Nursing Assignment: Case Studies and Health Education
VerifiedAdded on 2023/06/11
|46
|12534
|185
AI Summary
This nursing assignment covers case studies on quality measures, discharge planning, ethical dilemmas, and further assessments required for patients. It also includes a health education plan for infection control.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NURSING ASSIGNMENT
Case Studies
Name of the Student
Name of the University
Author Note
Case Studies
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1
NURSING ASSIGNMENT
Case study, Chapter 1
a)
Quality measures refer to that facilitate the measurement or quantification of major
healthcare processes, patient perceptions, outcomes, and organizational structure or systems,
associated with the capability of providing high-quality health care services. These major goals
include safe, effective, patient-centred, equitable, efficient, and timely care. Some of the tools
that can be used to determine the quality of the care services being delivered include the Hospital
Inpatient Quality Reporting (IQR) Program. The IQR involves collection of quality data from the
hospital with the aim of driving quality improvement by transparency and measurement of the
data that were publicly displayed, for helping the patient and her family to make informed
decisions about healthcare. This in turn would also encourage the hospital to improve the cost of
inpatient care that was provided to Suzanne Jones. The cost effectiveness of the care delivered to
the patient could be evaluated by performing a Cost-Effectiveness Analysis (CEA) that would
estimate the health gains and costs of the intervention being implemented in the scenario. This
would create provisions for quantification of the net cost associated with the interventions and
would also help in conducting an assessment of the costs per disability-adjusted life year of the
patient. The Consumer Assessment of Healthcare Providers and Systems (CAHPS) program can
also be put to use for quality measurement of the delivered healthcare services. This would
promote the use of surveys, encompassing the experience of the consumer or service user. It
would address a range of healthcare services and utilise comparative information, thereby
assisting the healthcare professionals to evaluate and improve their performance. The Six
Sigma/Toyota Production System will also help in decreasing the defects and operating costs of
the healthcare service, while improving the patient outcomes. Furthermore, the Lean Production
NURSING ASSIGNMENT
Case study, Chapter 1
a)
Quality measures refer to that facilitate the measurement or quantification of major
healthcare processes, patient perceptions, outcomes, and organizational structure or systems,
associated with the capability of providing high-quality health care services. These major goals
include safe, effective, patient-centred, equitable, efficient, and timely care. Some of the tools
that can be used to determine the quality of the care services being delivered include the Hospital
Inpatient Quality Reporting (IQR) Program. The IQR involves collection of quality data from the
hospital with the aim of driving quality improvement by transparency and measurement of the
data that were publicly displayed, for helping the patient and her family to make informed
decisions about healthcare. This in turn would also encourage the hospital to improve the cost of
inpatient care that was provided to Suzanne Jones. The cost effectiveness of the care delivered to
the patient could be evaluated by performing a Cost-Effectiveness Analysis (CEA) that would
estimate the health gains and costs of the intervention being implemented in the scenario. This
would create provisions for quantification of the net cost associated with the interventions and
would also help in conducting an assessment of the costs per disability-adjusted life year of the
patient. The Consumer Assessment of Healthcare Providers and Systems (CAHPS) program can
also be put to use for quality measurement of the delivered healthcare services. This would
promote the use of surveys, encompassing the experience of the consumer or service user. It
would address a range of healthcare services and utilise comparative information, thereby
assisting the healthcare professionals to evaluate and improve their performance. The Six
Sigma/Toyota Production System will also help in decreasing the defects and operating costs of
the healthcare service, while improving the patient outcomes. Furthermore, the Lean Production
2
NURSING ASSIGNMENT
System would also play an integral role in identifying the needs of the patient and would work
towards improving the healthcare delivery by removing steps that non-value added and incurred
high costs.
b)
The ASPIRE tool is most essential in determining evidence based implementation of high
quality healthcare services to the patient, which in turn would improve the patient outcome and
satisfaction. The importance of this quality performance measurement tool lies in the fact that it
has been developed with the aim of assisting allied healthcare professionals for evaluating their
clinical performance, in terms of bringing about improvements in the quality of the healthcare
service, administered upon the patient. The importance of the tool can be attributed to the fact
that it manages to capture the integral elements of healthcare performance measurement that
includes upfront goal articulation, performance measure identification, clinical area
prioritisation, and mapping measures to major information sources. The fact that the care
delivered shows adherence to evidence based practice can be established by analysing the
performance data and reporting the patient results. Thus, the tool ASPIRE will make use of a
collaborative approach between the healthcare professionals and skilled researchers, which in
turn will facilitate the process of conducting an appropriate performance evaluation. Satisfaction
of the patient Suzanne Jones can be determined with the use of a patient satisfaction survey tool
that will bring about quality improvement. The PSQ-18 tool can be used for this purpose. It
generally encompasses survey questions on general satisfaction of the patients, technical quality
of care, interpersonal manner, communication, time spent with doctors, convenience and
accessibility, and financial aspects of the care. Computing the scores of the responses provided
by the patient Suzanne will help in providing an accurate overview of the satisfaction levels.
NURSING ASSIGNMENT
System would also play an integral role in identifying the needs of the patient and would work
towards improving the healthcare delivery by removing steps that non-value added and incurred
high costs.
b)
The ASPIRE tool is most essential in determining evidence based implementation of high
quality healthcare services to the patient, which in turn would improve the patient outcome and
satisfaction. The importance of this quality performance measurement tool lies in the fact that it
has been developed with the aim of assisting allied healthcare professionals for evaluating their
clinical performance, in terms of bringing about improvements in the quality of the healthcare
service, administered upon the patient. The importance of the tool can be attributed to the fact
that it manages to capture the integral elements of healthcare performance measurement that
includes upfront goal articulation, performance measure identification, clinical area
prioritisation, and mapping measures to major information sources. The fact that the care
delivered shows adherence to evidence based practice can be established by analysing the
performance data and reporting the patient results. Thus, the tool ASPIRE will make use of a
collaborative approach between the healthcare professionals and skilled researchers, which in
turn will facilitate the process of conducting an appropriate performance evaluation. Satisfaction
of the patient Suzanne Jones can be determined with the use of a patient satisfaction survey tool
that will bring about quality improvement. The PSQ-18 tool can be used for this purpose. It
generally encompasses survey questions on general satisfaction of the patients, technical quality
of care, interpersonal manner, communication, time spent with doctors, convenience and
accessibility, and financial aspects of the care. Computing the scores of the responses provided
by the patient Suzanne will help in providing an accurate overview of the satisfaction levels.
3
NURSING ASSIGNMENT
Thus, there is a need to focus on achieving excellent or high rating of patient satisfaction, which
in turn would provide assistance to the concerned healthcare professionals to improve the quality
of healthcare service delivery (Thayaparan & Mahdi, 2013).
Case Study, Chapter 2
a)
Discharge is usually coordinated and planned with the patient, family members and
associated healthcare agencies. However, several steps must be ensured by a nursing
professional, prior to discharge of the patient Mr. Jones after his right knee replacement. The
following preparations should be taken in advance by the nurse:
Educating the patient about his diagnosis and the reason why he was admitted to
the healthcare centre in the first place. Understanding the condition would help in
a better transition from the healthcare setting to home.
Thorough discussions must be conducted with the concerned surgeons and
physicians
The patient must be adequately informed about the prescribed medications, its
benefits, potential adverse effects, dosage and mode of administration.
Owing to the fact that Mr. Jones will be injected Lovenox subcutaneously daily,
proper instructions should be given to his daughter for the injection
administration.
He should also be educated on the usage of medical equipment, such as, walking
crutches or wheelchair
Adequate information must be provided on lifestyle changes, if required
NURSING ASSIGNMENT
Thus, there is a need to focus on achieving excellent or high rating of patient satisfaction, which
in turn would provide assistance to the concerned healthcare professionals to improve the quality
of healthcare service delivery (Thayaparan & Mahdi, 2013).
Case Study, Chapter 2
a)
Discharge is usually coordinated and planned with the patient, family members and
associated healthcare agencies. However, several steps must be ensured by a nursing
professional, prior to discharge of the patient Mr. Jones after his right knee replacement. The
following preparations should be taken in advance by the nurse:
Educating the patient about his diagnosis and the reason why he was admitted to
the healthcare centre in the first place. Understanding the condition would help in
a better transition from the healthcare setting to home.
Thorough discussions must be conducted with the concerned surgeons and
physicians
The patient must be adequately informed about the prescribed medications, its
benefits, potential adverse effects, dosage and mode of administration.
Owing to the fact that Mr. Jones will be injected Lovenox subcutaneously daily,
proper instructions should be given to his daughter for the injection
administration.
He should also be educated on the usage of medical equipment, such as, walking
crutches or wheelchair
Adequate information must be provided on lifestyle changes, if required
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

4
NURSING ASSIGNMENT
His daughter must be educated on procedures of cleaning or dressing the scars or
wounds
The nurse should also make use of a discharge checklist, which will facilitate a
seamless and smooth transition from the hospital to home.
b)
There are a range of community resources that would facilitate the seamless transfer of
the patient Mr. Jones to his home or community. Some of the major referral and resources that
are crucial in this context are as follows:
Medical equipment- These will help in an easier recovery and increase
independence of the patient, following the surgery.
Grocery delivery- Presence of such community resource would help in shopping
and delivering groceries to the home of Mr. Jones
Signing up for ready-to-eat meal services will greatly assist the patient
Healthcare facility websites will provide adequate information on orthopaedic
surgeons and allied health facilities.
Physiotherapists will help in restoring mobility and muscle strength of the patient
Frequent follow-up visits with the surgeon will help in reclaiming an active
lifestyle
Other referrals would include organisations that would install toilet safety frames,
grab bars, tub chairs, hand held shower head and tub transfer benches, which in
turn would assist the patient to seamlessly conduct the daily activities.
Elderly social clubs would also play an integral role in helping Mr. Jones to meet
up with friends, acquaintances and socialise with them. These will provide a range
NURSING ASSIGNMENT
His daughter must be educated on procedures of cleaning or dressing the scars or
wounds
The nurse should also make use of a discharge checklist, which will facilitate a
seamless and smooth transition from the hospital to home.
b)
There are a range of community resources that would facilitate the seamless transfer of
the patient Mr. Jones to his home or community. Some of the major referral and resources that
are crucial in this context are as follows:
Medical equipment- These will help in an easier recovery and increase
independence of the patient, following the surgery.
Grocery delivery- Presence of such community resource would help in shopping
and delivering groceries to the home of Mr. Jones
Signing up for ready-to-eat meal services will greatly assist the patient
Healthcare facility websites will provide adequate information on orthopaedic
surgeons and allied health facilities.
Physiotherapists will help in restoring mobility and muscle strength of the patient
Frequent follow-up visits with the surgeon will help in reclaiming an active
lifestyle
Other referrals would include organisations that would install toilet safety frames,
grab bars, tub chairs, hand held shower head and tub transfer benches, which in
turn would assist the patient to seamlessly conduct the daily activities.
Elderly social clubs would also play an integral role in helping Mr. Jones to meet
up with friends, acquaintances and socialise with them. These will provide a range
5
NURSING ASSIGNMENT
of activities that will eliminate isolation and improve the overall patient health
(Moffet et al., 2015).
Case Study, Chapter 3
a)
Ethical dilemma faced by nursing professionals are generally vast in their scope, while
caring for end-of-life patients. Oncology and hospice nurses can navigate several ethical
dilemmas by delivering best possible care services, while allowing the concerned patient,
caregivers, and family members adequate opportunities for experiencing end of life with dignity.
One major ethical dilemma that arose in this context can be attributed to the failure in deciding
about the treatment plan for the patient Mrs. Elle. Decision making is a complex process of
perceptions and thoughts and sets up a range of challenges for the concerned patient and families
to decide for end of life. Healthcare professionals have the general duty of displaying respect
towards the rights of the patient for making decisions about the course of medical care, without
creating an influence on the decision of the patient. However, in this context, owing to the old
age of the patient, the healthcare professionals could not convince the person with the durable
power of attorney for taking the necessary healthcare decision. Although Mrs.Elle had stated her
wish of not undergoing any kind of amputation, the hospice nurse suggested for blood
transfusion, which might increase her life expectancy and develop the need for right foot
amputation, in spite of low chances of surviving the surgery. This resulted in an ethical concern
over conducting blood transfusion based on the laboratory reports or preventing all labs, while
respecting the patient’s wishes of dying peacefully. Owing to the fact that the hospice nurse is
called on for acting as a mediator through difficult situation, compromising with the patient
autonomy, while trying to advocate for the patient, presents several ethical challenges.
NURSING ASSIGNMENT
of activities that will eliminate isolation and improve the overall patient health
(Moffet et al., 2015).
Case Study, Chapter 3
a)
Ethical dilemma faced by nursing professionals are generally vast in their scope, while
caring for end-of-life patients. Oncology and hospice nurses can navigate several ethical
dilemmas by delivering best possible care services, while allowing the concerned patient,
caregivers, and family members adequate opportunities for experiencing end of life with dignity.
One major ethical dilemma that arose in this context can be attributed to the failure in deciding
about the treatment plan for the patient Mrs. Elle. Decision making is a complex process of
perceptions and thoughts and sets up a range of challenges for the concerned patient and families
to decide for end of life. Healthcare professionals have the general duty of displaying respect
towards the rights of the patient for making decisions about the course of medical care, without
creating an influence on the decision of the patient. However, in this context, owing to the old
age of the patient, the healthcare professionals could not convince the person with the durable
power of attorney for taking the necessary healthcare decision. Although Mrs.Elle had stated her
wish of not undergoing any kind of amputation, the hospice nurse suggested for blood
transfusion, which might increase her life expectancy and develop the need for right foot
amputation, in spite of low chances of surviving the surgery. This resulted in an ethical concern
over conducting blood transfusion based on the laboratory reports or preventing all labs, while
respecting the patient’s wishes of dying peacefully. Owing to the fact that the hospice nurse is
called on for acting as a mediator through difficult situation, compromising with the patient
autonomy, while trying to advocate for the patient, presents several ethical challenges.
6
NURSING ASSIGNMENT
b)
The key stakeholders in this scenario are the patient Mrs. Elle, the power of attorney, the
hospice nurse, and the physician. The major gain that the patient has is associated with the fact
that in spite of being incapable of exerting end-of-life decisions, her previous statements
regarding a peaceful death and wish against having an amputation are being given proper
consideration. Moreover, the fact that she has appointed a power of attorney is also advantageous
as the latter has the comprehensive power of advocating for the rights of Mrs. Elle for her end-
of-life decisions. However, the fact that her current physical condition requires blood
transfusion, which might increase her lifespan, against her wish is a major loss. The power of
attorney also faces a loss that can be attributed to the advantage of blood transfusion in
increasing the life expectancy of the patient, against the wishes. Advocating for the patient will
make the power of attorney fail to consider the benefits of treatment. The physician and hospice
nurse are also at a loss due to the fact that in spite of treatment provisions that will help them
enhance the survival of their patients, they will have to maintain respect towards the autonomy of
the client (Karlsson et al., 2013).
c)
During end of life care ethical dilemma might arise from a range of situations that
involve communication breakdown, compromise with patient autonomy, symptom management
inefficiency and shared decision making. The strategies to be adopted by the hospice nurse for
resolving the ethical dilemma include the following:
Identifying the ethical concern and defining guiding principles- The nurse will
have to adhere to the plethora of principles for biomedical ethics such as,
NURSING ASSIGNMENT
b)
The key stakeholders in this scenario are the patient Mrs. Elle, the power of attorney, the
hospice nurse, and the physician. The major gain that the patient has is associated with the fact
that in spite of being incapable of exerting end-of-life decisions, her previous statements
regarding a peaceful death and wish against having an amputation are being given proper
consideration. Moreover, the fact that she has appointed a power of attorney is also advantageous
as the latter has the comprehensive power of advocating for the rights of Mrs. Elle for her end-
of-life decisions. However, the fact that her current physical condition requires blood
transfusion, which might increase her lifespan, against her wish is a major loss. The power of
attorney also faces a loss that can be attributed to the advantage of blood transfusion in
increasing the life expectancy of the patient, against the wishes. Advocating for the patient will
make the power of attorney fail to consider the benefits of treatment. The physician and hospice
nurse are also at a loss due to the fact that in spite of treatment provisions that will help them
enhance the survival of their patients, they will have to maintain respect towards the autonomy of
the client (Karlsson et al., 2013).
c)
During end of life care ethical dilemma might arise from a range of situations that
involve communication breakdown, compromise with patient autonomy, symptom management
inefficiency and shared decision making. The strategies to be adopted by the hospice nurse for
resolving the ethical dilemma include the following:
Identifying the ethical concern and defining guiding principles- The nurse will
have to adhere to the plethora of principles for biomedical ethics such as,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
NURSING ASSIGNMENT
nonmaleficence, autonomy, justice, beneficence, confidentiality, privacy and
veracity.
