University Report: Chronic Kidney Failure Pathophysiology Analysis
VerifiedAdded on 2022/10/12
|11
|3011
|335
Report
AI Summary
This report provides a comprehensive analysis of the pathophysiology of chronic kidney failure, examining the structure and function of the renal system, the causes and risk factors of the disease, and the differences between acute and chronic kidney failure. It delves into the case study of a patient, detailing the patient's symptoms, diagnosis, and treatment, including hemodialysis and medications like valsartan and Eprex. The report explores the role of GFR and hemoglobin tests in assessing kidney function and anemia. It also discusses the nurse's responsibilities in medication administration, patient education using the teach-back method, and fluid management. The report highlights the importance of understanding the disease process and its impact on the patient's health and well-being, emphasizing the need for effective communication and patient-centered care.

Running head: PATHOPHYSIOLOGY
PATHOPHYSIOLOGY
Name of the Student
Name of the University
Author note
PATHOPHYSIOLOGY
Name of the Student
Name of the University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PATHOPHYSIOLOGY
Table of Contents
Part 1................................................................................................................................................2
Part 2................................................................................................................................................6
Part 3................................................................................................................................................8
References........................................................................................................................................9
Table of Contents
Part 1................................................................................................................................................2
Part 2................................................................................................................................................6
Part 3................................................................................................................................................8
References........................................................................................................................................9
2PATHOPHYSIOLOGY
Part 1
1.1 The human excretory system comprise of two kidneys, two ureters, one urinary bladder and
one urethra. The primary organ of the renal system are the two kidneys. The three main internal
region of kidney are renal cortex, renal medulla and renal pelvis. The cortex is the outer region
of the kidney and the medulla is the innermost region of kidney. The connection of the kidney to
the circulatory system is done by the renal pelvis. The nephron is the basic structural and
functional unit of the kidney which is responsible for filtering blood to do the regulation of the
chemical concentrations and in producing urine (Glassock & Rule, 2016).
The renal physiology refers to the study of the physiology of kidney involving all the
functions of the kidney. The main functions of kidney includes maintaining the balance of acid
an bases, regulating the balance of fluid. It is also involved in the regulation of sodium,
potassium and other electrolytes. The kidneys are also responsible for clearing toxins, absorption
of glucose, amino acids and other small molecules, regulation of blood pressure, the production
of various hormones and also in the activation of vitamin D. Much of the renal physiology are
studied at the nephron level (Klatte et al., 2015).
1.2. Chronic kidney failure or the end stage renal disease is a rapid and irreversible deterioration
of the function of kidneys. At this condition, the ability of the human body to maintain the
metabolic activity and balance of fluids and the electrolyte fails which results in development of
uremia. Uremia means increase of urea and nitrogenous wastes in the blood. This condition
happens as a result of the systematic effect of different diseases like diabetes mellitus,
hypertension, and obstruction of the urinary tract, different infections or medications. The effect
of the environment and the occupation leads to the occurrence of this disease (Ter Maaten et
Part 1
1.1 The human excretory system comprise of two kidneys, two ureters, one urinary bladder and
one urethra. The primary organ of the renal system are the two kidneys. The three main internal
region of kidney are renal cortex, renal medulla and renal pelvis. The cortex is the outer region
of the kidney and the medulla is the innermost region of kidney. The connection of the kidney to
the circulatory system is done by the renal pelvis. The nephron is the basic structural and
functional unit of the kidney which is responsible for filtering blood to do the regulation of the
chemical concentrations and in producing urine (Glassock & Rule, 2016).
The renal physiology refers to the study of the physiology of kidney involving all the
functions of the kidney. The main functions of kidney includes maintaining the balance of acid
an bases, regulating the balance of fluid. It is also involved in the regulation of sodium,
potassium and other electrolytes. The kidneys are also responsible for clearing toxins, absorption
of glucose, amino acids and other small molecules, regulation of blood pressure, the production
of various hormones and also in the activation of vitamin D. Much of the renal physiology are
studied at the nephron level (Klatte et al., 2015).
