Case Study: Nursing Practice and Management of Type 1 Diabetes
VerifiedAdded on 2022/10/17
|9
|1971
|11
Case Study
AI Summary
This case study presents the nursing practice related to a 50-year-old male, Mr. Kelvin, who was initially diagnosed with type 2 diabetes based on his fatigue, anxiety, family history, and initial blood tests. The case details the patient's history, including a physical exam, urinalysis, and BMI assessment. The initial treatment with metformin was followed by gliclazide. However, subsequent tests revealed the presence of glucose and ketones in the urine, leading to a diagnosis of type 1 diabetes. The paper discusses differential diagnoses, the characteristics of both type 1 and type 2 diabetes, and the diagnostic tests used, including fasting plasma glucose, oral glucose tolerance, random blood glucose, and Hemoglobin A1C tests. The treatment plan focuses on preventing infection, weight loss, and insulin deficiency, including dietary plans, medication, and monitoring of vital signs. Furthermore, the case highlights the importance of patient education, particularly regarding blood glucose monitoring and carbohydrate intake. The paper also includes references to support the nursing practice and treatment decisions.

Running head: NURSING PRACTICE 1
Nursing Practice
Name of Author
Institution of Affiliation
Date of Submission
Nursing Practice
Nursing Practice
Name of Author
Institution of Affiliation
Date of Submission
Nursing Practice
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING PRACTICE 2
History and Physical Exam
Mr Kelvin, a 50-year-old man with a five-month history of fatigue and anxiety. Besides
fatigue and stress, the patient also had a high level of urination, skin infection, and the dryness of
the eyes caused blurring vision which I suspected. His family had a history of diabetes type 2
from his paternal side. The patient had no history of cardiovascular disease, hypertension and
tobacco use. I assessed his blood pressure and confirmed it was normal. Besides, I did the
urinalysis test, which indicated negative. I also evaluated his BMI, which indicated 30kg/m2 and
applied daily blood tests which revealed he had HBA 1c of 71 mm/mol.
Based on his family history and BMI, I identified him with type 2 diabetes. I started him
on metformin but after three weeks the medication up-titrated. One month later, the patient came
for follow up and reported some weight loss and polyuria. He had become increasingly stressed
for his condition and noted that he had lost 4kg. I did a urine test for him and indicated that still,
the urinalysis remained negative.
Based on his condition, I administered a gliclazide and gave him lancets, strips and a
meter (Haas et al., 2012). I trained him about blood sugar monitoring DVLA rules and
hypoglycaemia. After six weeks, he attended for a review appointment and told me he had been
concordant with gliclazide drug. This time he reported a feeling of increased thirst, frequent
urination and blurred vision. The result from a laboratory test showed that the patient had a blood
sugar level of between 16mmol/l to 20mmol/l. Urinalysis at this time showed the presence of
glucose and ketones. The presence of glucose and ketone in urine assured me that the patient had
type 1- diabetes but not type 2, as I had earlier predicted.
Differential Diagnoses
History and Physical Exam
Mr Kelvin, a 50-year-old man with a five-month history of fatigue and anxiety. Besides
fatigue and stress, the patient also had a high level of urination, skin infection, and the dryness of
the eyes caused blurring vision which I suspected. His family had a history of diabetes type 2
from his paternal side. The patient had no history of cardiovascular disease, hypertension and
tobacco use. I assessed his blood pressure and confirmed it was normal. Besides, I did the
urinalysis test, which indicated negative. I also evaluated his BMI, which indicated 30kg/m2 and
applied daily blood tests which revealed he had HBA 1c of 71 mm/mol.
Based on his family history and BMI, I identified him with type 2 diabetes. I started him
on metformin but after three weeks the medication up-titrated. One month later, the patient came
for follow up and reported some weight loss and polyuria. He had become increasingly stressed
for his condition and noted that he had lost 4kg. I did a urine test for him and indicated that still,
the urinalysis remained negative.
