Post-Operative Care: Nursing Care Plan, Critical Analysis, and Discharge Plan
VerifiedAdded on 2023/06/07
|12
|3048
|325
AI Summary
This essay focuses on a case study of patient Eleanor Wilson, who underwent a right hemicolectomy under general anesthesia. The essay will focus on formulating the care plan for the patient for the next 24 hours. Secondly, a critical analysis of the patient condition postoperatively. Lastly, a discharge plan for the patient.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running Header: POST-OPERATIVE CARE 1
POST-OPERATIVE CARE
Student’s name
Institutional Affiliation
Course code
Date.
POST-OPERATIVE CARE
Student’s name
Institutional Affiliation
Course code
Date.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
POST-OPERATIVE CARE 2
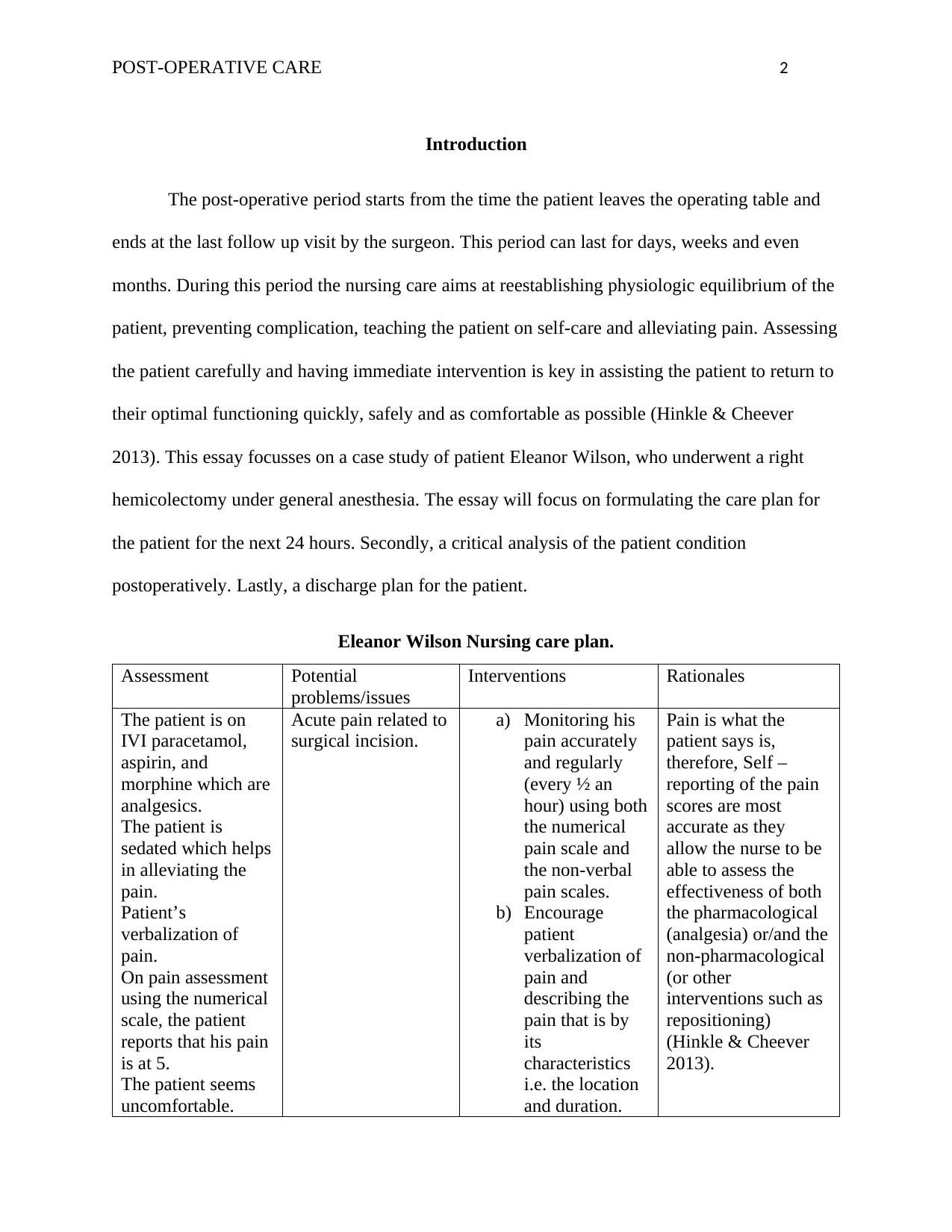
Introduction
The post-operative period starts from the time the patient leaves the operating table and
ends at the last follow up visit by the surgeon. This period can last for days, weeks and even
months. During this period the nursing care aims at reestablishing physiologic equilibrium of the
patient, preventing complication, teaching the patient on self-care and alleviating pain. Assessing
the patient carefully and having immediate intervention is key in assisting the patient to return to
their optimal functioning quickly, safely and as comfortable as possible (Hinkle & Cheever
2013). This essay focusses on a case study of patient Eleanor Wilson, who underwent a right
hemicolectomy under general anesthesia. The essay will focus on formulating the care plan for
the patient for the next 24 hours. Secondly, a critical analysis of the patient condition
postoperatively. Lastly, a discharge plan for the patient.
Eleanor Wilson Nursing care plan.
Assessment Potential
problems/issues
Interventions Rationales
The patient is on
IVI paracetamol,
aspirin, and
morphine which are
analgesics.
The patient is
sedated which helps
in alleviating the
pain.
Patient’s
verbalization of
pain.
On pain assessment
using the numerical
scale, the patient
reports that his pain
is at 5.
The patient seems
uncomfortable.
Acute pain related to
surgical incision.
a) Monitoring his
pain accurately
and regularly
(every ½ an
hour) using both
the numerical
pain scale and
the non-verbal
pain scales.
b) Encourage
patient
verbalization of
pain and
describing the
pain that is by
its
characteristics
i.e. the location
and duration.
