Physical Health Assessment of Mental Health Consumers: A Case Study of Max
VerifiedAdded on 2023/06/10
|16
|4598
|483
AI Summary
This paper highlights the benefits of conducting Physical Health Assessment over the mental health consumer with the help of the Gray’s tool. It includes a detailed case study of the focused consumer followed by the through diagnosis of his physical health complication with the help of the parameters of the Grays’ tool. The paper also highlights the required interventions and the evaluation of the nursing interventions in order to improve the overall health and wellbeing of the patient.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NURSING
Nursing
Name of the Student
Name of University
Author’s note
Nursing
Name of the Student
Name of University
Author’s note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1
NURSING
Table of Contents
Introduction......................................................................................................................................2
Metabolic Syndrome........................................................................................................................2
Obesity, metabolic syndrome and use of anti-psychotic medications.........................................3
T2DM..........................................................................................................................................4
Consumers’ Background.................................................................................................................4
Current admission........................................................................................................................5
Medication Profile of Max...........................................................................................................5
Physical Health Profile of Max....................................................................................................5
Interventions and Recommendations...............................................................................................7
Conclusion.....................................................................................................................................10
References......................................................................................................................................11
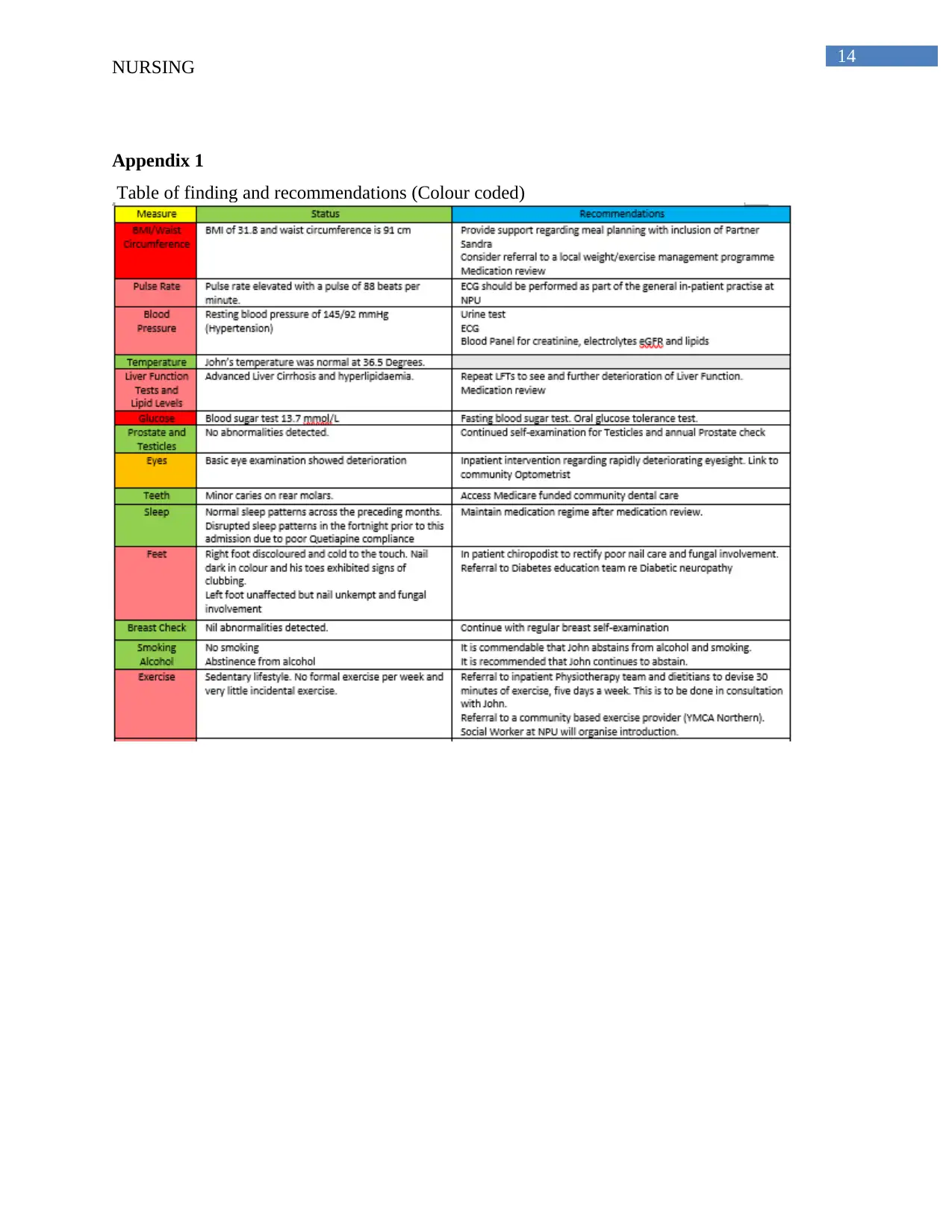
Appendix 1.....................................................................................................................................14
NURSING
Table of Contents
Introduction......................................................................................................................................2
Metabolic Syndrome........................................................................................................................2
Obesity, metabolic syndrome and use of anti-psychotic medications.........................................3
T2DM..........................................................................................................................................4
Consumers’ Background.................................................................................................................4
Current admission........................................................................................................................5
Medication Profile of Max...........................................................................................................5
Physical Health Profile of Max....................................................................................................5
Interventions and Recommendations...............................................................................................7
Conclusion.....................................................................................................................................10
References......................................................................................................................................11
Appendix 1.....................................................................................................................................14
2
NURSING
Introduction
People who are suffering from mental health complications are more vulnerable in
getting affected with physical disorders resulting in high rate of morbidity and mortality. The
high levels of mortality in mental health diseases either arise from suicides or from
cardiovascular complications/diabetes (Nash, 2013). With the prevalence of modifiable risk
factors associated with this population, the mental health nurses hold prime importance in
effective management of the health conditions. However, the mental health nurses experience
significant barriers towards performing a comprehensive physical assessment of their patients
and the reason behind this is lack of training (Fredriksen-Goldsen et al., 2013). The serious
mental illness Health Improvement Profile [HIP] is a clinical tool designed for the mental health
nurses for screening of the physical health profiles of their patients and accordingly setting the
clinical priority and designing evidence-based interventions. HIP must be performed upon
hospital admission or per year over the consumers with a Treatment Order or when the consumer
shows signs of physical deterioration. The following paper aims to highlight the benefits of
conducting Physical Health Assessment over the mental health consumer with the help of the
Gray’s tool (White et al., 2011). The essay will initiate with a detailed case study of the focused
consumer followed by the through diagnosis of his physical health complication with the help of
the parameters of the Grays’ tool. At the end, the paper will highlight the required interventions
and the evaluation of the nursing interventions in order to improve the overall health and well-
being of the patient.
Metabolic Syndrome
Metabolic syndrome is defined as a cluster of different disorders that occur together and
thereby increasing the risk of the patients towards developing non-communicable diseases
caused by modifiable risk factors like cardiovascular disease and type 2 diabetes mellitus
(T2DM). The main factors that are enrolled under the metabolic syndrome include central
obesity, hyperlipidaemia, lower levels of good cholesterol in blood (HDL), high blood pressure
and insulin resistance. The presence of any of these three factors out of five results in the
development of metabolic syndrome (White et al., 011).
NURSING
Introduction
People who are suffering from mental health complications are more vulnerable in
getting affected with physical disorders resulting in high rate of morbidity and mortality. The
high levels of mortality in mental health diseases either arise from suicides or from
cardiovascular complications/diabetes (Nash, 2013). With the prevalence of modifiable risk
factors associated with this population, the mental health nurses hold prime importance in
effective management of the health conditions. However, the mental health nurses experience
significant barriers towards performing a comprehensive physical assessment of their patients
and the reason behind this is lack of training (Fredriksen-Goldsen et al., 2013). The serious
mental illness Health Improvement Profile [HIP] is a clinical tool designed for the mental health
nurses for screening of the physical health profiles of their patients and accordingly setting the
clinical priority and designing evidence-based interventions. HIP must be performed upon
hospital admission or per year over the consumers with a Treatment Order or when the consumer
shows signs of physical deterioration. The following paper aims to highlight the benefits of
conducting Physical Health Assessment over the mental health consumer with the help of the
Gray’s tool (White et al., 2011). The essay will initiate with a detailed case study of the focused
consumer followed by the through diagnosis of his physical health complication with the help of
the parameters of the Grays’ tool. At the end, the paper will highlight the required interventions
and the evaluation of the nursing interventions in order to improve the overall health and well-
being of the patient.
