What do you consider to be normal/abnormal?
VerifiedAdded on 2022/08/20
|6
|2541
|15
AI Summary
Limb movements: left arm with normal power, No swelling assess Temperature=37.5 Blood loss: nil SpO2=99% Capillary refill:3 seconds Sensation: Normal No acute intracranial abnormality Skull fractures are absent. Blood pressure =120/80mmHg Pulse rate = 60-100bpm Respiratory Rate=12-20 bpm GCS (Glasgow Coma Scale) and=15 Pain: 0/10 (no pain) Neurovascular Assessment: Left toes Movement: wid and capillary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
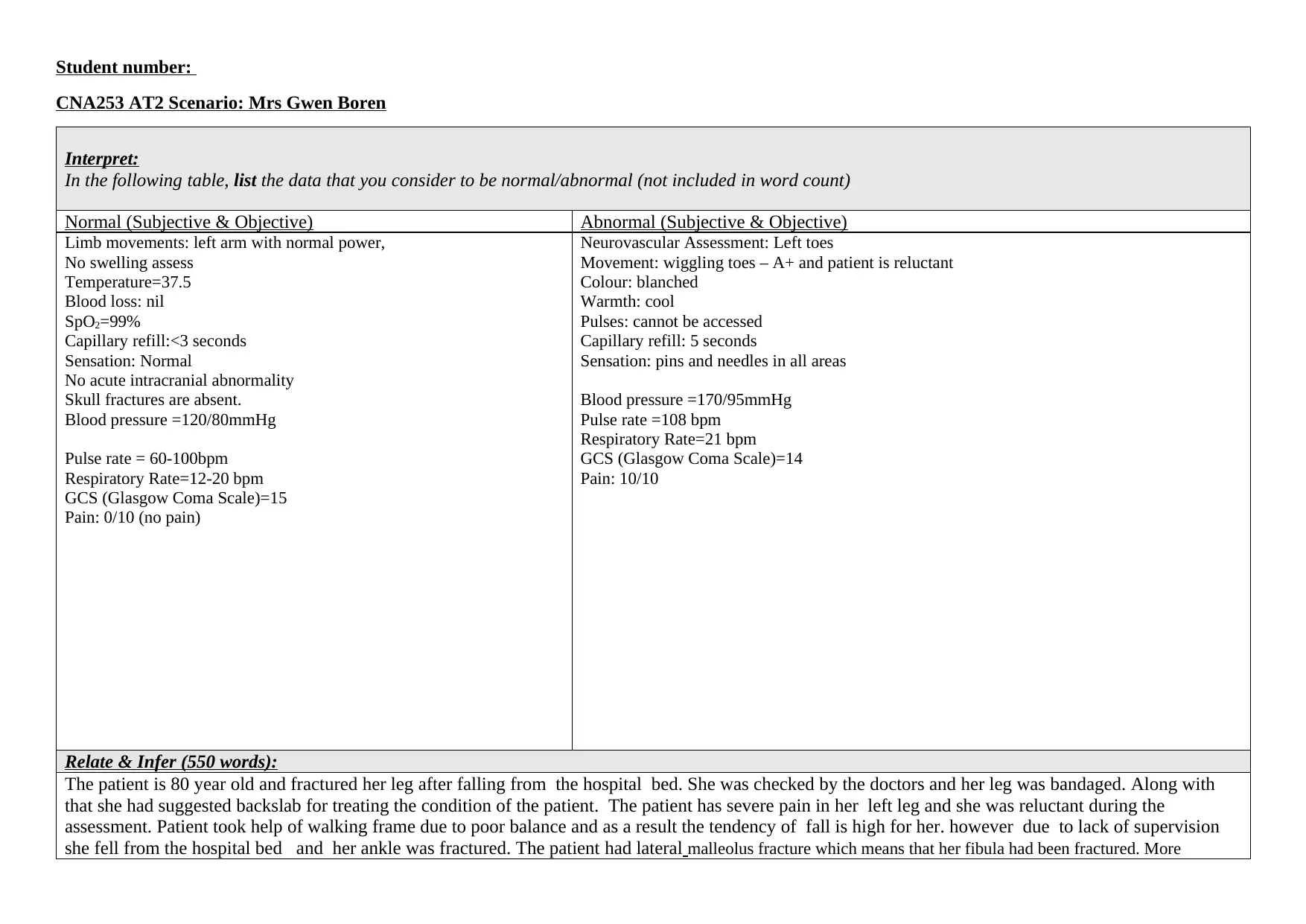
Student number:
CNA253 AT2 Scenario: Mrs Gwen Boren
Interpret:
In the following table, list the data that you consider to be normal/abnormal (not included in word count)
Normal (Subjective & Objective) Abnormal (Subjective & Objective)
Limb movements: left arm with normal power,
No swelling assess
Temperature=37.5
Blood loss: nil
SpO2=99%
Capillary refill:<3 seconds
Sensation: Normal
No acute intracranial abnormality
Skull fractures are absent.