The hospice nurse should also advocate for a meeting with the family if the
patient, in addition to the power of attorney, with the aim of clarifying the goals
of care for Mrs. Elle, with the life-limiting condition.
The nurse should separate all kinds of emotional responses from the primary
objective issue, which in turn will facilitate the decision making process
Additional information should be gathered from the practice setting, followed by
their review and discussion with the patient Mrs. Elle and her power of attorney
over alternate treatment options.
The nurse should inform the power of attorney about the probable benefits and
risks of the transfusion therapy
Efforts must be taken for conflict resolution through collaboration that involves
mutual evaluation of health information and identification of the interest of the
stakeholders
The values, culture, and beliefs of Mrs. Elle must be recognised, which in turn
will create provisions for honouring the dignity of the client
The nurse should also take attempts at compromising if all stakeholders are
morally certain about their unique stand on the care
The ethical dilemma can also be addressed by contacting the healthcare executive,
for ensuring adherence to certain policies that must be followed while guiding the
patient and power of attorney to make informed treatment preferences, by sharing
trustful information and appropriate prognosis of the health abnormality
NURSING ASSIGNMENT
nonmaleficence, autonomy, justice, beneficence, confidentiality, privacy and
veracity.
The hospice nurse should also advocate for a meeting with the family if the
patient, in addition to the power of attorney, with the aim of clarifying the goals
of care for Mrs. Elle, with the life-limiting condition.
The nurse should separate all kinds of emotional responses from the primary
objective issue, which in turn will facilitate the decision making process
Additional information should be gathered from the practice setting, followed by
their review and discussion with the patient Mrs. Elle and her power of attorney
over alternate treatment options.
The nurse should inform the power of attorney about the probable benefits and
risks of the transfusion therapy
Efforts must be taken for conflict resolution through collaboration that involves
mutual evaluation of health information and identification of the interest of the
stakeholders
The values, culture, and beliefs of Mrs. Elle must be recognised, which in turn
will create provisions for honouring the dignity of the client
The nurse should also take attempts at compromising if all stakeholders are
morally certain about their unique stand on the care
The ethical dilemma can also be addressed by contacting the healthcare executive,
for ensuring adherence to certain policies that must be followed while guiding the
patient and power of attorney to make informed treatment preferences, by sharing
trustful information and appropriate prognosis of the health abnormality
8
NURSING ASSIGNMENT
A post-event reflection should also be exercised by the nurse for evaluating the
scenario and assessing the major outcomes of the decision making process.
Case Study, Case Study 4
a)
Further assessments required for Mr. Smith are as follows:
Systemic collection of subjective data that will involve gathering information
based on his perceptions about his common symptoms and health condition.
Efforts must be taken to collect data about his health history that will encompass a
holistic assessment of factors that include health status, social life, family history,
cultural background, biographic and demographic data, physical, emotional and
mental data.
All prescribed and nonprescribed medications taken by him should also be
documented
The patient must be subjected to a vital signs assessment
An enquiry should also be made about the past illnesses that require medical
attention or hospitalisation
b)
The topics that will be addressed while providing health education to the patient include
the following:
Starting with the basics and ensuring that he is performing the simplest of all
infection control practices appropriately
NURSING ASSIGNMENT
A post-event reflection should also be exercised by the nurse for evaluating the
scenario and assessing the major outcomes of the decision making process.
Case Study, Case Study 4
a)
Further assessments required for Mr. Smith are as follows:
Systemic collection of subjective data that will involve gathering information
based on his perceptions about his common symptoms and health condition.
Efforts must be taken to collect data about his health history that will encompass a
holistic assessment of factors that include health status, social life, family history,
cultural background, biographic and demographic data, physical, emotional and
mental data.
All prescribed and nonprescribed medications taken by him should also be
documented
The patient must be subjected to a vital signs assessment
An enquiry should also be made about the past illnesses that require medical
attention or hospitalisation
b)
The topics that will be addressed while providing health education to the patient include
the following:
Starting with the basics and ensuring that he is performing the simplest of all
infection control practices appropriately
9
NURSING ASSIGNMENT
Adequate measures should be taken to demonstrate the effectiveness of hand
hygiene practices for infection control
Effective communication will help Mr. Smith report his concerns on issues of
patient safety
Delivering safe water guidelines are also essential for this purpose (Johnson et al.,
2014)
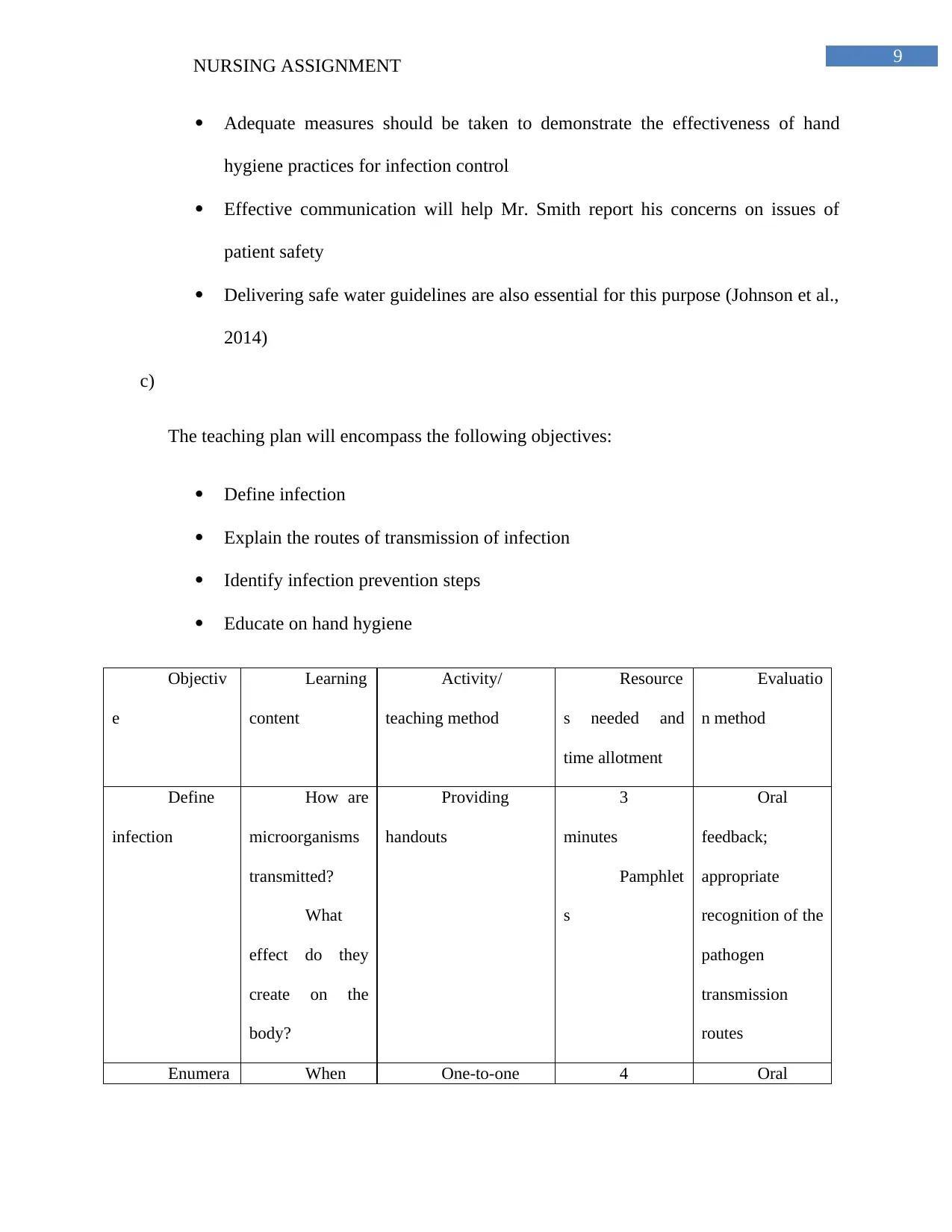
c)
The teaching plan will encompass the following objectives:
Define infection
Explain the routes of transmission of infection
Identify infection prevention steps
Educate on hand hygiene
Objectiv
e
Learning
content
Activity/
teaching method
Resource
s needed and
time allotment
Evaluatio
n method
Define
infection
How are
microorganisms
transmitted?
What
effect do they
create on the
body?
Providing
handouts
3
minutes
Pamphlet
s
Oral
feedback;
appropriate
recognition of the
pathogen
transmission
routes
Enumera When One-to-one 4 Oral
NURSING ASSIGNMENT
Adequate measures should be taken to demonstrate the effectiveness of hand
hygiene practices for infection control
Effective communication will help Mr. Smith report his concerns on issues of
patient safety
Delivering safe water guidelines are also essential for this purpose (Johnson et al.,
2014)
c)
The teaching plan will encompass the following objectives:
Define infection
Explain the routes of transmission of infection
Identify infection prevention steps
Educate on hand hygiene
Objectiv
e
Learning
content
Activity/
teaching method
Resource
s needed and
time allotment
Evaluatio
n method
Define
infection
How are
microorganisms
transmitted?
What
effect do they
create on the
body?
Providing
handouts
3
minutes
Pamphlet
s
Oral
feedback;
appropriate
recognition of the
pathogen
transmission
routes
Enumera When One-to-one 4 Oral
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
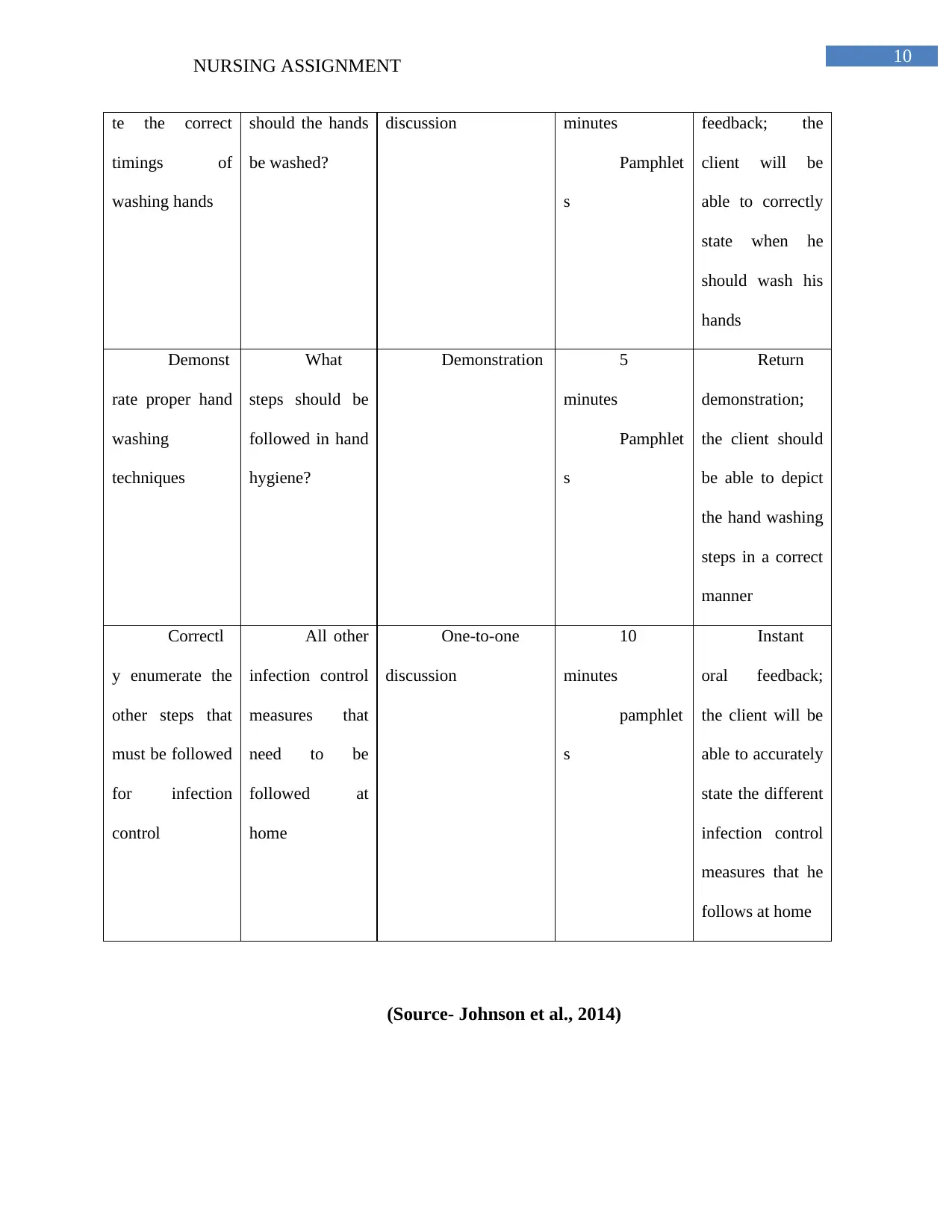
10
NURSING ASSIGNMENT
te the correct
timings of
washing hands
should the hands
be washed?
discussion minutes
Pamphlet
s
feedback; the
client will be
able to correctly
state when he
should wash his
hands
Demonst
rate proper hand
washing
techniques
What
steps should be
followed in hand
hygiene?
Demonstration 5
minutes
Pamphlet
s
Return
demonstration;
the client should
be able to depict
the hand washing
steps in a correct
manner
Correctl
y enumerate the
other steps that
must be followed
for infection
control
All other
infection control
measures that
need to be
followed at
home
One-to-one
discussion
10
minutes
pamphlet
s
Instant
oral feedback;
the client will be
able to accurately
state the different
infection control
measures that he
follows at home
(Source- Johnson et al., 2014)
NURSING ASSIGNMENT
te the correct
timings of
washing hands
should the hands
be washed?
discussion minutes
Pamphlet
s
feedback; the
client will be
able to correctly
state when he
should wash his
hands
Demonst
rate proper hand
washing
techniques
What
steps should be
followed in hand
hygiene?