Metabolic Syndrome
Metabolic syndrome is defined as a cluster of different disorders that occur together and
thereby increasing the risk of the patients towards developing non-communicable diseases
caused by modifiable risk factors like cardiovascular disease and type 2 diabetes mellitus
(T2DM). The main factors that are enrolled under the metabolic syndrome include central
obesity, hyperlipidaemia, lower levels of good cholesterol in blood (HDL), high blood pressure
and insulin resistance. The presence of any of these three factors out of five results in the
development of metabolic syndrome (White et al., 011).
3
NURSING
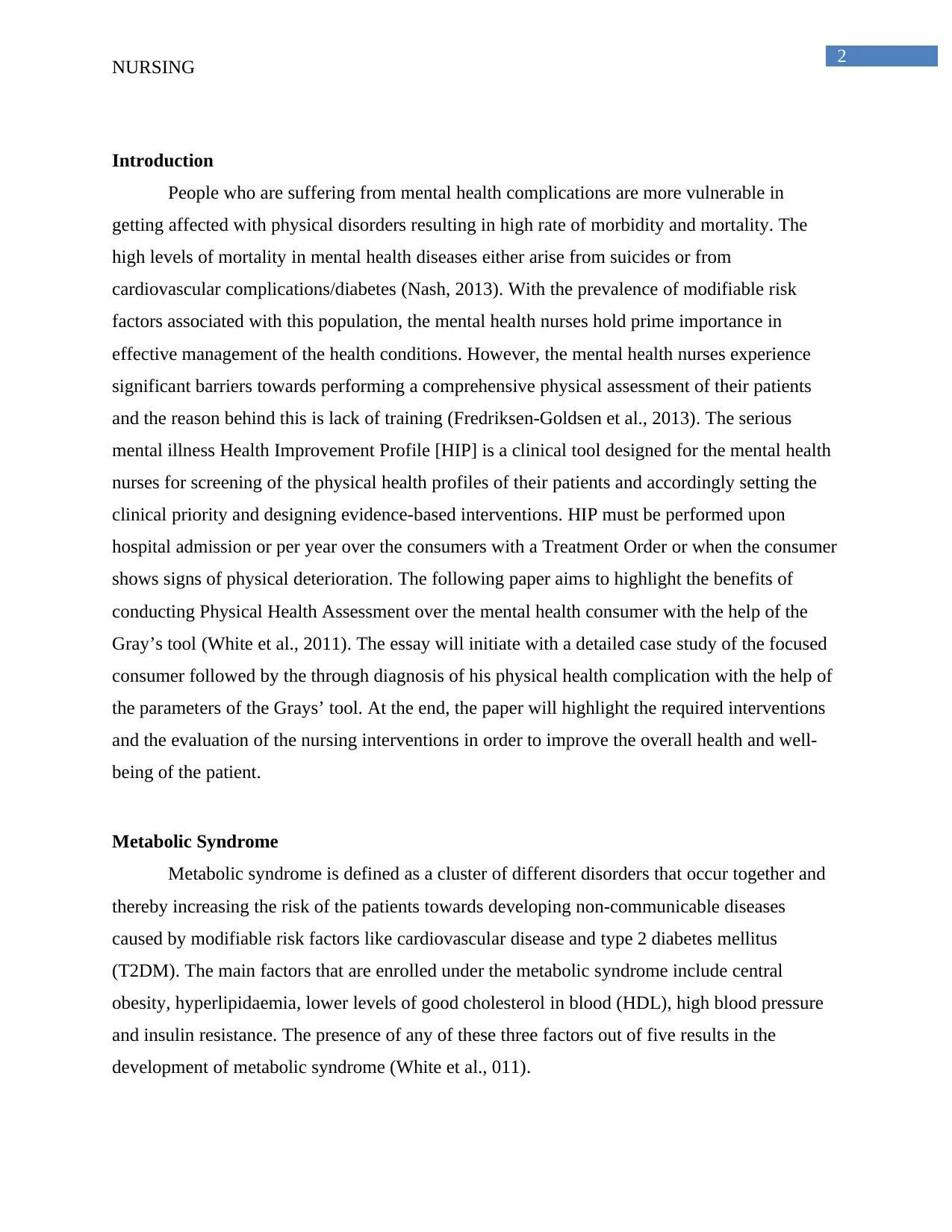
Obesity, metabolic syndrome and use of anti-psychotic medications
Patients who are suffering the serious mental ill health (SMI) and are on anti-psychotic
medications for a prolong period of time are vulnerable towards gaining massive weight leading
to obesity. The obesity in turn increases the severity of developing cardiovascular and thereby
reducing the total lifespan by 10 years in comparison to the other healthy individuals
(Vancampfort et al., 2015). The vulnerability of gaining drastic weight is common among 40 to
60% of the population of mental health service users who are suffering from bipolar disorder or
schizophrenia (Vancampfort et al., 2015). The risk is further increases in case of the patients who
are using second generation antipsychotic medication along with mood stabilizers (Tek et al.,
2016).
However, evidence suggests that long term use of anti-psychotic medications are not
solely linked with the development of adiposity or weight gain. The use of the mood stabilizers
and anti-depressant lie selective serotonin reuptake inhibitors (SSRIs) also increase the chance of
developing adiposity along with other metabolic syndrome like insulin resistance (Vancampfort
et al., 2015). Valpproate, a mood stabilizer possess the risk of developing insulin resistance
(Sharma & Taliyan, 2016).
Table 1: Classes of Drugs and impact on weight fluctuations
(Source: Domecq et al., 2015)
NURSING
Obesity, metabolic syndrome and use of anti-psychotic medications
Patients who are suffering the serious mental ill health (SMI) and are on anti-psychotic
medications for a prolong period of time are vulnerable towards gaining massive weight leading
to obesity. The obesity in turn increases the severity of developing cardiovascular and thereby
reducing the total lifespan by 10 years in comparison to the other healthy individuals
(Vancampfort et al., 2015). The vulnerability of gaining drastic weight is common among 40 to
60% of the population of mental health service users who are suffering from bipolar disorder or
schizophrenia (Vancampfort et al., 2015). The risk is further increases in case of the patients who
are using second generation antipsychotic medication along with mood stabilizers (Tek et al.,
2016).
However, evidence suggests that long term use of anti-psychotic medications are not
solely linked with the development of adiposity or weight gain. The use of the mood stabilizers
and anti-depressant lie selective serotonin reuptake inhibitors (SSRIs) also increase the chance of
developing adiposity along with other metabolic syndrome like insulin resistance (Vancampfort
et al., 2015). Valpproate, a mood stabilizer possess the risk of developing insulin resistance
(Sharma & Taliyan, 2016).