Pain is what the
patient says is,
therefore, Self –
reporting of the pain
scores are most
accurate as they
allow the nurse to be
able to assess the
effectiveness of both
the pharmacological
(analgesia) or/and the
non-pharmacological
(or other
interventions such as
repositioning)
(Hinkle & Cheever
2013).
Introduction
The post-operative period starts from the time the patient leaves the operating table and
ends at the last follow up visit by the surgeon. This period can last for days, weeks and even
months. During this period the nursing care aims at reestablishing physiologic equilibrium of the
patient, preventing complication, teaching the patient on self-care and alleviating pain. Assessing
the patient carefully and having immediate intervention is key in assisting the patient to return to
their optimal functioning quickly, safely and as comfortable as possible (Hinkle & Cheever
2013). This essay focusses on a case study of patient Eleanor Wilson, who underwent a right
hemicolectomy under general anesthesia. The essay will focus on formulating the care plan for
the patient for the next 24 hours. Secondly, a critical analysis of the patient condition
postoperatively. Lastly, a discharge plan for the patient.
Eleanor Wilson Nursing care plan.
Assessment Potential
problems/issues
Interventions Rationales
The patient is on
IVI paracetamol,
aspirin, and
morphine which are
analgesics.
The patient is
sedated which helps
in alleviating the
pain.
Patient’s
verbalization of
pain.
On pain assessment
using the numerical
scale, the patient
reports that his pain
is at 5.
The patient seems
uncomfortable.
Acute pain related to
surgical incision.
a) Monitoring his
pain accurately
and regularly
(every ½ an
hour) using both
the numerical
pain scale and
the non-verbal
pain scales.
b) Encourage
patient
verbalization of
pain and
describing the
pain that is by
its
characteristics
i.e. the location
and duration.
Pain is what the
patient says is,
therefore, Self –
reporting of the pain
scores are most
accurate as they
allow the nurse to be
able to assess the
effectiveness of both
the pharmacological
(analgesia) or/and the
non-pharmacological
(or other
interventions such as
repositioning)
(Hinkle & Cheever
2013).
POST-OPERATIVE CARE 3
The patient
localizes hi pain at
the incision site.
c) Use of the
pharmacological
interventions to
relieve the pain.
This includes
the use of
analgesics.
d) Use of the non-
pharmacological
interventions to
relieve pain
which includes;
proper
positioning and
distractions.
Poor management of
pain can lead to
complications in the
post-operative phase
such as a poor cough,
vasoconstriction, and
inadequate lung
expansion may lead
to atelectasis and
retention of
secretions. (Hinkle &
Cheever 2013).
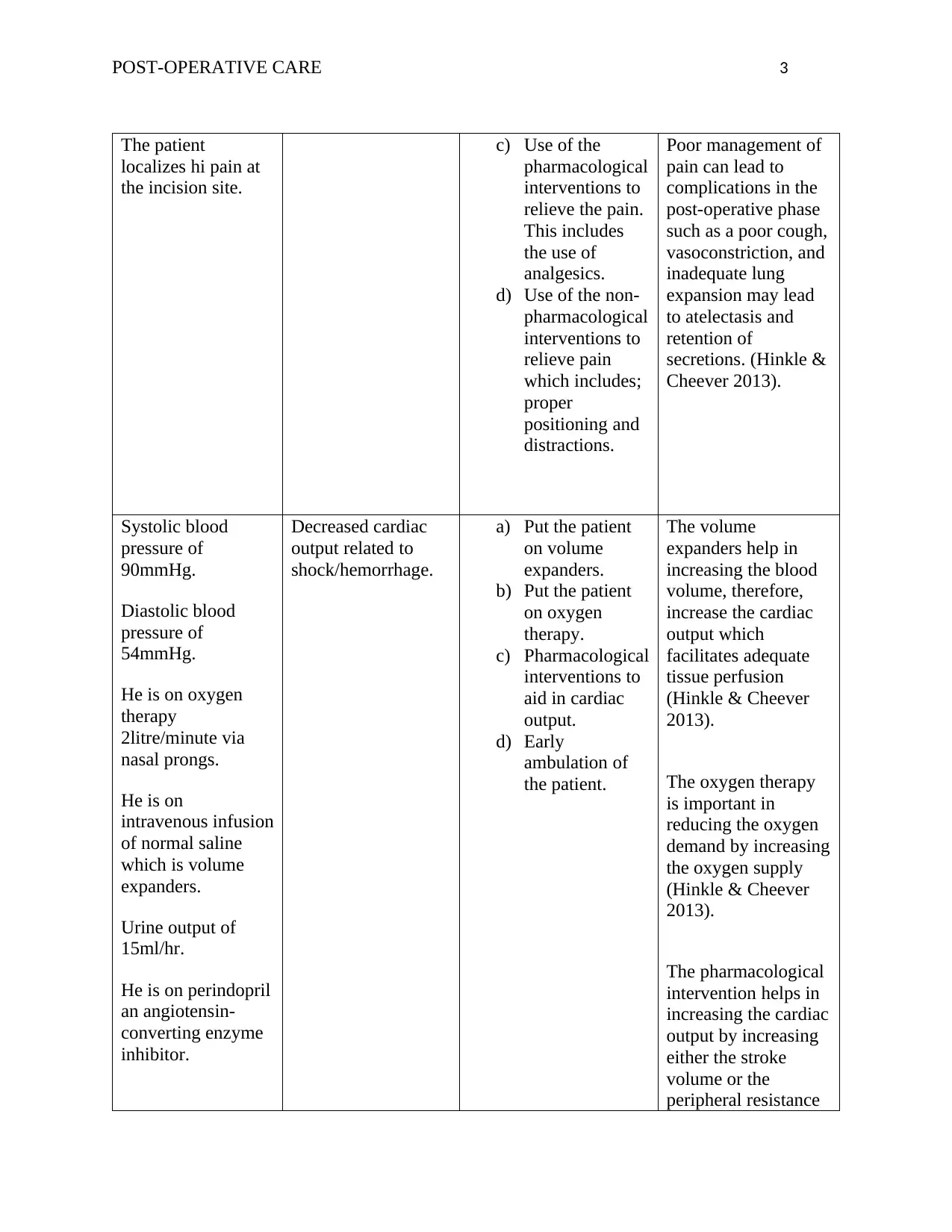
Systolic blood
pressure of
90mmHg.