Blood pressure =120/80mmHg
Pulse rate = 60-100bpm
Respiratory Rate=12-20 bpm
GCS (Glasgow Coma Scale)=15
Pain: 0/10 (no pain)
Neurovascular Assessment: Left toes
Movement: wiggling toes – A+ and patient is reluctant
Colour: blanched
Warmth: cool
Pulses: cannot be accessed
Capillary refill: 5 seconds
Sensation: pins and needles in all areas
Blood pressure =170/95mmHg
Pulse rate =108 bpm
Respiratory Rate=21 bpm
GCS (Glasgow Coma Scale)=14
Pain: 10/10
Relate & Infer (550 words):
The patient is 80 year old and fractured her leg after falling from the hospital bed. She was checked by the doctors and her leg was bandaged. Along with
that she had suggested backslab for treating the condition of the patient. The patient has severe pain in her left leg and she was reluctant during the
assessment. Patient took help of walking frame due to poor balance and as a result the tendency of fall is high for her. however due to lack of supervision
she fell from the hospital bed and her ankle was fractured. The patient had lateral malleolus fracture which means that her fibula had been fractured. More
CNA253 AT2 Scenario: Mrs Gwen Boren
Interpret:
In the following table, list the data that you consider to be normal/abnormal (not included in word count)
Normal (Subjective & Objective) Abnormal (Subjective & Objective)
Limb movements: left arm with normal power,
No swelling assess
Temperature=37.5
Blood loss: nil
SpO2=99%
Capillary refill:<3 seconds
Sensation: Normal
No acute intracranial abnormality
Skull fractures are absent.
Blood pressure =120/80mmHg
Pulse rate = 60-100bpm
Respiratory Rate=12-20 bpm
GCS (Glasgow Coma Scale)=15
Pain: 0/10 (no pain)
Neurovascular Assessment: Left toes
Movement: wiggling toes – A+ and patient is reluctant
Colour: blanched
Warmth: cool
Pulses: cannot be accessed
Capillary refill: 5 seconds
Sensation: pins and needles in all areas
Blood pressure =170/95mmHg
Pulse rate =108 bpm
Respiratory Rate=21 bpm
GCS (Glasgow Coma Scale)=14
Pain: 10/10
Relate & Infer (550 words):
The patient is 80 year old and fractured her leg after falling from the hospital bed. She was checked by the doctors and her leg was bandaged. Along with
that she had suggested backslab for treating the condition of the patient. The patient has severe pain in her left leg and she was reluctant during the
assessment. Patient took help of walking frame due to poor balance and as a result the tendency of fall is high for her. however due to lack of supervision
she fell from the hospital bed and her ankle was fractured. The patient had lateral malleolus fracture which means that her fibula had been fractured. More
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
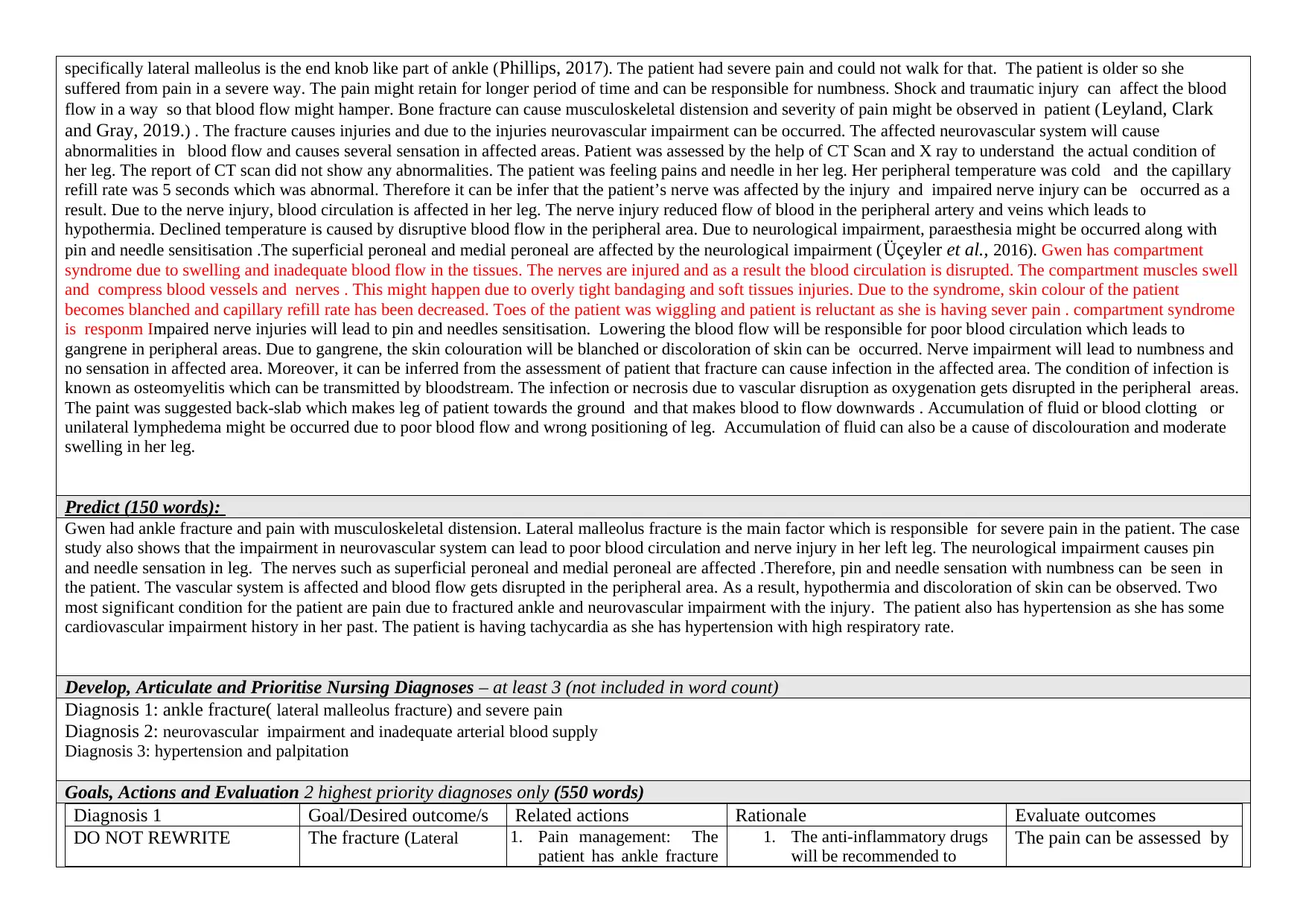
specifically lateral malleolus is the end knob like part of ankle (Phillips, 2017). The patient had severe pain and could not walk for that. The patient is older so she
suffered from pain in a severe way. The pain might retain for longer period of time and can be responsible for numbness. Shock and traumatic injury can affect the blood
flow in a way so that blood flow might hamper. Bone fracture can cause musculoskeletal distension and severity of pain might be observed in patient (Leyland, Clark
and Gray, 2019.) . The fracture causes injuries and due to the injuries neurovascular impairment can be occurred. The affected neurovascular system will cause
abnormalities in blood flow and causes several sensation in affected areas. Patient was assessed by the help of CT Scan and X ray to understand the actual condition of
her leg. The report of CT scan did not show any abnormalities. The patient was feeling pains and needle in her leg. Her peripheral temperature was cold and the capillary
refill rate was 5 seconds which was abnormal. Therefore it can be infer that the patient’s nerve was affected by the injury and impaired nerve injury can be occurred as a
result. Due to the nerve injury, blood circulation is affected in her leg. The nerve injury reduced flow of blood in the peripheral artery and veins which leads to
hypothermia. Declined temperature is caused by disruptive blood flow in the peripheral area. Due to neurological impairment, paraesthesia might be occurred along with
pin and needle sensitisation .The superficial peroneal and medial peroneal are affected by the neurological impairment (Üçeyler et al., 2016). Gwen has compartment
syndrome due to swelling and inadequate blood flow in the tissues. The nerves are injured and as a result the blood circulation is disrupted. The compartment muscles swell
and compress blood vessels and nerves . This might happen due to overly tight bandaging and soft tissues injuries. Due to the syndrome, skin colour of the patient
becomes blanched and capillary refill rate has been decreased. Toes of the patient was wiggling and patient is reluctant as she is having sever pain . compartment syndrome
is responm Impaired nerve injuries will lead to pin and needles sensitisation. Lowering the blood flow will be responsible for poor blood circulation which leads to