Table 1: Classes of Drugs and impact on weight fluctuations
(Source: Domecq et al., 2015)
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4
NURSING
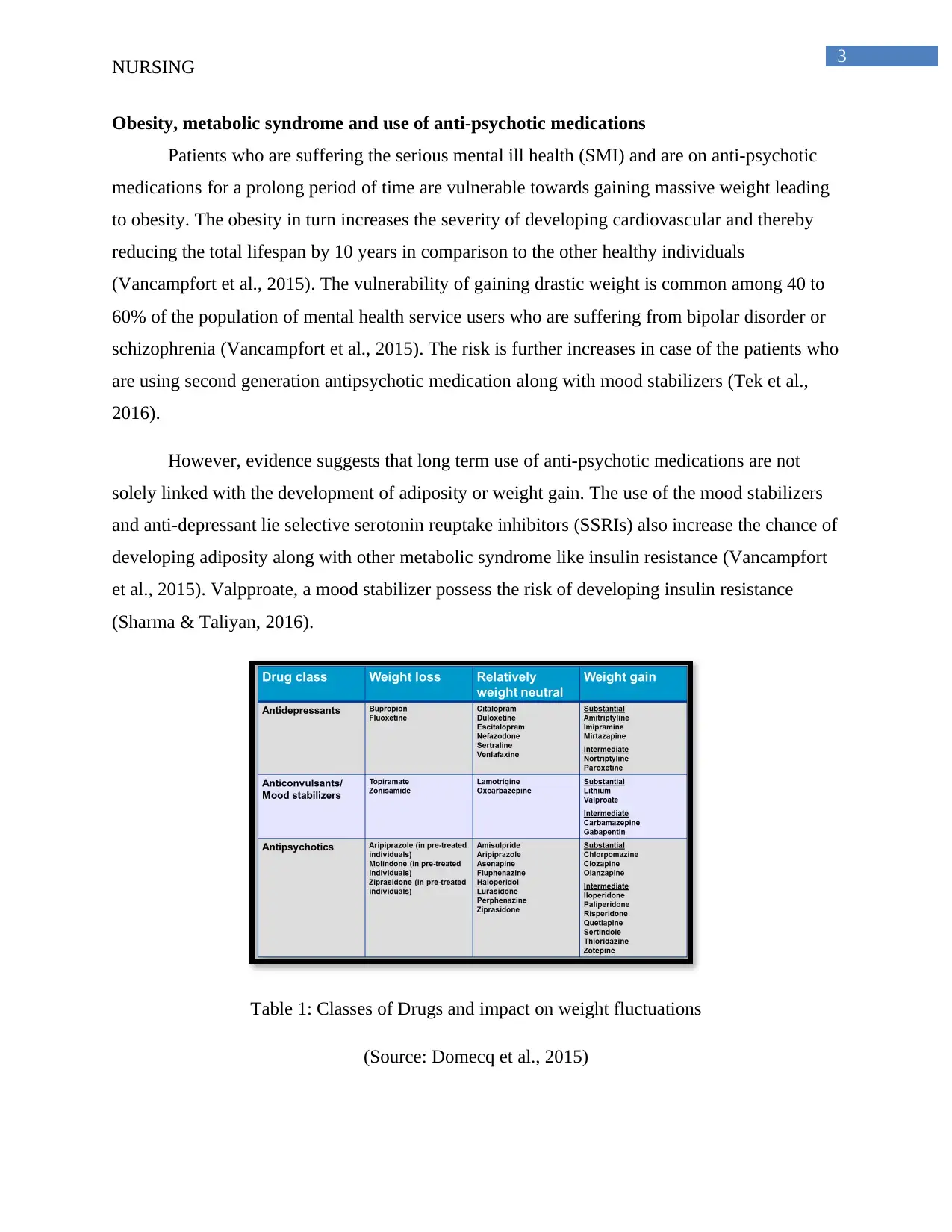
T2DM
The increases incidence of T2SM among the SMI is difficult to explain that it is
associated with several factors like the lifestyle factors: lack of proper diet plan, sedentary life
style and substance abuse along with increased use of the antipsychotic medications for the
prolong period of time (Holt & Mitchell, 2015). The consumption of second-generation
antipsychotics (SGAs) like the olanzapine and clozapine is associated with high risk of
developing metabolic syndrome (Suvisaari, Keinänen, Eskelinen & Mantere, 2016).
Figure: The metabolic screening and monitoring form
(Source: Holt & Mitchell, 2015)
Consumers’ Background
Max is a 50 year old married man and is a father of two children (20 years old and 10
years old). He is a victim of late onset Schizophrenia. Moreover, he is also suffering from
substance abuse and other physical health complications. His initial diagnosis with schizophrenia
was done 5 years ago when he was 345 years old. He is unemployed for the past 4 years after the
diagnosis of schizophrenia and his family is run by her wife who works in restaurant. Their elder
son, Charles (20 years old) lives out of station for his higher studies and the younger daughter
Ela (10 years old) stays with them. Max has done his studies up to 5th Grade and was working
since he was 14 years old and mainly serviced as manual labour. He has multiple physical health
NURSING
T2DM
The increases incidence of T2SM among the SMI is difficult to explain that it is
associated with several factors like the lifestyle factors: lack of proper diet plan, sedentary life
style and substance abuse along with increased use of the antipsychotic medications for the
prolong period of time (Holt & Mitchell, 2015). The consumption of second-generation
antipsychotics (SGAs) like the olanzapine and clozapine is associated with high risk of
developing metabolic syndrome (Suvisaari, Keinänen, Eskelinen & Mantere, 2016).
Figure: The metabolic screening and monitoring form
(Source: Holt & Mitchell, 2015)
Consumers’ Background
Max is a 50 year old married man and is a father of two children (20 years old and 10
years old). He is a victim of late onset Schizophrenia. Moreover, he is also suffering from
substance abuse and other physical health complications. His initial diagnosis with schizophrenia
was done 5 years ago when he was 345 years old. He is unemployed for the past 4 years after the
diagnosis of schizophrenia and his family is run by her wife who works in restaurant. Their elder
son, Charles (20 years old) lives out of station for his higher studies and the younger daughter
Ela (10 years old) stays with them. Max has done his studies up to 5th Grade and was working
since he was 14 years old and mainly serviced as manual labour. He has multiple physical health
5
NURSING
problems like high blood pressure, chronic obesity, ascetics that is associated with cirrhosis of
liver, hyperlipidemia and obstructive sleep apnoea.
Current admission
Max was admitted to the psychiatric unit of the state hospital after his wife Mary reported
signs of deterioration in his mental health. Marry reported that Max has visual and auditory
hallucinations, mainly remains confused throughout the day and shows signs of irritation when
asked to perform any household activity. While at home, Max was reviewed by Targeted Brief
Intervention (TBI) team. Max was found lying in bed, smoking a cigarette, with room filled with
thick smoke and was chanting words like he wants to go to hospital. Max was polite and pleasant
with the clinicians’ once in hospital and also agreed that lately he was facing trouble in
concentrating and is also hearing voices in his head. He gave consent for voluntary admission to
the Psychiatric Unit of the hospital.
Medication Profile of Max
Olanzapine
Quetiapine
Simvastin
Lithium
Enapril
Methodone
Valproate
Physical Health Profile of Max
Max is a tall guy with height of 172 cm and weighing 102 kilograms. His BMI was 30
and thus placing him under the obese range. His waist circumference is 92 cm. His pulse rate
was found moderately high, 88 beats per minute and resting blood pressure of 147/95 mmHg
(high blood pressure) (Dougherty & Lister, 2015). When asked, Max’s wife, Mary stated that he
was diagnosed with hypertension 10 years ago and for that he is on standing prescription of
Simvastin (50 mg per day post lunch). Max’s blood test revealed that his cholesterol level is 210
mg/dL with LDL (bad cholesterol count) of 170 mg/dL and showing visible signs of
hyperlipidemia (Dougherty & Lister, 2015). His liver cirrhosis was confirmed by the complete
liver function test (LFT). His alkaline phosphatse (ALP) level was normal and this no significant
NURSING
problems like high blood pressure, chronic obesity, ascetics that is associated with cirrhosis of
liver, hyperlipidemia and obstructive sleep apnoea.
Current admission
Max was admitted to the psychiatric unit of the state hospital after his wife Mary reported
signs of deterioration in his mental health. Marry reported that Max has visual and auditory
hallucinations, mainly remains confused throughout the day and shows signs of irritation when
asked to perform any household activity. While at home, Max was reviewed by Targeted Brief
Intervention (TBI) team. Max was found lying in bed, smoking a cigarette, with room filled with
thick smoke and was chanting words like he wants to go to hospital. Max was polite and pleasant
with the clinicians’ once in hospital and also agreed that lately he was facing trouble in
concentrating and is also hearing voices in his head. He gave consent for voluntary admission to
the Psychiatric Unit of the hospital.
Medication Profile of Max
Olanzapine
Quetiapine
Simvastin
Lithium
Enapril
Methodone
Valproate
Physical Health Profile of Max
Max is a tall guy with height of 172 cm and weighing 102 kilograms. His BMI was 30
and thus placing him under the obese range. His waist circumference is 92 cm. His pulse rate
was found moderately high, 88 beats per minute and resting blood pressure of 147/95 mmHg
(high blood pressure) (Dougherty & Lister, 2015). When asked, Max’s wife, Mary stated that he
was diagnosed with hypertension 10 years ago and for that he is on standing prescription of
Simvastin (50 mg per day post lunch). Max’s blood test revealed that his cholesterol level is 210
mg/dL with LDL (bad cholesterol count) of 170 mg/dL and showing visible signs of
hyperlipidemia (Dougherty & Lister, 2015). His liver cirrhosis was confirmed by the complete
liver function test (LFT). His alkaline phosphatse (ALP) level was normal and this no significant
6
NURSING
deterioration in his bile ducts. His total protein level is low indicating the signs of liver
dysfunction. The level of bilirubin in blood is high and thus indicating that his liver is suffering
from jaundice like condition that might have generated due to cirrhosis of liver (Dougherty &
Lister, 2015).
The body temperature of Max is found to be normal (36.5 degree C) with blood sugar
level (fasting) 13.6 mmol/L. This is way beyond the normal blood sugar level and thus
highlighting he is suffering from diabetes (Urden, Stacy & Lough, 2017). Testicular and prostate
examination stated that Max has no sexual abnormalities. When he was asked about his eye-
sight, Max stated that he was having double vision for the past 2 weeks and previously he used to
suffer from myopia (problem is viewing far places). He thinks his eyes on are gone.