1.2. Chronic kidney failure or the end stage renal disease is a rapid and irreversible deterioration
of the function of kidneys. At this condition, the ability of the human body to maintain the
metabolic activity and balance of fluids and the electrolyte fails which results in development of
uremia. Uremia means increase of urea and nitrogenous wastes in the blood. This condition
happens as a result of the systematic effect of different diseases like diabetes mellitus,
hypertension, and obstruction of the urinary tract, different infections or medications. The effect
of the environment and the occupation leads to the occurrence of this disease (Ter Maaten et
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3PATHOPHYSIOLOGY
al.,2015). In the given case, though the patient was not diagnosed with hypertension but the
history is showing that the she had suffered from severe headaches, palpitations since the last
five years as she was very much worried about the drought. At the time of admission in the
hospital the blood pressure of the patient was found to have increased a lot, it was 190/110 mm
Hg. The pathophysiology behind this is that, with the declining of the functions of renal organs,
the end products of the metabolism of proteins gets accumulated in the body, which are normally
excreted out through the urine. Uremia develops and because of this most of the other systems of
the body are affected. The more the waste products are accumulated, the more severe the
symptoms become (Bernal et al, 2015). The rate of the decline of the functions of kidney and the
development of chronic urinary disorders are related to the excretion of proteins and
hypertension. The condition gets more complex if the amount of the protein increases and also if
the hypertension increases. In the blood report of the patient of the case study it is found that the
amount of creatinine is very high and also the patient was having hypertension.
\ There are different risk factors of the disease chronic kidney failure. The genetics of the
patients is one of the risk factor of this disease and it is very essential to find whether the family
members of the patient had suffered from kidney failure or not. Age is another important factor
as most of the people who are above 45 years of age have tendencies to suffer from kidney
failures. The other risk factor of kidney disease is diabetes mellitus, and especially if the onset of
diabetes happen before age 20 it may take severe form during the later stage of their life. High
blood pressure is another risk factor, especially if the pressure is uncontrollable for a long period
of time. Smoking, poor blood glucose control and obesity are the other factors of the kidney
failure. In the given case study, the age factor, hypertension and high blood pressure are the risk
al.,2015). In the given case, though the patient was not diagnosed with hypertension but the
history is showing that the she had suffered from severe headaches, palpitations since the last
five years as she was very much worried about the drought. At the time of admission in the
hospital the blood pressure of the patient was found to have increased a lot, it was 190/110 mm
Hg. The pathophysiology behind this is that, with the declining of the functions of renal organs,
the end products of the metabolism of proteins gets accumulated in the body, which are normally
excreted out through the urine. Uremia develops and because of this most of the other systems of
the body are affected. The more the waste products are accumulated, the more severe the
symptoms become (Bernal et al, 2015). The rate of the decline of the functions of kidney and the
development of chronic urinary disorders are related to the excretion of proteins and
hypertension. The condition gets more complex if the amount of the protein increases and also if
the hypertension increases. In the blood report of the patient of the case study it is found that the
amount of creatinine is very high and also the patient was having hypertension.
\ There are different risk factors of the disease chronic kidney failure. The genetics of the
patients is one of the risk factor of this disease and it is very essential to find whether the family
members of the patient had suffered from kidney failure or not. Age is another important factor
as most of the people who are above 45 years of age have tendencies to suffer from kidney
failures. The other risk factor of kidney disease is diabetes mellitus, and especially if the onset of
diabetes happen before age 20 it may take severe form during the later stage of their life. High
blood pressure is another risk factor, especially if the pressure is uncontrollable for a long period
of time. Smoking, poor blood glucose control and obesity are the other factors of the kidney
failure. In the given case study, the age factor, hypertension and high blood pressure are the risk
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4PATHOPHYSIOLOGY
factors. The patient is 55 years of age, showed symptoms of palpitation and the blood pressure
was also very high.
The complications of the disease involves anemia, bone disease, high potassium levels,
development of heart diseases and fluid increase. The kidney help in creating the blood cells, so
if the kidney fails anemia will happen. When the kidneys are not working properly, the other
organs will also be affected. The consumption of potassium needs to be reduced as the kidney is
not able to filter extra potassium. The healthy fluids can filter and remove the extra fluids from
the body but when the kidneys are not working properly, it will not be able to excrete the extra
fluids from the body (Venkatachalam et al., 2015).
There are only two types of treatment options of kidney failures which are hemodialysis
or peritoneal dialysis. Apart from this the other option left is kidney transplantation. In the
present case scenario, the patient had undergone hemodialysis.
