Analysis of Heart Failure Pathophysiology in Elderly Patients - Report
VerifiedAdded on 2023/01/04
|18
|6448
|37
Report
AI Summary
This report provides a comprehensive analysis of heart failure in elderly patients, focusing on its pathophysiology within the New Zealand context. It begins with an abstract summarizing the prevalence of heart failure among the elderly population, highlighting its significant impact on mortality and healthcare resources. The introduction emphasizes the increasing incidence of heart failure in older adults, linking it to age-related changes in the cardiovascular system and associated comorbidities. The report then delves into the epidemiology of heart failure in New Zealand, presenting statistics on hospital admissions, mortality rates, and the disproportionate impact on the Maori population. The normal physiology of the cardiovascular system is described, followed by an in-depth examination of the pathophysiology of heart failure, including the mechanisms behind decreased cardiac efficiency, compensatory mechanisms, and the resulting clinical manifestations such as shortness of breath and chest pain. Diagnostic tests, including X-rays and echocardiograms, are discussed, along with current prevention and management options. The report concludes with recommendations for improving patient outcomes through dietary restrictions, lifestyle changes, and a focus on early intervention strategies, including comprehensive assessments.

Pathophysiology
Student name;
Institutional affiliation:
Student name;
Institutional affiliation:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEART FAILURE IN ELDERLY PATIENTS
ABSTRACT
Heart failure has a high incidence rate among elderly patient in New Zealand. On the
epidemiology of heart failure in New Zealand, it is found that there are of 12,000 admissions
every year and it contributes to 33% of deaths every year. Prevalence of heart failure keeps on
increasing over every decade. On normal physiology of the cardiovascular system, the main
function of the cardiovascular system is to transmit materials throughout the body. Materials
entering the body such as oxygen from the lungs and nutrients and also water through intestinal
tract are carried to cells. Arteries carry blood away from the heart and veins return blood to the
heart. Pathophysiology of heart failure usually manifests through a decrease in the efficiency of
the heart muscle either through work overload or damage. The main symptom of heart failure is
increased heart rate and is usually stimulated by increased sympathetic activity such that
adequate cardiac output is maintained. Other symptoms include shortness of breath, chest pain,
pulses alternans, pulmonary edema, cough, loss of appetite, excess urination, dizziness and
fatigues. Diagnostic tests important for the diagnosis of heart failure are the x-ray image,
electrocardiogram, blood test, echocardiogram, stress test, magnetic resonance imaging, coronary
angiogram, and cardiac computerized tomography. Preventive measures of heart failure include
lifestyle changes, treatment of risk factors, education and creation of public awareness on heart
failure disease. On management, the pharmacologic management includes the use of drugs such
as vasodilators and diuretics while there is also the use of invasive therapies. On non-
pharmacologic ways of managing heart failure, there is dietary management, lifestyle changes,
daily regular activities, and stress management. Recommendations of this study are mainly on
management and treatment. It involves implementation of the management and treatment of
heart failure for example recommendation on dietary restriction of salt and fat in the diet.
INTRODUCTION
Elderly patients are a group of people who are not homogenous with wide or weaknesses and
fitness for each age. Age-related changes in the heart contribute to progressive loss of cardiac
ABSTRACT
Heart failure has a high incidence rate among elderly patient in New Zealand. On the
epidemiology of heart failure in New Zealand, it is found that there are of 12,000 admissions
every year and it contributes to 33% of deaths every year. Prevalence of heart failure keeps on
increasing over every decade. On normal physiology of the cardiovascular system, the main
function of the cardiovascular system is to transmit materials throughout the body. Materials
entering the body such as oxygen from the lungs and nutrients and also water through intestinal
tract are carried to cells. Arteries carry blood away from the heart and veins return blood to the
heart. Pathophysiology of heart failure usually manifests through a decrease in the efficiency of
the heart muscle either through work overload or damage. The main symptom of heart failure is
increased heart rate and is usually stimulated by increased sympathetic activity such that
adequate cardiac output is maintained. Other symptoms include shortness of breath, chest pain,
pulses alternans, pulmonary edema, cough, loss of appetite, excess urination, dizziness and
fatigues. Diagnostic tests important for the diagnosis of heart failure are the x-ray image,
electrocardiogram, blood test, echocardiogram, stress test, magnetic resonance imaging, coronary
angiogram, and cardiac computerized tomography. Preventive measures of heart failure include
lifestyle changes, treatment of risk factors, education and creation of public awareness on heart
failure disease. On management, the pharmacologic management includes the use of drugs such
as vasodilators and diuretics while there is also the use of invasive therapies. On non-
pharmacologic ways of managing heart failure, there is dietary management, lifestyle changes,
daily regular activities, and stress management. Recommendations of this study are mainly on
management and treatment. It involves implementation of the management and treatment of
heart failure for example recommendation on dietary restriction of salt and fat in the diet.
INTRODUCTION
Elderly patients are a group of people who are not homogenous with wide or weaknesses and
fitness for each age. Age-related changes in the heart contribute to progressive loss of cardiac
cells, hypertrophy of the remaining cells and connective tissue accumulation which cause a
decline in diastolic function while systolic function with age. Heart disease is a very serious
problem in elderly patients which has caused high mortality and frequent hospitalization in
elderly patients (Lazzarini et.al, 2019), it is linked to deteriorating quality of life and aggressive
medical treatment which causes a lot of side effects for the elderly compared to younger people
because of differences in drug metabolism, drug interaction, wound healing, poor tolerance to
surgical procedures and impaired cognitive and psychosocial interaction leading to high
mortality rate for the elderly. Heart failure is a heart abnormality where the heart muscles are
unable to pump blood as well as it should be, it is also called congestive heart failure
(Ponikowski, et.al, 2014). It occurs as a result of narrowed arteries in the heart or too high blood
pressure that eventually leaves the heart too weak to be able to pump blood efficiently.
