CAM106A: Childhood Obesity in Australia and Public Health Initiatives
VerifiedAdded on 2022/10/17
|12
|2131
|40
Report
AI Summary
This report addresses the critical issue of childhood obesity in Australia, particularly among Indigenous children. It defines obesity, outlines diagnostic criteria, and explores the causes, including dietary imbalances, sedentary lifestyles, and socioeconomic factors. The report also examines the long-term health implications of childhood obesity, such as chronic diseases, and identifies key influencers like low socioeconomic status and cultural perceptions. Furthermore, it reviews public health initiatives, such as the Go4Fun program, and highlights the need for targeted strategies addressing social determinants, cultural competence, and remote area accessibility. The report emphasizes the importance of comprehensive public health approaches to effectively combat childhood obesity in vulnerable populations.

Running head: NUTRITION, SOCIETY AND PUBLIC HEALTH
NUTRITION, SOCIETY AND PUBLIC HEALTH
Name of the Student:
Name of the University:
Author note:
NUTRITION, SOCIETY AND PUBLIC HEALTH
Name of the Student:
Name of the University:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NUTRITION, SOCIETY AND PUBLIC HEALTH
Executive Summary
Childhood obesity continues to be a global public health issue with high rates observed in
Australia across both Aboriginal and Non-Aboriginal populations. The following report aimed to
shed light on the issue of childhood obesity in Australia, including key definitions, its criteria for
diagnosis, prevalent causes of the issue, long term implications of obesity on children’s health,
possible factors which may influence occurrence of childhood obesity and a public health
initiative to combat the same across Indigenous children in Australia. While impressive public
health initiatives exist, there is a need to target socioeconomic factors, remote residence, cultural
perceptions and healthcare accessibility and affordability issues to optimally eradicate childhood
obesity among Indigenous Australian children
Executive Summary
Childhood obesity continues to be a global public health issue with high rates observed in
Australia across both Aboriginal and Non-Aboriginal populations. The following report aimed to
shed light on the issue of childhood obesity in Australia, including key definitions, its criteria for
diagnosis, prevalent causes of the issue, long term implications of obesity on children’s health,
possible factors which may influence occurrence of childhood obesity and a public health
initiative to combat the same across Indigenous children in Australia. While impressive public
health initiatives exist, there is a need to target socioeconomic factors, remote residence, cultural
perceptions and healthcare accessibility and affordability issues to optimally eradicate childhood
obesity among Indigenous Australian children
2NUTRITION, SOCIETY AND PUBLIC HEALTH
Table of Contents
Introduction..........................................................................................................................2
Discussion............................................................................................................................2
Definitions.......................................................................................................................2
Diagnosis.........................................................................................................................3
Causes..............................................................................................................................3
Long term Implications....................................................................................................4
Influencers.......................................................................................................................4
Public Health Initiatives..................................................................................................5
Conclusion...........................................................................................................................5
References............................................................................................................................7
Appendix............................................................................................................................10
Table of Contents
Introduction..........................................................................................................................2
Discussion............................................................................................................................2
Definitions.......................................................................................................................2
Diagnosis.........................................................................................................................3
Causes..............................................................................................................................3
Long term Implications....................................................................................................4
Influencers.......................................................................................................................4
Public Health Initiatives..................................................................................................5
Conclusion...........................................................................................................................5
References............................................................................................................................7
Appendix............................................................................................................................10
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NUTRITION, SOCIETY AND PUBLIC HEALTH
Introduction
The incidence of childhood obesity across Australian children, especially those belonging
toAboriginal and Torre Strait Islander communities is escalating at an alarming rate (Dyer et al.,
2018).The following report will aim to discuss the issue of childhood obesity in Australia in
general and Indigenous children in particular.