Max has normal pattern of sleep and hence he has taken Quetiapine regularly however,
he stated that he was having disruptive sleep patterns in the fortnight prior to the admission in the
hospital. Breast examination failed to detect any abnormalities the foot examination revealed that
his right feet is cold to touch and the nails of his left feet is dark in colour and his toes showed
signs of clubbing. His right left seemed unaffected however the nail shows fungal infection.
Max lives sedentary life and do not follow any formal physical exercise pattern. His
driving licence has lapsed 5 years ago and the public transport he use is bus and the bus top is
approximately 500 meters from the home.
Max described that he consumes everything that he gets like ice-cream, potato chips, soft
drinks, chocolates. In dinner involves pizzas, pies and frozen chips and he drinks very little water
per day. Last month he reported that he is feeling thirty for the majority of the day with increased
tendency of urinating. In order to manage his thirst he takes Cappuccino. His urine is dark yellow
colour with pungent smell. His urine shows presence of glucose, ketones and micro albumin and
protein. He has regular bowel movements and stool is of foul smelling and poorly formed. He is
married with his wife for 30 years and have stable monogamous relationships. He engagement
unprotected sex but neither of them have STIs. He reports that he has a normal levels of libido.
NURSING
deterioration in his bile ducts. His total protein level is low indicating the signs of liver
dysfunction. The level of bilirubin in blood is high and thus indicating that his liver is suffering
from jaundice like condition that might have generated due to cirrhosis of liver (Dougherty &
Lister, 2015).
The body temperature of Max is found to be normal (36.5 degree C) with blood sugar
level (fasting) 13.6 mmol/L. This is way beyond the normal blood sugar level and thus
highlighting he is suffering from diabetes (Urden, Stacy & Lough, 2017). Testicular and prostate
examination stated that Max has no sexual abnormalities. When he was asked about his eye-
sight, Max stated that he was having double vision for the past 2 weeks and previously he used to
suffer from myopia (problem is viewing far places). He thinks his eyes on are gone.
Max has normal pattern of sleep and hence he has taken Quetiapine regularly however,
he stated that he was having disruptive sleep patterns in the fortnight prior to the admission in the
hospital. Breast examination failed to detect any abnormalities the foot examination revealed that
his right feet is cold to touch and the nails of his left feet is dark in colour and his toes showed
signs of clubbing. His right left seemed unaffected however the nail shows fungal infection.
Max lives sedentary life and do not follow any formal physical exercise pattern. His
driving licence has lapsed 5 years ago and the public transport he use is bus and the bus top is
approximately 500 meters from the home.
Max described that he consumes everything that he gets like ice-cream, potato chips, soft
drinks, chocolates. In dinner involves pizzas, pies and frozen chips and he drinks very little water
per day. Last month he reported that he is feeling thirty for the majority of the day with increased
tendency of urinating. In order to manage his thirst he takes Cappuccino. His urine is dark yellow
colour with pungent smell. His urine shows presence of glucose, ketones and micro albumin and
protein. He has regular bowel movements and stool is of foul smelling and poorly formed. He is
married with his wife for 30 years and have stable monogamous relationships. He engagement
unprotected sex but neither of them have STIs. He reports that he has a normal levels of libido.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
NURSING
Interventions and Recommendations
As per the evidences excess gain in weight is three or more times common among the
people who are suffering from SMI in comparison to the general population (Jørgensen et al.,
2017). Numerous antipsychotics medication elicits impaired glucose and lipid metabolism along
with gain in weight, high blood pressure and arrhythmias (Jørgensen et al., 2017). The BMI is a
measure of weight gain but it fails to highlight the areas of the body that has maximum
deposition of fat. Central level of adiposity is regarded as one of the important signs of insulin
resistance or other metabolic syndrome. A waist circumference that is greater than 90 cm as in
case of Max (in women this value is > 80 cm) is associated with an increased prevalence of
diabetes, hypertension along with high level of blood cholesterol and other cardiovascular
disease (Jørgensen et al., 2017). The BMI if Max is greater than 30 with waist circumference
greater than 90 indicating that he is under risk of developing cardiovascular disease (CVD) and
type 2 diabetes mellitus (T2DM) (White, Gray, Swift, Barton & Jones, 2011). As per the
working diagnosis of the Metabolic Syndrome, presence of three out of five risk factors
including adiposity, hypertension and hyperlipidaemia and thus Max can be diagnosed under
metabolic syndrome. It is recommended that Max must undertake further diagnosis for proper
estimation of the treat of developing T2DM and CVD.
Indicator of the cardiovascular health is increased pulse rate and high blood pressure.
Long term use of antipsychotics medication among the population of SMI is complicated as it is
associated with negative cardiovascular effects and thereby increasing the rate of morbidity and
mortality in comparison to the general population (Pringsheim et al., 2017). Antipsychotic
medications also have a potential threat of developing extended QT interval (in male the
prolonged rates are indicated when the value is greater than 450 ms and in females that value is
greater than 470 ms) (Takeuchi, Suzuki, Remington & Uchida, 2015). This high QT value affects
the resting heart rate of the consumers. The heart rate of Max is elevated 88bpm with resting
blood pressure is 142/92 mm Hg. This indicates that Max is a patient of hyper tension and his
previous case history also indicates the presence of hypertension as per this medication list that
contains anti-hypertension medication (Enanpril 2.5 mg per day). It is recommended that Max
must undertake a review of the medication as his blood pressure is elevated even after the
consumption of the blood pressure medication. Antipsychotic medications cross-reacts with
Enanpril and thus reducing its overall effect to reduce blood pressure (Arivazhahan, Bairy,
NURSING
Interventions and Recommendations
As per the evidences excess gain in weight is three or more times common among the
people who are suffering from SMI in comparison to the general population (Jørgensen et al.,
2017). Numerous antipsychotics medication elicits impaired glucose and lipid metabolism along
with gain in weight, high blood pressure and arrhythmias (Jørgensen et al., 2017). The BMI is a
measure of weight gain but it fails to highlight the areas of the body that has maximum
deposition of fat. Central level of adiposity is regarded as one of the important signs of insulin
resistance or other metabolic syndrome. A waist circumference that is greater than 90 cm as in
case of Max (in women this value is > 80 cm) is associated with an increased prevalence of
diabetes, hypertension along with high level of blood cholesterol and other cardiovascular
disease (Jørgensen et al., 2017). The BMI if Max is greater than 30 with waist circumference
greater than 90 indicating that he is under risk of developing cardiovascular disease (CVD) and
type 2 diabetes mellitus (T2DM) (White, Gray, Swift, Barton & Jones, 2011). As per the
working diagnosis of the Metabolic Syndrome, presence of three out of five risk factors
including adiposity, hypertension and hyperlipidaemia and thus Max can be diagnosed under
metabolic syndrome. It is recommended that Max must undertake further diagnosis for proper
estimation of the treat of developing T2DM and CVD.
Indicator of the cardiovascular health is increased pulse rate and high blood pressure.
Long term use of antipsychotics medication among the population of SMI is complicated as it is
associated with negative cardiovascular effects and thereby increasing the rate of morbidity and
mortality in comparison to the general population (Pringsheim et al., 2017). Antipsychotic
medications also have a potential threat of developing extended QT interval (in male the
prolonged rates are indicated when the value is greater than 450 ms and in females that value is
greater than 470 ms) (Takeuchi, Suzuki, Remington & Uchida, 2015). This high QT value affects
the resting heart rate of the consumers. The heart rate of Max is elevated 88bpm with resting
blood pressure is 142/92 mm Hg. This indicates that Max is a patient of hyper tension and his
previous case history also indicates the presence of hypertension as per this medication list that
contains anti-hypertension medication (Enanpril 2.5 mg per day). It is recommended that Max
must undertake a review of the medication as his blood pressure is elevated even after the
consumption of the blood pressure medication. Antipsychotic medications cross-reacts with
Enanpril and thus reducing its overall effect to reduce blood pressure (Arivazhahan, Bairy,
8
NURSING
Nayak & Kunder, 2017). Elevated blood pressure is associated with increased likelihood of
stroke and problem in proper function of kidneys. The urine test of Max showed presence of
bilirubin in urine and glucose and this might be due to liver cirrhosis (causing increase of
bilirubin urine) and high level of diabetes (causing high levels of glucose in urine) further
investigation of urine is recommended.
Max has normal body temperature that represents no visible signs of infections within the
body however; it is recommended that his body temperature is monitored regularly. Intervention
for Max will include proper combination of physical exercise and diet.