gangrene in peripheral areas. Due to gangrene, the skin colouration will be blanched or discoloration of skin can be occurred. Nerve impairment will lead to numbness and
no sensation in affected area. Moreover, it can be inferred from the assessment of patient that fracture can cause infection in the affected area. The condition of infection is
known as osteomyelitis which can be transmitted by bloodstream. The infection or necrosis due to vascular disruption as oxygenation gets disrupted in the peripheral areas.
The paint was suggested back-slab which makes leg of patient towards the ground and that makes blood to flow downwards . Accumulation of fluid or blood clotting or
unilateral lymphedema might be occurred due to poor blood flow and wrong positioning of leg. Accumulation of fluid can also be a cause of discolouration and moderate
swelling in her leg.
Predict (150 words):
Gwen had ankle fracture and pain with musculoskeletal distension. Lateral malleolus fracture is the main factor which is responsible for severe pain in the patient. The case
study also shows that the impairment in neurovascular system can lead to poor blood circulation and nerve injury in her left leg. The neurological impairment causes pin
and needle sensation in leg. The nerves such as superficial peroneal and medial peroneal are affected .Therefore, pin and needle sensation with numbness can be seen in
the patient. The vascular system is affected and blood flow gets disrupted in the peripheral area. As a result, hypothermia and discoloration of skin can be observed. Two
most significant condition for the patient are pain due to fractured ankle and neurovascular impairment with the injury. The patient also has hypertension as she has some
cardiovascular impairment history in her past. The patient is having tachycardia as she has hypertension with high respiratory rate.
Develop, Articulate and Prioritise Nursing Diagnoses – at least 3 (not included in word count)
Diagnosis 1: ankle fracture( lateral malleolus fracture) and severe pain
Diagnosis 2: neurovascular impairment and inadequate arterial blood supply
Diagnosis 3: hypertension and palpitation
Goals, Actions and Evaluation 2 highest priority diagnoses only (550 words)
Diagnosis 1 Goal/Desired outcome/s Related actions Rationale Evaluate outcomes
DO NOT REWRITE The fracture (Lateral 1. Pain management: The
patient has ankle fracture
1. The anti-inflammatory drugs
will be recommended to
The pain can be assessed by
suffered from pain in a severe way. The pain might retain for longer period of time and can be responsible for numbness. Shock and traumatic injury can affect the blood
flow in a way so that blood flow might hamper. Bone fracture can cause musculoskeletal distension and severity of pain might be observed in patient (Leyland, Clark
and Gray, 2019.) . The fracture causes injuries and due to the injuries neurovascular impairment can be occurred. The affected neurovascular system will cause
abnormalities in blood flow and causes several sensation in affected areas. Patient was assessed by the help of CT Scan and X ray to understand the actual condition of
her leg. The report of CT scan did not show any abnormalities. The patient was feeling pains and needle in her leg. Her peripheral temperature was cold and the capillary
refill rate was 5 seconds which was abnormal. Therefore it can be infer that the patient’s nerve was affected by the injury and impaired nerve injury can be occurred as a
result. Due to the nerve injury, blood circulation is affected in her leg. The nerve injury reduced flow of blood in the peripheral artery and veins which leads to
hypothermia. Declined temperature is caused by disruptive blood flow in the peripheral area. Due to neurological impairment, paraesthesia might be occurred along with
pin and needle sensitisation .The superficial peroneal and medial peroneal are affected by the neurological impairment (Üçeyler et al., 2016). Gwen has compartment
syndrome due to swelling and inadequate blood flow in the tissues. The nerves are injured and as a result the blood circulation is disrupted. The compartment muscles swell
and compress blood vessels and nerves . This might happen due to overly tight bandaging and soft tissues injuries. Due to the syndrome, skin colour of the patient
becomes blanched and capillary refill rate has been decreased. Toes of the patient was wiggling and patient is reluctant as she is having sever pain . compartment syndrome
is responm Impaired nerve injuries will lead to pin and needles sensitisation. Lowering the blood flow will be responsible for poor blood circulation which leads to
gangrene in peripheral areas. Due to gangrene, the skin colouration will be blanched or discoloration of skin can be occurred. Nerve impairment will lead to numbness and
no sensation in affected area. Moreover, it can be inferred from the assessment of patient that fracture can cause infection in the affected area. The condition of infection is
known as osteomyelitis which can be transmitted by bloodstream. The infection or necrosis due to vascular disruption as oxygenation gets disrupted in the peripheral areas.