Discussion
Definitions
Approximately 41 million children under the age of 5 were found to be suffering from
obesity and the overweight during the year 2016. Additionally, 340 million children as well as
adolescents belonging to the age group of 5 to 19 years were also found to be inflicted with
overweight and obesity in 2016 (World Health Organization, 2018). Approximately 24.9% of
Australian children within the ages 5 to 17 years have been found to be either obese or
overweight (Department of Health, 2019). Further according to the Australian Aboriginal and
Torres Strait Islander Health Survey performed by the Australian Bureau of Statistics in 2012-
2013, approximately a third of Indigenous Australian children within the ages g of 2 to 14 years
were estimated to be either overweight (20%) and obese (10%) respectively (Australian Bureau
of Statistics, 2019).
According to the Royal Children’s Hospital Melbourne, childhood overweight and
obesity can be implied as a state of health where children possess a weight for height greater than
the 90th percentile as per the growth charts formulated by the National Centre for Health
Introduction
The incidence of childhood obesity across Australian children, especially those belonging
toAboriginal and Torre Strait Islander communities is escalating at an alarming rate (Dyer et al.,
2018).The following report will aim to discuss the issue of childhood obesity in Australia in
general and Indigenous children in particular.
Discussion
Definitions
Approximately 41 million children under the age of 5 were found to be suffering from
obesity and the overweight during the year 2016. Additionally, 340 million children as well as
adolescents belonging to the age group of 5 to 19 years were also found to be inflicted with
overweight and obesity in 2016 (World Health Organization, 2018). Approximately 24.9% of
Australian children within the ages 5 to 17 years have been found to be either obese or
overweight (Department of Health, 2019). Further according to the Australian Aboriginal and
Torres Strait Islander Health Survey performed by the Australian Bureau of Statistics in 2012-
2013, approximately a third of Indigenous Australian children within the ages g of 2 to 14 years
were estimated to be either overweight (20%) and obese (10%) respectively (Australian Bureau
of Statistics, 2019).
According to the Royal Children’s Hospital Melbourne, childhood overweight and
obesity can be implied as a state of health where children possess a weight for height greater than
the 90th percentile as per the growth charts formulated by the National Centre for Health
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NUTRITION, SOCIETY AND PUBLIC HEALTH
Statistics (NCHS), or possess a weight greater than 120% of the median of weight as per the age,
height and sex of the concerned child (State Government Victoria, 2019).
Diagnosis
As postulated by the World Health Organization, childhood obesity can be
diagnosedwithin school going children using the growth reference charts of Body Mass Index
(BMI) for sex and age. A school going child can considered has overweight is he or she has a
BMI which is one standard deviation from the recommended BMI as per the sex and age of the
child. Similarly, a child can be considered to the obese if he or she has a BMI which is two
standard deviations from the recommended BMI as per the sex and age of the child (World
Health Organization., 2019).
Causes
As evidenced by World Health Organization, childhood obesity is primarily caused due
to an absence of equilibrium between the amount of calories which are ingested and the amount
of calories which are metabolized or expended. Such imbalances in the intake of calories occurs
due to an excessive consumption of calorie rich foods which are dense in sugars and fats but is
inadequate infibre and micronutrients such as minerals and vitamins (World Health
Organization, 2019). Additional causative factors includes increased adherence to sedentary
lifestyle such as lack of exercise, engagement in recreational activities with prolonged hours of
sitting and automation of transport characterized by reduced physical exertion. Another key
contributor of childhood obesity is the excessive consumption of sugary beverages especially in
developed countries (Sahoo et al., 2015).
Statistics (NCHS), or possess a weight greater than 120% of the median of weight as per the age,
height and sex of the concerned child (State Government Victoria, 2019).
Diagnosis
As postulated by the World Health Organization, childhood obesity can be
diagnosedwithin school going children using the growth reference charts of Body Mass Index
(BMI) for sex and age. A school going child can considered has overweight is he or she has a
BMI which is one standard deviation from the recommended BMI as per the sex and age of the
child. Similarly, a child can be considered to the obese if he or she has a BMI which is two
standard deviations from the recommended BMI as per the sex and age of the child (World
Health Organization., 2019).