Demonstration 5
minutes
Pamphlet
s
Return
demonstration;
the client should
be able to depict
the hand washing
steps in a correct
manner
Correctl
y enumerate the
other steps that
must be followed
for infection
control
All other
infection control
measures that
need to be
followed at
home
One-to-one
discussion
10
minutes
pamphlet
s
Instant
oral feedback;
the client will be
able to accurately
state the different
infection control
measures that he
follows at home
(Source- Johnson et al., 2014)
11
NURSING ASSIGNMENT
Case Study, Chapter 5
a)
As Mrs Varner described herself as overweight (height- 64 inches and weight- 165
pounds) for most of her adult life, it is important to compute her BMI. Moreover, after
calculating her BMI, it is estimated to be 28.2, (BMI = Weight (kg)/Height (m)2) that are more
than the standard scale of 25 being overweight. According to World Health Organization
(WHO), the healthy BMI range is between 18.5 and 24.9 and Mrs. Varner is 28.2 above the
normal range. Therefore, by measuring her BMI, it is easy to know that she is underweight or
obese. Furthermore, by consuming proper nutrients, she can gain ideal weight and reduce the
increased disease risk in overweight conditions.
b)
The ideal body weight (IBW) for females is calculated by adding 45.5 kg and 2.3 kg for
each inch over 5 feet. IBW is considered healthy weight that is considered maximally healthy for
an individual that is based on height and influenced by factors like age, gender and build. Mrs
Varner is 165 pounds and after calculating the ideal weight as per her height (in inches), weight
(in pounds), gender and age, the healthy BMI recommended weight is 54.70 kg or 120.59
pounds. On a contrary, her weight is 165 pounds that is more than the standard ideal body weight
range and BMI and therefore, she is overweight. Height of 64 inches or 5’3” with 141 to 168 lbs
confirms that Mrs. Varner is overweight.
c)
NURSING ASSIGNMENT
Case Study, Chapter 5
a)
As Mrs Varner described herself as overweight (height- 64 inches and weight- 165
pounds) for most of her adult life, it is important to compute her BMI. Moreover, after
calculating her BMI, it is estimated to be 28.2, (BMI = Weight (kg)/Height (m)2) that are more
than the standard scale of 25 being overweight. According to World Health Organization
(WHO), the healthy BMI range is between 18.5 and 24.9 and Mrs. Varner is 28.2 above the
normal range. Therefore, by measuring her BMI, it is easy to know that she is underweight or
obese. Furthermore, by consuming proper nutrients, she can gain ideal weight and reduce the
increased disease risk in overweight conditions.
b)
The ideal body weight (IBW) for females is calculated by adding 45.5 kg and 2.3 kg for
each inch over 5 feet. IBW is considered healthy weight that is considered maximally healthy for
an individual that is based on height and influenced by factors like age, gender and build. Mrs
Varner is 165 pounds and after calculating the ideal weight as per her height (in inches), weight
(in pounds), gender and age, the healthy BMI recommended weight is 54.70 kg or 120.59
pounds. On a contrary, her weight is 165 pounds that is more than the standard ideal body weight
range and BMI and therefore, she is overweight. Height of 64 inches or 5’3” with 141 to 168 lbs
confirms that Mrs. Varner is overweight.
c)
12
NURSING ASSIGNMENT
Waist circumference measurement is an important anthropometric measurement in
nutritional assessment. The procedure for waist measurement is done to get a clue of whether an
individual is at high risk for high blood pressure, type 2 diabetes, heart disease and high
cholesterol. Firstly, clothing is removed from the waistline and Mrs. Varner should stand with
feet shoulder wide apart and back straight. The hipbone top is located that is present at the waist
side and not at the front of the body. The area between the index finger and thumb is used to get
the exact location of the hipbone at the side of waist. The bottom edge of measuring tape is
aligned with hipbone top. The tape is wrapped, measured all the way throughout the waist
ensuring that tape measurement is parallel to the floor and not in twisted position. After that, two
normal breaths are taken and exhale on second breath that tightens the tape ensuring snug and
not digging into the skin. Finally, the waist measurement is taken to the nearest one fourth inches
or 0.5 cm.
d)
The ideal waist circumference for best health is less than 40 inches for men and for
women, it is less than 35 inches. If the measurement is more than this normal range, this
indicates health risk linked with excess fat that is present around the waist. Mrs. Varner’s waist
circumference is 38 inches that is more than the normal range that indicates her health is at risk
as in women 31.5 inches or over 80 cm waist circumference is considered high risk level and
obese (Ashwell, Gunn & Gibson, 2012).
e)
Protein test is done for measuring the levels of globulin and albumin in the blood (A/G)
ratio. This test measures various protein types present in plasma or serum portion of the blood.
NURSING ASSIGNMENT
Waist circumference measurement is an important anthropometric measurement in
nutritional assessment. The procedure for waist measurement is done to get a clue of whether an
individual is at high risk for high blood pressure, type 2 diabetes, heart disease and high
cholesterol. Firstly, clothing is removed from the waistline and Mrs. Varner should stand with
feet shoulder wide apart and back straight. The hipbone top is located that is present at the waist
side and not at the front of the body. The area between the index finger and thumb is used to get
the exact location of the hipbone at the side of waist. The bottom edge of measuring tape is
aligned with hipbone top. The tape is wrapped, measured all the way throughout the waist
ensuring that tape measurement is parallel to the floor and not in twisted position. After that, two
normal breaths are taken and exhale on second breath that tightens the tape ensuring snug and
not digging into the skin. Finally, the waist measurement is taken to the nearest one fourth inches
or 0.5 cm.
d)
The ideal waist circumference for best health is less than 40 inches for men and for
women, it is less than 35 inches. If the measurement is more than this normal range, this
indicates health risk linked with excess fat that is present around the waist. Mrs. Varner’s waist
circumference is 38 inches that is more than the normal range that indicates her health is at risk
as in women 31.5 inches or over 80 cm waist circumference is considered high risk level and
obese (Ashwell, Gunn & Gibson, 2012).
e)
Protein test is done for measuring the levels of globulin and albumin in the blood (A/G)
ratio. This test measures various protein types present in plasma or serum portion of the blood.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13
NURSING ASSIGNMENT
The normal protein tests range is 6.3 - 7.9 g/dl irrespective of gender and age. The amount of
protein in blood is measured to check the liver or kidney functioning, as these proteins are
synthesized in this organ. In healthy individuals, there is little more albumin than globulin as
albumin is 60% of the total protein present in the body.
Case Study, Chapter 6
a)
The causes of local infection due to a nail puncture depend on puncture depth, site of
puncture and type of object. Inflammation is the living tissue responses to injury comprising of
well-organized cascade of reactions of cellular and fluid changes occurring within the living
tissues. There are sequences of events those results in local inflammation that comprises of three
main stages that made Mary experience pain, redness, oedema and yellowish discharge. The
acute phase (swelling stage) lasts for 3 days where the three cardinal signs are witnessed. In this
stage, swelling and redness occurs due to vascular changes. There is neutralization of chemical
irritants while sealing of area from the surrounding tissues along with impairment of circulation
takes place. There is also cell activity of early fibroblasts when pain occurs at rest and may be
aggravated due to activity. Guarding and muscle spasm greatly restrict the passive movement.
Nail puncture caused injury that led to surface swelling, redness and oedema that was noticeable.
This phase is followed by sub-acute phase (regenerative stage) lasting from three to 4 days
corresponding to cleaning phase prior to repair phase. When the sub-acute phase is not resolved,
the inflammation becomes chronic (maturation of scar tissue and remodelling stage).
b)
NURSING ASSIGNMENT
The normal protein tests range is 6.3 - 7.9 g/dl irrespective of gender and age. The amount of
protein in blood is measured to check the liver or kidney functioning, as these proteins are
synthesized in this organ. In healthy individuals, there is little more albumin than globulin as
albumin is 60% of the total protein present in the body.
Case Study, Chapter 6
a)
The causes of local infection due to a nail puncture depend on puncture depth, site of
puncture and type of object. Inflammation is the living tissue responses to injury comprising of
well-organized cascade of reactions of cellular and fluid changes occurring within the living
tissues. There are sequences of events those results in local inflammation that comprises of three
main stages that made Mary experience pain, redness, oedema and yellowish discharge. The
acute phase (swelling stage) lasts for 3 days where the three cardinal signs are witnessed. In this
stage, swelling and redness occurs due to vascular changes. There is neutralization of chemical
irritants while sealing of area from the surrounding tissues along with impairment of circulation
takes place. There is also cell activity of early fibroblasts when pain occurs at rest and may be
aggravated due to activity. Guarding and muscle spasm greatly restrict the passive movement.
Nail puncture caused injury that led to surface swelling, redness and oedema that was noticeable.
This phase is followed by sub-acute phase (regenerative stage) lasting from three to 4 days
corresponding to cleaning phase prior to repair phase. When the sub-acute phase is not resolved,
the inflammation becomes chronic (maturation of scar tissue and remodelling stage).
b)
14
NURSING ASSIGNMENT
Histamines and kinins released causes vasodilation and there is increased permeability by
the blood vessels. Blood clots may be formed around an abscess for the prevention of infection
dissemination. Histamine is a chemical that is present in body cells (mast cells) in circulating
basophils, connective tissue and blood platelets. The release of this chemical is a direct response
to injured cells containing it. This is also released when phagocytic granulocytes get attracted
towards the injury that in turn also produces chemicals causing histamine release. Histamine
causes immune response against foreign pathogens produced by mast cells and basophils in
connective tissues. Concisely, histamine increases the capillaries’ permeability to proteins and
white blood cells allowing them to engage infectious agents in infected tissues.
The kinin–kallikrein system is poorly understood in terms of hormonal system consisting
of blood proteins playing an important role in inflammation, regulation, blood pressure control
and pain. There is limited research in terms of understanding the relationship between blood
pressure systems and inflammation. They are considered as inflammatory mediators that also
causes vascular permeability and blood vessels dilation. They are small peptides that are
synthesized from kininogen that in turn is produced by kallikrein broken down by enzymes,
kininases (Weissmann, 2013).
c)
The cardinal signs occur in acute inflammation phase that is characterized by tumor
(swelling), rubor (redness), calor (increased heat), functio laesa (loss of function) and dolor
(pain). Redness is caused by small blood vessels dilation at the injury area. Chemical mediators
contributing to temperature rise at the injury site mediate fever. Heat is caused due to increased
blood flow in the areas and Mary experienced it in the peripheral parts like skin. Oedema or
NURSING ASSIGNMENT
Histamines and kinins released causes vasodilation and there is increased permeability by
the blood vessels. Blood clots may be formed around an abscess for the prevention of infection
dissemination. Histamine is a chemical that is present in body cells (mast cells) in circulating
basophils, connective tissue and blood platelets. The release of this chemical is a direct response
to injured cells containing it. This is also released when phagocytic granulocytes get attracted
towards the injury that in turn also produces chemicals causing histamine release. Histamine
causes immune response against foreign pathogens produced by mast cells and basophils in
connective tissues. Concisely, histamine increases the capillaries’ permeability to proteins and
white blood cells allowing them to engage infectious agents in infected tissues.
The kinin–kallikrein system is poorly understood in terms of hormonal system consisting
of blood proteins playing an important role in inflammation, regulation, blood pressure control
and pain. There is limited research in terms of understanding the relationship between blood
pressure systems and inflammation. They are considered as inflammatory mediators that also
causes vascular permeability and blood vessels dilation. They are small peptides that are
synthesized from kininogen that in turn is produced by kallikrein broken down by enzymes,
kininases (Weissmann, 2013).
c)
The cardinal signs occur in acute inflammation phase that is characterized by tumor
(swelling), rubor (redness), calor (increased heat), functio laesa (loss of function) and dolor
(pain). Redness is caused by small blood vessels dilation at the injury area. Chemical mediators
contributing to temperature rise at the injury site mediate fever. Heat is caused due to increased
blood flow in the areas and Mary experienced it in the peripheral parts like skin. Oedema or
15
NURSING ASSIGNMENT
swelling is caused by fluid accumulation outside blood vessels. Mary experienced pain as there
was tissue distortion caused by swelling and induced by inflammatory chemical mediators like
prostaglandins, serotonin and bradykinin. Loss of function results from pain inhibiting mobility
and preventing movement in that particular area.
d)
As Mary’s injury was 5 days old, it is important to asses for the systemic effects of
inflammation. The local injury and acute inflammation results in systemic effects where
inflammatory mediators or cytokines diffuse into extracellular compartments of fluid and starts
circulating in the blood. The effects comprises of acute inflammation like leukocytosis, fever and
vascular changes. As the infection occurred 5 days ago, the pathogen may escape to the
immediate tissue through lymphatic or circulatory system. The infection may spread to other
body parts as it may gain access through lymph vessels or lymphatic system. The pathogen may
have transported via bloodstream to other body parts through lymph drainage and circulatory
system. When the inflammation phase overwhelms Mary’s body, there is need for assessing the
systemic effects and its response on the body. This is important as infection can result in sepsis
due to widespread infection because of nail puncture. During acute inflammation phase, high
systemic effects can occur in acute-phase proteins. This is beneficial and comprises of effects
including increase in blood pressure, decreased sweating and loss of appetite.
Case Study, Chapter 7
a)
In the given case study, mother of the patient is bilingual and it can be assumed that she
can speak both English and Spanish. She can communicate well with Mrs. Perez as she only
NURSING ASSIGNMENT
swelling is caused by fluid accumulation outside blood vessels. Mary experienced pain as there
was tissue distortion caused by swelling and induced by inflammatory chemical mediators like
prostaglandins, serotonin and bradykinin. Loss of function results from pain inhibiting mobility
and preventing movement in that particular area.
d)
As Mary’s injury was 5 days old, it is important to asses for the systemic effects of
inflammation. The local injury and acute inflammation results in systemic effects where
inflammatory mediators or cytokines diffuse into extracellular compartments of fluid and starts
circulating in the blood. The effects comprises of acute inflammation like leukocytosis, fever and
vascular changes. As the infection occurred 5 days ago, the pathogen may escape to the
immediate tissue through lymphatic or circulatory system. The infection may spread to other
body parts as it may gain access through lymph vessels or lymphatic system. The pathogen may
have transported via bloodstream to other body parts through lymph drainage and circulatory
system. When the inflammation phase overwhelms Mary’s body, there is need for assessing the
systemic effects and its response on the body. This is important as infection can result in sepsis
due to widespread infection because of nail puncture. During acute inflammation phase, high
systemic effects can occur in acute-phase proteins. This is beneficial and comprises of effects
including increase in blood pressure, decreased sweating and loss of appetite.
Case Study, Chapter 7
a)
In the given case study, mother of the patient is bilingual and it can be assumed that she
can speak both English and Spanish. She can communicate well with Mrs. Perez as she only
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16
NURSING ASSIGNMENT
speaks Spanish. As she is a woman, it will be easier for her to communicate about the
hysterectomy procedure to the patient. Moreover, the interpreter is patient’s mother and
therefore, Mrs. Perez have complete faith and trust in her and feel assured that whatever is being
communicated is for her health and well-being.
b)
Transcultural nursing actions are required for the given case scenario where the nurse
need to be sensitive towards the family’s cultural differences. The nurse need to focus on the
patient’s needs and preferences showing respect to their Hispanic culture and asking them about
their beliefs and health related care practices. The nurse needs to explain the medical jargons and
surgery procedure in their native language via an interpreter. Cultural skills are required for the
nurse in order to collect cultural data that is relevant to Mrs. Perez Hispanic culture. As the
family wants to see a priest at the hospital before the surgery, the nurse should arrange Catholic
priest for the family. A Catholic priest celebrates the Ash Wednesday and can be helpful in
giving a spiritual direction to Mrs. Perez and her family before the surgery. As a nurse, one
should be culturally diverse and have knowledge about how to provide patient-centred and
individualized care to Mrs. Perez. This can be helpful in developing the patient plan of care
aligning to the cultural beliefs and preferences in providing care. Apart from priest arrangement,
the nurse should understand how cultural and religious beliefs align with the patient’s hospital
stay regrading fulfilment of personal needs, staff communication and treatment decisions
(Douglas et al., 2014).