Based on his condition, I administered a gliclazide and gave him lancets, strips and a
meter (Haas et al., 2012). I trained him about blood sugar monitoring DVLA rules and
hypoglycaemia. After six weeks, he attended for a review appointment and told me he had been
concordant with gliclazide drug. This time he reported a feeling of increased thirst, frequent
urination and blurred vision. The result from a laboratory test showed that the patient had a blood
sugar level of between 16mmol/l to 20mmol/l. Urinalysis at this time showed the presence of
glucose and ketones. The presence of glucose and ketone in urine assured me that the patient had
type 1- diabetes but not type 2, as I had earlier predicted.
Differential Diagnoses
NURSING PRACTICE 3
Diabetes type 1 is a health condition that is common to children and adults. It is a chronic
metabolic disorder that is characterized by the failure of the pancreas to release the required
insulin that can regulate blood glucose level in the body. The level of insulin may be little or no
insulin when some of the cells that produce insulin are destroyed in the pancreas (Funnell et al.,
2012). Lack of enough insulin makes glucose to pile up in the blood instead of penetrating in the
tissues. As a result, one is unable to utilize sugar for energy. Furthermore, the increased levels of
sugar that remains in the bloodstream leads to excessive dehydration, frequent urination and
destruction of cell tissues that are found in the body system. This is the reason why Kelvin was
experiencing a high level of urination and skin infection (Marcolino et al., 2013).
Type I diabetes is an autoimmune disorder. It starts by attacking the immune system of
the body, which results in the destruction of insulin-producing cells, also referred to as beta cells
in the pancreas being destroyed (Kerner & Brückel, 2014). It is not well known on why the
immune system attacks and destroys beta cells but several studies have demonstrated that the
condition is genetically predisposed. This is why Kelvin’s family had a history of type 2
diabetes. That does not mean it is a must they will get the disorder, but they will be at a high risk
to the conditions. As it is evidenced by (Delamater et al., 2014), environment, viral infections
and diet trigger the type 1 diabetes in individuals with a genetic predisposition. The symptoms of
the conditions may include weakness, blurry vision, irritability, frequent urination and dizziness.
Hypoglycemia can result in a coma if not corrected immediately with the required diet.
Type I diabetes is diagnosed by the combination of symptoms plus a person’s age and
blood tests. The blood tests constitute tests for sugar levels and soluble substances such as
glucose or ketone. Diabetes type 1 can be diagnosed through various blood tests, namely:
Diabetes type 1 is a health condition that is common to children and adults. It is a chronic
metabolic disorder that is characterized by the failure of the pancreas to release the required
insulin that can regulate blood glucose level in the body. The level of insulin may be little or no
insulin when some of the cells that produce insulin are destroyed in the pancreas (Funnell et al.,
2012). Lack of enough insulin makes glucose to pile up in the blood instead of penetrating in the
tissues. As a result, one is unable to utilize sugar for energy. Furthermore, the increased levels of
sugar that remains in the bloodstream leads to excessive dehydration, frequent urination and
destruction of cell tissues that are found in the body system. This is the reason why Kelvin was
experiencing a high level of urination and skin infection (Marcolino et al., 2013).
Type I diabetes is an autoimmune disorder. It starts by attacking the immune system of
the body, which results in the destruction of insulin-producing cells, also referred to as beta cells
in the pancreas being destroyed (Kerner & Brückel, 2014). It is not well known on why the
immune system attacks and destroys beta cells but several studies have demonstrated that the
condition is genetically predisposed. This is why Kelvin’s family had a history of type 2
diabetes. That does not mean it is a must they will get the disorder, but they will be at a high risk
to the conditions. As it is evidenced by (Delamater et al., 2014), environment, viral infections
and diet trigger the type 1 diabetes in individuals with a genetic predisposition. The symptoms of
the conditions may include weakness, blurry vision, irritability, frequent urination and dizziness.