Causes
As evidenced by World Health Organization, childhood obesity is primarily caused due
to an absence of equilibrium between the amount of calories which are ingested and the amount
of calories which are metabolized or expended. Such imbalances in the intake of calories occurs
due to an excessive consumption of calorie rich foods which are dense in sugars and fats but is
inadequate infibre and micronutrients such as minerals and vitamins (World Health
Organization, 2019). Additional causative factors includes increased adherence to sedentary
lifestyle such as lack of exercise, engagement in recreational activities with prolonged hours of
sitting and automation of transport characterized by reduced physical exertion. Another key
contributor of childhood obesity is the excessive consumption of sugary beverages especially in
developed countries (Sahoo et al., 2015).

5NUTRITION, SOCIETY AND PUBLIC HEALTH
As reported by the Australian Institute of Health and Welfare (AIHW) Australian
children and adolescents of Indigenous ethnicity have greater susceptibility of acquiring or
obesity, especially those who reside in remote regions or belong to groups which are
socioeconomically disadvantaged (Australian Institute of Health and Welfare, 2017). It is
worthwhile to remember that obesity has multidimensional and multidisciplinary facets and its
causes are not merely limited to dietary intake and sedentary lifestyle but also due to levels of
community awareness, prevalence of health reforms and policies, rates of urbanization,
marketing and advertisement of processed food items as well as affordability and accessibility
towards healthcare educational and intervention resources – which are often compromised across
Indigenous populations (Hardy et al., 2019). Children, moreover, in comparison to adults, lack
the ability to opt for the environment in which they reside and eat, lack the awareness and
understanding of the impact of unhealthy behaviors and hence, are passive targets to the dietary
and lifestyle habits adhered to by adults (Rohit et al., 2019).
Long term Implications
Childhood is the foundational stage of establishing long term growth and development
and hence a state of overweight and obesity at this state, predisposes children to maintain such
unhealthy anthropometric measurements in the future throughout adulthood. Lack of mitigation
of obesity increases long term risks of acquiring chronic metabolic diseases in the future such as
diabetes mellitus, hypertension and hyperlipidaemia. Further, long term prevalence of obesity
also paves the way for bone related disorders such as osteoporosis, along with hepatic and renal
disorders and even cancer (Gurnani, Birken& Hamilton, 2015).
As reported by the Australian Institute of Health and Welfare (AIHW) Australian
children and adolescents of Indigenous ethnicity have greater susceptibility of acquiring or
obesity, especially those who reside in remote regions or belong to groups which are
socioeconomically disadvantaged (Australian Institute of Health and Welfare, 2017). It is
worthwhile to remember that obesity has multidimensional and multidisciplinary facets and its
causes are not merely limited to dietary intake and sedentary lifestyle but also due to levels of
community awareness, prevalence of health reforms and policies, rates of urbanization,
marketing and advertisement of processed food items as well as affordability and accessibility
towards healthcare educational and intervention resources – which are often compromised across
Indigenous populations (Hardy et al., 2019). Children, moreover, in comparison to adults, lack
the ability to opt for the environment in which they reside and eat, lack the awareness and
understanding of the impact of unhealthy behaviors and hence, are passive targets to the dietary
and lifestyle habits adhered to by adults (Rohit et al., 2019).
Long term Implications
Childhood is the foundational stage of establishing long term growth and development
and hence a state of overweight and obesity at this state, predisposes children to maintain such
unhealthy anthropometric measurements in the future throughout adulthood. Lack of mitigation
of obesity increases long term risks of acquiring chronic metabolic diseases in the future such as
diabetes mellitus, hypertension and hyperlipidaemia. Further, long term prevalence of obesity
also paves the way for bone related disorders such as osteoporosis, along with hepatic and renal
disorders and even cancer (Gurnani, Birken& Hamilton, 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NUTRITION, SOCIETY AND PUBLIC HEALTH
Influencers
One of the strongest influencers of childhood obesity among Indigenous Australians is
their low socioeconomic status and residence in remote areas which predisposes them to food
insecurity and inadequate accessibility and affordability to procure and consume foods a
nutritionally balanced diet and rely more on cheaper, energy dense, easily available foods, such
as starchy vegetables, rice and sugary beverages or processed foods rich in high and fat for those
residing in urban areas (Hickie, Douglas &Ciszek, 2016). Such groups, due to lack of cultural
competence and social disadvantage are often deprived of access to healthcare educational
resources and interventions resulting in low rates of health literacy. Cultural perceptions is
another key influencer of Indigenous lifestyle behaviours - exercise interventions which focus
on physical activity and close ties Aboriginal’s possess with their natural resources like their land
and procurement of food and wood have greater rates of engagement and success (Dahlberg et
al., 2017).