Case Study, Chapter 8
a)
NURSING ASSIGNMENT
speaks Spanish. As she is a woman, it will be easier for her to communicate about the
hysterectomy procedure to the patient. Moreover, the interpreter is patient’s mother and
therefore, Mrs. Perez have complete faith and trust in her and feel assured that whatever is being
communicated is for her health and well-being.
b)
Transcultural nursing actions are required for the given case scenario where the nurse
need to be sensitive towards the family’s cultural differences. The nurse need to focus on the
patient’s needs and preferences showing respect to their Hispanic culture and asking them about
their beliefs and health related care practices. The nurse needs to explain the medical jargons and
surgery procedure in their native language via an interpreter. Cultural skills are required for the
nurse in order to collect cultural data that is relevant to Mrs. Perez Hispanic culture. As the
family wants to see a priest at the hospital before the surgery, the nurse should arrange Catholic
priest for the family. A Catholic priest celebrates the Ash Wednesday and can be helpful in
giving a spiritual direction to Mrs. Perez and her family before the surgery. As a nurse, one
should be culturally diverse and have knowledge about how to provide patient-centred and
individualized care to Mrs. Perez. This can be helpful in developing the patient plan of care
aligning to the cultural beliefs and preferences in providing care. Apart from priest arrangement,
the nurse should understand how cultural and religious beliefs align with the patient’s hospital
stay regrading fulfilment of personal needs, staff communication and treatment decisions
(Douglas et al., 2014).
Case Study, Chapter 8
a)
17
NURSING ASSIGNMENT
The genes present on the chromosomes in body cells provide the genetic information,
growth and body functioning. This genetic information is passed from one generation to next
called pattern of inheritance. In mutation, there is permanent alteration of genome nucleotide
sequences in the organism. Out of four, autosomal dominant inheritance takes place when the
mutated gene is dominant located on the autosomes or non-sex chromosomes. In this inheritance,
only one mutated gene is needed to make an individual get affected by this disorder. For
example, an individual with autosomal dominant disorder has 50% chance of having an affected
child with one dominant or mutated gene and 50% chance of having unaffected child with
recessive or normal genes.
In the given case study, familial hypercholesterolemia (FH) is inherited in Mr. Wayne’s
family in an autosomal dominant pattern. As Mr. Wayne’s father died of this disease and
brothers are taking medications for controlling their cholesterol levels, it is quite evident that he
is at risk of inheriting this disease. Mr. Wayne’s father carried an altered gene causing that
condition and therefore, had one in two (50%) chance of passing this altered gene to each of his
children (Mr. Wayne and his siblings). As Mr. Wayne’s inherited mutated copy of the gene from
one of his parents, it is evident that it is homozygous FH. This form of the disease is much more
severe as compared to heterozygous FH as Mr. Wayne’s children will inherit one copy of
mutated gene and will have heterozygous form of the disease.
b)
The mutation of the gene that causes FH is due to autosomal dominant pattern of
inheritance. In the given case study, it is evident that one parent with FH disorder has 50%
chance of passing the mutated gene to each of his children. As the mutated gene is dominant, Mr.
NURSING ASSIGNMENT
The genes present on the chromosomes in body cells provide the genetic information,
growth and body functioning. This genetic information is passed from one generation to next
called pattern of inheritance. In mutation, there is permanent alteration of genome nucleotide
sequences in the organism. Out of four, autosomal dominant inheritance takes place when the
mutated gene is dominant located on the autosomes or non-sex chromosomes. In this inheritance,
only one mutated gene is needed to make an individual get affected by this disorder. For
example, an individual with autosomal dominant disorder has 50% chance of having an affected
child with one dominant or mutated gene and 50% chance of having unaffected child with
recessive or normal genes.
In the given case study, familial hypercholesterolemia (FH) is inherited in Mr. Wayne’s
family in an autosomal dominant pattern. As Mr. Wayne’s father died of this disease and
brothers are taking medications for controlling their cholesterol levels, it is quite evident that he
is at risk of inheriting this disease. Mr. Wayne’s father carried an altered gene causing that
condition and therefore, had one in two (50%) chance of passing this altered gene to each of his
children (Mr. Wayne and his siblings). As Mr. Wayne’s inherited mutated copy of the gene from
one of his parents, it is evident that it is homozygous FH. This form of the disease is much more
severe as compared to heterozygous FH as Mr. Wayne’s children will inherit one copy of
mutated gene and will have heterozygous form of the disease.
b)
The mutation of the gene that causes FH is due to autosomal dominant pattern of
inheritance. In the given case study, it is evident that one parent with FH disorder has 50%
chance of passing the mutated gene to each of his children. As the mutated gene is dominant, Mr.
18
NURSING ASSIGNMENT
Wayne’s children will have FH as the gene is are located on the autosomes and not sex
chromosomes. Therefore, it does not matter that if the father or the mother has the mutated gene
or both are having it, it will be passed on the next generation, as it is autosomally dominant.
Considering the above situation, the nurse must understand that disclosing information
about risk for FH (hereditary disease) may affect Mr. Wayne and his family members. The nurse
needs to share this information without breaching of confidentiality and consider the potential
harms that are involved in disclosure. The nurse should be empathetic while responding to his
question focusing on the quality of the communication. Interpersonal skills are important as the
nurse need to understand him and his expressions. The nurse should communicate in a way that
makes him comfortable by showing sincere attention in understanding the concerns of Mr.
Wayne. Therefore, effective communication exhibited by the nurse is an important prerequisite
in establishing healthy therapeutic relationship and in expressing sincere concern for the patent
while disclosing the genetic information.
c)
In genetics, penetrance is the proportion of individuals who carries a particular allele or
variant of a genotype or gene that is expressed as an associated trait or phenotype. The
penetrance of a mutation that can cause disease is the proportion of individuals exhibiting
clinical symptoms with the mutation. In autosomal dominant pattern of inheritance, there is
complete penetrance as there is presentation of clinical symptoms in all the individuals having
the disease causing mutated gene. In the given case, FH has penetrance more than 90% and
therefore, more than 95% including Mr Wayne and his children will develop this disease. As FH
NURSING ASSIGNMENT
Wayne’s children will have FH as the gene is are located on the autosomes and not sex
chromosomes. Therefore, it does not matter that if the father or the mother has the mutated gene
or both are having it, it will be passed on the next generation, as it is autosomally dominant.
Considering the above situation, the nurse must understand that disclosing information
about risk for FH (hereditary disease) may affect Mr. Wayne and his family members. The nurse
needs to share this information without breaching of confidentiality and consider the potential
harms that are involved in disclosure. The nurse should be empathetic while responding to his
question focusing on the quality of the communication. Interpersonal skills are important as the
nurse need to understand him and his expressions. The nurse should communicate in a way that
makes him comfortable by showing sincere attention in understanding the concerns of Mr.
Wayne. Therefore, effective communication exhibited by the nurse is an important prerequisite
in establishing healthy therapeutic relationship and in expressing sincere concern for the patent
while disclosing the genetic information.
c)
In genetics, penetrance is the proportion of individuals who carries a particular allele or
variant of a genotype or gene that is expressed as an associated trait or phenotype. The
penetrance of a mutation that can cause disease is the proportion of individuals exhibiting
clinical symptoms with the mutation. In autosomal dominant pattern of inheritance, there is
complete penetrance as there is presentation of clinical symptoms in all the individuals having
the disease causing mutated gene. In the given case, FH has penetrance more than 90% and
therefore, more than 95% including Mr Wayne and his children will develop this disease. As FH
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
19
NURSING ASSIGNMENT
is highly penetrant, the symptoms exhibiting alleles are highly heritable showing the symptoms
of FH condition with 100% penetrance (Finsterer et al., 2012).
Case Study, Chapter 9
a)
The nursing considerations for Mr. Edward related to his disability are-
There is chance of pressure ulcer as the patient is wheelchair ridden
Further impairment of the sensory and motor functions so it needs to be
assessed every four hours
The nurse must consider the pain and fatigue- It may be due to Edward’s
long immobility, treatment, and mental health issues. The patient may
report pain above the level of injury as he may be lacking the relaxation
techniques
Risk of impaired skin integrity due to poor mobility of Edward, nurse
must assess the risk factor
The nurse must consider the cleanliness and dryness of the bed to protect
Edward’s body from infection
The nurse must consider the impaired urinary elimination in Edward due
to urinary stricture.
The nurse must consider the excess fluid volume and infection
Incontinence issues must be considered
NURSING ASSIGNMENT
is highly penetrant, the symptoms exhibiting alleles are highly heritable showing the symptoms
of FH condition with 100% penetrance (Finsterer et al., 2012).
Case Study, Chapter 9
a)
The nursing considerations for Mr. Edward related to his disability are-
There is chance of pressure ulcer as the patient is wheelchair ridden
Further impairment of the sensory and motor functions so it needs to be
assessed every four hours
The nurse must consider the pain and fatigue- It may be due to Edward’s
long immobility, treatment, and mental health issues. The patient may
report pain above the level of injury as he may be lacking the relaxation
techniques
Risk of impaired skin integrity due to poor mobility of Edward, nurse
must assess the risk factor
The nurse must consider the cleanliness and dryness of the bed to protect
Edward’s body from infection
The nurse must consider the impaired urinary elimination in Edward due
to urinary stricture.
The nurse must consider the excess fluid volume and infection
Incontinence issues must be considered
20
NURSING ASSIGNMENT
The nurse must also consider the patient’s knowledge deficit in regards to
self care and handling the disability related issues. The patent may have
incorrect information related to comorbidities or may incorrectly interpret
the information
b)
The nurse needs to educate patient on the techniques to prevent pressure sores such as
frequent change of positions and maintaining skin care. The nurse must refer Edward to physical
therapists to improve the mobility and strength. Learning exercises will help improve the
patient’s ROM as well as improve the fitness. It will help Edward to know how to move from
bed to a chair. There are other learning needs of Edward such as dressing and bathing as well as
other work related needs. Therefore, the nurse must refer Edward to the occupational therapists
to teach the work related skills. The nurse must educate the patient to manage the bowel
movement and urinate through bowel and bladder programs. The nurse must promote
opportunities for Edward to take part in commonly held life activities. The environment can be
barrier to follow the good health practices. The nurse can promote the patient health by
eliminating the environmental obstacles. To prevent anxiety and stress, Edward must be educated
to understand the medication management and cope with the side effects. Edward needs
education on good hygiene, and sleep habits. It will promote positive health behaviour. The
nurse must address the nutrition needs of the patient by educating on the appropriate diet to be
taken to prevent malnutrition. To address the pain related issues the patient needs education on
the comfort measures such as massage, warm, and change in position. Thus, the patient can
prevent pain by taking alternate actions. To prevent drop the patient may be given a retaining
NURSING ASSIGNMENT
The nurse must also consider the patient’s knowledge deficit in regards to
self care and handling the disability related issues. The patent may have
incorrect information related to comorbidities or may incorrectly interpret
the information
b)
The nurse needs to educate patient on the techniques to prevent pressure sores such as
frequent change of positions and maintaining skin care. The nurse must refer Edward to physical
therapists to improve the mobility and strength. Learning exercises will help improve the
patient’s ROM as well as improve the fitness. It will help Edward to know how to move from
bed to a chair. There are other learning needs of Edward such as dressing and bathing as well as
other work related needs. Therefore, the nurse must refer Edward to the occupational therapists
to teach the work related skills. The nurse must educate the patient to manage the bowel
movement and urinate through bowel and bladder programs. The nurse must promote
opportunities for Edward to take part in commonly held life activities. The environment can be
barrier to follow the good health practices. The nurse can promote the patient health by
eliminating the environmental obstacles. To prevent anxiety and stress, Edward must be educated
to understand the medication management and cope with the side effects. Edward needs
education on good hygiene, and sleep habits. It will promote positive health behaviour. The
nurse must address the nutrition needs of the patient by educating on the appropriate diet to be
taken to prevent malnutrition. To address the pain related issues the patient needs education on
the comfort measures such as massage, warm, and change in position. Thus, the patient can
prevent pain by taking alternate actions. To prevent drop the patient may be given a retaining
21
NURSING ASSIGNMENT
board and to prevent contractures, by using muscle orthopaedic, hand splints and circulations
(Benevides et al., 2017).
Case Study, Chapter 10
a)
Pressure ulcer is the localised injury to the skin on bony prominence caused by pressure
and by shear and friction. Skin overlying the coccyx, heels, feet, over the heads, buttocks, and
back of the head is the common area and the same is evident from Mrs. Adams. Pressure ulcer
arises by pressure applied to underlying soft tissue and is common when a person is bed ridden.
Reperfusion injury results in the inadequate blood supply which is the underlying
pathophysiology of the pressure ulcer. If the pressure is high enough it may damage the cell
membrane of the muscle cells. It starts with the reddening of the area as observed in case of
Mrs. Adams. The skin is fed through blood vessels and the muscle cell dies causing deep tissue
injury.
Mrs Adam had reddened areas on her coccyx and heels due to pressure lying on bed. The
risk factor for pressure ulcer is malnutrition. In the given case, Mrs Adam, does not eat and
drink, which may be sign of malnutrition. Malnutrition makes the skin less resilience and prone
to damage or tear. Rubbing and friction makes the skin easily vulnerable to tear and pressure
sores. In case of Mrs. Adams it was found the patients is regularly dragged on to bed when she
slid down. The force adds to pressure on skin and patient skin being thin easily prone to tear. It
is because good muscle mass acts as a cushion over the bony areas. However, with loss of
muscle mass, the skin becomes thin and there is less natural padding to protect the body areas. It
NURSING ASSIGNMENT
board and to prevent contractures, by using muscle orthopaedic, hand splints and circulations
(Benevides et al., 2017).
Case Study, Chapter 10
a)
Pressure ulcer is the localised injury to the skin on bony prominence caused by pressure
and by shear and friction. Skin overlying the coccyx, heels, feet, over the heads, buttocks, and
back of the head is the common area and the same is evident from Mrs. Adams. Pressure ulcer
arises by pressure applied to underlying soft tissue and is common when a person is bed ridden.
Reperfusion injury results in the inadequate blood supply which is the underlying
pathophysiology of the pressure ulcer. If the pressure is high enough it may damage the cell
membrane of the muscle cells. It starts with the reddening of the area as observed in case of
Mrs. Adams. The skin is fed through blood vessels and the muscle cell dies causing deep tissue
injury.
Mrs Adam had reddened areas on her coccyx and heels due to pressure lying on bed. The
risk factor for pressure ulcer is malnutrition. In the given case, Mrs Adam, does not eat and
drink, which may be sign of malnutrition. Malnutrition makes the skin less resilience and prone
to damage or tear. Rubbing and friction makes the skin easily vulnerable to tear and pressure
sores. In case of Mrs. Adams it was found the patients is regularly dragged on to bed when she
slid down. The force adds to pressure on skin and patient skin being thin easily prone to tear. It
is because good muscle mass acts as a cushion over the bony areas. However, with loss of
muscle mass, the skin becomes thin and there is less natural padding to protect the body areas. It
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
22
NURSING ASSIGNMENT
makes the skin to easily break down even in small amount of pressure. Less body mass thus
gives less protection and more pressure on the thin skin layers.