Incidences of congestive heart failure among elderly patient is increasing (Parén, et.al, 2014)
because they present with many complicated comorbidities for example hypertension, atrial
fibrillation, peripheral vascular disease, kidney failure, anemia and excess use of pharmaceutical
drugs which leads to many side effects, its management is hard because of the many of many
complications mentioned above. It is important to relate these conditions for proper management
of the condition. Its significance to New Zealand is that it is the major and gradually growing
problem that comes as are a result of its poor prognosis and it has an impact on health care is
costly placing a financial burden on the health care system. Non pharmacological strategies such
as dietary interventions for example restrictions of some diet intake such as potassium and
sodium-rich food, exercise training are important in reducing heart failure, functional and
cognitive assessment of this patients reduces risk of heart failure and it helps in guiding the
management in older heart failure patients and clinical trials that help in assessing the functional
status and quality of life and heart disease should be encouraged to help in guiding management
of this age group. A comprehensive assessment is important key action in the management of
patients of heart failure for early treatment of symptoms and monitoring of progress (O'Gara,
2013).
EPIDEMIOLOGY OF HEART FAILURE
decline in diastolic function while systolic function with age. Heart disease is a very serious
problem in elderly patients which has caused high mortality and frequent hospitalization in
elderly patients (Lazzarini et.al, 2019), it is linked to deteriorating quality of life and aggressive
medical treatment which causes a lot of side effects for the elderly compared to younger people
because of differences in drug metabolism, drug interaction, wound healing, poor tolerance to
surgical procedures and impaired cognitive and psychosocial interaction leading to high
mortality rate for the elderly. Heart failure is a heart abnormality where the heart muscles are
unable to pump blood as well as it should be, it is also called congestive heart failure
(Ponikowski, et.al, 2014). It occurs as a result of narrowed arteries in the heart or too high blood
pressure that eventually leaves the heart too weak to be able to pump blood efficiently.
Incidences of congestive heart failure among elderly patient is increasing (Parén, et.al, 2014)
because they present with many complicated comorbidities for example hypertension, atrial
fibrillation, peripheral vascular disease, kidney failure, anemia and excess use of pharmaceutical
drugs which leads to many side effects, its management is hard because of the many of many
complications mentioned above. It is important to relate these conditions for proper management
of the condition. Its significance to New Zealand is that it is the major and gradually growing
problem that comes as are a result of its poor prognosis and it has an impact on health care is
costly placing a financial burden on the health care system. Non pharmacological strategies such
as dietary interventions for example restrictions of some diet intake such as potassium and
sodium-rich food, exercise training are important in reducing heart failure, functional and
cognitive assessment of this patients reduces risk of heart failure and it helps in guiding the
management in older heart failure patients and clinical trials that help in assessing the functional
status and quality of life and heart disease should be encouraged to help in guiding management
of this age group. A comprehensive assessment is important key action in the management of
patients of heart failure for early treatment of symptoms and monitoring of progress (O'Gara,
2013).
EPIDEMIOLOGY OF HEART FAILURE
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Heart failure is becoming a global public health issue and is significantly increased over time. Its
diagnosis is majorly associated with low quality of life, poverty and high morbidity and mortality
rates despite management in the hospital. Overall, the number of heart failure patients aged ≥80
are more than a quarter of the community (Fowkes, 2013).
In New Zealand, it is estimated that every year there are about 12,000 hospital admissions of
nearly 5,500 patients heart failure. These patients stay in the hospital for an average length of 5
days. An average1.5-2% of the health budget is channeled towards Heart failure associated costs,
hence representing a notable burden in the healthcare system of New Zealand (Milne, 2012). The
Maori people have been found to get diagnosed with heart failure 10-15 years earlier than the
non-Maori individuals (Wang, 2013). It is estimated that the mortality from heart failure among
Maori males aged 45-64 years is eight times higher than the non-Maori. The Maori with age of
65 years and above also experience heart failure approximately 3 times higher than non-Maori.
Similar cases of high mortality rate are also seen in the Maori females, whereby, there is about 8
to 9 times more hospital admission among the compared than the non-Maori.
Further statistics have indicated that the number of people living with heart disease in New
Zealand is 186,000 which implies one in every 20 adults. Cardiovascular disease also is
responsible for 33% of deaths annually, which makes it the leading cause of death in New
Zealand. It includes; stroke, blood vessels, and stroke disease.
As the population ages, the prevalence of Heart failure keeps on increasing and over the next few
decades the number of people diagnosed with this condition will have gone up by 50%
NORMAL PHYSIOLOGY OF CARDIOVASCULAR SYSTEM
The following diagram illustrates the normal physiology of the cardiovascular system
diagnosis is majorly associated with low quality of life, poverty and high morbidity and mortality
rates despite management in the hospital. Overall, the number of heart failure patients aged ≥80
are more than a quarter of the community (Fowkes, 2013).