Public Health Initiatives
A number of public health initiatives have been executed by the New South Wales
(NSW) government, of which the Go4Fun program, aiming to lifestyle in children aged 7 to 13
years has proven to be a success. Aboriginal Go4Fun was further implemented in 2015, to
specifically target Aboriginal groups across metropolitan areas of NSW. Additionally, 90% of
schools and 97% of early childhood organizations with increased proportion of Aboriginal
children participated in the Live Life Well School Program and Munch & Moe program
respectively (NSW Government, 2019). While targeted delivery of public health initiatives
towards Indigenous children may contribute to its efficacy, ineffective long term results may still
be achieved due to lack of program expansion to include Aboriginals in remote areas of NSW
Influencers
One of the strongest influencers of childhood obesity among Indigenous Australians is
their low socioeconomic status and residence in remote areas which predisposes them to food
insecurity and inadequate accessibility and affordability to procure and consume foods a
nutritionally balanced diet and rely more on cheaper, energy dense, easily available foods, such
as starchy vegetables, rice and sugary beverages or processed foods rich in high and fat for those
residing in urban areas (Hickie, Douglas &Ciszek, 2016). Such groups, due to lack of cultural
competence and social disadvantage are often deprived of access to healthcare educational
resources and interventions resulting in low rates of health literacy. Cultural perceptions is
another key influencer of Indigenous lifestyle behaviours - exercise interventions which focus
on physical activity and close ties Aboriginal’s possess with their natural resources like their land
and procurement of food and wood have greater rates of engagement and success (Dahlberg et
al., 2017).
Public Health Initiatives
A number of public health initiatives have been executed by the New South Wales
(NSW) government, of which the Go4Fun program, aiming to lifestyle in children aged 7 to 13
years has proven to be a success. Aboriginal Go4Fun was further implemented in 2015, to
specifically target Aboriginal groups across metropolitan areas of NSW. Additionally, 90% of
schools and 97% of early childhood organizations with increased proportion of Aboriginal
children participated in the Live Life Well School Program and Munch & Moe program
respectively (NSW Government, 2019). While targeted delivery of public health initiatives
towards Indigenous children may contribute to its efficacy, ineffective long term results may still
be achieved due to lack of program expansion to include Aboriginals in remote areas of NSW
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NUTRITION, SOCIETY AND PUBLIC HEALTH
where every child may not have access to schools and early childhood services (Gifford et al.,
2018).
Conclusion
This report demonstrates the role of socioeconomic disadvantage and cultural perceptions
as key contributors to childhood obesity across Aboriginals. To conclude, public health
initiatives must target social determinants, disadvantages and cultural competence for optimum
effectiveness.
where every child may not have access to schools and early childhood services (Gifford et al.,
2018).
Conclusion
This report demonstrates the role of socioeconomic disadvantage and cultural perceptions
as key contributors to childhood obesity across Aboriginals. To conclude, public health
initiatives must target social determinants, disadvantages and cultural competence for optimum
effectiveness.
8NUTRITION, SOCIETY AND PUBLIC HEALTH
References
Australian Bureau of Statistics. (2019). 4727.0.55.001 - Australian Aboriginal and Torres Strait
Islander Health Survey: First Results, Australia, 2012-13. Retrieved 30 July 2019, from
https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4727.0.55.001Chapter3102012-13.
Australian Institute of Health and Welfare. (2017). A picture of overweight and obesity in
Australia (2017). Retrieved 30 July 2019, from
https://www.aihw.gov.au/getmedia/172fba28-785e-4a08-ab37-2da3bbae40b8/aihw-phe-
216.pdf.aspx?inline=true.