Dyslipidaemia is the principal component of metabolic syndrome and is regarded as an
important precursor of cardiovascular disease. It is well accepted that prolong use of the
antipsychotic medication increases the risk of developing dyslpidaemia (Yogaratnam, Biswas,
Vadivel & Jacob, 2017). The total cholesterol level of Max is 210 mg/dL with LDL (bad
cholesterol count) of 170 mg/dL and showing visible signs of hyperlipidemia, Max takes
Simvastin as a part of his daily medication however his lipid medication is still high. Simvastin
mainly acts through HMG-CoA inhibitor mechanism in order to level of cholesterol. Prolong use
of the anti schizophrenia drugs hamper the mechanism of HMG-CoA inhibitor mechanism and
thus might be the reason for medication inactivity (Kain, Kapadia, Misra & Saxena, 2015).
Diabetes is common among the proper suffering from schizophrenia. The risk factor for
T2DM also increases the hereditary pre-disposition, unhealthy lifestyle habits like sedentary
lifestyle , consumption of alcohol, smoking and unhealthy diet (Nemani et al., 2017). The
antipsychotic medications like the olanzapine and clozapine are associated with the onset of
T2DM as these medications are associated with increased gain in body mass by modulating the
glucose regulation (Nemani et al., 2017) The waist circumference of Max is high. He also leads a
sedentary lifestyle, consumes antipsychotic medication and consumes junk food. All these
tendencies have promoted the process of development of T2DM. This urine test also reveals the
presence of glucose along with fasting blood glucose of 13.6 mmol/L further test of HbAc1 is
required to be undertaken in order to specify the severity of blood glucose level (White, Gray
Swift, Barton & Jones, 2011).
NURSING
Nayak & Kunder, 2017). Elevated blood pressure is associated with increased likelihood of
stroke and problem in proper function of kidneys. The urine test of Max showed presence of
bilirubin in urine and glucose and this might be due to liver cirrhosis (causing increase of
bilirubin urine) and high level of diabetes (causing high levels of glucose in urine) further
investigation of urine is recommended.
Max has normal body temperature that represents no visible signs of infections within the
body however; it is recommended that his body temperature is monitored regularly. Intervention
for Max will include proper combination of physical exercise and diet.
Dyslipidaemia is the principal component of metabolic syndrome and is regarded as an
important precursor of cardiovascular disease. It is well accepted that prolong use of the
antipsychotic medication increases the risk of developing dyslpidaemia (Yogaratnam, Biswas,
Vadivel & Jacob, 2017). The total cholesterol level of Max is 210 mg/dL with LDL (bad
cholesterol count) of 170 mg/dL and showing visible signs of hyperlipidemia, Max takes
Simvastin as a part of his daily medication however his lipid medication is still high. Simvastin
mainly acts through HMG-CoA inhibitor mechanism in order to level of cholesterol. Prolong use
of the anti schizophrenia drugs hamper the mechanism of HMG-CoA inhibitor mechanism and
thus might be the reason for medication inactivity (Kain, Kapadia, Misra & Saxena, 2015).
Diabetes is common among the proper suffering from schizophrenia. The risk factor for
T2DM also increases the hereditary pre-disposition, unhealthy lifestyle habits like sedentary
lifestyle , consumption of alcohol, smoking and unhealthy diet (Nemani et al., 2017). The
antipsychotic medications like the olanzapine and clozapine are associated with the onset of
T2DM as these medications are associated with increased gain in body mass by modulating the
glucose regulation (Nemani et al., 2017) The waist circumference of Max is high. He also leads a
sedentary lifestyle, consumes antipsychotic medication and consumes junk food. All these
tendencies have promoted the process of development of T2DM. This urine test also reveals the
presence of glucose along with fasting blood glucose of 13.6 mmol/L further test of HbAc1 is
required to be undertaken in order to specify the severity of blood glucose level (White, Gray
Swift, Barton & Jones, 2011).
9
NURSING
Testicle cancer amounts about 1% of cancer among men and however, testicles of Max
did not showed any prominent abnormality. However, yearly screening is recommended in order
to reduce the risk of developing testicle cancer as it is one of the common cancer among the
older adults (men). Moreover, Razdan et al. (2018) stated that over use of the antipsychotic
medication leads to erectile dysfunction. Thus screening of the genital organs is important.
However, at present Max has normal level of libido.
The prolong use of the antipsychotic medication can lead to permanent damage of lens
and cornea. It also leads to the development of cataract (Seymour, Rhodes, Stein & Langdon,
2016). The decreased eye sight of Max might be due to his prolong use of the antipsychotic
medication. Moreover, it might also be the base of diabetic retinopathy. A detailed in-patient
follow-up of the eye-sight checking is recommended followed by a community referral to an
Ophthalmologist. Use of the antipsychotic medications, lead to poor dental health like swelling
and bleeding of gums and generation of foul smell in the mouth. However, Max is found to have
a standard oral health and hygiene.
The individuals who fall under SMI suffer from insomnia. At standard sleep of 7 to 8
hours is recommended in order to maintain a standard health and well-being (Tan et al., 2016).
The medication of Quetiapine has helped Max to enjoy a peaceful sleep at night.
High level of blood glucose arising out of T2DM leads to poor circulation of blood at the
peripheral extremities of the body. This is known as peripheral neuropathy and mainly arises
from the narrowing of the arteries and nerve damage (Sharma & Taliyan, 2016). Max feet have
visible signs of peripheral neuropathy as it is cold to touch. It also indicates the signs of poor
hygiene as reflected from the overgrown nails and fungal infection. Proper diabetes education is
recommended by a trained diabetic team in order to increase his knowledge about foot care and
maintenance of proper feet hygiene.
The diet of Max mainly includes high saturated fatty acids and refined sugar along with
consumption of instant meals. Max has minimal intake of fruit and vegetables with little
consumptions of lean protein. It is recommended that the nutritional planning of Max must be
done under the controlled supervision of trained professional nurse. Max mainly needs a strict
diabetic plan along with proper health literacy so that he refrain himself from consuming
NURSING
Testicle cancer amounts about 1% of cancer among men and however, testicles of Max
did not showed any prominent abnormality. However, yearly screening is recommended in order
to reduce the risk of developing testicle cancer as it is one of the common cancer among the
older adults (men). Moreover, Razdan et al. (2018) stated that over use of the antipsychotic
medication leads to erectile dysfunction. Thus screening of the genital organs is important.
However, at present Max has normal level of libido.
The prolong use of the antipsychotic medication can lead to permanent damage of lens
and cornea. It also leads to the development of cataract (Seymour, Rhodes, Stein & Langdon,
2016). The decreased eye sight of Max might be due to his prolong use of the antipsychotic
medication. Moreover, it might also be the base of diabetic retinopathy. A detailed in-patient
follow-up of the eye-sight checking is recommended followed by a community referral to an
Ophthalmologist. Use of the antipsychotic medications, lead to poor dental health like swelling
and bleeding of gums and generation of foul smell in the mouth. However, Max is found to have
a standard oral health and hygiene.
The individuals who fall under SMI suffer from insomnia. At standard sleep of 7 to 8
hours is recommended in order to maintain a standard health and well-being (Tan et al., 2016).
The medication of Quetiapine has helped Max to enjoy a peaceful sleep at night.
High level of blood glucose arising out of T2DM leads to poor circulation of blood at the
peripheral extremities of the body. This is known as peripheral neuropathy and mainly arises
from the narrowing of the arteries and nerve damage (Sharma & Taliyan, 2016). Max feet have
visible signs of peripheral neuropathy as it is cold to touch. It also indicates the signs of poor
hygiene as reflected from the overgrown nails and fungal infection. Proper diabetes education is
recommended by a trained diabetic team in order to increase his knowledge about foot care and
maintenance of proper feet hygiene.
The diet of Max mainly includes high saturated fatty acids and refined sugar along with
consumption of instant meals. Max has minimal intake of fruit and vegetables with little
consumptions of lean protein. It is recommended that the nutritional planning of Max must be
done under the controlled supervision of trained professional nurse. Max mainly needs a strict
diabetic plan along with proper health literacy so that he refrain himself from consuming
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10
NURSING
unhealthy diet like junk food in the absence of his wife. Max also has poor intake of water and
high intake of caffeine. This restricted intake of fluid might lead to dehydration and renal
malfunction. Thus proper yet regulated intake of water must be monitored for Max.
Consumption of coffee must be reduced as it may cast significant damage of the nerves. His
excess urge to urination might be due to diabetes thus consultation with a diabetic expert is
recommended (Sharma & Taliyan, 2016).
Thus in-patient service with which the health lifestyle interventions of Max are linked
include: Diabetic education team, diabetic expert, professional yet trained dietician or nutritionist
and a physiotherapist. Max must also be involved under the community health checkup service
for periodic monitoring of this blood glucose level, BMI, blood pressure, pulse rate, oxygen
saturation, heart rate, and body weight and eye sight. Max also needs to attend a community
based physical exercise session at least thrice a week in order to reduce his wait circumference
and BMI.