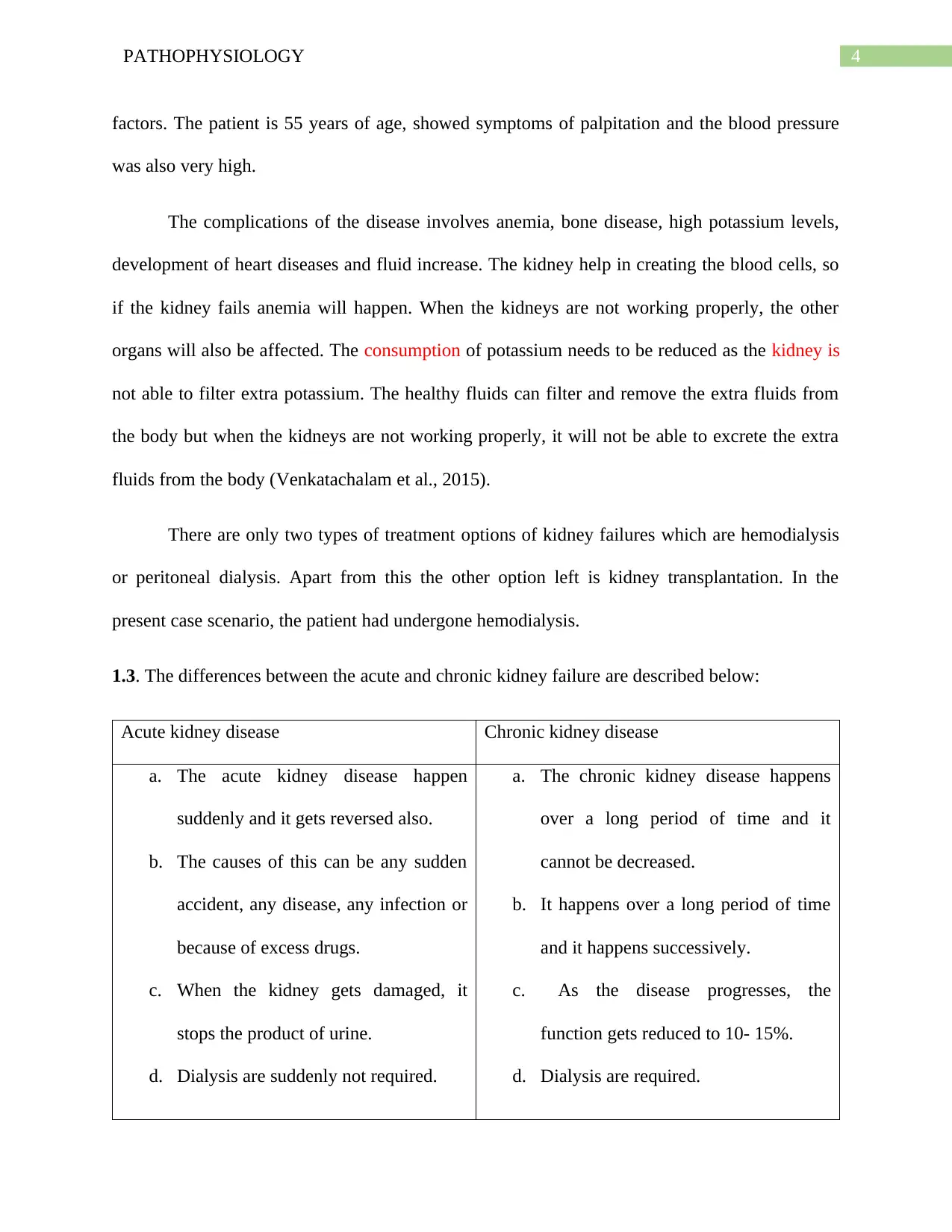
1.3. The differences between the acute and chronic kidney failure are described below:
Acute kidney disease Chronic kidney disease
a. The acute kidney disease happen
suddenly and it gets reversed also.
b. The causes of this can be any sudden
accident, any disease, any infection or
because of excess drugs.
c. When the kidney gets damaged, it
stops the product of urine.
d. Dialysis are suddenly not required.
a. The chronic kidney disease happens
over a long period of time and it
cannot be decreased.
b. It happens over a long period of time
and it happens successively.
c. As the disease progresses, the
function gets reduced to 10- 15%.
d. Dialysis are required.
factors. The patient is 55 years of age, showed symptoms of palpitation and the blood pressure
was also very high.
The complications of the disease involves anemia, bone disease, high potassium levels,
development of heart diseases and fluid increase. The kidney help in creating the blood cells, so
if the kidney fails anemia will happen. When the kidneys are not working properly, the other
organs will also be affected. The consumption of potassium needs to be reduced as the kidney is
not able to filter extra potassium. The healthy fluids can filter and remove the extra fluids from
the body but when the kidneys are not working properly, it will not be able to excrete the extra
fluids from the body (Venkatachalam et al., 2015).