Dahlberg, E., Hamilton, S., Hamid, F., & Thompson, S. (2018). Indigenous Australians
Perceptions’ of Physical Activity: A Qualitative Systematic Review. International
journal of environmental research and public health, 15(7), 1492.
Department of Health. (2019). Department of Health | Overweight and Obesity. Retrieved 30
July 2019, from
https://www1.health.gov.au/internet/main/publishing.nsf/Content/Overweight-and-
Obesity.
Dyer, S. M., Gomersall, J. S., Smithers, L. G., Davy, C., Coleman, D. T., & Street, J. M. (2017).
Prevalence and characteristics of overweight and obesity in indigenous Australian
children: a systematic review. Critical reviews in food science and nutrition, 57(7), 1365-
1376.
Gifford, J., Gwynn, J., Hardy, L., Turner, N., Henderson, L., Innes-Hughes, C., & Flood, V.
(2018). Review of Short-Form Questions for the Evaluation of a Diet, Physical Activity,
References
Australian Bureau of Statistics. (2019). 4727.0.55.001 - Australian Aboriginal and Torres Strait
Islander Health Survey: First Results, Australia, 2012-13. Retrieved 30 July 2019, from
https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4727.0.55.001Chapter3102012-13.
Australian Institute of Health and Welfare. (2017). A picture of overweight and obesity in
Australia (2017). Retrieved 30 July 2019, from
https://www.aihw.gov.au/getmedia/172fba28-785e-4a08-ab37-2da3bbae40b8/aihw-phe-
216.pdf.aspx?inline=true.
Dahlberg, E., Hamilton, S., Hamid, F., & Thompson, S. (2018). Indigenous Australians
Perceptions’ of Physical Activity: A Qualitative Systematic Review. International
journal of environmental research and public health, 15(7), 1492.
Department of Health. (2019). Department of Health | Overweight and Obesity. Retrieved 30
July 2019, from
https://www1.health.gov.au/internet/main/publishing.nsf/Content/Overweight-and-
Obesity.
Dyer, S. M., Gomersall, J. S., Smithers, L. G., Davy, C., Coleman, D. T., & Street, J. M. (2017).
Prevalence and characteristics of overweight and obesity in indigenous Australian
children: a systematic review. Critical reviews in food science and nutrition, 57(7), 1365-
1376.
Gifford, J., Gwynn, J., Hardy, L., Turner, N., Henderson, L., Innes-Hughes, C., & Flood, V.
(2018). Review of Short-Form Questions for the Evaluation of a Diet, Physical Activity,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NUTRITION, SOCIETY AND PUBLIC HEALTH
and Sedentary Behaviour Intervention in a Community Program Targeting Vulnerable
Australian Children. Children, 5(7), 95.
Gurnani, M., Birken, C., & Hamilton, J. (2015). Childhood obesity: causes, consequences, and
management. Pediatric Clinics, 62(4), 821-840.
Hardy, L. L., MacNiven, R., Esgin, T., &Mihrshahi, S. (2019). Cross-sectional changes in weight
status and weight related behaviors among Australian children and Australian Indigenous
children between 2010 and 2015. PloS one, 14(7), e0211249.
Hickie, M., Douglas, K., &Ciszek, K. (2016). RACGP - The prevalence of overweight and
obesity in Indigenous kindergarten children – a cross sectional population based study.
Retrieved 30 July 2019, from https://www.racgp.org.au/afp/2013/july/indigenous-child-
obesity/.
NSW Government. (2019). Preventive Health Pr0grams: Aboriginal Health. Retrieved 30 July
2019, from https://www.health.nsw.gov.au/aboriginal/Publications/snapshot-aboriginal-
prev-health.pdf.
Rohit, A., Tonkin, E., Maple-Brown, L., Golley, R., McCarthy, L., &Brimblecombe, J. (2019).
Parent Feeding Practices in the Australian Indigenous Population within the Context of
non-Indigenous Australians and Indigenous Populations in Other High-Income Countries
—A Scoping Review. Advances in Nutrition, 10(1), 89-103.