Diastolic blood
pressure of
54mmHg.
He is on oxygen
therapy
2litre/minute via
nasal prongs.
He is on
intravenous infusion
of normal saline
which is volume
expanders.
Urine output of
15ml/hr.
He is on perindopril
an angiotensin-
converting enzyme
inhibitor.
Decreased cardiac
output related to
shock/hemorrhage.
a) Put the patient
on volume
expanders.
b) Put the patient
on oxygen
therapy.
c) Pharmacological
interventions to
aid in cardiac
output.
d) Early
ambulation of
the patient.
The volume
expanders help in
increasing the blood
volume, therefore,
increase the cardiac
output which
facilitates adequate
tissue perfusion
(Hinkle & Cheever
2013).
The oxygen therapy
is important in
reducing the oxygen
demand by increasing
the oxygen supply
(Hinkle & Cheever
2013).
The pharmacological
intervention helps in
increasing the cardiac
output by increasing
either the stroke
volume or the
peripheral resistance
The patient
localizes hi pain at
the incision site.
c) Use of the
pharmacological
interventions to
relieve the pain.
This includes
the use of
analgesics.
d) Use of the non-
pharmacological
interventions to
relieve pain
which includes;
proper
positioning and
distractions.
Poor management of
pain can lead to
complications in the
post-operative phase
such as a poor cough,
vasoconstriction, and
inadequate lung
expansion may lead
to atelectasis and
retention of
secretions. (Hinkle &
Cheever 2013).
Systolic blood
pressure of
90mmHg.
Diastolic blood
pressure of
54mmHg.
He is on oxygen
therapy
2litre/minute via
nasal prongs.
He is on
intravenous infusion
of normal saline
which is volume
expanders.
Urine output of
15ml/hr.
He is on perindopril
an angiotensin-
converting enzyme
inhibitor.
Decreased cardiac
output related to
shock/hemorrhage.
a) Put the patient
on volume
expanders.
b) Put the patient
on oxygen
therapy.
c) Pharmacological
interventions to
aid in cardiac
output.
d) Early
ambulation of
the patient.
The volume
expanders help in
increasing the blood
volume, therefore,
increase the cardiac
output which
facilitates adequate
tissue perfusion
(Hinkle & Cheever
2013).
The oxygen therapy
is important in
reducing the oxygen
demand by increasing
the oxygen supply
(Hinkle & Cheever
2013).
The pharmacological
intervention helps in
increasing the cardiac
output by increasing
either the stroke
volume or the
peripheral resistance
POST-OPERATIVE CARE 4
(Hinkle & Cheever
2013).
.
Early ambulation is
important as it helps
in venous return
preventing
complications
(Hinkle & Cheever
2013).
.
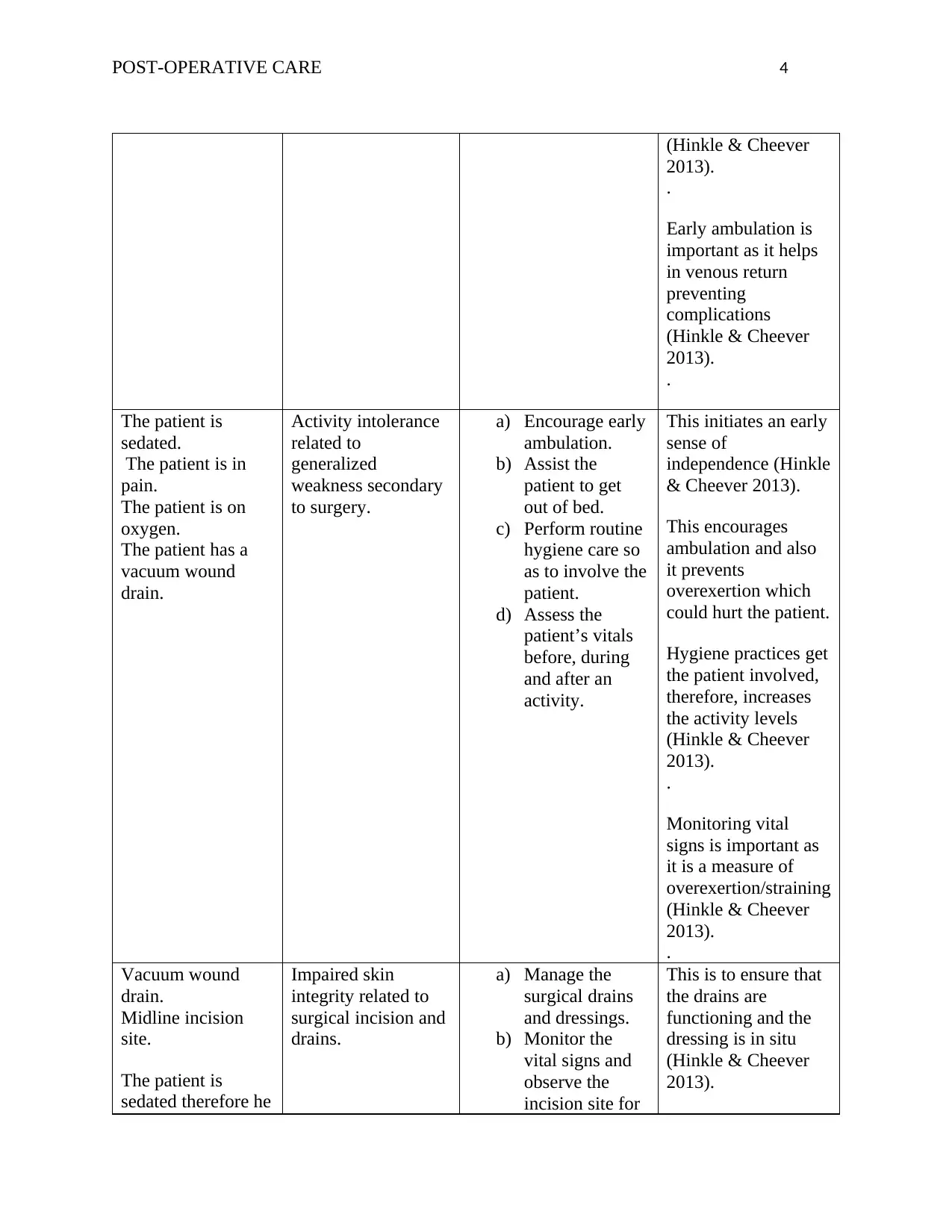
The patient is
sedated.