There are only two types of treatment options of kidney failures which are hemodialysis
or peritoneal dialysis. Apart from this the other option left is kidney transplantation. In the
present case scenario, the patient had undergone hemodialysis.
1.3. The differences between the acute and chronic kidney failure are described below:
Acute kidney disease Chronic kidney disease
a. The acute kidney disease happen
suddenly and it gets reversed also.
b. The causes of this can be any sudden
accident, any disease, any infection or
because of excess drugs.
c. When the kidney gets damaged, it
stops the product of urine.
d. Dialysis are suddenly not required.
a. The chronic kidney disease happens
over a long period of time and it
cannot be decreased.
b. It happens over a long period of time
and it happens successively.
c. As the disease progresses, the
function gets reduced to 10- 15%.
d. Dialysis are required.
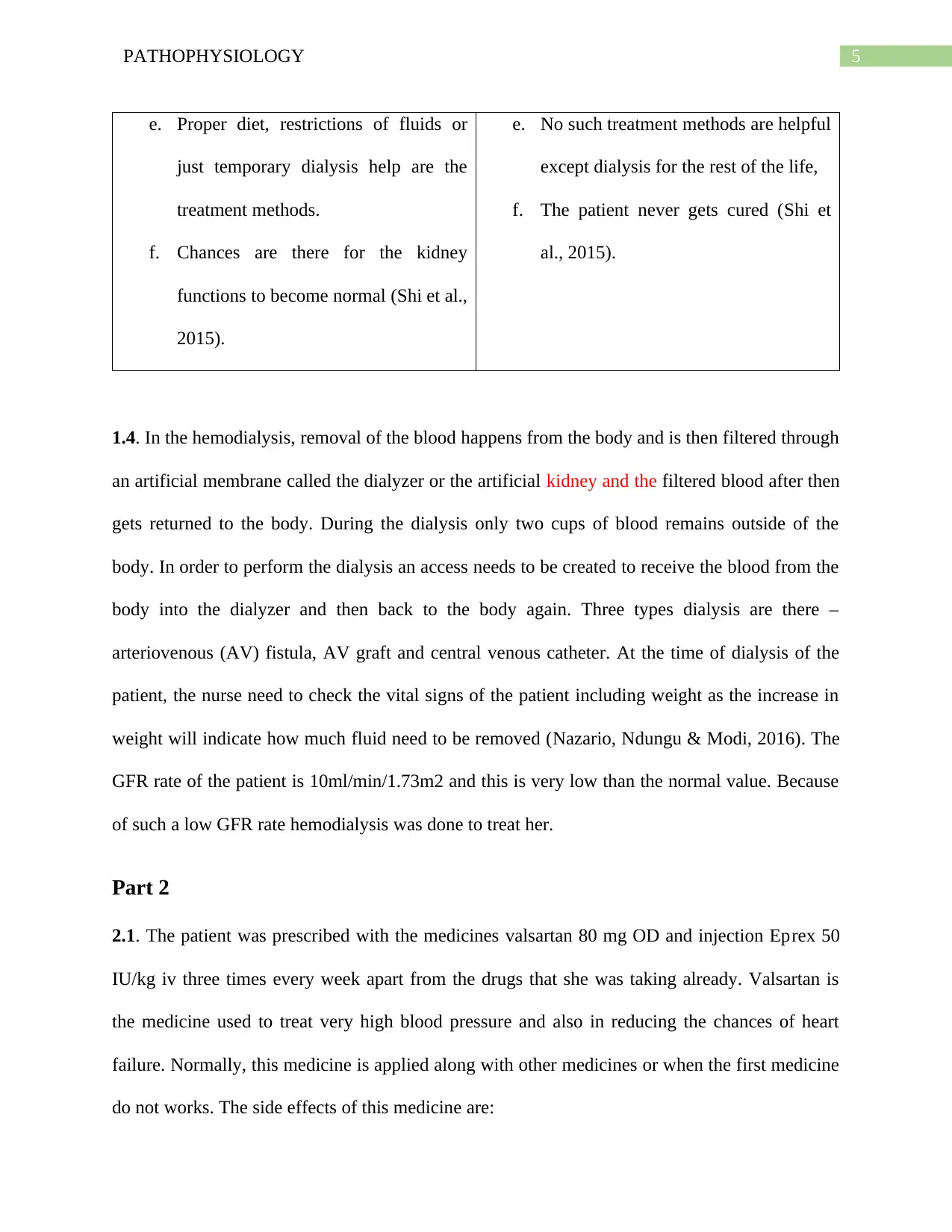
5PATHOPHYSIOLOGY
e. Proper diet, restrictions of fluids or
just temporary dialysis help are the
treatment methods.
f. Chances are there for the kidney
functions to become normal (Shi et al.,
2015).
e. No such treatment methods are helpful
except dialysis for the rest of the life,
f. The patient never gets cured (Shi et
al., 2015).
