Post-Operative Nursing Care Priority
VerifiedAdded on 2023/01/19
|8
|1552
|41
AI Summary
This student response template discusses the priority of post-operative nursing care and potential complications such as wound infection and urinary retention. It provides rationale for each priority and suggests nursing management strategies. References are also included.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
NUR2226 iSAP Erica Gardner
Part A: Student response template
Student Number: XXXXXXXX
Post-operative nursing care priority Rationale
1.
Assessment of the patient to rule out presence and intensity of pain in
a scale of 0-10 including its location, and severity. The evidence of
pain includes patient’s verbalization, mourning, and facial mask
indicating pain.
This would be essential since the patient must be in pain after the
surgical operation. Regardless of the fact that the patient was operated
under anaesthesia, she will be experienced pain after recovering pain
from the anaesthesia. This would be critical to control and
management the pain through the implementation of the most
appropriate interventions to relieve pain and ensure comfortability of
the patient. The nurse ca control the pain by administering injectable
such as diclofenac (Chatchumni, Namvongprom,Eriksson, &
Mazaheri, 2016).
2.
Taking the patient’s vital signs including her temperature, respiration
rate, blood pressure, oxygen saturation, and pulse rate and her level of
The assessment of the patient’s is essential to ensure that she is alert
and well-oriented to time, place, and person since she is at a high risk
of deterioration post-operation. Post-operatively, the vital signs would
help as the key indicators of the patient’s pathophysiological status.
Part A: Student response template
Student Number: XXXXXXXX
Post-operative nursing care priority Rationale
1.
Assessment of the patient to rule out presence and intensity of pain in
a scale of 0-10 including its location, and severity. The evidence of
pain includes patient’s verbalization, mourning, and facial mask
indicating pain.
This would be essential since the patient must be in pain after the
surgical operation. Regardless of the fact that the patient was operated
under anaesthesia, she will be experienced pain after recovering pain
from the anaesthesia. This would be critical to control and
management the pain through the implementation of the most
appropriate interventions to relieve pain and ensure comfortability of
the patient. The nurse ca control the pain by administering injectable
such as diclofenac (Chatchumni, Namvongprom,Eriksson, &
Mazaheri, 2016).
2.
Taking the patient’s vital signs including her temperature, respiration
rate, blood pressure, oxygen saturation, and pulse rate and her level of
The assessment of the patient’s is essential to ensure that she is alert
and well-oriented to time, place, and person since she is at a high risk
of deterioration post-operation. Post-operatively, the vital signs would
help as the key indicators of the patient’s pathophysiological status.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NUR2226 iSAP Erica Gardner
Part A: Student response template
Student Number: XXXXXXXX
consciousness. This would necessitate the implementation of the best measures of
stabilizing her vital signs in case of any abnormalities. The patient
may also develop hypothermia evidenced by shivering and chills due
to alteration of the thermoregulation mechanism of the body during
operation (Joshi, Schug, & Kehlet, 2014).
3.
Monitoring the patient after awakening from the anaesthesia and
rehydration.
The patient may or may not wake up from the anaesthesia. It would
therefore be essential to monitor her since anaesthesia has significant
impact on the physiological processes of the patient’s body and may
alter the functioning of the some of body organs like the heart and
lungs. After recovering from anaesthesia, the patient may nausea and
vomiting associated with surgery. Monitoring the patient for these
signs would enable him or her administer anti-nausea or ant-emetic
medications to control the symptoms. During the surgical operation,
the patient loses a certain amount of blood which increases the risk of
fluid imbalance. The patient should be rehydrated with intravenous
fluids to restore fluid balance and prevent kidney problems associated
Part A: Student response template
Student Number: XXXXXXXX
consciousness. This would necessitate the implementation of the best measures of
stabilizing her vital signs in case of any abnormalities. The patient
may also develop hypothermia evidenced by shivering and chills due
to alteration of the thermoregulation mechanism of the body during
operation (Joshi, Schug, & Kehlet, 2014).