The patient is in
pain.
The patient is on
oxygen.
The patient has a
vacuum wound
drain.
Activity intolerance
related to
generalized
weakness secondary
to surgery.
a) Encourage early
ambulation.
b) Assist the
patient to get
out of bed.
c) Perform routine
hygiene care so
as to involve the
patient.
d) Assess the
patient’s vitals
before, during
and after an
activity.
This initiates an early
sense of
independence (Hinkle
& Cheever 2013).
This encourages
ambulation and also
it prevents
overexertion which
could hurt the patient.
Hygiene practices get
the patient involved,
therefore, increases
the activity levels
(Hinkle & Cheever
2013).
.
Monitoring vital
signs is important as
it is a measure of
overexertion/straining
(Hinkle & Cheever
2013).
.
Vacuum wound
drain.
Midline incision
site.
The patient is
sedated therefore he
Impaired skin
integrity related to
surgical incision and
drains.
a) Manage the
surgical drains
and dressings.
b) Monitor the
vital signs and
observe the
incision site for
This is to ensure that
the drains are
functioning and the
dressing is in situ
(Hinkle & Cheever
2013).
(Hinkle & Cheever
2013).
.
Early ambulation is
important as it helps
in venous return
preventing
complications
(Hinkle & Cheever
2013).
.
The patient is
sedated.
The patient is in
pain.
The patient is on
oxygen.
The patient has a
vacuum wound
drain.
Activity intolerance
related to
generalized
weakness secondary
to surgery.
a) Encourage early
ambulation.
b) Assist the
patient to get
out of bed.
c) Perform routine
hygiene care so
as to involve the
patient.
d) Assess the
patient’s vitals
before, during
and after an
activity.
This initiates an early
sense of
independence (Hinkle
& Cheever 2013).
This encourages
ambulation and also
it prevents
overexertion which
could hurt the patient.
Hygiene practices get
the patient involved,
therefore, increases
the activity levels
(Hinkle & Cheever
2013).
.
Monitoring vital
signs is important as
it is a measure of
overexertion/straining
(Hinkle & Cheever
2013).
.
Vacuum wound
drain.
Midline incision
site.
The patient is
sedated therefore he
Impaired skin
integrity related to
surgical incision and
drains.
a) Manage the
surgical drains
and dressings.
b) Monitor the
vital signs and
observe the
incision site for
This is to ensure that
the drains are
functioning and the
dressing is in situ
(Hinkle & Cheever
2013).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
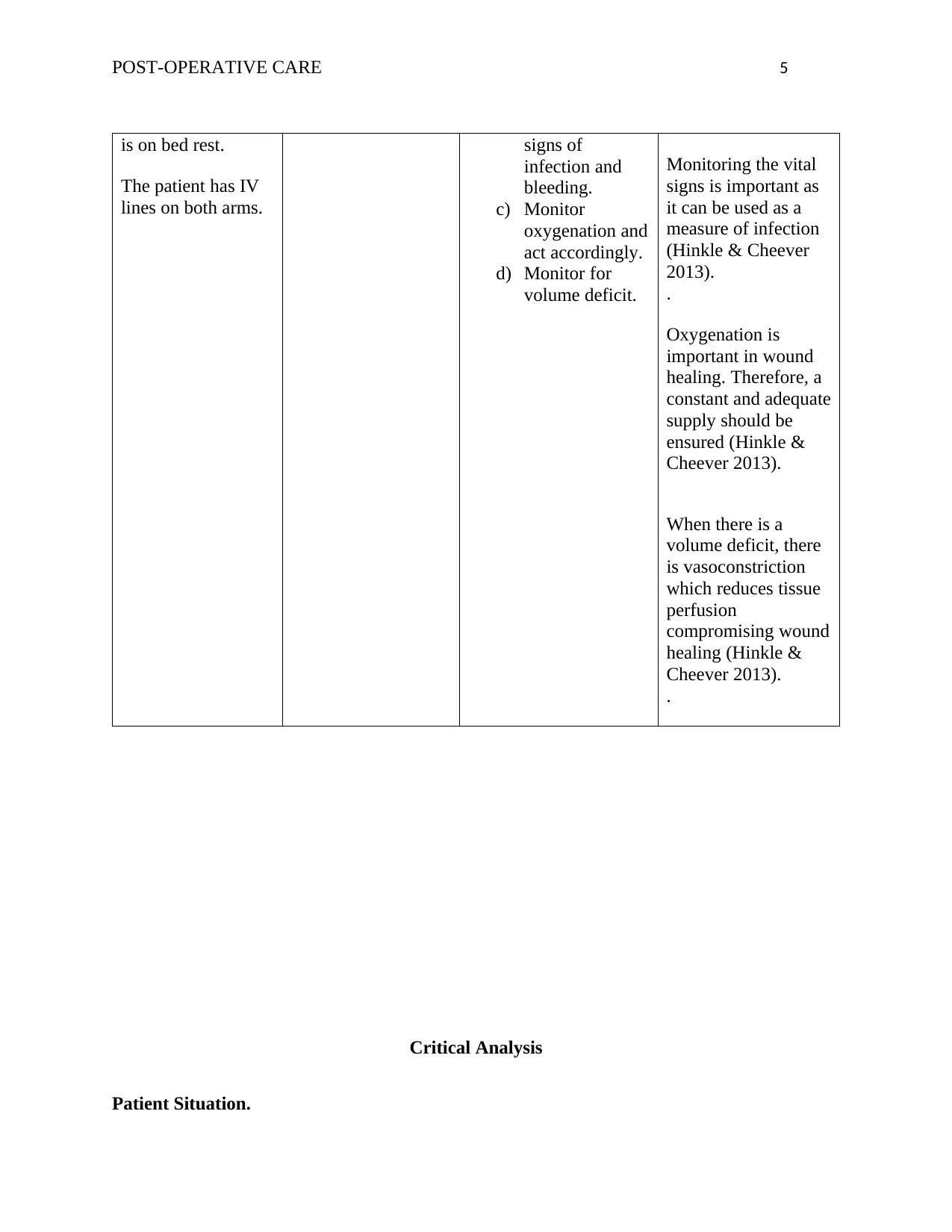
POST-OPERATIVE CARE 5
is on bed rest.