Hypoglycemia can result in a coma if not corrected immediately with the required diet.
Type I diabetes is diagnosed by the combination of symptoms plus a person’s age and
blood tests. The blood tests constitute tests for sugar levels and soluble substances such as
glucose or ketone. Diabetes type 1 can be diagnosed through various blood tests, namely:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING PRACTICE 4
Fasting plasma glucose test (FPGT) where a blood test is assessed toward the beginning of the
day in the wake of fasting overnight. In normal cases, blood sugar levels will remain between 70
-100 mg/dl. Diabetes type 1 is recognized if fasting blood sugar levels are higher than 100mg/dl
(Leete et al., 2016). The other test that can be done is the Oral glucose tolerance test (OGTT). In
this case, the glucose is assessed two hours subsequent to drinking 75 grams of glucose. In the
event that the glucose level is above 200mg/dl, then the patient is determined to have type 1
diabetes.
Another type of diagnoses is random blood glucose test. In the event that the test
demonstrates the glucose of 200mg/dl or higher together with combined side effects of diabetes
is adequate to make a conclusion. Furthermore, is the Hemoglobin A1C glycohemoglobin test,
which estimates the average glucose level over the two to three month. Diabetes is indicated if
the HAIC level is higher than 6.5 per cent like in the case of Kelvin.
Treatment Plan:
Infection can be as a result of high glucose levels which can lead to a decrease in
functioning white blood cells. To prevent such risk factors, I decided to observe for any signs of
infection frequently ensured the patient maintains a good diet by providing him diet plan. Also,
for every follow-up, I administered him with antibiotics and ensured his he kept his skin dry
(Kerner & Brückel, 2014).
To prevent the patient from weight loss, weakness and insulin deficiency, I developed a
care plan which involved the following activities for every follow-up.
Weighing of the patient and get dietary recall by comparing his current intake of food.
Checking of the bowel sounds and making of reports
Checking for any signs and symptoms of hypoglycemia
Fasting plasma glucose test (FPGT) where a blood test is assessed toward the beginning of the
day in the wake of fasting overnight. In normal cases, blood sugar levels will remain between 70
-100 mg/dl. Diabetes type 1 is recognized if fasting blood sugar levels are higher than 100mg/dl
(Leete et al., 2016). The other test that can be done is the Oral glucose tolerance test (OGTT). In
this case, the glucose is assessed two hours subsequent to drinking 75 grams of glucose. In the
event that the glucose level is above 200mg/dl, then the patient is determined to have type 1
diabetes.
Another type of diagnoses is random blood glucose test. In the event that the test
demonstrates the glucose of 200mg/dl or higher together with combined side effects of diabetes
is adequate to make a conclusion. Furthermore, is the Hemoglobin A1C glycohemoglobin test,
which estimates the average glucose level over the two to three month. Diabetes is indicated if
the HAIC level is higher than 6.5 per cent like in the case of Kelvin.
Treatment Plan:
Infection can be as a result of high glucose levels which can lead to a decrease in
functioning white blood cells. To prevent such risk factors, I decided to observe for any signs of
infection frequently ensured the patient maintains a good diet by providing him diet plan. Also,
for every follow-up, I administered him with antibiotics and ensured his he kept his skin dry
(Kerner & Brückel, 2014).
To prevent the patient from weight loss, weakness and insulin deficiency, I developed a
care plan which involved the following activities for every follow-up.
Weighing of the patient and get dietary recall by comparing his current intake of food.