In New Zealand, it is estimated that every year there are about 12,000 hospital admissions of
nearly 5,500 patients heart failure. These patients stay in the hospital for an average length of 5
days. An average1.5-2% of the health budget is channeled towards Heart failure associated costs,
hence representing a notable burden in the healthcare system of New Zealand (Milne, 2012). The
Maori people have been found to get diagnosed with heart failure 10-15 years earlier than the
non-Maori individuals (Wang, 2013). It is estimated that the mortality from heart failure among
Maori males aged 45-64 years is eight times higher than the non-Maori. The Maori with age of
65 years and above also experience heart failure approximately 3 times higher than non-Maori.
Similar cases of high mortality rate are also seen in the Maori females, whereby, there is about 8
to 9 times more hospital admission among the compared than the non-Maori.
Further statistics have indicated that the number of people living with heart disease in New
Zealand is 186,000 which implies one in every 20 adults. Cardiovascular disease also is
responsible for 33% of deaths annually, which makes it the leading cause of death in New
Zealand. It includes; stroke, blood vessels, and stroke disease.
As the population ages, the prevalence of Heart failure keeps on increasing and over the next few
decades the number of people diagnosed with this condition will have gone up by 50%
NORMAL PHYSIOLOGY OF CARDIOVASCULAR SYSTEM
The following diagram illustrates the normal physiology of the cardiovascular system
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
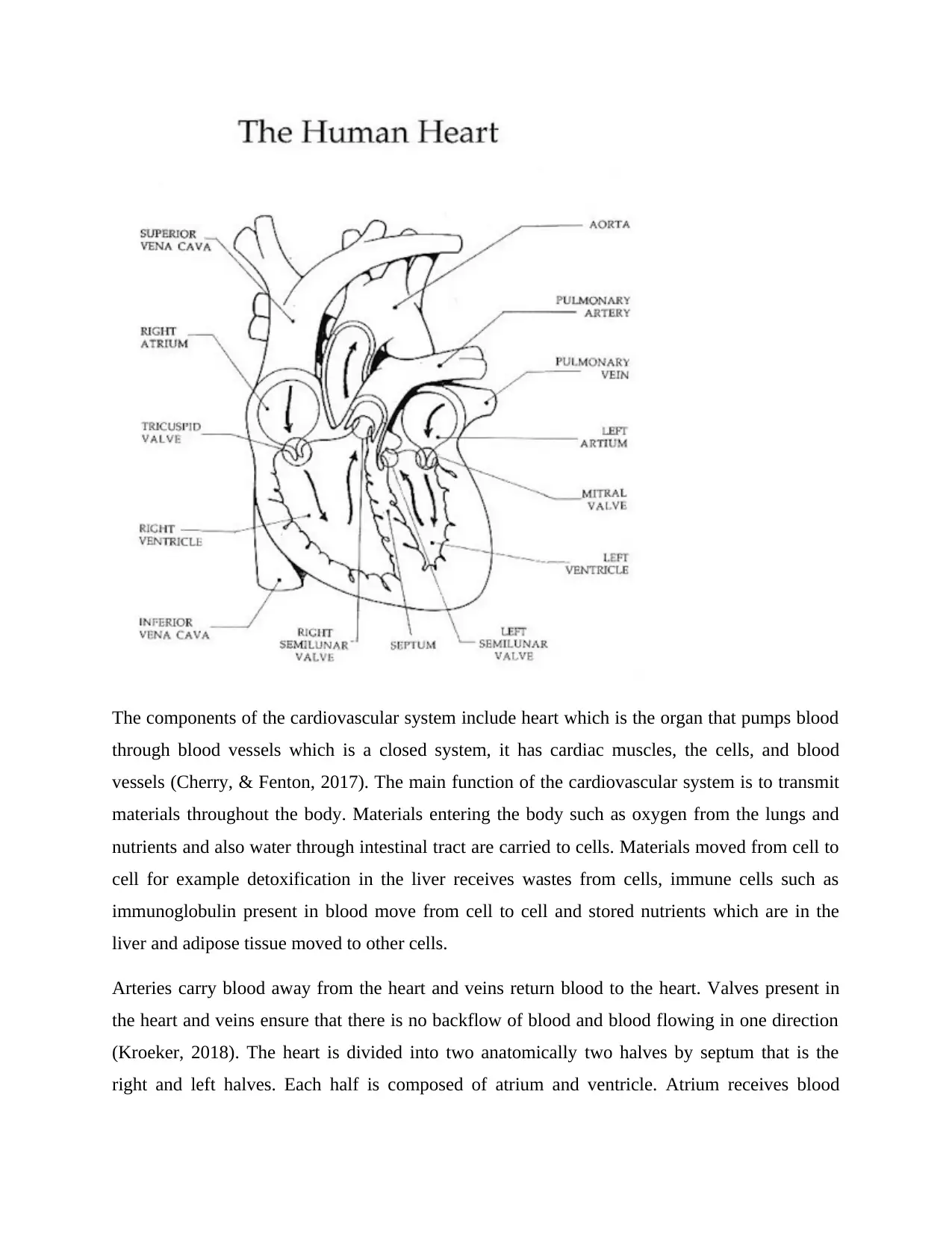
The components of the cardiovascular system include heart which is the organ that pumps blood
through blood vessels which is a closed system, it has cardiac muscles, the cells, and blood
vessels (Cherry, & Fenton, 2017). The main function of the cardiovascular system is to transmit
materials throughout the body. Materials entering the body such as oxygen from the lungs and
nutrients and also water through intestinal tract are carried to cells. Materials moved from cell to
cell for example detoxification in the liver receives wastes from cells, immune cells such as
immunoglobulin present in blood move from cell to cell and stored nutrients which are in the
liver and adipose tissue moved to other cells.