1.4. In the hemodialysis, removal of the blood happens from the body and is then filtered through
an artificial membrane called the dialyzer or the artificial kidney and the filtered blood after then
gets returned to the body. During the dialysis only two cups of blood remains outside of the
body. In order to perform the dialysis an access needs to be created to receive the blood from the
body into the dialyzer and then back to the body again. Three types dialysis are there –
arteriovenous (AV) fistula, AV graft and central venous catheter. At the time of dialysis of the
patient, the nurse need to check the vital signs of the patient including weight as the increase in
weight will indicate how much fluid need to be removed (Nazario, Ndungu & Modi, 2016). The
GFR rate of the patient is 10ml/min/1.73m2 and this is very low than the normal value. Because
of such a low GFR rate hemodialysis was done to treat her.
Part 2
2.1. The patient was prescribed with the medicines valsartan 80 mg OD and injection Eprex 50
IU/kg iv three times every week apart from the drugs that she was taking already. Valsartan is
the medicine used to treat very high blood pressure and also in reducing the chances of heart
failure. Normally, this medicine is applied along with other medicines or when the first medicine
do not works. The side effects of this medicine are:
e. Proper diet, restrictions of fluids or
just temporary dialysis help are the
treatment methods.
f. Chances are there for the kidney
functions to become normal (Shi et al.,
2015).
e. No such treatment methods are helpful
except dialysis for the rest of the life,
f. The patient never gets cured (Shi et
al., 2015).
1.4. In the hemodialysis, removal of the blood happens from the body and is then filtered through
an artificial membrane called the dialyzer or the artificial kidney and the filtered blood after then
gets returned to the body. During the dialysis only two cups of blood remains outside of the
body. In order to perform the dialysis an access needs to be created to receive the blood from the
body into the dialyzer and then back to the body again. Three types dialysis are there –
arteriovenous (AV) fistula, AV graft and central venous catheter. At the time of dialysis of the
patient, the nurse need to check the vital signs of the patient including weight as the increase in
weight will indicate how much fluid need to be removed (Nazario, Ndungu & Modi, 2016). The
GFR rate of the patient is 10ml/min/1.73m2 and this is very low than the normal value. Because
of such a low GFR rate hemodialysis was done to treat her.
Part 2
2.1. The patient was prescribed with the medicines valsartan 80 mg OD and injection Eprex 50
IU/kg iv three times every week apart from the drugs that she was taking already. Valsartan is
the medicine used to treat very high blood pressure and also in reducing the chances of heart
failure. Normally, this medicine is applied along with other medicines or when the first medicine
do not works. The side effects of this medicine are:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6PATHOPHYSIOLOGY
Common side effects – The common side effects of this medicine are feeling dizzy or
having the sensations of spinning. Headaches and sudden feeling of sickness are other
side effects. The patient may suffer from vomiting or diarrhea or excess pain in the joints.
Serious side effects- Sudden yellowing of the skin or the eyes have also turned yellow.
These are the symptoms of serious problems of liver. The other serious side effects
includes paling of skin, feeling tired frequently, spots of purple color, any kind of
bleeding, sore throat or sudden fever. The side effects also includes, irregular heartbeat
and muscle cramp (Ragab et al., 2017).
The nurse must consider the facts that the patient was already taking ibuprofen, so this aspect
must be considered. The nurse have to consider the age of the patient and after that the medicine
should be administered. The third important factor was that the dose must be applied after
carefully analyzing the blood pressure of the patient. The fourth factor was that the nurse must
consider that whether the medicine does not increase the headache of the patient as she already
suffers from headache.
The next medicine injection Eprex 50 IU/kg iv is prescribed to patients in order to treat
anemia associated with the chronic renal failure. This medicine is applied to the patient a she is
unable to produce sufficient erythropoietin. Apart from this, this medicine is also applied to the
patients who are suffering from cancer. The side effect of this medicine are described below;
Common side effects- The common side effects involve feeling of tiredness or feeling of
weakness. It also includes pain, stinging, redness and swelling around the site of the
infection.