The paint was suggested back-slab which makes leg of patient towards the ground and that makes blood to flow downwards . Accumulation of fluid or blood clotting or
unilateral lymphedema might be occurred due to poor blood flow and wrong positioning of leg. Accumulation of fluid can also be a cause of discolouration and moderate
swelling in her leg.
Predict (150 words):
Gwen had ankle fracture and pain with musculoskeletal distension. Lateral malleolus fracture is the main factor which is responsible for severe pain in the patient. The case
study also shows that the impairment in neurovascular system can lead to poor blood circulation and nerve injury in her left leg. The neurological impairment causes pin
and needle sensation in leg. The nerves such as superficial peroneal and medial peroneal are affected .Therefore, pin and needle sensation with numbness can be seen in
the patient. The vascular system is affected and blood flow gets disrupted in the peripheral area. As a result, hypothermia and discoloration of skin can be observed. Two
most significant condition for the patient are pain due to fractured ankle and neurovascular impairment with the injury. The patient also has hypertension as she has some
cardiovascular impairment history in her past. The patient is having tachycardia as she has hypertension with high respiratory rate.
Develop, Articulate and Prioritise Nursing Diagnoses – at least 3 (not included in word count)
Diagnosis 1: ankle fracture( lateral malleolus fracture) and severe pain
Diagnosis 2: neurovascular impairment and inadequate arterial blood supply
Diagnosis 3: hypertension and palpitation
Goals, Actions and Evaluation 2 highest priority diagnoses only (550 words)
Diagnosis 1 Goal/Desired outcome/s Related actions Rationale Evaluate outcomes
DO NOT REWRITE The fracture (Lateral 1. Pain management: The
patient has ankle fracture
1. The anti-inflammatory drugs
will be recommended to
The pain can be assessed by
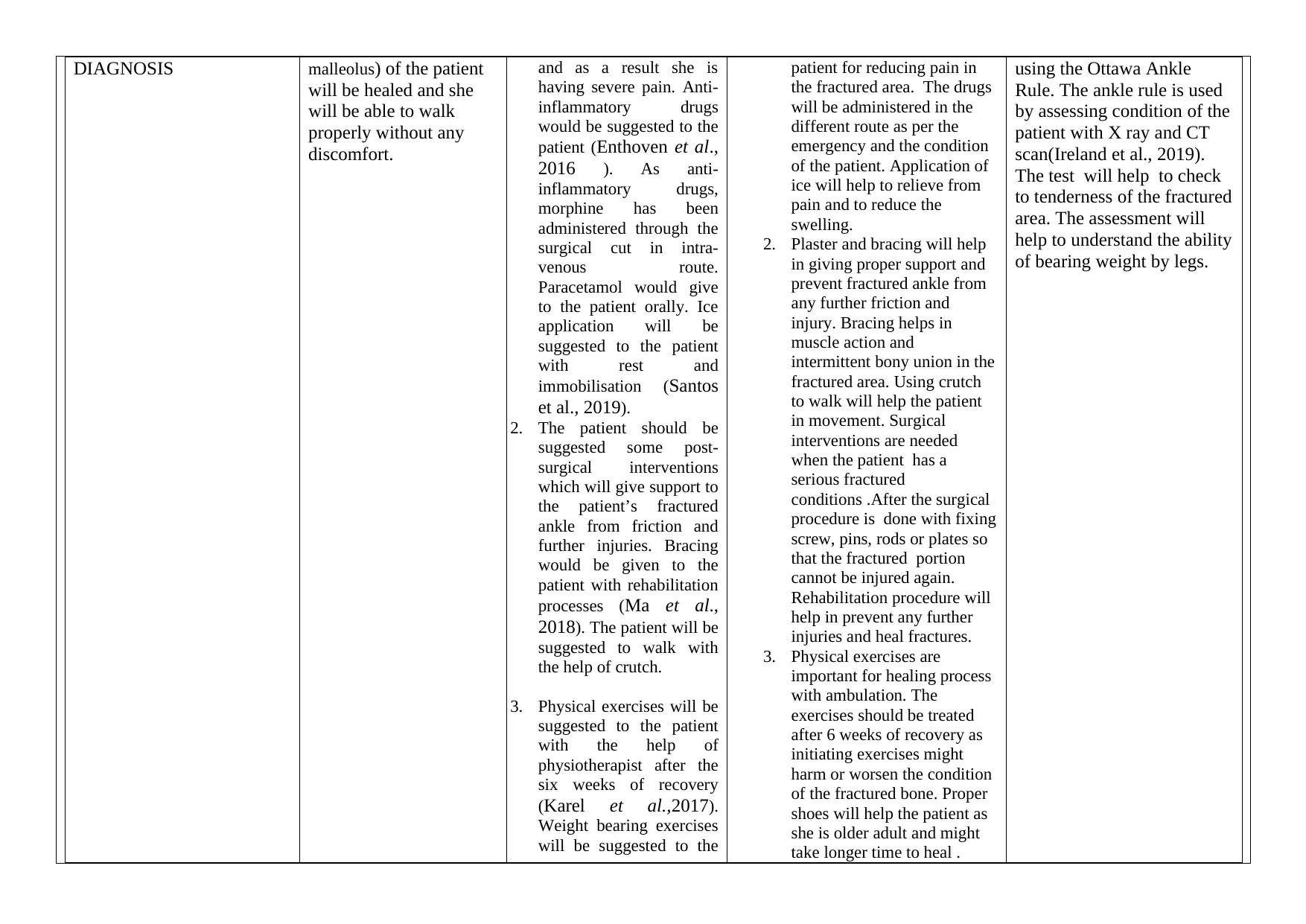
DIAGNOSIS malleolus) of the patient
will be healed and she
will be able to walk
properly without any
discomfort.