Arteries carry blood away from the heart and veins return blood to the heart. Valves present in
the heart and veins ensure that there is no backflow of blood and blood flowing in one direction
(Kroeker, 2018). The heart is divided into two anatomically two halves by septum that is the
right and left halves. Each half is composed of atrium and ventricle. Atrium receives blood
through blood vessels which is a closed system, it has cardiac muscles, the cells, and blood
vessels (Cherry, & Fenton, 2017). The main function of the cardiovascular system is to transmit
materials throughout the body. Materials entering the body such as oxygen from the lungs and
nutrients and also water through intestinal tract are carried to cells. Materials moved from cell to
cell for example detoxification in the liver receives wastes from cells, immune cells such as
immunoglobulin present in blood move from cell to cell and stored nutrients which are in the
liver and adipose tissue moved to other cells.
Arteries carry blood away from the heart and veins return blood to the heart. Valves present in
the heart and veins ensure that there is no backflow of blood and blood flowing in one direction
(Kroeker, 2018). The heart is divided into two anatomically two halves by septum that is the
right and left halves. Each half is composed of atrium and ventricle. Atrium receives blood
returning to the heart while ventricles pump the blood out into the rest of the body. Atrium and
ventricles also halves which prevent back prevent backflow of blood.
The lungs are responsible for pulmonary circulation which goes from the right side of the heart
and returns it to the left side of the heart with oxygenated blood, oxygen is picked and carbon
dioxide expelled.
The systemic circulation is made up of vessels that go from the left side of the heart to tissues
and back to the right side of the heart. Systemic and pulmonary circulation work together in that
deoxygenated blood returning from the body enters the right atrium of the heart (Stephenson,
Adams, & Vaccarezza, 2017). The blood then passes through the tricuspid valves and enters into
the right ventricle where it is pumped to the lungs. In the lungs it becomes oxygenated in the
lungs, capillaries, it is then carried to the left atrium by the pulmonary veins. Blood passes to the
left ventricle through the bicuspid also called the bicuspid valves where it is pumped into the
aorta through the aortic valves where blood is now pumped to the rest of the body. Aorta
branches into smaller and smaller arteries that the eventually lead to capillary bed of the tissue
where oxygen is exchanged for oxygen and the returned through the veins which join to the main
vena cava which is the inferior vena cava and superior vena cava. Both inferior and superior
vena cava empties into the right atrium. Any changes with occurs to anatomical structures such
as the heart muscles cause abnormal functioning of the cardiovascular system which then
reduces the efficiency of the heart as the heart will be overworked eventually leading to heart
failure (Bristow, et.al 2017).
PATHOPHYSIOLOGY OF HEART FAILURE
The main pathophysiology of heart failure usually manifests through a decrease in the efficiency
of the heart muscle either through work overload or damage (Heusch, et.al, 2014). This can be
caused by caused by a variety of conditions which include; hypertension ( which raises the
contraction force that is required to pump blood), myocardial infarction ( whereby the muscles of
the heart are deprived of oxygen and get necrosed), and amyloidosis ( in which there is
deposition of the misfolded proteins in the heart muscle making it be stiff). With time these
increasing workload will start to produce alteration to the hearing itself.
ventricles also halves which prevent back prevent backflow of blood.
The lungs are responsible for pulmonary circulation which goes from the right side of the heart
and returns it to the left side of the heart with oxygenated blood, oxygen is picked and carbon
dioxide expelled.
The systemic circulation is made up of vessels that go from the left side of the heart to tissues
and back to the right side of the heart. Systemic and pulmonary circulation work together in that
deoxygenated blood returning from the body enters the right atrium of the heart (Stephenson,
Adams, & Vaccarezza, 2017). The blood then passes through the tricuspid valves and enters into
the right ventricle where it is pumped to the lungs. In the lungs it becomes oxygenated in the
lungs, capillaries, it is then carried to the left atrium by the pulmonary veins. Blood passes to the
left ventricle through the bicuspid also called the bicuspid valves where it is pumped into the
aorta through the aortic valves where blood is now pumped to the rest of the body. Aorta
branches into smaller and smaller arteries that the eventually lead to capillary bed of the tissue
where oxygen is exchanged for oxygen and the returned through the veins which join to the main
vena cava which is the inferior vena cava and superior vena cava. Both inferior and superior
vena cava empties into the right atrium. Any changes with occurs to anatomical structures such
as the heart muscles cause abnormal functioning of the cardiovascular system which then
reduces the efficiency of the heart as the heart will be overworked eventually leading to heart
failure (Bristow, et.al 2017).
PATHOPHYSIOLOGY OF HEART FAILURE
The main pathophysiology of heart failure usually manifests through a decrease in the efficiency
of the heart muscle either through work overload or damage (Heusch, et.al, 2014). This can be
caused by caused by a variety of conditions which include; hypertension ( which raises the
contraction force that is required to pump blood), myocardial infarction ( whereby the muscles of
the heart are deprived of oxygen and get necrosed), and amyloidosis ( in which there is
deposition of the misfolded proteins in the heart muscle making it be stiff). With time these
increasing workload will start to produce alteration to the hearing itself.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The ventricle of a person with heart failure gets overloaded hence leading to the lowered force of
contraction. According to the Frank-Staling law of the heart, when there is an increased filling of
the ventricle then the contraction force also increased and hence an increase in the cardiac
output. This mechanism, however, fails in heart failure since the ventricle is loaded with blood
until it reached a point where the efficiency of contraction of the heart muscle is lowered. The
reason behind this is that when the heart muscles get overstretched then the ability to cross-link
actin and myosin filaments is a reduce.