The patient has IV
lines on both arms.
signs of
infection and
bleeding.
c) Monitor
oxygenation and
act accordingly.
d) Monitor for
volume deficit.
Monitoring the vital
signs is important as
it can be used as a
measure of infection
(Hinkle & Cheever
2013).
.
Oxygenation is
important in wound
healing. Therefore, a
constant and adequate
supply should be
ensured (Hinkle &
Cheever 2013).
When there is a
volume deficit, there
is vasoconstriction
which reduces tissue
perfusion
compromising wound
healing (Hinkle &
Cheever 2013).
.
Critical Analysis
Patient Situation.
is on bed rest.
The patient has IV
lines on both arms.
signs of
infection and
bleeding.
c) Monitor
oxygenation and
act accordingly.
d) Monitor for
volume deficit.
Monitoring the vital
signs is important as
it can be used as a
measure of infection
(Hinkle & Cheever
2013).
.
Oxygenation is
important in wound
healing. Therefore, a
constant and adequate
supply should be
ensured (Hinkle &
Cheever 2013).
When there is a
volume deficit, there
is vasoconstriction
which reduces tissue
perfusion
compromising wound
healing (Hinkle &
Cheever 2013).
.
Critical Analysis
Patient Situation.
POST-OPERATIVE CARE 6
Patient Eleanor Wilson manifestations point to hypovolemic shock. Shock is a medical
emergency. The systemic blood pressure is inadequate to effectively deliver nutrients and
oxygen for the support of the cellular functioning and for the vital organs. This is a life-
threatening condition. When there is inadequate blood flow there is inadequate tissue perfusion
as the tissues receive inadequate oxygen and nutrients. This causes cellular starvation which
translates to cell death. This cell death further causes organ dysfunction which progresses to
organ failure and eventually causing death (Hinkle & Cheever 2013).
The patient is at the third stage of hypovolemic shock, the progressive stage. This is as a
result of the mechanisms that regulate blood pressure being unable to compensate. the patient’s
systolic pressure is 90mmHg, the diastolic blood pressure is 54mmH, heart rate of 88 beats per
minute, respiration rate of 12 breaths/minute, oxygen saturation of 96%, temperatures of 36’ C
and a urine output of 15-20mls/hour. This is as a result of heart dysfunctional which results from
being overworked and the inability of the body to meet the oxygen demand which translates to
ischemia and myocardial depression as a result of overly produced biochemical mediators. This
leads to cardiac pump failure even if the shock does not originate from the cardiac (Lewis,
Dirksen & McLean 2013). In addition to this, there is increased capillary permeability as a result
of the failure of the microcirculation autoregulatory function as a result of its response to the
numerous biochemical mediators released by the cells. Worsening the condition are areas of
arteriolar and venous constriction that further compromises perfusion. At this phase, the patient’s
prognosis of worsens. There is a relaxation of the precapillary sphincters which causes the
capillaries to leak fluid and this causes interstitial edema and reduces the hearts pre-load (Glynn
& Drake 2014).
Patient Eleanor Wilson manifestations point to hypovolemic shock. Shock is a medical
emergency. The systemic blood pressure is inadequate to effectively deliver nutrients and
oxygen for the support of the cellular functioning and for the vital organs. This is a life-
threatening condition. When there is inadequate blood flow there is inadequate tissue perfusion
as the tissues receive inadequate oxygen and nutrients. This causes cellular starvation which
translates to cell death. This cell death further causes organ dysfunction which progresses to
organ failure and eventually causing death (Hinkle & Cheever 2013).
The patient is at the third stage of hypovolemic shock, the progressive stage. This is as a
result of the mechanisms that regulate blood pressure being unable to compensate. the patient’s
systolic pressure is 90mmHg, the diastolic blood pressure is 54mmH, heart rate of 88 beats per
minute, respiration rate of 12 breaths/minute, oxygen saturation of 96%, temperatures of 36’ C
and a urine output of 15-20mls/hour. This is as a result of heart dysfunctional which results from
being overworked and the inability of the body to meet the oxygen demand which translates to
ischemia and myocardial depression as a result of overly produced biochemical mediators. This
leads to cardiac pump failure even if the shock does not originate from the cardiac (Lewis,
Dirksen & McLean 2013). In addition to this, there is increased capillary permeability as a result
of the failure of the microcirculation autoregulatory function as a result of its response to the
numerous biochemical mediators released by the cells. Worsening the condition are areas of
arteriolar and venous constriction that further compromises perfusion. At this phase, the patient’s
prognosis of worsens. There is a relaxation of the precapillary sphincters which causes the
capillaries to leak fluid and this causes interstitial edema and reduces the hearts pre-load (Glynn
& Drake 2014).