Serious side effects- The serious side effects includes clotting of the vascular access site
because of dialysis. Diarrhea is another side effect, edema of face, fingers, feet and lower
Common side effects – The common side effects of this medicine are feeling dizzy or
having the sensations of spinning. Headaches and sudden feeling of sickness are other
side effects. The patient may suffer from vomiting or diarrhea or excess pain in the joints.
Serious side effects- Sudden yellowing of the skin or the eyes have also turned yellow.
These are the symptoms of serious problems of liver. The other serious side effects
includes paling of skin, feeling tired frequently, spots of purple color, any kind of
bleeding, sore throat or sudden fever. The side effects also includes, irregular heartbeat
and muscle cramp (Ragab et al., 2017).
The nurse must consider the facts that the patient was already taking ibuprofen, so this aspect
must be considered. The nurse have to consider the age of the patient and after that the medicine
should be administered. The third important factor was that the dose must be applied after
carefully analyzing the blood pressure of the patient. The fourth factor was that the nurse must
consider that whether the medicine does not increase the headache of the patient as she already
suffers from headache.
The next medicine injection Eprex 50 IU/kg iv is prescribed to patients in order to treat
anemia associated with the chronic renal failure. This medicine is applied to the patient a she is
unable to produce sufficient erythropoietin. Apart from this, this medicine is also applied to the
patients who are suffering from cancer. The side effect of this medicine are described below;
Common side effects- The common side effects involve feeling of tiredness or feeling of
weakness. It also includes pain, stinging, redness and swelling around the site of the
infection.
Serious side effects- The serious side effects includes clotting of the vascular access site
because of dialysis. Diarrhea is another side effect, edema of face, fingers, feet and lower
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PATHOPHYSIOLOGY
legs. Flu-like symptoms may occur, the headaches may get increased, and blood pressure
can get increased. The patient of the case study might suffer from all these symptoms.
The patient might consult with doctor if chest pain, allergy or stroke happens (Dhayef,
Manuti & Abutabiekh, 2017).
In the given case study, the nurse should consider the vital conditions of the patient
before applying the injection. Secondly, the nurse must make sure that the condition of heart
was good or not as she suffered from hypertension. Thirdly, the high blood pressure of the
patient must be considered. Finally, the other medicines of the patients must be considered.
2.2. The glomerular filtration rate provides the doctor the clear indication of the extent of the
damage of the kidney and also in determining the stage of the kidney disease. This can be
done by looking after the changes in the GFR over a specified period of time. The test
defines the sum of the filtration rates of all the nephrons functioning together (Sharma et al.,
2016). The calculation is done by the formula = 140 – (age of the patient). The normal value
of this disease is 100-140 mls/min. In the given case study, the value of the patient is 10
ml/min. This shows that the patient was having severe kidney disease.
The hemoglobin test is done to measure the amount of oxygen in the blood. This also
gives people information about the overall health of the person, for diagnosing a medical
condition and to monitor a particular medical functions (Saliba et al, 2015). For doing this
test, a person can eat or drink before the test is done (Gore & McGuire, 2016). The normal
value for this test is12 to 15.5 gms/dl and the patient had 95 gms/L which means 9.5
gms/deciliter. The patient was suffering from anemia.
legs. Flu-like symptoms may occur, the headaches may get increased, and blood pressure
can get increased. The patient of the case study might suffer from all these symptoms.
The patient might consult with doctor if chest pain, allergy or stroke happens (Dhayef,
Manuti & Abutabiekh, 2017).
In the given case study, the nurse should consider the vital conditions of the patient
before applying the injection. Secondly, the nurse must make sure that the condition of heart
was good or not as she suffered from hypertension. Thirdly, the high blood pressure of the
patient must be considered. Finally, the other medicines of the patients must be considered.
2.2. The glomerular filtration rate provides the doctor the clear indication of the extent of the
damage of the kidney and also in determining the stage of the kidney disease. This can be
done by looking after the changes in the GFR over a specified period of time. The test
defines the sum of the filtration rates of all the nephrons functioning together (Sharma et al.,
2016). The calculation is done by the formula = 140 – (age of the patient). The normal value
of this disease is 100-140 mls/min. In the given case study, the value of the patient is 10
ml/min. This shows that the patient was having severe kidney disease.
The hemoglobin test is done to measure the amount of oxygen in the blood. This also
gives people information about the overall health of the person, for diagnosing a medical
condition and to monitor a particular medical functions (Saliba et al, 2015). For doing this
test, a person can eat or drink before the test is done (Gore & McGuire, 2016). The normal
value for this test is12 to 15.5 gms/dl and the patient had 95 gms/L which means 9.5
gms/deciliter. The patient was suffering from anemia.