Mrs Adams has paralysis, which is disease known to reduce the skin sensation and reduce
the healing of pressure ulcer. It is due to reduction in blood flow to the paralysed part of body,
reducing the nutrients and preventing skin nourishment. In normal condition the nerves sends the
messages of pain and discomfort, while signalling the brain to shift position due to pressure.
However, due to paralysis, Mrs Adams does not feel senses and no warning signs reach the brain
when the skin is facing pressure. In addition the age of the patient is also the risk factor for
slowing of the healing of pressure ulcers. Mrs Adams is 72 years and may at increased
vulnerability to pressure ulcer. Critical illness also hinders the detection and prevention of
pressure ulcer and treatment. Immobility is one of the major risk factors of pressure ulcer. In case
of Mrs Adams, she was diagnosed with stroke, and paralysed on right side. Lack of feeling in
right side of body makes the pressure ulcer difficulty in detecting and treatment. The primary
prevention of the pressure ulcer is repositioning of the patient frequently. However, Mrs Adams
refuses to reposition on bed which is the cause of increases in pressure ulcer. The other cause of
the pressure ulcer is the urinary incontinence. Urine turns to ammonia and is erosive to the skin
and speed up breakdown.
b)
Nursing measures for the patient in this condition includes –
The nurse must assess the specific risk factors for pressure ulcer development and
determine the general condition of the skin
The nurse must assess the serum albumin levels and asses the client’s weight loss
NURSING ASSIGNMENT
makes the skin to easily break down even in small amount of pressure. Less body mass thus
gives less protection and more pressure on the thin skin layers.
Mrs Adams has paralysis, which is disease known to reduce the skin sensation and reduce
the healing of pressure ulcer. It is due to reduction in blood flow to the paralysed part of body,
reducing the nutrients and preventing skin nourishment. In normal condition the nerves sends the
messages of pain and discomfort, while signalling the brain to shift position due to pressure.
However, due to paralysis, Mrs Adams does not feel senses and no warning signs reach the brain
when the skin is facing pressure. In addition the age of the patient is also the risk factor for
slowing of the healing of pressure ulcers. Mrs Adams is 72 years and may at increased
vulnerability to pressure ulcer. Critical illness also hinders the detection and prevention of
pressure ulcer and treatment. Immobility is one of the major risk factors of pressure ulcer. In case
of Mrs Adams, she was diagnosed with stroke, and paralysed on right side. Lack of feeling in
right side of body makes the pressure ulcer difficulty in detecting and treatment. The primary
prevention of the pressure ulcer is repositioning of the patient frequently. However, Mrs Adams
refuses to reposition on bed which is the cause of increases in pressure ulcer. The other cause of
the pressure ulcer is the urinary incontinence. Urine turns to ammonia and is erosive to the skin
and speed up breakdown.
b)
Nursing measures for the patient in this condition includes –
The nurse must assess the specific risk factors for pressure ulcer development and
determine the general condition of the skin
The nurse must assess the serum albumin levels and asses the client’s weight loss
23
NURSING ASSIGNMENT
Daily skin assessment is required for monitoring the increasing number of risk
factors such as environmental moisture
The nurse must apply the local vasodilator for increasing the skin circulation
To prevent the shear and friction the nurse may apply the flexible hydrocolloid
dressing or a vapour permeable dressings for skin moisturiser
The nurse may apply the vitamin enriched emollient every day for moisturising
skin
The nurse may provide the negative pressure wound therapy a wound dressing
system that continuously applies the subatmospheric pressure to the wound
surface to assist healing (Moore et al., 2015).
Case Study, Chapter 11
a)
Factors causing urinary incontinence in Mrs Jones are-
Weakening of the pelvic floor muscles or overactive bladder muscle
It may also be possible that the patient is recognising the urge to void but cannot
access the toileting facility on time due to bed ridden or disability or illness and is
need of support. It may be the reason that the patients is crying “I never should
have come to the senior centre”
Damage to the nerves due to conditions like multiple sclerosis delay the
transmission of nerve signals involved in bladder control
NURSING ASSIGNMENT
Daily skin assessment is required for monitoring the increasing number of risk
factors such as environmental moisture
The nurse must apply the local vasodilator for increasing the skin circulation
To prevent the shear and friction the nurse may apply the flexible hydrocolloid
dressing or a vapour permeable dressings for skin moisturiser
The nurse may apply the vitamin enriched emollient every day for moisturising
skin
The nurse may provide the negative pressure wound therapy a wound dressing
system that continuously applies the subatmospheric pressure to the wound
surface to assist healing (Moore et al., 2015).
Case Study, Chapter 11
a)
Factors causing urinary incontinence in Mrs Jones are-
Weakening of the pelvic floor muscles or overactive bladder muscle
It may also be possible that the patient is recognising the urge to void but cannot
access the toileting facility on time due to bed ridden or disability or illness and is
need of support. It may be the reason that the patients is crying “I never should
have come to the senior centre”
Damage to the nerves due to conditions like multiple sclerosis delay the
transmission of nerve signals involved in bladder control
24
NURSING ASSIGNMENT
Older people are highly represented in Alzheimer’s disease which prevents the
transmission of messages between the brain and bladder. It results in loss of
control in emptying the bladder or bowel
In older patients this problem is very common as they fail to recognise the urge to
void.
b)
The nurse may empathise with Mrs Jones and console her explaining her illness and
reassure to treat. The nurse may conduct a holistic assessment to promote continence to Mrs
Jones. The nurse may complete a focused record of the problem such as leakage episode, and
other aggravating factors. The nurse may assess the patient’s ability to recognise the need to
void. The nurse may determine if there is any irreversible cause of the urinary incontinence
(transient or acute). The nurse may help Mrs Jones by recording the voiding and the optimum
time between the visits. The nurse may initially instigate the short toileting time. The nurse may
respond to this situation in the patient centered manner.
With the help of the specialist continence nurse, a regular toileting programme must be
developed for emptying bladder before the incontinence occurs. The patient’s dignity may be
preserved by using absorbent body worn pads. It might give the patient a sense of independence.
In case the patient has persistent urinary retention, the nurse may use catheters with the patient’s
consent. As the long dwelling catheter is associated with many complications such as leakage
and infection, the nurse may consider using the intermittent catheterisation for emptying the
bladder. If the patient is not in mental capacity to carry out then indwelling catheter may be used.
NURSING ASSIGNMENT
Older people are highly represented in Alzheimer’s disease which prevents the
transmission of messages between the brain and bladder. It results in loss of
control in emptying the bladder or bowel
In older patients this problem is very common as they fail to recognise the urge to
void.
b)
The nurse may empathise with Mrs Jones and console her explaining her illness and
reassure to treat. The nurse may conduct a holistic assessment to promote continence to Mrs
Jones. The nurse may complete a focused record of the problem such as leakage episode, and
other aggravating factors. The nurse may assess the patient’s ability to recognise the need to
void. The nurse may determine if there is any irreversible cause of the urinary incontinence
(transient or acute). The nurse may help Mrs Jones by recording the voiding and the optimum
time between the visits. The nurse may initially instigate the short toileting time. The nurse may
respond to this situation in the patient centered manner.
With the help of the specialist continence nurse, a regular toileting programme must be
developed for emptying bladder before the incontinence occurs. The patient’s dignity may be
preserved by using absorbent body worn pads. It might give the patient a sense of independence.
In case the patient has persistent urinary retention, the nurse may use catheters with the patient’s
consent. As the long dwelling catheter is associated with many complications such as leakage
and infection, the nurse may consider using the intermittent catheterisation for emptying the
bladder. If the patient is not in mental capacity to carry out then indwelling catheter may be used.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
25
NURSING ASSIGNMENT
The nurse may ensure the availability of the toileting facility. The nurse may decrease the
patient’s distance of bed or chair from the toilet. The patients should be provided with alarm to
immediately call for the nurse during emergency and also provide the physical assistive devices
such as wheelchair to increase mobility and for functional continence. It may help remove
environmental barriers. The nurse must assess the patient’s strength to remove clothing to urinate
and accordingly respond to it by promoting optimal toilet access. The nurse may help the patient
to reduce the fluid intake beefier bed time (Hälleberg et al., 2017).
Case Study, Chapter 12
a)
Considering the age of the Mr Wills he may be administered with morphine instead of
Oxycodone as the former is more effective in lowering the pain. When compared to the
Oxycodone, Morphine is the stronger opioid. In the pain management plan the nurse must
mention that the patient should be given a less load of medicine. The patient being aged and
having undergone recent surgery needs lesser load of medicine which is possible by morphine.
Morphine will decrease the need of drug metabolism. Higher dose of the Oxycodone 10 mg
every 4 hours PRN may be given if the patient is opioid tolerant. However, with morphine a less
dosage can be administered. Morphine is effective for both moderate to severe pain. The nurse
must monitor the viral signs to address any adverse effects such as respiratory depression. The
nurse may monitor the signs of convulsions in patients. To ensure medication adherence the
nurse may educate the patient about taking medicines in right dosage and on time. ER or
extended release formulations are a viable option for acute to severe pain. It ensures compliance
and less clock watching due to simpler dosing schedule.
NURSING ASSIGNMENT
The nurse may ensure the availability of the toileting facility. The nurse may decrease the
patient’s distance of bed or chair from the toilet. The patients should be provided with alarm to
immediately call for the nurse during emergency and also provide the physical assistive devices
such as wheelchair to increase mobility and for functional continence. It may help remove
environmental barriers. The nurse must assess the patient’s strength to remove clothing to urinate
and accordingly respond to it by promoting optimal toilet access. The nurse may help the patient
to reduce the fluid intake beefier bed time (Hälleberg et al., 2017).
Case Study, Chapter 12
a)
Considering the age of the Mr Wills he may be administered with morphine instead of
Oxycodone as the former is more effective in lowering the pain. When compared to the
Oxycodone, Morphine is the stronger opioid. In the pain management plan the nurse must
mention that the patient should be given a less load of medicine. The patient being aged and
having undergone recent surgery needs lesser load of medicine which is possible by morphine.
Morphine will decrease the need of drug metabolism. Higher dose of the Oxycodone 10 mg
every 4 hours PRN may be given if the patient is opioid tolerant. However, with morphine a less
dosage can be administered. Morphine is effective for both moderate to severe pain. The nurse
must monitor the viral signs to address any adverse effects such as respiratory depression. The
nurse may monitor the signs of convulsions in patients. To ensure medication adherence the
nurse may educate the patient about taking medicines in right dosage and on time. ER or
extended release formulations are a viable option for acute to severe pain. It ensures compliance
and less clock watching due to simpler dosing schedule.
26
NURSING ASSIGNMENT
b)
The nurse must perform the systematic assessment of pain outcomes as well as vital
signs. The nurse may encourage the patient to cough, splint and turn to help him prevent adverse
effects of the analgesic agents. It is because administering the opiod reflex will decrease the
patient’s cough reflex. The nurse may promote deep breathing to prevent atelectasis. The patient
may be encouraged to cough up the sputum. The nurse may assist patient to ambulate frequently.
Other vital signs must be regularly monitored such as pain by asking the patient to rate the pain
score on the scale of 10. Further, the nurse may observe the cardiac output if decreased and the
decreased oxygen saturation to prevent respiratory depression. It will help in addressing the
occurrence of dysthymias. The nurse may educate the patient about the side effects and inform
him to report on time in case of confusion, shallow breathing, and feeling of passing out. It will
help in taking measures to administer alternate medicine with lesser side effects. Emphasising on
taking right dosage may prevent overdose of medicines and its adverse effects. It will prevent
abuse of medically subscribed opiods.
c)
The nurse may use the relaxation techniques such as massage with guided imagery. It is
known to be an effective supplement for pain management as it will give Mr Will a greater sense
of control over pain. Both relaxation technique and the guided imagery can be used during any
phase of health or illness. Considering the patient’s preferences the nurse may play light music
for relaxing. If Mr Wills is experiencing chronic or sever pain then nurse may promote relaxation
by yoga. It will better help the patient to manage the pain and restore the functionality. The nurse
may use gentle movement such as tai chi and breathing techniques or meditation to receive
NURSING ASSIGNMENT
b)
The nurse must perform the systematic assessment of pain outcomes as well as vital
signs. The nurse may encourage the patient to cough, splint and turn to help him prevent adverse
effects of the analgesic agents. It is because administering the opiod reflex will decrease the
patient’s cough reflex. The nurse may promote deep breathing to prevent atelectasis. The patient
may be encouraged to cough up the sputum. The nurse may assist patient to ambulate frequently.
Other vital signs must be regularly monitored such as pain by asking the patient to rate the pain
score on the scale of 10. Further, the nurse may observe the cardiac output if decreased and the
decreased oxygen saturation to prevent respiratory depression. It will help in addressing the
occurrence of dysthymias. The nurse may educate the patient about the side effects and inform
him to report on time in case of confusion, shallow breathing, and feeling of passing out. It will
help in taking measures to administer alternate medicine with lesser side effects. Emphasising on
taking right dosage may prevent overdose of medicines and its adverse effects. It will prevent
abuse of medically subscribed opiods.
c)
The nurse may use the relaxation techniques such as massage with guided imagery. It is
known to be an effective supplement for pain management as it will give Mr Will a greater sense
of control over pain. Both relaxation technique and the guided imagery can be used during any
phase of health or illness. Considering the patient’s preferences the nurse may play light music
for relaxing. If Mr Wills is experiencing chronic or sever pain then nurse may promote relaxation
by yoga. It will better help the patient to manage the pain and restore the functionality. The nurse
may use gentle movement such as tai chi and breathing techniques or meditation to receive
27
NURSING ASSIGNMENT
patient of anxiety and stress. As per literature, acupuncture is known to be effective for pain
relief. The nurse may also use gel packs to ease the localised pain. These packs can be chilled or
warmed as required. The nurse may maintain a comfortable and relaxing environment for the
patient by making sure that there is no background noise or chaos around his room. If the patient
is not in state to move then the nurse may ensure bed rest while helping him move his hands and
feet. Later with decrease in severity of pain the nurse may promote physical therapy (Ambrose &
Golightly, 2015).
Case Study, Chapter 13
a)
The possible cause of the low potassium level may be the NPO. NPO status stands for
“Nil Per Os” which means nothing by mouth. Further the patient is also taking Furosemide
regularly which is known as loop diuretic, which may decreases the potassium level in the body
and hinders the electrolyte balance. Diuretics results in loos of excess secretion of the potassium
in urine. Furosemide works by inhibiting the parts of Kidney that reabsorb the electrolytes
sodium and chloride from the urine. Consequently it results in low absorption of water while
increasing the urine volume. It makes the absorption of the potassium by Kidney very difficult.
Therefore, most potassium is lost in urine. This condition is known as hypokalemia.
Dehydration also decreases the electrolyte level in the body. Hypokalemia is caused by low
suction as the patient is fed through nasogastric tube and loss of gastric hydrochloric acid.
b)
The nurse must call the doctor on an emergency basis. Immediate administration of the
potassium should be suggested for Mrs Dean’s recovery. The nurse must focus on four facets
NURSING ASSIGNMENT
patient of anxiety and stress. As per literature, acupuncture is known to be effective for pain
relief. The nurse may also use gel packs to ease the localised pain. These packs can be chilled or
warmed as required. The nurse may maintain a comfortable and relaxing environment for the
patient by making sure that there is no background noise or chaos around his room. If the patient
is not in state to move then the nurse may ensure bed rest while helping him move his hands and
feet. Later with decrease in severity of pain the nurse may promote physical therapy (Ambrose &
Golightly, 2015).