3.
Monitoring the patient after awakening from the anaesthesia and
rehydration.
The patient may or may not wake up from the anaesthesia. It would
therefore be essential to monitor her since anaesthesia has significant
impact on the physiological processes of the patient’s body and may
alter the functioning of the some of body organs like the heart and
lungs. After recovering from anaesthesia, the patient may nausea and
vomiting associated with surgery. Monitoring the patient for these
signs would enable him or her administer anti-nausea or ant-emetic
medications to control the symptoms. During the surgical operation,
the patient loses a certain amount of blood which increases the risk of
fluid imbalance. The patient should be rehydrated with intravenous
fluids to restore fluid balance and prevent kidney problems associated
NUR2226 iSAP Erica Gardner
Part A: Student response template
Student Number: XXXXXXXX
with alteration of fluid balance. From the case study, Erica has not
been feeding and taking fluids adequately and she also complains of
dry mouth. The dryness of her mouth is one of the key indicators of
dehydration which necessitates her rehydration (Joshi et al., 2014).
4.
Assessing and evaluating the incision site or surgical site to ensure
that the sutures are intact and the surgical wound is well covered as
expected.
If the surgical wound is not well covered, it is exposed to bacterial
and other disease-causing microorganisms which might lead to
infections and poor healing of the wound. Assessing the wound would
help the nurse identify any bleeding which should be controlled to
prevent other complications associated with increased risk of fluid
imbalance (Wilson, Orff, Gerry, Shirley, Tabor, Caiazzo, & Rouleau,
2013).
5. Ensuring patency of the patient’s airway and check for signs of
hypoxia such as changes in skin color, cough, confusion, increased
pulse rate, sweating, and shortness of breath.
The patient might experience breathing problems after awakening
from anaesthesia. So, the nurse may need to assess the patient to
prevent breathing difficulties which may lead to the deterioration of
the patient’s condition. (Lewis, Collier, & Heitkemper, 2017).
Part A: Student response template
Student Number: XXXXXXXX
with alteration of fluid balance. From the case study, Erica has not
been feeding and taking fluids adequately and she also complains of
dry mouth. The dryness of her mouth is one of the key indicators of
dehydration which necessitates her rehydration (Joshi et al., 2014).
4.
Assessing and evaluating the incision site or surgical site to ensure
that the sutures are intact and the surgical wound is well covered as
expected.
If the surgical wound is not well covered, it is exposed to bacterial
and other disease-causing microorganisms which might lead to
infections and poor healing of the wound. Assessing the wound would
help the nurse identify any bleeding which should be controlled to
prevent other complications associated with increased risk of fluid
imbalance (Wilson, Orff, Gerry, Shirley, Tabor, Caiazzo, & Rouleau,
2013).
5. Ensuring patency of the patient’s airway and check for signs of
hypoxia such as changes in skin color, cough, confusion, increased
pulse rate, sweating, and shortness of breath.
The patient might experience breathing problems after awakening
from anaesthesia. So, the nurse may need to assess the patient to
prevent breathing difficulties which may lead to the deterioration of
the patient’s condition. (Lewis, Collier, & Heitkemper, 2017).