Failure of diastole and/or diastole may result in a reduction of stroke volume. A rise in end
systolic volume is usually caused be lowered contractility while a lowered end-diastolic volume
is caused by an impaired ventricular filling which happens when there is a fall in the compliance
of ventricle, that is, the walls become stiff. The amount of cardiac output can be high whenever
there is an increase in oxygen demand, for example, during exercise. This adds up to the
intolerance often experienced in heart failure. It also to one losing the heart’s ability to work
harder during physical activities that are strenuous and hence becoming to meet the metabolic
demands of the body.
Increased heart rate is a common finding in heart failure and is usually stimulated by increased
sympathetic activity such that adequate cardiac output is maintained (Ponikowski, et.al, 2016).
At first, it is a compensatory mechanism for heart failure but with time, it makes myocardium
strain and hence increasing the coronary perfusion requirements which may result in worsening
of ischemic disease. Abnormal heart rhythms that are fatal may result from a sympathetic
activity. The physical size of the heart's muscular layer may also increase because of the
differentiated heart muscle fibers which increase in an attempt to improve contractility. Stiffness
increase and thus decrease in relaxation during diastole (Craft, et.al, 2015). Ventricles may also
enlarge and adds up to the enlargement and changes in the shape of the heart.
When there is lowered cardiac output, cardiac arrest also usually occurs due to abnormal
ventricular heart rhythm (Kemp, & Conte, 2012). Tissue perfusion is also reduced. This usually
to various physiological compensations including; falling arterial blood pressure, kidney’s ability
to release sodium and water is also reduced, reduced perfusion of skeletal muscle (which causes
atrophy of the muscle fibers)
contraction. According to the Frank-Staling law of the heart, when there is an increased filling of
the ventricle then the contraction force also increased and hence an increase in the cardiac
output. This mechanism, however, fails in heart failure since the ventricle is loaded with blood
until it reached a point where the efficiency of contraction of the heart muscle is lowered. The
reason behind this is that when the heart muscles get overstretched then the ability to cross-link
actin and myosin filaments is a reduce.
Failure of diastole and/or diastole may result in a reduction of stroke volume. A rise in end
systolic volume is usually caused be lowered contractility while a lowered end-diastolic volume
is caused by an impaired ventricular filling which happens when there is a fall in the compliance
of ventricle, that is, the walls become stiff. The amount of cardiac output can be high whenever
there is an increase in oxygen demand, for example, during exercise. This adds up to the
intolerance often experienced in heart failure. It also to one losing the heart’s ability to work
harder during physical activities that are strenuous and hence becoming to meet the metabolic
demands of the body.
Increased heart rate is a common finding in heart failure and is usually stimulated by increased
sympathetic activity such that adequate cardiac output is maintained (Ponikowski, et.al, 2016).
At first, it is a compensatory mechanism for heart failure but with time, it makes myocardium
strain and hence increasing the coronary perfusion requirements which may result in worsening
of ischemic disease. Abnormal heart rhythms that are fatal may result from a sympathetic
activity. The physical size of the heart's muscular layer may also increase because of the
differentiated heart muscle fibers which increase in an attempt to improve contractility. Stiffness
increase and thus decrease in relaxation during diastole (Craft, et.al, 2015). Ventricles may also
enlarge and adds up to the enlargement and changes in the shape of the heart.
When there is lowered cardiac output, cardiac arrest also usually occurs due to abnormal
ventricular heart rhythm (Kemp, & Conte, 2012). Tissue perfusion is also reduced. This usually
to various physiological compensations including; falling arterial blood pressure, kidney’s ability
to release sodium and water is also reduced, reduced perfusion of skeletal muscle (which causes
atrophy of the muscle fibers)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The elevated peripheral resistance and high blood volume increases the strain on the heart and
fasten the damage to the heart. Hydrostatic pressure in the capillaries is increased due to
vasoconstriction and the retention of fluid. This shifts the balance of forces. The interstitial fluid
formation is favored since high pressure moves extra fluid into the tissue from the blood. This
causes edema.
In right-sided heart failure, edema begins in the ankles because gravity leads to high venous
pressure in this part of the body. A bedridden patient, however, may develop edema beginning
with the sacral region. In left-sided heart failure, cardiogenic pulmonary edema develops. This is
where edema occurs in the lungs. This results in shortness of breath, paroxysmal nocturnal
dyspnea, and orthopnea. This is because the lungs stiffen due to reduced capacity hence gas
exchange efficiency is reduced.
CLINICAL MANIFESTATION OF HEART FAILURE
The symptoms of heart failure are majorly determined by the side of the heart which falls (Craft,
et.al, 2015). Blood from the right side is pumped into the systemic circulation while blood from
the left goes into the pulmonary circulation. The initial symptoms of a right-sided failure,
however, show up as a result of pulmonary circulation effects. The ejection fraction is lowered in
systolic dysfunction hence causing abnormally increased blood volume in the left ventricle. The
end-diastolic ventricular pressure, however, will be increased in diastolic dysfunction. This
elevation in volume and pressure affects the left atrium and then to the pulmonary veins thus
altering the normal drainage of alveoli. This also encourages fluid flow to the lung parenchyma
from the capillaries leading to pulmonary edema. This affects the exchange of gases. Failure of
the left side presents with respiratory symptoms like shortness of breath, paroxysmal nocturnal
dyspnea, and orthopnea. The following are a discussion of the signs and symptoms and how they
are linked to the pathophysiology of heart failure.