Case Study, Chapter 13
a)
The possible cause of the low potassium level may be the NPO. NPO status stands for
“Nil Per Os” which means nothing by mouth. Further the patient is also taking Furosemide
regularly which is known as loop diuretic, which may decreases the potassium level in the body
and hinders the electrolyte balance. Diuretics results in loos of excess secretion of the potassium
in urine. Furosemide works by inhibiting the parts of Kidney that reabsorb the electrolytes
sodium and chloride from the urine. Consequently it results in low absorption of water while
increasing the urine volume. It makes the absorption of the potassium by Kidney very difficult.
Therefore, most potassium is lost in urine. This condition is known as hypokalemia.
Dehydration also decreases the electrolyte level in the body. Hypokalemia is caused by low
suction as the patient is fed through nasogastric tube and loss of gastric hydrochloric acid.
b)
The nurse must call the doctor on an emergency basis. Immediate administration of the
potassium should be suggested for Mrs Dean’s recovery. The nurse must focus on four facets
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
28
NURSING ASSIGNMENT
such as replenishment of potassium stores, reduction of potassium losses, evaluation for potential
toxicities, and determination of all the causes to prevent the future episodes. The nurse may
discontinue the diuretics. In case the diuretic therapy is required the nurse may administer the
potassium-sparing diuretics. Further, the nurse may administer medications for controlling the
high blood pressure in Mrs Dean as the low potassium may further continue to increases the
blood pressure. The nurse mayst administer the H2 blockers to Mrs Dean as she is receiving the
nasogastric suction.
c)
The clinical manifestations that the nurse might assist in the patient are-
Decreased bowel motility,
Hypoactive reflexes- lack of response from nerve tissue to the normal stimuli
decreases the deep tendon reflexes.
Anorexia- due to the decrease in the peristaltic activity, anorexia and constipation
results
Nauseas and vomiting which may decrease the potassium levels even more
muscle weakness and fatigue due to low potassium level and need of greater
stimulation of cell
Abdominal distension and polyuria.
leg cramps due to disturbed function of the skeletal muscles
ventricular asystole or fibrillation,
ileus,
parasthesias
NURSING ASSIGNMENT
such as replenishment of potassium stores, reduction of potassium losses, evaluation for potential
toxicities, and determination of all the causes to prevent the future episodes. The nurse may
discontinue the diuretics. In case the diuretic therapy is required the nurse may administer the
potassium-sparing diuretics. Further, the nurse may administer medications for controlling the
high blood pressure in Mrs Dean as the low potassium may further continue to increases the
blood pressure. The nurse mayst administer the H2 blockers to Mrs Dean as she is receiving the
nasogastric suction.
c)
The clinical manifestations that the nurse might assist in the patient are-
Decreased bowel motility,
Hypoactive reflexes- lack of response from nerve tissue to the normal stimuli
decreases the deep tendon reflexes.
Anorexia- due to the decrease in the peristaltic activity, anorexia and constipation
results
Nauseas and vomiting which may decrease the potassium levels even more
muscle weakness and fatigue due to low potassium level and need of greater
stimulation of cell
Abdominal distension and polyuria.
leg cramps due to disturbed function of the skeletal muscles
ventricular asystole or fibrillation,
ileus,
parasthesias
29
NURSING ASSIGNMENT
Further clinical manifestations that needs to be assed in case of ECG flattened are-
T waves, prolonged PR interval, prominent U waves, ST depression. ECG gives valuable
information about the hypokalemia (Field, 2016).
Case Study, Chapter 14
a)
Hypovolemic shock is caused by blood loss and fluid loss. The pathophysiologic
sequence of events in this case includes major accident, pain in the abdomen followed by the
bleeding in the abdominal organs and the digestive tract. The next event in the sequence is the
internal bleeding which results in the more than 20% blood loss. The next event is the drop in
blood pressure 90/54 and fluctuation of the other vital signs such as temperature 100.9°F and
heart rate 120 bpm followed by the alteration of the mental health status which is manifested as
the dizziness. It is attributed to the pain in the abdominal cavity.
It can be explained by the response of the human body to the accident by activating the
coagulating cascade. By release of the thromboxane the blood vessels contracts which in turn
activates the platelets. It results in immature clot at the site of bleeding. The next event in the
sequence is the exposure of the collagen, fibrin deposition and clot stabilisation. The increase in
heat rate is the response of the cardiovascular system. The system increases the myocardial
contractility. It results in the constrictions of the peripheral blood vessels. The cardiovascular
system also responds to the redistribution of the blood to the heart, kidney, brain, away from skin
and GI. There is a decrease in the cardiac output thereby increasing the heart rate to pump more
blood. The baroreceptors in the arteries detect the hypotension due to decreases in circulatory
volume and release in norepinephrine and epinephrine, which causes the increases in heart rate.
NURSING ASSIGNMENT
Further clinical manifestations that needs to be assed in case of ECG flattened are-
T waves, prolonged PR interval, prominent U waves, ST depression. ECG gives valuable
information about the hypokalemia (Field, 2016).
Case Study, Chapter 14
a)
Hypovolemic shock is caused by blood loss and fluid loss. The pathophysiologic
sequence of events in this case includes major accident, pain in the abdomen followed by the
bleeding in the abdominal organs and the digestive tract. The next event in the sequence is the
internal bleeding which results in the more than 20% blood loss. The next event is the drop in
blood pressure 90/54 and fluctuation of the other vital signs such as temperature 100.9°F and
heart rate 120 bpm followed by the alteration of the mental health status which is manifested as
the dizziness. It is attributed to the pain in the abdominal cavity.
It can be explained by the response of the human body to the accident by activating the
coagulating cascade. By release of the thromboxane the blood vessels contracts which in turn
activates the platelets. It results in immature clot at the site of bleeding. The next event in the
sequence is the exposure of the collagen, fibrin deposition and clot stabilisation. The increase in
heat rate is the response of the cardiovascular system. The system increases the myocardial
contractility. It results in the constrictions of the peripheral blood vessels. The cardiovascular
system also responds to the redistribution of the blood to the heart, kidney, brain, away from skin
and GI. There is a decrease in the cardiac output thereby increasing the heart rate to pump more
blood. The baroreceptors in the arteries detect the hypotension due to decreases in circulatory
volume and release in norepinephrine and epinephrine, which causes the increases in heart rate.
30
NURSING ASSIGNMENT
There is respiratory insufficiency that increased the cell hypoxia in Carlos Adams. It is due to
this reason that the patients respiratory rate is 20 breathes per minute. It is because the oxygen
demand is greater than the oxygen supply. There is loss of blood internally and cellular damage.
The body responses to this buy increase in blood flow developing an inflammatory response
from the affected area. It is the source of rise in temperature in Carlos Adams. In this situation
the sympathetic nervous system is stimulated leading to rapid and deep respirations.
b)
The medical management goals for the patient’s are-
Blood to be administered safely
Assess the client’s ECG as hypoxia may result in cardiac dysrhythmias
Assess the central peripheral pulses and capillary refill time
Asses for the level of confusion
Monitor the oxygen saturation and asses the respiratory rhythm
Maintain the blood pressure, temperature and heart rate at normal rate
Maintain the patient’s skin turgor and orientation to pace, person and time
Maintain the fluid volume at the functional level
c)
The two large-bore IVs are used for the patient or fluid and blood administration in case
of trauma and accident. Considering the situation of hypovolemic shock, it is necessary to
control the bleeding in the Carlos Adams and restore the normal blood volume. When the
peripheral IV is started, it is possible to gain the access to the peripheral circulation of the
patient. It helps to sample the blood as well as infuse the IV medications and fluid. IV access is
NURSING ASSIGNMENT
There is respiratory insufficiency that increased the cell hypoxia in Carlos Adams. It is due to
this reason that the patients respiratory rate is 20 breathes per minute. It is because the oxygen
demand is greater than the oxygen supply. There is loss of blood internally and cellular damage.
The body responses to this buy increase in blood flow developing an inflammatory response
from the affected area. It is the source of rise in temperature in Carlos Adams. In this situation
the sympathetic nervous system is stimulated leading to rapid and deep respirations.
b)
The medical management goals for the patient’s are-
Blood to be administered safely
Assess the client’s ECG as hypoxia may result in cardiac dysrhythmias
Assess the central peripheral pulses and capillary refill time
Asses for the level of confusion
Monitor the oxygen saturation and asses the respiratory rhythm
Maintain the blood pressure, temperature and heart rate at normal rate
Maintain the patient’s skin turgor and orientation to pace, person and time
Maintain the fluid volume at the functional level
c)
The two large-bore IVs are used for the patient or fluid and blood administration in case
of trauma and accident. Considering the situation of hypovolemic shock, it is necessary to
control the bleeding in the Carlos Adams and restore the normal blood volume. When the
peripheral IV is started, it is possible to gain the access to the peripheral circulation of the
patient. It helps to sample the blood as well as infuse the IV medications and fluid. IV access is
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
31
NURSING ASSIGNMENT
essential as the patient in the given case study is critical ill due to motor vehicle accident. In this
case two large bore IVs are inserted in the patient for high volume fluid resuscitation. It is used
in the anticipation of the potential problems in the future as fluid volume restoration is necessary.
The need of using the large bore IV is because the rate of flow is proportion to the radius to the
power of four. It is also inversely proportional to the length. It means the fluid can be
administered faster if the tube is shorter and larger in diameter
d)
The advantage of using the 0.9% NS is because it is cheapest of all fluids used for
resuscitation. It will help restore the fluid loss and maintain sodium chloride balance in Carlos
Adams. It is advantageous in dilution of other medicines before its injection into body. It is also
effective choice for blood transfusion. It does not contain dextrose therefore the red blood cells
may not clump. The patient since is not in condition to take the nutrients from mouth, norm
saline will be useful in supplying the daily water and slats demands. It will help in providing
extra water to rehydrate the patient. It is useful for both purpose of isotonic volume expander
and electrolyte replacement. Since, Carlos Adams is at increased risk of sodium depletion and
extracellular dehydration, 0.9% NaCl is advantageous in preventing the same. It will help
restore the intravascular volume by administering the small amount of fluids
e)
Carlos Adams has been placed in the modified Trendelenburg position, which is used for
surgery of the abdomen and genitourinary system. It allows the practioner to easily access the
pelvic organs by the gravitational pull in hypovolemic shock treatment. Since the patient is
diagnosed with hypovolemic shock, maintaining this position will help in blood flow to brain. It
NURSING ASSIGNMENT
essential as the patient in the given case study is critical ill due to motor vehicle accident. In this
case two large bore IVs are inserted in the patient for high volume fluid resuscitation. It is used
in the anticipation of the potential problems in the future as fluid volume restoration is necessary.
The need of using the large bore IV is because the rate of flow is proportion to the radius to the
power of four. It is also inversely proportional to the length. It means the fluid can be
administered faster if the tube is shorter and larger in diameter
d)
The advantage of using the 0.9% NS is because it is cheapest of all fluids used for
resuscitation. It will help restore the fluid loss and maintain sodium chloride balance in Carlos
Adams. It is advantageous in dilution of other medicines before its injection into body. It is also
effective choice for blood transfusion. It does not contain dextrose therefore the red blood cells
may not clump. The patient since is not in condition to take the nutrients from mouth, norm
saline will be useful in supplying the daily water and slats demands. It will help in providing
extra water to rehydrate the patient. It is useful for both purpose of isotonic volume expander
and electrolyte replacement. Since, Carlos Adams is at increased risk of sodium depletion and
extracellular dehydration, 0.9% NaCl is advantageous in preventing the same. It will help
restore the intravascular volume by administering the small amount of fluids
e)
Carlos Adams has been placed in the modified Trendelenburg position, which is used for
surgery of the abdomen and genitourinary system. It allows the practioner to easily access the
pelvic organs by the gravitational pull in hypovolemic shock treatment. Since the patient is
diagnosed with hypovolemic shock, maintaining this position will help in blood flow to brain. It
32
NURSING ASSIGNMENT
is useful in creating the better perfusion during respiratory distress. It is also beneficial in
surgical decrease in abdominal hernia (Arslan et al., 2016).
Case Study, Chapter 15
a)
After taking the vital signs the nurse maintain the position of the head of the patient at 45
degrees. It will help promote oxygenation of the patient. The nurse must obtain the ABGs on
room air, or take help of respiratory therapist. It is needed before starting the patient on oxygen
at 2 litres per minute. The nurse must observe the pulse oximetery and ensure the oxygen
saturation of more than 95%. It means the oxygen takes first position in the sequence of events.
The baseline of the patient’s oxygen status is obtained from the ABGs. The next step is to obtain
the labs that can be drawn from the venipuncture site. At this site IV are placed for
administration of fluids and antibiotics. The third step is to obtain culture for administrations of
antibiotics. The nurse may then administer the broad-spectrum antibiotics to cure the infection.
The oxygen status if stabilised the nurse may proceed with taking X-ray. It will help detect any
abnormality in lungs, and possible urinary obstructions that may have led to infection.
b)
The nurse needs to assess the vital signs such as respiratory rate, temperature and
hemodynamic status. Further, the level of consciousness and changes in the patient’s orientation
must be determined. The nurse must assess the fluid balance and electrolyte status. The chart
recordings of input and output as well as renal profile should be monitored for changes. The
nurse must assess the oxygen saturation via ABG and pulse oximetry.
NURSING ASSIGNMENT
is useful in creating the better perfusion during respiratory distress. It is also beneficial in
surgical decrease in abdominal hernia (Arslan et al., 2016).
Case Study, Chapter 15
a)
After taking the vital signs the nurse maintain the position of the head of the patient at 45
degrees. It will help promote oxygenation of the patient. The nurse must obtain the ABGs on
room air, or take help of respiratory therapist. It is needed before starting the patient on oxygen
at 2 litres per minute. The nurse must observe the pulse oximetery and ensure the oxygen
saturation of more than 95%. It means the oxygen takes first position in the sequence of events.
The baseline of the patient’s oxygen status is obtained from the ABGs. The next step is to obtain
the labs that can be drawn from the venipuncture site. At this site IV are placed for
administration of fluids and antibiotics. The third step is to obtain culture for administrations of
antibiotics. The nurse may then administer the broad-spectrum antibiotics to cure the infection.
The oxygen status if stabilised the nurse may proceed with taking X-ray. It will help detect any
abnormality in lungs, and possible urinary obstructions that may have led to infection.
b)
The nurse needs to assess the vital signs such as respiratory rate, temperature and
hemodynamic status. Further, the level of consciousness and changes in the patient’s orientation
must be determined. The nurse must assess the fluid balance and electrolyte status. The chart
recordings of input and output as well as renal profile should be monitored for changes. The
nurse must assess the oxygen saturation via ABG and pulse oximetry.

33
NURSING ASSIGNMENT
c)
The nurse may educate the patient about the hand hygiene and health eating behaviour.