POST-OPERATIVE CARE 7
Patient’s Eleanor’s Co-morbidities.
Patient Eleanor has a history of myocardial infarction and hypercholesterolemia which
was diagnosed in the year 2007 with stenting on the left coronary artery. He smokes two
cigarettes daily and he has a familial history of bowel cancer as his father died of bowel cancer.
The above predisposes him to a cardiac event. The patient was put on general anesthesia, which
predisposed him to hemodynamic instability and cardiac depression (Barrett, Barman & Boitano,
2017). In addition to this, the anesthesia has a vasodilatory effect that further worsens the
hypotension and also has a negative inotropy. The effects of the surgery in an additive to the
anesthesia adversely affects the cardiovascular system through; blood loss, hypothermia, and
myocardial ischemia. Considering that the patient is hypertensive and has a history of MI this
threatens the wellbeing of the patient (Reed, Pearson, Douglas, Swinburne and Wilding, 2012).
Potential Clinical complication.
As mentioned above, his smoking habit, his history of MI, his cholesterol levels, he is
anemic, his hypertension when combined with the surgery effects and the general anesthesia
effects. This predisposes him to hypotension and hypovolemic shock. Hypotension arises from
the blood lost during surgery (Colledge, Walker & Ralston, 2013). Secondly, from the effects of
the general anesthesia which causes hemodynamic instabilities, depresses the cardiac functioning
and causes vasodilation which worsens the hypotension. Lastly, from his anemia, his hemoglobin
levels, hematocrit, and erythrocyte count is very low. The hypovolemic shock results from the
inadequacy to perfuse the tissues which result from hypotension (Ackley, Ladwig & Makic,
2016).
Nursing Intervention.
Patient’s Eleanor’s Co-morbidities.
Patient Eleanor has a history of myocardial infarction and hypercholesterolemia which
was diagnosed in the year 2007 with stenting on the left coronary artery. He smokes two
cigarettes daily and he has a familial history of bowel cancer as his father died of bowel cancer.
The above predisposes him to a cardiac event. The patient was put on general anesthesia, which
predisposed him to hemodynamic instability and cardiac depression (Barrett, Barman & Boitano,
2017). In addition to this, the anesthesia has a vasodilatory effect that further worsens the
hypotension and also has a negative inotropy. The effects of the surgery in an additive to the
anesthesia adversely affects the cardiovascular system through; blood loss, hypothermia, and
myocardial ischemia. Considering that the patient is hypertensive and has a history of MI this
threatens the wellbeing of the patient (Reed, Pearson, Douglas, Swinburne and Wilding, 2012).
Potential Clinical complication.
As mentioned above, his smoking habit, his history of MI, his cholesterol levels, he is
anemic, his hypertension when combined with the surgery effects and the general anesthesia
effects. This predisposes him to hypotension and hypovolemic shock. Hypotension arises from
the blood lost during surgery (Colledge, Walker & Ralston, 2013). Secondly, from the effects of
the general anesthesia which causes hemodynamic instabilities, depresses the cardiac functioning
and causes vasodilation which worsens the hypotension. Lastly, from his anemia, his hemoglobin
levels, hematocrit, and erythrocyte count is very low. The hypovolemic shock results from the
inadequacy to perfuse the tissues which result from hypotension (Ackley, Ladwig & Makic,
2016).
Nursing Intervention.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
POST-OPERATIVE CARE 8
The potential complications include; hypotension and hypovolemic shock. As mentioned
above, the shock is a life-threatening condition. To avoid the patient condition from
deteriorating, the following nursing interventions should be put into consideration: put the
patient on fluid therapy and vasoactive agents (Tisherman et al., 2015). These interventions aim
at reducing the oxygen and nutrients demand by increasing the oxygen and nutrients supply. This
will be achieved through the increased intravascular volume that is achieved by increasing the
oncotic pressure by giving them colloid infusions. Lastly, to increase the cardiac output the vaso-
active agents should be used so as to increase the heart contractility and the heart rate (de Nadal,
Pérez-Hoyos, Montejo-González, Pearse & Aldecoa, 2018).
Discharge plan
Effective discharge plan.
A discharge from the hospital is a process not a solitary/ isolated event. It should involve
formulating and implementing a plan/strategy so as to aid in the transfer of a patient/client from
the hospital setting to the most appropriate setting. For the effectiveness of the discharge plan,
the client and the client’s caregivers should participate in the process. They need to be updated
and informed on the patient’s care of plan regularly. It is an ongoing process which begins before
admission. Lastly, for both an effective and timely discharge, availability of alternatives and
appropriate care intervention/options so as to ensure rehabilitation, a continuation of health,
recuperation, and the social care needs can be identified and met (Sandy, 2010).
Discharge plan for patient Eleanor Wilson.
Patient Eleanor Wilson underwent a hemicolectomy due to an adenocarcinoma of the
ascending colon that had poorly differentiated and had lymph node metastasis. The procedure
The potential complications include; hypotension and hypovolemic shock. As mentioned
above, the shock is a life-threatening condition. To avoid the patient condition from
deteriorating, the following nursing interventions should be put into consideration: put the
patient on fluid therapy and vasoactive agents (Tisherman et al., 2015). These interventions aim
at reducing the oxygen and nutrients demand by increasing the oxygen and nutrients supply. This
will be achieved through the increased intravascular volume that is achieved by increasing the
oncotic pressure by giving them colloid infusions. Lastly, to increase the cardiac output the vaso-
active agents should be used so as to increase the heart contractility and the heart rate (de Nadal,
Pérez-Hoyos, Montejo-González, Pearse & Aldecoa, 2018).
Discharge plan
Effective discharge plan.