Checking of the bowel sounds and making of reports
Checking for any signs and symptoms of hypoglycemia
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING PRACTICE 5
Administering of glucose and insulin as required
The other risk factor for his condition is deficient in fluid volume. The urine output can
reduce as a result of diabetes leading to hypotension, poor skin and confusion. To prevent this
from happening, I monitored and controlled his blood pressure, temperature and his respiratory
rate and pattern after every two days. Also, I maintained his fluid intake and output. Patients with
diabetes type 1 are exposed to risk for activity intolerance (Worswick et al., 2013). This may be
as a result of high blood pressure or decreased muscle strength and high pulse rate. To intervene
on the risk, I used to assess his muscle strength before and after his medication intake. I also
encouraged the patients to actively participate in activities that can strengthen his muscles
(Dunphy et al., 2015).
Teaching
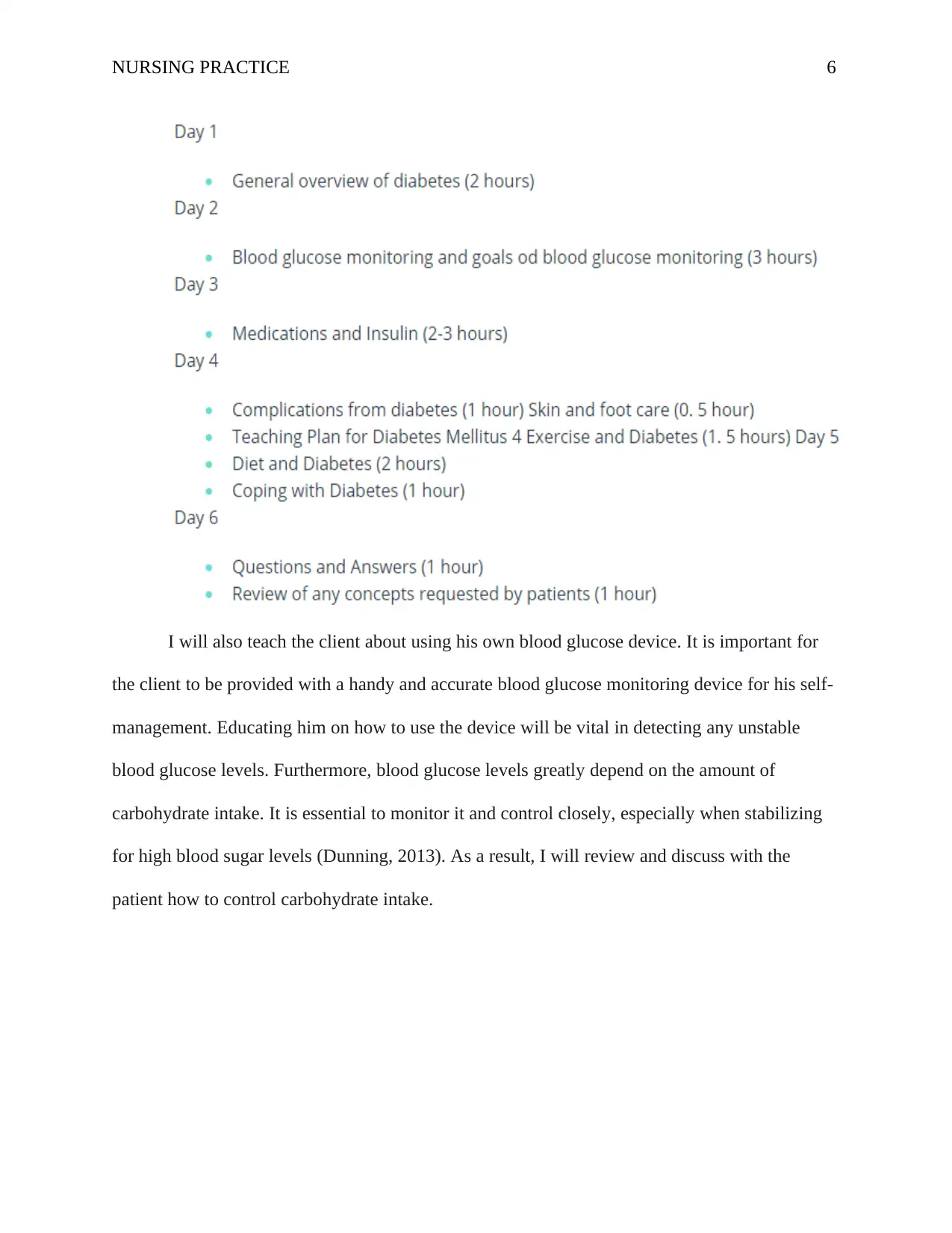
My first priority as a nurse is to educate the patient about the significance of adhering to
the prescribed diabetic therapy. Efforts to control sugar levels in the blood are important it
ensures a good flow of blood around all parts of the body. High glucose levels in the blood can
lead to poor blood circulation, which delays wound healing, thus the need for education
(Bashshur et al., 2015). Below is the teaching session that I will use to make sure the client is
aware of main issues that are linked to his condition.