Sahoo, K., Sahoo, B., Choudhury, A. K., Sofi, N. Y., Kumar, R., &Bhadoria, A. S. (2015).
Childhood obesity: causes and consequences. Journal of family medicine and primary
care, 4(2), 187.
and Sedentary Behaviour Intervention in a Community Program Targeting Vulnerable
Australian Children. Children, 5(7), 95.
Gurnani, M., Birken, C., & Hamilton, J. (2015). Childhood obesity: causes, consequences, and
management. Pediatric Clinics, 62(4), 821-840.
Hardy, L. L., MacNiven, R., Esgin, T., &Mihrshahi, S. (2019). Cross-sectional changes in weight
status and weight related behaviors among Australian children and Australian Indigenous
children between 2010 and 2015. PloS one, 14(7), e0211249.
Hickie, M., Douglas, K., &Ciszek, K. (2016). RACGP - The prevalence of overweight and
obesity in Indigenous kindergarten children – a cross sectional population based study.
Retrieved 30 July 2019, from https://www.racgp.org.au/afp/2013/july/indigenous-child-
obesity/.
NSW Government. (2019). Preventive Health Pr0grams: Aboriginal Health. Retrieved 30 July
2019, from https://www.health.nsw.gov.au/aboriginal/Publications/snapshot-aboriginal-
prev-health.pdf.
Rohit, A., Tonkin, E., Maple-Brown, L., Golley, R., McCarthy, L., &Brimblecombe, J. (2019).
Parent Feeding Practices in the Australian Indigenous Population within the Context of
non-Indigenous Australians and Indigenous Populations in Other High-Income Countries
—A Scoping Review. Advances in Nutrition, 10(1), 89-103.
Sahoo, K., Sahoo, B., Choudhury, A. K., Sofi, N. Y., Kumar, R., &Bhadoria, A. S. (2015).
Childhood obesity: causes and consequences. Journal of family medicine and primary
care, 4(2), 187.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NUTRITION, SOCIETY AND PUBLIC HEALTH
State Government Victoria. (2019). Overweight and obesity. Retrieved 30 July 2019, from
https://education.vic.gov.au/Documents/childhood/professionals/support/
overweightobesity.pdf.
World Health Organization. (2018). Obesity and overweight. Retrieved 30 July 2019, from
https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
World Health Organization. (2019). Childhood overweight and obesity. Retrieved 30 July 2019,
from https://www.who.int/dietphysicalactivity/childhood/en/.
World Health Organization. (2019). Childhood overweight and obesity. Retrieved 30 July 2019,
from https://www.who.int/dietphysicalactivity/childhood/en/.
State Government Victoria. (2019). Overweight and obesity. Retrieved 30 July 2019, from
https://education.vic.gov.au/Documents/childhood/professionals/support/
overweightobesity.pdf.
World Health Organization. (2018). Obesity and overweight. Retrieved 30 July 2019, from
https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
World Health Organization. (2019). Childhood overweight and obesity. Retrieved 30 July 2019,
from https://www.who.int/dietphysicalactivity/childhood/en/.
World Health Organization. (2019). Childhood overweight and obesity. Retrieved 30 July 2019,
from https://www.who.int/dietphysicalactivity/childhood/en/.