A discharge from the hospital is a process not a solitary/ isolated event. It should involve
formulating and implementing a plan/strategy so as to aid in the transfer of a patient/client from
the hospital setting to the most appropriate setting. For the effectiveness of the discharge plan,
the client and the client’s caregivers should participate in the process. They need to be updated
and informed on the patient’s care of plan regularly. It is an ongoing process which begins before
admission. Lastly, for both an effective and timely discharge, availability of alternatives and
appropriate care intervention/options so as to ensure rehabilitation, a continuation of health,
recuperation, and the social care needs can be identified and met (Sandy, 2010).
Discharge plan for patient Eleanor Wilson.
Patient Eleanor Wilson underwent a hemicolectomy due to an adenocarcinoma of the
ascending colon that had poorly differentiated and had lymph node metastasis. The procedure
POST-OPERATIVE CARE 9
entailed a midline incision with a closed dressed that is not supposed to be dressed until the
surgeon reviews it. Currently, the patient is on IV fluids and medication and oxygen therapy.
One of the principles in discharge planning is that unnecessary admissions should be avoided
therefore the patient should be discharged as early as he is clinically stable and can perform some
level of daily living activities. Secondly, the family should be involved in every step of
formulating the discharge plan for it to be effective (Guo & DiPietro, 2010).
On discharge, the following should be put into consideration; firstly, there should be pain
management intervention plan. the patient underwent an open surgery and pain anticipated. To
ensure that the patient’s comfort is achieved, he should be sent home with a prescription of
analgesics. He should also be instructed that in case of severe pain or if the pain worsens he
should come back (Conway, 2012). Secondly, on wound healing, as he has a midline incision,
the following instructions should be given; for wound dressing, a health professional should be
the one to do it. The patient should continue with the prescribed antibiotics to avoid wound
infection. The patient should understand that a hard lumpy feeling on the wound, itchiness,
numbness, and tingling are a normal sensation in wound healing (Jaganathan, Conway &
Dunlap, 2017). Thirdly, on the diet, the patient should take a balanced diet to enhance wound
healing. The patient should also ensure that he takes plenty of water and low fiber foods as they
slow down the bowel movement which helps in preventing injury to the colon. Fourthly, on
bathing and showering, the patient should avoid soaking the wound while showering. Fifthly, on
exercising and activities, the patient should perform daily activities that are gentle to help in
building the muscle strength. The patient should avoid bending, stretching and lifting for the first
few weeks (Thiele, 2015). Sixthly, there should be follow-up after 2-3weeks in the outpatient
department by the colorectal cancer nurse. Lastly, the patient should report to the healthcare
entailed a midline incision with a closed dressed that is not supposed to be dressed until the
surgeon reviews it. Currently, the patient is on IV fluids and medication and oxygen therapy.
One of the principles in discharge planning is that unnecessary admissions should be avoided
therefore the patient should be discharged as early as he is clinically stable and can perform some
level of daily living activities. Secondly, the family should be involved in every step of
formulating the discharge plan for it to be effective (Guo & DiPietro, 2010).
On discharge, the following should be put into consideration; firstly, there should be pain
management intervention plan. the patient underwent an open surgery and pain anticipated. To
ensure that the patient’s comfort is achieved, he should be sent home with a prescription of
analgesics. He should also be instructed that in case of severe pain or if the pain worsens he
should come back (Conway, 2012). Secondly, on wound healing, as he has a midline incision,
the following instructions should be given; for wound dressing, a health professional should be
the one to do it. The patient should continue with the prescribed antibiotics to avoid wound
infection. The patient should understand that a hard lumpy feeling on the wound, itchiness,
numbness, and tingling are a normal sensation in wound healing (Jaganathan, Conway &
Dunlap, 2017). Thirdly, on the diet, the patient should take a balanced diet to enhance wound
healing. The patient should also ensure that he takes plenty of water and low fiber foods as they
slow down the bowel movement which helps in preventing injury to the colon. Fourthly, on
bathing and showering, the patient should avoid soaking the wound while showering. Fifthly, on
exercising and activities, the patient should perform daily activities that are gentle to help in
building the muscle strength. The patient should avoid bending, stretching and lifting for the first
few weeks (Thiele, 2015). Sixthly, there should be follow-up after 2-3weeks in the outpatient
department by the colorectal cancer nurse. Lastly, the patient should report to the healthcare
POST-OPERATIVE CARE 10
professional in case of: fever, nausea, vomiting, wound swelling/draining pus, trouble urinating,
coughing blood, chest pain, shortness of breath, severe pain, stitches coming off or/and being
unable to pass gas/bowel movement (Scarborough, Mantyh, Sun, & Migaly, 2015).
References
Ackley, B. J., Ladwig, G. B., & Makic, M. B. F. (2016). Nursing Diagnosis Handbook-E-Book:
An Evidence-Based Guide to Planning Care. Elsevier Health Sciences.
Barrett, E., Barman, M., Boitano, S. (2017). Burns. Ganong’s Review of Medical Physiology.
(24th ed). New York, N.Y: McGraw Hill Medical.
professional in case of: fever, nausea, vomiting, wound swelling/draining pus, trouble urinating,
coughing blood, chest pain, shortness of breath, severe pain, stitches coming off or/and being
unable to pass gas/bowel movement (Scarborough, Mantyh, Sun, & Migaly, 2015).
References
Ackley, B. J., Ladwig, G. B., & Makic, M. B. F. (2016). Nursing Diagnosis Handbook-E-Book:
An Evidence-Based Guide to Planning Care. Elsevier Health Sciences.
Barrett, E., Barman, M., Boitano, S. (2017). Burns. Ganong’s Review of Medical Physiology.
(24th ed). New York, N.Y: McGraw Hill Medical.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
POST-OPERATIVE CARE 11
Colledge, N., Walker, R, & Ralston, S. (2013). Colorectal. Davidson’s Principles and Practice
of Medicine. (21st ed). New York, N.Y: Edinburgh.