Administering of glucose and insulin as required
The other risk factor for his condition is deficient in fluid volume. The urine output can
reduce as a result of diabetes leading to hypotension, poor skin and confusion. To prevent this
from happening, I monitored and controlled his blood pressure, temperature and his respiratory
rate and pattern after every two days. Also, I maintained his fluid intake and output. Patients with
diabetes type 1 are exposed to risk for activity intolerance (Worswick et al., 2013). This may be
as a result of high blood pressure or decreased muscle strength and high pulse rate. To intervene
on the risk, I used to assess his muscle strength before and after his medication intake. I also
encouraged the patients to actively participate in activities that can strengthen his muscles
(Dunphy et al., 2015).
Teaching
My first priority as a nurse is to educate the patient about the significance of adhering to
the prescribed diabetic therapy. Efforts to control sugar levels in the blood are important it
ensures a good flow of blood around all parts of the body. High glucose levels in the blood can
lead to poor blood circulation, which delays wound healing, thus the need for education
(Bashshur et al., 2015). Below is the teaching session that I will use to make sure the client is
aware of main issues that are linked to his condition.
NURSING PRACTICE 6
I will also teach the client about using his own blood glucose device. It is important for
the client to be provided with a handy and accurate blood glucose monitoring device for his self-
management. Educating him on how to use the device will be vital in detecting any unstable
blood glucose levels. Furthermore, blood glucose levels greatly depend on the amount of
