechanisms. Liver
International, 37(7), pp.936-949.
Rahmani, S., Asgary, S., Askari, G., Keshvari, M., Hatamipour, M., Feizi, A. and Sahebkar, A.,
2016. Treatment of non‐alcoholic fatty liver disease with curcumin: A randomized placebo‐
controlled trial. Phytotherapy Research, 30(9), pp.1540-1548.
Rotman, Y. and Sanyal, A.J., 2017. Current and upcoming pharmacotherapy for non-alcoholic
fatty liver disease. Gut, 66(1), pp.180-190.
Targher, G., Byrne, C.D., Lonardo, A., Zoppini, G. and Barbui, C., 2016. Non-alcoholic fatty
liver disease and risk of incident cardiovascular disease: a meta-analysis. Journal of
hepatology, 65(3), pp.589-600.
Van Wagner, L.B., Koppe, S.W., Brunt, E.M., Gottstein, J., Gardikiotes, K., Green, R.M. and
Rinella, M.E., 2016. Pentoxifylline for the treatment of non-alcoholic steatohepatitis: a
randomized controlled trial. Annals of hepatology, 10(3), pp.277-286.
Younossi, Z.M., Koenig, A.B., Abdelatif, D., Fazel, Y., Henry, L. and Wymer, M., 2016. Global
epidemiology of nonalcoholic fatty liver disease—meta‐analytic assessment of prevalence,
incidence, and outcomes. Hepatology, 64(1), pp.73-84.
Zelber‐Sagi, S., Salomone, F. and Mlynarsky, L., 2017. The Mediterranean dietary pattern as the
diet of choice for non‐alcoholic fatty liver disease: Evidence and plausible mechanisms. Liver
International, 37(7), pp.936-949.
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