Mr. Jones should be taught to wash hands before and after touching face, eating food, and
drinking. Mr Jones may be explained that cancer leads to compromise of immune system due to
chemotherapy. It affects the production of white blood cells and cause of myelosuppression
especially the neutrophils. The neutrophils fight the infection. The patient may be aware of signs
of complications in this process. The nurse must inform Mr. Jones to stay away from people
with contagious illness, cold or cough. The family members are educated to avoid contacting the
patient in case of infection like symptoms such as fever, cough with sputum, chills, body ache
and others. The nurse must educate the patient on balanced nutrition. He must be report to
oncologist immediately in case of adverse symptoms such as nausea, vomiting, unable to take
liquids or having liquid stools, fever, sore throat, wound drainage. The nurse must educate and
ask patient to report any urinary tract infections (Ettinger et al., 2016).
Case Study, Chapter 16
a)
Hospice service is for caring of the patients of all age group irrespective of cultural and
linguistic background. The principle of hospice care for Ms. Williams who have no further
treatment options includes provision of whole spectrum of care. It includes spiritual, cultural,
social and psychological. Holistic approach includes good medical practice along with caring
attitude. The nurse must respect the individuality, and dignity of the patient. The nurse must take
the patient’s consent, and involve family for shared decision making. The nurse must give the
NURSING ASSIGNMENT
c)
The nurse may educate the patient about the hand hygiene and health eating behaviour.
Mr. Jones should be taught to wash hands before and after touching face, eating food, and
drinking. Mr Jones may be explained that cancer leads to compromise of immune system due to
chemotherapy. It affects the production of white blood cells and cause of myelosuppression
especially the neutrophils. The neutrophils fight the infection. The patient may be aware of signs
of complications in this process. The nurse must inform Mr. Jones to stay away from people
with contagious illness, cold or cough. The family members are educated to avoid contacting the
patient in case of infection like symptoms such as fever, cough with sputum, chills, body ache
and others. The nurse must educate the patient on balanced nutrition. He must be report to
oncologist immediately in case of adverse symptoms such as nausea, vomiting, unable to take
liquids or having liquid stools, fever, sore throat, wound drainage. The nurse must educate and
ask patient to report any urinary tract infections (Ettinger et al., 2016).
Case Study, Chapter 16
a)
Hospice service is for caring of the patients of all age group irrespective of cultural and
linguistic background. The principle of hospice care for Ms. Williams who have no further
treatment options includes provision of whole spectrum of care. It includes spiritual, cultural,
social and psychological. Holistic approach includes good medical practice along with caring
attitude. The nurse must respect the individuality, and dignity of the patient. The nurse must take
the patient’s consent, and involve family for shared decision making. The nurse must give the
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
34
NURSING ASSIGNMENT
patient and the family the choice of site of care. The nurse must engage in effective
communication and provide treatment that is appropriate for the metastatic disease in Ms
Williams spine
b)
The physician may inform Ms Williams that she is terminally and is eligible for the
Medicare/ Medicaid coverage. The physician may inform about close medical and supportive
care and emphasise on comfort care rather than cure provided by Medicare/ Medicaid. A teh
patient may be informed about the specialised therapies such as home health aide services,
specialised therapy such as speech and physical therapy, medical social services, respite care,
counselling services including dietary and bereavement counselling, and medical supplied to be
given. The patient may choose statement related to Medicare and/or Medicaid. The physician
must aware the patient about the recertification process, way to make payment, and what is not
covered by the programme.
c)
Ms Williams may be reassured by informing that hospice care does provide the service
of pain management. She may receive pain medication to control pain. The certified hospice
nurse may ensure Ms Williams may be comforted by explaining that the pain management in
hospice focuses on the physical, emotional and spiritual aspects. It means the patient is assured
that the treating pain is the top priority of hospice care. The patient may be assured of high
quality pain management in hospice care (Cea et al., 2016).
NURSING ASSIGNMENT
patient and the family the choice of site of care. The nurse must engage in effective
communication and provide treatment that is appropriate for the metastatic disease in Ms
Williams spine
b)
The physician may inform Ms Williams that she is terminally and is eligible for the
Medicare/ Medicaid coverage. The physician may inform about close medical and supportive
care and emphasise on comfort care rather than cure provided by Medicare/ Medicaid. A teh
patient may be informed about the specialised therapies such as home health aide services,
specialised therapy such as speech and physical therapy, medical social services, respite care,
counselling services including dietary and bereavement counselling, and medical supplied to be
given. The patient may choose statement related to Medicare and/or Medicaid. The physician
must aware the patient about the recertification process, way to make payment, and what is not
covered by the programme.
c)
Ms Williams may be reassured by informing that hospice care does provide the service
of pain management. She may receive pain medication to control pain. The certified hospice
nurse may ensure Ms Williams may be comforted by explaining that the pain management in
hospice focuses on the physical, emotional and spiritual aspects. It means the patient is assured
that the treating pain is the top priority of hospice care. The patient may be assured of high
quality pain management in hospice care (Cea et al., 2016).
35
NURSING ASSIGNMENT
Case Study, Chapter 17
a)
To assist with recovery the nurse may educate the patient’s queries. It will ensure
patient’s contentment. Awareness will decrease postoperative complications. The nurse must
help patient in retaining information and asses further learning needs. It must be ensured that the
anxiety level is lower before surgery 5-14 days. It will maximise the benefits of teaching and
better assess all the vital signs. Having adequate time will help give patient centered care and
develop patient’s confidence. The nurse may proceed with taking history of patient, followed by
complete physical examination, radiographic examination and electrocardiogram. The nurse may
ensure the family support level and conduct other psychosocial assessment. The nurse may
assist the patient’s functional level. The nurse may asses if the patient has any fear related to
CABG and surgical procedure and addresses the same.
b)
The nurse may ensure the normal range of peripheral pulses, peripheral oedema,
auscultation of heart, and inspect the palpation of heart. The nurse must ensure that all the
instruments are available in surgical room and complete the typing and cross matching of
patient’s blood. Encourage the patient to verbalise feelings about outcomes of CABG surgery.
The nurse may ensure that the patient is aware of complications postoperation. The nurse may
ensure two identity bands present and must handover to receiving nurse. The nurse must check
that all the safety measures are followed. The nurse may ensure cardiac life support and
emotional support to relieve anxiety (Sweeney et al., 2017).
NURSING ASSIGNMENT
Case Study, Chapter 17
a)
To assist with recovery the nurse may educate the patient’s queries. It will ensure
patient’s contentment. Awareness will decrease postoperative complications. The nurse must
help patient in retaining information and asses further learning needs. It must be ensured that the
anxiety level is lower before surgery 5-14 days. It will maximise the benefits of teaching and
better assess all the vital signs. Having adequate time will help give patient centered care and
develop patient’s confidence. The nurse may proceed with taking history of patient, followed by
complete physical examination, radiographic examination and electrocardiogram. The nurse may
ensure the family support level and conduct other psychosocial assessment. The nurse may
assist the patient’s functional level. The nurse may asses if the patient has any fear related to
CABG and surgical procedure and addresses the same.
b)
The nurse may ensure the normal range of peripheral pulses, peripheral oedema,
auscultation of heart, and inspect the palpation of heart. The nurse must ensure that all the
instruments are available in surgical room and complete the typing and cross matching of
patient’s blood. Encourage the patient to verbalise feelings about outcomes of CABG surgery.
The nurse may ensure that the patient is aware of complications postoperation. The nurse may
ensure two identity bands present and must handover to receiving nurse. The nurse must check
that all the safety measures are followed. The nurse may ensure cardiac life support and
emotional support to relieve anxiety (Sweeney et al., 2017).
36
NURSING ASSIGNMENT
Case Study, Chapter 18
a)
The age of the patient is itself risk factor for postoperative morbidity and mortality. The
nurse is responsible for close monitoring of patient’s status, as well as comorbidities. The nurse
must collaborate with the anaesthesia team to determine the dosage of anaesthesia and duration
of surgery and urgency. It will help prevent confusion and altered mental health status after
surgery. The history of COPD and smoking increases the risk of pulmonary complications in the
operating room. The nurse may assess the viral signs and hydration status of the patient. Before
surgery the nurse may assess the psychological status and administer preoperative medications.
The nurse must educate patient on smoking cessation. Considering the patient’s age there is high
risk of cardiovascular complications. Thus, the nurse must ensure, effective fluid balance to
prevent fluid overload, and hypo/hypervolemia. The nurse must maintain the titration of the
vasoactive drugs for preventing heart dysfunction is essential. The nurse must provide the patient
with adequate oxygen delivery.
b)
The role of nurse in patient safety includes promoting the principle of asepsis,
homeostasis, safe administration of anaesthesia to prevent pain. The surgical set up to be
performed by scrub nurse to maintain surgical sepsis. The nurse must also consider the infection
control procedures such as sterilisation of operating room and sterile table. The circulating nurse
will deliver supplies to the sterile filed and carry out nursing care plan. The nurse must ensure
position that will not prevent vascular supply. The nurse must ensure that the arms are not more
than 90° and keep the knee strap (Allegranzi et al., 2016).
NURSING ASSIGNMENT
Case Study, Chapter 18
a)
The age of the patient is itself risk factor for postoperative morbidity and mortality. The
nurse is responsible for close monitoring of patient’s status, as well as comorbidities. The nurse
must collaborate with the anaesthesia team to determine the dosage of anaesthesia and duration
of surgery and urgency. It will help prevent confusion and altered mental health status after
surgery. The history of COPD and smoking increases the risk of pulmonary complications in the
operating room. The nurse may assess the viral signs and hydration status of the patient. Before
surgery the nurse may assess the psychological status and administer preoperative medications.
The nurse must educate patient on smoking cessation. Considering the patient’s age there is high
risk of cardiovascular complications. Thus, the nurse must ensure, effective fluid balance to
prevent fluid overload, and hypo/hypervolemia. The nurse must maintain the titration of the
vasoactive drugs for preventing heart dysfunction is essential. The nurse must provide the patient
with adequate oxygen delivery.
b)
The role of nurse in patient safety includes promoting the principle of asepsis,
homeostasis, safe administration of anaesthesia to prevent pain. The surgical set up to be
performed by scrub nurse to maintain surgical sepsis. The nurse must also consider the infection
control procedures such as sterilisation of operating room and sterile table. The circulating nurse
will deliver supplies to the sterile filed and carry out nursing care plan. The nurse must ensure
position that will not prevent vascular supply. The nurse must ensure that the arms are not more
than 90° and keep the knee strap (Allegranzi et al., 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
37
NURSING ASSIGNMENT
Case Study, Chapter 19
1
a)
The assessment parameters to provide clues to detect postoperative problems are as
follows-
1. Oxygen saturation
2. Temperature
3. Respiratory rate
4. Pulse rate
5. Systolic blood pressure
6. Level of consciousness
Level of consciousness is altered when the infusion rate is too high. It is necessary to
initially well control the pain and well managed initially by the anaesthetist. It would ensure that
the patient has adequate analgesia. It would have ensured that the patient is alert enough to
communicate in postoperative period. In the given scenario the patient has O2 at 2 L per nasal
cannula with a pulse oximetry reading of 95%. It means the patient is in need of more oxygen to
avoid complication of respiratory insufficiency as indicated by respiratory rate of 16 breaths/min
in current sate. Assessment of airway is needed as respiratory depression is indicated by
bradypnoea The possible interventions include prescription of oxygen therapy continuously and
at correct rate to prevent drying of mucous membrane. Oxygen saturation shall be maintained
above 95%. To prevent complications such as peripheral vasoconstriction and dried blood on
finger the finger probe must be clean, and there should be change in finger probe to prevent
NURSING ASSIGNMENT
Case Study, Chapter 19
1
a)
The assessment parameters to provide clues to detect postoperative problems are as
follows-
1. Oxygen saturation
2. Temperature
3. Respiratory rate
4. Pulse rate
5. Systolic blood pressure
6. Level of consciousness
Level of consciousness is altered when the infusion rate is too high. It is necessary to
initially well control the pain and well managed initially by the anaesthetist. It would ensure that
the patient has adequate analgesia. It would have ensured that the patient is alert enough to
communicate in postoperative period. In the given scenario the patient has O2 at 2 L per nasal
cannula with a pulse oximetry reading of 95%. It means the patient is in need of more oxygen to
avoid complication of respiratory insufficiency as indicated by respiratory rate of 16 breaths/min
in current sate. Assessment of airway is needed as respiratory depression is indicated by
bradypnoea The possible interventions include prescription of oxygen therapy continuously and
at correct rate to prevent drying of mucous membrane. Oxygen saturation shall be maintained
above 95%. To prevent complications such as peripheral vasoconstriction and dried blood on
finger the finger probe must be clean, and there should be change in finger probe to prevent
38
NURSING ASSIGNMENT
sores. The vital signs are altered such as blood pressure, 100/50 mm Hg; heart rate 110 bpm in
patient mainly when intravenous opiates are given. Altered systolic blood pressure in the given
case scenario is indicating tachycardia. It may be due to shock/ haemorrhage and needs to be
maintained in normal temperature. Tachycardia is also indicative of pain in patient, overloaded
with fluid, or anxious. Inadequate pain control also leads to hypertension. Body temperature
needs to be assessed as there is risk of hypothermia. High temperature is indicated by bacterial
infection. Currently the patient does not have fever. In the given case study the patient has
altered consciousness which may be due to shock. There is also need to monitor adequate fluid
balance to prevent complications such as hypovolemia,
Other parameters to be considered are as follows-
Early nausea and vomiting- can be treated with antiemetics and also nasogastric
tube drainage
Identify the POI by abdominal pain and distension
Identify the failure to pass the faeces- passage of stool is the indication that the
normal movement has returned in colon
Compromised mobility- difficulty in return of bowel functions and normal blood
circulations
Compromised bowel functions
b)
The gerentological postoperative considerations for nurses are-
NURSING ASSIGNMENT
sores. The vital signs are altered such as blood pressure, 100/50 mm Hg; heart rate 110 bpm in
patient mainly when intravenous opiates are given. Altered systolic blood pressure in the given
case scenario is indicating tachycardia. It may be due to shock/ haemorrhage and needs to be
maintained in normal temperature. Tachycardia is also indicative of pain in patient, overloaded
with fluid, or anxious. Inadequate pain control also leads to hypertension. Body temperature
needs to be assessed as there is risk of hypothermia. High temperature is indicated by bacterial
infection. Currently the patient does not have fever. In the given case study the patient has
altered consciousness which may be due to shock. There is also need to monitor adequate fluid
balance to prevent complications such as hypovolemia,
Other parameters to be considered are as follows-
Early nausea and vomiting- can be treated with antiemetics and also nasogastric
tube drainage
Identify the POI by abdominal pain and distension
Identify the failure to pass the faeces- passage of stool is the indication that the
normal movement has returned in colon
Compromised mobility- difficulty in return of bowel functions and normal blood
circulations
Compromised bowel functions
b)
The gerentological postoperative considerations for nurses are-
39
NURSING ASSIGNMENT
Maintenance of adequate body system functions
Maintenance of therapeutic environment
Restore of homeostasis- ease of breathing, clear lung auscultations, stable vital
signs, and body temperature
Pain alleviation and intact wound edges
Prevention of postoperative complications
Assess for skin integrity to prevent infections and pressure sores
Assessment and management of voluntary voiding
Careful monitoring of the haemoglobin and hematocrit levels
Assessment of urinary output as the patient is at risk for poor fluid and electrolyte
imbalances
In case of confusion the nurse may avoid any kind of restraints. Instead the nurse
must maintain the physical activity as elderly patient are at risk of delirium
Provide adequate discharge planning for patient (Schenning & Deiner, 2015)
2
a)
The four phases of the Mr Smith’s wound healing includes
Homeostasis phase- In this phase the objective is to stop bleeding so the body stimulates
repair system, blood clot mechanism and block of drainage. It includes collagen exposure,
platelet aggregation and activation.