carbohydrate intake. It is essential to monitor it and control closely, especially when stabilizing
for high blood sugar levels (Dunning, 2013). As a result, I will review and discuss with the
patient how to control carbohydrate intake.
I will also teach the client about using his own blood glucose device. It is important for
the client to be provided with a handy and accurate blood glucose monitoring device for his self-
management. Educating him on how to use the device will be vital in detecting any unstable
blood glucose levels. Furthermore, blood glucose levels greatly depend on the amount of
carbohydrate intake. It is essential to monitor it and control closely, especially when stabilizing
for high blood sugar levels (Dunning, 2013). As a result, I will review and discuss with the
patient how to control carbohydrate intake.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING PRACTICE 7
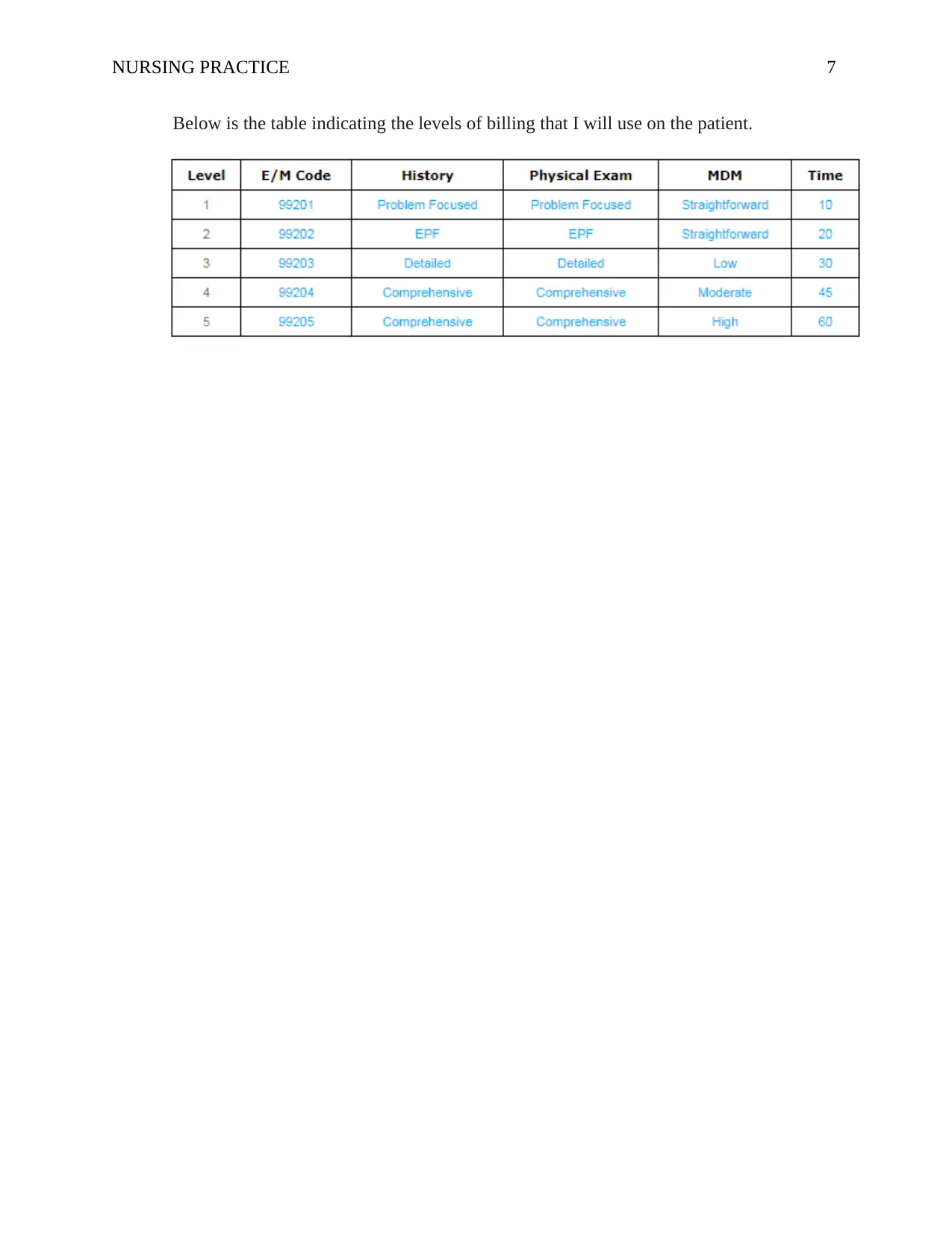
Below is the table indicating the levels of billing that I will use on the patient.
Below is the table indicating the levels of billing that I will use on the patient.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING PRACTICE 8
References
Bashshur, R. L., Shannon, G. W., Smith, B. R., & Woodward, M. A. (2015). The empirical
evidence for the telemedicine intervention in diabetes management. Telemedicine and e-
Health, 21(5), 321-354.
Delamater, A. M., de Wit, M., McDarby, V., Malik, J., & Acerini, C. L. (2014). Psychological
care of children and adolescents with type 1 diabetes. Pediatric diabetes, 15(S20), 232-
244.
Dunning, T. (2013). Care of people with diabetes: a manual of nursing practice. John Wiley &
Sons.