Conclusion
Thus from the above discussion, it can be concluded that the proper application of the
clinical tool by the mental health nursing professionals helps to increase the overall quality of
care. The clinical tool helps in highlighting the physical abnormality that might have resulted due
to the long-term use of the antipsychotic medication. Proper physical assessment performance
with the help to the clinical tool like the Grays’ tool helps in the identification of the co-
morbidities associated with the long-term use of the antipsychotic medication and thereby
helping to frame the interventions in order to improve the overall outcome of care. Early and
timely interventions can help to ameliorate the high population morbidity and mortality
associated with the metabolic disorders and other cardiovascular disease.
NURSING
unhealthy diet like junk food in the absence of his wife. Max also has poor intake of water and
high intake of caffeine. This restricted intake of fluid might lead to dehydration and renal
malfunction. Thus proper yet regulated intake of water must be monitored for Max.
Consumption of coffee must be reduced as it may cast significant damage of the nerves. His
excess urge to urination might be due to diabetes thus consultation with a diabetic expert is
recommended (Sharma & Taliyan, 2016).
Thus in-patient service with which the health lifestyle interventions of Max are linked
include: Diabetic education team, diabetic expert, professional yet trained dietician or nutritionist
and a physiotherapist. Max must also be involved under the community health checkup service
for periodic monitoring of this blood glucose level, BMI, blood pressure, pulse rate, oxygen
saturation, heart rate, and body weight and eye sight. Max also needs to attend a community
based physical exercise session at least thrice a week in order to reduce his wait circumference
and BMI.
Conclusion
Thus from the above discussion, it can be concluded that the proper application of the
clinical tool by the mental health nursing professionals helps to increase the overall quality of
care. The clinical tool helps in highlighting the physical abnormality that might have resulted due
to the long-term use of the antipsychotic medication. Proper physical assessment performance
with the help to the clinical tool like the Grays’ tool helps in the identification of the co-
morbidities associated with the long-term use of the antipsychotic medication and thereby
helping to frame the interventions in order to improve the overall outcome of care. Early and
timely interventions can help to ameliorate the high population morbidity and mortality
associated with the metabolic disorders and other cardiovascular disease.

11
NURSING
References
Arivazhahan, A., Bairy, L. K., Nayak, V., & Kunder, S. K. (2017). A Study to Assess the
Therapeutic Effect of Enalapril on Olanzapine Induced Metabolic Syndrome in Wistar
Rats. Journal of Clinical and Diagnostic Research: JCDR, 11(2), FF01.
Domecq, J. P., Prutsky, G., Leppin, A., Sonbol, M. B., Altayar, O., Undavalli, C., ... & Lababidi,
M. H. (2015). Drugs commonly associated with weight change: a systematic review and
meta-analysis. The Journal of Clinical Endocrinology & Metabolism, 100(2), 363-370.
https://doi.org/10.1210/jc.2014-3421
Dougherty, L., & Lister, S. (Eds.). (2015). The Royal Marsden manual of clinical nursing
procedures. John Wiley & Sons.
Fredriksen-Goldsen, K. I., Cook-Daniels, L., Kim, H. J., Erosheva, E. A., Emlet, C. A., Hoy-
Ellis, C. P., ... & Muraco, A. (2013). Physical and mental health of transgender older
adults: An at-risk and underserved population. The Gerontologist, 54(3), 488-500.
https://doi.org/10.1093/geront/gnt021
Holt, R. I., & Mitchell, A. J. (2015). Diabetes mellitus and severe mental illness: mechanisms
and clinical implications. Nature Reviews Endocrinology, 11(2), 79. Retrieved from:
https://www.nature.com/articles/nrendo.2014.203
Jørgensen, K. N., Nesvåg, R., Nerland, S., Mørch‐Johnsen, L., Westlye, L. T., Lange, E. H., ... &
Agartz, I. (2017). Brain volume change in first‐episode psychosis: an effect of
antipsychotic medication independent of BMI change. Acta Psychiatrica
Scandinavica, 135(2), 117-126. https://doi.org/10.1111/acps.12677
Kain, V., Kapadia, B., Misra, P., & Saxena, U. (2015). Simvastatin may induce insulin resistance
through a novel fatty acid mediated cholesterol independent mechanism. Scientific
reports, 5, 13823. Retrieved from: https://www.nature.com/articles/srep13823
NURSING
References
Arivazhahan, A., Bairy, L. K., Nayak, V., & Kunder, S. K. (2017). A Study to Assess the
Therapeutic Effect of Enalapril on Olanzapine Induced Metabolic Syndrome in Wistar
Rats. Journal of Clinical and Diagnostic Research: JCDR, 11(2), FF01.
Domecq, J. P., Prutsky, G., Leppin, A., Sonbol, M. B., Altayar, O., Undavalli, C., ... & Lababidi,
M. H. (2015). Drugs commonly associated with weight change: a systematic review and
meta-analysis. The Journal of Clinical Endocrinology & Metabolism, 100(2), 363-370.
https://doi.org/10.1210/jc.2014-3421
Dougherty, L., & Lister, S. (Eds.). (2015). The Royal Marsden manual of clinical nursing
procedures. John Wiley & Sons.
Fredriksen-Goldsen, K. I., Cook-Daniels, L., Kim, H. J., Erosheva, E. A., Emlet, C. A., Hoy-
Ellis, C. P., ... & Muraco, A. (2013). Physical and mental health of transgender older
adults: An at-risk and underserved population. The Gerontologist, 54(3), 488-500.
https://doi.org/10.1093/geront/gnt021
Holt, R. I., & Mitchell, A. J. (2015). Diabetes mellitus and severe mental illness: mechanisms
and clinical implications. Nature Reviews Endocrinology, 11(2), 79. Retrieved from:
https://www.nature.com/articles/nrendo.2014.203
Jørgensen, K. N., Nesvåg, R., Nerland, S., Mørch‐Johnsen, L., Westlye, L. T., Lange, E. H., ... &
Agartz, I. (2017). Brain volume change in first‐episode psychosis: an effect of
antipsychotic medication independent of BMI change. Acta Psychiatrica
Scandinavica, 135(2), 117-126. https://doi.org/10.1111/acps.12677
Kain, V., Kapadia, B., Misra, P., & Saxena, U. (2015). Simvastatin may induce insulin resistance
through a novel fatty acid mediated cholesterol independent mechanism. Scientific
reports, 5, 13823. Retrieved from: https://www.nature.com/articles/srep13823
12
NURSING
Nash, M. (2013). Diagnostic overshadowing: a potential barrier to physical health care for
mental health service users. Mental Health Practice, 17(4).
doi: 10.7748/mhp2013.12.17.4.22.e862
Nemani, K. L., Greene, M. C., Ulloa, M., Vincenzi, B., Copeland, P. M., Al-Khadari, S., &
Henderson, D. C. (2017). Clozapine, diabetes mellitus, cardiovascular risk and mortality:
results of a 21-year naturalistic study in patients with schizophrenia and schizoaffective
disorder. Clinical schizophrenia & related psychoses.
https://doi.org/10.3371/CSRP.KNMG.111717
Pringsheim, T., Kelly, M., Urness, D., Teehan, M., Ismail, Z., & Gardner, D. (2017). Physical
Health and Drug Safety in individuals with schizophrenia. The Canadian Journal of
Psychiatry, 62(9), 673-683. https://doi.org/10.1177/0706743717719898
Razdan, S., Greer, A. B., Patel, A., Alameddine, M., Jue, J. S., & Ramasamy, R. (2018). Effect
of prescription medications on erectile dysfunction. Postgraduate medical
journal, 94(1109), 171-178. http://dx.doi.org/10.1136/postgradmedj-2017-135233
Seymour, K., Rhodes, G., Stein, T., & Langdon, R. (2016). Intact unconscious processing of eye
contact in schizophrenia. Schizophrenia research: cognition, 3, 15-19.
https://doi.org/10.1016/j.scog.2015.11.001
Sharma, S., & Taliyan, R. (2016). Histone deacetylase inhibitors: Future therapeutics for insulin
resistance and type 2 diabetes. Pharmacological research, 113, 320-326.
https://doi.org/10.1016/j.phrs.2016.09.009
Suvisaari, J., Keinänen, J., Eskelinen, S., & Mantere, O. (2016). Diabetes and
schizophrenia. Current diabetes reports, 16(2), 16. https://doi.org/10.1007/s11892-015-
0704-4
Takeuchi, H., Suzuki, T., Remington, G., & Uchida, H. (2015). Antipsychotic polypharmacy and
corrected QT interval: a systematic review. The Canadian Journal of Psychiatry, 60(5),
215-222. https://doi.org/10.1177/070674371506000503
NURSING
Nash, M. (2013). Diagnostic overshadowing: a potential barrier to physical health care for
mental health service users. Mental Health Practice, 17(4).