and as a result she is
having severe pain. Anti-
inflammatory drugs
would be suggested to the
patient (Enthoven et al.,
2016 ). As anti-
inflammatory drugs,
morphine has been
administered through the
surgical cut in intra-
venous route.
Paracetamol would give
to the patient orally. Ice
application will be
suggested to the patient
with rest and
immobilisation (Santos
et al., 2019).
2. The patient should be
suggested some post-
surgical interventions
which will give support to
the patient’s fractured
ankle from friction and
further injuries. Bracing
would be given to the
patient with rehabilitation
processes (Ma et al.,
2018). The patient will be
suggested to walk with
the help of crutch.
3. Physical exercises will be
suggested to the patient
with the help of
physiotherapist after the
six weeks of recovery
(Karel et al.,2017).
Weight bearing exercises
will be suggested to the
patient for reducing pain in
the fractured area. The drugs
will be administered in the
different route as per the
emergency and the condition
of the patient. Application of
ice will help to relieve from
pain and to reduce the
swelling.
2. Plaster and bracing will help
in giving proper support and
prevent fractured ankle from
any further friction and
injury. Bracing helps in
muscle action and
intermittent bony union in the
fractured area. Using crutch
to walk will help the patient
in movement. Surgical
interventions are needed
when the patient has a
serious fractured
conditions .After the surgical
procedure is done with fixing
screw, pins, rods or plates so
that the fractured portion
cannot be injured again.
Rehabilitation procedure will
help in prevent any further
injuries and heal fractures.
3. Physical exercises are
important for healing process
with ambulation. The
exercises should be treated
after 6 weeks of recovery as
initiating exercises might
harm or worsen the condition
of the fractured bone. Proper
shoes will help the patient as
she is older adult and might
take longer time to heal .
using the Ottawa Ankle
Rule. The ankle rule is used
by assessing condition of the
patient with X ray and CT
scan(Ireland et al., 2019).
The test will help to check
to tenderness of the fractured
area. The assessment will
help to understand the ability
of bearing weight by legs.
will be healed and she
will be able to walk
properly without any
discomfort.
and as a result she is
having severe pain. Anti-
inflammatory drugs
would be suggested to the
patient (Enthoven et al.,
2016 ). As anti-
inflammatory drugs,
morphine has been
administered through the
surgical cut in intra-
venous route.
Paracetamol would give
to the patient orally. Ice
application will be
suggested to the patient
with rest and
immobilisation (Santos
et al., 2019).
2. The patient should be
suggested some post-
surgical interventions
which will give support to
the patient’s fractured
ankle from friction and
further injuries. Bracing
would be given to the
patient with rehabilitation
processes (Ma et al.,
2018). The patient will be
suggested to walk with
the help of crutch.
3. Physical exercises will be
suggested to the patient
with the help of
physiotherapist after the
six weeks of recovery
(Karel et al.,2017).
Weight bearing exercises
will be suggested to the
patient for reducing pain in
the fractured area. The drugs
will be administered in the
different route as per the
emergency and the condition
of the patient. Application of
ice will help to relieve from
pain and to reduce the
swelling.
2. Plaster and bracing will help
in giving proper support and
prevent fractured ankle from
any further friction and
injury. Bracing helps in
muscle action and
intermittent bony union in the
fractured area. Using crutch
to walk will help the patient
in movement. Surgical
interventions are needed
when the patient has a
serious fractured
conditions .After the surgical
procedure is done with fixing
screw, pins, rods or plates so
that the fractured portion
cannot be injured again.
Rehabilitation procedure will
help in prevent any further
injuries and heal fractures.
3. Physical exercises are
important for healing process
with ambulation. The
exercises should be treated
after 6 weeks of recovery as
initiating exercises might
harm or worsen the condition
of the fractured bone. Proper
shoes will help the patient as
she is older adult and might
take longer time to heal .
using the Ottawa Ankle
Rule. The ankle rule is used
by assessing condition of the
patient with X ray and CT
scan(Ireland et al., 2019).
The test will help to check
to tenderness of the fractured
area. The assessment will
help to understand the ability
of bearing weight by legs.
patient (Peeler and
Ripat, 2018). Moreover,
proper shoe (high-top
tennis shoe to a short leg
cast) should be suggested
to the patient (Brotzman,
2017.).