Shortness of breath
The major symptom of heart failure is shortness of breath which can occur when the patient is
either at rest, with activity, while lying flat, while awakening the person from sleep this is called
paroxysmal nocturnal dyspnea or because of accumulation in the lungs which causes pulmonary
edema. Shortness of breath occurs because the blood in the body accumulates in the blood
fasten the damage to the heart. Hydrostatic pressure in the capillaries is increased due to
vasoconstriction and the retention of fluid. This shifts the balance of forces. The interstitial fluid
formation is favored since high pressure moves extra fluid into the tissue from the blood. This
causes edema.
In right-sided heart failure, edema begins in the ankles because gravity leads to high venous
pressure in this part of the body. A bedridden patient, however, may develop edema beginning
with the sacral region. In left-sided heart failure, cardiogenic pulmonary edema develops. This is
where edema occurs in the lungs. This results in shortness of breath, paroxysmal nocturnal
dyspnea, and orthopnea. This is because the lungs stiffen due to reduced capacity hence gas
exchange efficiency is reduced.
CLINICAL MANIFESTATION OF HEART FAILURE
The symptoms of heart failure are majorly determined by the side of the heart which falls (Craft,
et.al, 2015). Blood from the right side is pumped into the systemic circulation while blood from
the left goes into the pulmonary circulation. The initial symptoms of a right-sided failure,
however, show up as a result of pulmonary circulation effects. The ejection fraction is lowered in
systolic dysfunction hence causing abnormally increased blood volume in the left ventricle. The
end-diastolic ventricular pressure, however, will be increased in diastolic dysfunction. This
elevation in volume and pressure affects the left atrium and then to the pulmonary veins thus
altering the normal drainage of alveoli. This also encourages fluid flow to the lung parenchyma
from the capillaries leading to pulmonary edema. This affects the exchange of gases. Failure of
the left side presents with respiratory symptoms like shortness of breath, paroxysmal nocturnal
dyspnea, and orthopnea. The following are a discussion of the signs and symptoms and how they
are linked to the pathophysiology of heart failure.
Shortness of breath
The major symptom of heart failure is shortness of breath which can occur when the patient is
either at rest, with activity, while lying flat, while awakening the person from sleep this is called
paroxysmal nocturnal dyspnea or because of accumulation in the lungs which causes pulmonary
edema. Shortness of breath occurs because the blood in the body accumulates in the blood
vessels, which then returns blood from the lungs to the heart because the heart is unable to pump
blood out of them effectively. Therefore, this causes fluid to leak into the lungs causing
congestion which in turn causes shortness of breath.
Chest pain
It is chest pain or discomfort that last more than 15 minutes. It is also called angina, it is usually
felt in the chest but sometimes it is felt in the upper abdomen, the shoulders, arms and radiate to
the back. It mainly occurs when the patient has coronary heart disease. This is when there is right
heart failure, left side failure or even both. It is explained as a discomfort, heaviness, aching or
squeezing feeling in the chest. It is caused when the heart doesn’t get enough oxygen-rich blood.
It is and a sign of heart attack that’s why it should be treated as a serious symptom.
Cyanosis
It is the bluish discoloration of the peripheral part of the body such as lips, fingers, and the toes
that are caused by low oxygen level supplied to the tissues. The affected part of the body feels
cold on touch and the color can return to normal after warming. It occurs due to stagnation of
blood in the venous system and also due to severe congestion in the lungs causing imperfect
oxygenation of blood.
Pulsus alternans
They are regular pulses with alternating weak and strong amplitude happening due to atrial
fibrillation in the right-sided failure or combination of left-sided heart failure and right-sided
heart failure
Pulmonary edema
It is the buildup of fluid in the lungs that lead to shortness of breath. It occurs when the heart is
unable to pump blood efficiently and this causes veins to accumulate blood and it takes them to
the lungs. The fluid is then pushed to air spaces in the lungs. This fluid reduces the surface area
for oxygen conduction which causes shortness of breath
Cough
blood out of them effectively. Therefore, this causes fluid to leak into the lungs causing
congestion which in turn causes shortness of breath.
Chest pain
It is chest pain or discomfort that last more than 15 minutes. It is also called angina, it is usually
felt in the chest but sometimes it is felt in the upper abdomen, the shoulders, arms and radiate to
the back. It mainly occurs when the patient has coronary heart disease. This is when there is right
heart failure, left side failure or even both. It is explained as a discomfort, heaviness, aching or
squeezing feeling in the chest. It is caused when the heart doesn’t get enough oxygen-rich blood.
It is and a sign of heart attack that’s why it should be treated as a serious symptom.
Cyanosis
It is the bluish discoloration of the peripheral part of the body such as lips, fingers, and the toes
that are caused by low oxygen level supplied to the tissues. The affected part of the body feels
cold on touch and the color can return to normal after warming. It occurs due to stagnation of
blood in the venous system and also due to severe congestion in the lungs causing imperfect
oxygenation of blood.