doi: 10.7748/mhp2013.12.17.4.22.e862
Nemani, K. L., Greene, M. C., Ulloa, M., Vincenzi, B., Copeland, P. M., Al-Khadari, S., &
Henderson, D. C. (2017). Clozapine, diabetes mellitus, cardiovascular risk and mortality:
results of a 21-year naturalistic study in patients with schizophrenia and schizoaffective
disorder. Clinical schizophrenia & related psychoses.
https://doi.org/10.3371/CSRP.KNMG.111717
Pringsheim, T., Kelly, M., Urness, D., Teehan, M., Ismail, Z., & Gardner, D. (2017). Physical
Health and Drug Safety in individuals with schizophrenia. The Canadian Journal of
Psychiatry, 62(9), 673-683. https://doi.org/10.1177/0706743717719898
Razdan, S., Greer, A. B., Patel, A., Alameddine, M., Jue, J. S., & Ramasamy, R. (2018). Effect
of prescription medications on erectile dysfunction. Postgraduate medical
journal, 94(1109), 171-178. http://dx.doi.org/10.1136/postgradmedj-2017-135233
Seymour, K., Rhodes, G., Stein, T., & Langdon, R. (2016). Intact unconscious processing of eye
contact in schizophrenia. Schizophrenia research: cognition, 3, 15-19.
https://doi.org/10.1016/j.scog.2015.11.001
Sharma, S., & Taliyan, R. (2016). Histone deacetylase inhibitors: Future therapeutics for insulin
resistance and type 2 diabetes. Pharmacological research, 113, 320-326.
https://doi.org/10.1016/j.phrs.2016.09.009
Suvisaari, J., Keinänen, J., Eskelinen, S., & Mantere, O. (2016). Diabetes and
schizophrenia. Current diabetes reports, 16(2), 16. https://doi.org/10.1007/s11892-015-
0704-4
Takeuchi, H., Suzuki, T., Remington, G., & Uchida, H. (2015). Antipsychotic polypharmacy and
corrected QT interval: a systematic review. The Canadian Journal of Psychiatry, 60(5),
215-222. https://doi.org/10.1177/070674371506000503
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13
NURSING
Tan, L., Zhou, J., Liang, B., Li, Y., Lei, F., Du, L., ... & Tang, X. (2016). A case of quetiapine-
induced rapid eye movement sleep behavior disorder. Biological psychiatry, 79(5), e11-
e12. DOI: https://doi.org/10.1016/j.biopsych.2014.08.002
Tek, C., Kucukgoncu, S., Guloksuz, S., Woods, S. W., Srihari, V. H., & Annamalai, A. (2016).
Antipsychotic‐induced weight gain in first‐episode psychosis patients: a meta‐analysis of
differential effects of antipsychotic medications. Early intervention in psychiatry, 10(3),
193-202. ttps://doi.org/10.1111/eip.12251
Urden, L. D., Stacy, K. M., & Lough, M. E. (2017). Critical care nursing: diagnosis and
management. Elsevier Health Sciences.
Vancampfort, D., Stubbs, B., Mitchell, A. J., De Hert, M., Wampers, M., Ward, P. B., ... &
Correll, C. U. (2015). Risk of metabolic syndrome and its components in people with