Conway, G., (2012). Effective Discharge Planning. In Short Stay Management of Acute Heart
Failure (pp. 207-215). Humana Press, Totowa, NJ. Retrieved 30/8/2018
https://link.springer.com/chapter/10.1007/978-1-61779-627-2_17
de Nadal, M., Pérez-Hoyos, S., Montejo-González, J. C., Pearse, R., & Aldecoa, C. (2018).
Intensive care admission and hospital mortality in the elderly after non-cardiac surgery.
Medicine intensive.
Glynn, M. & Drake, W. (2014). Colorectal. Hutchinson’s Clinical Methods: an integrated
approach to clinical practice. London: Elsevier.
Guo, S.A. and DiPietro, L.A., (2010). Factors affecting wound healing. Journal of dental
research, 89(3), pp.219-229. Retrieved 30/8/2018
http://journals.sagepub.com/doi/10.1177/0022034509359125
Hinkle, J.L, Cheever, K.H. (2013). Colorectal. Brunner and Saddarth’s Textbook of Medical and
Surgical Nursing, (13th ed) Philadelphia, PA: Wolters Kluwer Health/Lippincott
Williams & Wilkins.
Jaganathan, S.P., Conway, G. and Dunlap, S., (2017). Effective Discharge Planning. In Short
Stay Management of Acute Heart Failure (pp. 233-242). Humana Press, Cham Retrieved
30/8/2018 https://link.springer.com/chapter/10.1007/978-3-319-44006-4_18
Lewis, l., Dirksen, R., McLean, M., (2013) medical-surgical nursing: assessment and
management of clinical problems, 8th edition.
Colledge, N., Walker, R, & Ralston, S. (2013). Colorectal. Davidson’s Principles and Practice
of Medicine. (21st ed). New York, N.Y: Edinburgh.
Conway, G., (2012). Effective Discharge Planning. In Short Stay Management of Acute Heart
Failure (pp. 207-215). Humana Press, Totowa, NJ. Retrieved 30/8/2018
https://link.springer.com/chapter/10.1007/978-1-61779-627-2_17
de Nadal, M., Pérez-Hoyos, S., Montejo-González, J. C., Pearse, R., & Aldecoa, C. (2018).
Intensive care admission and hospital mortality in the elderly after non-cardiac surgery.
Medicine intensive.
Glynn, M. & Drake, W. (2014). Colorectal. Hutchinson’s Clinical Methods: an integrated
approach to clinical practice. London: Elsevier.
Guo, S.A. and DiPietro, L.A., (2010). Factors affecting wound healing. Journal of dental
research, 89(3), pp.219-229. Retrieved 30/8/2018
http://journals.sagepub.com/doi/10.1177/0022034509359125
Hinkle, J.L, Cheever, K.H. (2013). Colorectal. Brunner and Saddarth’s Textbook of Medical and
Surgical Nursing, (13th ed) Philadelphia, PA: Wolters Kluwer Health/Lippincott
Williams & Wilkins.
Jaganathan, S.P., Conway, G. and Dunlap, S., (2017). Effective Discharge Planning. In Short
Stay Management of Acute Heart Failure (pp. 233-242). Humana Press, Cham Retrieved
30/8/2018 https://link.springer.com/chapter/10.1007/978-3-319-44006-4_18
Lewis, l., Dirksen, R., McLean, M., (2013) medical-surgical nursing: assessment and
management of clinical problems, 8th edition.
POST-OPERATIVE CARE 12
Reed, J., Pearson, P., Douglas, B., Swinburne, S. and Wilding, H., (2012). Going home from the
hospital–an appreciative inquiry study. Health & social care in the community, 10(1),
pp.36-45. https://doi.org/10.1046/j.0966-0410.2001.00341.
Scarborough, J. E., Mantyh, C. R., Sun, Z., & Migaly, J. (2015). Combined mechanical and oral
antibiotic bowel preparation reduces incisional surgical site infection and anastomotic
leak rates after elective colorectal resection. Annals of surgery, 262(2), 331-337.
Thiele, R. H., Rea, K. M., Turrentine, F. E., Friel, C. M., Hassinger, T. E., Goudreau, B. J., ... &
McMurry, T. L. (2015). Standardization of care: the impact of an enhanced recovery
protocol on the length of stay, complications, and direct costs after colorectal surgery.
Journal of the American College of Surgeons, 220(4), 430-443.
Tisherman, S. A., Schmicker, R. H., Brasel, K. J., Bulger, E. M., Kerby, J. D., Minei, J. P., ... &
Schreiber, M. A. (2015). A detailed description of all deaths in both the shock and
traumatic brain injury hypertonic saline trials of the Resuscitation Outcomes Consortium.
Annals of surgery, 261(3), 586.
Reed, J., Pearson, P., Douglas, B., Swinburne, S. and Wilding, H., (2012). Going home from the
hospital–an appreciative inquiry study. Health & social care in the community, 10(1),
pp.36-45. https://doi.org/10.1046/j.0966-0410.2001.00341.
Scarborough, J. E., Mantyh, C. R., Sun, Z., & Migaly, J. (2015). Combined mechanical and oral
antibiotic bowel preparation reduces incisional surgical site infection and anastomotic
leak rates after elective colorectal resection. Annals of surgery, 262(2), 331-337.
Thiele, R. H., Rea, K. M., Turrentine, F. E., Friel, C. M., Hassinger, T. E., Goudreau, B. J., ... &
McMurry, T. L. (2015). Standardization of care: the impact of an enhanced recovery
protocol on the length of stay, complications, and direct costs after colorectal surgery.
Journal of the American College of Surgeons, 220(4), 430-443.
Tisherman, S. A., Schmicker, R. H., Brasel, K. J., Bulger, E. M., Kerby, J. D., Minei, J. P., ... &
Schreiber, M. A. (2015). A detailed description of all deaths in both the shock and
traumatic brain injury hypertonic saline trials of the Resuscitation Outcomes Consortium.
Annals of surgery, 261(3), 586.
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