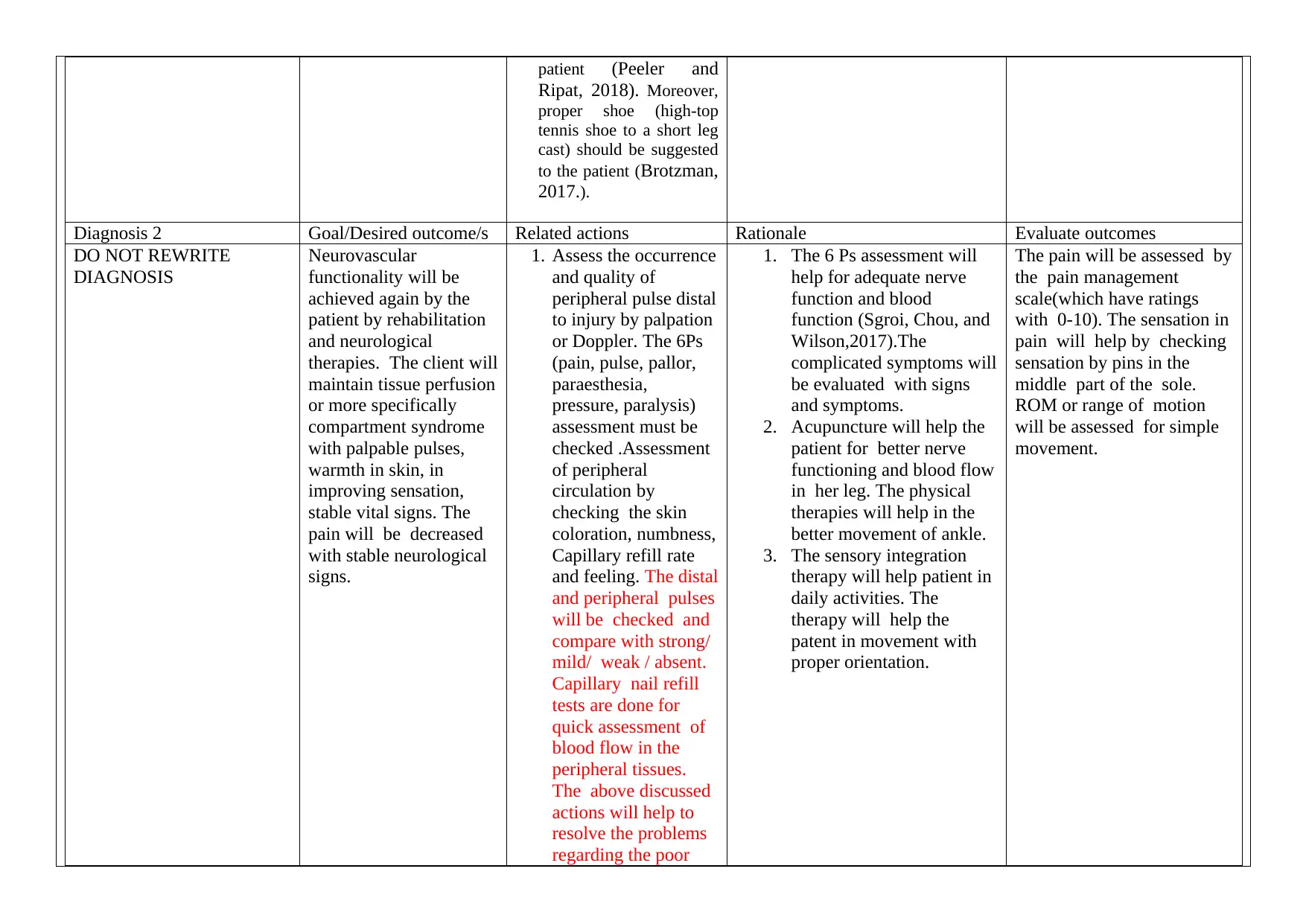
Diagnosis 2 Goal/Desired outcome/s Related actions Rationale Evaluate outcomes
DO NOT REWRITE
DIAGNOSIS
Neurovascular
functionality will be
achieved again by the
patient by rehabilitation
and neurological
therapies. The client will
maintain tissue perfusion
or more specifically
compartment syndrome
with palpable pulses,
warmth in skin, in
improving sensation,
stable vital signs. The
pain will be decreased
with stable neurological
signs.
1. Assess the occurrence
and quality of
peripheral pulse distal
to injury by palpation
or Doppler. The 6Ps
(pain, pulse, pallor,
paraesthesia,
pressure, paralysis)
assessment must be
checked .Assessment
of peripheral
circulation by
checking the skin
coloration, numbness,
Capillary refill rate
and feeling. The distal
and peripheral pulses
will be checked and
compare with strong/
mild/ weak / absent.
Capillary nail refill
tests are done for
quick assessment of
blood flow in the
peripheral tissues.
The above discussed
actions will help to
resolve the problems
regarding the poor
1. The 6 Ps assessment will
help for adequate nerve
function and blood
function (Sgroi, Chou, and
Wilson,2017).The
complicated symptoms will
be evaluated with signs
and symptoms.
2. Acupuncture will help the
patient for better nerve
functioning and blood flow
in her leg. The physical
therapies will help in the
better movement of ankle.
3. The sensory integration
therapy will help patient in
daily activities. The
therapy will help the
patent in movement with
proper orientation.
The pain will be assessed by
the pain management
scale(which have ratings
with 0-10). The sensation in
pain will help by checking
sensation by pins in the
middle part of the sole.
ROM or range of motion
will be assessed for simple
movement.
Ripat, 2018). Moreover,
proper shoe (high-top
tennis shoe to a short leg
cast) should be suggested
to the patient (Brotzman,
2017.).