Inflammation phase- In this phase the bacteria is destroyed and a new growth of tissue is
stimulated. Inflammation in Smith has begun as it is indicated by the calf area red, warm and
NURSING ASSIGNMENT
Maintenance of adequate body system functions
Maintenance of therapeutic environment
Restore of homeostasis- ease of breathing, clear lung auscultations, stable vital
signs, and body temperature
Pain alleviation and intact wound edges
Prevention of postoperative complications
Assess for skin integrity to prevent infections and pressure sores
Assessment and management of voluntary voiding
Careful monitoring of the haemoglobin and hematocrit levels
Assessment of urinary output as the patient is at risk for poor fluid and electrolyte
imbalances
In case of confusion the nurse may avoid any kind of restraints. Instead the nurse
must maintain the physical activity as elderly patient are at risk of delirium
Provide adequate discharge planning for patient (Schenning & Deiner, 2015)
2
a)
The four phases of the Mr Smith’s wound healing includes
Homeostasis phase- In this phase the objective is to stop bleeding so the body stimulates
repair system, blood clot mechanism and block of drainage. It includes collagen exposure,
platelet aggregation and activation.
Inflammation phase- In this phase the bacteria is destroyed and a new growth of tissue is
stimulated. Inflammation in Smith has begun as it is indicated by the calf area red, warm and
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
40
NURSING ASSIGNMENT
hard to touch, and edematous. This process includes entry of neutrophils to destroy bacteria
followed by arrival of macrophages to clear the debris. The proteins and growth factors secreted
attract the immune system to repair the wound. The extravasation of blood vessels and action of
killing bacteria results in redness, pain, heat and edema due to infiltration of immunological
agent in calf area of patient such as white blood cells, nutrients, enzymes, antibodies, and other
beneficial elements. This is the sign of healing of wound as the bleeding is halted and clot is
formed.
Proliferative phase- In this stage Mr Smith’s wound would progress towards the filling of
wound with red granulation tissue and formation of new blood vessels. It will be followed by the
arise of epithelial cells, to cover the entire wound
Maturation phase- In this stage the wound gains flexibility and strength due to
reorganisation of collagen fibres. The tissue rematures at this stage.
Mr smith’s wound is healing and is in the middle of inflammatory phase and will soon
progress to subsequent steps to wound healing.
b)
Firstly the nurse may check the patient’s chart to confirm the requested wet to dry
dressing. The nurse shall conduct the change of dressing as scheduled. The nurse must prepare
on tray all the materials such as sterile gloves, sterile solution, tape, and 4-by-4 gauze. The nurse
must perform hand hygiene from elbow using soap and warm water and wear sterile gloves.
Before beginning the process the nurse may inform Smith and address any questions. The old
NURSING ASSIGNMENT
hard to touch, and edematous. This process includes entry of neutrophils to destroy bacteria
followed by arrival of macrophages to clear the debris. The proteins and growth factors secreted
attract the immune system to repair the wound. The extravasation of blood vessels and action of
killing bacteria results in redness, pain, heat and edema due to infiltration of immunological
agent in calf area of patient such as white blood cells, nutrients, enzymes, antibodies, and other
beneficial elements. This is the sign of healing of wound as the bleeding is halted and clot is
formed.
Proliferative phase- In this stage Mr Smith’s wound would progress towards the filling of
wound with red granulation tissue and formation of new blood vessels. It will be followed by the
arise of epithelial cells, to cover the entire wound
Maturation phase- In this stage the wound gains flexibility and strength due to
reorganisation of collagen fibres. The tissue rematures at this stage.
Mr smith’s wound is healing and is in the middle of inflammatory phase and will soon
progress to subsequent steps to wound healing.
b)
Firstly the nurse may check the patient’s chart to confirm the requested wet to dry
dressing. The nurse shall conduct the change of dressing as scheduled. The nurse must prepare
on tray all the materials such as sterile gloves, sterile solution, tape, and 4-by-4 gauze. The nurse
must perform hand hygiene from elbow using soap and warm water and wear sterile gloves.
Before beginning the process the nurse may inform Smith and address any questions. The old
41
NURSING ASSIGNMENT
dressing shall be removed from edges while bunching on centre. The dressing may be loosened
using sterile saline avoiding disturbance to new skin. Wound is cleaned using saline and idoform
gauge. The wound is pat until dry and is inspected for consistency, colour, and odour. Signs of
improper healing are monitored followed by new dressing. A new piece of dressing is moistened
with sterile solution idoform gauge is placed on wound with dry dressing. It is then secured with
paper tape. As per the wound requirement nurse may apply more gauge or tape (Chetter et al.,
2017).
NURSING ASSIGNMENT
dressing shall be removed from edges while bunching on centre. The dressing may be loosened
using sterile saline avoiding disturbance to new skin. Wound is cleaned using saline and idoform
gauge. The wound is pat until dry and is inspected for consistency, colour, and odour. Signs of
improper healing are monitored followed by new dressing. A new piece of dressing is moistened
with sterile solution idoform gauge is placed on wound with dry dressing. It is then secured with
paper tape. As per the wound requirement nurse may apply more gauge or tape (Chetter et al.,
2017).
42
NURSING ASSIGNMENT
References
Allegranzi, B., Zayed, B., Bischoff, P., Kubilay, N. Z., de Jonge, S., de Vries, F., ... & Abbas, M.
(2016). New WHO recommendations on intraoperative and postoperative measures for
surgical site infection prevention: an evidence-based global perspective. The Lancet
Infectious Diseases, 16(12), e288-e303.
Ambrose, K. R., & Golightly, Y. M. (2015). Physical exercise as non-pharmacological treatment
of chronic pain: why and when. Best Practice & Research Clinical Rheumatology, 29(1),
120-130.
Arslan, D., Tokgöz, N., Armut, F., Deşer, S. B., & Demirağ, M. K. (2016). PP-030 Nursing Care
in Patients with Dic and Hypovolemic Shock. American Journal of Cardiology, 117, S53.
Ashwell, M., Gunn, P., & Gibson, S. (2012). Waist‐to‐height ratio is a better screening tool than
waist circumference and BMI for adult cardiometabolic risk factors: systematic review
and meta‐analysis. Obesity reviews, 13(3), 275-286.
Benevides, J. L., Coutinho, J. F. V., Tomé, M. A. B. G., Gubert, F. D. A., Silva, T. B. D. C., &
de Oliveira, S. K. P. (2017). Nursing strategies for the prevention of pressure ulcers in
intensive therapy: integrative review. Journal of Nursing UFPE on line, 11(5), 1943-
1952.
Cea, M. E., Reid, M. C., Inturrisi, C., Witkin, L. R., Prigerson, H. G., & Bao, Y. (2016). Pain
assessment, management, and control among patients 65 years or older receiving hospice
care in the US. Journal of pain and symptom management, 52(5), 663-672.
NURSING ASSIGNMENT
References
Allegranzi, B., Zayed, B., Bischoff, P., Kubilay, N. Z., de Jonge, S., de Vries, F., ... & Abbas, M.
(2016). New WHO recommendations on intraoperative and postoperative measures for
surgical site infection prevention: an evidence-based global perspective. The Lancet
Infectious Diseases, 16(12), e288-e303.
Ambrose, K. R., & Golightly, Y. M. (2015). Physical exercise as non-pharmacological treatment
of chronic pain: why and when. Best Practice & Research Clinical Rheumatology, 29(1),
120-130.
Arslan, D., Tokgöz, N., Armut, F., Deşer, S. B., & Demirağ, M. K. (2016). PP-030 Nursing Care
in Patients with Dic and Hypovolemic Shock. American Journal of Cardiology, 117, S53.
Ashwell, M., Gunn, P., & Gibson, S. (2012). Waist‐to‐height ratio is a better screening tool than
waist circumference and BMI for adult cardiometabolic risk factors: systematic review
and meta‐analysis. Obesity reviews, 13(3), 275-286.
Benevides, J. L., Coutinho, J. F. V., Tomé, M. A. B. G., Gubert, F. D. A., Silva, T. B. D. C., &
de Oliveira, S. K. P. (2017). Nursing strategies for the prevention of pressure ulcers in
intensive therapy: integrative review. Journal of Nursing UFPE on line, 11(5), 1943-
1952.
Cea, M. E., Reid, M. C., Inturrisi, C., Witkin, L. R., Prigerson, H. G., & Bao, Y. (2016). Pain
assessment, management, and control among patients 65 years or older receiving hospice
care in the US. Journal of pain and symptom management, 52(5), 663-672.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
43
NURSING ASSIGNMENT
Chetter, I. C., Oswald, A. V., Fletcher, M., Dumville, J. C., & Cullum, N. A. (2017). A survey of
patients with surgical wounds healing by secondary intention; an assessment of
prevalence, aetiology, duration and management. Journal of tissue viability, 26(2), 103-
107.
Douglas, M. K., Rosenkoetter, M., Pacquiao, D. F., Callister, L. C., Hattar-Pollara, M.,
Lauderdale, J., ... & Purnell, L. (2014). Guidelines for implementing culturally competent
nursing care. Journal of Transcultural Nursing, 25(2), 109-121.
Ettinger, D. S., Wood, D. E., Akerley, W., Bazhenova, L. A., Borghaei, H., Camidge, D. R., ... &
Dobelbower, M. C. (2016). NCCN guidelines insights: non–small cell lung cancer,
version 4.2016. Journal of the National Comprehensive Cancer Network, 14(3), 255-264.
Field, L. (2016). Nursing & Health Survival Guide: Nutrition and Hydration. Routledge.
Finsterer, J., Löscher, W., Quasthoff, S., Wanschitz, J., Auer-Grumbach, M., & Stevanin, G.
(2012). Hereditary spastic paraplegias with autosomal dominant, recessive, X-linked, or
maternal trait of inheritance. Journal of the neurological sciences, 318(1), 1-18.
Hälleberg Nyman, M., Forsman, H., Ostaszkiewicz, J., Hommel, A., & Eldh, A. C. (2017).
Urinary incontinence and its management in patients aged 65 and older in orthopaedic
care–what nursing and rehabilitation staff know and do. Journal of clinical
nursing, 26(21-22), 3345-3353.
Johnson, L., Grueber, S., Schlotzhauer, C., Phillips, E., Bullock, P., Basnett, J., & Hahn-Cover,
K. (2014). A multifactorial action plan improves hand hygiene adherence and
NURSING ASSIGNMENT
Chetter, I. C., Oswald, A. V., Fletcher, M., Dumville, J. C., & Cullum, N. A. (2017). A survey of
patients with surgical wounds healing by secondary intention; an assessment of
prevalence, aetiology, duration and management. Journal of tissue viability, 26(2), 103-
107.
Douglas, M. K., Rosenkoetter, M., Pacquiao, D. F., Callister, L. C., Hattar-Pollara, M.,
Lauderdale, J., ... & Purnell, L. (2014). Guidelines for implementing culturally competent
nursing care. Journal of Transcultural Nursing, 25(2), 109-121.
Ettinger, D. S., Wood, D. E., Akerley, W., Bazhenova, L. A., Borghaei, H., Camidge, D. R., ... &
Dobelbower, M. C. (2016). NCCN guidelines insights: non–small cell lung cancer,
version 4.2016. Journal of the National Comprehensive Cancer Network, 14(3), 255-264.
Field, L. (2016). Nursing & Health Survival Guide: Nutrition and Hydration. Routledge.
Finsterer, J., Löscher, W., Quasthoff, S., Wanschitz, J., Auer-Grumbach, M., & Stevanin, G.
(2012). Hereditary spastic paraplegias with autosomal dominant, recessive, X-linked, or
maternal trait of inheritance. Journal of the neurological sciences, 318(1), 1-18.
Hälleberg Nyman, M., Forsman, H., Ostaszkiewicz, J., Hommel, A., & Eldh, A. C. (2017).
Urinary incontinence and its management in patients aged 65 and older in orthopaedic
care–what nursing and rehabilitation staff know and do. Journal of clinical
nursing, 26(21-22), 3345-3353.
Johnson, L., Grueber, S., Schlotzhauer, C., Phillips, E., Bullock, P., Basnett, J., & Hahn-Cover,
K. (2014). A multifactorial action plan improves hand hygiene adherence and
44
NURSING ASSIGNMENT
significantly reduces central line–associated bloodstream infections. American journal of
infection control, 42(11), 1146-1151.
Karlsson, M., Karlsson, C., Barbosa da Silva, A., Berggren, I., & Söderlund, M. (2013).
Community nurses' experiences of ethical problems in end‐of‐life care in the patient's
own home. Scandinavian journal of caring sciences, 27(4), 831-838.
Moffet, H., Tousignant, M., Nadeau, S., Mérette, C., Boissy, P., Corriveau, H., ... & Dimentberg,
R. (2015). In-home telerehabilitation compared with face-to-face rehabilitation after total
knee arthroplasty: a noninferiority randomized controlled trial. JBJS, 97(14), 1129-1141.
Moore, Z. E., Webster, J., & Samuriwo, R. (2015). Wound‐care teams for preventing and
treating pressure ulcers. The Cochrane Library.
Schenning, K. J., & Deiner, S. G. (2015). Postoperative delirium in the geriatric
patient. Anesthesiology clinics, 33(3), 505-516.
Sweeney, N., Allen, K., Miller, B., Nolan, T., & Sheerin, K. (2017). Perioperative Nursing
Management of Donor and Recipient Patients Undergoing Face Transplantation. AORN
journal, 106(1), 8-19.
Thayaparan, A. J., & Mahdi, E. (2013). The Patient Satisfaction Questionnaire Short Form (PSQ-
18) as an adaptable, reliable, and validated tool for use in various settings. Medical
education online, 18, 1-2.
Weissmann, G. (Ed.). (2013). Mediators of inflammation. Springer Science & Business Media
NURSING ASSIGNMENT
significantly reduces central line–associated bloodstream infections. American journal of
infection control, 42(11), 1146-1151.
Karlsson, M., Karlsson, C., Barbosa da Silva, A., Berggren, I., & Söderlund, M. (2013).
Community nurses' experiences of ethical problems in end‐of‐life care in the patient's
own home. Scandinavian journal of caring sciences, 27(4), 831-838.
Moffet, H., Tousignant, M., Nadeau, S., Mérette, C., Boissy, P., Corriveau, H., ... & Dimentberg,
R. (2015). In-home telerehabilitation compared with face-to-face rehabilitation after total
knee arthroplasty: a noninferiority randomized controlled trial. JBJS, 97(14), 1129-1141.
Moore, Z. E., Webster, J., & Samuriwo, R. (2015). Wound‐care teams for preventing and
treating pressure ulcers. The Cochrane Library.
Schenning, K. J., & Deiner, S. G. (2015). Postoperative delirium in the geriatric
patient. Anesthesiology clinics, 33(3), 505-516.
Sweeney, N., Allen, K., Miller, B., Nolan, T., & Sheerin, K. (2017). Perioperative Nursing
Management of Donor and Recipient Patients Undergoing Face Transplantation. AORN
journal, 106(1), 8-19.
Thayaparan, A. J., & Mahdi, E. (2013). The Patient Satisfaction Questionnaire Short Form (PSQ-
18) as an adaptable, reliable, and validated tool for use in various settings. Medical
education online, 18, 1-2.
Weissmann, G. (Ed.). (2013). Mediators of inflammation. Springer Science & Business Media

45
NURSING ASSIGNMENT
NURSING ASSIGNMENT
1 out of 46
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