NUR2226 iSAP Erica Gardner
Part A: Student response template
Student Number: XXXXXXXX
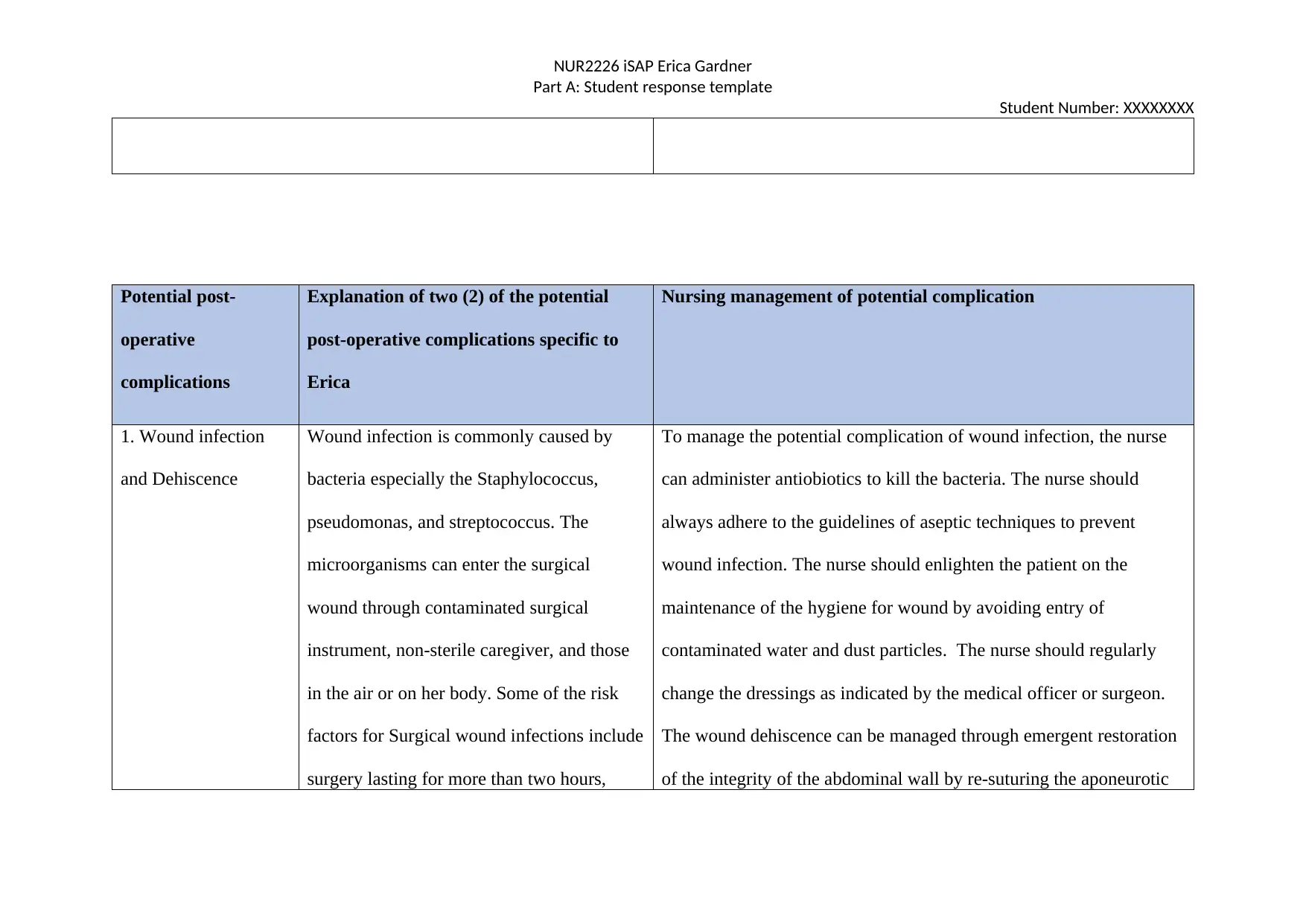
Potential post-
operative
complications
Explanation of two (2) of the potential
post-operative complications specific to
Erica
Nursing management of potential complication
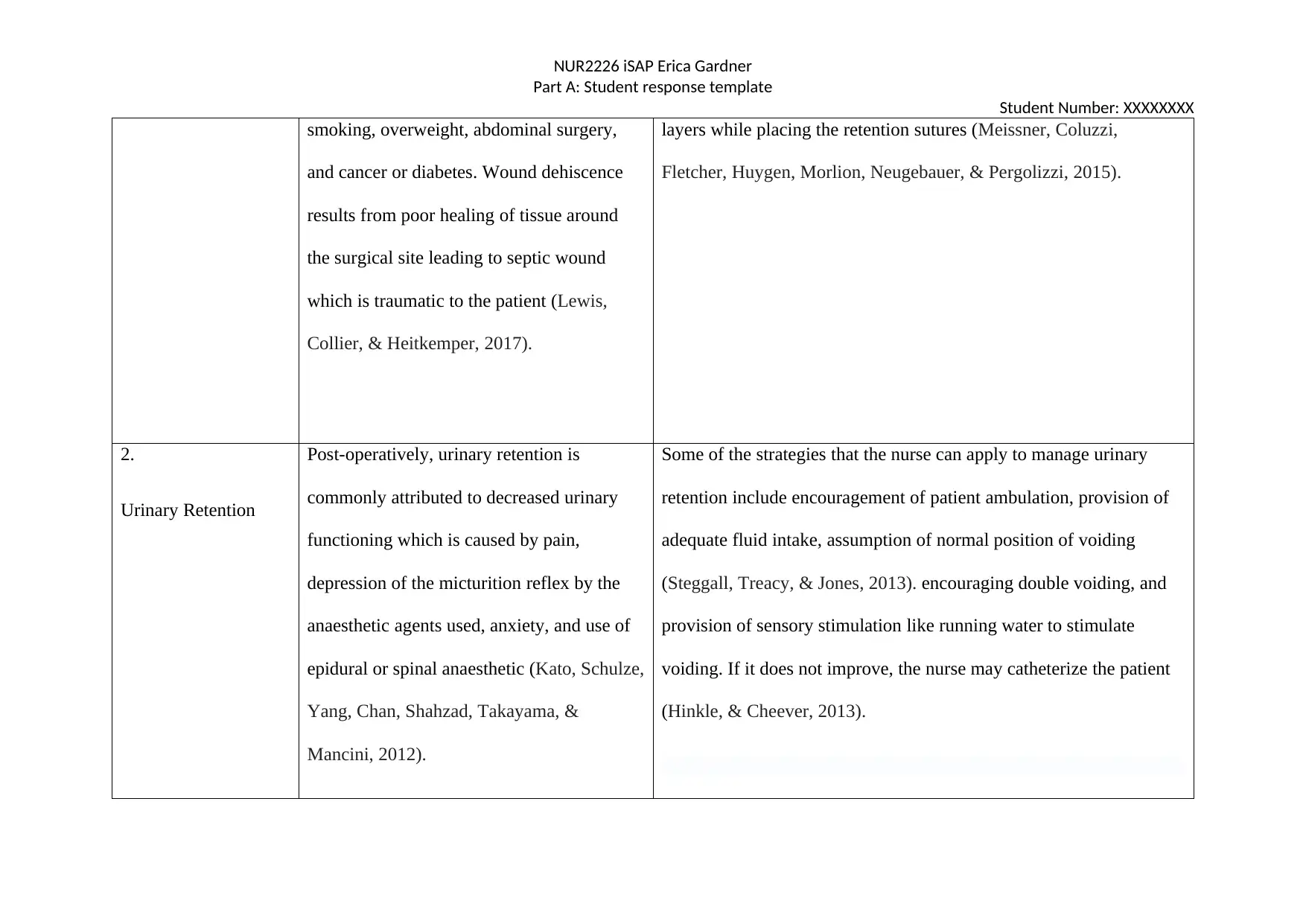
1. Wound infection
and Dehiscence
Wound infection is commonly caused by
bacteria especially the Staphylococcus,
pseudomonas, and streptococcus. The
microorganisms can enter the surgical
wound through contaminated surgical
instrument, non-sterile caregiver, and those
in the air or on her body. Some of the risk
factors for Surgical wound infections include
surgery lasting for more than two hours,
To manage the potential complication of wound infection, the nurse
can administer antiobiotics to kill the bacteria. The nurse should
always adhere to the guidelines of aseptic techniques to prevent
wound infection. The nurse should enlighten the patient on the
maintenance of the hygiene for wound by avoiding entry of
contaminated water and dust particles. The nurse should regularly
change the dressings as indicated by the medical officer or surgeon.