Diagnosis 2 Goal/Desired outcome/s Related actions Rationale Evaluate outcomes
DO NOT REWRITE
DIAGNOSIS
Neurovascular
functionality will be
achieved again by the
patient by rehabilitation
and neurological
therapies. The client will
maintain tissue perfusion
or more specifically
compartment syndrome
with palpable pulses,
warmth in skin, in
improving sensation,
stable vital signs. The
pain will be decreased
with stable neurological
signs.
1. Assess the occurrence
and quality of
peripheral pulse distal
to injury by palpation
or Doppler. The 6Ps
(pain, pulse, pallor,
paraesthesia,
pressure, paralysis)
assessment must be
checked .Assessment
of peripheral
circulation by
checking the skin
coloration, numbness,
Capillary refill rate
and feeling. The distal
and peripheral pulses
will be checked and
compare with strong/
mild/ weak / absent.
Capillary nail refill
tests are done for
quick assessment of
blood flow in the
peripheral tissues.
The above discussed
actions will help to
resolve the problems
regarding the poor
1. The 6 Ps assessment will
help for adequate nerve
function and blood
function (Sgroi, Chou, and
Wilson,2017).The
complicated symptoms will
be evaluated with signs
and symptoms.
2. Acupuncture will help the
patient for better nerve
functioning and blood flow
in her leg. The physical
therapies will help in the
better movement of ankle.
3. The sensory integration
therapy will help patient in
daily activities. The
therapy will help the
patent in movement with
proper orientation.
The pain will be assessed by
the pain management
scale(which have ratings
with 0-10). The sensation in
pain will help by checking
sensation by pins in the
middle part of the sole.
ROM or range of motion
will be assessed for simple
movement.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
arterial blood supply.
2. Acupuncture and
massage are also
suggested to give
relief to the
symptoms of
paraesthesia. Fixation
and post traumatic
management of injury
might be given to the
patient(Coutaux,
2017). The isometric
and isotonic ankle
planter-flexion and
dorsiflexion will be
helpful for the patient.
3. Sensory integration
therapy and low
intensity exercises
will be suggested to
the patient for better
result for movement.
Reference list:
Brotzman, S.B., 2017. Inferior heel pain (plantar fasciitis). Clinical Orthopaedic Rehabilitation: A Team Approach E-Book, 9(925), p.281.
https://books.google.co.in/books?hl=en&lr=&id=ufHWDQAAQBAJ&oi=fnd&pg=PA281&dq=proper+shoe+(high-top+tennis+shoe+to+a+short+leg+cast)
+should+be+suggested+to+the+patient&ots=atVpHXfZ6-&sig=QC1-OGBw8Y_S9TLRydCp2eakJlg&redir_esc=y#v=onepage&q&f=false
Coutaux, A., 2017. Non-pharmacological treatments for pain relief: TENS and acupuncture. Joint Bone Spine, 84(6), pp.657-661.
https://www.sciencedirect.com/science/article/pii/S1297319X17300167
Enthoven, W.T., Roelofs, P.D., Deyo, R.A., van Tulder, M.W. and Koes, B.W., 2016. Non‐steroidal anti‐inflammatory drugs for chronic low back
pain. Cochrane Database of Systematic Reviews, (2). https://doi.org/10.1002/14651858.CD012087
Ireland, N., Nabi, S., Chand, K., Deveson, P., Harding, K., Cannon, E., Turner, D., Krishan, P. and Welch, C., 2019. Toolbox-Ottawa knee and ankle
rules. Pulse, 50(2019). http://www.pulsetoday.co.uk/clinical/toolbox-ottawa-knee-and-ankle-rules/20002175.article
Karel, Y.H., Scholten-Peeters, G.G.M., Thoomes-de Graaf, M., Duijn, E., van Broekhoven, J.B., Koes, B.W. and Verhagen, A.P., 2017. Physiotherapy for
patients with shoulder pain in primary care: a descriptive study of diagnostic-and therapeutic management. Physiotherapy, 103(4), pp.369-378.
2. Acupuncture and
massage are also
suggested to give
relief to the
symptoms of
paraesthesia. Fixation
and post traumatic
management of injury
might be given to the
patient(Coutaux,
2017). The isometric
and isotonic ankle
planter-flexion and
dorsiflexion will be
helpful for the patient.
3. Sensory integration
therapy and low
intensity exercises
will be suggested to
the patient for better
result for movement.
Reference list:
Brotzman, S.B., 2017. Inferior heel pain (plantar fasciitis). Clinical Orthopaedic Rehabilitation: A Team Approach E-Book, 9(925), p.281.
https://books.google.co.in/books?hl=en&lr=&id=ufHWDQAAQBAJ&oi=fnd&pg=PA281&dq=proper+shoe+(high-top+tennis+shoe+to+a+short+leg+cast)
+should+be+suggested+to+the+patient&ots=atVpHXfZ6-&sig=QC1-OGBw8Y_S9TLRydCp2eakJlg&redir_esc=y#v=onepage&q&f=false
Coutaux, A., 2017. Non-pharmacological treatments for pain relief: TENS and acupuncture. Joint Bone Spine, 84(6), pp.657-661.