schizophrenia and related psychotic disorders, bipolar disorder and major depressive
disorder: a systematic review and meta‐analysis. World Psychiatry, 14(3), 339-347.
https://doi.org/10.1002/wps.20252
White, J., Gray, R. J., Swift, L., Barton, G. R., & Jones, M. (2011). The serious mental illness
health improvement profile [HIP]: study protocol for a cluster randomised controlled
trial. Trials, 12(1), 167. https://doi.org/10.1186/1745-6215-12-167
Yogaratnam, J., Biswas, N., Vadivel, R., & Jacob, R. (2017). Metabolic complications of
schizophrenia and antipsychotic medications--an updated review. URI: https://open-
access.imh.com.sg/handle/123456789/4690
NURSING
Tan, L., Zhou, J., Liang, B., Li, Y., Lei, F., Du, L., ... & Tang, X. (2016). A case of quetiapine-
induced rapid eye movement sleep behavior disorder. Biological psychiatry, 79(5), e11-
e12. DOI: https://doi.org/10.1016/j.biopsych.2014.08.002
Tek, C., Kucukgoncu, S., Guloksuz, S., Woods, S. W., Srihari, V. H., & Annamalai, A. (2016).
Antipsychotic‐induced weight gain in first‐episode psychosis patients: a meta‐analysis of
differential effects of antipsychotic medications. Early intervention in psychiatry, 10(3),
193-202. ttps://doi.org/10.1111/eip.12251
Urden, L. D., Stacy, K. M., & Lough, M. E. (2017). Critical care nursing: diagnosis and
management. Elsevier Health Sciences.
Vancampfort, D., Stubbs, B., Mitchell, A. J., De Hert, M., Wampers, M., Ward, P. B., ... &
Correll, C. U. (2015). Risk of metabolic syndrome and its components in people with
schizophrenia and related psychotic disorders, bipolar disorder and major depressive
disorder: a systematic review and meta‐analysis. World Psychiatry, 14(3), 339-347.
https://doi.org/10.1002/wps.20252
White, J., Gray, R. J., Swift, L., Barton, G. R., & Jones, M. (2011). The serious mental illness
health improvement profile [HIP]: study protocol for a cluster randomised controlled
trial. Trials, 12(1), 167. https://doi.org/10.1186/1745-6215-12-167
Yogaratnam, J., Biswas, N., Vadivel, R., & Jacob, R. (2017). Metabolic complications of
schizophrenia and antipsychotic medications--an updated review. URI: https://open-
access.imh.com.sg/handle/123456789/4690
14
NURSING
Appendix 1
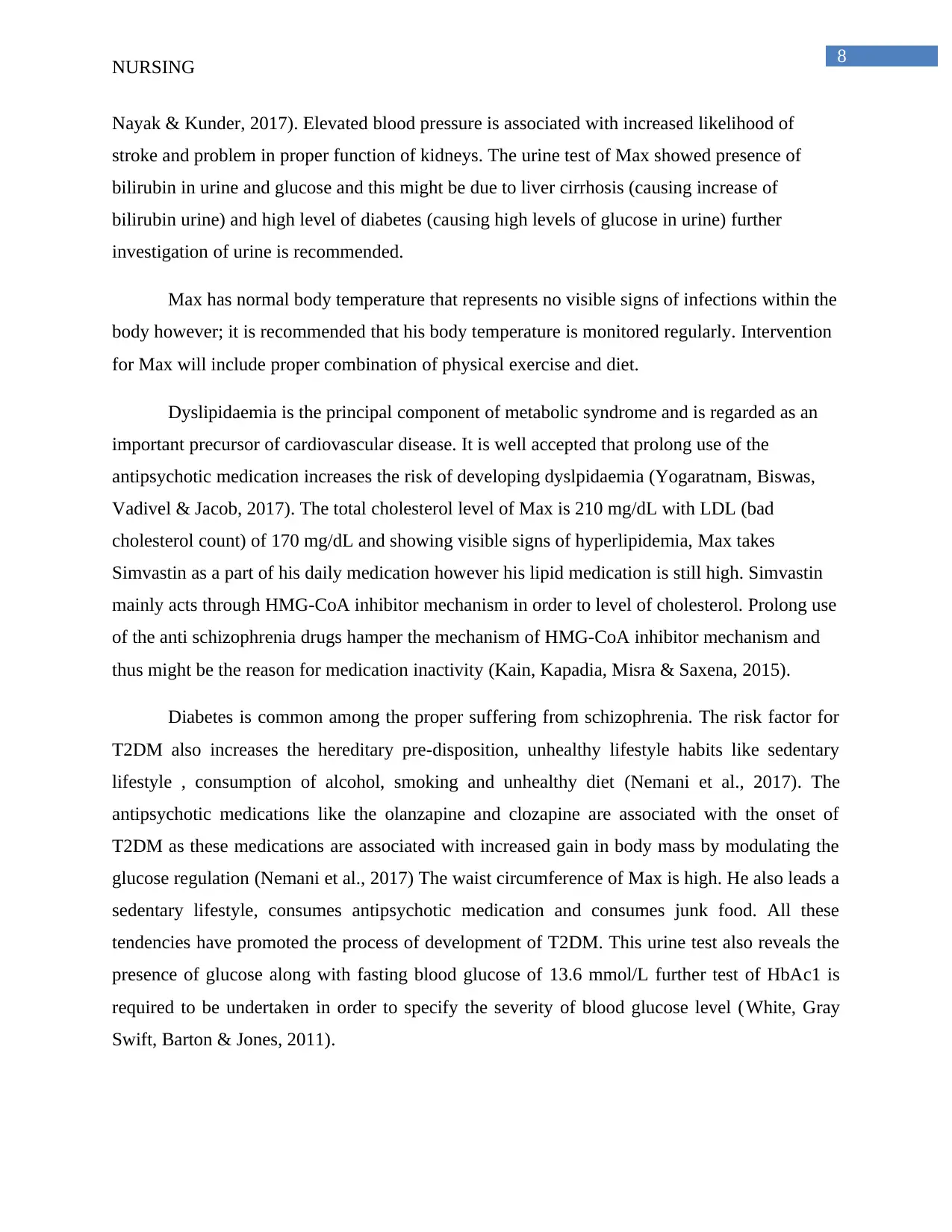
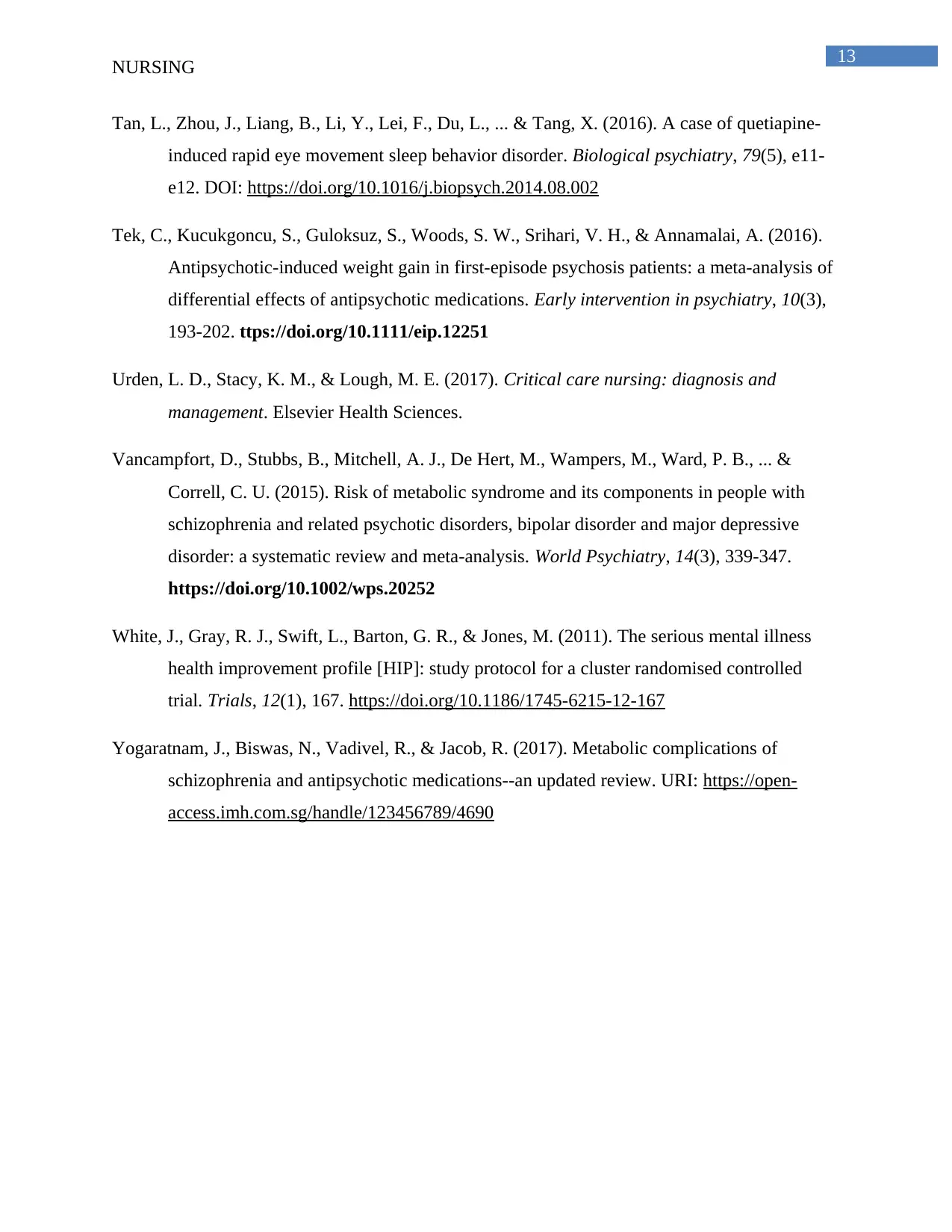
Table of finding and recommendations (Colour coded)
NURSING
Appendix 1
Table of finding and recommendations (Colour coded)
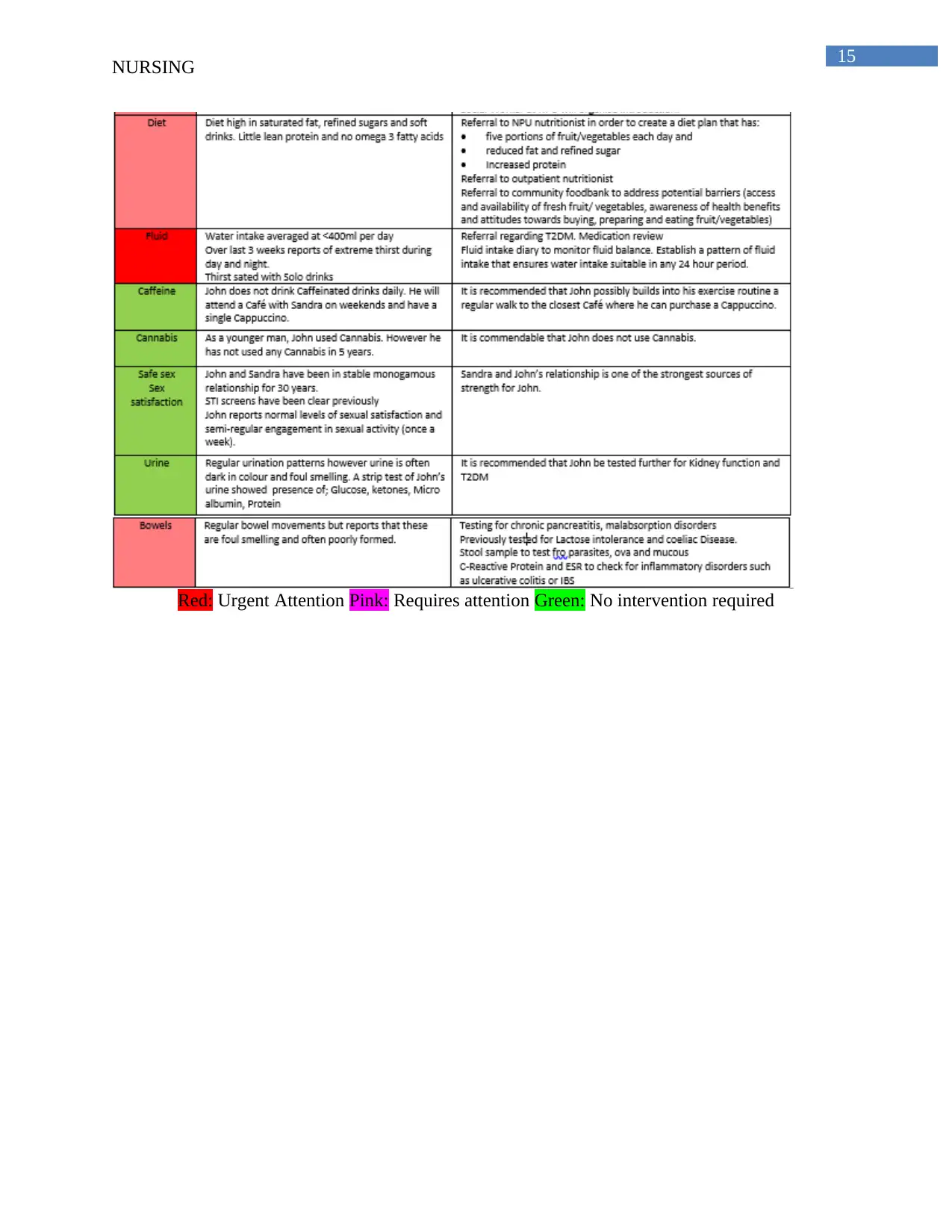
15
NURSING
Red: Urgent Attention Pink: Requires attention Green: No intervention required
NURSING
Red: Urgent Attention Pink: Requires attention Green: No intervention required
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