The wound dehiscence can be managed through emergent restoration
of the integrity of the abdominal wall by re-suturing the aponeurotic
Part A: Student response template
Student Number: XXXXXXXX
Potential post-
operative
complications
Explanation of two (2) of the potential
post-operative complications specific to
Erica
Nursing management of potential complication
1. Wound infection
and Dehiscence
Wound infection is commonly caused by
bacteria especially the Staphylococcus,
pseudomonas, and streptococcus. The
microorganisms can enter the surgical
wound through contaminated surgical
instrument, non-sterile caregiver, and those
in the air or on her body. Some of the risk
factors for Surgical wound infections include
surgery lasting for more than two hours,
To manage the potential complication of wound infection, the nurse
can administer antiobiotics to kill the bacteria. The nurse should
always adhere to the guidelines of aseptic techniques to prevent
wound infection. The nurse should enlighten the patient on the
maintenance of the hygiene for wound by avoiding entry of
contaminated water and dust particles. The nurse should regularly
change the dressings as indicated by the medical officer or surgeon.
The wound dehiscence can be managed through emergent restoration
of the integrity of the abdominal wall by re-suturing the aponeurotic
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NUR2226 iSAP Erica Gardner
Part A: Student response template
Student Number: XXXXXXXX
smoking, overweight, abdominal surgery,
and cancer or diabetes. Wound dehiscence
results from poor healing of tissue around
the surgical site leading to septic wound
which is traumatic to the patient (Lewis,
Collier, & Heitkemper, 2017).
layers while placing the retention sutures (Meissner, Coluzzi,
Fletcher, Huygen, Morlion, Neugebauer, & Pergolizzi, 2015).
2.
Urinary Retention
Post-operatively, urinary retention is
commonly attributed to decreased urinary
functioning which is caused by pain,
depression of the micturition reflex by the
anaesthetic agents used, anxiety, and use of
epidural or spinal anaesthetic (Kato, Schulze,
Yang, Chan, Shahzad, Takayama, &
Mancini, 2012).
Some of the strategies that the nurse can apply to manage urinary
retention include encouragement of patient ambulation, provision of
adequate fluid intake, assumption of normal position of voiding
(Steggall, Treacy, & Jones, 2013). encouraging double voiding, and
provision of sensory stimulation like running water to stimulate
voiding. If it does not improve, the nurse may catheterize the patient
(Hinkle, & Cheever, 2013).
Part A: Student response template
Student Number: XXXXXXXX
smoking, overweight, abdominal surgery,
and cancer or diabetes. Wound dehiscence
results from poor healing of tissue around
the surgical site leading to septic wound
which is traumatic to the patient (Lewis,
Collier, & Heitkemper, 2017).
layers while placing the retention sutures (Meissner, Coluzzi,
Fletcher, Huygen, Morlion, Neugebauer, & Pergolizzi, 2015).
2.
Urinary Retention
Post-operatively, urinary retention is
commonly attributed to decreased urinary
functioning which is caused by pain,
depression of the micturition reflex by the
anaesthetic agents used, anxiety, and use of
epidural or spinal anaesthetic (Kato, Schulze,
Yang, Chan, Shahzad, Takayama, &
Mancini, 2012).
Some of the strategies that the nurse can apply to manage urinary
retention include encouragement of patient ambulation, provision of
adequate fluid intake, assumption of normal position of voiding
(Steggall, Treacy, & Jones, 2013). encouraging double voiding, and
provision of sensory stimulation like running water to stimulate
voiding. If it does not improve, the nurse may catheterize the patient
(Hinkle, & Cheever, 2013).