11NUTRITION, SOCIETY AND PUBLIC HEALTH
Appendix
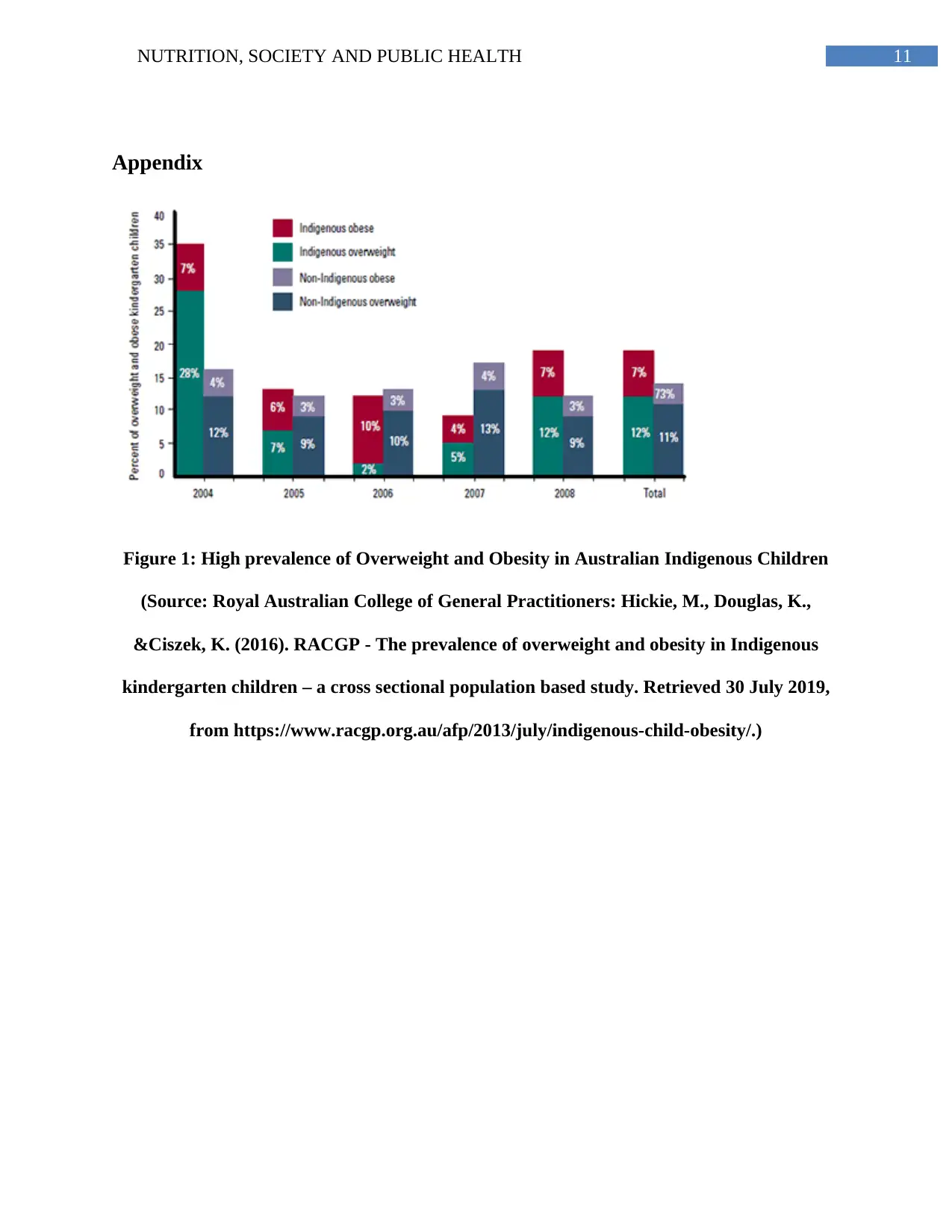
Figure 1: High prevalence of Overweight and Obesity in Australian Indigenous Children
(Source: Royal Australian College of General Practitioners: Hickie, M., Douglas, K.,
&Ciszek, K. (2016). RACGP - The prevalence of overweight and obesity in Indigenous
kindergarten children – a cross sectional population based study. Retrieved 30 July 2019,
from https://www.racgp.org.au/afp/2013/july/indigenous-child-obesity/.)
Appendix
Figure 1: High prevalence of Overweight and Obesity in Australian Indigenous Children
(Source: Royal Australian College of General Practitioners: Hickie, M., Douglas, K.,
&Ciszek, K. (2016). RACGP - The prevalence of overweight and obesity in Indigenous
kindergarten children – a cross sectional population based study. Retrieved 30 July 2019,
from https://www.racgp.org.au/afp/2013/july/indigenous-child-obesity/.)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