8PATHOPHYSIOLOGY
Part 3
The teach-back method is communication confirmation method which are used by the
healthcare providers in order to confirm that the patients have understood or not everything that
have been explained to them. If the patient is able to understand then the teach-back method is
effective and accurate and if the patient is no able to understand to what that has been told to the
patient then the method is not effective (Dinh et al., 2016). The patient must be communicated
effectively by the nurses in order to make her understand about the needs to take care of herself.
The patient should know the ways to manage her fluid intake in relation to her diet. The patient
of the case study was suffering from chronic kidney disorder, so the nurse must make her
understand that she should take fluids according to the diet she is following (Caplin, & Saunders,
2015). As a nurse I would describe and demonstrate the patient about the serious consequences
that may happen if the patient is unable to manage the fluid intake according to the diet.
Part 3
The teach-back method is communication confirmation method which are used by the
healthcare providers in order to confirm that the patients have understood or not everything that
have been explained to them. If the patient is able to understand then the teach-back method is
effective and accurate and if the patient is no able to understand to what that has been told to the
patient then the method is not effective (Dinh et al., 2016). The patient must be communicated
effectively by the nurses in order to make her understand about the needs to take care of herself.
The patient should know the ways to manage her fluid intake in relation to her diet. The patient
of the case study was suffering from chronic kidney disorder, so the nurse must make her
understand that she should take fluids according to the diet she is following (Caplin, & Saunders,
2015). As a nurse I would describe and demonstrate the patient about the serious consequences
that may happen if the patient is unable to manage the fluid intake according to the diet.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9PATHOPHYSIOLOGY
References
Bernal, W., Jalan, R., Quaglia, A., Simpson, K., Wendon, J., & Burroughs, A. (2015). Acute-on-
chronic liver failure. The Lancet, 386(10003), 1576-1587.
Caplin, M., & Saunders, T. (2015). Utilizing teach-back to reinforce patient education: A step-
by-step approach. Orthopaedic Nursing, 34(6), 365-368.
Dhayef, A. K., Manuti, J. K., & Abutabiekh, A. S. (2017). Anemia response to Methoxy
Polyethylene Glycol-Epoetin Beta (Mircera) versus Epoetin Alfa (Eprex) in patients with
chronic Kidney disease on Hemodialysis. Methods, 17, 19.
Dinh, T. T. H., Bonner, A., Clark, R., Ramsbotham, J., & Hines, S. (2016). The effectiveness of
the teach-back method on adherence and self-management in health education for people
with chronic disease: a systematic review. JBI database of systematic reviews and
implementation reports, 14(1), 210-247.
Glassock, R. J., & Rule, A. D. (2016). Aging and the kidneys: anatomy, physiology and
consequences for defining chronic kidney disease. Nephron, 134(1), 25-29.
Gore, M. O., & McGuire, D. K. (2016). A test in context: hemoglobin A1c and cardiovascular
disease. Journal of the American College of Cardiology, 68(22), 2479-2486.
Klatte, T., Ficarra, V., Gratzke, C., Kaouk, J., Kutikov, A., Macchi, V., ... & Russo, P. (2015). A
literature review of renal surgical anatomy and surgical strategies for partial
nephrectomy. European urology, 68(6), 980-992.
References
Bernal, W., Jalan, R., Quaglia, A., Simpson, K., Wendon, J., & Burroughs, A. (2015). Acute-on-
chronic liver failure. The Lancet, 386(10003), 1576-1587.
Caplin, M., & Saunders, T. (2015). Utilizing teach-back to reinforce patient education: A step-
by-step approach. Orthopaedic Nursing, 34(6), 365-368.
Dhayef, A. K., Manuti, J. K., & Abutabiekh, A. S. (2017). Anemia response to Methoxy
Polyethylene Glycol-Epoetin Beta (Mircera) versus Epoetin Alfa (Eprex) in patients with
chronic Kidney disease on Hemodialysis. Methods, 17, 19.
Dinh, T. T. H., Bonner, A., Clark, R., Ramsbotham, J., & Hines, S. (2016). The effectiveness of
the teach-back method on adherence and self-management in health education for people
with chronic disease: a systematic review. JBI database of systematic reviews and
implementation reports, 14(1), 210-247.