NUR2226 iSAP Erica Gardner
Part A: Student response template
Student Number: XXXXXXXX
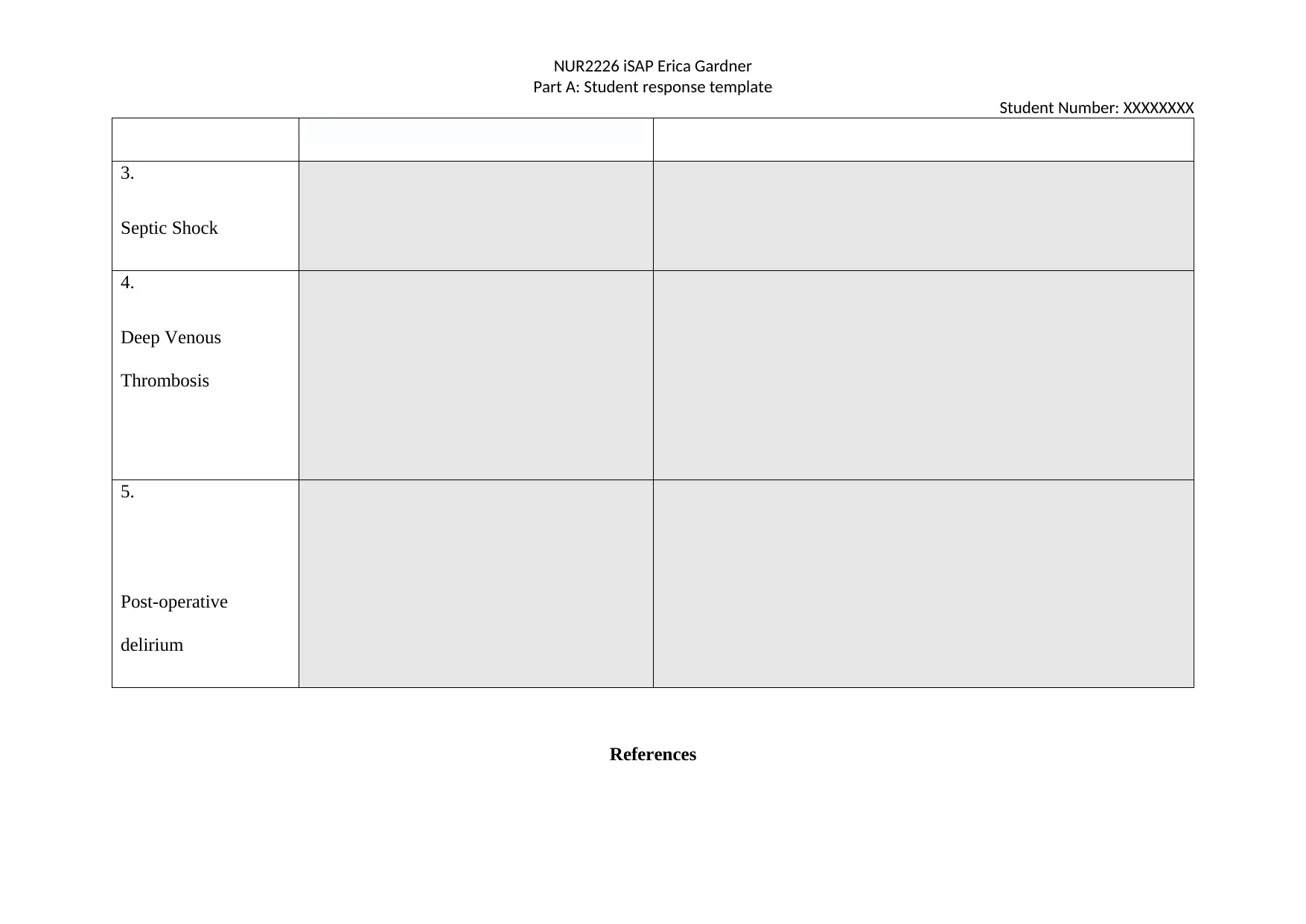
3.
Septic Shock
4.
Deep Venous
Thrombosis
5.
Post-operative
delirium
References
Part A: Student response template
Student Number: XXXXXXXX
3.
Septic Shock
4.
Deep Venous
Thrombosis
5.