Pulsus alternans
They are regular pulses with alternating weak and strong amplitude happening due to atrial
fibrillation in the right-sided failure or combination of left-sided heart failure and right-sided
heart failure
Pulmonary edema
It is the buildup of fluid in the lungs that lead to shortness of breath. It occurs when the heart is
unable to pump blood efficiently and this causes veins to accumulate blood and it takes them to
the lungs. The fluid is then pushed to air spaces in the lungs. This fluid reduces the surface area
for oxygen conduction which causes shortness of breath
Cough
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
In patients with heart failure they cough persistently in an attempt to eliminate the excess fluid,
this is because the heart contracts less than it should be. Coughing allows fluid that has
accumulated in the lungs to be eliminated. Cough is usually accompanied by shortness of breath
and exercise intolerance. Once a heart failure has been identified and it has been treated cough
should disappear.
Loss of appetite
Many symptoms of heart failure such as shortness of breath, fatigue, and nausea make it hard for
patients with heart failure to take enough food and nutrients causing muscle wasting and weight
loss.
Excess urination
Due to the weak heart which is unable to pump blood efficiently, leading to fluid accumulation
in the body causing kidneys to work to get rid of excess fluids causing a large amount of urine to
be produced thus causing frequent urination.
Dizziness
This is a feeling that makes someone be light-headed, feeling to faint mainly occurring due to a
reduction of blood flow to the brain due to a weak heart which is unable to pump blood forcibly.
This symptom may cause sudden loss of consciousness which is an indicator that blood to the
brain is seriously reduced. Dizziness is a major side effect of the drugs used to treat heart failure.
Fatigue
This is a feeling of being overtired with low energy and a strong feeling to sleep.it mainly
interferes with normal daily activities. It occurs due to the inability of the heart to supply enough
oxygen to the tissues and it can also be as a result of side effects of medications used to treat
heart failure.
Diagnostic test and assessments and rationale
1) x-ray images. A chest x-ray is important as it helps the doctor see the condition of the heart
and lungs if there is abnormality such as narrowed arteries or edema in the lungs. Through x-ray
this is because the heart contracts less than it should be. Coughing allows fluid that has
accumulated in the lungs to be eliminated. Cough is usually accompanied by shortness of breath
and exercise intolerance. Once a heart failure has been identified and it has been treated cough
should disappear.
Loss of appetite
Many symptoms of heart failure such as shortness of breath, fatigue, and nausea make it hard for
patients with heart failure to take enough food and nutrients causing muscle wasting and weight
loss.
Excess urination
Due to the weak heart which is unable to pump blood efficiently, leading to fluid accumulation
in the body causing kidneys to work to get rid of excess fluids causing a large amount of urine to
be produced thus causing frequent urination.
Dizziness
This is a feeling that makes someone be light-headed, feeling to faint mainly occurring due to a
reduction of blood flow to the brain due to a weak heart which is unable to pump blood forcibly.
This symptom may cause sudden loss of consciousness which is an indicator that blood to the
brain is seriously reduced. Dizziness is a major side effect of the drugs used to treat heart failure.
Fatigue
This is a feeling of being overtired with low energy and a strong feeling to sleep.it mainly
interferes with normal daily activities. It occurs due to the inability of the heart to supply enough
oxygen to the tissues and it can also be as a result of side effects of medications used to treat
heart failure.
Diagnostic test and assessments and rationale
1) x-ray images. A chest x-ray is important as it helps the doctor see the condition of the heart
and lungs if there is abnormality such as narrowed arteries or edema in the lungs. Through x-ray
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
other conditions other than heart may be identified which may explain signs and symptoms
presented for example dyspnea due to myocardial infarction.
2) Electrocardiogram (ECG). This is a test that helps trace the electrical activity of the heart
using electrodes that are attached to the skin. It helps the doctor diagnose the heart rhythm is it is
regular or irregular through this damage that has occurred in the heart will be identified and
treated appropriately.
3) Blood test. The blood sample is taken for any disease that may affect the heart. For example,
some infection can cause damage to heart muscles causing heart failure. Some bacterial such
streptococcus B causes acute rheumatic fever which eventually causes heart failure as it causes
damage of heart valves which prevent backflow of blood and muscle which enables contraction
for pumping of blood to body organs. If the diagnosis is not identifiable and yet there are systems
of heart failure, a chemical called N- terminal pro-B-type natriuretic peptide can be checked for
any abnormality.
4) Echocardiogram. This diagnostic method uses sound waves to produce a video image of how
the heart works. It helps doctors see the anatomical size and shape of the heart or any present
abnormality. In case the heart size is bigger than normal it shows signs of heart failure. It also
measures the ejection fraction that flows to the body system, it helps measure how well the heart
pumping activity is okay, it is used to classify heart failure and also gives a guide of how the
treatment should be given to patients.
5) Stress test. It measures the health of the heart by how it responds to the strain. This is done by
instructing the patient to work for a specified distance while still attached to an ECG machine or
an alternative is to give the patient a drug that stimulates heart just same as exercise could have
done. It can also be done by wearing a mask that measures the ability of the heart and lungs to
take oxygen and give out carbon dioxide and be compared to a normal level.
6) Cardiac computerized tomography. It helps visualize the heart and collect images of the heart
and the chest. In this technique the patient should lie in a table inside a doughnut-shaped
machine, there is an x-ray tube inside the machine which rotates around the body of the patient
and it is able to collect images and any abnormality will be detected.
presented for example dyspnea due to myocardial infarction.