Dunphy, L. M., Winland-Brown, J., Porter, B., & Thomas, D. (2015). Primary care: Art and
science of advanced practice nursing. FA Davis
Funnell, M. M., Brown, T. L., Childs, B. P., Haas, L. B., Hosey, G. M., Jensen, B., ... &
Siminerio, L. M. (2012). National standards for diabetes self-management
education. Diabetes care, 31(Supplement 1), S97-S104.
Haas, L., Maryniuk, M., Beck, J., Cox, C. E., Duker, P., Edwards, L., ... & McLaughlin, S.
(2012). National standards for diabetes self-management education and support. The
Diabetes Educator, 38(5), 619-629.
Kerner, W., & Brückel, J. (2014). Definition, classification and diagnosis of diabetes
mellitus. Experimental and Clinical Endocrinology & Diabetes, 122(07), 384-386.
References
Bashshur, R. L., Shannon, G. W., Smith, B. R., & Woodward, M. A. (2015). The empirical
evidence for the telemedicine intervention in diabetes management. Telemedicine and e-
Health, 21(5), 321-354.
Delamater, A. M., de Wit, M., McDarby, V., Malik, J., & Acerini, C. L. (2014). Psychological
care of children and adolescents with type 1 diabetes. Pediatric diabetes, 15(S20), 232-
244.
Dunning, T. (2013). Care of people with diabetes: a manual of nursing practice. John Wiley &
Sons.
Dunphy, L. M., Winland-Brown, J., Porter, B., & Thomas, D. (2015). Primary care: Art and
science of advanced practice nursing. FA Davis
Funnell, M. M., Brown, T. L., Childs, B. P., Haas, L. B., Hosey, G. M., Jensen, B., ... &
Siminerio, L. M. (2012). National standards for diabetes self-management
education. Diabetes care, 31(Supplement 1), S97-S104.
Haas, L., Maryniuk, M., Beck, J., Cox, C. E., Duker, P., Edwards, L., ... & McLaughlin, S.
(2012). National standards for diabetes self-management education and support. The
Diabetes Educator, 38(5), 619-629.
Kerner, W., & Brückel, J. (2014). Definition, classification and diagnosis of diabetes
mellitus. Experimental and Clinical Endocrinology & Diabetes, 122(07), 384-386.
NURSING PRACTICE 9
Leete, P., Willcox, A., Krogvold, L., Dahl-Jørgensen, K., Foulis, A. K., Richardson, S. J., &
Morgan, N. G. (2016). Differential insulitic profiles determine the extent of β-cell
destruction and the age at onset of type 1 diabetes. Diabetes, 65(5), 1362-1369.
Marcolino, M. S., Maia, J. X., Alkmim, M. B. M., Boersma, E., & Ribeiro, A. L. (2013).
Telemedicine application in the care of diabetes patients: systematic review and meta-
analysis. PloS one, 8(11), e79246.
Worswick, J., Wayne, S. C., Bennett, R., Fiander, M., Mayhew, A., Weir, M. C., ... & Grimshaw,
J. M. (2013). Improving quality of care for persons with diabetes: an overview of
systematic reviews-what does the evidence tell us?. Systematic reviews, 2(1), 26.
Leete, P., Willcox, A., Krogvold, L., Dahl-Jørgensen, K., Foulis, A. K., Richardson, S. J., &
Morgan, N. G. (2016). Differential insulitic profiles determine the extent of β-cell
destruction and the age at onset of type 1 diabetes. Diabetes, 65(5), 1362-1369.
Marcolino, M. S., Maia, J. X., Alkmim, M. B. M., Boersma, E., & Ribeiro, A. L. (2013).
Telemedicine application in the care of diabetes patients: systematic review and meta-
analysis. PloS one, 8(11), e79246.
Worswick, J., Wayne, S. C., Bennett, R., Fiander, M., Mayhew, A., Weir, M. C., ... & Grimshaw,
J. M. (2013). Improving quality of care for persons with diabetes: an overview of
systematic reviews-what does the evidence tell us?. Systematic reviews, 2(1), 26.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