Post-operative
delirium
References
NUR2226 iSAP Erica Gardner
Part A: Student response template
Student Number: XXXXXXXX
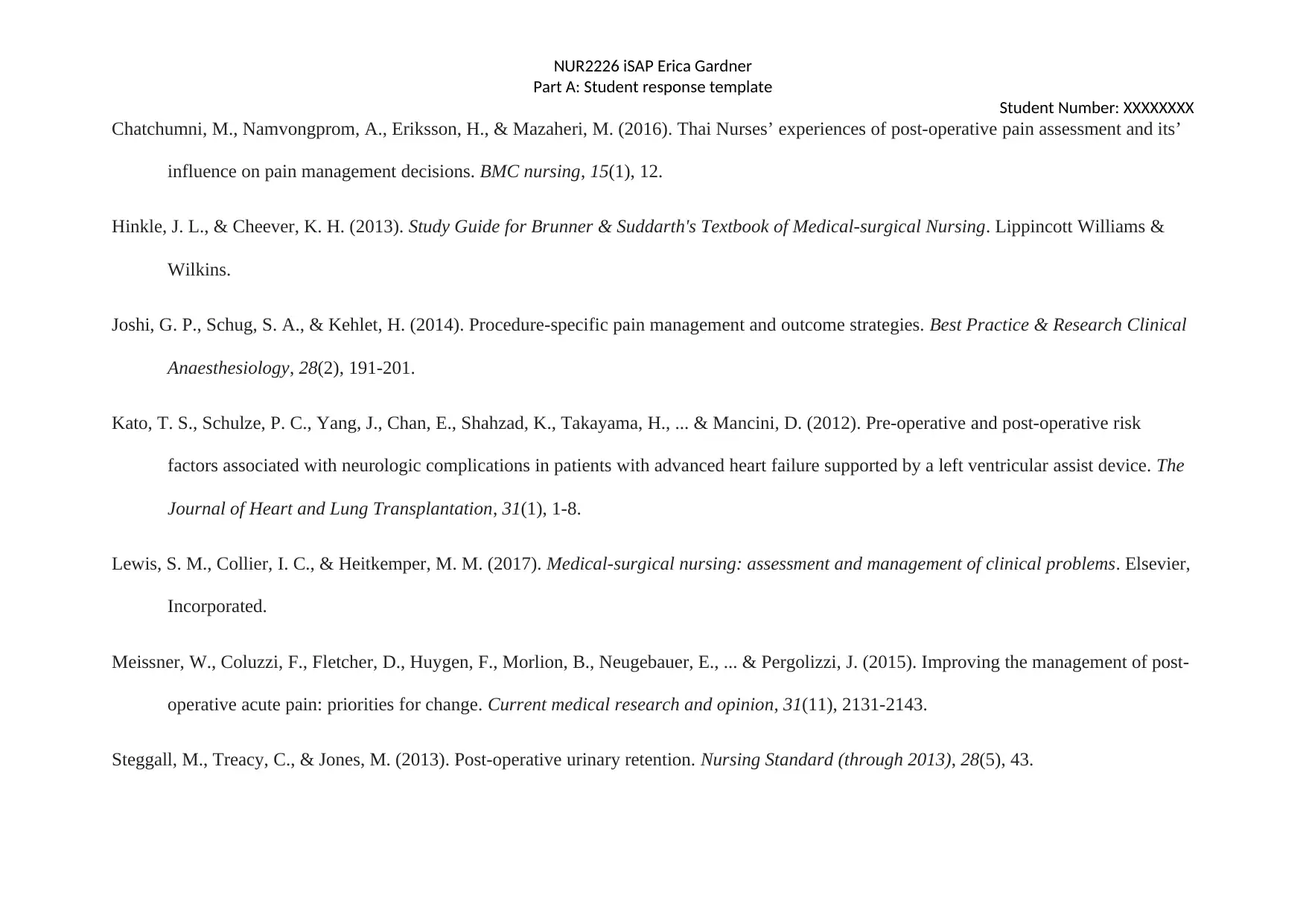
Chatchumni, M., Namvongprom, A., Eriksson, H., & Mazaheri, M. (2016). Thai Nurses’ experiences of post-operative pain assessment and its’
influence on pain management decisions. BMC nursing, 15(1), 12.