2) Electrocardiogram (ECG). This is a test that helps trace the electrical activity of the heart
using electrodes that are attached to the skin. It helps the doctor diagnose the heart rhythm is it is
regular or irregular through this damage that has occurred in the heart will be identified and
treated appropriately.
3) Blood test. The blood sample is taken for any disease that may affect the heart. For example,
some infection can cause damage to heart muscles causing heart failure. Some bacterial such
streptococcus B causes acute rheumatic fever which eventually causes heart failure as it causes
damage of heart valves which prevent backflow of blood and muscle which enables contraction
for pumping of blood to body organs. If the diagnosis is not identifiable and yet there are systems
of heart failure, a chemical called N- terminal pro-B-type natriuretic peptide can be checked for
any abnormality.
4) Echocardiogram. This diagnostic method uses sound waves to produce a video image of how
the heart works. It helps doctors see the anatomical size and shape of the heart or any present
abnormality. In case the heart size is bigger than normal it shows signs of heart failure. It also
measures the ejection fraction that flows to the body system, it helps measure how well the heart
pumping activity is okay, it is used to classify heart failure and also gives a guide of how the
treatment should be given to patients.
5) Stress test. It measures the health of the heart by how it responds to the strain. This is done by
instructing the patient to work for a specified distance while still attached to an ECG machine or
an alternative is to give the patient a drug that stimulates heart just same as exercise could have
done. It can also be done by wearing a mask that measures the ability of the heart and lungs to
take oxygen and give out carbon dioxide and be compared to a normal level.
6) Cardiac computerized tomography. It helps visualize the heart and collect images of the heart
and the chest. In this technique the patient should lie in a table inside a doughnut-shaped
machine, there is an x-ray tube inside the machine which rotates around the body of the patient
and it is able to collect images and any abnormality will be detected.
7) Magnetic resonance imaging. In this procedure, the patient lies on a table inside a long tube
machine that produces a magnetic field which helps in visualizing body tissues by aligning
atomic particles in some cells. Radio waves are broadcasted towards the aligned atomic particles
which produce signals that that create images of the heart.
8) Coronary Angiogram. This procedure enables doctors to spots blockages in arteries. A thin
flexible catheter with dye injected is inserted into the blood vessel at the position of arm or groin
and it is guided through the aorta into the coronary arteries. Dye injected through the catheter
makes visible the heart on x-ray.
PREVENTION AND MANAGEMENT OF HEART FAILURE
I) Prevention
Lifestyle changes
Health lifestyle reduces the risk of heart failure. Keeping a healthy weight that is proportional to
body surface area is important, avoiding smoking, engaging in exercise and healthy diet which
includes consumption of breakfast cereal and plenty of fruit and vegetable intake are the main
health lifestyle changes that need to be adhered to. Regular physical activity and also
maintaining a healthy body weight are important factors in preventing heart failure. Low
consumption of alcohol and cocaine abuse. Drinking a moderate amount of coffee and eating fish
lowers the risk of heart failure.
Treatment of risk factors
Type 2 diabetes is associated with the development of heart failure and thus treatment of diabetes
lowers blood sugar together with a lot of exercises, diet management and use of ant diabetic
medications. Cholesterol causes atherosclerosis of coronary arteries that can result to heart
attacks, lowering level of cholesterol by given medications such as statin and aspirin and
reducing it in the diet reduces cholesterol level thus reduced risk of heart failure (Ponikowski,
et.al, 2014). Treatment of hypertension reduces risk of heart failure, use of medicines such as
diuretics and angiotensin-converting enzyme inhibitors helps in lowering blood pressure and
eventually reduce heart failure risk.
Education/public awareness
machine that produces a magnetic field which helps in visualizing body tissues by aligning
atomic particles in some cells. Radio waves are broadcasted towards the aligned atomic particles
which produce signals that that create images of the heart.
8) Coronary Angiogram. This procedure enables doctors to spots blockages in arteries. A thin
flexible catheter with dye injected is inserted into the blood vessel at the position of arm or groin
and it is guided through the aorta into the coronary arteries. Dye injected through the catheter
makes visible the heart on x-ray.
PREVENTION AND MANAGEMENT OF HEART FAILURE
I) Prevention
Lifestyle changes
Health lifestyle reduces the risk of heart failure. Keeping a healthy weight that is proportional to
body surface area is important, avoiding smoking, engaging in exercise and healthy diet which
includes consumption of breakfast cereal and plenty of fruit and vegetable intake are the main
health lifestyle changes that need to be adhered to. Regular physical activity and also
maintaining a healthy body weight are important factors in preventing heart failure. Low
consumption of alcohol and cocaine abuse. Drinking a moderate amount of coffee and eating fish
lowers the risk of heart failure.
Treatment of risk factors
Type 2 diabetes is associated with the development of heart failure and thus treatment of diabetes
lowers blood sugar together with a lot of exercises, diet management and use of ant diabetic
medications. Cholesterol causes atherosclerosis of coronary arteries that can result to heart
attacks, lowering level of cholesterol by given medications such as statin and aspirin and
reducing it in the diet reduces cholesterol level thus reduced risk of heart failure (Ponikowski,
et.al, 2014). Treatment of hypertension reduces risk of heart failure, use of medicines such as
diuretics and angiotensin-converting enzyme inhibitors helps in lowering blood pressure and
eventually reduce heart failure risk.
Education/public awareness
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