https://www.sciencedirect.com/science/article/pii/S1297319X17300167
Enthoven, W.T., Roelofs, P.D., Deyo, R.A., van Tulder, M.W. and Koes, B.W., 2016. Non‐steroidal anti‐inflammatory drugs for chronic low back
pain. Cochrane Database of Systematic Reviews, (2). https://doi.org/10.1002/14651858.CD012087
Ireland, N., Nabi, S., Chand, K., Deveson, P., Harding, K., Cannon, E., Turner, D., Krishan, P. and Welch, C., 2019. Toolbox-Ottawa knee and ankle
rules. Pulse, 50(2019). http://www.pulsetoday.co.uk/clinical/toolbox-ottawa-knee-and-ankle-rules/20002175.article
Karel, Y.H., Scholten-Peeters, G.G.M., Thoomes-de Graaf, M., Duijn, E., van Broekhoven, J.B., Koes, B.W. and Verhagen, A.P., 2017. Physiotherapy for
patients with shoulder pain in primary care: a descriptive study of diagnostic-and therapeutic management. Physiotherapy, 103(4), pp.369-378.
https://www.researchgate.net/profile/Marloes_Graaf/publication/311094966_Physiotherapy_for_patients_with_shoulder_pain_in_primary_care_A_descriptiv
e_study_of_diagnostic-_and_therapeutic_management/links/59a83063aca27202ed5f488e/Physiotherapy-for-patients-with-shoulder-pain-in-primary-care-A-
descriptive-study-of-diagnostic-and-therapeutic-management.pdf
Leyland, S., Clark, E. and Gray, A., 2019. The role of exercise after osteoporotic vertebral fracture. Injury, 50(4), pp.825-826.
https://www.injuryjournal.com/article/S0020-1383(19)30222-0/abstract
Ma, H., Zhong, C., Chen, B., Chan, K.M. and Liao, W.H., 2018. User-adaptive assistance of assistive knee braces for gait rehabilitation. IEEE Transactions
on Neural Systems and Rehabilitation Engineering, 26(10), pp.1994-2005. https://ieeexplore.ieee.org/abstract/document/8454752/
Peeler, J. and Ripat, J., 2018. The effect of low-load exercise on joint pain, function, and activities of daily living in patients with knee osteoarthritis. The
Knee, 25(1), pp.135-145. http://sciencedirect.com/science/article/pii/S0968016017303332
Phillips, G.A., Bonutti Research Inc, 2017. Ankle foot orthosis. U.S. Patent Application 15/420,663. https://patents.google.com/patent/US20170231795A1/en
Santos, V.B., Melo, L.M.E., Assis, A.R.V.D., Moraes, J.B.D., Lopes, C.T., Lopes, J.D.L. and Barros, A.L.B.L.D., 2019. Decreasing length of limb
immobilisation following nonelective transfemoral percutaneous coronary intervention: A randomised clinical trial. Journal of clinical nursing, 28(17-18),
pp.3140-3148. https://onlinelibrary.wiley.com/doi/abs/10.1111/jocn.14860
Sgroi, M.D., Chou, E.L. and Wilson, S.E., 2017. Clinical examination of the vascular system. In Vascular Surgery (pp. 79-88). CRC Press.
https://www.taylorfrancis.com/books/e/9781315381770/chapters/10.1201/9781315381770-12
Üçeyler, N., Schäfer, K.A., Mackenrodt, D., Sommer, C. and Müllges, W., 2016. High-resolution ultrasonography of the superficial peroneal motor and sural
sensory nerves may be a non-invasive approach to the diagnosis of vasculitic neuropathy. Frontiers in neurology, 7, p.48.
https://www.frontiersin.org/articles/10.3389/fneur.2016.00048/full
e_study_of_diagnostic-_and_therapeutic_management/links/59a83063aca27202ed5f488e/Physiotherapy-for-patients-with-shoulder-pain-in-primary-care-A-
descriptive-study-of-diagnostic-and-therapeutic-management.pdf
Leyland, S., Clark, E. and Gray, A., 2019. The role of exercise after osteoporotic vertebral fracture. Injury, 50(4), pp.825-826.
https://www.injuryjournal.com/article/S0020-1383(19)30222-0/abstract
Ma, H., Zhong, C., Chen, B., Chan, K.M. and Liao, W.H., 2018. User-adaptive assistance of assistive knee braces for gait rehabilitation. IEEE Transactions
on Neural Systems and Rehabilitation Engineering, 26(10), pp.1994-2005. https://ieeexplore.ieee.org/abstract/document/8454752/
Peeler, J. and Ripat, J., 2018. The effect of low-load exercise on joint pain, function, and activities of daily living in patients with knee osteoarthritis. The
Knee, 25(1), pp.135-145. http://sciencedirect.com/science/article/pii/S0968016017303332
Phillips, G.A., Bonutti Research Inc, 2017. Ankle foot orthosis. U.S. Patent Application 15/420,663. https://patents.google.com/patent/US20170231795A1/en
Santos, V.B., Melo, L.M.E., Assis, A.R.V.D., Moraes, J.B.D., Lopes, C.T., Lopes, J.D.L. and Barros, A.L.B.L.D., 2019. Decreasing length of limb
immobilisation following nonelective transfemoral percutaneous coronary intervention: A randomised clinical trial. Journal of clinical nursing, 28(17-18),
pp.3140-3148. https://onlinelibrary.wiley.com/doi/abs/10.1111/jocn.14860
Sgroi, M.D., Chou, E.L. and Wilson, S.E., 2017. Clinical examination of the vascular system. In Vascular Surgery (pp. 79-88). CRC Press.
https://www.taylorfrancis.com/books/e/9781315381770/chapters/10.1201/9781315381770-12
Üçeyler, N., Schäfer, K.A., Mackenrodt, D., Sommer, C. and Müllges, W., 2016. High-resolution ultrasonography of the superficial peroneal motor and sural
sensory nerves may be a non-invasive approach to the diagnosis of vasculitic neuropathy. Frontiers in neurology, 7, p.48.
https://www.frontiersin.org/articles/10.3389/fneur.2016.00048/full
1 out of 6
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