Hinkle, J. L., & Cheever, K. H. (2013). Study Guide for Brunner & Suddarth's Textbook of Medical-surgical Nursing. Lippincott Williams &
Wilkins.
Joshi, G. P., Schug, S. A., & Kehlet, H. (2014). Procedure-specific pain management and outcome strategies. Best Practice & Research Clinical
Anaesthesiology, 28(2), 191-201.
Kato, T. S., Schulze, P. C., Yang, J., Chan, E., Shahzad, K., Takayama, H., ... & Mancini, D. (2012). Pre-operative and post-operative risk
factors associated with neurologic complications in patients with advanced heart failure supported by a left ventricular assist device. The
Journal of Heart and Lung Transplantation, 31(1), 1-8.
Lewis, S. M., Collier, I. C., & Heitkemper, M. M. (2017). Medical-surgical nursing: assessment and management of clinical problems. Elsevier,
Incorporated.
Meissner, W., Coluzzi, F., Fletcher, D., Huygen, F., Morlion, B., Neugebauer, E., ... & Pergolizzi, J. (2015). Improving the management of post-
operative acute pain: priorities for change. Current medical research and opinion, 31(11), 2131-2143.
Steggall, M., Treacy, C., & Jones, M. (2013). Post-operative urinary retention. Nursing Standard (through 2013), 28(5), 43.
Part A: Student response template
Student Number: XXXXXXXX
Chatchumni, M., Namvongprom, A., Eriksson, H., & Mazaheri, M. (2016). Thai Nurses’ experiences of post-operative pain assessment and its’
influence on pain management decisions. BMC nursing, 15(1), 12.
Hinkle, J. L., & Cheever, K. H. (2013). Study Guide for Brunner & Suddarth's Textbook of Medical-surgical Nursing. Lippincott Williams &
Wilkins.
Joshi, G. P., Schug, S. A., & Kehlet, H. (2014). Procedure-specific pain management and outcome strategies. Best Practice & Research Clinical
Anaesthesiology, 28(2), 191-201.
Kato, T. S., Schulze, P. C., Yang, J., Chan, E., Shahzad, K., Takayama, H., ... & Mancini, D. (2012). Pre-operative and post-operative risk
factors associated with neurologic complications in patients with advanced heart failure supported by a left ventricular assist device. The
Journal of Heart and Lung Transplantation, 31(1), 1-8.
Lewis, S. M., Collier, I. C., & Heitkemper, M. M. (2017). Medical-surgical nursing: assessment and management of clinical problems. Elsevier,
Incorporated.
Meissner, W., Coluzzi, F., Fletcher, D., Huygen, F., Morlion, B., Neugebauer, E., ... & Pergolizzi, J. (2015). Improving the management of post-
operative acute pain: priorities for change. Current medical research and opinion, 31(11), 2131-2143.
Steggall, M., Treacy, C., & Jones, M. (2013). Post-operative urinary retention. Nursing Standard (through 2013), 28(5), 43.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NUR2226 iSAP Erica Gardner
Part A: Student response template
Student Number: XXXXXXXX
Wilson, L., Orff, S., Gerry, T., Shirley, B. R., Tabor, D., Caiazzo, K., & Rouleau, D. (2013). Evolution of an innovative role: the clinical nurse
leader. Journal of Nursing Management, 21(1), 175-181.
Part A: Student response template
Student Number: XXXXXXXX
Wilson, L., Orff, S., Gerry, T., Shirley, B. R., Tabor, D., Caiazzo, K., & Rouleau, D. (2013). Evolution of an innovative role: the clinical nurse
leader. Journal of Nursing Management, 21(1), 175-181.
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