Glassock, R. J., & Rule, A. D. (2016). Aging and the kidneys: anatomy, physiology and
consequences for defining chronic kidney disease. Nephron, 134(1), 25-29.
Gore, M. O., & McGuire, D. K. (2016). A test in context: hemoglobin A1c and cardiovascular
disease. Journal of the American College of Cardiology, 68(22), 2479-2486.
Klatte, T., Ficarra, V., Gratzke, C., Kaouk, J., Kutikov, A., Macchi, V., ... & Russo, P. (2015). A
literature review of renal surgical anatomy and surgical strategies for partial
nephrectomy. European urology, 68(6), 980-992.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10PATHOPHYSIOLOGY
Nazario, H. E., Ndungu, M., & Modi, A. A. (2016). Sofosbuvir and simeprevir in hepatitis C
genotype 1‐patients with end‐stage renal disease on haemodialysis or GFR< 30
ml/min. Liver International, 36(6), 798-801.
Ragab, M. A., Galal, S. M., Korany, M. A., & Ahmed, A. R. (2017). First derivative emission
spectrofluorimetric method for the determination of LCZ696, a newly approved FDA
supramolecular complex of valsartan and sacubitril in tablets. Luminescence, 32(8),
1417-1425.
Saliba, W., Barnett-Griness, O., Elias, M., & Rennert, G. (2015). Glycated hemoglobin and risk
of first episode stroke in diabetic patients with atrial fibrillation: a cohort study. Heart
Rhythm, 12(5), 886-892.
Sharma, A., Zaragoza, J. J., Villa, G., Ribeiro, L. C., Lu, R., Sartori, M., ... & Brocca, A. (2016).
Optimizing a kidney stress test to evaluate renal functional reserve. Clinical
nephrology, 86(1), 18.
Shi, Y., Yang, Y., Hu, Y., Wu, W., Yang, Q., Zheng, M., ... & Chen, Z. (2015). Acute‐on‐
chronic liver failure precipitated by hepatic injury is distinct from that precipitated by
extrahepatic insults. Hepatology, 62(1), 232-242.
Ter Maaten, J. M., Valente, M. A., Damman, K., Hillege, H. L., Navis, G., & Voors, A. A.
(2015). Diuretic response in acute heart failure—pathophysiology, evaluation, and
therapy. Nature Reviews Cardiology, 12(3), 184.
Venkatachalam, M. A., Weinberg, J. M., Kriz, W., & Bidani, A. K. (2015). Failed tubule
recovery, AKI-CKD transition, and kidney disease progression. Journal of the American
Society of Nephrology, 26(8), 1765-1776.
Nazario, H. E., Ndungu, M., & Modi, A. A. (2016). Sofosbuvir and simeprevir in hepatitis C
genotype 1‐patients with end‐stage renal disease on haemodialysis or GFR< 30
ml/min. Liver International, 36(6), 798-801.
Ragab, M. A., Galal, S. M., Korany, M. A., & Ahmed, A. R. (2017). First derivative emission
spectrofluorimetric method for the determination of LCZ696, a newly approved FDA
supramolecular complex of valsartan and sacubitril in tablets. Luminescence, 32(8),
1417-1425.
Saliba, W., Barnett-Griness, O., Elias, M., & Rennert, G. (2015). Glycated hemoglobin and risk
of first episode stroke in diabetic patients with atrial fibrillation: a cohort study. Heart
Rhythm, 12(5), 886-892.
Sharma, A., Zaragoza, J. J., Villa, G., Ribeiro, L. C., Lu, R., Sartori, M., ... & Brocca, A. (2016).
Optimizing a kidney stress test to evaluate renal functional reserve. Clinical
nephrology, 86(1), 18.
Shi, Y., Yang, Y., Hu, Y., Wu, W., Yang, Q., Zheng, M., ... & Chen, Z. (2015). Acute‐on‐
chronic liver failure precipitated by hepatic injury is distinct from that precipitated by
extrahepatic insults. Hepatology, 62(1), 232-242.
Ter Maaten, J. M., Valente, M. A., Damman, K., Hillege, H. L., Navis, G., & Voors, A. A.
(2015). Diuretic response in acute heart failure—pathophysiology, evaluation, and
therapy. Nature Reviews Cardiology, 12(3), 184.
Venkatachalam, M. A., Weinberg, J. M., Kriz, W., & Bidani, A. K. (2015). Failed tubule
recovery, AKI-CKD transition, and kidney disease progression. Journal of the American
Society of Nephrology, 26(8), 1765-1776.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





